Whole Dietary Patterns, Cognitive Decline and Cognitive Disorders: A Systematic Review of Prospective and Intervention Studies
Abstract
:1. Introduction
Review Aims
- i.
- What are the associations between any a-priori or a-posteriori DP and outcomes of cognitive ageing across the adult life course?
- ii.
- What is the effect of DPs on cognitive ageing outcomes?
2. Methods
2.1. Study Protocol
2.2. Inclusion and Exclusion Criteria
2.3. Search Strategy and Data Sources
2.4. Data Selection and Extraction
2.5. Risk of Bias Assessment
2.6. Data Synthesis
3. Results
3.1. Study Selection
3.2. Overview of Prospective Studies
3.2.1. Assessment of Dietary Intake in Prospective Studies
3.2.2. Assessment of DPs in Prospective Studies
3.3. Risk of Bias in Prospective Studies
3.4. Associations between DPs and Global Cognitive Performance
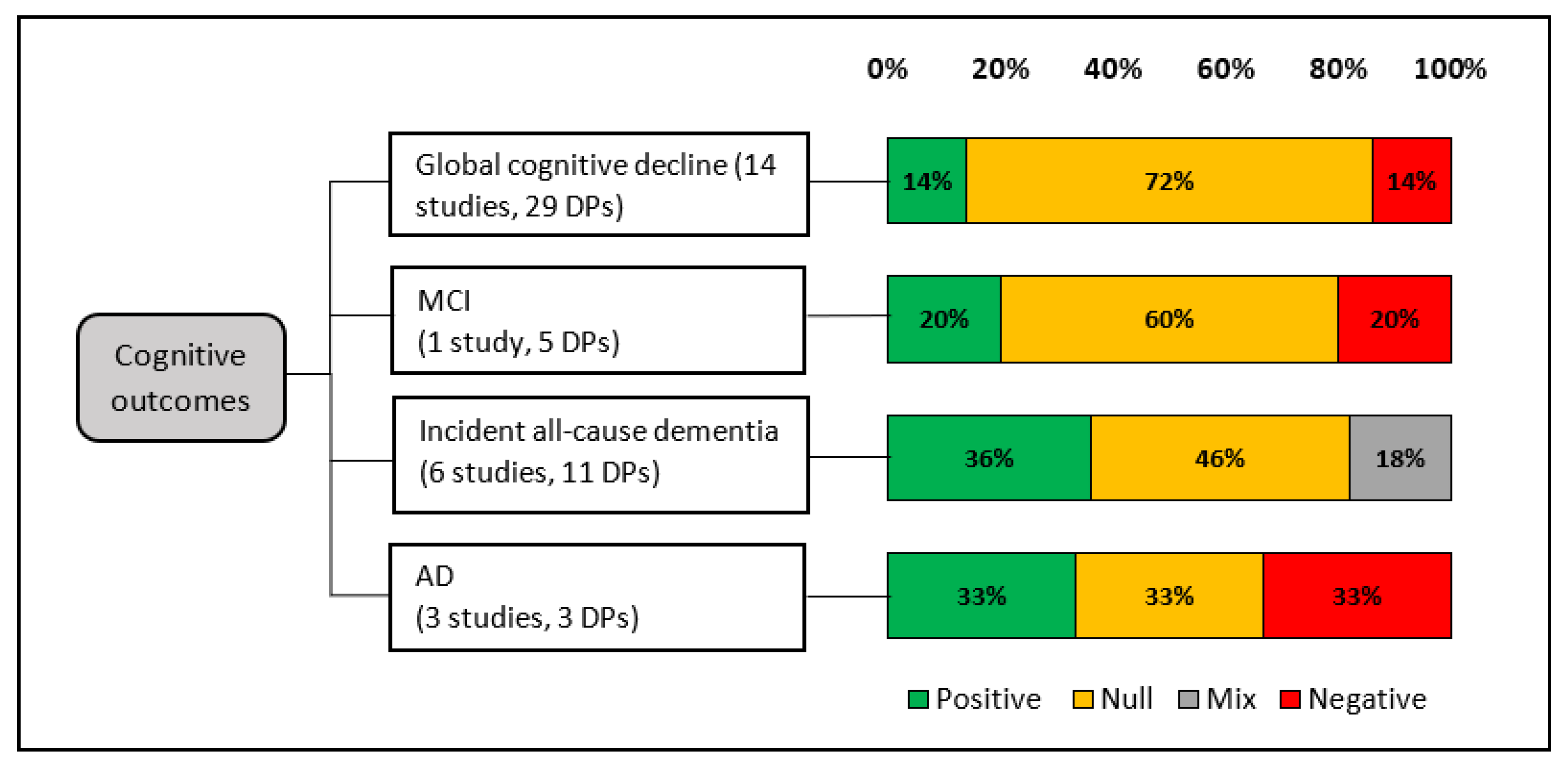
3.4.1. Associations between DPs and Global Cognitive Decline
Mediterranean Diet and Global Cognitive Decline
DASH Diet and Global Cognitive Decline
MIND Diet and Global Cognitive Decline
AHEI-2010 and Global Cognitive Decline
Other a-Priori DPs and Global Cognitive Decline
A-Posteriori DPs and Global Cognitive Decline
3.5. Associations between DPs and Cognitive Disorders
3.5.1. DPs and MCI
3.5.2. DPs and Incident All-Cause Dementia
3.5.3. Adherence to Examined DPs and AD
3.5.4. Adherence to Examined DPs and Other Outcomes Related to Cognitive Disorders
3.6. Overview of Intervention Studies
3.6.1. Diet Intervention
3.6.2. Assessment of Outcomes
3.6.3. Effect of Mediterranean Diet on Cognitive Outcomes
3.6.4. Effects of Other Diets on Cognitive Outcomes
3.7. Risk of Bias in Intervention Studies
4. Discussion
4.1. Summary of Overall Findings
4.1.1. Methodological Inconsistencies in Prospective Studies
Assessment of Dietary Patterns Exposure
Assessment of Cognitive Outcomes in the Prospective Studies
Population and Duration of Exposure
4.2. Strengths
4.3. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Livingston, G.; Huntley, J.; Sommerlad, A.; Ames, D.; Ballard, C.; Banerjee, S.; Brayne, C.; Burns, A.; Cohen-Mansfield, J.; Cooper, C. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 2020, 396, 413–446. [Google Scholar] [PubMed]
- McEvoy, C.T.; Leng, Y.; Peeters, G.M.; Kaup, A.R.; Allen, I.E.; Yaffe, K. Interventions involving a major dietary component improve cognitive function in cognitively healthy adults: A systematic review and meta-analysis. Nutr. Res. 2019, 66, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yassine, H.N.; Samieri, C.; Livingston, G.; Glass, K.; Wagner, M.; Tangney, C.; Plassman, B.L.; Ikram, M.A.; Voigt, R.M.; Gu, Y.; et al. Nutrition state of science and dementia prevention: Recommendations of the Nutrition for Dementia Prevention Working Group. Lancet Healthy Longev. 2022, 3, e501–e512. [Google Scholar] [CrossRef] [PubMed]
- Tapsell, L.C.; Neale, E.P.; Satija, A.; Hu, F.B. Foods, nutrients, and dietary patterns: Interconnections and implications for dietary guidelines. Adv. Nutr. 2016, 7, 445–454. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schulz, C.-A.; Oluwagbemigun, K.; Nöthlings, U. Advances in dietary pattern analysis in nutritional epidemiology. Eur. J. Nutr. 2021, 60, 4115–4130. [Google Scholar] [CrossRef] [PubMed]
- Shakersain, B.; Santoni, G.; Larsson, S.C.; Faxen-Irving, G.; Fastbom, J.; Fratiglioni, L.; Xu, W. Prudent diet may attenuate the adverse effects of Western diet on cognitive decline. Alzheimer’s Dement. 2016, 12, 100–109. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Trichopoulou, A.; Kyrozis, A.; Rossi, M.; Katsoulis, M.; Trichopoulos, D.; la Vecchia, C.; Lagiou, P. Mediterranean diet and cognitive decline over time in an elderly Mediterranean population. Eur. J. Nutr. 2015, 54, 1311–1321. [Google Scholar] [CrossRef]
- Tanaka, T.; Talegawkar, S.A.; Jin, Y.; Colpo, M.; Ferrucci, L.; Bandinelli, S. Adherence to a mediterranean diet protects from cognitive decline in the invecchiare in Chianti study of aging. Nutrients 2018, 10, 207. [Google Scholar] [CrossRef] [Green Version]
- Munoz-Garcia, M.I.; Toledo, E.; Razquin, C.; Dominguez, L.J.; Maragarone, D.; Martinez-Gonzalez, J.; Martinez-Gonzalez, M.A. “a-priori” Dietary Patterns and Cognitive Function in the SUN Project. Neuroepidemiology 2020, 54, 45–57. [Google Scholar] [CrossRef]
- Akbaraly, T.N.; Singh-Manoux, A.; Dugravot, A.; Brunner, E.J.; Kivimaki, M.; Sabia, S. Association of Midlife Diet with Subsequent Risk for Dementia. JAMA J. Am. Med. Assoc. 2019, 321, 957–968. [Google Scholar] [CrossRef]
- Cherbuin, N.; Anstey, K.J. The mediterranean diet is not related to cognitive change in a large prospective investigation: The PATH through life study. Am. J. Geriatr. Psychiatry 2012, 20, 635–639. [Google Scholar] [CrossRef]
- Martinez-Lapiscina, E.H.; Clavero, P.; Toledo, E.; Estruch, R.; Salas-Salvado, J.; San Julian, B.; Sanchez-Tainta, A.; Ros, E.; Valls-Pedret, C.; Martinez-Gonzalez, M.A. Mediterranean diet improves cognition: The PREDIMED-NAVARRA randomised trial. J. Neurol. Neurosurg. Psychiatry 2013, 84, 1318–1325. [Google Scholar] [CrossRef] [Green Version]
- Valls-Pedret, C.; Sala-Vila, A.; Serra-Mir, M.; Corella, D.; de la Torre, R.; Martinez-Gonzalez, M.A.; Martinez-Lapiscina, E.H.; Fito, M.; Perez-Heras, A.; Salas-Salvado, J.; et al. Mediterranean diet and age-related cognitive decline: A randomized clinical trial. JAMA Intern. Med. 2015, 175, 1094–1103. [Google Scholar] [CrossRef] [Green Version]
- Knight, A.; Bryan, J.; Wilson, C.; Hodgson, J.M.; Davis, C.R.; Murphy, K.J. The mediterranean diet and cognitive function among healthy older adults in a 6-month randomised controlled trial: The MedLey study. Nutrients 2016, 8, 579. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van de Rest, O.; Berendsen, A.A.; Haveman-Nies, A.; de Groot, L.C. Dietary patterns, cognitive decline, and dementia: A systematic review. Adv. Nutr. 2015, 6, 154–168. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van den Brink, A.C.; Brouwer-Brolsma, E.M.; Berendsen, A.A.M.; van de Rest, O. The Mediterranean, Dietary Approaches to Stop Hypertension (DASH), and Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) Diets Are Associated with Less Cognitive Decline and a Lower Risk of Alzheimer’s Disease-A Review. Adv. Nutr. 2019, 10, 1040–1065. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, X.; Maguire, B.; Brodaty, H.; O’Leary, F. Dietary patterns and cognitive health in older adults: A systematic review. J. Alzheimer’s Dis. 2019, 67, 583–619. [Google Scholar] [CrossRef]
- Gauci, S.; Young, L.M.; Arnoldy, L.; Lassemillante, A.-C.; Scholey, A.; Pipingas, A. Dietary patterns in middle age: Effects on concurrent neurocognition and risk of age-related cognitive decline. Nutr. Rev. 2021. [Google Scholar] [CrossRef]
- Rodrigues, B.; Asamane, E.A.; Magalhães, R.; Sousa, N.; Thompson, J.L.; Santos, N.C. The association of dietary patterns with cognition through the lens of neuroimaging—A systematic review. Ageing Res. Rev. 2020, 63, 101145. [Google Scholar] [CrossRef]
- Samadi, M.; Moradi, S.; Moradinazar, M.; Mostafai, R.; Pasdar, Y. Dietary pattern in relation to the risk of Alzheimer’s disease: A systematic review. Neurol. Sci. 2019, 40, 2031–2043. [Google Scholar] [CrossRef]
- Liu, Y.H.; Gao, X.; Na, M.; Kris-Etherton, P.M.; Mitchell, D.C.; Jensen, G.L. Dietary Pattern, Diet Quality, and Dementia: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. J Alzheimers Dis. 2020, 78, 151–168. [Google Scholar] [CrossRef]
- Milte, C.M.; McNaughton, S.A. Dietary patterns and successful ageing: A systematic review. Eur. J. Nutr. 2016, 55, 423–450. [Google Scholar] [CrossRef] [Green Version]
- Cao, L.; Tan, L.; Wang, H.F.; Jiang, T.; Zhu, X.C.; Lu, H.; Tan, M.S.; Yu, J.T. Dietary Patterns and Risk of Dementia: A Systematic Review and Meta-Analysis of Cohort Studies. Mol. Neurobiol. 2016, 53, 6144–6154. [Google Scholar] [CrossRef]
- McBean, L.; O’Reilly, S. Diet quality interventions to prevent neurocognitive decline: A systematic review and meta-analysis. Eur. J. Clin. Nutr. 2021, 76, 1060–1072. [Google Scholar] [CrossRef]
- Limongi, F.; Siviero, P.; Bozanic, A.; Noale, M.; Veronese, N.; Maggi, S. The effect of adherence to the Mediterranean diet on late-life cognitive disorders: A systematic review. J. Am. Med. Dir. Assoc. 2020, 21, 1402–1409. [Google Scholar] [CrossRef]
- Moradi, S.; Moloudi, J.; Moradinazar, M.; Sarokhani, D.; Nachvak, S.M.; Samadi, M. Adherence to Healthy Diet Can Delay Alzheimer’s Diseases Development: A Systematic Review and Meta-Analysis. Prev. Nutr. Food Sci. 2020, 25, 325–337. [Google Scholar] [CrossRef]
- Kheirouri, S.; Alizadeh, M. MIND diet and cognitive performance in older adults: A systematic review. Crit. Rev. Food Sci. Nutr. 2022, 62, 8059–8077. [Google Scholar] [CrossRef]
- Hosking, D.E.; Nettelbeck, T.; Wilson, C.; Danthiir, V. Retrospective lifetime dietary patterns predict cognitive performance in community-dwelling older Australians. Br. J. Nutr. 2014, 112, 228–237. [Google Scholar] [CrossRef] [Green Version]
- Salthouse, T.A. When does age-related cognitive decline begin? Neurobiol. Aging 2009, 30, 507–514. [Google Scholar] [CrossRef] [Green Version]
- Townsend, R.F.; Woodside, J.V.; Prinelli, F.; O’Neill, R.F.; McEvoy, C.T. Associations Between Dietary Patterns and Neuroimaging Markers: A Systematic Review. Front. Nutr. 2022, 9. [Google Scholar] [CrossRef]
- Black, D.W.; Grant, J.E. DSM-5® Guidebook: The Essential Companion to the Diagnostic and Statistical Manual of Mental Disorders; American Psychiatric Pub: Washington, DC, USA, 2014. [Google Scholar]
- Bramer, W.; Bain, P. Updating search strategies for systematic reviews using EndNote. J. Med. Libr. Assoc. JMLA 2017, 105, 285. [Google Scholar] [CrossRef]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses; Ottawa Hospital Research Institute: Ottawa, ON, Canada, 2000. [Google Scholar]
- Sterne, J.A.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366. [Google Scholar] [CrossRef] [Green Version]
- Cadar, D.; Pikhart, H.; Mishra, G.; Stephen, A.; Kuh, D.; Richards, M. The role of lifestyle behaviors on 20-year cognitive decline. J. Aging Res. 2012, 2012, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Chou, Y.C.; Lee, M.S.; Chiou, J.M.; Chen, T.F.; Chen, Y.C.; Chen, J.H. Association of diet quality and vegetable variety with the risk of cognitive decline in Chinese older adults. Nutrients 2019, 11, 1666. [Google Scholar] [CrossRef] [Green Version]
- Daniel, G.D.; Chen, H.; Bertoni, A.G.; Rapp, S.R.; Fitzpatrick, A.L.; Luchsinger, J.A.; Wood, A.C.; Hughes, T.M.; Burke, G.L.; Hayden, K.M. DASH diet adherence and cognitive function: Multi-ethnic study of atherosclerosis. Clin. Nutr. ESPEN 2021, 46, 223–231. [Google Scholar] [CrossRef]
- Hossain, S.; Beydoun, M.A.; Weiss, J.; Kuczmarski, M.F.; Evans, M.K.; Zonderman, A.B. Longitudinal associations between dietary quality and Alzheimer’s disease genetic risk on cognitive performance among African American adults. Br. J. Nutr. 2020, 124, 1264–1276. [Google Scholar] [CrossRef] [Green Version]
- Lutski, M.; Weinstein, G.; Ben-Zvi, S.; Goldbourt, U.; Tanne, D. Adherence to Mediterranean diet and subsequent cognitive decline in men with cardiovascular disease. Nutr. Neurosci. 2020, 25, 91–99. [Google Scholar] [CrossRef]
- Mannikko, R.; Komulainen, P.; Schwab, U.; Heikkila, H.M.; Savonen, K.; Hassinen, M.; Hanninen, T.; Kivipelto, M.; Rauramaa, R. The Nordic diet and cognition—The DR’s EXTRA Study. Br. J. Nutr. 2015, 114, 231–239. [Google Scholar] [CrossRef] [Green Version]
- McEvoy, C.T.; Hoang, T.; Sidney, S.; Steffen, L.M.; Jacobs, D.R.; Shikany, J.M.; Wilkins, J.T.; Yaffe, K. Dietary patterns during adulthood and cognitive performance in midlife: The CARDIA study. Neurology 2019, 92, E1589–E1599. [Google Scholar] [CrossRef]
- Moustafa, B.; Trifan, G.; Isasi, C.R.; Lipton, R.B.; Sotres-Alvarez, D.; Cai, J.; Tarraf, W.; Stickel, A.; Mattei, J.; Talavera, G.A.; et al. Association of Mediterranean Diet with Cognitive Decline Among Diverse Hispanic or Latino Adults from the Hispanic Community Health Study/Study of Latinos. JAMA Netw. Open 2022, 5, E2221982. [Google Scholar] [CrossRef]
- Van Lent, D.M.; O’Donnell, A.; Beiser, A.S.; Vasan, R.S.; Decarli, C.S.; Scarmeas, N.; Wagner, M.; Jacques, P.F.; Seshadri, S.; Himali, J.J.; et al. Mind Diet Adherence and Cognitive Performance in the Framingham Heart Study. J. Alzheimer’s Dis. 2021, 82, 827–839. [Google Scholar] [CrossRef]
- Wade, A.T.; Elias, M.F.; Murphy, K.J. Adherence to a Mediterranean diet is associated with cognitive function in an older non-Mediterranean sample: Findings from the Maine-Syracuse Longitudinal Study. Nutr. Neurosci. 2019, 24, 542–553. [Google Scholar] [CrossRef] [PubMed]
- Charisis, S.; Ntanasi, E.; Yannakoulia, M.; Anastasiou, C.A.; Kosmidis, M.H.; Dardiotis, E.; Hadjigeorgiou, G.; Sakka, P.; Scarmeas, N. Mediterranean diet and risk for dementia and cognitive decline in a Mediterranean population. J. Am. Geriatr. Soc. 2021, 69, 1548–1559. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.C.; Jung, C.C.; Chen, J.H.; Chiou, J.M.; Chen, T.F.; Chen, Y.F.; Tang, S.C.; Yeh, S.J.; Lee, M.S. Association of Dietary Patterns with Global and Domain-Specific Cognitive Decline in Chinese Elderly. J. Am. Geriatr. Soc. 2017, 65, 1159–1167. [Google Scholar] [CrossRef]
- Mazza, E.; Fava, A.; Ferro, Y.; Moraca, M.; Rotundo, S.; Colica, C.; Provenzano, F.; Terracciano, R.; Greco, M.; Foti, D.; et al. Impact of legumes and plant proteins consumption on cognitive performances in the elderly. J. Transl. Med. 2017, 15, 109. [Google Scholar] [CrossRef] [Green Version]
- Nishi, S.K.; Babio, N.; Gomez-Martinez, C.; Martinez-Gonzalez, M.A.; Ros, E.; Corella, D.; Castaner, O.; Martinez, J.A.; Alonso-Gomez, A.M.; Warnberg, J.; et al. Mediterranean, DASH, and MIND Dietary Patterns and Cognitive Function: The 2-Year Longitudinal Changes in an Older Spanish Cohort. Front Aging Neurosci. 2021, 13, 782067. [Google Scholar] [CrossRef]
- Shang, X.; Hodge, A.M.; Hill, E.; Zhu, Z.; He, M. Associations of dietary pattern and sleep duration with cognitive decline in community-dwelling older adults: A seven-year follow-up cohort study. J. Alzheimer’s Dis. 2021, 82, 1559–1571. [Google Scholar] [CrossRef]
- Walters, M.J.; Sterling, J.; Quinn, C.; Ganzer, C.; Osorio, R.S.; Andrews, R.D.; Matthews, D.C.; Vallabhajosula, S.; de Leon, M.J.; Isaacson, R.S. Associations of lifestyle and vascular risk factors with Alzheimer’s brain biomarker changes during middle age: A 3-year longitudinal study in the broader New York City area. BMJ Open 2018, 8, e023664. [Google Scholar] [CrossRef] [Green Version]
- Berendsen, A.M.; Kang, J.H.; Feskens, E.J.M.; de Groot, C.; Grodstein, F.; van de Rest, O. Association of Long-Term Adherence to the MIND Diet with Cognitive Function and Cognitive Decline in American Women. J. Nutr. Health Aging 2018, 22, 222–229. [Google Scholar] [CrossRef]
- Mattei, J.; Bigornia, S.J.; Sotos-Prieto, M.; Scott, T.; Gao, X.; Tucker, K.L. The Mediterranean diet and 2-year change in cognitive function by status of type 2 diabetes and glycemic control. Diabetes Care 2019, 42, 1372–1379. [Google Scholar] [CrossRef]
- Agarwal, P.; Dhana, K.; Barnes, L.L.; Holl, T.M.; Zhang, Y.; Evans, D.A.; Morris, M.C. Unhealthy foods may attenuate the beneficial relation of a Mediterranean diet to cognitive decline. Alzheimer’s Dement. 2021, 17, 1157–1165. [Google Scholar] [CrossRef] [PubMed]
- Berendsen, A.A.M.; Kang, J.H.; van de Rest, O.; Feskens, E.J.M.; de Groot, L.; Grodstein, F. The Dietary Approaches to Stop Hypertension Diet, Cognitive Function, and Cognitive Decline in American Older Women. J. Am. Med. Dir. Assoc. 2017, 18, 427–432. [Google Scholar] [CrossRef] [PubMed]
- Boumenna, T.; Scott, T.M.; Lee, J.S.; Zhang, X.; Kriebel, D.; Tucker, K.L.; Palacios, N. MIND Diet and Cognitive Function in Puerto Rican Older Adults. J. Gerontol. A Biol. Sci. Med. Sci. 2022, 77, 605–613. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Liu, Z.; Sachdev, P.S.; Kochan, N.A.; Brodaty, H.; O’Leary, F. Association of adherence to the Australian Dietary Guidelines with cognitive performance and cognitive decline in the Sydney Memory and Ageing Study: A longitudinal analysis. J. Nutr. Sci. 2021, 10, e86. [Google Scholar] [CrossRef]
- Chen, X.; Liu, Z.; Sachdev, P.S.; Kochan, N.A.; O’Leary, F.; Brodaty, H. Association of Dietary Patterns with Cognitive Function and Cognitive Decline in Sydney Memory and Ageing Study: A Longitudinal Analysis. J. Acad. Nutr. Diet. 2022, 122, 949–960.e915. [Google Scholar] [CrossRef]
- Corley, J.; Deary, I.J. Dietary patterns and trajectories of global- and domain-specific cognitive decline in the Lothian Birth Cohort 1936. Br. J. Nutr. 2021, 126, 1237–1246. [Google Scholar] [CrossRef]
- Dearborn-Tomazos, J.L.; Wu, A.; Steffen, L.M.; Anderson, C.A.M.; Hu, E.A.; Knopman, D.; Mosley, T.H.; Gottesman, R.F. Association of Dietary Patterns in Midlife and Cognitive Function in Later Life in US Adults without Dementia. JAMA Netw. Open 2019, 2, e1916641. [Google Scholar] [CrossRef] [Green Version]
- Feart, C.; Samieri, C.; Rondeau, V.; Amieva, H.; Portet, F.; Dartigues, J.F.; Scarmeas, N.; Barberger-Gateau, P. Adherence to a mediterranean diet, cognitive decline, and risk of dementia. JAMA J. Am. Med. Assoc. 2009, 302, 638–648. [Google Scholar] [CrossRef] [Green Version]
- Gardener, S.L.; Rainey-Smith, S.R.; Barnes, M.B.; Sohrabi, H.R.; Weinborn, M.; Lim, Y.Y.; Harrington, K.; Taddei, K.; Gu, Y.; Rembach, A.; et al. Dietary patterns and cognitive decline in an Australian study of ageing. Mol. Psychiatry 2015, 20, 860–866. [Google Scholar] [CrossRef]
- Granic, A.; Davies, K.; Adamson, A.; Kirkwood, T.; Hill, T.R.; Siervo, M.; Mathers, J.C.; Jagger, C. Dietary patterns high in red meat, potato, gravy, and butter are associated with poor cognitive functioning but not with rate of cognitive decline in very old adults. J. Nutr. 2016, 146, 265–274. [Google Scholar] [CrossRef]
- Keenan, T.D.; Agron, E.; Mares, J.A.; Clemons, T.E.; van Asten, F.; Swaroop, A.; Chew, E.Y.; AREDS and AREDS2 Research Groups. R. Adherence to a Mediterranean diet and cognitive function in the Age-Related Eye Disease Studies 1 & 2. Alzheimers Dement. 2020, 16, 831–842. [Google Scholar] [CrossRef]
- Koyama, A.; Houston, D.K.; Simonsick, E.M.; Lee, J.S.; Ayonayon, H.N.; Shahar, D.R.; Rosano, C.; Satterfield, S.; Yaffe, K. Association between the Mediterranean diet and cognitive decline in a biracial population. J. Gerontol. Ser. A-Biol. Sci. Med. Sci. 2015, 70, 354–359. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lotan, R.; Ravona-Springer, R.; Mandel, J.; Lin, H.-M.; Ouyang, Y.; Shahar, D.R.; Bezalel, S.; Agarwal, P.; Dhana, K.; Heymann, A.; et al. Greater intake of the MEDI diet is associated with better cognitive trajectory in older adults with type 2 diabetes. Diabetes Res. Clin. Pract. 2022, 190, 109989. [Google Scholar] [CrossRef] [PubMed]
- Morris, M.C.; Tangney, C.C.; Wang, Y.; Sacks, F.M.; Barnes, L.L.; Bennett, D.A.; Aggarwal, N.T. MIND diet slows cognitive decline with aging. Alzheimer’s Dement. 2015, 11, 1015–1022. [Google Scholar] [CrossRef] [Green Version]
- Mueller, K.D.; Norton, D.; Koscik, R.L.; Morris, M.C.; Jonaitis, E.M.; Clark, L.R.; Fields, T.; Allison, S.; Berman, S.; Kraning, S.; et al. Self-reported health behaviors and longitudinal cognitive performance in late middle age: Results from the Wisconsin Registry for Alzheimer’s Prevention. PLoS ONE 2020, 15, e0221985. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Munoz-Garcia, M.I.; Martinez-Gonzalez, M.A.; Razquin, C.; Fernandez-Matarrubia, M.; Guillen-Grima, F.; Toledo, E. Exploratory dietary patterns and cognitive function in the “Seguimiento Universidad de Navarra” (SUN) Prospective Cohort. Eur. J. Clin. Nutr. 2021, 76, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Nooyens, A.C.J.; Yildiz, B.; Hendriks, L.G.; Bas, S.; van Boxtel, M.P.J.; Picavet, H.S.J.; Boer, J.M.A.; Verschuren, W.M.M. Adherence to dietary guidelines and cognitive decline from middle age: The Doetinchem Cohort Study. Am. J. Clin Nutr. 2021, 114, 871–881. [Google Scholar] [CrossRef] [PubMed]
- Ozawa, M.; Shipley, M.; Kivimaki, M.; Singh-Manoux, A.; Brunner, E.J. Dietary pattern, inflammation and cognitive decline: The Whitehall II prospective cohort study. Clin. Nutr. 2017, 36, 506–512. [Google Scholar] [CrossRef] [Green Version]
- Parrott, M.D.; Shatenstein, B.; Ferland, G.; Payette, H.; Morais, J.A.; Belleville, S.; Kergoat, M.J.; Gaudreau, P.; Greenwood, C.E. Relationship between diet quality and cognition depends on socioeconomic position in healthy older adults. J. Nutr. 2013, 143, 1767–1773. [Google Scholar] [CrossRef] [Green Version]
- Qin, B.; Adair, L.S.; Plassman, B.L.; Batis, C.; Edwards, L.J.; Popkin, B.M.; Mendez, M.A. Dietary Patterns and Cognitive Decline among Chinese Older Adults. Epidemiology 2015, 26, 758–768. [Google Scholar] [CrossRef]
- Richard, E.L.; Laughlin, G.A.; Kritz-Silverstein, D.; Reas, E.T.; Barrett-Connor, E.; McEvoy, L.K. Dietary patterns and cognitive function among older community-dwelling adults. Nutrients 2018, 10, 1088. [Google Scholar] [CrossRef] [Green Version]
- Samieri, C.; Grodstein, F.; Rosner, B.A.; Kang, J.H.; Cook, N.R.; Manson, J.E.; Buring, J.E.; Willett, W.C.; Okereke, O.I. Mediterranean diet and cognitive function in older age. Epidemiology 2013, 24, 490–499. [Google Scholar] [CrossRef] [PubMed]
- Samieri, C.; Okereke, O.I.; Devore, E.E.; Grodstein, F. Long-term adherence to the Mediterranean diet is associated with overall cognitive status, but not cognitive decline, in women. J. Nutr. 2013, 143, 493–499. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scarmeas, N.; Stern, Y.; Tang, M.X.; Mayeux, R.; Luchsinger, J.A. Mediterranean diet and risk for Alzheimer’s disease. Ann. Neurol. 2006, 59, 912–921. [Google Scholar] [CrossRef] [Green Version]
- Shakersain, B.; Rizzuto, D.; Larsson, S.C.; Faxen-Irving, G.; Fratiglioni, L.; Xu, W.L. The nordic prudent diet reduces risk of cognitive decline in the Swedish older adults: A population- based cohort study. Nutrients 2018, 10, 229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shatenstein, B.; Ferland, G.; Belleville, S.; Gray-Donald, K.; Kergoat, M.J.; Morais, J.; Gaudreau, P.; Payette, H.; Greenwood, C. Diet quality and cognition among older adults from the NuAge study. Exp. Gerontol. 2012, 47, 353–360. [Google Scholar] [CrossRef]
- Shi, Z.; El-Obeid, T.; Li, M.; Xu, X.; Liu, J. Iron-related dietary pattern increases the risk of poor cognition. Nutr. J. 2019, 18, 48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smyth, A.; Dehghan, M.; O’Donnell, M.; Anderson, C.; Teo, K.; Gao, P.; Sleight, P.; Dagenais, G.; Probstfield, J.L.; Mente, A.; et al. Healthy eating and reduced risk of cognitive decline: A cohort from 40 countries. Neurology 2015, 84, 2258–2265. [Google Scholar] [CrossRef] [Green Version]
- Soldevila-Domenech, N.; Forcano, L.; Vintro-Alcaraz, C.; Cuenca-Royo, A.; Pinto, X.; Jimenez-Murcia, S.; Garcia-Gavilan, J.F.; Nishi, S.K.; Babio, N.; Gomis-Gonzalez, M.; et al. Interplay between cognition and weight reduction in individuals following a Mediterranean Diet: Three-year follow-up of the PREDIMED-Plus trial. Clin. Nutr. 2021, 40, 5221–5237. [Google Scholar] [CrossRef]
- Tangney, C.C.; Kwasny, M.J.; Li, H.; Wilson, R.S.; Evans, D.A.; Morris, M.C. Adherence to a Mediterranean-type dietary pattern and cognitive decline in a community population. Am. J. Clin. Nutr. 2011, 93, 601–607. [Google Scholar] [CrossRef]
- Tangney, C.C.; Li, H.; Wang, Y.; Barnes, L.; Schneider, J.A.; Bennett, D.A.; Morris, M.C. Relation of DASH- and Mediterranean-like dietary patterns to cognitive decline in older persons. Neurology 2014, 83, 1410–1416. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tong, E.H.; Lai, J.S.; Whitton, C.; Neelakantan, N.; Zhou, Y.; Chen, C.; van Dam, R.M.; Feng, L.; Pan, A.; Chong, M.F.; et al. Changes in Diet Quality from Mid- to Late Life Are Associated with Cognitive Impairment in the Singapore Chinese Health Study. J. Nutr. 2021, 151, 2800–2807. [Google Scholar] [CrossRef] [PubMed]
- Tsai, H.J. Dietary patterns and cognitive decline in Taiwanese aged 65years and older. Int. J. Geriatr. Psychiatry 2015, 30, 523–530. [Google Scholar] [CrossRef] [PubMed]
- Vercambre, M.N.; Grodstein, F.; Berr, C.; Kang, J.H. Mediterranean diet and cognitive decline in women with cardiovascular disease or risk factors. J. Acad. Nutr. Diet. 2012, 112, 816–823. [Google Scholar] [CrossRef] [Green Version]
- Vu, T.H.T.; Beck, T.; Bennett, D.A.; Schneider, J.A.; Hayden, K.M.; Shadyab, A.H.; Rajan, K.B.; Morris, M.C.; Cornelis, M.C. Adherence to MIND Diet, Genetic Susceptibility, and Incident Dementia in Three US Cohorts. Nutrients 2022, 14, 2759. [Google Scholar] [CrossRef]
- Wengreen, H.; Munger, R.G.; Cutler, A.; Quach, A.; Bowles, A.; Corcoran, C.; Tschanz, J.T.; Norton, M.C.; Welsh-Bohmer, K.A. Prospective study of Dietary Approaches to Stop Hypertension-and Mediterranean-style dietary patterns and age-related cognitive change: The Cache County Study on Memory, Health and Aging. Am. J. Clin. Nutr. 2013, 98, 1263–1271. [Google Scholar] [CrossRef] [Green Version]
- Wengreen, H.J.; Neilson, C.; Munger, R.; Corcoran, C. Diet quality is associated with better cognitive test performance among aging men and women. J. Nutr. 2009, 139, 1944–1949. [Google Scholar] [CrossRef] [Green Version]
- Zhu, A.; Yuan, C.; Pretty, J.; Ji, J.S. Plant-based dietary patterns and cognitive function: A prospective cohort analysis of elderly individuals in China (2008–2018). Brain Behav. 2022, 12, e2670. [Google Scholar] [CrossRef]
- Haring, B.; Wu, C.; Mossavar-Rahmani, Y.; Snetselaar, L.; Brunner, R.; Wallace, R.B.; Neuhouser, M.L.; Wassertheil-Smoller, S. No Association between Dietary Patterns and Risk for Cognitive Decline in Older Women with 9-Year Follow-Up: Data from the Women’s Health Initiative Memory Study. J. Acad. Nutr. Diet. 2016, 116, 921–930.e921. [Google Scholar] [CrossRef] [Green Version]
- Scarmeas, N.; Stern, Y.; Mayeux, R.; Manly, J.J.; Schupf, N.; Luchsinger, J.A. Mediterranean diet and mild cognitive impairment. Arch. Neurol. 2009, 66, 216–225. [Google Scholar] [CrossRef]
- Zhang, X.; Wang, Y.; Liu, W.; Wang, T.; Wang, L.; Hao, L.; Ju, M.; Xiao, R. Diet quality, gut microbiota, and microRNAs associated with mild cognitive impairment in middle-aged and elderly Chinese population. Am. J. Clin. Nutr. 2021, 114, 429–440. [Google Scholar] [CrossRef]
- Hosking, D.E.; Eramudugolla, R.; Cherbuin, N.; Anstey, K.J. MIND not Mediterranean diet related to 12-year incidence of cognitive impairment in an Australian longitudinal cohort study. Alzheimer’s Dement. 2019, 15, 581–589. [Google Scholar] [CrossRef] [PubMed]
- Pearson, K.E.; Wadley, V.G.; McClure, L.A.; Shikany, J.M.; Unverzagt, F.W.; Judd, S.E. Dietary patterns are associated with cognitive function in the REasons for Geographic and Racial Differences in Stroke (REGARDS) cohort. J. Nutr. Sci. 2016, 5, e38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsivgoulis, G.; Judd, S.; Letter, A.J.; Alexandrov, A.V.; Howard, G.; Nahab, F.; Unverzagt, F.W.; Moy, C.; Howard, V.J.; Kissela, B.; et al. Adherence to a Mediterranean diet and risk of incident cognitive impairment. Neurology 2013, 80, 1684–1692. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nicoli, C.; Galbussera, A.A.; Bosetti, C.; Franchi, C.; Gallus, S.; Mandelli, S.; Marcon, G.; Quadri, P.; Riso, P.; Riva, E.; et al. The role of diet on the risk of dementia in the oldest old: The Monzino 80-plus population-based study. Clin Nutr. 2021, 40, 4783–4791. [Google Scholar] [CrossRef]
- Samuelsson, J.; Najar, J.; Wallengren, O.; Kern, S.; Wetterberg, H.; Mellqvist Fassberg, M.; Zetterberg, H.; Blennow, K.; Lissner, L.; Rothenberg, E.; et al. Interactions between dietary patterns and genetic factors in relation to incident dementia among 70-year-olds. Eur. J. Nutr. 2022, 61, 871–884. [Google Scholar] [CrossRef] [PubMed]
- Sindi, S.; Kareholt, I.; Eskelinen, M.; Hooshmand, B.; Lehtisalo, J.; Soininen, H.; Ngandu, T.; Kivipelto, M. Healthy dietary changes in midlife are associated with reduced dementia risk later in life. Nutrients 2018, 10, 1649. [Google Scholar] [CrossRef] [Green Version]
- Tomata, Y.; Sugiyama, K.; Kaiho, Y.; Honkura, K.; Watanabe, T.; Zhang, S.; Sugawara, Y.; Tsuji, I. Dietary Patterns and Incident Dementia in Elderly Japanese: The Ohsaki Cohort 2006 Study. J. Gerontol. Ser. A-Biol. Sci. Med. Sci. 2016, 71, 1322–1328. [Google Scholar] [CrossRef] [Green Version]
- Gu, Y.; Scarmeas, N. Dietary patterns in Alzheimer’s disease and cognitive aging. Curr. Alzheimer. Res. 2011, 8, 510–519. [Google Scholar] [CrossRef] [Green Version]
- Liu, L.; Volpe, S.L.; Ross, J.A.; Grimm, J.A.; van Bockstaele, E.J.; Eisen, H.J. Dietary sugar intake and risk of Alzheimer’s disease in older women. Nutr. Neurosci. 2021, 102, 106270. [Google Scholar] [CrossRef]
- Morris, M.C.; Tangney, C.C.; Wang, Y.; Sacks, F.M.; Bennett, D.A.; Aggarwal, N.T. MIND diet associated with reduced incidence of Alzheimer’s disease. Alzheimer’s Dement. 2015, 11, 1007–1014. [Google Scholar] [CrossRef] [Green Version]
- Olsson, E.; Karlstrom, B.; Kilander, L.; Byberg, L.; Cederholm, T.; Sjogren, P. Dietary patterns and cognitive dysfunction in a 12-year follow-up study of 70 year old men. J. Alzheimer’s Dis. 2015, 43, 109–119. [Google Scholar] [CrossRef] [PubMed]
- Ozawa, M.; Ninomiya, T.; Ohara, T.; Doi, Y.; Uchida, K.; Shirota, T.; Yonemoto, K.; Kitazono, T.; Kiyohara, Y. Dietary patterns and risk of dementia in an elderly Japanese population: The Hisayama Study. Am. J. Clin. Nutr. 2013, 97, 1076–1082. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gu, Y.; Nieves, J.W.; Stern, Y.; Luchsinger, J.A.; Scarmeas, N. Food combination and alzheimer disease risk: A protective diet. Arch. Neurol. 2010, 67, 699–706. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hu, E.A.; Wu, A.; Dearborn, J.L.; Gottesman, R.F.; Sharrett, A.R.; Steffen, L.M.; Coresh, J.; Rebholz, C.M. Adherence to Dietary Patterns and Risk of Incident Dementia: Findings from the Atherosclerosis Risk in Communities Study. J. Alzheimer’s Dis. 2020, 78, 827–835. [Google Scholar] [CrossRef]
- Andreu-Reinon, M.E.; Chirlaque, M.D.; Gavrila, D.; Amiano, P.; Mar, J.; Tainta, M.; Ardanaz, E.; Larumbe, R.; Colorado-Yohar, S.M.; Navarro-Mateu, F.; et al. Mediterranean Diet and Risk of Dementia and Alzheimer’s Disease in the EPIC-Spain Dementia Cohort Study. Nutrients 2021, 13, 700. [Google Scholar] [CrossRef] [PubMed]
- De Crom, T.O.E.; Mooldijk, S.S.; Ikram, M.K.; Ikram, M.A.; Voortman, T. MIND diet and the risk of dementia: A population-based study. Alzheimers Res. Ther. 2022, 14, 8. [Google Scholar] [CrossRef]
- Lu, Y.; Matsuyama, S.; Sugawara, Y.; Sone, T.; Tsuji, I. Changes in a specific dietary pattern and incident dementia: A prospective cohort study. Clin Nutr. 2021, 40, 3495–3502. [Google Scholar] [CrossRef]
- Chuang, S.Y.; Lo, Y.L.; Wu, S.Y.; Wang, P.N.; Pan, W.H. Dietary Patterns and Foods Associated with Cognitive Function in Taiwanese Older Adults: The Cross-sectional and Longitudinal Studies. J. Am. Med. Dir. Assoc. 2019, 20, 544–550.e544. [Google Scholar] [CrossRef]
- Samieri, C.; Sun, Q.; Townsend, M.K.; Chiuve, S.E.; Okereke, O.I.; Willett, C.; Stampfer, M.; Grodstein, F. The association between dietary patterns at midlife and health in aging an observational study. Ann. Intern. Med. 2013, 159, 584–591. [Google Scholar] [CrossRef]
- Trichopoulou, A.; Costacou, T.; Bamia, C.; Trichopoulos, D. Adherence to a Mediterranean diet and survival in a Greek population. N. Engl. J. Med. 2003, 348, 2599–2608. [Google Scholar] [CrossRef] [Green Version]
- Panagiotakos, D.B.; Pitsavos, C.; Arvaniti, F.; Stefanadis, C. Adherence to the Mediterranean food pattern predicts the prevalence of hypertension, hypercholesterolemia, diabetes and obesity, among healthy adults; the accuracy of the MedDietScore. Prev. Med. 2007, 44, 335–340. [Google Scholar] [CrossRef]
- Martínez-González, M.A.; García-Arellano, A.; Toledo, E.; Salas-Salvado, J.; Buil-Cosiales, P.; Corella, D.; Covas, M.I.; Schröder, H.; Arós, F.; Gómez-Gracia, E. A 14-item Mediterranean diet assessment tool and obesity indexes among high-risk subjects: The PREDIMED trial. PLoS ONE 2012, 7, e43134. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lopez-Garcia, E.; Rodriguez-Artalejo, F.; Li, T.Y.; Fung, T.T.; Li, S.; Willett, W.C.; Rimm, E.B.; Hu, F.B. The Mediterranean-style dietary pattern and mortality among men and women with cardiovascular disease. Am. J. Clin. Nutr. 2014, 99, 172–180. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fung, T.T.; Chiuve, S.E.; McCullough, M.L.; Rexrode, K.M.; Logroscino, G.; Hu, F.B. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch. Intern. Med. 2008, 168, 713–720. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Folsom, A.R.; Parker, E.D.; Harnack, L.J. Degree of concordance with DASH diet guidelines and incidence of hypertension and fatal cardiovascular disease. Am. J. Hypertens. 2007, 20, 225–232. [Google Scholar] [CrossRef] [Green Version]
- Smith, P.J.; Blumenthal, J.A.; Babyak, M.A.; Craighead, L.; Welsh-Bohmer, K.A.; Browndyke, J.N.; Strauman, T.A.; Sherwood, A. Effects of the dietary approaches to stop hypertension diet, exercise, and caloric restriction on neurocognition in overweight adults with high blood pressure. Hypertension 2010, 55, 1331–1338. [Google Scholar] [CrossRef] [Green Version]
- Chiuve, S.E.; Fung, T.T.; Rimm, E.B.; Hu, F.B.; McCullough, M.L.; Wang, M.; Stampfer, M.J.; Willett, W.C. Alternative dietary indices both strongly predict risk of chronic disease. J. Nutr. 2012, 142, 1009–1018. [Google Scholar] [CrossRef] [Green Version]
- Larsson, S.C.; Wolk, A. The role of lifestyle factors and sleep duration for late-onset dementia: A cohort study. J. Alzheimer’s Dis. 2018, 66, 579–586. [Google Scholar] [CrossRef] [Green Version]
- Samuelsson, J.; Rothenberg, E.; Lissner, L.; Eiben, G.; Zettergren, A.; Skoog, I. Time trends in nutrient intake and dietary patterns among five birth cohorts of 70-year-olds examined 1971-2016: Results from the Gothenburg H70 birth cohort studies, Sweden. Nutr. J. 2019, 18, 66. [Google Scholar] [CrossRef]
- Wade, A.T.; Davis, C.R.; Dyer, K.A.; Hodgson, J.M.; Woodman, R.J.; Keage, H.A.D.; Murphy, K.J. A Mediterranean diet supplemented with dairy foods improves mood and processing speed in an Australian sample: Results from the MedDairy randomized controlled trial. Nutr. Neurosci. 2018, 23, 646–658. [Google Scholar] [CrossRef]
- Wade, A.T.; Davis, C.R.; Dyer, K.A.; Hodgson, J.M.; Woodman, R.J.; Keage, H.A.D.; Murphy, K.J. A mediterranean diet with fresh, lean pork improves processing speed and mood: Cognitive findings from the medpork randomised controlled trial. Nutrients 2019, 11, 1521. [Google Scholar] [CrossRef] [Green Version]
- Chlebowski, R.T.; Rapp, S.; Aragaki, A.K.; Pan, K.; Neuhouser, M.L.; Snetselaar, L.G.; Manson, J.E.; Wactawski-Wende, J.; Johnson, K.C.; Hayden, K.; et al. Low-fat dietary pattern and global cognitive function: Exploratory analyses of the Women’s Health Initiative (WHI) randomized Dietary Modification trial. EClinicalMedicine 2020, 18, 100240. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kwok, T.C.; Lam, L.C.; Sea, M.M.; Goggins, W.; Woo, J. A randomized controlled trial of dietetic interventions to prevent cognitive decline in old age hostel residents. Eur. J. Clin. Nutr. 2012, 66, 1135–1140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arjmand, G.; Abbas-Zadeh, M.; Eftekhari, M.H. Effect of MIND diet intervention on cognitive performance and brain structure in healthy obese women: A randomized controlled trial. Sci. Rep. 2022, 12, 2871. [Google Scholar] [CrossRef] [PubMed]
- Marseglia, A.; Xu, W.; Fratiglioni, L.; Fabbri, C.; Berendsen, A.A.M.; Bialecka-Debek, A.; Jennings, A.; Gillings, R.; Meunier, N.; Caumon, E.; et al. Effect of the NU-AGE diet on cognitive functioning in older adults: A randomized controlled trial. Front. Physiol. 2018, 9, 349. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, A.; Tovar, J.; Johansson, M.; Radeborg, K.; Bjorck, I. A diet based on multiple functional concepts improves cognitive performance in healthy subjects. Nutr. Metab. 2013, 10, 49. [Google Scholar] [CrossRef] [Green Version]
- Brenowitz, W.D.; Xiang, Y.; McEvoy, C.T.; Yang, C.; Yaffe, K.; Le, W.-D.; Leng, Y. Current Alzheimer disease research highlights: Evidence for novel risk factors. Chin. Med. J. 2021, 134, 2150–2159. [Google Scholar] [CrossRef] [PubMed]
- Mecocci, P.; Mariani, E.; Cornacchiola, V.; Polidori, M. Antioxidants for the treatment of mild cognitive impairment. Neurol. Res. 2004, 26, 598–602. [Google Scholar] [CrossRef]
- Alles, B.; Samieri, C.; Feart, C.; Jutand, M.A.; Laurin, D.; Barberger-Gateau, P. Dietary patterns: A novel approach to examine the link between nutrition and cognitive function in older individuals. Nutr. Res. Rev. 2012, 25, 207–222. [Google Scholar] [CrossRef]
- Carroll, R.J.; Midthune, D.; Subar, A.F.; Shumakovich, M.; Freedman, L.S.; Thompson, F.E.; Kipnis, V. Taking advantage of the strengths of 2 different dietary assessment instruments to improve intake estimates for nutritional epidemiology. Am. J. Epidemiol. 2012, 175, 340–347. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kristal, A.R.; Peters, U.; Potter, J.D. Is it time to abandon the food frequency questionnaire? Cancer Epidemiol. Biomarkers Prev. 2005, 14, 2826–2828. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kipnis, V.; Subar, A.F.; Midthune, D.; Freedman, L.S.; Ballard-Barbash, R.; Troiano, R.P.; Bingham, S.; Schoeller, D.A.; Schatzkin, A.; Carroll, R.J. Structure of dietary measurement error: Results of the OPEN biomarker study. Am. J. Epidemiol. 2003, 158, 14–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Freedman, L.S.; Commins, J.M.; Moler, J.E.; Arab, L.; Baer, D.J.; Kipnis, V.; Midthune, D.; Moshfegh, A.J.; Neuhouser, M.L.; Prentice, R.L. Pooled results from 5 validation studies of dietary self-report instruments using recovery biomarkers for energy and protein intake. Am. J. Epidemiol. 2014, 180, 172–188. [Google Scholar] [CrossRef] [Green Version]
- Franco-Marina, F.; García-González, J.J.; Wagner-Echeagaray, F.; Gallo, J.; Ugalde, O.; Sánchez-García, S.; Espinel-Bermúdez, C.; Juárez-Cedillo, T.; Rodríguez, M.Á.V.; García-Peña, C. The Mini-mental State Examination revisited: Ceiling and floor effects after score adjustment for educational level in an aging Mexican population. Int. Psychogeriatr. 2010, 22, 72–81. [Google Scholar] [CrossRef] [PubMed]
- Knight, A.; Bryan, J.; Murphy, K. The Mediterranean diet and age-related cognitive functioning: A systematic review of study findings and neuropsychological assessment methodology. Nutr. Neurosci. 2017, 20, 449–468. [Google Scholar] [CrossRef] [PubMed]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Townsend, R.F.; Logan, D.; O’Neill, R.F.; Prinelli, F.; Woodside, J.V.; McEvoy, C.T. Whole Dietary Patterns, Cognitive Decline and Cognitive Disorders: A Systematic Review of Prospective and Intervention Studies. Nutrients 2023, 15, 333. https://doi.org/10.3390/nu15020333
Townsend RF, Logan D, O’Neill RF, Prinelli F, Woodside JV, McEvoy CT. Whole Dietary Patterns, Cognitive Decline and Cognitive Disorders: A Systematic Review of Prospective and Intervention Studies. Nutrients. 2023; 15(2):333. https://doi.org/10.3390/nu15020333
Chicago/Turabian StyleTownsend, Rebecca F., Danielle Logan, Roisin F. O’Neill, Federica Prinelli, Jayne V. Woodside, and Claire T. McEvoy. 2023. "Whole Dietary Patterns, Cognitive Decline and Cognitive Disorders: A Systematic Review of Prospective and Intervention Studies" Nutrients 15, no. 2: 333. https://doi.org/10.3390/nu15020333
APA StyleTownsend, R. F., Logan, D., O’Neill, R. F., Prinelli, F., Woodside, J. V., & McEvoy, C. T. (2023). Whole Dietary Patterns, Cognitive Decline and Cognitive Disorders: A Systematic Review of Prospective and Intervention Studies. Nutrients, 15(2), 333. https://doi.org/10.3390/nu15020333




