Applying the Adjusted Chinese Dietary Balance Index-16 to Assess the Dietary Quality of Chinese Postpartum Lactating Mothers
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measurements
2.3. Statistical Analysis
3. Results
3.1. Characteristics of the Participants
3.2. Distribution of DBI Components in Food Intake Scores of Lactating Women
3.3. Distribution of Diet Quality Indicators by DBI for Lactating Mothers
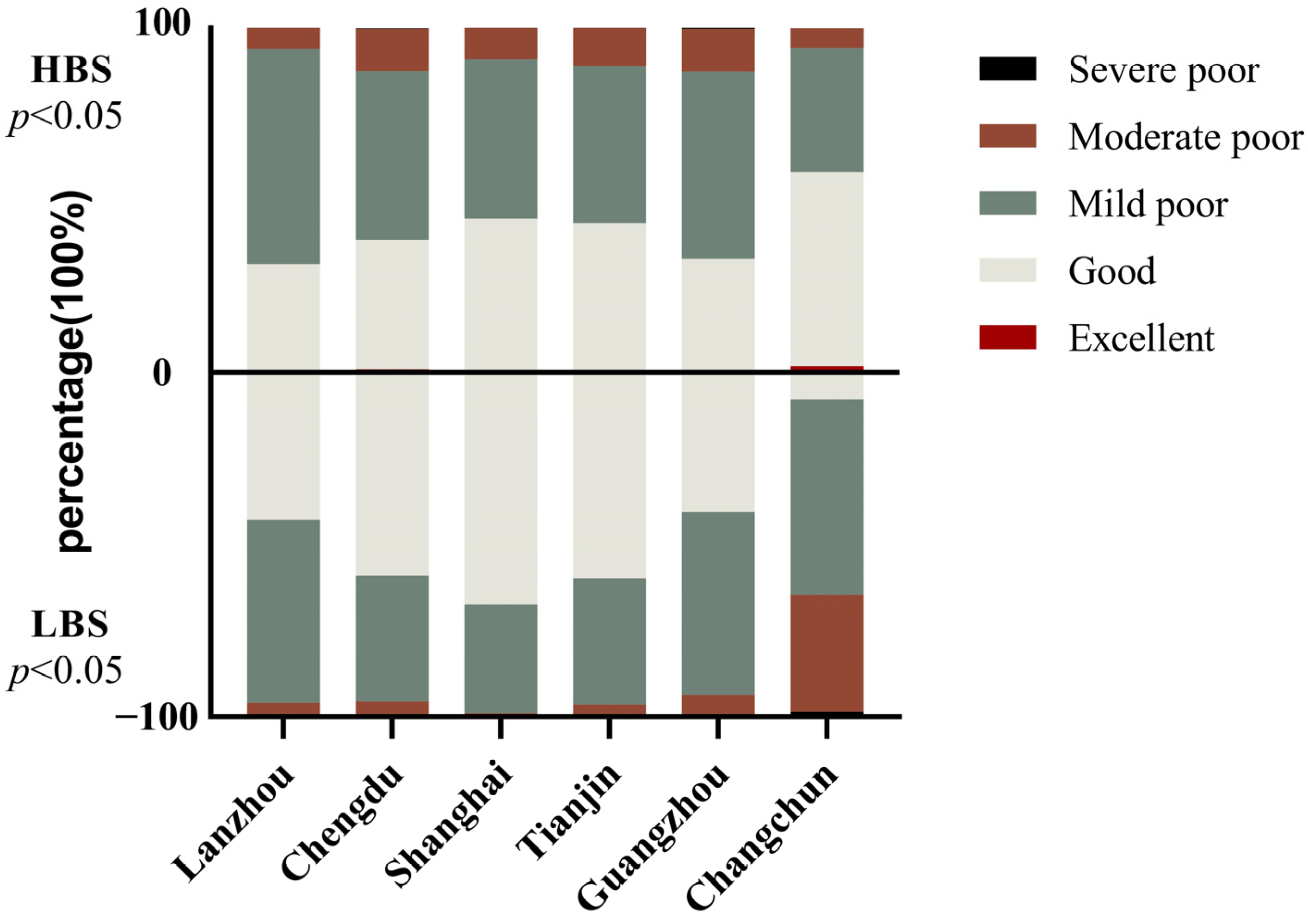
3.4. Dietary Assessment of Lactating Mothers in Different Cities
3.5. The Distribution of the Diet Quality Distance of Lactating Mothers
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bravi, F.; Wiens, F.; Decarli, A.; Dal Pont, A.; Agostoni, C.; Ferraroni, M. Impact of maternal nutrition on breast-milk composition: A systematic review. Am. J. Clin. Nutr. 2016, 104, 646–662. [Google Scholar] [CrossRef] [PubMed]
- Raymond, J.; Kassim, N.; Rose, J.W.; Agaba, M. Optimal dietary patterns designed from local foods to achieve maternal nutritional goals. BMC Public Health 2018, 18, 451. [Google Scholar] [CrossRef] [PubMed]
- Agosti, M.; Tandoi, F.; Morlacchi, L.; Bossi, A. Nutritional and metabolic programming during the first thousand days of life. Pediatr. Med. Chir. 2017, 39, 157. [Google Scholar] [CrossRef] [PubMed]
- Chinese Nutrition Society. Chinese Dietary Guidelines (2016); People’s Health Publishing House: Beijing, China, 2016. [Google Scholar]
- Mao, L.; Ma, L.; Liu, N.; Chen, B.; Liu, Q.; Ying, C.; Sun, X. Self-reported health problems related to traditional dietary practices in postpartum women from urban, suburban, and rural areas of Hubei province, China: The “zuò yuèzi”. Asia Pac. J. Clin. Nutr. 2016, 25, 158–164. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.Y.; Zhou, M.L.; Xu, Y.Q. A study on the dietary nutrition of lactating women in Fuzhou City. Mod. Prev. Med. 2015, 42, 2722–2725. [Google Scholar]
- Liu, Y.Q.; Petrini, M.; Maloni, J.A. “Doing the month”: Postpartum practices in Chinese women. Nurs. Health Sci. 2014, 17, 5–14. [Google Scholar] [CrossRef]
- Cheng, Y.Y.; Guo, C.C. Introduction to the Dietary Guidelines for U.S. Residents 2020–2025. J. Nutr. 2021, 43, 3–8. [Google Scholar]
- Popkin, B.; Keyou, G.; Zhai, F.; Guo, X.; Ma, H.; Zohoori, N. The nutrition transition in China: A cross-sectional analysis. Eur. J. Clin. Nutr. 1993, 47, 333–346. [Google Scholar] [PubMed]
- Kelly, O.; Gilman, J.; Ilich, J. Utilizing Dietary Micronutrient Ratios in Nutritional Research May be More Informative than Focusing on Single Nutrients. Nutrients 2018, 10, 107. [Google Scholar] [CrossRef]
- Zhao, J.; Li, Z.; Gao, Q.; Zhao, H.; Chen, S.; Huang, L.; Wang, W.; Wang, T. A review of statistical methods for dietary pattern analysis. Nutr. J. 2021, 20, 37. [Google Scholar] [CrossRef]
- Krebs-Smith, S.M.; Pannucci, T.E.; Subar, A.F.; Kirkpatrick, S.I.; Lerman, J.L.; Tooze, J.A.; Wilson, M.M.; Reedy, J. Update of the Healthy Eating Index: HEI-2015. J. Acad. Nutr. Diet. 2018, 118, 1591–1602. [Google Scholar] [CrossRef]
- Haines, P.S.; Siega-Riz, A.M.; Popkin, B.M. The Diet Quality Index Revised. J. Am. Diet. Assoc. 1999, 99, 697–704. [Google Scholar] [CrossRef]
- Martínez-González, M.A.; Fernández-Jarne, E.; Serrano-Martínez, M.; Marti, A.; Martinez, J.A.; Martín-Moreno, J.M. Mediterranean diet and reduction in the risk of a first acute myocardial infarction: An operational healthy dietary score. Eur. J. Nutr. 2002, 41, 153–160. [Google Scholar] [CrossRef]
- He, Y.N. Establishment of the Chinese Dietary Balance Index. Health Res. 2005, 2, 208–211. [Google Scholar]
- He, Y.N.; Fang, Y.H.; Xia, J.J. Revision of the Chinese dietary balance index: DBI-16. J. Nutr. 2018, 40, 526–530. [Google Scholar]
- Pang, M.R.; Tang, J.L.; Lu, Z.L.; Yang, Y.X.; Zhang, Z.H.; Ren, X.M.; Yin, Z.X.; Ma, J.X. Application of the Chinese Dietary Balance Index to evaluate the dietary quality of adult residents in Shandong Province. Mod. Prev. Med. 2023, 50, 1222–1226+1255. [Google Scholar]
- Zhong, W.X.; Mao, S.; Lan, H.L.; Situ, W.Y.; Zhao, A.; Wang, P.Y.; Zhang, Y.M. Application of the Chinese Pregnancy Dietary Balance Index to evaluate the dietary quality of pregnant women in 10 cities. J. Nutr. 2022, 44, 544–548. [Google Scholar]
- Su, X.; Zhu, W.; Li, N.; Sun, J.; Zhu, Y.; Liu, T.; Xia, T.; Dai, Z.; Zhang, Y.; Pan, L. Adjusting DBI-2016 to dietary balance index for Chinese maternal women and assessing the association between maternal dietary quality and postpartum weight retention: A longitudinal study. PLoS ONE 2020, 15, e0237225. [Google Scholar] [CrossRef]
- Wang, L.S.; Zhang, B.; Wang, H.J.; Du, W.W.; Zhang, J.G.; Wang, Z.H. Establishment of the “China Dietary Guidelines Index for the Elderly 2018” and its application in the evaluation of diets for residents aged 60 years and above in 15 provinces (autonomous regions and municipalities directly under the central government) of China. Health Res. 2019, 48, 41–48. [Google Scholar]
- Lingrui, L.; Huilan, L.; Yanfeng, G.; Xueyan, W.; Gexiang, Z.; Cheng, M. Establishment of dietary balance index for preschool children in urban areas of Lanzhou. Health Res. 2019, 48, 244–248. [Google Scholar]
- Chinese Society of Nutrition. Dietary guidelines for lactating women. J. Clin. Pediatr. 2016, 34, 958–960. [Google Scholar]
- Yao, Y.Q. Chinese Nutrition Society Releases 2013 Revised Edition of the Dietary Nutrient Reference Intakes for Chinese Residents. J. Nutr. 2014, 36, 308. [Google Scholar]
- Michels, K.B.; Schulze, M.B. Can dietary patterns help us detect diet–disease associations? Nutr. Res. Rev. 2005, 18, 241–248. [Google Scholar] [CrossRef] [PubMed]
- Newby, P.K.; Tucker, K.L. Empirically Derived Eating Patterns Using Factor or Cluster Analysis: A Review. Nutr. Rev. 2004, 62, 177–203. [Google Scholar] [CrossRef] [PubMed]
- Moeller, S.M.; Reedy, J.; Millen, A.E.; Dixon, L.B.; Newby, P.K.; Tucker, K.L.; Krebs-Smith, S.M.; Guenther, P.M. Dietary Patterns: Challenges and Opportunities in Dietary Patterns Research. J. Am. Diet. Assoc. 2007, 107, 1233–1239. [Google Scholar] [CrossRef]
- Ocké, M.C. Evaluation of methodologies for assessing the overall diet: Dietary quality scores and dietary pattern analysis. Proc. Nutr. Soc. 2013, 72, 191–199. [Google Scholar] [CrossRef]
- Waijers, P.M.C.M.; Feskens, E.J.M.; Ocké, M.C. A critical review of predefined diet quality scores. Br. J. Nutr. 2007, 97, 219–231. [Google Scholar] [CrossRef]
- Trijsburg, L.; Talsma, E.F.; de Vries, J.H.M.; Kennedy, G.; Kuijsten, A.; Brouwer, I.D. Diet quality indices for research in low- and middle-income countries: A systematic review. Nutr. Rev. 2019, 77, 515–540. [Google Scholar] [CrossRef]
- Schwingshackl, L.; Hoffmann, G. Diet Quality as Assessed by the Healthy Eating Index, the Alternate Healthy Eating Index, the Dietary Approaches to Stop Hypertension Score, and Health Outcomes: A Systematic Review and Meta-Analysis of Cohort Studies. J. Acad. Nutr. Diet. 2015, 115, 780–800.e5. [Google Scholar] [CrossRef]
- Chiuve, S.E.; Fung, T.T.; Rimm, E.B.; Hu, F.B.; McCullough, M.L.; Wang, M.; Stampfer, M.J.; Willett, W.C. Alternative Dietary Indices Both Strongly Predict Risk of Chronic Disease. J. Nutr. 2012, 142, 1009–1018. [Google Scholar] [CrossRef]
- Fung, T.T.; Rexrode, K.M.; Mantzoros, C.S.; Manson, J.E.; Willett, W.C.; Hu, F.B. Mediterranean Diet and Incidence of and Mortality From Coronary Heart Disease and Stroke in Women. Circulation 2009, 119, 1093–1100. [Google Scholar] [CrossRef]
- George, S.M.; Ballard-Barbash, R.; Manson, J.E.; Reedy, J.; Shikany, J.M.; Subar, A.F.; Tinker, L.F.; Vitolins, M.; Neuhouser, M.L. Comparing Indices of Diet Quality with Chronic Disease Mortality Risk in Postmenopausal Women in the Women’s Health Initiative Observational Study: Evidence to Inform National Dietary Guidance. Am. J. Epidemiol. 2014, 180, 616–625. [Google Scholar] [CrossRef] [PubMed]
- Krebs-Smith, S.M.; Subar, A.F.; Reedy, J. Examining Dietary Patterns in Relation to Chronic Disease. Circulation 2015, 132, 790–793. [Google Scholar] [CrossRef]
- Weikert, C.; Schulze, M.B. Evaluating dietary patterns. Curr. Opin. Clin. Nutr. Metab. Care 2016, 19, 341–346. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Li, R.; Liu, D.; Dai, Z.; Liu, J.; Zhang, J.; Zhou, R.; Zeng, G. Evaluation of the dietary quality by diet balance index for pregnancy among pregnant women. Wei Sheng Yan Jiu = J. Hyg. Res. 2016, 45, 211–216. [Google Scholar]
- Movassagh, E.Z.; Vatanparast, H. Current Evidence on the Association of Dietary Patterns and Bone Health: A Scoping Review. Adv. Nutr. 2017, 8, 12–16. [Google Scholar] [CrossRef]
- He, Y.N.; Fang, Y.H.; Yang, X.G.; Ding, G.Q. Establishment and application of the Chinese Healthy Diet Index. J. Nutr. 2017, 39, 436–441. [Google Scholar]
- Tang, N.; Pan, W.T.; Chen, Y.J.; Chen, Y.M.; Cai, L. Revision of the lactation dietary balance index and evaluation of puerperal dietary quality in China. J. Nutr. 2021, 43, 230–235. [Google Scholar]
- Zeng, Y.F. Investigation and analysis of the dietary structure and its influencing factors among women in the puerperium in Yuexiu District, Guangzhou. J. Guangdong Med. Coll. 2012, 30, 674–676. [Google Scholar]
- Bo, Y.; Shaoming, H.; Changya, J.; Jie, H.; Qinggui, L.; Limei, M. Survey on the dietary nutrition and health status of peripartum women in suburban Guangzhou. China Matern. Child. Health Care 2014, 29, 3127–3130. [Google Scholar]
- Wang, P.; Chen, H.J.; Ma, J.; Chen, Y.; Li, H.W. Survey on the dietary nutrition of lactating mothers in the puerperium in Xiamen. J. Prev. Med. Intell. 2010, 26, 453–456. [Google Scholar]
- Mao, L.-M.; Sun, X.-F.; Liu, L.-G.; Jiao, C.-Y.; Chen, B.-H.; Liu, N. A follow-up survey on the nutritional status of puerperal diet among urban and rural women in Hubei Province. China Matern. Child. Health Care 2010, 25, 950–953. [Google Scholar]
- LiG Dietary investigation and influencing factors analysis of lactating mothers during puerperium. Matern. Child. Health Care China 2015, 30, 3029–3032.
- Dai, X.; Shen, G.H.; Xia Hoye Wang, L.; Wen, T.L.; Zhu, W.L. Dietary behavior of puerperal women and its associated factors. China Matern. Child. Health Res. 2016, 27, 1052–1055. [Google Scholar]
- Cuervo, M.; Sayon-Orea, C.; Santiago, S.; Martínez, J. Dietary and Health Profiles of Spanish Women in Preconception, Pregnancy and Lactation. Nutrients 2014, 6, 4434–4451. [Google Scholar] [CrossRef]
- Wiltheiss, G.A.; Lovelady, C.A.; West, D.G.; Brouwer, R.J.N.; Krause, K.M.; Østbye, T. Diet Quality and Weight Change among Overweight and Obese Postpartum Women Enrolled in a Behavioral Intervention Program. J. Acad. Nutr. Diet. 2013, 113, 54–62. [Google Scholar] [CrossRef]
- Snetselaar, L.G.; de Jesus, J.M.; DeSilva, D.M.; Stoody, E.E. Dietary Guidelines for Americans, 2020–2025. Nutr. Today 2021, 56, 287–295. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.H.; Zhai, F.Y.; He, Y.N.; Wang, H.; Yu, W.T.; Yu, D.M.M. Effect of economic income level on dietary nutrient intake and dietary structure of Chinese urban and rural residents. Health Res. 2008, 1, 62–64. [Google Scholar]
- Ge, K.Y. The Complete Book of Chinese Nutrition Science; People’s Health Publishing House, People’s Health Press: Beijing, China, 2004; p. 1253-1. [Google Scholar]

| Components | Representative Foods | Score Ranges |
|---|---|---|
| C1—cereal | Rice, pasta, coarse grains, potatoes, and mixed beans | (−12)–12 |
| C2—vegetable and fruit | Dark vegetables | (−6)–0 |
| light vegetables | ||
| Fruits | (−6)–0 | |
| C3—dairy, soybean, and nut | Dairy | (−6)–0 |
| Soybean and nut | (−6)–0 | |
| C4—animal food | Meat and poultry (animal offal) | (−4)–4 |
| Fish and shrimp | (−4)–0 | |
| Eggs | (−4)–4 | |
| C5—empty energy food | Cooking oil | 0–6 |
| Alcoholic beverage | 0–6 | |
| C6—condiments | Added sugar | 0–6 |
| Salt | 0–6 |
| Components | Groups | Range | Guidelines | Scoring Definition |
|---|---|---|---|---|
| C1—cereal a | Cereal | (−12)−12 | Cereal 225–275 g, potato 75 g | 0 g = −12; 275–325 g = 0; >600 g = 12; score increases 1 with intake amount decrease 25 g. |
| C2—vegetable and fruit | Vegetable | (−6)−0 | 400–500 g | ≥450 g = 0; 360–449 g = (−1); score decrease 1 with intake amount decrease 90 g; 0 g = (−6). |
| Fruit | (−6)−0 | 200–350 g | ≥300 g = 0; 240–299 g = (−1); score decrease 1 with intake amount decrease 60 g; 0 g = (−6). | |
| C3—dairy, soybean, and nut | Dairy | (−6)−0 | 300–500 | ≥400 g = 0; Score decreased 1 with intake amount decreased by 80 g; 0 g = −6 |
| soybean and nut | (−6)−0 | Soybean 25 g, nut 10 g | ≥35 g = 0; 28–34 = −1; score decrease 1 with intake amount decrease 7 g; 0 g = (−6). | |
| C4—animal food | Meat and poultry | (−4)−4 | 50–75 g | 0 g = (−4); 1–25 g = (−3); 26–50 g = (−2); 51–75 g = (−1); 76–95 g = 0; 96–120 g = 1; 121–145 g = 2; 146–170 g = 3; >170 g = 4. |
| Fish and shrimp | (−4)−0 | 75–100 g | <15 g = (−4); 15–34 g =(−3); 35–54 g = (−2); 55–74 g = (−1); ≥75 g = 0. | |
| Eggs | (−4)−4 | 50 g | 0 g = −4; 1–15 g = −3; 16–30 g = −2; 31–45 g = −1; 46–55 g = 0;56–70 g = 1; 71–85 g = 2; 86–100 g= 3; >100 g =4 | |
| C5—empty energy food | Cooking oil | 0–6 | 25 g | ≤25 g = 0; 26–30 g = 1; >50 g = 6 |
| Alcoholic beverage b | 0–6 | 0 | 0 g = 0; 1–10 g = 1; score increases 1 with intake amount increase 10 g; >50 g = 6. | |
| C6—condiments | Added sugar | 0–6 | 25 g | ≤25 g = 0; 26–30 g = 1; score increase 1 with intake amount increase 5 g; >50 g = 6. |
| Salt | 0–6 | <5 g | <5 g = 0; 5–6 g = 1; 7–8 g = 2; score increase 1 with intake amount increase 2 g; >15 g = 6. | |
| C7—food variety | Food variety | (−12)−0 | 12 | ≥12 kinds of food (soybean is 5 g) = 0; Score decreased by 1 with food variety decreased by 1. |
| Characteristics (n = 2532) | n | Percentage (%) |
|---|---|---|
| Age (years) | ||
| Mean ± SD | 29.75 ± 3.55 | |
| 19–34 | 2275 | 89.8 |
| 35–44 | 257 | 10.2 |
| Gestational age (weeks) | ||
| Mean ± SD | 39.29 ± 1.75 | |
| Pre-pregnancy BMI (kg/m2) | ||
| Mean ± SD | 21.01 ± 2.88 | |
| Predelivery BMI (kg/m2) | ||
| Mean ± SD | 26.41 ± 3.19 | |
| Primary delivery | 1790 | 70.7 |
| Vaginal delivery | 1653 | 65.3 |
| Lactation stage | ||
| <30 days | 639 | 25.2 |
| 40–90 days | 562 | 22.2 |
| 200–240 days | 1331 | 52.6 |
| Offspring gender | ||
| Male | 1296 | 51.3 |
| Offspring weight (g) | ||
| Mean ± SD | 3318.79 ± 441.40 | |
| Offspring length (cm) | ||
| Mean ± SD | 49.96 ± 2.20 | |
| DBI-L a Components | Mean | −12~ | −10~ | −8~ | −6~ | −4~ | −2~ | 0 | 1~ | 3~ | 5~ | 7~ | 9~ | 11~ |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cereal | 5.63 | 0.6 | 0.5 | 1.1 | 2.9 | 4 | 5.9 | 9 | 7.7 | 9.7 | 9.8 | 8.6 | 7.5 | 32.7 |
| Vegetable | −2.48 | 10.8 | 43.0 | 25.3 | 20.9 | |||||||||
| Fruit | −2.97 | 26.8 | 32.7 | 19.6 | 20.9 | |||||||||
| Dairy | −3.26 | 34.8 | 20.1 | 31.8 | 13.3 | |||||||||
| Soybean and nut | −1.73 | 21.5 | 9.8 | 8.4 | 60.3 | |||||||||
| Meat and poultry | 1.29 | 9.0 | 19.6 | 7.0 | 22.6 | 41.8 | ||||||||
| Fish and shrimp | −2.04 | 44.0 | 25.4 | 30.6 | ||||||||||
| Egg | 0.02 | 17.0 | 12.5 | 41.4 | 7.7 | 21.4 | ||||||||
| Cooking oil | 0.04 | 98.3 | 1.2 | 0.4 | 0.2 | |||||||||
| Alcoholic beverage | 0.08 | 98.0 | 0.7 | 0.6 | 0.8 | |||||||||
| Added sugar | 0.09 | 97.9 | 0.4 | 0.2 | 1.4 | |||||||||
| Salt | 1.85 | 5.8 | 77.6 | 9.1 | 7.5 |
| Indicator | Mean ± SD | Excellent # | Good | Mild Poor | Moderate Poor | Severe Poor |
|---|---|---|---|---|---|---|
| HBS a | 10.99 ± 5.77 | 16 (0.6) | 1054 (41.6) | 1225 (48.4) | 235 (9.3) | 2 (0.1) |
| LBS b | 14.50 ± 7.43 | 4 (0.2) | 850 (33.6) | 1060 (41.9) | 516 (20.4) | 102 (4.0) |
| DQD c | 25.47 ± 7.87 | 0 (0.0) | 198 (7.8) | 1581 (62.4) | 705 (27.8) | 48 (1.9) |
| HBS | LBS | DQD | ||||
|---|---|---|---|---|---|---|
| Mean ± SD | p | Mean ± SD | p | Mean ± SD | p | |
| Postpartum | ||||||
| <30 days | 9.45 ± 5.63 b | <0.05 | 13.38 ± 8.32 b | <0.05 | 22.83 ± 8.64 b | <0.05 |
| 40–90 days | 11.40 ± 5.57 a | 15.43 ± 6.64 a | 26.83 ± 6.98 a | |||
| 200–240 days | 11.56 ± 5.8 a | 14.61 ± 7.26 a | 26.17 ± 7.54 a | |||
| Cities | ||||||
| Lanzhou | 11.71 ± 4.89 ab | <0.05 | 13.88 ± 5.92 b | <0.05 | 25.59 ± 6.62 b | <0.05 |
| Chengdu | 11.62 ± 6.14 a | 12.19 ± 6.22 c | 23.80 ± 6.88 c | |||
| Shanghai | 10.70 ± 5.81 b | 10.31 ± 5.35 d | 21.01 ± 6.85 d | |||
| Tianjin | 10.90 ± 6.09 b | 11.89 ± 6.51 c | 22.79 ± 7.09 c | |||
| Guangzhou | 12.47 ± 5.55 a | 14.01 ± 6.61 b | 26.48 ± 7.29 b | |||
| Changchun | 9.06 ± 5.48 c | 21.89 ± 6.72 a | 30.95 ± 7.82 a | |||
| RNI (g/day) | Lanzhou (n = 397) | Chengdu (n = 409) | Shanghai (n = 365) | Tianjin (n = 402) | Guangzhou (n = 427) | Changchun (n = 532) | p | |
|---|---|---|---|---|---|---|---|---|
| Cereal | 300–350 | 547.66 ± 192.27 a | 526.74 ± 300.70 b | 481.17 ± 202.26 c | 499.38 ± 264.15 bc | 565.68 ± 311.41 a | 421.44 ± 197.75 c | <0.05 |
| Vegetable | 400–500 | 253.11 ± 132.43 c | 382.75 ± 286.24 b | 348.07 ± 181.89 b | 425.13 ± 210.53 a | 287.05 ± 232.50 c | 179.15 ± 132.80 d | <0.05 |
| Fruit | 200–350 | 165.61 ± 140.60 b | 229.88 ± 257.75 a | 230.31 ± 167.33 a | 172.37 ± 159.48 b | 143.68 ± 144.05 b | 146.50 ± 176.83 b | <0.05 |
| Dairy | 300–500 | 176.58 ± 157.93 c | 250.36 ± 177.44 ab | 255.93 ± 189.17 a | 223.68 ± 177.60 b | 220.44 ± 209.88 b | 90.47 ± 150.08 d | <0.05 |
| Soybean and nut | 35 | 99.59 ± 91.53 b | 83.3 ± 97.216 bc | 78.7 ± 94.33 c | 124.73 ± 147.20 a | 73.07 ± 105.88 c | 46.84 ± 87.10 d | <0.05 |
| Meat and poultry | 50–75 | 106.70 ± 85.58 c | 177.98 ± 178.11 b | 169.53 ± 125.06 b | 115.11 ± 94.15 c | 249.53 ± 172.45 a | 116.73 ± 108.10 c | <0.05 |
| Fish and shrimp | 75–100 | 56.21 ± 76.93 c | 59.28 ± 72.26 c | 107.75 ± 103.81 a | 67.51 ± 76.30 c | 84.18 ± 109.41 b | 37.15 ± 77.06 d | <0.05 |
| Egg | 50 | 48.46 ± 29.04 c | 60.75 ± 56.47 ab | 58.24 ± 35.01 b | 68.99 ± 47.48 a | 47.53 ± 66.53 c | 65.99 ± 70.08 ab | <0.05 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jiang, J.; Huang, J.; Su, Y.; Wang, Y. Applying the Adjusted Chinese Dietary Balance Index-16 to Assess the Dietary Quality of Chinese Postpartum Lactating Mothers. Nutrients 2023, 15, 4499. https://doi.org/10.3390/nu15214499
Jiang J, Huang J, Su Y, Wang Y. Applying the Adjusted Chinese Dietary Balance Index-16 to Assess the Dietary Quality of Chinese Postpartum Lactating Mothers. Nutrients. 2023; 15(21):4499. https://doi.org/10.3390/nu15214499
Chicago/Turabian StyleJiang, Junyue, Jiating Huang, Yanyan Su, and Yu Wang. 2023. "Applying the Adjusted Chinese Dietary Balance Index-16 to Assess the Dietary Quality of Chinese Postpartum Lactating Mothers" Nutrients 15, no. 21: 4499. https://doi.org/10.3390/nu15214499
APA StyleJiang, J., Huang, J., Su, Y., & Wang, Y. (2023). Applying the Adjusted Chinese Dietary Balance Index-16 to Assess the Dietary Quality of Chinese Postpartum Lactating Mothers. Nutrients, 15(21), 4499. https://doi.org/10.3390/nu15214499






