The Global Burden of Type 2 Diabetes Attributable to Dietary Risks: Insights from the Global Burden of Disease Study 2019
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Sources and Definitions
2.2. Estimation of T2DM Burden
2.3. Estimation of Attributable Burden
2.4. Selection of Dietary Risk Factors
2.5. Socio-Demographic Index
2.6. Statistical Analysis
3. Results
3.1. Global Trends in T2DM Burden Attributable to Dietary Risk Factors from 1990 to 2019
3.2. Global Trends in T2DM Attributable to Dietary Risk Factors by Gender and Age in 2019
3.3. Global Trends in T2DM Burden Attributable to Dietary Risk Factors by Region
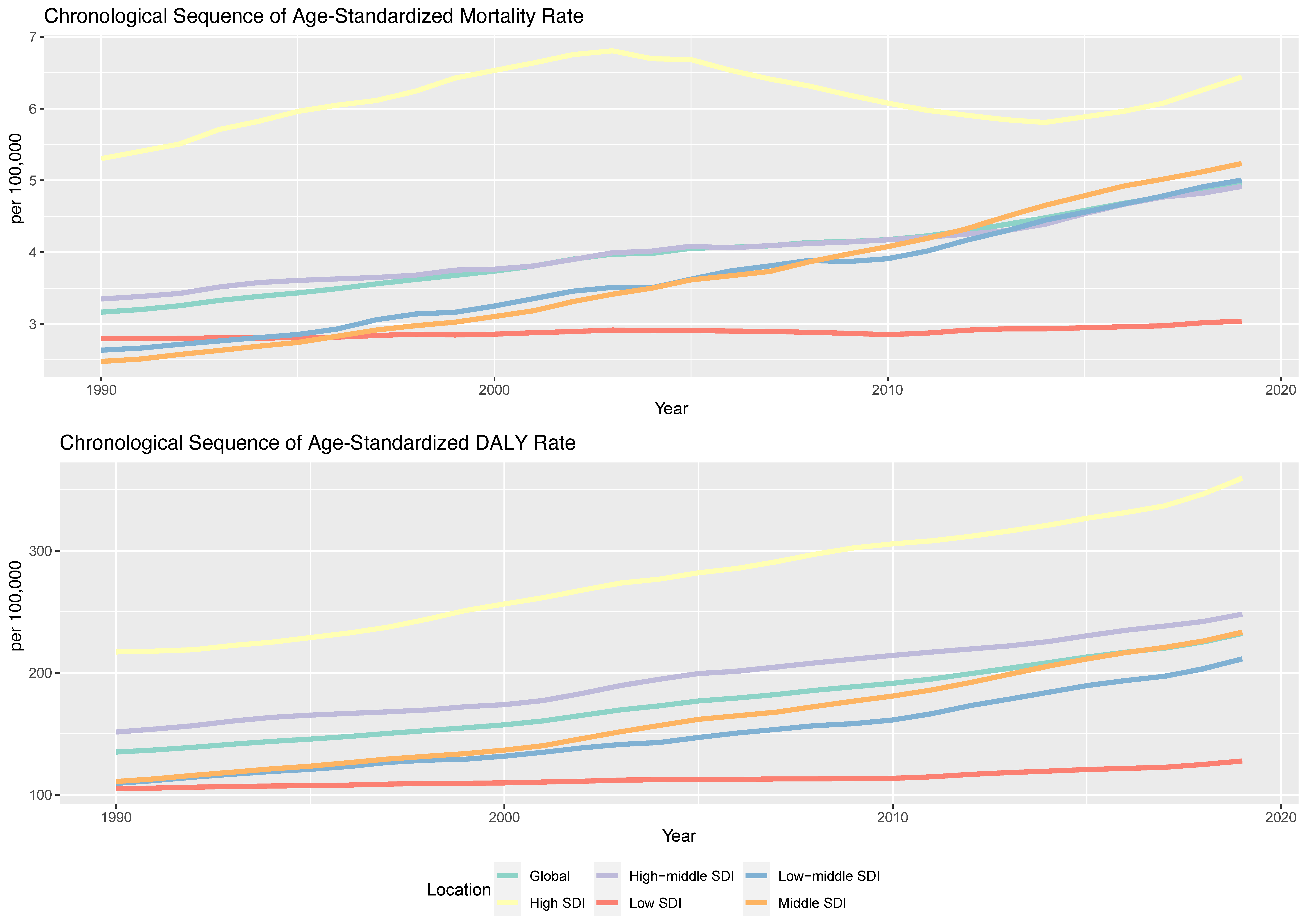
3.4. Influences of SDI Values on T2DM Burden Attributable to Dietary Risk Factors
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Sun, H.; Saeedi, P.; Karuranga, S.; Pinkepank, M.; Ogurtsova, K.; Duncan, B.B.; Stein, C.; Basit, A.; Chan, J.C.N.; Mbanya, J.C.; et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res. Clin. Pract. 2022, 183, 109119. [Google Scholar] [CrossRef] [PubMed]
- Ye, J.; Wu, Y.; Yang, S.; Zhu, D.; Chen, F.; Chen, J.; Ji, X.; Hou, K. The global, regional and national burden of Type 2 Diabetes Mellitus in the past, present and future: A systematic analysis of the Global Burden of Disease Study 2019. Front. Endocrinol. 2023, 14, 1192629. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Bai, R.; Chai, Z.; Cooper, M.E.; Zimmet, P.Z.; Zhang, L. Low- and middle-income countries demonstrate rapid growth of type 2 diabetes: An analysis based on Global Burden of Disease 1990–2019 data. Diabetologia 2022, 65, 1339–1352. [Google Scholar] [CrossRef]
- Collaborators, G.B.D.D. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: A systematic analysis for the Global Burden of Disease Study 2021. Lancet 2023, 402, 203–234. [Google Scholar] [CrossRef]
- GBD Diabetes in the Americas Collaborators. Burden of diabetes and hyperglycaemia in adults in the Americas, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Diabetes Endocrinol. 2022, 10, 655–667. [Google Scholar] [CrossRef]
- World Health Organization. Diabetes. Available online: https://www.who.int/news-room/fact-sheets/detail/diabetes (accessed on 12 September 2023).
- Goodall, R.; Alazawi, A.; Hughes, W.; Bravis, V.; Salciccioli, J.D.; Marshall, D.C.; Crowley, C.; Shalhoub, J. Trends in Type 2 Diabetes Mellitus disease burden in European Union countries between 1990 and 2019. Sci. Rep. 2021, 11, 15356. [Google Scholar] [CrossRef]
- Sun, P.; Wen, H.; Liu, X.; Ma, Y.; Jang, J.; Yu, C. Time trends in Type 2 Diabetes Mellitus incidence across the BRICS from 1990 to 2019: An age-period-cohort analysis. BMC Public Health 2022, 22, 65. [Google Scholar] [CrossRef]
- Al Kaabi, J.; Mustafa, H.; Govender, R.D.; King, J.K.; Hashim, M.J.; Khan, M.A.B. Epidemiology of Type 2 Diabetes—Global Burden of Disease and Forecasted Trends. J. Epidemiol. Glob. Health 2019, 10, 107. [Google Scholar] [CrossRef]
- Alhazmi, A.; Stojanovski, E.; McEvoy, M.; Garg, M.L. The association between dietary patterns and type 2 diabetes: A systematic review and meta-analysis of cohort studies. J. Hum. Nutr. Diet. 2014, 27, 251–260. [Google Scholar] [CrossRef]
- Papamichou, D.; Panagiotakos, D.B.; Itsiopoulos, C. Dietary patterns and management of type 2 diabetes: A systematic review of randomised clinical trials. Nutr. Metab. Cardiovasc. Dis. 2019, 29, 531–543. [Google Scholar] [CrossRef]
- Zeraattalab-Motlagh, S.; Jayedi, A.; Shab-Bidar, S. Mediterranean dietary pattern and the risk of type 2 diabetes: A systematic review and dose-response meta-analysis of prospective cohort studies. Eur. J. Nutr. 2022, 61, 1735–1748. [Google Scholar] [CrossRef] [PubMed]
- Fang, M.; Hu, Z.F.; Feng, L.J. Association between dietary pattern and the risk of Type 2 Diabetes Mellitus in Zhejiang Province, China: A case-control study. Asia Pac. J. Clin. Nutr. 2020, 29, 821–826. [Google Scholar] [CrossRef]
- He, C.; Wang, W.; Chen, Q.; Shen, Z.; Pan, E.; Sun, Z.; Lou, P.; Zhang, X. Association between dietary patterns and stroke in patients with Type 2 Diabetes Mellitus in China: A propensity score-matched analysis. Public. Health Nutr. 2022, 25, 1–25. [Google Scholar] [CrossRef] [PubMed]
- O’Hearn, M.; Lara-Castor, L.; Cudhea, F.; Miller, V.; Reedy, J.; Shi, P.; Zhang, J.; Wong, J.B.; Economos, C.D.; Micha, R.; et al. Incident type 2 diabetes attributable to suboptimal diet in 184 countries. Nat. Med. 2023, 29, 982–995. [Google Scholar] [CrossRef]
- Singh, G.M.; Micha, R.; Khatibzadeh, S.; Lim, S.; Ezzati, M.; Mozaffarian, D.; Global Burden of Diseases, N.; Chronic Diseases Expert, G. Estimated Global, Regional, and National Disease Burdens Related to Sugar-Sweetened Beverage Consumption in 2010. Circulation 2015, 132, 639–666. [Google Scholar] [CrossRef] [PubMed]
- Mari-Sanchis, A.; Gea, A.; Basterra-Gortari, F.J.; Martinez-Gonzalez, M.A.; Beunza, J.J.; Bes-Rastrollo, M. Meat Consumption and Risk of Developing Type 2 Diabetes in the SUN Project: A Highly Educated Middle-Class Population. PLoS ONE 2016, 11, e0157990. [Google Scholar] [CrossRef] [PubMed]
- Sanders, L.M.; Wilcox, M.L.; Maki, K.C. Red meat consumption and risk factors for type 2 diabetes: A systematic review and meta-analysis of randomized controlled trials. Eur. J. Clin. Nutr. 2023, 77, 156–165. [Google Scholar] [CrossRef]
- Otto, M.C.; Afshin, A.; Micha, R.; Khatibzadeh, S.; Fahimi, S.; Singh, G.; Danaei, G.; Sichieri, R.; Monteiro, C.A.; Louzada, M.L.; et al. The Impact of Dietary and Metabolic Risk Factors on Cardiovascular Diseases and Type 2 Diabetes Mortality in Brazil. PLoS ONE 2016, 11, e0151503. [Google Scholar] [CrossRef]
- Institute for Health Metrics and Evaluation (IHME), University of Washington. GBD Results. Available online: https://vizhub.healthdata.org/gbd-results/ (accessed on 1 August 2023).
- GBD Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1223–1249. [Google Scholar] [CrossRef]
- GBD Diseases Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- Stevens, G.A.; Alkema, L.; Black, R.E.; Boerma, J.T.; Collins, G.S.; Ezzati, M.; Grove, J.T.; Hogan, D.R.; Hogan, M.C.; Horton, R.; et al. Guidelines for Accurate and Transparent Health Estimates Reporting: The GATHER statement. Lancet 2016, 388, e19–e23. [Google Scholar] [CrossRef] [PubMed]
- GBD DALYs HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1859–1922. [Google Scholar] [CrossRef] [PubMed]
- Pan, Z.; Zhang, J.; Cheng, H.; Bu, Q.; Li, N.; Deng, Y.; Zhou, L.; Dai, Z.; Lyu, J. Trends of the incidence of drug use disorders from 1990 to 2017: An analysis based on the Global Burden of Disease 2017 data. Epidemiol. Psychiatr. Sci. 2020, 29, e148. [Google Scholar] [CrossRef] [PubMed]
- Weisman, A.; Fazli, G.S.; Johns, A.; Booth, G.L. Evolving Trends in the Epidemiology, Risk Factors, and Prevention of Type 2 Diabetes: A Review. Can. J. Cardiol. 2018, 34, 552–564. [Google Scholar] [CrossRef]
- Rygg, L.Ø.; Løhre, A.; Hellzèn, P.O. Lifestyle Changes in Diet and Physical Activities after Group Education for Type 2 Diabetes—The Active Ingredient in the Education. A Qualitative Study. Open J. Nurs. 2017, 7, 1181–1195. [Google Scholar] [CrossRef]
- Pearson-Stuttard, J.; Buckley, J.; Cicek, M.; Gregg, E.W. The Changing Nature of Mortality and Morbidity in Patients with Diabetes. Endocrinol. Metab. Clin. North. Am. 2021, 50, 357–368. [Google Scholar] [CrossRef]
- Rastogi, S.S.; Singh, R.B.; Singh, N.K.; Alam, S.M.; Singh, R.G.; Tripathi, K.K.; Srivastav, R.K.; Vajpeyee, S.K.; Gupta, H.; Muthusamy, V.V.; et al. Prevention of Cardiovascular Disease and Diabetes Mellitus In Low and Middle Income Countries. Open Nutraceuticals J. 2011, 4, 97–106. [Google Scholar] [CrossRef]
- Wang, P.Y.; Fang, J.C.; Gao, Z.H.; Zhang, C.; Xie, S.Y. Higher intake of fruits, vegetables or their fiber reduces the risk of type 2 diabetes: A meta-analysis. J. Diabetes Investig. 2016, 7, 56–69. [Google Scholar] [CrossRef]
- Halvorsen, R.E.; Elvestad, M.; Molin, M.; Aune, D. Fruit and vegetable consumption and the risk of type 2 diabetes: A systematic review and dose-response meta-analysis of prospective studies. BMJ Nutr. Prev. Health 2021, 4, 519–531. [Google Scholar] [CrossRef]
- Malik, F.; Iqbal, A.; Zia, S.; Ranjha, M.M.A.N.; Khalid, W.; Nadeem, M.; Selim, S.; Hadidi, M.; Moreno, A.; Manzoor, M.F.; et al. Role and mechanism of fruit waste polyphenols in diabetes management. Open Chem. 2023, 21, 20220272. [Google Scholar] [CrossRef]
- Solikhah, S.; Lestari, A. Processed meat consumption increases risk of Type 2 Diabetes Mellitus in adults aged 40 years and older. Universa Med. 2022, 41, 18–28. [Google Scholar] [CrossRef]
- Fretts, A.M.; Follis, J.L.; Nettleton, J.A.; Lemaitre, R.N.; Ngwa, J.S.; Wojczynski, M.K.; Kalafati, I.P.; Varga, T.V.; Frazier-Wood, A.C.; Houston, D.K.; et al. Consumption of meat is associated with higher fasting glucose and insulin concentrations regardless of glucose and insulin genetic risk scores: A meta-analysis of 50,345 Caucasians. Am. J. Clin. Nutr. 2015, 102, 1266–1278. [Google Scholar] [CrossRef] [PubMed]
- Shahinfar, H.; Jayedi, A.; Shab-Bidar, S. Dietary iron intake and the risk of type 2 diabetes: A systematic review and dose-response meta-analysis of prospective cohort studies. Eur. J. Nutr. 2022, 61, 2279–2296. [Google Scholar] [CrossRef]
- Bertoni, A.G.; Krop, J.S.; Anderson, G.F.; Brancati, F.L. Diabetes-related morbidity and mortality in a national sample of U.S. elders. Diabetes Care 2002, 25, 471–475. [Google Scholar] [CrossRef] [PubMed]
- Huang, E.S.; Laiteerapong, N.; Liu, J.Y.; John, P.M.; Moffet, H.H.; Karter, A.J. Rates of complications and mortality in older patients with diabetes mellitus: The diabetes and aging study. JAMA Intern. Med. 2014, 174, 251–258. [Google Scholar] [CrossRef] [PubMed]
- Basanta-Alario, M.L.; Ferri, J.; Civera, M.; Martinez-Hervas, S.; Ascaso, J.F.; Real, J.T. Differences in clinical and biological characteristics and prevalence of chronic complications related to aging in patients with type 2 diabetes. Endocrinol. Nutr. 2016, 63, 79–86. [Google Scholar] [CrossRef] [PubMed]
- Puig-Garcia, M.; Caicedo-Montano, C.; Marquez-Figueroa, M.; Chilet-Rosell, E.; Montalvo-Villacis, G.; Benazizi-Dahbi, I.; Peralta, A.; Torres-Castillo, A.L.; Parker, L.A. Prevalence and gender disparities of Type 2 Diabetes Mellitus and obesity in Esmeraldas, Ecuador: A population-based survey in a hard-to-reach setting. Int. J. Equity Health 2023, 22, 124. [Google Scholar] [CrossRef]
- Kautzky-Willer, A.; Leutner, M.; Abrahamian, H.; Fruhwald, L.; Hoppichler, F.; Lechleitner, M.; Harreiter, J. Sex and gender-specific aspects in prediabetes and diabetes mellitus-clinical recommendations (Update 2023). Wien. Klin. Wochenschr. 2023, 135, 275–285. [Google Scholar] [CrossRef]
- Ding, E.L.; Song, Y.; Malik, V.S.; Liu, S. Sex differences of endogenous sex hormones and risk of type 2 diabetes: A systematic review and meta-analysis. JAMA 2006, 295, 1288–1299. [Google Scholar] [CrossRef]
- Nakayama, Y.; Yamaguchi, S.; Shinzato, Y.; Okamoto, S.; Millman, J.F.; Yamashiro, K.; Takemoto, N.; Uema, T.; Arakaki, K.; Higa, M.; et al. Retrospective exploratory analyses on gender differences in determinants for incidence and progression of diabetic retinopathy in Japanese patients with Type 2 Diabetes Mellitus. Endocr. J. 2021, 68, 655–669. [Google Scholar] [CrossRef]
- Vandenheede, H.; Deboosere, P.; Espelt, A.; Bopp, M.; Borrell, C.; Costa, G.; Eikemo, T.A.; Gnavi, R.; Hoffmann, R.; Kulhanova, I.; et al. Educational inequalities in diabetes mortality across Europe in the 2000s: The interaction with gender. Int. J. Public Health 2015, 60, 401–410. [Google Scholar] [CrossRef] [PubMed]
- Safiri, S.; Karamzad, N.; Kaufman, J.S.; Bell, A.W.; Nejadghaderi, S.A.; Sullman, M.J.M.; Moradi-Lakeh, M.; Collins, G.; Kolahi, A.A. Prevalence, Deaths and Disability-Adjusted-Life-Years (DALYs) Due to Type 2 Diabetes and Its Attributable Risk Factors in 204 Countries and Territories, 1990–2019: Results From the Global Burden of Disease Study 2019. Front. Endocrinol. 2022, 13, 838027. [Google Scholar] [CrossRef] [PubMed]
- Qiao, J.; Lin, X.; Wu, Y.; Huang, X.; Pan, X.; Xu, J.; Wu, J.; Ren, Y.; Shan, P.F. Global burden of non-communicable diseases attributable to dietary risks in 1990–2019. J. Hum. Nutr. Diet 2022, 35, 202–213. [Google Scholar] [CrossRef]
- Hu, F.B. Globalization of diabetes: The role of diet, lifestyle, and genes. Diabetes Care 2011, 34, 1249–1257. [Google Scholar] [CrossRef] [PubMed]
- Ley, S.H.; Hamdy, O.; Mohan, V.; Hu, F.B. Prevention and management of type 2 diabetes: Dietary components and nutritional strategies. Lancet 2014, 383, 1999–2007. [Google Scholar] [CrossRef]
- Kastorini, C.M.; Panagiotakos, D.B. Dietary patterns and prevention of type 2 diabetes: From research to clinical practice; a systematic review. Curr. Diabetes Rev. 2009, 5, 221–227. [Google Scholar] [CrossRef] [PubMed]
- Deepa, M.; Anjana, R.M.; Mohan, V. Role of lifestyle factors in the epidemic of diabetes: Lessons learnt from India. Eur. J. Clin. Nutr. 2017, 71, 825–831. [Google Scholar] [CrossRef]
- Karatzi, K.; Manios, Y. The Role of Lifestyle, Eating Habits and Social Environment in the Prevention and Treatment of Type 2 Diabetes and Hypertension. Nutrients 2021, 13, 1460. [Google Scholar] [CrossRef]
- Hansen, K.L.; Golubovic, S.; Eriksen, C.U.; Jorgensen, T.; Toft, U. Effectiveness of food environment policies in improving population diets: A review of systematic reviews. Eur. J. Clin. Nutr. 2022, 76, 637–646. [Google Scholar] [CrossRef]








| Dietary Factor | Age-Standardized Rate Per 100,000 People (95% UI) | Estimated Annual Percentage Change from 1990 to 2019 (95% CI) | ||||
|---|---|---|---|---|---|---|
| 1990 | 2019 | |||||
| Death Rate | DALY Rate | Death Rate | DALY Rate | Death Rate | DALY Rate | |
| Dietary risks | 3.17 (2.61, 3.70) | 135.00 (104.85, 165.97) | 4.96 (4.07, 5.82) | 232.12 (176.48, 292.50) | 1.46 (1.39, 1.52) | 1.89 (1.85, 1.93) |
| Diet low in fruits | 0.76 (0.48, 1.06) | 33.36 (20.79, 48.12) | 1.14 (0.72, 1.63) | 51.00 (30.63, 76.36) | 1.3 (1.24, 1.37) | 1.35 (1.29, 1.40) |
| Diet high in red meat | 0.65 (0.36, 0.90) | 28.49 (16.32, 41.26) | 1.06 (0.59, 1.49) | 53.29 (31.46, 77.06) | 1.61 (1.53, 1.68) | 2.28 (2.22, 2.34) |
| Diet high in processed meat | 0.64 (0.45, 0.77) | 27.06 (18.61, 35.35) | 0.95 (0.66, 1.14) | 47.56 (31.42, 63.10) | 1.2 (1.12, 1.28) | 2.06 (2.01, 2.12) |
| Diet low in whole grains | 0.58 (0.20, 0.85) | 24.09 (8.43, 36.92) | 0.94 (0.33, 1.40) | 42.65 (14.60, 66.49) | 1.62 (1.56, 1.67) | 1.99 (1.95, 2.02) |
| Diet high in sugar-sweetened beverages | 0.38 (0.26, 0.48) | 16.15 (10.81, 21.30) | 0.63 (0.39, 0.82) | 30.17 (17.89, 41.87) | 1.63 (1.55, 1.71) | 2.18 (2.12, 2.24) |
| Diet low in fiber | 0.38 (0.18, 0.59) | 15.76 (7.11, 24.64) | 0.53 (0.23, 0.84) | 22.99 (9.39, 37.17) | 1.03 (0.93, 1.12) | 1.26 (1.21, 1.31) |
| Diet low in nuts and seeds | 0.24 (0.06, 0.48) | 10.30 (2.41, 20.66) | 0.37 (0.11, 0.71) | 17.01 (4.81, 33.20) | 1.51 (1.44, 1.58) | 1.76 (1.68, 1.84) |
| Region | Age-Standardized Rate Per 100,000 People (95% UI) | Estimated Annual Percentage Change from 1990 to 2019 (95% CI) | ||||
|---|---|---|---|---|---|---|
| 1990 | 2019 | |||||
| Death Rate | DALY Rate | Death Rate | DALY Rate | Death Rate | DALY Rate | |
| Global | 3.17 (2.61, 3.70) | 135.00 (104.85, 165.97) | 4.96 (4.07, 5.82) | 232.12 (176.48, 292.50) | 1.46 (1.39, 1.52) | 1.89 (1.85, 1.93) |
| SDI | ||||||
| High SDI | 5.30 (4.48, 6.10) | 217.00 (170.58, 270.68) | 6.44 (5.36, 7.49) | 359.59 (267.05, 470.45) | 0.21 (−0.07, 0.48) | 1.77 (1.71, 1.83) |
| High-middle SDI | 3.35 (2.80, 3.88) | 151.44 (116.43, 189.58) | 4.91 (4.04, 5.74) | 247.97 (185.29, 318.94) | 1.21 (1.14, 1.28) | 1.73 (1.67, 1.78) |
| Middle SDI | 2.48 (1.98, 2.96) | 110.81 (85.27, 138.27) | 5.23 (4.16, 6.21) | 233.17 (178.27, 296.05) | 2.71 (2.66, 2.76) | 2.66 (2.6, 2.71) |
| Low-middle SDI | 2.64 (2.10, 3.20) | 109.27 (85.93, 134.46) | 5.00 (4.08, 5.91) | 211.27 (163.45, 261.36) | 2.25 (2.18, 2.31) | 2.22 (2.14, 2.3) |
| Low SDI | 2.79 (2.21, 3.41) | 104.85 (80.78, 128.68) | 3.04 (2.42, 3.67) | 127.66 (96.62, 158.69) | 0.23 (0.19, 0.27) | 0.57 (0.51, 0.63) |
| Southeast Asia, East Asia, and Oceania Region | 2.15 (1.71, 2.58) | 103.26 (77.86, 130.21) | 4.22 (3.26, 5.11) | 203.71 (153.06, 261.17) | 2.45 (2.37, 2.53) | 2.47 (2.38, 2.56) |
| East Asia | 1.51 (1.18, 1.88) | 90.39 (66.50, 118.01) | 3.10 (2.35, 3.85) | 181.14 (131.13, 241.61) | 2.6 (2.39, 2.82) | 2.59 (2.4, 2.78) |
| Southeast Asia | 3.73 (2.90, 4.52) | 134.13 (103.85, 164.34) | 6.51 (4.89, 8.06) | 247.24 (186.80, 309.68) | 2.01 (1.86, 2.17) | 2.11 (1.95, 2.27) |
| Oceania | 8.49 (6.18, 11.04) | 312.07 (222.80, 404.46) | 12.93 (9.36, 17.15) | 498.11 (353.54, 651.27) | 1.3 (1.13, 1.46) | 1.54 (1.41, 1.67) |
| Central Europe, Eastern Europe, and Central Asia Region | 2.71 (2.30, 3.10) | 160.13 (122.19, 203.10) | 5.18 (4.26, 6.02) | 291.70 (217.85, 377.29) | 2.03 (1.74, 2.32) | 1.98 (1.86, 2.09) |
| Central Asia | 2.09 (1.77, 2.40) | 118.48 (91.19, 149.12) | 6.02 (4.91, 7.21) | 303.60 (230.56, 383.03) | 3.03 (2.69, 3.36) | 3.03 (2.87, 3.19) |
| Central Europe | 4.41 (3.67, 5.08) | 228.09 (173.66, 288.47) | 7.43 (6.00, 8.95) | 436.28 (321.48, 571.21) | 2.14 (1.95, 2.34) | 2.48 (2.32, 2.65) |
| Eastern Europe | 1.97 (1.68, 2.26) | 135.98 (103.24, 173.47) | 3.57 (2.88, 4.27) | 207.74 (155.38, 267.95) | 1.33 (0.64, 2.02) | 1.08 (0.88, 1.28) |
| High-income Region | 6.04 (5.12, 6.92) | 232.48 (183.56, 288.60) | 7.18 (6.01, 8.34) | 376.21 (279.78, 490.85) | 0.19 (−0.03, 0.42) | 1.68 (1.61, 1.75) |
| High-income Asia Pacific | 2.45 (1.99, 2.91) | 134.45 (99.88, 173.86) | 3.30 (2.59, 3.99) | 239.35 (169.86, 320.99) | 0.82 (0.56, 1.09) | 1.73 (1.54, 1.92) |
| Australasia | 4.76 (4.07, 5.44) | 163.79 (131.31, 201.31) | 6.22 (5.16, 7.28) | 268.90 (201.59, 346.25) | 0.57 (0.26, 0.88) | 1.48 (1.33, 1.63) |
| Western Europe | 7.43 (6.24, 8.53) | 251.82 (198.36, 312.94) | 7.77 (6.42, 9.10) | 366.59 (268.99, 480.43) | −0.08 (−0.17, 0.01) | 1.17 (1.12, 1.23) |
| Southern Latin America | 6.57 (5.59, 7.48) | 216.87 (174.98, 259.84) | 8.38 (7.07, 9.63) | 345.82 (266.94, 437.30) | 0.45 (0.26, 0.65) | 1.35 (1.23, 1.47) |
| High-income North America | 6.35 (5.40, 7.30) | 274.25 (218.41, 340.33) | 8.32 (6.98, 9.64) | 472.14 (365.09, 610.56) | 0.24 (−0.21, 0.69) | 2.18 (2.04, 2.32) |
| Latin America and Caribbean Region | 4.54 (3.61, 5.42) | 183.84 (141.85, 230.77) | 8.44 (6.71, 10.07) | 348.72 (266.30, 437.57) | 2.08 (1.99, 2.17) | 2.24 (2.15, 2.34) |
| Caribbean | 6.14 (4.61, 7.65) | 229.35 (169.25, 295.13) | 8.00 (5.69, 10.21) | 341.23 (243.42, 456.60) | 0.72 (0.6, 0.85) | 1.25 (1.13, 1.37) |
| Andean Latin America | 2.16 (1.61, 2.70) | 80.96 (59.43, 102.90) | 4.48 (3.23, 5.79) | 173.56 (126.22, 227.38) | 2.67 (2.53, 2.81) | 2.7 (2.61, 2.79) |
| Central Latin America | 4.96 (3.93, 5.94) | 206.80 (158.01, 261.31) | 9.90 (7.67, 12.15) | 420.57 (318.47, 537.62) | 2.23 (2.04, 2.41) | 2.42 (2.27, 2.58) |
| Tropical Latin America | 4.30 (3.44, 5.13) | 174.39 (135.64, 219.59) | 8.02 (6.57, 9.50) | 319.77 (248.35, 397.51) | 2.21 (2.16, 2.27) | 2.25 (2.18, 2.32) |
| North Africa and Middle East Region | 2.17 (1.60, 2.76) | 87.74 (63.62, 113.42) | 3.21 (2.43, 4.01) | 167.81 (118.61, 223.20) | 1.51 (1.31, 1.72) | 2.48 (2.27, 2.69) |
| South Asia Region | 2.32 (1.83, 2.87) | 102.98 (79.08, 129.34) | 4.89 (3.98, 5.90) | 217.29 (166.32, 271.73) | 2.61 (2.52, 2.71) | 2.46 (2.37, 2.55) |
| Sub-Saharan Africa Region | 3.28 (2.61, 3.96) | 108.87 (85.13, 131.84) | 3.36 (2.66, 4.09) | 118.99 (93.62, 145.19) | 0.09 (0, 0.17) | 0.28 (0.23, 0.33) |
| Central Sub-Saharan Africa | 3.87 (3.08, 4.68) | 112.10 (88.26, 136.49) | 4.24 (3.38, 5.15) | 130.10 (102.65, 158.47) | −0.29 (−0.38, −0.21) | 0.31 (0.25, 0.36) |
| Eastern Sub-Saharan Africa | 2.76 (2.20, 3.36) | 109.63 (86.76, 133.08) | 3.02 (2.39, 3.67) | 118.39 (93.42, 144.10) | −1.01 (−1.15, −0.86) | −0.74 (−0.89, −0.6) |
| Southern Sub-Saharan Africa | 2.42 (1.92, 2.95) | 88.60 (69.88, 107.80) | 2.51 (1.99, 3.07) | 94.28 (74.34, 114.88) | 3.17 (2.77, 3.57) | 3.01 (2.71, 3.32) |
| Western Sub-Saharan Africa | 4.11 (3.27, 5.02) | 118.08 (93.62, 142.96) | 4.47 (3.55, 5.45) | 136.21 (108.19, 165.09) | −0.16 (−0.26, −0.07) | 0.14 (0.08, 0.19) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Forray, A.I.; Coman, M.A.; Simonescu-Colan, R.; Mazga, A.I.; Cherecheș, R.M.; Borzan, C.M. The Global Burden of Type 2 Diabetes Attributable to Dietary Risks: Insights from the Global Burden of Disease Study 2019. Nutrients 2023, 15, 4613. https://doi.org/10.3390/nu15214613
Forray AI, Coman MA, Simonescu-Colan R, Mazga AI, Cherecheș RM, Borzan CM. The Global Burden of Type 2 Diabetes Attributable to Dietary Risks: Insights from the Global Burden of Disease Study 2019. Nutrients. 2023; 15(21):4613. https://doi.org/10.3390/nu15214613
Chicago/Turabian StyleForray, Alina Ioana, Mădălina Adina Coman, Ruxandra Simonescu-Colan, Andreea Isabela Mazga, Răzvan Mircea Cherecheș, and Cristina Maria Borzan. 2023. "The Global Burden of Type 2 Diabetes Attributable to Dietary Risks: Insights from the Global Burden of Disease Study 2019" Nutrients 15, no. 21: 4613. https://doi.org/10.3390/nu15214613
APA StyleForray, A. I., Coman, M. A., Simonescu-Colan, R., Mazga, A. I., Cherecheș, R. M., & Borzan, C. M. (2023). The Global Burden of Type 2 Diabetes Attributable to Dietary Risks: Insights from the Global Burden of Disease Study 2019. Nutrients, 15(21), 4613. https://doi.org/10.3390/nu15214613








