Assessing Nutritional Status and Frailty among Poor Elderly Individuals in Requena del Tapiche, Peru
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethical Approval and Consent to Participate
2.2. Variables and Rating Scales
2.2.1. Frailty Evaluation Using the Fried Assessment
2.2.2. Mini Nutritional Assessment Scale
2.2.3. Barthel Index
2.2.4. Timed Get up and Go Test
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Decade of Healthy Aging 2021–2030. Available online: https://www.who.int/es/initiatives/decade-of-healthy-ageing (accessed on 9 August 2023).
- Beard, J.R.; Officer, A.; de Carvalho, I.A.; Sadana, R.; Pot, A.M.; Michel, J.-P.; Lloyd-Sherlock, P.; Epping-Jordan, J.E.; Peeters, G.M.E.E.G.; Mahanani, W.R.; et al. The World report on ageing and health: A policy framework for healthy ageing. Lancet 2016, 387, 2145–2154. [Google Scholar] [CrossRef] [PubMed]
- Clegg, A.; Young, J.; Iliffe, S.; Rikkert, M.O.; Rockwood, K. Frailty in elderly people. Lancet 2013, 381, 752–762, Erratum in: Lancet 2013, 382, 1328. [Google Scholar] [CrossRef] [PubMed]
- Yanase, T.; Yanagita, I.; Muta, K.; Nawata, H. Frailty in elderly diabetes patients. Endocr. J. 2018, 65, 1–11. [Google Scholar] [CrossRef]
- Kane, A.E.; Howlett, S.E. Sex differences in frailty: Comparisons between humans and preclinical models. Mech. Ageing Dev. 2021, 198, 111546. [Google Scholar] [CrossRef]
- Del Portillo, R.C.; MiIla, S.P.; Váquez, N.G.; López, B.P.; López, L.B.; Serván, P.R.; García-Luna, P.P.; Gómez-Candela, C. Assessment of nutritional status in the healthcare setting in Spain. Nutr. Hosp. 2015, 31, 196–207. [Google Scholar] [CrossRef]
- Diekmann, R.; Winning, K.; Uter, W.; Kaiser, M.J.; Sieber, C.C.; Volkert, D.; Bauer, J.M. Screening for malnutrition among nursing home residents—A comparative analysis of the Mini Nutritional Assessment, the Nutritional Risk Screening, and the Malnutrition Universal Screening Tool. J. Nutr. Health Aging 2012, 17, 326–331. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in Older adults: Evidence for a phenotype. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef]
- Couso, M.R. Geriatric interventions in the older with cancer based on comprehensive geriatric assessment. Optimization areas: What the geriatrician can contribute to the multidisciplinar team. Nutr. Hosp. 2020, 34, 38–47. [Google Scholar] [CrossRef]
- Cortés, A.R.; Villarreal, E.; Galicia, L.; Martínez, L.; Vargas, E.R. Evaluación geriátrica integral del adulto mayor. Rev. Méd. Chile 2011, 139, 725–731. [Google Scholar] [CrossRef]
- Freedman, A.; Nicolle, J. Social isolation and loneliness: The new geriatric giants: Approach for primary care. Can. Fam. Physician 2020, 66, 176–182. [Google Scholar]
- Domènech-Abella, J.; Lara, E.; Rubio-Valera, M.; Olaya, B.; Moneta, M.V.; Rico-Uribe, L.A.; Ayuso-Mateos, J.L.; Mundó, J.; Haro, J.M. Loneliness and depression in the elderly: The role of social network. Soc. Psychiatry 2017, 52, 381–390. [Google Scholar] [CrossRef] [PubMed]
- United Nations. Addressing Poverty. Available online: https://www.un.org/en/academic-impact/addressing-poverty#:~:text=Nearly%20half%20of%20the%20world’s,than%20US%20%241.25%20a%20day (accessed on 21 August 2023).
- Instituto Nacional de Estadística e Informática (INEI). Envejecer en el Perú: Informe Sobre la Situación de las Personas Adultas Mayores; Defensoría del Pueblo: Lima, Peru, 2019; Available online: https://www.defensoria.gob.pe/wp-content/uploads/2019/08/DEFENSOR%C3%8DA-DEL-PUEBLO-INFORME-ENVEJECER-EN-EL-PER%C3%9A.pdf (accessed on 9 August 2023).
- Anaya, J.-M.; Rojas, M.; Salinas, M.L.; Rodríguez, Y.; Roa, G.; Lozano, M.; Rodríguez-Jiménez, M.; Montoya, N.; Zapata, E.; Monsalve, D.M.; et al. Post-COVID syndrome. A case series and comprehensive review. Autoimmun. Rev. 2021, 20, 102947. [Google Scholar] [CrossRef] [PubMed]
- Wanden-Berghe, C. Valoración geriátrica integral. Hosp. Domic. 2021, 5, 115. [Google Scholar] [CrossRef]
- Mudge, A.M.; Ross, L.J.; Young, A.M.; Isenring, E.A.; Banks, M.D. Helping understand nutritional gaps in the elderly (HUNGER): A prospective study of patient factors associated with inadequate nutritional intake in older medical inpatients. Clin. Nutr. 2011, 30, 320–325. [Google Scholar] [CrossRef] [PubMed]
- Hickman, I.; Tapsell, L. Evidence based practice guidelines for the nutritional management of malnutrition in adult patients across the continuum of care. Nutr. Diet. 2009, 66, S1–S34. [Google Scholar] [CrossRef]
- Kondrup, J.; Allison, S.P.; Elia, M.; Vellas, B.; Plauth, M.; Educational and Clinical Practice Committee, European Society of Par-enteral and Enteral Nutrition (ESPEN). ESPEN guidelines for nutrition screening 2002. Clin. Nutr. 2003, 22, 415–421. [Google Scholar] [CrossRef]
- Casanovas, A.S. The mini nutritional assessment. Twenty years contributing to nutritional assessment. Rev. Esp. Geriatr. Gerontol. 2012, 47, 245–246. [Google Scholar] [CrossRef]
- Triana, F.C.; González, C.R.; Martín, P.M. Valoración nutricional en el anciano. Med. Programa Form. Méd. Contin. Acreditado 2006, 9, 4037–4047. [Google Scholar] [CrossRef]
- De Luis, A.D.; Mongil, R.L.; Sagrado, M.G.; Trigo, J.A.L.; Mora, P.F.; Sanz, J.C.; Group NOVOMET. Evaluation of the mini-nutritional assessment short-form (MNA-SF) among institutionalized older patients in Spain. Nutr. Hosp. 2012, 26, 1350–1354. [Google Scholar] [CrossRef]
- Vellas, B.; Villars, H.; Abellan, G.; Soto, M.E.; Rolland, Y.; Guigoz, Y.; Morley, J.E.; Chumlea, W.; Salva, A.; Rubenstein, L.Z.; et al. Overview of the MNA®-Its history and challenges. J. Nutr. Health Aging 2006, 10, 456–465. [Google Scholar]
- Guigoz, Y. The Mini Nutritional Assessment (MNA) review of the literature—What does it tell us? J. Nutr. Health Aging 2006, 10, 466. [Google Scholar] [PubMed]
- Tarazona Santabalbina, F.J.; Belenguer Varea, A.; Doménech Pascual, J.R.; Gac Espínola, H.; Cuesta Peredo, D.; Medina Domínguez, L.; Salvador Pérez, M.I.; Avellana Zaragoza, J.A. Validation of MNA scale score as a nutritional risk factor in institutionalized geri-atric patients with moderate and severe cognitive impairment. Nutr. Hosp. 2009, 24, 724–731. [Google Scholar] [PubMed]
- Mahoney, F.I.; Barthel, D.W. Functional evaluation: The Barthel Index. Md. State Med. J. 1965, 14, 61–65. [Google Scholar] [PubMed]
- Aguarón, M.J.; Ricomà, R. Valoración Geriátrica Integral: Instrumentos de Valoración. In Enfermería de la Persona Mayor; Nuin, C., Ed.; Editorial Centro de Estudios Ramón Areces, S.A.: Madrid, Spain, 2011; pp. 157–173. [Google Scholar]
- Cabañero-Martínez, M.J.; Cabrero-García, J.; Richart-Martínez, M.; Muñoz-Mendoza, C.L. Structured review of activities of daily living measures in older people. Rev. Esp. Geriatr. Gerontol. 2008, 43, 271–283. [Google Scholar] [CrossRef] [PubMed]
- Trigás-Ferrín, M.; Ferreira-González, L.; Meijide-Míguez, H. Escalas de valoración funcional en el anciano. Galicia Clin. 2011, 72, 11–16. Available online: https://galiciaclinica.info/pdf/11/225.pdf (accessed on 9 August 2023).
- Gresham, G.E.; Phillips, T.F.; Labi, M.L. ADL status in stroke: Relative merits of three standard indexes. Arch. Phys. Med. Rehabil. 1980, 61, 355–358. [Google Scholar]
- Shah, S.; Vanclay, F.; Cooper, B. Improving the sensitivity of the Barthel Index for stroke rehabilitation. J. Clin. Epidemiol. 1989, 42, 703–709. [Google Scholar] [CrossRef]
- Wade, D.T.; Collin, C. The Barthel ADL Index: A standard measure of physical disability? Int. Disabil. Stud. 1988, 10, 64–67. [Google Scholar] [CrossRef]
- Stone, S.P.; Ali, B.; Auberleek, I.; Thompsell, A.; Young, A. The Barthel index in clinical practice: Use on a rehabilitation ward for elderly people. J. R. Coll. Physicians Lond. 1994, 28, 419–423. [Google Scholar]
- Wall, J.C.; Bell, C.; Campbell, S.; Davis, J. The Timed Get-up-and-Go test revisited: Measurement of the component tasks. J. Rehabil. Res. Dev. 2000, 37, 109–114. [Google Scholar]
- Otero, M.R.; Estrada, G.M.R. Valoración nutricional de las personas mayores de 60 años de la ciudad de pasto, colombia. Cienc. Enferm. 2017, 23, 23–34. [Google Scholar] [CrossRef]
- Restrepo, G.C.D.; Betancur, L.F.R.; Vargas, J.E.V.; Álvarez, D.V. Evaluación nutricional de adultos mayores con el Mini Nutritional Assessment: MNA. Univ. Salud 2016, 18, 494. [Google Scholar] [CrossRef]
- Giraldo Giraldo, N.A.; Paredes Arturo, Y.V.; Idarraga Idarraga, Y.; Aguirre Acevedo, D.C. Factores asociados a la desnutrición o al riesgo de desnutrición en adultos mayores de San Juan de Pasto, Colombia: Un estudio transversal. Rev. Esp. Nutr. Humana Diet. 2017, 21, 39–48. [Google Scholar] [CrossRef]
- Pereira ML, A.S.; de Almeida Moreira, P.; de Oliveira, C.C.; Roriz AK, C.; Amaral MT, R.; Mello, A.L.; Ramos, L.B. Nutritional status of institutionalized elderly Brazilians: A study with the Mini Nutritional Assessment. Nutr. Hosp. 2015, 31, 1198–1204. [Google Scholar] [CrossRef]
- Díaz Amador, Y. Evaluación de la funcionalidad y el grado de dependencia de adultos mayores de una Fundación para la Inclusión Social. Rev. Cuba. Enferm. 2020, 36, e3100. Available online: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0864-03192020000300005&lng=es (accessed on 9 August 2023).
- Cano-Gutiérrez, C.; Borda, M.G.; Reyes-Ortiz, C.; Arciniegas, A.J.; Samper-Ternent, R. Assessment of factors associated with functionality in older adults over 60 years in Bogotá, Colombia. Biomédica 2016, 37, 57–65. [Google Scholar] [CrossRef]
- Bayona Marzo, I.; Fernández de Santiago, F.J.; Martínez León, M.; Navas Cámara, F.J. La dependencia funcional del anciano institucionalizado valorada mediante el índice de Barthel. Gerokomos 2012, 23, 19–22. [Google Scholar] [CrossRef]
- Roqueta, C.; de Jaime, E.; Miralles, R.; Cervera, A.M. Experiencia en la evaluación del riesgo de caídas. Comparación entre el test de Tinetti y el Timed Up & Go. Rev. Esp. Geriatr. Gerontol. 2007, 42, 319–327. [Google Scholar] [CrossRef]
- Mora, A. Propiedades métricas del “timed get up and go versión modificada” en el riesgo de caídas en mujeres activas. Colomb. Méd. 2017, 48, 19–24. Available online: http://www.bioline.org.br/abstract?rc17007 (accessed on 9 August 2023).
- Mancilla, E.; Valenzuela, J.; Escobar, M. Rendimiento en las pruebas “Timed Up and Go” y “Estación Unipodal” en adultos mayores chilenos entre 60 y 89 años. Clin. Med. 2015, 143, 39–46. [Google Scholar] [CrossRef]
- Ugarte LL, J.; Vargas, F. Sensibilidad y especificidad de la prueba Timed Up and Go. Tiempos de corte y edad en adultos mayores. Rev. Méd. Chile 2021, 149, 1302–1310. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Action Plan on Physical Activity 2018–2030: More Active People for a Healthier World; World Health Organization: Geneva, Switzerland, 2018. Available online: http://apps.who.int/iris/bitstream/handle/10665/272722/9789241514187-eng.pdf (accessed on 9 August 2023).
- Sousa, M.; Dos Santos, T. Factores asociados al síndrome de fragilidad en ancianos residentes en área urbana. Rev. Lat. Am. Enferm. 2014, 22, 874–882. [Google Scholar] [CrossRef]
- Troncoso-Pantoja, C.; Concha-Cisternas, Y.; Leiva-Ordoñez, A.M.; Martínez-Sanguinetti, M.A.; Petermann-Rocha, F.; Díaz-Martínez, X.; Martorell, M.; Nazar, G.; Ulloa, N.; Cigarroa-Cuevas, I.; et al. Prevalencia de fragilidad en personas mayores de Chile: Resultados de la Encuesta Nacional de Salud 2016–2017. Rev. Méd. Chile 2020, 148, 1418–1426. [Google Scholar] [CrossRef] [PubMed]
- Herrera-Perez, D.; Soriano-Moreno, A.N.; Rodrigo-Gallardo, P.K.; Toro-Huamanchumo, C.J. Prevalencia del síndrome de fragilidad y factores asociados en adultos mayores. Rev. Cuba. Med. Gen. Integr. 2020, 36, e1098. Available online: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0864-21252020000200008&lng=es (accessed on 9 August 2023).
- Real, C.; Peralta, L. Todos los caminos conducen a la pérdida de masa muscular: Desnutrición, fragilidad, sarcopenia y caquexia. Diaeta 2021, 39, 45–58. Available online: http://www.scielo.org.ar/scielo.php?script=sci_arttext&pid=S1852-73372021000100045&lng=es (accessed on 9 August 2023).
- Menéndez-González, L.; Izaguirre-Riesgo, A.; Tranche-Iparraguirre, S.; Montero-Rodríguez, A.; Orts-Cortés, M.I. Prevalencia y factores asociados de fragilidad en adultos mayores de 70 años en la comunidad. Aten. Primaria 2021, 53, 102128. [Google Scholar] [CrossRef]
- Herrera, L.E.; Gómez, J.R. Situaciones de dependencia en personas mayores en las residencias de ancianos en España. Ene 2015, 9. [Google Scholar] [CrossRef]
| n (%) | |
|---|---|
| Sex | |
| Male | 27 (45.0) |
| Female | 33 (55.0) |
| District | |
| Prolongación Requenino | 4 (6.67) |
| Requena | 8 (13.34) |
| Nueva Requena | 7 (11.67) |
| Monopolio | 1 (1.67) |
| Vargas Guerra | 4 (6.67) |
| Jerusalem | 4 (6.67) |
| Aeropuerto | 2 (3.34) |
| San Pedro | 2 (3.34) |
| Jose Carlos Maria Tegui | 5 (8.34) |
| Padre Giner | 2 (3.34) |
| Pedrera | 2 (3.34) |
| Petroperu | 3 (5.00) |
| Emilio San Martin | 1 (1.67) |
| Sancho Roca | 3 (5.00) |
| Union | 2 (3.34) |
| Manaos | 1 (1.67) |
| Sargento Lores | 1 (1.67) |
| Independencia | 1 (1.67) |
| Avenida del ejército | 1 (1.67) |
| Ayacucho | 1 (1.67) |
| San Juan | 1 (1.67) |
| Pedroche | 1 (1.67) |
| Atenas | 2 (3.34) |
| Yanira | 1 (1.67) |
| Allergies | |
| Yes | 3 (5.00) |
| No | 57 (95.0) |
| Family history | |
| Yes | 16 (26.67) |
| No | 44 (73.33) |
| Hospitalization in the last five years | |
| Yes | 7 (11.67) |
| No | 53 (88.33) |
| General physical appearance | |
| Healthy | 25 (41.67) |
| Dirty–Poor condition | 12 (20.00) |
| Improvable | 12 (20.00) |
| Unkempt | 11 (18.33) |
| n (%) | |
|---|---|
| Frailty | 36 (60.0) |
| Male | 15 (25.0) |
| Female | 21 (35.0) |
| MNA | |
| Satisfactory nutritional status | 9 (15.0) |
| At risk of malnutrition | 29 (48.3) |
| Malnutrition | 22 (36.7) |
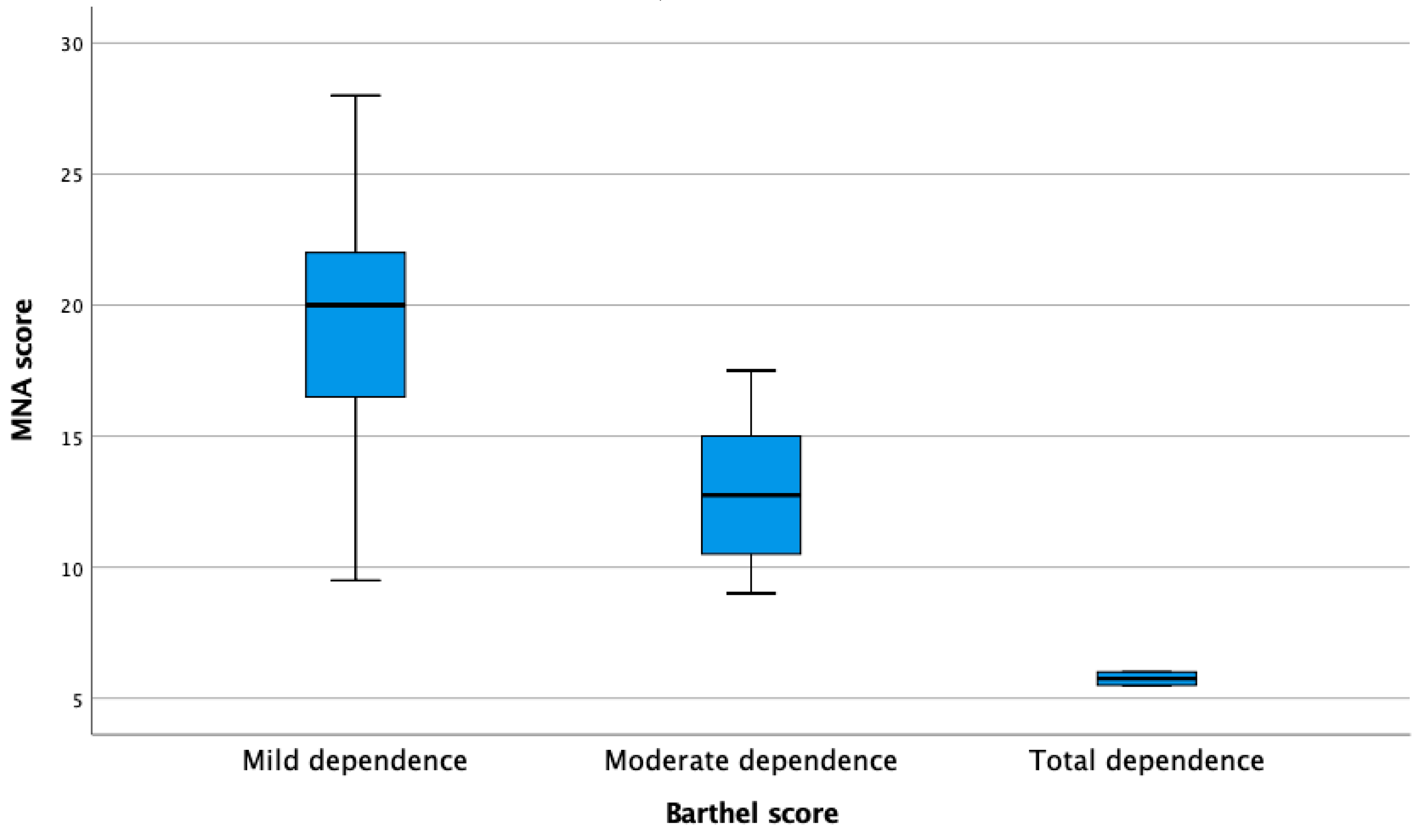
| Barthel | |
| Mild dependence | 52 (86.7) |
| Moderate dependence | 6 (10.0) |
| Total dependence | 2 (3.3) |
| Timed get up and go | |
| Normal | 25 (41.7) |
| Normal for frail people | 20 (33.3) |
| Needed assistance | 7 (11.7) |
| Could not perform | 8 (13.3) |
| No (n = 24) | Yes (n = 36) | p-Value * | |
|---|---|---|---|
| MNA score (mean (SD)) | 28.63 (6.05) | 17.97 (4.77) | 0.019 |
| Barthel score (mean (SD)) | 89.72 (18.44) | 69.79 (11.83) | 0.034 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Murillo-Llorente, M.T.; Lafuente-Sarabia, B.; Samper de la Paz, J.; Flores-Púa, M.; Tejeda-Adell, M.; Legidos-García, M.E.; Perez-Bermejo, M. Assessing Nutritional Status and Frailty among Poor Elderly Individuals in Requena del Tapiche, Peru. Nutrients 2023, 15, 3840. https://doi.org/10.3390/nu15173840
Murillo-Llorente MT, Lafuente-Sarabia B, Samper de la Paz J, Flores-Púa M, Tejeda-Adell M, Legidos-García ME, Perez-Bermejo M. Assessing Nutritional Status and Frailty among Poor Elderly Individuals in Requena del Tapiche, Peru. Nutrients. 2023; 15(17):3840. https://doi.org/10.3390/nu15173840
Chicago/Turabian StyleMurillo-Llorente, María Teresa, Blanca Lafuente-Sarabia, Jennifer Samper de la Paz, Merita Flores-Púa, Manuel Tejeda-Adell, María Ester Legidos-García, and Marcelino Perez-Bermejo. 2023. "Assessing Nutritional Status and Frailty among Poor Elderly Individuals in Requena del Tapiche, Peru" Nutrients 15, no. 17: 3840. https://doi.org/10.3390/nu15173840
APA StyleMurillo-Llorente, M. T., Lafuente-Sarabia, B., Samper de la Paz, J., Flores-Púa, M., Tejeda-Adell, M., Legidos-García, M. E., & Perez-Bermejo, M. (2023). Assessing Nutritional Status and Frailty among Poor Elderly Individuals in Requena del Tapiche, Peru. Nutrients, 15(17), 3840. https://doi.org/10.3390/nu15173840





