Dietary and Nutritional Interventions in Nonalcoholic Fatty Liver Disease in Pediatrics
Abstract
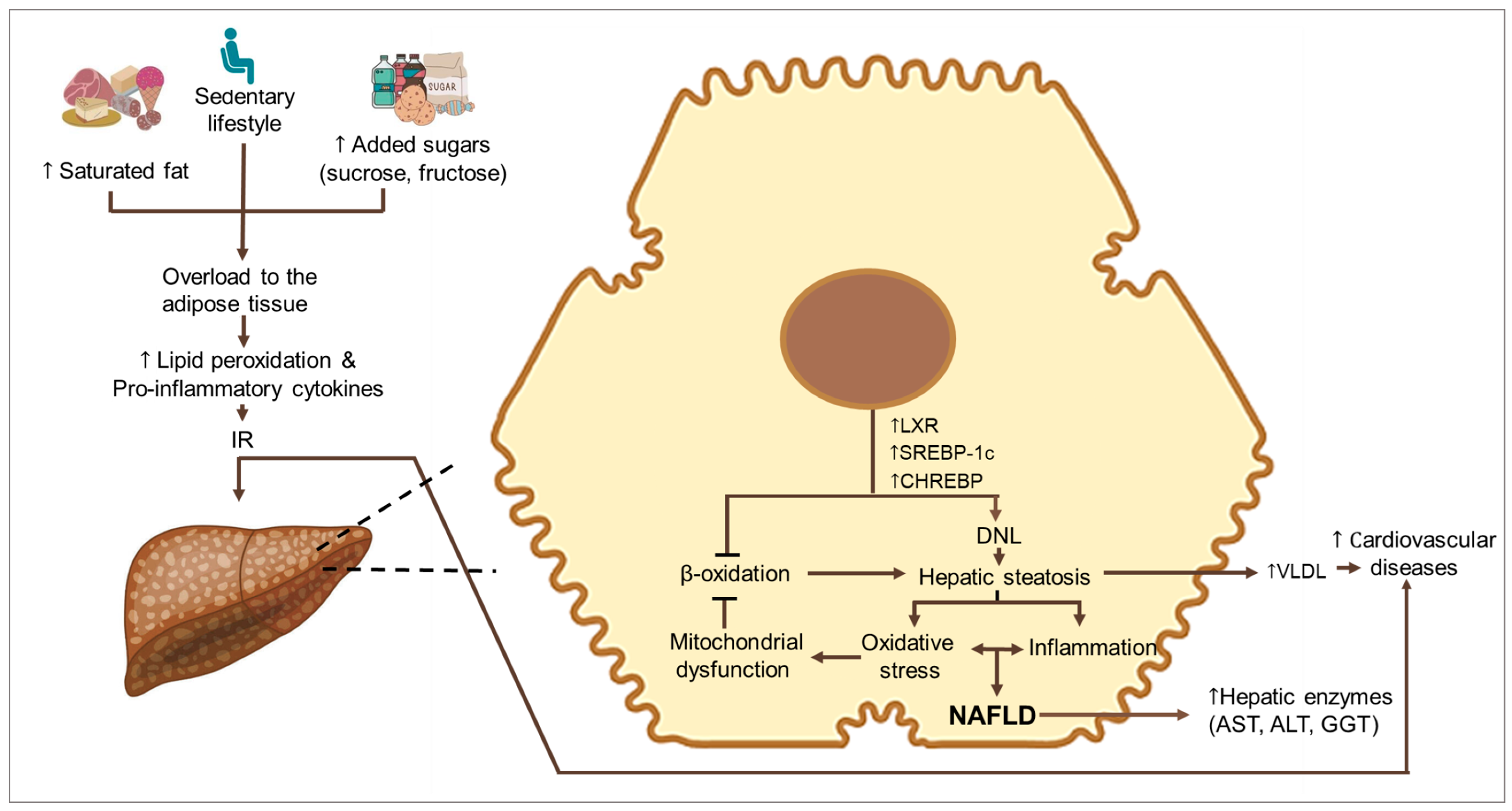
:1. Introduction
2. Methods
3. Lifestyle Modifications
3.1. Exercise and Dietary Changes
3.2. Exercise Interventions
4. Specific Dietary Interventions
4.1. Carbohydrates
4.1.1. Low Carbohydrate Diets
4.1.2. Low-Free-Sugars Diets
4.1.3. Low Fructose Diets
4.2. Fatty Acids
Low-Fat Diets
4.3. Dietary Patterns
4.3.1. Mediterranean Diet
| Intervention | Age Group | Duration | n | Results | References |
|---|---|---|---|---|---|
| Restricted carbohydrate diet in children and adolescents (Intervention Study). | 9–17 years old | 8 weeks | 25 | The intervention had beneficial effects on liver lipids (−6.0 ± 4.7%, by MRI), ↓ ALT (fat restrictive diet: −5.8 U/L; restrictive carbohydrate diet −23.6 U/L), ↓ AST (fat restrictive diet: −2.8 U/L; restrictive carbohydrate diet −20.7 U/L), ↓ body weight (fat restrictive diet: −0.4 kg; restrictive carbohydrate diet −3.0 kg), and IR. | [14] |
| Diet low in free sugars (glucose, fructose, and sucrose) in male adolescents (Intervention Study). | 11–16 years old | 8 weeks | 20 | ↓ hepatic steatosis (−6.23%, by MRI-PDFF) and decrease in ALT (−42 U/L). | [17] |
| Diet low in added sugars in children and adolescents (Intervention Study). | 11–16 years old | 8 weeks | 29 | ↓ hepatic DNL (34.6% to 24.1%), hepatic steatosis (−8%, by MRI-PDFF), ALT (−30.5 U/L), and ↓ fasting insulin. | [30] |
| Reduced fructose diet in adolescents (Intervention Study). | 11–18 years old | 4 weeks | 21 | ↓ hepatic fat (fructose reduction: −0.9%, glucose reduction: 0.2%, by MRS). | [13] |
| Follow-up of dietary records in a cohort of adolescents (Intervention Study). | 14–17 years old | 3 years follow up | 592 | For every 1 g increase in fructose energy-adjusted, the odds of NAFLD in obese adolescents increased by 9% (OR). | [15] |
| Oral absorption of fructose in obese children with NAFLD (Intervention Study). | 8–18 years old | 1 day | 9 | Children with NAFLD absorb and metabolize fructose more efficiently than lean subjects. | [31] |
| Assess fructose intake in obese children and its relation to NAFLD. (Case-control study). | 6–14 years old | Observational study | 85 | High fructose intake is associated with increased P3NP ( Procollagen type III N-terminal peptide) and increased NAFLD grade. P3NP may serve as a marker of NAFLD in obese children with a proposed cutoff value of 8.5 ng/mL | [32] |
| Diet evaluation in pediatric patients with NAFLD. (Case-control study). | 8–18 years old | 4 weeks | 24 | There is a lower consumption of polyunsaturated fatty acids and a higher intake of saturated fatty acids in patients with NAFLD. | [43] |
| Mediterranean and low-fat diet in children (Intervention Study). | 11–18 years old | 12 weeks | 44 | ↓ Body weight (−5.1 kg), serum ALT levels (−18 U/L), AST (−10 U/L) and ↓ IR, no significant differences with low-fat diet. | [33] |
| Mediterranean and low-fat diet in children (Intervention Study). | 9–17 years old | 12 weeks | 60 | ↓ hepatic steatosis (Mediterranean diet: −0.8%; low fat diet: −0.8%, by ultrasonography), ALT (Mediterranean diet: −25.4 U/L); low fat diet: −24.0 U/L), AST (Mediterranean diet: −10.4 U/L; low fat diet: −15.7 U/L), and ↓ IR improvement. | [34] |
| Association of the Mediterranean diet and NAFLD in children (Observational study). | 8–15 years old | Cross-sectional study | 181 | Diet compliance is lower in children with NAFLD than in healthy children, a low score on the KIDMED index was associated with a high BMI and obesity in children. | [38] |
| Association of the Mediterranean diet and NAFLD in children (Observational study). | 11–15 years old | Cross-sectional study | 113 | Diet compliance is lower in children with the pathology than in healthy children; poor adherence to the diet was correlated with liver damage. | [41] |
| Influence of Chinese dietary patterns on NAFLD among adolescents in Shandong, China (Observational study). | 16–23 years old | Cross-sectional study | 1639 | It was shown that the traditional diet provides a protective effect in preventing NAFLD, while the occidental eating pattern was associated with the pathology. | [42] |
4.3.2. Chinese Diets
5. Nutritional Interventions
5.1. N-3 Polyunsaturated Fatty Acids
5.2. Amino Acids
5.2.1. Cysteine
5.2.2. L-carnitine
5.3. Vitamins
5.3.1. Vitamin E (Alpha-Tocopherol)
5.3.2. Vitamin D
5.4. Probiotics
5.4.1. Lactobacillus Rhamnosus GG (LGG)
5.4.2. Multi-Strain Probiotics
| Intervention | Age Group | Duration | n | Results | References |
|---|---|---|---|---|---|
| Supplementation with n-3 LCPUFA (450–1300 mg/day) or placebo in overweight children diagnosed with NAFLD. | Children > 5 years and <19 years old | 24 weeks | 30 | No reduction in ALT levels or hepatic steatosis, ↓ levels of AST (−11 U/L) and GGT (−9 U/L). | [45] |
| Supplementation with 250 or 500 mg/day of DHA or placebo. | 11 to 13 years | 6 months | 60 | ↓ steatosis (The odds of more severe versus less severe steatosis after treatment with DHA 250 mg/day (OR = 0.01) and DHA 500 mg/ day (OR = 0.04), by ultrasonography) and TG. It ↑ in insulin sensitivity. | [46] |
| Delayed-release cysteamine bitartrate supplementation in children with NAFLD, placebo-controlled. | 8 to 17 years | 52 weeks | 88 | No histological improvement of the disease, significantly greater improvement for lobular inflammation (−15%), and a decrease in alanine aminotransferase (−45 U/L) and aspartate aminotransferase (−27 U/L). | [51] |
| Supplementation with L-carnitine 50 mg/kg/day twice a day, in children and adolescents with NAFLD, controlled with a placebo. | 5 to 15 years | 3 months | 31 | No improvements in biochemical and ultrasound markers of NAFLD were observed. | [52] |
| Lifestyle intervention with or without supplementation with 600 mg/day of vitamin E in obese children with liver steatosis. | 6 to 10 years | 6 months | 24 | Significant ↓ oxidative stress, ALT (−7.7 U/L), lipid profile and HOMA-IR. | [55] |
| Supplementation with 2000 IU/day of vitamin D or placebo in children with NAFLD confirmed by biopsy. | 9 to 18 years | 6 months | 55 | ↓ liver steatosis and lobular inflammation (by liver biopsy), AST (−16 U/L), and ALT levels (−28.4 U/L), ↓ improvement in lipid profile parameters and IR, and ↑ in vitamin D levels (+27.7 ng/mL). | [63] |
| LGG (1.2 × 1010 CFU/day) supplementation in children with obesity, persistent hypertransaminasaemia, and bright liver echo pattern. | 10.7 ± 2.1 years | 8 weeks | 20 | ↓ ALT (up to normalization in 80% of cases). | [67] |
| VSL#3 supplementation (1 or 2 sachets) versus placebo in children with obesity and NAFLD confirmed by biopsy. | 9 to 12 years | 4 months | 32 | NAFLD improvement (More severe versus less severe steatosis OR: 0.001, by ultrasound), BMI, and ↑ in anorexigenic intestinal hormones (including GLP-1 and GLP-2). | [69] |
| Probiotic capsule supplementation placebo-controlled for obese children and adolescents with NAFLD confirmed by liver ultrasound. | 10 to 18 years | 12 weeks | 43 | Normal liver sonography was reported in 53.1% of patients, ↓ mean levels of ALT (−9.7 U/L), AST (−7.9 U/L), total cholesterol, waist circumference, LDL, and TG. | [70] |
| Bio-Kult® supplementation in obese children and adolescents with ultrasound evidence of hepatic steatosis and NASH. | 5 to 15 years | 6 months | 84 | Probiotics had no advantage over lifestyle modification in improving obesity-associated metabolic disorders in children. | [71] |
6. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Trandafir, L.M.; Frasinariu, O.E.; Leon-Constantin, M.M.; Chiriac, Ş.; Trandafirescu, M.F.; Miron, I.C.; Luca, A.C.; Iordache, A.C.; Cojocaru, E. Pediatric nonalcoholic fatty liver disease—A changing diagnostic paradigm. Rom. J. Morphol. Embryol. 2020, 61, 1023–1031. [Google Scholar] [CrossRef]
- Anderson, E.L.; Howe, L.D.; Jones, H.E.; Higgins, J.P.; Lawlor, D.A.; Fraser, A. The Prevalence of Non-Alcoholic Fatty Liver Disease in Children and Adolescents: A Systematic Review and Meta-Analysis. PLoS ONE 2015, 10, e0140908. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Ha, A.; Rui, F.; Zou, B.; Yang, H.; Xue, Q.; Hu, X.; Xu, Y.; Henry, L.; Barakat, M.; et al. Meta-analysis: Global prevalence, trend and forecasting of non-alcoholic fatty liver disease in children and adolescents, 2000–2021. Aliment. Pharmacol. Ther. 2022, 56, 396–406. [Google Scholar] [CrossRef] [PubMed]
- Shaunak, M.; Byrne, C.D.; Davis, N.; Afolabi, P.; Faust, S.N.; Davies, J.H. Non-alcoholic fatty liver disease and childhood obesity. Arch. Dis. Child. 2021, 106, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Tan, Z.; Jiang, Z.; Li, M.; Wang, W.; Huang, Y.; Sun, J. Comparative efficacy and safety of traditional Chinese patent medicine for NAFLD in childhood or adolescence: A protocol for a Bayesian network meta analysis. Medicine 2021, 100, e24277. [Google Scholar] [CrossRef] [PubMed]
- Soullane, S.; Willems, P.; Lee, G.E.; Auger, N. Early life programming of nonalcoholic fatty liver disease in children. Early Hum. Dev. 2022, 168, 105578. [Google Scholar] [CrossRef] [PubMed]
- Cuzmar, V.; Alberti, G.; Uauy, R.; Pereira, A.; García, C.; De Barbieri, F.; Corvalán, C.; Santos, J.L.; Mericq, V.; Villarroel, L.; et al. Early Obesity: Risk Factor for Fatty Liver Disease. J. Pediatr. Gastroenterol. Nutr. 2020, 70, 93–98. [Google Scholar] [CrossRef]
- Ueda, P.; Kondo, N.; Fujiwara, T. The global economic crisis, household income and pre-adolescent overweight and underweight: A nationwide birth cohort study in Japan. Int. J. Obes. 2015, 39, 1414–1420. [Google Scholar] [CrossRef]
- Zheng, W.; Yokomichi, H.; Matsubara, H.; Ishikuro, M.; Kikuya, M.; Isojima, T.; Yokoya, S.; Tanaka, T.; Kato, N.; Chida, S.; et al. Longitudinal changes in body mass index of children affected by the Great East Japan Earthquake. Int. J. Obes. 2017, 41, 606–612. [Google Scholar] [CrossRef]
- Mandala, A.; Janssen, R.C.; Palle, S.; Short, K.R.; Friedman, J.E. Pediatric Non-Alcoholic Fatty Liver Disease: Nutritional Origins and Potential Molecular Mechanisms. Nutrients 2020, 12, 3166. [Google Scholar] [CrossRef]
- Alberti, G.; Gana, J.C.; Santos, J.L. Fructose, Omega 3 Fatty Acids, and Vitamin E: Involvement in Pediatric Non-Alcoholic Fatty Liver Disease. Nutrients 2020, 12, 3531. [Google Scholar] [CrossRef] [PubMed]
- Ramírez-Mejía, M.M.; Díaz-Orozco, L.E.; Barranco-Fragoso, B.; Méndez-Sánchez, N. A Review of the Increasing Prevalence of Metabolic-Associated Fatty Liver Disease (MAFLD) in Children and Adolescents Worldwide and in Mexico and the Implications for Public Health. Med. Sci. Monit. 2021, 27, e934134. [Google Scholar] [CrossRef]
- Jin, R.; Welsh, J.A.; Le, N.A.; Holzberg, J.; Sharma, P.; Martin, D.R.; Vos, M.B. Dietary fructose reduction improves markers of cardiovascular disease risk in Hispanic-American adolescents with NAFLD. Nutrients 2014, 6, 3187–3201. [Google Scholar] [CrossRef] [PubMed]
- Goss, A.M.; Dowla, S.; Pendergrass, M.; Ashraf, A.; Bolding, M.; Morrison, S.; Amerson, A.; Soleymani, T.; Gower, B. Effects of a carbohydrate-restricted diet on hepatic lipid content in adolescents with non-alcoholic fatty liver disease: A pilot, randomized trial. Pediatr. Obes. 2020, 15, e12630. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, T.A.; Oddy, W.H.; Bremner, A.P.; Sherriff, J.L.; Ayonrinde, O.T.; Olynyk, J.K.; Beilin, L.J.; Mori, T.A.; Adams, L.A. Lower fructose intake may help protect against development of nonalcoholic fatty liver in adolescents with obesity. J. Pediatr. Gastroenterol. Nutr. 2014, 58, 624–631. [Google Scholar] [CrossRef] [PubMed]
- Gibson, P.S.; Lang, S.; Gilbert, M.; Kamat, D.; Bansal, S.; Ford-Adams, M.E.; Desai, A.P.; Dhawan, A.; Fitzpatrick, E.; Moore, J.B.; et al. Assessment of Diet and Physical Activity in Paediatric Non-Alcoholic Fatty Liver Disease Patients: A United Kingdom Case Control Study. Nutrients 2015, 7, 9721–9733. [Google Scholar] [CrossRef] [PubMed]
- Schwimmer, J.B.; Ugalde-Nicalo, P.; Welsh, J.A.; Angeles, J.E.; Cordero, M.; Harlow, K.E.; Alazraki, A.; Durelle, J.; Knight-Scott, J.; Newton, K.P.; et al. Effect of a Low Free Sugar Diet vs Usual Diet on Nonalcoholic Fatty Liver Disease in Adolescent Boys: A Randomized Clinical Trial. JAMA 2019, 321, 256–265. [Google Scholar] [CrossRef] [PubMed]
- Vos, M.B.; Abrams, S.H.; Barlow, S.E.; Caprio, S.; Daniels, S.R.; Kohli, R.; Mouzaki, M.; Sathya, P.; Schwimmer, J.B.; Sundaram, S.S.; et al. NASPGHAN Clinical Practice Guideline for the Diagnosis and Treatment of Nonalcoholic Fatty Liver Disease in Children: Recommendations from the Expert Committee on NAFLD (ECON) and the North American Society of Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN). J. Pediatr. Gastroenterol. Nutr. 2017, 64, 319–334. [Google Scholar] [CrossRef]
- Baethge, C.; Goldbeck-Wood, S.; Mertens, S. SANRA—A scale for the quality assessment of narrative review articles. Res. Integr. Peer Rev. 2019, 4, 5. [Google Scholar] [CrossRef]
- Malecki, P.; Mania, A.; Mazur-Melewska, K.; Sluzewski, W.; Figlerowicz, M. A Decline in Aminotransferase Activity Due to Lifestyle Modification in Children with NAFLD. J. Pediatr. Res. 2021, 8, 41–48. [Google Scholar] [CrossRef]
- Grønbæk, H.; Lange, A.; Birkebæk, N.H.; Holland-Fischer, P.; Solvig, J.; Hørlyck, A.; Kristensen, K.; Rittig, S.; Vilstrup, H. Effect of a 10-week weight loss camp on fatty liver disease and insulin sensitivity in obese Danish children. J. Pediatr. Gastroenterol. Nutr. 2012, 54, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Utz-Melere, M.; Targa-Ferreira, C.; Lessa-Horta, B.; Epifanio, M.; Mouzaki, M.; Mattos, A.A. Non-Alcoholic Fatty Liver Disease in Children and Adolescents: Lifestyle Change—A Systematic Review and Meta-Analysis. Ann. Hepatol. 2018, 17, 345–354. [Google Scholar] [CrossRef] [PubMed]
- Chan, D.F.; Nelson, E.A.; Li, A.M.; Woo, J.; Sea, M.M.; Chan, R.S.; Chu, W.C.; Chan, M.; So, H.K. Lifestyle intervention in obese Chinese adolescents with non-alcoholic fatty liver disease: A randomised controlled study. Hong Kong Med. J. 2018, 24 (Suppl. S4), 12–15. [Google Scholar] [PubMed]
- De Piano, A.; de Mello, M.T.; Sanches Pde, L.; da Silva, P.L.; Campos, R.M.; Carnier, J.; Corgosinho, F.; Foschini, D.; Masquio, D.L.; Tock, L.; et al. Long-term effects of aerobic plus resistance training on the adipokines and neuropeptides in nonalcoholic fatty liver disease obese adolescents. Eur. J. Gastroenterol. Hepatol. 2012, 24, 1313–1324. [Google Scholar] [CrossRef] [PubMed]
- De Lira, C.T.; Dos Santos, M.A.; Gomes, P.P.; Fidelix, Y.L.; Dos Santos, A.C.; Tenório, T.R.; Lofrano-Prado, M.C.; do Prado, W.L. Aerobic training performed at ventilatory threshold improves liver enzymes and lipid profile related to non-alcoholic fatty liver disease in adolescents with obesity. Nutr. Health 2017, 23, 281–288. [Google Scholar] [CrossRef]
- Iraji, H.; Minasian, V.; Kelishadi, R. Changes in Liver Enzymes and Metabolic Profile in Adolescents with Fatty Liver following Exercise Interventions. Pediatr. Gastroenterol. Hepatol. Nutr. 2021, 24, 54–64. [Google Scholar] [CrossRef]
- Kang, D.W.; Park, J.H.; Lee, M.K.; Kim, Y.; Kong, I.D.; Chung, C.H.; Lee, Y.H.; Jeon, J.Y. Effect of a short-term physical activity intervention on liver fat content in obese children. Appl. Physiol. Nutr. Metab. 2018, 43, 553–557. [Google Scholar] [CrossRef]
- Nishida, C.; Martinez Nocito, F. FAO/WHO scientific update on carbohydrates in human nutrition: Introduction. Eur. J. Clin. Nutr. 2007, 61 (Suppl. S1), S1–S4. [Google Scholar] [CrossRef]
- WHO. Guideline: Sugars Intake for Adults and Children; WHO: Geneva, Switzerland, 2015. [Google Scholar]
- Cohen, C.C.; Li, K.W.; Alazraki, A.L.; Beysen, C.; Carrier, C.A.; Cleeton, R.L.; Dandan, M.; Figueroa, J.; Knight-Scott, J.; Knott, C.J.; et al. Dietary sugar restriction reduces hepatic de novo lipogenesis in adolescent boys with fatty liver disease. J. Clin. Investig. 2021, 131, e150996. [Google Scholar] [CrossRef]
- Sullivan, J.S.; Le, M.T.; Pan, Z.; Rivard, C.; Love-Osborne, K.; Robbins, K.; Johnson, R.J.; Sokol, R.J.; Sundaram, S.S. Oral fructose absorption in obese children with non-alcoholic fatty liver disease. Pediatr. Obes. 2015, 10, 188–195. [Google Scholar] [CrossRef]
- Hamza, R.T.; Ahmed, A.Y.; Rezk, D.G.; Hamed, A.I. Dietary fructose intake in obese children and adolescents: Relation to procollagen type III N-terminal peptide (P3NP) and non-alcoholic fatty liver disease. J. Pediatr. Endocrinol. Metab. 2016, 29, 1345–1352. [Google Scholar] [CrossRef] [PubMed]
- Yurtdaş, G.; Akbulut, G.; Baran, M.; Yılmaz, C. The effects of Mediterranean diet on hepatic steatosis, oxidative stress, and inflammation in adolescents with non-alcoholic fatty liver disease: A randomized controlled trial. Pediatr. Obes. 2022, 17, e12872. [Google Scholar] [CrossRef] [PubMed]
- Akbulut, U.E.; Isik, I.A.; Atalay, A.; Eraslan, A.; Durmus, E.; Turkmen, S.; Yurttas, A.S. The effect of a Mediterranean diet vs. a low-fat diet on non-alcoholic fatty liver disease in children: A randomized trial. Int. J. Food Sci. Nutr. 2022, 73, 357–366. [Google Scholar] [CrossRef]
- Nutrition Division. Fats and Fatty Acids in Human Nutrition. Expert Consultation. Ginebra 2010. Available online: https://www.fao.org/publications/card/es/c/94a18d21-5d48-5893-bb02-ec5755354845/ (accessed on 1 July 2023).
- Clark, P.; Mendoza-Gutiérrez, C.F.; Montiel-Ojeda, D.; Denova-Gutiérrez, E.; López-González, D.; Moreno-Altamirano, L.; Reyes, A. A Healthy Diet Is Not More Expensive than Less Healthy Options: Cost-Analysis of Different Dietary Patterns in Mexican Children and Adolescents. Nutrients 2021, 13, 3871. [Google Scholar] [CrossRef]
- La Fauci, V.; Alessi, V.; Assefa, D.Z.; Giudice, D.L.; Calimeri, S.; Ceccio, C.; Antonuccio, G.M.; Genovese, C.; Squeri, R. Mediterranean diet: Knowledge and adherence in Italian young people. Clin. Ter. 2020, 171, e437–e443. [Google Scholar] [PubMed]
- Martini, D.; Bes-Restrollo, M. Is Mediterranean diet still a common dietary pattern in the Mediterranean area? Int. J. Food Sci. Nutr. 2020, 71, 395–396. [Google Scholar] [CrossRef]
- Liberali, R.; Kupek, E.; Assis, M.A.A. Dietary Patterns and Childhood Obesity Risk: A Systematic Review. Child. Obes. 2020, 16, 70–85. [Google Scholar] [CrossRef] [PubMed]
- Cakir, M.; Akbulut, U.E.; Okten, A. Association between Adherence to the Mediterranean Diet and Presence of Nonalcoholic Fatty Liver Disease in Children. Child. Obes. 2016, 12, 279–285. [Google Scholar] [CrossRef]
- Della Corte, C.; Mosca, A.; Vania, A.; Alterio, A.; Iasevoli, S.; Nobili, V. Good adherence to the Mediterranean diet reduces the risk for NASH and diabetes in pediatric patients with obesity: The results of an Italian Study. Nutrition 2017, 39–40, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Kim, R.J.; Lopez, R.; Snair, M.; Tang, A. Mediterranean diet adherence and metabolic syndrome in US adolescents. Int. J. Food Sci. Nutr. 2021, 72, 537–547. [Google Scholar] [CrossRef]
- Iaccarino Idelson, P.; Scalfi, L.; Valerio, G. Adherence to the Mediterranean Diet in children and adolescents: A systematic review. Nutr. Metab. Cardiovasc. Dis. 2017, 27, 283–299. [Google Scholar] [CrossRef] [PubMed]
- Zhen, S.; Ma, Y.; Zhao, Z.; Yang, X.; Wen, D. Dietary pattern is associated with obesity in Chinese children and adolescents: Data from China Health and Nutrition Survey (CHNS). Nutr. J. 2018, 17, 68. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Peng, Y.; Chen, S.; Sun, Q. An observational study on the association between major dietary patterns and non-alcoholic fatty liver disease in Chinese adolescents. Medicine 2018, 97, e0576. [Google Scholar] [CrossRef] [PubMed]
- Spahis, S.; Alvarez, F.; Dubois, J.; Ahmed, N.; Peretti, N.; Levy, E. Plasma fatty acid composition in French-Canadian children with non-alcoholic fatty liver disease: Effect of n-3 PUFA supplementation. Prostaglandins Leukot. Essent. Fatty Acids 2015, 99, 25–34. [Google Scholar] [CrossRef] [PubMed]
- Silva Figueiredo, P.; Carla Inada, A.; Marcelino, G.; Maiara Lopes Cardozo, C.; de Cássia Freitas, K.; de Cássia Avellaneda Guimarães, R.; Pereira de Castro, A.; Aragão do Nascimento, V.; Aiko Hiane, P. Fatty Acids Consumption: The Role Metabolic Aspects Involved in Obesity and Its Associated Disorders. Nutrients 2017, 9, 1158. [Google Scholar] [CrossRef]
- Janczyk, W.; Lebensztejn, D.; Wierzbicka-Rucińska, A.; Mazur, A.; Neuhoff-Murawska, J.; Matusik, P.; Socha, P. Omega-3 Fatty acids therapy in children with nonalcoholic Fatty liver disease: A randomized controlled trial. J. Pediatr. 2015, 166, 1358–1363.e3. [Google Scholar] [CrossRef] [PubMed]
- Nobili, V.; Bedogni, G.; Alisi, A.; Pietrobattista, A.; Risé, P.; Galli, C.; Agostoni, C. Docosahexaenoic acid supplementation decreases liver fat content in children with non-alcoholic fatty liver disease: Double-blind randomised controlled clinical trial. Arch. Dis. Child. 2011, 96, 350–353. [Google Scholar] [CrossRef]
- Zöhrer, E.; Alisi, A.; Jahnel, J.; Mosca, A.; Della Corte, C.; Crudele, A.; Fauler, G.; Nobili, V. Efficacy of docosahexaenoic acid-choline-vitamin E in paediatric NASH: A randomized controlled clinical trial. Appl. Physiol. Nutr. Metab. 2017, 42, 948–954. [Google Scholar] [CrossRef]
- Della Corte, C.; Carpino, G.; De Vito, R.; De Stefanis, C.; Alisi, A.; Cianfarani, S.; Overi, D.; Mosca, A.; Stronati, L.; Cucchiara, S.; et al. Docosahexanoic Acid Plus Vitamin D Treatment Improves Features of NAFLD in Children with Serum Vitamin D Deficiency: Results from a Single Centre Trial. PLoS ONE 2016, 11, e0168216. [Google Scholar] [CrossRef] [PubMed]
- Jin, R.; Banton, S.; Tran, V.T.; Konomi, J.V.; Li, S.; Jones, D.P.; Vos, M.B. Amino Acid Metabolism is Altered in Adolescents with Nonalcoholic Fatty Liver Disease—An Untargeted, High Resolution Metabolomics Study. J. Pediatr. 2016, 172, 14–19.e5. [Google Scholar] [CrossRef] [PubMed]
- Lischka, J.; Schanzer, A.; Hojreh, A.; Ba Ssalamah, A.; Item, C.B.; de Gier, C.; Walleczek, N.K.; Metz, T.F.; Jakober, I.; Greber-Platzer, S.; et al. A branched-chain amino acid-based metabolic score can predict liver fat in children and adolescents with severe obesity. Pediatr. Obes. 2021, 16, e12739. [Google Scholar] [CrossRef] [PubMed]
- Schwimmer, J.B.; Lavine, J.E.; Wilson, L.A.; Neuschwander-Tetri, B.A.; Xanthakos, S.A.; Kohli, R.; Barlow, S.E.; Vos, M.B.; Karpen, S.J.; Molleston, J.P.; et al. In Children with Nonalcoholic Fatty Liver Disease, Cysteamine Bitartrate Delayed Release Improves Liver Enzymes but Does Not Reduce Disease Activity Scores. Gastroenterology 2016, 151, 1141–1154.e9. [Google Scholar] [CrossRef] [PubMed]
- Saneian, H.; Khalilian, L.; Heidari-Beni, M.; Khademian, M.; Famouri, F.; Nasri, P.; Hassanzadeh, A.; Kelishadi, R. Effect of l-carnitine supplementation on children and adolescents with nonalcoholic fatty liver disease (NAFLD): A randomized, triple-blind, placebo-controlled clinical trial. J. Pediatr. Endocrinol. Metab. 2021, 34, 897–904. [Google Scholar] [CrossRef] [PubMed]
- Phung, N.; Pera, N.; Farrell, G.; Leclercq, I.; Hou, J.Y.; George, J. Pro-oxidant-mediated hepatic fibrosis and effects of antioxidant intervention in murine dietary steatohepatitis. Int. J. Mol. Med. 2009, 24, 171–180. [Google Scholar] [CrossRef]
- Abramovitch, S.; Dahan-Bachar, L.; Sharvit, E.; Weisman, Y.; Ben Tov, A.; Brazowski, E.; Reif, S. Vitamin D inhibits proliferation and profibrotic marker expression in hepatic stellate cells and decreases thioacetamide-induced liver fibrosis in rats. Gut 2011, 60, 1728–1737. [Google Scholar] [CrossRef]
- Nobili, V.; Manco, M.; Devito, R.; Ciampalini, P.; Piemonte, F.; Marcellini, M. Effect of vitamin E on aminotransferase levels and insulin resistance in children with non-alcoholic fatty liver disease. Aliment. Pharmacol. Ther. 2006, 24, 1553–1561. [Google Scholar] [CrossRef] [PubMed]
- Lavine, J.E.; Schwimmer, J.B.; Van Natta, M.L.; Molleston, J.P.; Murray, K.F.; Rosenthal, P.; Abrams, S.H.; Scheimann, A.O.; Sanyal, A.J.; Chalasani, N.; et al. Effect of vitamin E or metformin for treatment of nonalcoholic fatty liver disease in children and adolescents: The TONIC randomized controlled trial. JAMA 2011, 305, 1659–1668. [Google Scholar] [CrossRef]
- Nobili, V.; Alisi, A.; Mosca, A.; Crudele, A.; Zaffina, S.; Denaro, M.; Smeriglio, A.; Trombetta, D. The Antioxidant Effects of Hydroxytyrosol and Vitamin E on Pediatric Nonalcoholic Fatty Liver Disease, in a Clinical Trial: A New Treatment? Antioxid. Redox Signal. 2019, 31, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Mosca, A.; Crudele, A.; Smeriglio, A.; Braghini, M.R.; Panera, N.; Comparcola, D.; Alterio, A.; Sartorelli, M.R.; Tozzi, G.; Raponi, M.; et al. Antioxidant activity of Hydroxytyrosol and Vitamin E reduces systemic inflammation in children with paediatric NAFLD. Dig. Liver Dis. 2021, 53, 1154–1158. [Google Scholar] [CrossRef]
- D’Adamo, E.; Marcovecchio, M.L.; Giannini, C.; de Giorgis, T.; Chiavaroli, V.; Chiarelli, F.; Mohn, A. Improved oxidative stress and cardio-metabolic status in obese prepubertal children with liver steatosis treated with lifestyle combined with Vitamin E. Free Radic. Res. 2013, 47, 146–153. [Google Scholar] [CrossRef] [PubMed]
- Torquato, P.; Giusepponi, D.; Alisi, A.; Galarini, R.; Bartolini, D.; Piroddi, M.; Goracci, L.; Di Veroli, A.; Cruciani, G.; Crudele, A.; et al. Nutritional and lipidomics biomarkers of docosahexaenoic acid-based multivitamin therapy in pediatric NASH. Sci. Rep. 2019, 9, 2045. [Google Scholar] [CrossRef] [PubMed]
- Valenzuela, R.; Videla, L.A. Impact of the Co-Administration of N-3 Fatty Acids and Olive Oil Components in Preclinical Nonalcoholic Fatty Liver Disease Models: A Mechanistic View. Nutrients 2020, 12, 499. [Google Scholar] [CrossRef]
- Wang, X.; Li, W.; Zhang, Y.; Yang, Y.; Qin, G. Association between vitamin D and non-alcoholic fatty liver disease/non-alcoholic steatohepatitis: Results from a meta-analysis. Int. J. Clin. Exp. Med. 2015, 8, 17221–17234. [Google Scholar] [PubMed]
- El Amrousy, D.; Abdelhai, D.; Shawky, D. Vitamin D and nonalcoholic fatty liver disease in children: A randomized controlled clinical trial. Eur. J. Pediatr. 2022, 181, 579–586. [Google Scholar] [CrossRef]
- Namakin, K.; Hosseini, M.; Zardast, M.; Mohammadifard, M. Vitamin D Effect on Ultrasonography and Laboratory Indices and Biochemical Indicators in the Blood: An Interventional Study on 12 to 18-Year-Old Children with Fatty Liver. Pediatr. Gastroenterol. Hepatol. Nutr. 2021, 24, 187–196. [Google Scholar] [CrossRef] [PubMed]
- Tokuhara, D. Role of the Gut Microbiota in Regulating Non-alcoholic Fatty Liver Disease in Children and Adolescents. Front. Nutr. 2021, 8, 700058. [Google Scholar] [CrossRef]
- Yang, Y.J.; Ni, Y.H. Gut microbiota and pediatric obesity/non-alcoholic fatty liver disease. J. Formos. Med. Assoc. 2019, 118 (Suppl. S1), S55–S61. [Google Scholar] [CrossRef] [PubMed]
- Vajro, P.; Mandato, C.; Licenziati, M.R.; Franzese, A.; Vitale, D.F.; Lenta, S.; Caropreso, M.; Vallone, G.; Meli, R. Effects of Lactobacillus rhamnosus strain GG in pediatric obesity-related liver disease. J. Pediatr. Gastroenterol. Nutr. 2011, 52, 740–743. [Google Scholar] [CrossRef]
- De Angelis, M.; Rizzello, C.G.; Fasano, A.; Clemente, M.G.; De Simone, C.; Silano, M.; De Vincenzi, M.; Losito, I.; Gobbetti, M. VSL#3 probiotic preparation has the capacity to hydrolyze gliadin polypeptides responsible for Celiac Sprue. Biochim. Biophys. Acta 2006, 1762, 80–93. [Google Scholar] [CrossRef]
- Alisi, A.; Bedogni, G.; Baviera, G.; Giorgio, V.; Porro, E.; Paris, C.; Giammaria, P.; Reali, L.; Anania, F.; Nobili, V. Randomised clinical trial: The beneficial effects of VSL#3 in obese children with non-alcoholic steatohepatitis. Aliment. Pharmacol. Ther. 2014, 39, 1276–1285. [Google Scholar] [CrossRef]
- Famouri, F.; Shariat, Z.; Hashemipour, M.; Keikha, M.; Kelishadi, R. Effects of Probiotics on Nonalcoholic Fatty Liver Disease in Obese Children and Adolescents. J. Pediatr. Gastroenterol. Nutr. 2017, 64, 413–417. [Google Scholar] [CrossRef] [PubMed]
- Thushara, R.; Dulani, S.; Nimali Seneviratne, S.; De Silva, A.P.; Fernando, J.; De Silva, H.J.; Jayasekera Wickramasinghe, V.P. Effects of probiotics combined with dietary and lifestyle modification on clinical, biochemical, and radiological parameters in obese children with nonalcoholic fatty liver disease/nonalcoholic steatohepatitis: A randomized clinical trial. Clin. Exp. Pediatr. 2022, 65, 304–311. [Google Scholar] [CrossRef]
- Ishaque, S.M.; Khosruzzaman, S.M.; Ahmed, D.S.; Sah, M.P. A randomized placebo-controlled clinical trial of a multi-strain probiotic formulation (Bio-Kult®) in the management of diarrhea-predominant irritable bowel syndrome. BMC Gastroenterol. 2018, 18, 71. [Google Scholar] [CrossRef] [PubMed]

| Intervention | Age Group | Duration | n | Results | References |
|---|---|---|---|---|---|
| Mediterranean diet and moderate-intensity aerobic physical exercise of at least 60 min, 5 days a week. | In children between 3 and 16 years. | 5 days a week. | 49 | ↓ ALT (with BMI reduction: −26.7 U/L). | [20] |
| Hypocaloric diet (1550 kcal) along with physical exercise for 1 h a day. | In adolescents between 11 and 13 years. | For 10 weeks. | 117 | ↓ 7.1 ± 2.7 kg body weight, an increase in insulin sensitivity, and an improvement in NAFLD parameters (−30% liver echogenicity, −8% had plump liver sign, and −4% changed liver texture by ultrasound). | [21] |
| Advice on diet restriction and exercise once a week. | In adolescents between 14 and 18 years. | Four months. | 52 | ↓ body fat (−6.0 ± 4.7%) and hepatic lipid content (−32%, by MRI). | [23] |
| Intervention | Age Group | Duration | n | Results | References |
|---|---|---|---|---|---|
| Aerobic exercise and aerobic exercise plus resistance exercises for 3 h a week, for one year. | In adolescents between 15 and 19 years. | One year. | 68 | Greater efficiency in the combination of aerobic exercise plus resistance exercises, achieving a ↓ value of insulin, insulin resistance index (HOMA-IR), and ↓ ALT in aerobic training (–21.84 ± 23.76 U/L) and with aerobic plus resistance training (–5.78 ± 9.73 U/L). | [24] |
| Low or high-intensity training for 3 h a week for 12 weeks. | In adolescents between 14 and 16 years. | 12 weeks. | 107 | Improvement of the biomarkers of both groups. ↓ ALT, AST (High-Intensity Training: −3.08 and −2.4 U/L, respectively; Low-Intensity Training: −0.9 and −0.9 U/L, respectively) and ↑ 15% HDL of both groups. | [25] |
| School exercise and high-intensity interval training for 3 days per week for 8 weeks. | In adolescents between 10 and 15 years. | 8 weeks. | 34 | Significant ↓ 1% in body fat, IR, TG, total cholesterol, ALT (−4.4 ± 0.3 U/L), and AST (−3 ± 2 U/L) in both types of training. | [26] |
| Effect of intense physical activity in a short period of 7 days (3 h per day). | In adolescents between 11 and 13 years. | 7 days. | 57 | Acute weight ↓ (2.53 ± 0.85 kg) and ↓ liver fat content (−1.78 ± 5.53, by abdominal computed tomography) independent of IR. | [27] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Farías, C.; Cisternas, C.; Gana, J.C.; Alberti, G.; Echeverría, F.; Videla, L.A.; Mercado, L.; Muñoz, Y.; Valenzuela, R. Dietary and Nutritional Interventions in Nonalcoholic Fatty Liver Disease in Pediatrics. Nutrients 2023, 15, 4829. https://doi.org/10.3390/nu15224829
Farías C, Cisternas C, Gana JC, Alberti G, Echeverría F, Videla LA, Mercado L, Muñoz Y, Valenzuela R. Dietary and Nutritional Interventions in Nonalcoholic Fatty Liver Disease in Pediatrics. Nutrients. 2023; 15(22):4829. https://doi.org/10.3390/nu15224829
Chicago/Turabian StyleFarías, Camila, Camila Cisternas, Juan Cristobal Gana, Gigliola Alberti, Francisca Echeverría, Luis A. Videla, Lorena Mercado, Yasna Muñoz, and Rodrigo Valenzuela. 2023. "Dietary and Nutritional Interventions in Nonalcoholic Fatty Liver Disease in Pediatrics" Nutrients 15, no. 22: 4829. https://doi.org/10.3390/nu15224829
APA StyleFarías, C., Cisternas, C., Gana, J. C., Alberti, G., Echeverría, F., Videla, L. A., Mercado, L., Muñoz, Y., & Valenzuela, R. (2023). Dietary and Nutritional Interventions in Nonalcoholic Fatty Liver Disease in Pediatrics. Nutrients, 15(22), 4829. https://doi.org/10.3390/nu15224829









