Predictive Potential of Biomarkers of Intestinal Barrier Function for Therapeutic Management with Teduglutide in Patients with Short Bowel Syndrome
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Individuals
2.2. Citrulline Concentrations
2.3. Sequence Analysis of GLP-2 Receptor Gene
- SIFT (sorting intolerant from tolerant) [30]
- 2.
- PolyPhen (Polymorphism Phenotyping) [31]
2.4. RNA Extraction, cDNA Synthesis, and Real-Time qRT-PCR
2.5. Immunohistochemistry
2.6. Intestinal Permeability Measuring
2.7. Statistical Analysis
3. Results
3.1. Study Cohort
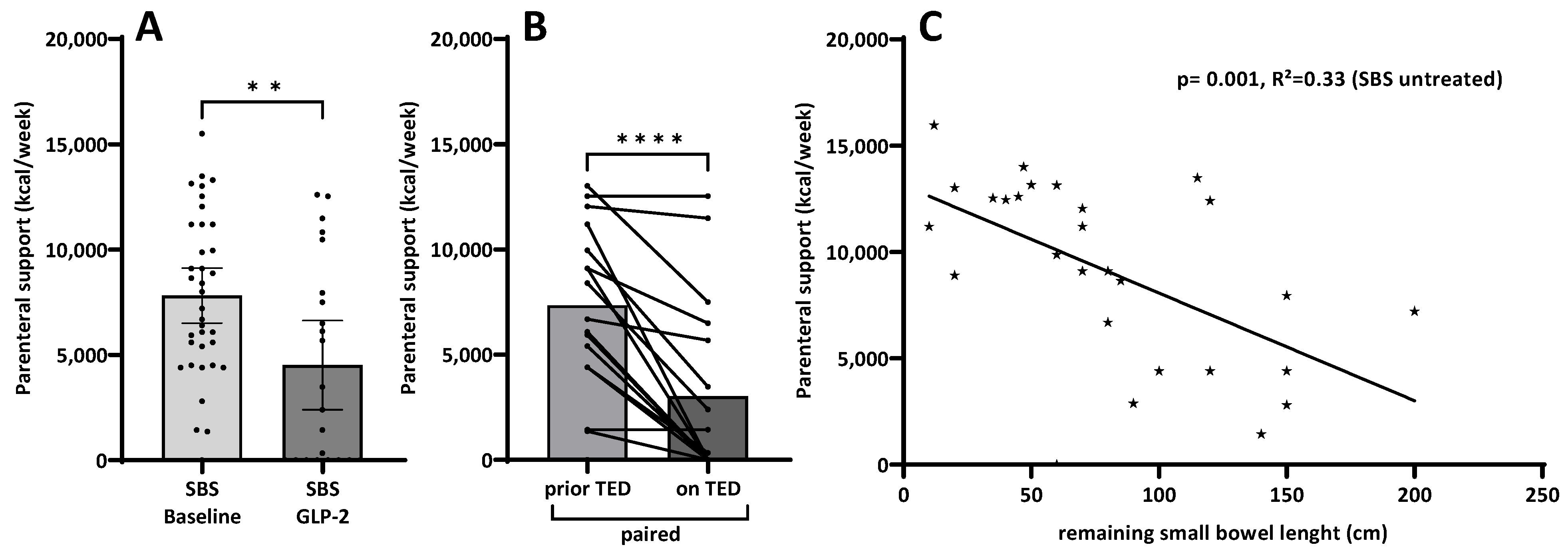
3.2. Parenteral Support
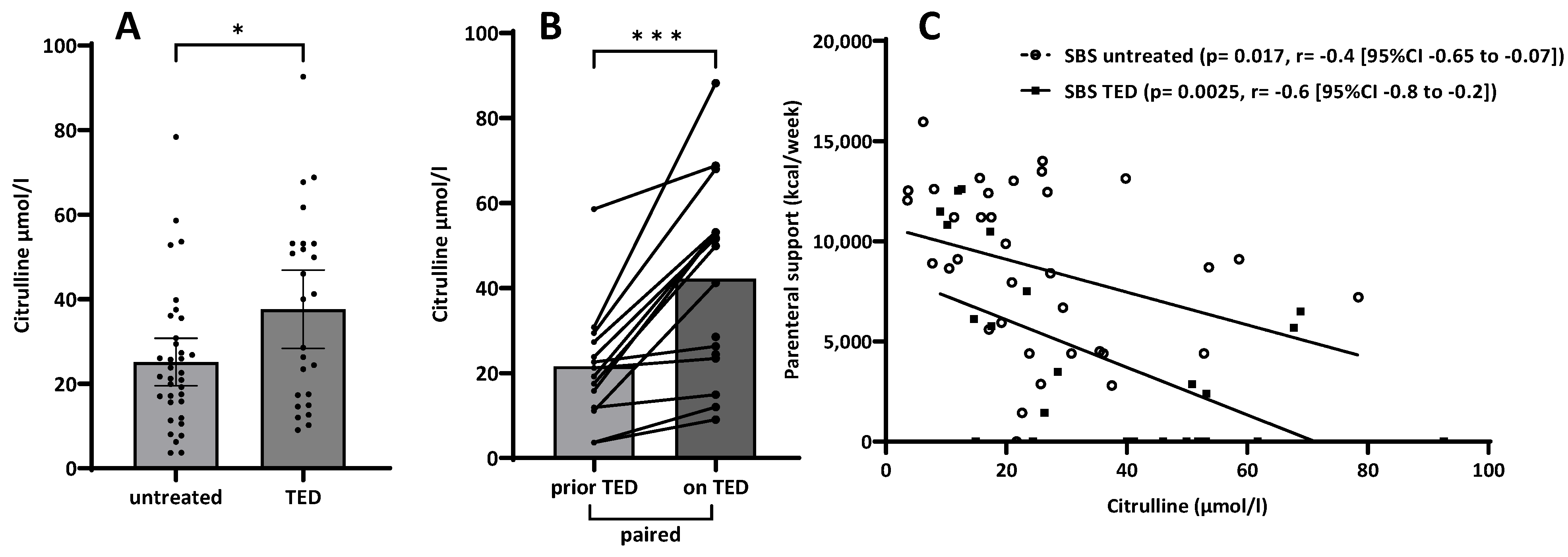
3.3. Citrulline
3.4. Sequence Analysis of GLP-2 Receptor Gene
3.5. qPCR Expression Profiles of Tight Junction Genes and Epithelial Markers
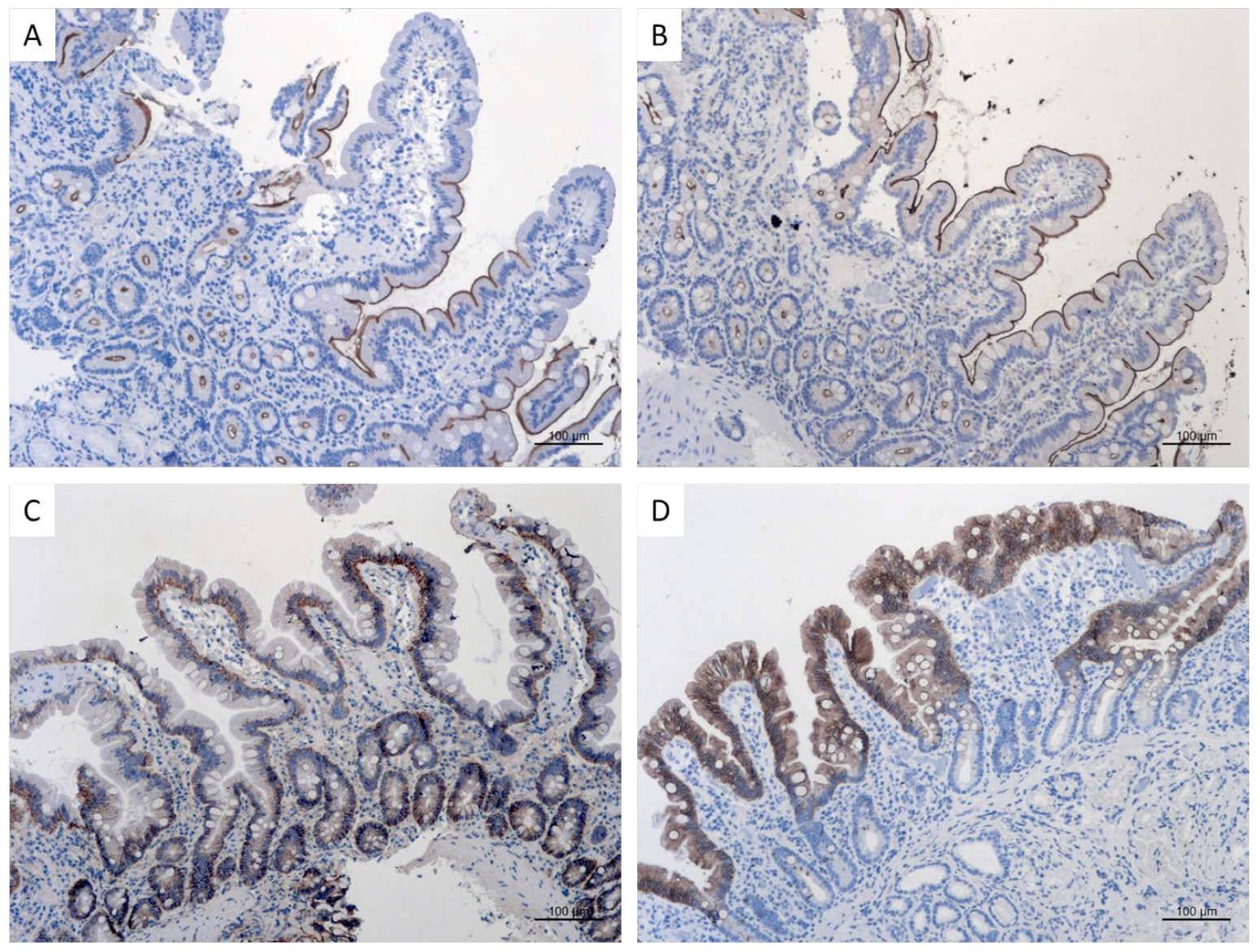
3.6. Immunohistochemistry
3.7. Intestinal Permeability Testing
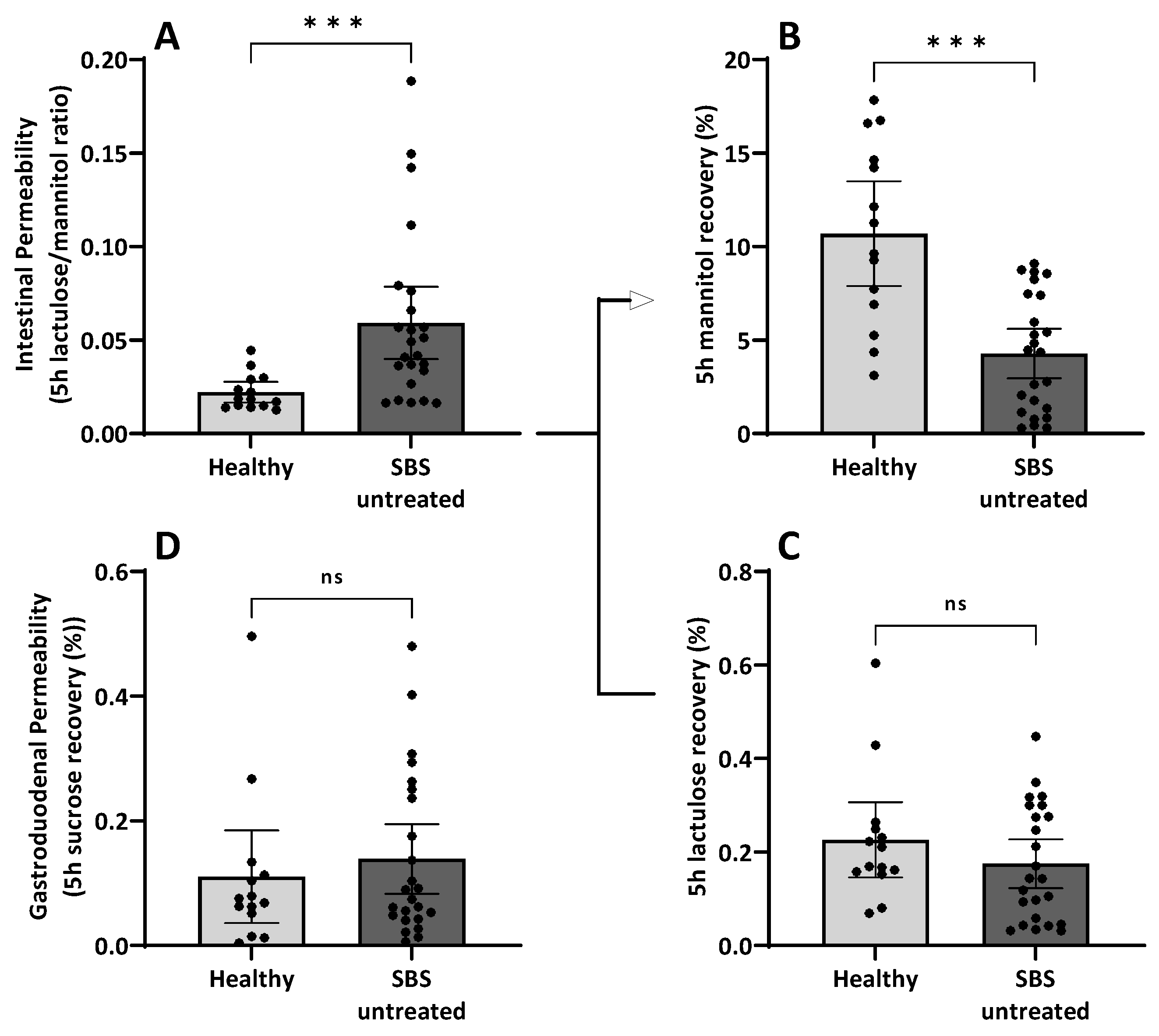
3.7.1. Intestinal Permeability in Short Bowel Syndrome
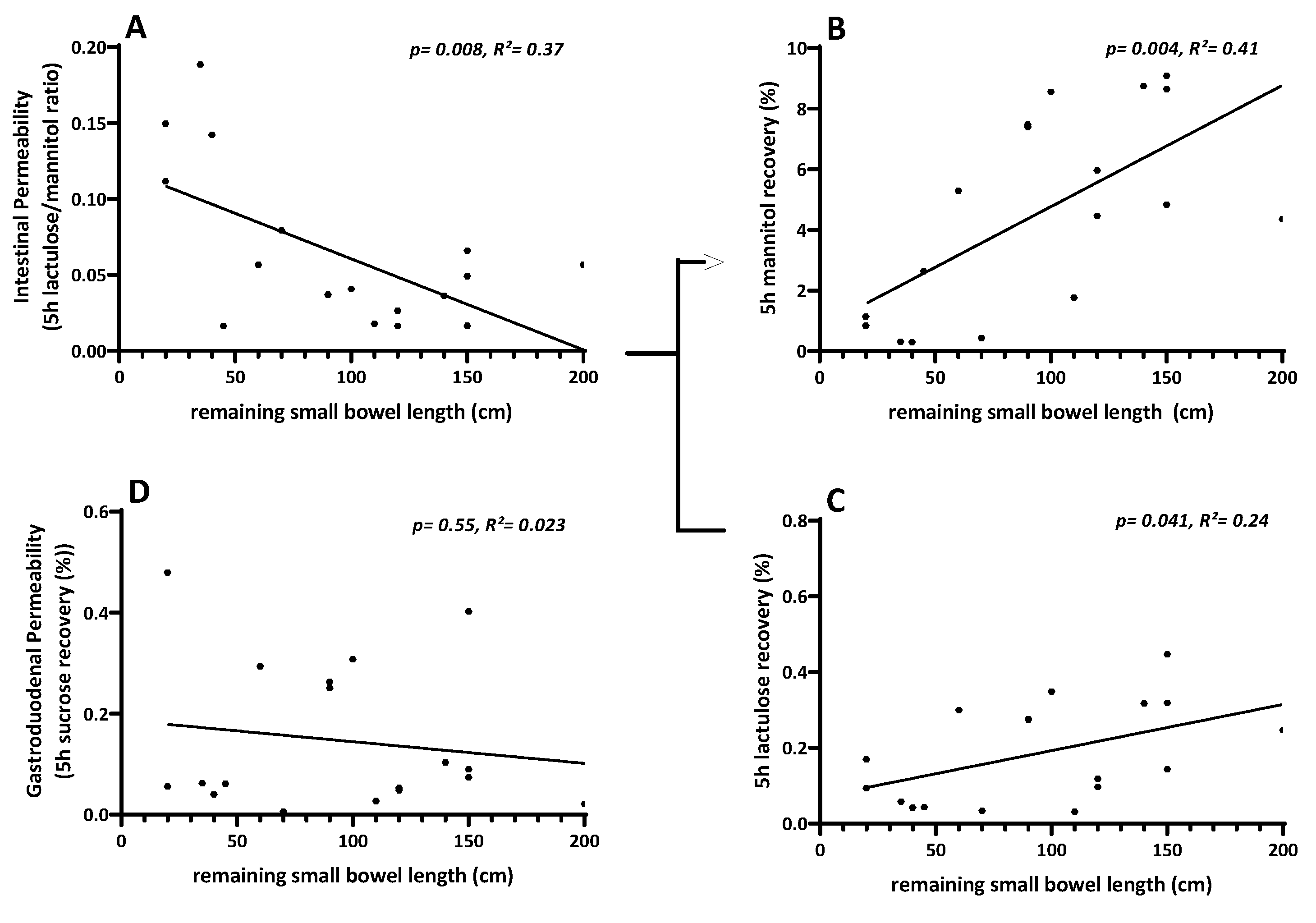
3.7.2. Linear Regression of Intestinal Permeability Testing with Remaining Small Bowel Length
3.7.3. Intestinal Permeability Testing and Treatment with Teduglutide
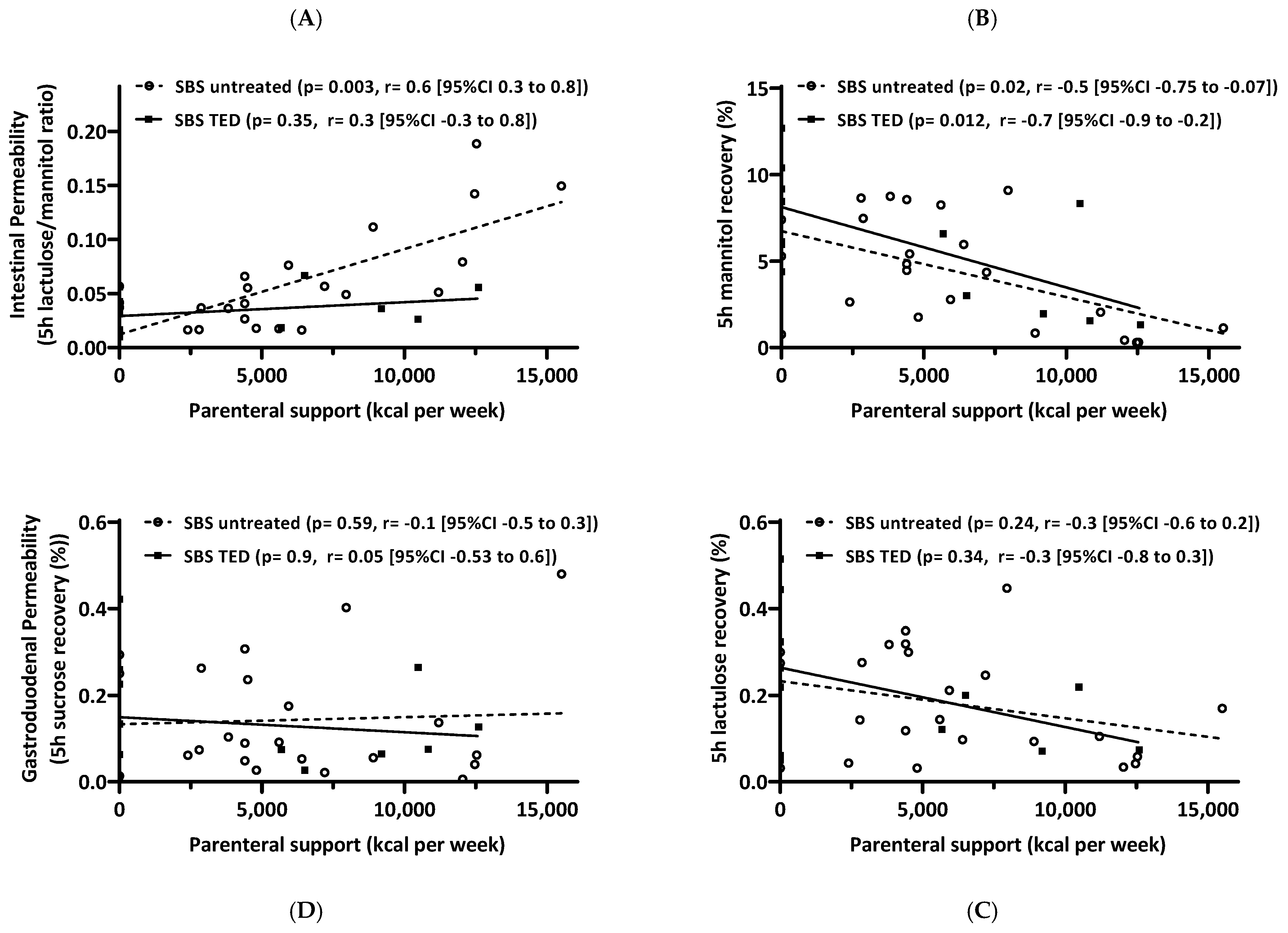
3.7.4. Correlation of Intestinal Permeability Testing and Parenteral Support
4. Discussion
4.1. Summary of Results
4.2. Parenteral Support as a Clinical Surrogate for Small Intestinal Function
4.3. Citrulline as a Biomarker
4.4. GLP-2 Receptor Gene Analysis
4.5. Gene Expression Analysis of Multiple Epithelial Small Intestinal Genes
4.6. Functional Assessment of Intestinal Barrier by Intestinal Permeability Testing
4.7. Limitations of the Studies
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Jeppesen, P.B. Spectrum of short bowel syndrome in adults: Intestinal insufficiency to intestinal failure. JPEN J. Parenter. Enter. Nutr. 2014, 38 (Suppl. S1), 8S–13S. [Google Scholar] [CrossRef]
- Massironi, S.; Cavalcoli, F.; Rausa, E.; Invernizzi, P.; Braga, M.; Vecchi, M. Understanding short bowel syndrome: Current status and future perspectives. Dig. Liver Dis. 2020, 52, 253–261. [Google Scholar] [CrossRef]
- Pironi, L.; Arends, J.; Bozzetti, F.; Cuerda, C.; Gillanders, L.; Jeppesen, P.B.; Joly, F.; Kelly, D.; Lal, S.; Staun, M.; et al. Chronic Intestinal Failure Special Interest Group of, ESPEN guidelines on chronic intestinal failure in adults. Clin. Nutr. 2016, 35, 247–307. [Google Scholar] [CrossRef] [PubMed]
- Jeppesen, P.B. The Long Road to the Development of Effective Therapies for the Short Gut Syndrome: A Personal Perspective. Dig. Dis. Sci. 2019, 64, 2717–2735. [Google Scholar] [CrossRef]
- Pape, U.F.; Maasberg, S.; Pascher, A. Pharmacological strategies to enhance adaptation in intestinal failure. Curr. Opin. Organ. Transplant. 2016, 21, 147–152. [Google Scholar] [CrossRef]
- Tappenden, K.A. Intestinal adaptation following resection. JPEN J. Parenter. Enter. Nutr. 2014, 38 (Suppl. S1), 23S–31S. [Google Scholar] [CrossRef] [PubMed]
- Drucker, D.J. Minireview: The glucagon-like peptides. Endocrinology 2001, 142, 521–527. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, M.A.; McKay, D.M.; Yang, P.-C.; Cameron, H.; Perdue, M.H. Glucagon-like peptide-2 enhances intestinal epithelial barrier function of both transcellular and paracellular pathways in the mouse. Gut 2000, 47, 112–119. [Google Scholar] [CrossRef]
- Drucker, D.J. Biologic actions and therapeutic potential of the proglucagon-derived peptides. Nat. Clin. Pract. Endocrinol. Metab. 2005, 1, 22–31. [Google Scholar] [CrossRef]
- Brubaker, P.L. Glucagon-like Peptide-2 and the Regulation of Intestinal Growth and Function. Compr. Physiol. 2018, 8, 1185–1210. [Google Scholar]
- Munroe, D.G.; Gupta, A.K.; Kooshesh, F.; Vyas, T.B.; Rizkalla, G.; Wang, H.; Demchyshyn, L.; Yang, Z.-J.; Kamboj, R.K.; Chen, H.; et al. Prototypic G protein-coupled receptor for the intestinotrophic factor glucagon-like peptide 2. Proc. Natl. Acad. Sci. USA 1999, 96, 1569–1573. [Google Scholar] [CrossRef] [PubMed]
- Yusta, B.; Huang, L.; Munroe, D.; Wolff, G.; Fantaske, R.; Sharma, S.; Demchyshyn, L.; Asa, S.L.; Drucker, D.J. Enteroendocrine localization of GLP-2 receptor expression in humans and rodents. Gastroenterology 2000, 119, 744–755. [Google Scholar] [CrossRef]
- Drucker, D.J. The Discovery of GLP-2 and Development of Teduglutide for Short Bowel Syndrome. ACS Pharmacol. Transl. Sci. 2019, 2, 134–142. [Google Scholar] [CrossRef] [PubMed]
- Jeppesen, P.B.; Sanguinetti, E.L.; Buchman, A.; Howard, L.; Scolapio, J.S.; Ziegler, T.R.; Gregory, J.; A Tappenden, K.; Holst, J.; Mortensen, P.B. Teduglutide (ALX-0600), a dipeptidyl peptidase IV resistant glucagon-like peptide 2 analogue, improves intestinal function in short bowel syndrome patients. Gut 2005, 54, 1224–1231. [Google Scholar] [CrossRef] [PubMed]
- Pape, U.-F.; Iyer, K.R.; Jeppesen, P.B.; Kunecki, M.; Pironi, L.; Schneider, S.M.; Seidner, D.L.; Lee, H.-M.; Caminis, J. Teduglutide for the treatment of adults with intestinal failure associated with short bowel syndrome: Pooled safety data from four clinical trials. Ther. Adv. Gastroenterol. 2020, 13, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Pironi, L.; Allard, J.P.; Joly, F.; Geransar, P.; Genestin, E.; Pape, U. Use of teduglutide in adults with short bowel syndrome-associated intestinal failure. Nutr. Clin. Pract. 2023; online ahead of print. [Google Scholar] [CrossRef]
- Schwartz, L.K.; O’Keefe, S.J.D.; Fujioka, K.; Gabe, S.M.; Lamprecht, G.; Pape, U.-F.; Li, B.; Youssef, N.N.; Jeppesen, P.B. Long-Term Teduglutide for the Treatment of Patients with Intestinal Failure Associated with Short Bowel Syndrome. Clin. Transl. Gastroenterol. 2016, 7, e142. [Google Scholar] [CrossRef]
- Seidner, D.L.; Gabe, S.M.; Lee, H.; Olivier, C.; Jeppesen, P.B. Enteral Autonomy and Days Off Parenteral Support with Teduglutide Treatment for Short Bowel Syndrome in the STEPS Trials. JPEN J. Parenter. Enter. Nutr. 2020, 44, 697–702. [Google Scholar] [CrossRef]
- Tee CTWallis, K.; Gabe, S.M. Emerging treatment options for short bowel syndrome: Potential role of teduglutide. Clin. Exp. Gastroenterol. 2011, 4, 189–196. [Google Scholar]
- Pironi, L. Definitions of intestinal failure and the short bowel syndrome. Best Pract. Res. Clin. Gastroenterol. 2016, 30, 173–185. [Google Scholar] [CrossRef]
- Jeppesen, P.B.; Pertkiewicz, M.; Messing, B.; Iyer, K.; Seidner, D.L.; O’Keefe, S.J.; Forbes, A.; Heinze, H.; Joelsson, B. Teduglutide reduces need for parenteral support among patients with short bowel syndrome with intestinal failure. Gastroenterology 2012, 143, 1473–1481.e3. [Google Scholar] [CrossRef]
- Crenn, P.; Coudray–Lucas, C.; Thuillier, F.; Cynober, L.; Messing, B. Postabsorptive plasma citrulline concentration is a marker of absorptive enterocyte mass and intestinal failure in humans. Gastroenterology 2000, 119, 1496–1505. [Google Scholar] [CrossRef] [PubMed]
- Moran, G.W.; O’Neill, C.; McLaughlin, J.T. GLP-2 enhances barrier formation and attenuates TNFalpha-induced changes in a Caco-2 cell model of the intestinal barrier. Regul. Pept. 2012, 178, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Greif, S.; Maasberg, S.; Wehkamp, J.; Fusco, S.; Zopf, Y.; Herrmann, H.J.; Lamprecht, G.; Jacob, T.; Schiefke, I.; von Websky, M.W.; et al. Long-term results of teduglutide treatment for chronic intestinal failure—Insights from a national, multi-centric patient home-care service program. Clin. Nutr. ESPEN 2022, 51, 222–230. [Google Scholar] [CrossRef] [PubMed]
- Pevny, S.; Maasberg, S.; Rieger, A.; Karber, M.; Blüthner, E.; Knappe-Drzikova, B.; Thurmann, D.; Büttner, J.; Weylandt, K.-H.; Wiedenmann, B.; et al. Experience with teduglutide treatment for short bowel syndrome in clinical practice. Clin. Nutr. 2019, 38, 1745–1755. [Google Scholar] [CrossRef]
- Crenn, P.; Vahedi, K.; Lavergne-Slove, A.; Cynober, L.; Matuchansky, C.; Messing, B. Plasma citrulline: A marker of enterocyte mass in villous atrophy-associated small bowel disease. Gastroenterology 2003, 124, 1210–1219. [Google Scholar] [CrossRef]
- Maric, S.; Flüchter, P.; Guglielmetti, L.C.; Staerkle, R.F.; Sasse, T.; Restin, T.; Schneider, C.; Holland-Cunz, S.G.; Crenn, P.; Vuille-Dit-Bille, R.N. Plasma citrulline correlates with basolateral amino acid transporter LAT4 expression in human small intestine. Clin. Nutr. 2021, 40, 2244–2251. [Google Scholar] [CrossRef] [PubMed]
- Lovshin, J.; Estall, J.; Yusta, B.; Brown, T.J.; Drucker, D.J. Glucagon-like peptide (GLP)-2 action in the murine central nervous system is enhanced by elimination of GLP-1 receptor signaling. J. Biol. Chem. 2001, 276, 21489–21499. [Google Scholar] [CrossRef] [PubMed]
- Prager, M.; Durmus, T.; Büttner, J.; Molnar, T.; de Jong, D.J.; Drenth, J.P.; Baumgart, D.C.; Sturm, A.; Farkas, K.; Witt, H.; et al. Myosin IXb variants and their pivotal role in maintaining the intestinal barrier: A study in Crohn’s disease. Scand. J. Gastroenterol. 2014, 49, 1191–1200. [Google Scholar] [CrossRef] [PubMed]
- Ng, P.C.; Henikoff, S. Predicting deleterious amino acid substitutions. Genome Res. 2011, 11, 863–874. [Google Scholar] [CrossRef]
- Adzhubei, I.A.; Schmidt, S.; Peshkin, L.; Ramensky, V.E.; Gerasimova, A.; Bork, P.; Kondrashov, A.S.; Sunyaev, S.R. A method and server for predicting damaging missense mutations. Nat. Methods 2010, 7, 248–249. [Google Scholar] [CrossRef] [PubMed]
- Bamias, G.; Goukos, D.; Laoudi, E.; Balla, I.G.; Siakavellas, S.I.; Daikos, G.L.; Ladas, S.D. Comparative study of candidate housekeeping genes for quantification of target gene messenger RNA expression by real-time PCR in patients with inflammatory bowel disease. Inflamm. Bowel Dis. 2013, 19, 2840–2847. [Google Scholar] [CrossRef]
- Buhner, S.; Reese, I.; Kuehl, F.; Lochs, H.; Zuberbier, T. Pseudoallergic reactions in chronic urticaria are associated with altered gastroduodenal permeability. Allergy 2004, 59, 1118–1123. [Google Scholar] [CrossRef]
- Wyatt, J.; Vogelsang, H.; Hübl, W.; Waldhoer, T.; Lochs, H. Intestinal permeability and the prediction of relapse in Crohn’s disease. Lancet 1993, 341, 1437–1439. [Google Scholar] [CrossRef]
- Buchman, A.L. The medical and surgical management of short bowel syndrome. MedGenMed 2004, 6, 12. [Google Scholar]
- Buchman, A.L.; Scolapio, J.; Fryer, J. AGA technical review on short bowel syndrome and intestinal transplantation. Gastroenterology 2003, 124, 1111–1134. [Google Scholar] [CrossRef]
- D’Agostino, R. Tests for Normal Distribution. In Goodness-of-Fit Techniques; D’Agostino, R.B., Stepenes, M.A., Eds.; Macel Decker: New York, NY, USA, 1986. [Google Scholar]
- Motulsky, H.J. Test for Appropriate Weighting/Homoscedasticity. GraphPad Prism 10 Curve Fitting Guide 2023. 13 June 2023. Available online: https://www.graphpad.com/guides/prism/latest/curve-fitting/reg_test_for_homoscedasticity.htm (accessed on 5 September 2023).
- Traber, P.G.; Yu, L.; Wu, G.D.; Judge, T.A. Sucrase-isomaltase gene expression along crypt-villus axis of human small intestine is regulated at level of mRNA abundance. Am. J. Physiol. 1992, 262, G123–G130. [Google Scholar] [CrossRef]
- Cohen, A.R.; Wood, D.F.; Marfatia, S.M.; Walther, Z.; Chishti, A.H.; Anderson, J.M. Human CASK/LIN-2 binds syndecan-2 and protein 4.1 and localizes to the basolateral membrane of epithelial cells. J. Cell Biol. 1998, 142, 129–138. [Google Scholar] [CrossRef] [PubMed]
- Drucker, D.J.; Yusta, B. Physiology and pharmacology of the enteroendocrine hormone glucagon-like peptide-2. Annu. Rev. Physiol. 2014, 76, 561–583. [Google Scholar] [CrossRef] [PubMed]
- Tsai, C.H.; Hill, M.; Asa, S.L.; Brubaker, P.L.; Drucker, D.J. Intestinal growth-promoting properties of glucagon-like peptide-2 in mice. Am. J. Physiol. 1997, 273, E77–E84. [Google Scholar] [CrossRef]
- Jeppesen, P.B.; Gilroy, R.; Pertkiewicz, M.; Allard, J.P.; Messing, B.; O’Keefe, S.J. Randomised placebo-controlled trial of teduglutide in reducing parenteral nutrition and/or intravenous fluid requirements in patients with short bowel syndrome. Gut 2011, 60, 902–914. [Google Scholar] [CrossRef] [PubMed]
- Joly, F.; Seguy, D.; Nuzzo, A.; Chambrier, C.; Beau, P.; Poullenot, F.; Thibault, R.; Debeir, L.A.; Layec, S.; Boehm, V.; et al. Six-month outcomes of teduglutide treatment in adult patients with short bowel syndrome with chronic intestinal failure: A real-world French observational cohort study. Clin. Nutr. 2020, 39, 2856–2862. [Google Scholar] [CrossRef]
- Jeppesen, P.B.; Gabe, S.M.; Seidner, D.L.; Lee, H.-M.; Olivier, C. Factors Associated with Response to Teduglutide in Patients with Short-Bowel Syndrome and Intestinal Failure. Gastroenterology 2018, 154, 874–885. [Google Scholar] [CrossRef] [PubMed]
- Crenn, P.; Messing, B.; Cynober, L. Citrulline as a biomarker of intestinal failure due to enterocyte mass reduction. Clin. Nutr. 2008, 27, 328–339. [Google Scholar] [CrossRef]
- Curis, E.; Crenn, P.; Cynober, L. Citrulline and the gut. Curr. Opin Clin. Nutr. Metab. Care 2007, 10, 620–626. [Google Scholar] [CrossRef] [PubMed]
- Curis, E.; Nicolis, I.; Moinard, C.; Osowska, S.; Zerrouk, N.; Bénazeth, S.; Cynober, L. Almost all about citrulline in mammals. Amino Acids 2005, 29, 177–205. [Google Scholar] [CrossRef]
- Walker, V. Ammonia metabolism and hyperammonemic disorders. Adv. Clin. Chem. 2014, 67, 73–150. [Google Scholar]
- Windmueller, H.G.; Spaeth, A.E. Source and fate of circulating citrulline. Am. J. Physiol. 1981, 241, E473–E480. [Google Scholar] [CrossRef]
- Picot, D.; Garin, L.; Trivin, F.; Kossovsky, M.P.; Darmaun, D.; Thibault, R. Plasma citrulline is a marker of absorptive small bowel length in patients with transient enterostomy and acute intestinal failure. Clin. Nutr. 2010, 29, 235–242. [Google Scholar] [CrossRef]
- Fragkos, K.C.; Forbes, A. Citrulline as a marker of intestinal function and absorption in clinical settings: A systematic review and meta-analysis. United Eur. Gastroenterol. J. 2018, 6, 181–191. [Google Scholar] [CrossRef]
- Lau, T.; Owen, W.; Yu, Y.M.; Noviski, N.; Lyons, J.; Zurakowski, D.; Tsay, R.; Ajami, A.; Young, V.R.; Castillo, L. Arginine, citrulline, and nitric oxide metabolism in end-stage renal disease patients. J. Clin. Investig. 2000, 105, 1217–1225. [Google Scholar] [CrossRef]
- Marini, J.C.; Agarwal, U.; Robinson, J.L.; Yuan, Y.; Didelija, I.C.; Stoll, B.; Burrin, D.G. The intestinal-renal axis for arginine synthesis is present and functional in the neonatal pig. Am. J. Physiol. Endocrinol. Metab. 2017, 313, E233–E242. [Google Scholar] [CrossRef] [PubMed]
- Reddy, Y.S.; Kiranmayi, V.S.; Bitla, A.R.; Krishna, G.S.; Rao, P.V.; Sivakumar, V. Nitric oxide status in patients with chronic kidney disease. Indian J. Nephrol. 2015, 25, 287–291. [Google Scholar] [PubMed]
- Lovshin, J.; Yusta, B.; Iliopoulos, I.; Migirdicyan, A.; Dableh, L.; Brubaker, P.L.; Drucker, D.J. Ontogeny of the glucagon-like peptide-2 receptor axis in the developing rat intestine. Endocrinology 2000, 141, 4194–4201. [Google Scholar] [CrossRef]
- Wu, G.D.; Wang, W.; Traber, P.G. Isolation and characterization of the human sucrase-isomaltase gene and demonstration of intestine-specific transcriptional elements. J. Biol. Chem. 1992, 267, 7863–7870. [Google Scholar] [CrossRef] [PubMed]
- Honma, K.; Mochizuki, K.; Goda, T. Carbohydrate/fat ratio in the diet alters histone acetylation on the sucrase–isomaltase gene and its expression in mouse small intestine. Biochem. Biophys. Res. Commun. 2007, 357, 1124–1129. [Google Scholar] [CrossRef]
- Kitchen, P.A.; Fitzgerald, A.J.; Goodlad, R.A.; Barley, N.F.; Ghatei, M.A.; Legon, S.; Bloom, S.R.; Price, A.; Walters, J.R.F.; Forbes, A.; et al. Glucagon-like peptide-2 increases sucrase-isomaltase but not caudal-related homeobox protein-2 gene expression. Am. J. Physiol. Gastrointest. Liver Physiol. 2000, 278, G425–G428. [Google Scholar] [CrossRef] [PubMed]
- Petersen, Y.M.; Elnif, J.; Schmidt, M.; Sangild, P.T. Glucagon-like peptide 2 enhances maltase-glucoamylase and sucrase-isomaltase gene expression and activity in parenterally fed premature neonatal piglets. Pediatr. Res. 2002, 52, 498–503. [Google Scholar] [CrossRef]
- Chen, J.; Williams, S.; Ho, S.; Loraine, H.; Hagan, D.; Whaley, J.M.; Feder, J.N. Quantitative PCR tissue expression profiling of the human SGLT2 gene and related family members. Diabetes Ther. 2010, 1, 57–92. [Google Scholar] [CrossRef] [PubMed]
- Koepsell, H. Glucose transporters in the small intestine in health and disease. Pflugers Arch. 2020, 472, 1207–1248. [Google Scholar] [CrossRef] [PubMed]
- Lehmann, A.; Hornby, P.J. Intestinal SGLT1 in metabolic health and disease. Am. J. Physiol. Gastrointest. Liver Physiol. 2016, 310, G887–G898. [Google Scholar] [CrossRef] [PubMed]
- Brubaker, P.L.; Izzo, A.; Hill, M.; Drucker, D.J. Intestinal function in mice with small bowel growth induced by glucagon-like peptide-2. Am. J. Physiol. 1997, 272, E1050–E1058. [Google Scholar] [CrossRef]
- Cheeseman, C.I. Upregulation of SGLT-1 transport activity in rat jejunum induced by GLP-2 infusion in vivo. Am. J. Physiol. 1997, 273, R1965–R1971. [Google Scholar] [CrossRef]
- Kim, H.R.; Park, S.W.; Cho, H.J.; Chae, K.A.; Sung, J.M.; Kim, J.S.; Landowski, C.P.; Sun, D.; El-Aty, A.M.A.; Amidon, G.L.; et al. Comparative gene expression profiles of intestinal transporters in mice, rats and humans. Pharmacol. Res. 2007, 56, 224–236. [Google Scholar] [CrossRef]
- Kaech, S.M.; Whitfield, C.W.; Kim, S.K. The LIN-2/LIN-7/LIN-10 complex mediates basolateral membrane localization of the C. elegans EGF receptor LET-23 in vulval epithelial cells. Cell 1998, 94, 761–771. [Google Scholar] [CrossRef] [PubMed]
- Lozovatsky, L.; Abayasekara, N.; Piawah, S.; Walther, Z. CASK deletion in intestinal epithelia causes mislocalization of LIN7C and the DLG1/Scrib polarity complex without affecting cell polarity. Mol. Biol. Cell 2009, 20, 4489–4499. [Google Scholar] [CrossRef] [PubMed]
- Grimes, J.; Schaudies, P.; Davis, D.; Williams, C.; Curry, B.J.; Walker, M.D.; Koldovsky, O. Effect of short-term fasting/refeeding on epidermal growth factor content in the gastrointestinal tract of suckling rats. Proc. Soc. Exp. Biol. Med. 1992, 199, 75–80. [Google Scholar] [CrossRef]
- Nelson, D.W.; Murali, S.G.; Liu, X.; Koopmann, M.C.; Holst, J.J.; Ney, D.M. Insulin-like growth factor I and glucagon-like peptide-2 responses to fasting followed by controlled or ad libitum refeeding in rats. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2008, 294, R1175–R1184. [Google Scholar] [CrossRef] [PubMed]
- Bahrami, J.; Yusta, B.; Drucker, D.J. ErbB activity links the glucagon-like peptide-2 receptor to refeeding-induced adaptation in the murine small bowel. Gastroenterology 2010, 138, 2447–2456. [Google Scholar] [CrossRef]
- Gerdes, J.; Lemke, H.; Baisch, H.; Wacker, H.H.; Schwab, U.; Stein, H. Cell cycle analysis of a cell proliferation-associated human nuclear antigen defined by the monoclonal antibody Ki-67. J. Immunol. 1984, 133, 1710–1715. [Google Scholar] [CrossRef] [PubMed]
- Scholzen, T.; Gerdes, J. The Ki-67 protein: From the known and the unknown. J. Cell Physiol. 2000, 182, 311–322. [Google Scholar] [CrossRef]
- Drucker, D.J.; Erlich, P.; Asa, S.L.; Brubaker, P.L. Induction of intestinal epithelial proliferation by glucagon-like peptide 2. Proc. Natl. Acad. Sci. USA 1996, 93, 7911–7916. [Google Scholar] [CrossRef]
- Ørskov, C.; Hartmann, B.; Poulsen, S.S.; Thulesen, J.; Hare, K.J.; Holst, J.J. GLP-2 stimulates colonic growth via KGF, released by subepithelial myofibroblasts with GLP-2 receptors. Regul. Pept. 2005, 124, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Falco, E.C.; Lezo, A.; Calvo, P.; Rigazio, C.; Opramolla, A.; Verdun, L.; Cenacchi, G.; Pellegrini, M.; Spada, M.; Canavese, G. Case Report: Morphologic and Functional Characteristics of Intestinal Mucosa in a Child with Short Bowel Syndrome After Treatment with Teduglutide: Evidence in Favor of GLP-2 Analog Safety. Front. Nutr. 2022, 9, 866048. [Google Scholar] [CrossRef] [PubMed]
- Cheng, W.; Wang, K.; Zhao, Z.; Mao, Q.; Wang, G.; Li, Q.; Fu, Z.; Jiang, Z.; Wang, J.; Li, J. Exosomes-mediated Transfer of miR-125a/b in Cell-to-cell Communication: A Novel Mechanism of Genetic Exchange in the Intestinal Microenvironment. Theranostics 2020, 10, 7561–7580. [Google Scholar] [CrossRef]
- Zhou, Q.; Toivola, D.M.; Feng, N.; Greenberg, H.B.; Franke, W.W.; Omary, M.B. Keratin 20 helps maintain intermediate filament organization in intestinal epithelia. Mol. Biol. Cell 2003, 14, 2959–2971. [Google Scholar] [CrossRef] [PubMed]
- Bayrak, R.; Haltas, H.; Yenidunya, S. The value of CDX2 and cytokeratins 7 and 20 expression in differentiating colorectal adenocarcinomas from extraintestinal gastrointestinal adenocarcinomas: Cytokeratin 7-/20+ phenotype is more specific than CDX2 antibody. Diagn. Pathol. 2012, 7, 9. [Google Scholar] [CrossRef]
- Chan, C.W.M.; Wong, N.A.; Liu, Y.; Bicknell, D.; Turley, H.; Hollins, L.; Miller, C.J.; Wilding, J.L.; Bodmer, W.F. Gastrointestinal differentiation marker Cytokeratin 20 is regulated by homeobox gene CDX1. Proc. Natl. Acad. Sci. USA 2009, 106, 1936–1941. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.M.; Wang, H.L. Alteration of cytokeratin 7 and cytokeratin 20 expression profile is uniquely associated with tumorigenesis of primary adenocarcinoma of the small intestine. Am. J. Surg. Pathol. 2004, 28, 1352–1359. [Google Scholar] [CrossRef]
- Moll, R.; Franke, W.W.; Schiller, D.L.; Geiger, B.; Krepler, R. The catalog of human cytokeratins: Patterns of expression in normal epithelia, tumors and cultured cells. Cell 1982, 31, 11–24. [Google Scholar] [CrossRef]
- Moll, R.; Schiller, D.L.; Franke, W.W. Identification of protein IT of the intestinal cytoskeleton as a novel type I cytokeratin with unusual properties and expression patterns. J. Cell Biol. 1990, 111, 567–580. [Google Scholar] [CrossRef] [PubMed]
- Reiner, J.; Berlin, P.; Wobar, J.; Schäffler, H.; Bannert, K.; Bastian, M.; Vollmar, B.; Jaster, R.; Lamprecht, G.; Witte, M. Teduglutide Promotes Epithelial Tight Junction Pore Function in Murine Short Bowel Syndrome to Alleviate Intestinal Insufficiency. Dig. Dis. Sci. 2020, 65, 3521–3537. [Google Scholar] [CrossRef]
- Camilleri, M.; Madsen, K.; Spiller, R.; Van Meerveld, B.G.; Verne, G.N. Intestinal barrier function in health and gastrointestinal disease. Neurogastroenterol. Motil. 2012, 24, 503–512. [Google Scholar] [CrossRef]
- Schoultz, I.; Keita, A.V. The Intestinal Barrier and Current Techniques for the Assessment of Gut Permeability. Cells 2020, 9, 1909. [Google Scholar] [CrossRef]
- Bischoff, S.C.; Barbara, G.; Buurman, W.; Ockhuizen, T.; Schulzke, J.-D.; Serino, M.; Tilg, H.; Watson, A.; Wells, J.M.; Pihlsgård, M.; et al. Intestinal permeability—A new target for disease prevention and therapy. BMC Gastroenterol. 2014, 14, 189. [Google Scholar] [CrossRef]
- Fischer, A.; Gluth, M.; Pape, U.-F.; Wiedenmann, B.; Theuring, F.; Baumgart, D.C. Adalimumab prevents barrier dysfunction and antagonizes distinct effects of TNF-α on tight junction proteins and signaling pathways in intestinal epithelial cells. Am. J. Physiol. Gastrointest. Liver Physiol. 2013, 304, G970–G979. [Google Scholar] [CrossRef] [PubMed]
- Fischer, A.; Gluth, M.; Weege, F.; Pape, U.-F.; Wiedenmann, B.; Baumgart, D.C.; Theuring, F. Glucocorticoids regulate barrier function and claudin expression in intestinal epithelial cells via MKP-1. Am. J. Physiol. Gastrointest. Liver Physiol. 2014, 306, G218–G228. [Google Scholar] [CrossRef]
- Schulzke, J.-D.; Fromm, M.; Bentzel, C.J.; Zeitz, M.; Menge, H.; Riecken, E.-O. Ion transport in the experimental short bowel syndrome of the rat. Gastroenterology 1992, 102, 497–504. [Google Scholar] [CrossRef]
- Schulzke, J.; Fromm, M.; Hippel, C.V.; Sandforth, F.; Menge, H.; Bentzel, C.; Riecken, E. Adaptation of epithelial ion transport in the short bowel syndrome. Digestion 1990, 46 (Suppl. S2), 467–471. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, B.; Kolli, A.R.; Esch, M.B.; Abaci, H.E.; Shuler, M.L.; Hickman, J.J. TEER measurement techniques for in vitro barrier model systems. J. Lab. Autom. 2015, 20, 107–126. [Google Scholar] [CrossRef]
- Brown, D.R.; O’Grady, S.M. The Ussing chamber and measurement of drug actions on mucosal ion transport. Curr. Protoc. Pharmacol. 2008, 7, 12. [Google Scholar] [CrossRef] [PubMed]
- Galipeau, H.J.; Verdu, E.F. The complex task of measuring intestinal permeability in basic and clinical science. Neurogastroenterol. Motil. 2016, 28, 957–965. [Google Scholar] [CrossRef] [PubMed]
- Fromm, M.; Krug, S.M.; Zeissig, S.; Richter, J.F.; Rosenthal, R.; Schulzke, J.-D.; Günzel, D. High-resolution analysis of barrier function. Ann. N. Y. Acad. Sci. 2009, 1165, 74–81. [Google Scholar] [CrossRef]
- Krug, S.M.; Schulzke, J.D.; Fromm, M. Tight junction, selective permeability, and related diseases. Semin. Cell Dev. Biol. 2014, 36, 166–176. [Google Scholar] [CrossRef]
- Awad, K.; Barmeyer, C.; Bojarski, C.; Nagel, O.; Lee, I.-F.M.; Schweiger, M.R.; Schulzke, J.-D.; Bücker, R. Impaired Intestinal Permeability of Tricellular Tight Junctions in Patients with Irritable Bowel Syndrome with Mixed Bowel Habits (IBS-M). Cells 2023, 12, 236. [Google Scholar] [CrossRef] [PubMed]
- González-González, M.; Díaz-Zepeda, C.; Eyzaguirre-Velásquez, J.; González-Arancibia, C.; Bravo, J.A.; Julio-Pieper, M. Investigating Gut Permeability in Animal Models of Disease. Front. Physiol. 2018, 9, 1962. [Google Scholar] [CrossRef]
- Khoshbin, K.; Khanna, L.; Maselli, D.; Atieh, J.; Breen-Lyles, M.; Arndt, K.; Rhoten, D.; Dyer, R.B.; Singh, R.J.; Nayar, S.; et al. Development and Validation of Test for “Leaky Gut” Small Intestinal and Colonic Permeability Using Sugars in Healthy Adults. Gastroenterology 2021, 161, 463–475.e13. [Google Scholar] [CrossRef]
- Meddings, J.B. Review article: Intestinal permeability in Crohn’s disease. Aliment. Pharmacol. Ther. 1997, 11 (Suppl. S3), 47–53; discussion 53–56. [Google Scholar] [CrossRef] [PubMed]
- Buhner, S.; Buning, C.; Genschel, J.; Kling, K.; Herrmann, D.; Dignass, A.; Kuechler, I.; Krueger, S.; Schmidt, H.H.-J.; Lochs, H. Genetic basis for increased intestinal permeability in families with Crohn’s disease: Role of CARD15 3020insC mutation? Gut 2006, 55, 342–347. [Google Scholar] [CrossRef]
- Büning, C.; Geissler, N.; Prager, M.; Sturm, A.; Baumgart, D.C.; Büttner, J.; Bühner, S.; Haas, V.; Lochs, H. Increased small intestinal permeability in ulcerative colitis: Rather genetic than environmental and a risk factor for extensive disease? Inflamm. Bowel Dis. 2012, 18, 1932–1939. [Google Scholar] [CrossRef]
- Bijlsma, P.B.; Peeters, R.A.; Groot, J.A.; Dekker, P.R.; Taminiau, J.A.; Van Der Meer, R. Differential in vivo and in vitro intestinal permeability to lactulose and mannitol in animals and humans: A hypothesis. Gastroenterology 1995, 108, 687–696. [Google Scholar] [CrossRef]
- Delahunty, T.; Hollander, D. A comparison of intestinal permeability between humans and three common laboratory animals. Comp. Biochem. Physiol. Part A Physiol. 1987, 86, 565–567. [Google Scholar] [CrossRef]
- Hallbäck, D.-A.; Hultén, L.; Jodal, M.; Lindhagen, J.; Lundgren, O. Evidence for the existence of a countercurrent exchanger in the small intestine in man. Gastroenterology 1978, 74, 683–690. [Google Scholar] [CrossRef] [PubMed]
- Hallback, D.A.; Jodal, M.; Mannischeff, M.; Lundgren, O. Tissue osmolality in intestinal villi of four mammals in vivo and in vitro. Acta Physiol. Scand. 1991, 143, 271–277. [Google Scholar] [CrossRef]
- Prager, M.; Büttner, J.; Grunert, P.; Ellinghaus, D.; Büning, C. A Promoter Variant Within the Aryl Hydrocarbon Receptor Gene Is Associated with an Epithelial Barrier Defect in Smokers with Crohn’s Disease. Inflamm. Bowel Dis. 2016, 22, 2356–2368. [Google Scholar] [CrossRef] [PubMed]
- Bjarnason, I. Intestinal permeability. Gut 1994, 35 (Suppl. S1), S18–S22. [Google Scholar] [CrossRef]
- Prager, M.; Büttner, J.; Haas, V.; Baumgart, D.C.; Sturm, A.; Zeitz, M.; Büning, C. The JAK2 variant rs10758669 in Crohn’s disease: Altering the intestinal barrier as one mechanism of action. Int. J. Color. Dis. 2012, 27, 565–573. [Google Scholar] [CrossRef]
- Iturrino, J.; Camilleri, M.; Acosta, A.; O’neill, J.; Burton, D.; Varayil, J.E.; Carlson, P.J.; Zinsmeister, A.R.; Hurt, R. Acute Effects of a Glucagon-Like Peptide 2 Analogue, Teduglutide, on Gastrointestinal Motor Function and Permeability in Adult Patients with Short Bowel Syndrome on Home Parenteral Nutrition. JPEN J. Parenter. Enter. Nutr. 2016, 40, 1089–1095. [Google Scholar] [CrossRef] [PubMed]
- Sigalet, D.L.; Martin, G.R.; Poole, A. Differential sugar absorption as a marker for adaptation in short bowel syndrome. J. Pediatr. Surg. 2000, 35, 661–664. [Google Scholar] [CrossRef]
- Hadjiyanni, I.; Li, K.K.; Drucker, D.J. Glucagon-like peptide-2 reduces intestinal permeability but does not modify the onset of type 1 diabetes in the nonobese diabetic mouse. Endocrinology 2009, 150, 592–599. [Google Scholar] [CrossRef]
- Kouris, G.J.; Liu, Q.; Rossi, H.; Djuricin, G.; Gattuso, P.; Nathan, C.; A Weinstein, R.; A Prinz, R. The effect of glucagon-like peptide 2 on intestinal permeability and bacterial translocation in acute necrotizing pancreatitis. Am. J. Surg. 2001, 181, 571–575. [Google Scholar] [CrossRef] [PubMed]


| Short Bowel Syndrome | Control | |
|---|---|---|
| Number | 59 | 19 |
| Age (median years [range]) | 60 (21–88) | 55 (33–86) |
| Sex (m/f) | 21 (36%)/38 (64%) | 4 (21%)/15 (79%) |
| Teduglutide treatment (yes/no) | 41 (70%)/18 (30%) | - |
| Disease duration (years) | 11.1 (±8.3) | |
| Short bowel syndrome etiology | ||
| Vascular disease | 21 (35.6%) | |
| Inflammatory bowel disease | 13 (22.0%) | |
| Traumatic injury | 6 (10.2%) | |
| Bowel obstruction | 11 (18.7%) | |
| Cancer | 3 (5.1%) | |
| Other (Diverticulitis, Perforation, Aganglionosis) | 5 (8.5%) | |
| Colon continuity | ||
| continuity | 40 | healthy colon |
| remaining small bowel length (cm) | 74.2 (±41.2) | |
| no continuity | 19 | |
| remaining small bowel length (cm) | 83.4 (±50.0) | |
| Parenteral support (kcal/week) | 7471 (±4259) |
| Variant | Exon | Functional Domain | SNP Database | Amino Acid Exchange | Nucleotide Exchange | SIFT Score | PolyPhen Score |
|---|---|---|---|---|---|---|---|
| p.R41S | 1 | N-Terminus | rs114271428 | Arg<Ser | AGG<AGC | 0.04 | 0.00 |
| p.V234I | 6 | Transmembrane 2 | rs61730822 | Val<Ile | GTC<ATC | 0.22 | 0.003 |
| p.D470N | 13 | C-Terminus | rs17681684 | Asn<Asp | GAC<AAC | 0.89 | 0.00 |
| p.G158G | 4 | Gly<Gly | GAA<GAG | ||||
| p.H504H | 13 | His<His | CAT<CAC | ||||
| c.1-199g<a | 5’UTR | pot. promoter | rs3760507 | Common Polymorphism | |||
| c.1-608a<a | 5’UTR | pot. promoter | rs3760508 | Common Polymorphism | |||
| c.1-635c<g | 5’UTR | pot. promoter | no entry | ||||
| c.1-770c<g | 5’UTR | pot. promoter | rs2047664 | Common Polymorphism | |||
| Relative Gene Expression | Relative Gene Expression (n = 18) | |||||
|---|---|---|---|---|---|---|
| Gene | Control (n = 7) | SBS-(Untreated) (n = 37) | p-Value § | SBS Prior Treatment | SBS on TED | p-Value # |
| Mean (±SD) | Mean (±SD) | Mean (±SD) | Mean (±SD) | |||
| Tight junction | ||||||
| CLDN10 | 0.0007 (±0.001) | 0.0008 (±0.0017) | 0.66 | 0.0003 (±0.0017) | 0.0001 (±0.0002) | 0.27 |
| CLDN15 | 0.0103 (±0.0118) | 0.0132 (±0.014) | 0.75 | 0.0132 (±0.017) | 0.016 (±0.01) | 0.30 |
| OCLN | 0.0028 (±0.0009) | 0.0026 (±0.0011) | 0.79 | 0.0025 (±0.0009) | 0.0029 (±0.0015) | 0.55 |
| ZO-1 | 0.0514 (±0.045) | 0.0357 (±0.031) | 0.21 | 0.031 (±0.015) | 0.033 (±0.008) | 0.73 |
| CRB3 | 0.013 (±0.003) | 0.015 (±0.008) | 0.80 | 0.0158 (±0.016) | 0.0128 (±0.0028) | 0.68 |
| CASK | 0.053 (±0.012) | 0.043 (±0.014) | 0.006 | 0.0389 (±0.013) | 0.054 (±0.014) | 0.009 |
| Nutrient transport | ||||||
| SI | 0.72 (±0.023) | 0.477 (±0.313) | 0.030 | 0.417 (±0.296) | 0.673 (±0.311) | 0.024 |
| SGLT1 | 0.262 (±0.082) | 0.211 (±0.145) | 0.30 | 0.169 (±0.127) | 0.309 (±0.146) | 0.002 |
| Proliferation | ||||||
| MKI67 | 0.0066 (±0.002) | 0.00723 (±0.005) | 0.93 | 0.0071 (±0.0039) | 0.0069 (±0.0052) | 0.78 |
| Structure | ||||||
| CK20 | 0.534 (±0.201) | 1.05 (±1.55) | 0.93 | 1.0 (±1.2) | 0.449 (±0.181) | 0.06 |
| Citrulline (µmol/L) | - | 26.8 (±17.7) | 23.0 (±14) | 42.2 (±22.3) | <0.001 | |
| kcal/week | - | 7755 (±3818) | 7255 (±3928) | 3362 (±4342) | <0.001 | |
| rSBL (cm) | - | 77.2 (±42.1) | 68.8 (±38.3) | 68.8 (±38.3) | - | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Büttner, J.; Blüthner, E.; Greif, S.; Kühl, A.; Elezkurtaj, S.; Ulrich, J.; Maasberg, S.; Jochum, C.; Tacke, F.; Pape, U.-F. Predictive Potential of Biomarkers of Intestinal Barrier Function for Therapeutic Management with Teduglutide in Patients with Short Bowel Syndrome. Nutrients 2023, 15, 4220. https://doi.org/10.3390/nu15194220
Büttner J, Blüthner E, Greif S, Kühl A, Elezkurtaj S, Ulrich J, Maasberg S, Jochum C, Tacke F, Pape U-F. Predictive Potential of Biomarkers of Intestinal Barrier Function for Therapeutic Management with Teduglutide in Patients with Short Bowel Syndrome. Nutrients. 2023; 15(19):4220. https://doi.org/10.3390/nu15194220
Chicago/Turabian StyleBüttner, Janine, Elisabeth Blüthner, Sophie Greif, Anja Kühl, Sefer Elezkurtaj, Jan Ulrich, Sebastian Maasberg, Christoph Jochum, Frank Tacke, and Ulrich-Frank Pape. 2023. "Predictive Potential of Biomarkers of Intestinal Barrier Function for Therapeutic Management with Teduglutide in Patients with Short Bowel Syndrome" Nutrients 15, no. 19: 4220. https://doi.org/10.3390/nu15194220
APA StyleBüttner, J., Blüthner, E., Greif, S., Kühl, A., Elezkurtaj, S., Ulrich, J., Maasberg, S., Jochum, C., Tacke, F., & Pape, U. -F. (2023). Predictive Potential of Biomarkers of Intestinal Barrier Function for Therapeutic Management with Teduglutide in Patients with Short Bowel Syndrome. Nutrients, 15(19), 4220. https://doi.org/10.3390/nu15194220








