Mental Health Variables Impact Weight Loss, Especially in Patients with Obesity and Binge Eating: A Mediation Model on the Role of Eating Disorder Pathology
Abstract
:1. Introduction
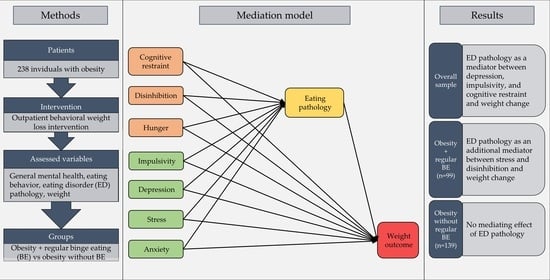
2. Materials and Methods
2.1. Study Design, Participants, and Procedures
2.2. Measurements
2.2.1. BMI
2.2.2. Impulsivity
2.2.3. Depression
2.2.4. Stress
2.2.5. Anxiety
2.2.6. Eating Disorder Pathology and Frequency of Binge Eating
2.2.7. Eating Behavior
2.3. Statistical Analysis
3. Results
3.1. Sample Characteristics
3.2. Correlation Analyses
3.3. Mediation Analyses
3.3.1. Overall Sample
3.3.2. Patients with Obesity and with Regular Binge-Eating Episodes
3.3.3. Patients with Obesity and without Regular Binge Eating Episodes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Obesity and Overweight. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 7 September 2023).
- World Health Organization. Noncommunicable Diseases. 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed on 7 September 2023).
- Abiri, B.; Hosseinpanah, F.; Banihashem, S.; Madinehzad, S.A.; Valizadeh, M. Mental Health and Quality of Life in Different Obesity Phenotypes: A Systematic Review. Health Qual. Life Outcomes 2022, 20, 63. [Google Scholar] [CrossRef]
- Endalifer, M.L.; Diress, G. Epidemiology, Predisposing Factors, Biomarkers, and Prevention Mechanism of Obesity: A Systematic Review. J. Obes. 2020, 2020, 6134362. [Google Scholar] [CrossRef]
- Bray, G.A.; Ryan, D.H. Evidence-based Weight Loss Interventions: Individualized Treatment Options to Maximize Patient Outcomes. Diabetes Obes. Metab. 2021, 23, 50–62. [Google Scholar] [CrossRef]
- Garvey, W.T.; Mechanick, J.I.; Brett, E.M.; Garber, A.J.; Hurley, D.L.; Jastreboff, A.M.; Nadolsky, K.; Pessah-Pollack, R.; Plodkowski, R. American Association of Clinical Endocrinologists and American College of Endocrinology Comprehensive Clinical Practice Guidelines for Medical Care of Patients with Obesity. Endocr. Pract. 2016, 22, 842–884. [Google Scholar] [CrossRef]
- Ryan, D.H.; Kahan, S. Guideline Recommendations for Obesity Management. Med. Clin. North Am. 2018, 102, 49–63. [Google Scholar] [CrossRef]
- Bauer, K.; Lau, T.; Schwille-Kiuntke, J.; Schild, S.; Hauner, H.; Stengel, A.; Zipfel, S.; Mack, I. Conventional Weight Loss Interventions across the Different BMI Obesity Classes: A Systematic Review and Quantitative Comparative Analysis. Eur. Eat. Disord. Rev. 2020, 28, 492–512. [Google Scholar] [CrossRef] [PubMed]
- Varkevisser, R.D.M.; van Stralen, M.M.; Kroeze, W.; Ket, J.C.F.; Steenhuis, I.H.M. Determinants of Weight Loss Maintenance: A Systematic Review: Determinants of Weight Loss Maintenance. Obes. Rev. 2019, 20, 171–211. [Google Scholar] [CrossRef] [PubMed]
- Manasse, S.M.; Flack, D.; Dochat, C.; Zhang, F.; Butryn, M.L.; Forman, E.M. Not so Fast: The Impact of Impulsivity on Weight Loss Varies by Treatment Type. Appetite 2017, 113, 193–199. [Google Scholar] [CrossRef] [PubMed]
- McGuire, M.T.; Wing, R.R.; Klem, M.L.; Lang, W.; Hill, J.O. What Predicts Weight Regain in a Group of Successful Weight Losers? J. Consult. Clin. Psychol. 1999, 67, 177–185. [Google Scholar] [CrossRef]
- Geiker, N.R.W.; Astrup, A.; Hjorth, M.F.; Sjödin, A.; Pijls, L.; Markus, C.R. Does Stress Influence Sleep Patterns, Food Intake, Weight Gain, Abdominal Obesity and Weight Loss Interventions and Vice Versa? Obes. Rev. 2018, 19, 81–97. [Google Scholar] [CrossRef]
- Aylward, L.; Lilly, C.; Tabone, L.; Szoka, N.; Abunnaja, S.; Cox, S. Anxiety Predicts Reduced Weight Loss 30 Months after Bariatric Surgery. Surg. Obes. Relat. Dis. 2022, 18, 919–927. [Google Scholar] [CrossRef]
- Urbanek, J.K.; Metzgar, C.J.; Hsiao, P.Y.; Piehowski, K.E.; Nickols-Richardson, S.M. Increase in Cognitive Eating Restraint Predicts Weight Loss and Change in Other Anthropometric Measurements in Overweight/Obese Premenopausal Women. Appetite 2015, 87, 244–250. [Google Scholar] [CrossRef]
- Amundsen, T.; Strømmen, M.; Martins, C. Suboptimal Weight Loss and Weight Regain after Gastric Bypass Surgery-Postoperative Status of Energy Intake, Eating Behavior, Physical Activity, and Psychometrics. Obes. Surg. 2017, 27, 1316–1323. [Google Scholar] [CrossRef]
- Burgmer, R.; Grigutsch, K.; Zipfel, S.; Wolf, A.M.; Zwaan, M.; Husemann, B.; Albus, C.; Senf, W.; Herpertz, S. The Influence of Eating Behavior and Eating Pathology on Weight Loss after Gastric Restriction Operations. Obes. Surg. 2005, 15, 684–691. [Google Scholar] [CrossRef] [PubMed]
- Legenbauer, T.; Müller, A.; Zwaan, M.; Fischer, C.; Burgmer, R.; Herpertz, S. The Impact of Self-Reported Impulsivity on the Course of Weight Is Mediated by Disinhibited Eating. Eur. Eat. Disord. Rev. 2018, 26, 38–45. [Google Scholar] [CrossRef] [PubMed]
- De Zwaan, M.; Mitchell, J.E.; Seim, H.C.; Specker, S.M.; Pyle, R.L.; Raymond, N.C.; Crosby, R.B. Eating Related and General Psychopathology in Obese Females with Binge Eating Disorder. Int. J. Eat. Disord. 1994, 15, 43–52. [Google Scholar] [CrossRef]
- Cox, S.; Brode, C. Predictors of Binge Eating among Bariatric Surgery Candidates: Disinhibition as a Mediator of the Relationship between Depressive Symptoms and Binge Eating. Obes. Surg. 2018, 28, 1990–1996. [Google Scholar] [CrossRef] [PubMed]
- van Strien, T.; Konttinen, H.; Homberg, J.R.; Engels, R.C.M.E.; Winkens, L.H.H. Emotional Eating as a Mediator between Depression and Weight Gain. Appetite 2016, 100, 216–224. [Google Scholar] [CrossRef] [PubMed]
- Smith, K.E.; Mason, T.B.; Wang, W.-L.; Schumacher, L.M.; Pellegrini, C.A.; Goldschmidt, A.B.; Unick, J.L. Dynamic Associations between Anxiety, Stress, Physical Activity, and Eating Regulation over the Course of a Behavioral Weight Loss Intervention. Appetite 2022, 168, 105706. [Google Scholar] [CrossRef]
- Christaki, E.; Kokkinos, A.; Costarelli, V.; Alexopoulos, E.C.; Chrousos, G.P.; Darviri, C. Stress Management Can Facilitate Weight Loss in Greek Overweight and Obese Women: A Pilot Study. J. Hum. Nutr. Diet. 2013, 26, 132–139. [Google Scholar] [CrossRef]
- Hindle, A.; Piedad Garcia, X.; Hayden, M.; O’Brien, P.E.; Restraint, B.L.P.; Hunger, P. Disinhibition and Emotional Eating Predict Weight Loss at 2 Years Post-Laparoscopic Adjustable Gastric Banding. Obes. Surg. 2020, 30, 1347–1359. [Google Scholar] [CrossRef]
- Cheung, V.; Aylward, L.; Tabone, L.; Szoka, N.; Abunnaja, S.; Cox, S. Hunger Mediates the Relationship between Food Insecurity and Binge Eating among Bariatric Surgery Candidates. Surg. Obes. Relat. Dis. 2022, 18, 530–537. [Google Scholar] [CrossRef]
- Boswell, R.G.; Potenza, M.N.; Grilo, C.M. The Neurobiology of Binge-Eating Disorder Compared with Obesity: Implications for Differential Therapeutics. Clin. Ther. 2021, 43, 50–69. [Google Scholar] [CrossRef]
- Gerlach, G.; Herpertz, S.; Loeber, S. Personality traits and obesity: A systematic review. Obes. Rev. 2015, 16, 32–63. [Google Scholar] [CrossRef] [PubMed]
- Giel, K.E.; Bulik, C.M.; Fernandez-Aranda, F.; Hay, P.; Keski-Rahkonen, A.; Schag, K.; Schmidt, U.; Zipfel, S. Binge Eating Disorder. Nat. Rev. Dis. Primers 2022, 8, 16. [Google Scholar] [CrossRef]
- Kessler, R.M.; Hutson, P.H.; Herman, B.K.; Potenza, M.N. The Neurobiological Basis of Binge-Eating Disorder. Neurosci. Biobehav. Rev. 2016, 63, 223–238. [Google Scholar] [CrossRef] [PubMed]
- Schag, K.; Schönleber, J.; Teufel, M.; Zipfel, S.; Giel, K.E. Food-related impulsivity in obesity and Binge Eating Disorder—A systematic review. Obes. Rev. 2013, 14, 477–495. [Google Scholar] [CrossRef]
- Kessler, R.C.; Berglund, P.A.; Chiu, W.T.; Deitz, A.C.; Hudson, J.I.; Shahly, V.; Aguilar-Gaxiola, S.; Alonso, J.; Angermeyer, M.C.; Benjet, C.; et al. The Prevalence and Correlates of Binge Eating Disorder in the World Health Organization World Mental Health Surveys. Biol. Psychiatry 2013, 73, 904–914. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- World Health Organization. ICD-11: International Statistical Classification of Diseases 11th Revision and Related Health Problems. ICD, 2019. Available online: https://icd.who.int/ (accessed on 26 July 2023).
- Dawe, S.; Loxton, N.J. The Role of Impulsivity in the Development of Substance Use and Eating Disorders. Neurosci. Biobehav. Rev. 2004, 28, 343–351. [Google Scholar] [CrossRef] [PubMed]
- Schag, K.; Rennhak, S.K.; Leehr, E.J.; Skoda, E.M.; Becker, S.; Bethge, W.; Martus, P.; Zipfel, S.; Giel, K.E. IMPULS: Impulsivity-Focused Group Intervention to Reduce Binge Eating Episodes in Patients with Binge Eating Disorder—A Randomised Controlled Trial. Psychother. Psychosom. 2019, 88, 141–153. [Google Scholar] [CrossRef]
- Bauer, K.; Schild, S.; Sauer, H.; Teufel, M.; Stengel, A.; Giel, K.E.; Schellhorn, P.; Junne, F.; Nieß, A.; Zipfel, S.; et al. How Attitude towards Bariatric Surgery Influences the Effects of Behavioural Weight Loss Treatment. Obes. Facts 2021, 14, 531–542. [Google Scholar] [CrossRef]
- Mack, I.; Ölschläger, S.; Sauer, H.; Feilitzsch, M.; Weimer, K.; Junne, F.; Peeraully, R.; Enck, P.; Zipfel, S.; Teufel, M. Does Laparoscopic Sleeve Gastrectomy Improve Depression, Stress and Eating Behaviour? A 4-Year Follow-up Study. Obes. Surg. 2016, 26, 2967–2973. [Google Scholar] [CrossRef] [PubMed]
- Schag, K.; Mack, I.; Giel, K.E.; Ölschläger, S.; Skoda, E.M.; Feilitzsch, M.; Zipfel, S.; Teufel, M. The Impact of Impulsivity on Weight Loss Four Years after Bariatric Surgery. Nutrients 2016, 8, 721. [Google Scholar] [CrossRef] [PubMed]
- Wirth, A.; Wabitsch, M.; Hauner, H. The Prevention and Treatment of Obesity. Dtsch. Ärztebl. Int. 2014, 111, 705. [Google Scholar] [CrossRef] [PubMed]
- Meule, A.; Vögele, C.; Kübler, A. Psychometrische Evaluation der deutschen Barratt Impulsiveness Scale—Kurzversion (BIS-15). Diagnostica 2011, 57, 126–133. [Google Scholar] [CrossRef]
- Sharma, L.; Markon, K.E.; Clark, L.A. Toward a Theory of Distinct Types of “Impulsive” Behaviors: A Meta-Analysis of Self-Report and Behavioral Measures. Psychol. Bull. 2014, 140, 374–408. [Google Scholar] [CrossRef] [PubMed]
- Levenstein, S.; Prantera, C.; Varvo, V.; Scribano, M.L.; Berto, E.; Luzi, C.; Andreoli, A. Development of the Perceived Stress Questionnaire: A New Tool for Psychosomatic Research. J. Psychosom. Res. 1993, 37, 19–32. [Google Scholar] [CrossRef] [PubMed]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [PubMed]
- Hilbert, A.; Tuschen-Caffier, B. Eating Disorder Examination, 2nd ed.; Dgvt-Verlag: Tübingen, Germany, 2016; ISBN 978-3-87159-411-3. [Google Scholar]
- Pudel, V.; Westenhöfer, J. Fragebogen zum Essverhalten (FEV)-Handanweisung; Verlag für Psychologie Dr. C. J. Hogrefe: Göttingen, Germany, 1989. [Google Scholar]
- Stunkard, A.J.; Messick, S. The Three-Factor Eating Questionnaire to Measure Dietary Restraint, Disinhibition and Hunger. J. Psychosom. Res. 1985, 29, 71–83. [Google Scholar] [CrossRef]
- Rosseel, Y. Lavaan: An R Package for Structural Equation Modeling. J. Stat. Soft. 2012, 48, 1–36. [Google Scholar] [CrossRef]
- Agler, R.; Boeck, P. On the Interpretation and Use of Mediation: Multiple Perspectives on Mediation Analysis. Front. Psychol. 2017, 8, 1984. [Google Scholar] [CrossRef] [PubMed]
- Lv, N.; Azar, K.M.J.; Rosas, L.G.; Wulfovich, S.; Xiao, L.; Ma, J. Behavioral Lifestyle Interventions for Moderate and Severe Obesity: A Systematic Review. Prev. Med. 2017, 100, 180–193. [Google Scholar] [CrossRef]
- Jensen, M.D.; Ryan, D.H.; Apovian, C.M.; Ard, J.D.; Comuzzie, A.G.; Donato, K.A.; Hu, F.B.; Hubbard, V.S.; Jakicic, J.M.; Kushner, R.F.; et al. AHA/ACC/TOS Guideline for the Management of Overweight and Obesity in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Obesity Society. Circulation 2013, 129 (Suppl. S2), S102–S138. [Google Scholar] [CrossRef]
- Ross, K.M.; Eastman, A.; Ugwoaba, U.A.; Demos, K.E.; Lillis, J.; Wing, R.R. Food Reward Sensitivity, Impulsivity, and Weight Change during and after a 3-Month Weight Loss Program. PLoS ONE 2020, 15, 0243530. [Google Scholar] [CrossRef] [PubMed]
- Marcus, M.D.; Wing, R.R.; Guare, J.; Blair, E.H.; Jawad, A. Lifetime Prevalence of Major Depression and Its Effect on Treatment Outcome in Obese Type II Diabetic Patients. Diabetes Care 1992, 15, 253–255. [Google Scholar] [CrossRef] [PubMed]
- Ludman, E.; Simon, G.E.; Ichikawa, L.E.; Operskalski, B.H.; Arterburn, D.; Linde, J.A.; Jeffery, R.W.; Rohde, P.; Finch, E.A. Does Depression Reduce the Effectiveness of Behavioral Weight Loss Treatment? Behav. Med. 2009, 35, 126–134. [Google Scholar] [CrossRef]
- Ma, J.; Rosas, L.G.; Lv, N.; Xiao, L.; Snowden, M.B.; Venditti, E.M.; Lewis, M.A.; Goldhaber-Fiebert, J.D.; Lavori, P.W. Effect of Integrated Behavioral Weight Loss Treatment and Problem-Solving Therapy on Body Mass Index and Depressive Symptoms Among Patients with Obesity and Depression: The RAINBOW Randomized Clinical Trial. J. Am. Med. Assoc. 2019, 321, 869–879. [Google Scholar] [CrossRef] [PubMed]
- Smith, C.E.; Hawkins, M.A.W.; Williams-Kerver, G.A.; Duncan, J. Depression Subtypes, Binge Eating, and Weight Loss in Bariatric Surgery Candidates. Surg. Obes. Relat. Dis. 2020, 16, 690–697. [Google Scholar] [CrossRef]
- Grilo, C.M.; Gueorguieva, R.; Pittman, B. Examining Depression Scores as Predictors and Moderators of Treatment Outcomes in Patients with Binge-eating Disorder. Int. J. Eat. Disord. 2021, 54, 1555–1559. [Google Scholar] [CrossRef]
- Ziser, K.; Finklenburg, C.; Behrens, S.C.; Giel, K.E.; Becker, S.; Skoda, E.-M.; Teufel, M.; Mack, I.; Zipfel, S.; Junne, F. Perceived Stress Mediates the Relationship of Body Image and Depressive Symptoms in Individuals with Obesity. Front. Psychiatry 2019, 10, 852. [Google Scholar] [CrossRef]
- Vidmar, A.P.; Yamashita, N.; Fox, D.S.; Hegedus, E.; Wee, C.P.; Salvy, S.J. Can a Behavioral Weight-Loss Intervention Change Adolescents’ Food Addiction Severity? Child. Obes. 2022, 18, 206–212. [Google Scholar] [CrossRef] [PubMed]
- McLean, R.C.; Morrison, D.S.; Shearer, R.; Boyle, S.; Logue, J. Attrition and Weight Loss Outcomes for Patients with Complex Obesity, Anxiety and Depression Attending a Weight Management Programme with Targeted Psychological Treatment: HADS in Weight Management: Attrition & Weight Loss. Clin. Obes. 2016, 6, 133–142. [Google Scholar] [CrossRef]
- Bernabéu-Brotóns, E.; Marchena-Giráldez, C. Emotional Eating and Perfectionism as Predictors of Symptoms of Binge Eating Disorder: The Role of Perfectionism as a Mediator between Emotional Eating and Body Mass Index. Nutrients 2022, 14, 3361. [Google Scholar] [CrossRef] [PubMed]
- Strober, M.; Freeman, R.; Lampert, C.; Diamond, J. The Association of Anxiety Disorders and Obsessive Compulsive Personality Disorder with Anorexia Nervosa: Evidence from a Family Study with Discussion of Nosological and Neurodevelopmental Implications. Int. J. Eat. Disord. 2007, 40, S46–S51. [Google Scholar] [CrossRef]
- Michael, M.L.; Juarascio, A. Elevated Cognitive Dietary Restraint Mediates the Relationship between Greater Impulsivity and More Frequent Binge Eating in Individuals with Binge-Spectrum Eating Disorders. Eat. Weight. Disord. 2021, 26, 2795–2800. [Google Scholar] [CrossRef]
- Sairanen, E.; Lappalainen, R.; Lapveteläinen, A.; Tolvanen, A.; Karhunen, L. Flexibility in Weight Management. Eat. Behav. 2014, 15, 218–224. [Google Scholar] [CrossRef] [PubMed]
- Bryant, E.J.; Rehman, J.; Pepper, L.B.; Walters, E.R. Obesity and Eating Disturbance: The Role of TFEQ Restraint and Disinhibition. Curr. Obes. Rep. 2019, 8, 363–372. [Google Scholar] [CrossRef]
- Jacobsen, E.; Boyers, D.; Manson, P.; Avenell, A. A Systematic Review of the Evidence for Non-Surgical Weight Management for Adults with Severe Obesity: What Is Cost Effective and What Are the Implications for the Design of Health Services? Curr. Obes. Rep. 2022, 11, 356–385. [Google Scholar] [CrossRef]




| Variables | Overall Sample (n = 238) | Patients without Regular Binge Eating (n = 139) | Patients with Regular Binge Eating (n = 99) | Group Difference |
|---|---|---|---|---|
| Females | 189 (79.4%) | 110 (79.1%) | 79 (79.8%) | p = 0.901 |
| Age | 41.3 +/− 12.1 | 41.7 +/− 12.2 | 40.8 +/− 12.0 | p = 0.575 |
| Previous history of weight loss (yes/no) | 83/126 (65.9%) | 47/71 (66.2%) | 36 (65.5%) | p = 0.931 |
| Time Since Maximum Weight Recorded (months) | 30.8 +/− 53.5 | 28.5 +/− 46.0 | 33.6 +/− 61.6 | p = 0.102 |
| Maximum previous weight (kg) | 129.1 +/− 21.9 | 128.5 +/− 21.2 | 130.0 +/− 22.9 | p = 0.578 |
| Admission weight (kg) | 122.6 +/− 19.8 | 122.2 +/− 19.5 | 123.1 +/− 20.3 | p = 0.542 |
| Discharge weight (kg) | 120.2 +/− 20.5 | 119.5 +/− 20.3 | 121.3 +/− 21.0 | p = 0.691 |
| Admission BMI (kg/m2) | 42.4 +/− 5.3 | 42.3 +/− 5.0 | 42.5 +/− 5.6 | p = 0.909 |
| Discharge BMI (kg/m2) | 41.5 +/− 5.6 | 41.2 +/− 5.6 | 41.9 +/− 5.6 | p = 0.525 |
| Discharge-Admission BMI difference | −0.9 +/− 2.1 | −1.1 +/− 2.1 | −0.7 +/− 2.1 | p = 0.258 |
| BIS total score | 35.0 +/− 4.9 | 34.4 +/− 5.2 | 35.9 +/− 4.4 | p = 0.037 |
| GAD total score | 7.7 +/− 5.0 | 6.8 +/− 4.6 | 9.0 +/− 5.1 | p = 0.001 |
| PSQ total score | 0.5 +/− 0.2 | 0.5 +/− 0.2 | 0.6 +/− 0.2 | p = 0.001 |
| PHQ-9 score | 9.1 +/− 5.5 | 8.2 +/− 5.8 | 10.5 +/− 4.8 | p < 0.001 |
| EDE-Q total score | 2.9 +/− 1.0 | 2.7 +/− 0.9 | 3.2 +/− 1.0 | p < 0.001 |
| Binge eating frequency acc. to EDE-Q | 6.0 +/− 9.5 | 0.6 +/− 1.0 | 13.5 +/− 11.0 | p < 0.001 |
| TFEQ cognitive restraint | 8.2 +/− 4.0 | 8.9 +/− 4.1 | 7.4 +/− 3.7 | p = 0.009 |
| TFEQ disinhibition | 9.6 +/− 3.8 | 8.5 +/− 3.6 | 11.1 +/− 3.6 | p < 0.001 |
| TFEQ hunger | 9.2 +/− 3.2 | 6.3 +/− 3.5 | 7.6 +/− 3.6 | p < 0.001 |
| BMI Difference | BIS | TFEQ Cognitive Restraint | TFEQ Disinhibition | TFEQ Hunger | GAD | PHQ-9 | PSQ | EDE-Q | |
|---|---|---|---|---|---|---|---|---|---|
| BMI difference | / | −0.026 | 0.044 | −0.137 * | −0.105 | −0.029 | −0.107 | −0.100 | −0.192 ** |
| BIS | / | / | −0.003 | 0.191 * | 0.217 * | 0.155 * | 0.065 | 0.086 | 0.242 ** |
| TFEQ cognitive restraint | / | / | / | −0.281 ** | −0.331 ** | −0.031 | −0.057 | 0.024 | 0.164 * |
| TFEQ disinhibition | / | / | / | / | 0.705 ** | 0.311 ** | 0.353 * | 0.331 * | 0.388 ** |
| TFEQ hunger | / | / | / | / | / | 0.245 ** | 0.295 ** | 0.241 ** | 0.315 ** |
| GAD | / | / | / | / | / | / | 0.712 ** | 0.748 ** | 0.435 ** |
| PHQ-9 | / | / | / | / | / | / | / | 0.660 ** | 0.505 ** |
| PSQ | / | / | / | / | / | / | / | / | 0.476 ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pruccoli, J.; Mack, I.; Klos, B.; Schild, S.; Stengel, A.; Zipfel, S.; Giel, K.E.; Schag, K. Mental Health Variables Impact Weight Loss, Especially in Patients with Obesity and Binge Eating: A Mediation Model on the Role of Eating Disorder Pathology. Nutrients 2023, 15, 3915. https://doi.org/10.3390/nu15183915
Pruccoli J, Mack I, Klos B, Schild S, Stengel A, Zipfel S, Giel KE, Schag K. Mental Health Variables Impact Weight Loss, Especially in Patients with Obesity and Binge Eating: A Mediation Model on the Role of Eating Disorder Pathology. Nutrients. 2023; 15(18):3915. https://doi.org/10.3390/nu15183915
Chicago/Turabian StylePruccoli, Jacopo, Isabelle Mack, Bea Klos, Sandra Schild, Andreas Stengel, Stephan Zipfel, Katrin Elisabeth Giel, and Kathrin Schag. 2023. "Mental Health Variables Impact Weight Loss, Especially in Patients with Obesity and Binge Eating: A Mediation Model on the Role of Eating Disorder Pathology" Nutrients 15, no. 18: 3915. https://doi.org/10.3390/nu15183915