Nutritional Status and Feeding Behavior of Children with Autism Spectrum Disorder in the Middle East and North Africa Region: A Systematic Review
Abstract
:1. Introduction
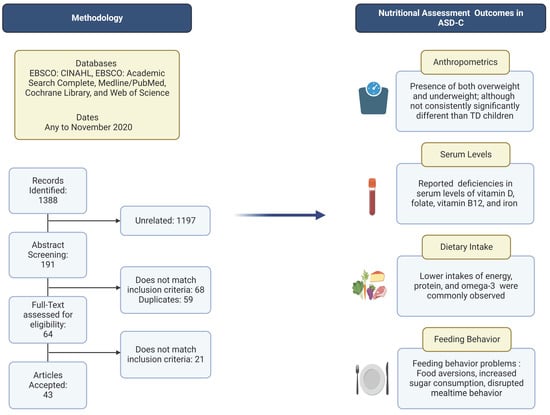
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Search Strategy
2.3. Study Selection
2.4. Data Collection
2.5. Quality Appraisal
3. Results
3.1. Study Description
3.2. Risk of Bias Assessment
3.3. Study Findings
3.3.1. Anthropometric Data
3.3.2. Serum-Level Data
3.3.3. Nutrient Intake Data
3.3.4. Feeding Behavior Data
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- American Psychiatric Association. What Is Autism Spectrum Disorder? Available online: https://www.psychiatry.org/patients-families/autism/what-is-autism-spectrum-disorder (accessed on 8 June 2021).
- Al-Mamri, W.; Idris, A.B.; Dakak, S.; Al-Shekaili, M.; Al-Harthi, Z.; Alnaamani, A.M.; Alhinai, F.I.; Jalees, S.; Al Hatmi, M.; El-Naggari, M.A.; et al. Revisiting the Prevalence of Autism Spectrum Disorder among Omani Children. Sultan Qaboos Univ. Med. J. 2019, 19, e305–e309. [Google Scholar] [CrossRef] [PubMed]
- Salhia, H.O.; Al-Nasser, L.A.; Taher, L.S.; Al-Khathaami, A.M.; El-Metwally, A.A. Systemic Review of the Epidemiology of Autism in Arab Gulf Countries. Neurosciences 2014, 19, 291–296. [Google Scholar] [PubMed]
- Virolainen, S.; Hussien, W.; Dalibalta, S. Autism Spectrum Disorder in the United Arab Emirates: Potential Environmental Links. Rev. Environ. Health 2020, 35, 359–369. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.S.; Leventhal, B.L. Genetic Epidemiology and Insights into Interactive Genetic and Environmental Effects in Autism Spectrum Disorders. Biol. Psychiatry 2015, 77, 66–74. [Google Scholar] [CrossRef] [Green Version]
- Hisle-Gorman, E.; Susi, A.; Stokes, T.; Gorman, G.; Erdie-Lalena, C.; Nylund, C.M. Prenatal, Perinatal, and Neonatal Risk Factors of Autism Spectrum Disorder. Pediatr. Res. 2018, 84, 190–198. [Google Scholar] [CrossRef] [Green Version]
- Kim, J.Y.; Son, M.J.; Son, C.Y.; Radua, J.; Eisenhut, M.; Gressier, F.; Koyanagi, A.; Carvalho, A.F.; Stubbs, B.; Solmi, M.; et al. Environmental Risk Factors and Biomarkers for Autism Spectrum Disorder: An Umbrella Review of the Evidence. Lancet Psychiatry 2019, 6, 590–600. [Google Scholar] [CrossRef] [Green Version]
- Modabbernia, A.; Velthorst, E.; Reichenberg, A. Environmental Risk Factors for Autism: An Evidence-Based Review of Systematic Reviews and Meta-Analyses. Mol. Autism 2017, 8, 13. [Google Scholar] [CrossRef] [Green Version]
- Al-Farsi, Y.M.; Al-Sharbati, M.M.; Waly, M.I.; Al-Farsi, O.A.; Al Shafaee, M.A.; Deth, R.C. Malnutrition among Preschool-Aged Autistic Children in Oman. Res. Autism Spectr. Disord. 2011, 5, 1549–1552. [Google Scholar] [CrossRef]
- Bölte, S.; Özkara, N.; Poustka, F. Autism Spectrum Disorders and Low Body Weight: Is There Really a Systematic Association? Int. J. Eat. Disord. 2002, 31, 349–351. [Google Scholar] [CrossRef]
- Curtin, C.; Jojic, M.; Bandini, L.G. Obesity in Children with Autism Spectrum Disorders. Harv. Rev. Psychiatry 2014, 22, 93–103. [Google Scholar] [CrossRef]
- Dhaliwal, K.K.; Orsso, C.E.; Richard, C.; Haqq, A.M.; Zwaigenbaum, L. Risk Factors for Unhealthy Weight Gain and Obesity among Children with Autism Spectrum Disorder. Int. J. Mol. Sci. 2019, 20, 3285. [Google Scholar] [CrossRef] [Green Version]
- Hill, A.P.; Zuckerman, K.E.; Fombonne, E. Obesity and Autism. Pediatrics 2015, 136, 1051–1061. [Google Scholar] [CrossRef] [Green Version]
- Schreck, K.A.; Williams, K.; Smith, A.F. A Comparison of Eating Behaviors between Children with and without Autism. Autism Dev. Disord 2004, 34, 433–438. [Google Scholar] [CrossRef]
- Cannell, J.J. Vitamin D and Autism, What’s New? Rev. Endocr. Metab. Disord. 2017, 18, 183–193. [Google Scholar] [CrossRef]
- Castro, K.; Faccioli, L.S.; Baronio, D.; Gottfried, C.; Perry, I.S.; Riesgo, R. Feeding Behavior and Dietary Intake of Male Children and Adolescents with Autism Spectrum Disorder: A Case-Control Study. Int. J. Dev. Neurosci. 2016, 53, 68–74. [Google Scholar] [CrossRef]
- Malhi, P.; Venkatesh, L.; Bharti, B.; Singhi, P. Feeding Problems and Nutrient Intake in Children with and without Autism: A Comparative Study. Indian J. Pediatr. 2017, 84, 283–288. [Google Scholar] [CrossRef]
- Xia, W.; Zhou, Y.; Sun, C.; Wang, J.; Wu, L. A Preliminary Study on Nutritional Status and Intake in Chinese Children with Autism. Eur. J. Pediatr. 2010, 169, 1201–1206. [Google Scholar] [CrossRef]
- Guo, M.; Zhu, J.; Yang, T.; Lai, X.; Lei, Y.; Chen, J.; Li, T. Vitamin A and Vitamin D Deficiencies Exacerbate Symptoms in Children with Autism Spectrum Disorders. Nutr. Neurosci. 2019, 22, 637–647. [Google Scholar] [CrossRef]
- Saad, K.; Abdel-Rahman, A.A.; Elserogy, Y.M.; Al-Atram, A.A.; Cannell, J.J.; Bjørklund, G.; Abdel-Reheim, M.K.; Othman, H.A.K.; El-Houfey, A.A.; Abd El-Aziz, N.H.R.; et al. Vitamin D Status in Autism Spectrum Disorders and the Efficacy of Vitamin D Supplementation in Autistic Children. Nutr. Neurosci. 2016, 19, 346–351. [Google Scholar] [CrossRef]
- Lee, B.K.; Eyles, D.W.; Magnusson, C.; Newschaffer, C.J.; McGrath, J.J.; Kvaskoff, D.; Ko, P.; Dalman, C.; Karlsson, H.; Gardner, R.M. Developmental Vitamin D and Autism Spectrum Disorders: Findings from the Stockholm Youth Cohort. Mol. Psychiatry 2019. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, T.P. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Academy of Nutrition and Dietetics. Evidence Analysis Manual: Steps in the Academy Evidence Analysis Process; Academy of Nutrition and Dietetics: Chicago, IL, USA, 2016; pp. 8–91. [Google Scholar]
- Aghaeinejad, M.; Djafarian, K.; Mahmoudi, M.; Daneshi, M. Comparison of Energy and Macronutrients Intake between Children with Autism and Healthy Children. Int. Res. J. Appl. Basic Sci. 2013, 5, 667–670. [Google Scholar]
- Al-Ali, S.F.; Russo, D.S.; Alkaissi, D.A. Association between Autism Spectrum Disorder and Iron Deficiency in Children Diagnosed Autism Spectrum Disorder in the Northern West Bank. J. Health Med. Nur. 2015, 10. [Google Scholar]
- Al-Bazzaz, A.; A-Dahir, K.; Almashhadani, A.; Al-Ani, I. Estimation of Fasting Serum Levels of Glucose, Zinc, Copper, Zinc /Copper Ratio and Their Relation to the Measured Lipid Profile in Autistic Patients and Non-Autistic Controls in Jordan. Biomed. Pharmacol. J. 2020, 13, 481–488. [Google Scholar] [CrossRef]
- Al-Farsi, Y.M.; Waly, M.I.; Deth, R.C.; Al-Sharbati, M.M.; Al-Shafaee, M.; Al-Farsi, O.; Al-Khaduri, M.M.; Gupta, I.; Ali, A.; Al-Khalili, M.; et al. Low Folate and Vitamin B12 Nourishment Is Common in Omani Children with Newly Diagnosed Autism. Nutrition 2013, 29, 537–541. [Google Scholar] [CrossRef]
- Al-Farsi, Y.M.; Waly, M.I.; Deth, R.C.; Al-Sharbati, M.M.; Al-Shafaee, M.; Al-Farsi, O.; Al-Khaduri, M.M.; Al-Adawi, S.; Hodgson, N.W.; Gupta, I.; et al. Impact of Nutrition on Serum Levels of Docosahexaenoic Acid among Omani Children with Autism. Nutrition 2013, 29, 1142–1146. [Google Scholar] [CrossRef]
- Ali, A.; Waly, M.I.; Al-Farsi, Y.M.; Essa, M.M.; Al-Sharbati, M.M.; Deth, R.C. Hyperhomocysteinemia among Omani Autistic Children: A Case-Control Study. Acta Biochim. Pol. 2011, 58. [Google Scholar] [CrossRef]
- Alkazemi, D.; Rahman, A.; AlSaad, S.; Kubow, S. Parental Perceptions and Concerns of Weight Status in Children with Autism Spectrum Disorders in Kuwait. Res. Autism Spectr. Disord. 2016, 22, 1–9. [Google Scholar] [CrossRef]
- Al-Kindi, N.M.; Al-Farsi, Y.M.; Waly, M.I.; A-Shafaee, M.S.; Bakheit, C.S. Dietary Intake and Food Preferences of Autistic Children Versus Children with Typical Development: A Comparative Cross-Sectional Study. EC Nutrition 2016, 6, 72–85. [Google Scholar]
- Al-Kindi, N.M.; Al-Farsi, Y.M.; Al-Bulushi, B.; Ali, A.; Rizvi, S.G.A.; Essa, M.M. Food Selection and Preferences of Omani Autistic Children. Adv Neurobiol. 2020, 24, 505–523. [Google Scholar] [CrossRef]
- Alzghoul, L.; AL-Eitan, L.N.; Aladawi, M.; Odeh, M.; Abu Hantash, O. The Association Between Serum Vitamin D3 Levels and Autism Among Jordanian Boys. J. Autism Dev. Disord. 2020, 50, 3149–3154. [Google Scholar] [CrossRef]
- Arastoo, A.A.; Khojastehkia, H.; Rahimi, Z.; Khafaie, M.A.; Hosseini, S.A.; Mansouri, M.T.; Yosefyshad, S.; Abshirini, M.; Karimimalekabadi, N.; Cheraghi, M. Evaluation of Serum 25-Hydroxy Vitamin D Levels in Children with Autism Spectrum Disorder. Ital. J. Pediatr. 2018, 44, 150. [Google Scholar] [CrossRef] [Green Version]
- Ashour, N.A.; Ashour, A.A.; Basha, S. Association between Body Mass Index and Dental Caries among Special Care Female Children in Makkah City. Ann. Saudi Med. 2018, 38, 28–35. [Google Scholar] [CrossRef]
- Attlee, A.; Kassem, H.; Hashim, M.; Obaid, R.S. Physical Status and Feeding Behavior of Children with Autism. Indian J. Pediatr. 2015, 82, 682–687. [Google Scholar] [CrossRef]
- Bener, A.; Khattab, A.O.; Al-Dabbagh, M.M. Is High Prevalence of Vitamin D Deficiency Evidence for Autism Disorder?: In a Highly Endogamous Population. J. Pediatr. Neurosci. 2014, 9, 227–233. [Google Scholar] [CrossRef] [Green Version]
- Bener, A.; Khattab, A.; Bhugra, D.; Hoffmann, G. Iron and Vitamin D Levels among Autism Spectrum Disorders Children. Ann. Afr. Med. 2017, 16, 186. [Google Scholar] [CrossRef]
- Cherif, L.; Boudabous, J.; Khemekhem, K.; Mkawer, S.; Ayadi, H.; Moalla, Y. Feeding Problems in Children with Autism Spectrum Disorders. J. Fam. Med. 2018, 1, 30–39. [Google Scholar] [CrossRef] [Green Version]
- Desoky, T.; Hassan, M.H.; Fayed, H.; Sakhr, H.M. Biochemical Assessments of Thyroid Profile, Serum 25-Hydroxycholecalciferol and Cluster of Differentiation 5 Expression Levels among Children with Autism. NDT 2017, 13, 2397–2403. [Google Scholar] [CrossRef] [Green Version]
- El-Ansary, A.; Al-Daihan, S.; Al-Dbass, A.; Al-Ayadhi, L. Measurement of Selected Ions Related to Oxidative Stress and Energy Metabolism in Saudi Autistic Children. Clin. Biochem. 2010, 43, 63–70. [Google Scholar] [CrossRef]
- El-Ansary, A.K.; Ben Bacha, A.G.; Al-Ayahdi, L.Y. Impaired Plasma Phospholipids and Relative Amounts of Essential Polyunsaturated Fatty Acids in Autistic Patients from Saudi Arabia. Lipids Health Dis. 2011, 10, 63. [Google Scholar] [CrossRef] [Green Version]
- El-Ansary, A.; Cannell, J.J.; Bjørklund, G.; Bhat, R.S.; Al Dbass, A.M.; Alfawaz, H.A.; Chirumbolo, S.; Al-Ayadhi, L. In the Search for Reliable Biomarkers for the Early Diagnosis of Autism Spectrum Disorder: The Role of Vitamin D. Metab. Brain Dis. 2018, 33, 917–931. [Google Scholar] [CrossRef] [PubMed]
- ElBaz, F.M.; Zaki, M.M.; Youssef, A.M.; ElDorry, G.F.; Elalfy, D.Y. Study of Plasma Amino Acid Levels in Children with Autism: An Egyptian Sample. Egypt. J. Med. Hum. Genet. 2014, 15, 181–186. [Google Scholar] [CrossRef] [Green Version]
- El-Khatib, A.A.; tekeya, M.E.; Tantawi, M.E.; Omar, T. Oral Health Status and Behaviours of Children with Autism Spectrum Disorder: A Case-Control Study. Int. J. Paediatr. Dent. 2014. [Google Scholar] [CrossRef]
- Fahmy, F.; Sabri, N.; El Hamamsy, M.; El Sawi, M.; Zaki, O. Vitamin D Intake and Sun Exposure in Autistic Children. Int. J. Pharm. Sci. Res. 2016, 7, 1043–1049. [Google Scholar]
- Ghodsi, R.; Kheirouri, S.; Nosrati, R. Carnosine Supplementation Does Not Affect Serum Concentrations of Advanced Glycation and Precursors of Lipoxidation End Products in Autism: A Randomized Controlled Clinical Trial. Ann. Clin. Biochem. 2019, 56, 148–154. [Google Scholar] [CrossRef]
- Hammouda, S.A.I.; Farghal, S.; Al-Harbi, G.; Abduallah, M.; Al-Rehaly, R.; Al-Johani, G. Assessment of Nutritional Risk Factors Predisposing to Autism among Saudi Children. Nat. Food 2018, 6. [Google Scholar] [CrossRef]
- Hashemzadeh, M.; Moharreri, F.; Soltanifar, A. Comparative Study of Vitamin D Levels in Children with Autism Spectrum Disorder and Normal Children: A Case-Control Study. J. Fundam. Ment. Health 2015, 6, 197–201. [Google Scholar]
- Hawari, I.; Eskandar, M.B.; Alzeer, S. The Role of Lead, Manganese, and Zinc in Autism Spectrum Disorders (ASDs) and Attention-Deficient Hyperactivity Disorder (ADHD): A Case-Control Study on Syrian Children Affected by the Syrian Crisis. Biol. Trace Elem. Res. 2020, 197, 107–114. [Google Scholar] [CrossRef]
- Javadfar, Z.; Abdollahzad, H.; Moludi, J.; Rezaeian, S.; Amirian, H.; Foroughi, A.A.; Nachvak, S.M.; Goharmehr, N.; Mostafai, R. Effects of Vitamin D Supplementation on Core Symptoms, Serum Serotonin, and Interleukin-6 in Children with Autism Spectrum Disorders: A Randomized Clinical Trial. Nutrition 2020, 79–80, 110986. [Google Scholar] [CrossRef]
- Meguid, N.A.; Atta, H.M.; Gouda, A.S.; Khalil, R.O. Role of Polyunsaturated Fatty Acids in the Management of Egyptian Children with Autism. Clin. Biochem. 2008, 41, 1044–1048. [Google Scholar] [CrossRef]
- Meguid, N.A.; Hashish, A.F.; Anwar, M.; Sidhom, G. Reduced Serum Levels of 25-Hydroxy and 1,25-Dihydroxy Vitamin D in Egyptian Children with Autism. J. Altern. Complement. Med. 2010, 16, 641–645. [Google Scholar] [CrossRef]
- Meguid, N.; Anwar, M.; Zaki, S.; Kandeel, W.; Ahmed, N.; Tewfik, I. Dietary Patterns of Children with Autism Spectrum Disorder: A Study Based in Egypt. Open Access Maced. J. Med. Sci. 2015, 3, 262–267. [Google Scholar] [CrossRef] [Green Version]
- Meguid, N.A.; Anwar, M.; Bjørklund, G.; Hashish, A.; Chirumbolo, S.; Hemimi, M.; Sultan, E. Dietary Adequacy of Egyptian Children with Autism Spectrum Disorder Compared to Healthy Developing Children. Metab. Brain Dis. 2017, 32, 607–615. [Google Scholar] [CrossRef]
- Meguid, N.A.; Bjørklund, G.; Gebril, O.H.; Doşa, M.D.; Anwar, M.; Elsaeid, A.; Gaber, A.; Chirumbolo, S. The Role of Zinc Supplementation on the Metallothionein System in Children with Autism Spectrum Disorder. Acta Neurol Belg. 2019, 119, 577–583. [Google Scholar] [CrossRef]
- Metwally, F.M.; Rashad, H.; Zeidan, H.M.; Kilany, A.; Abdol Raouf, E.R. Study of the Effect of Bisphenol A on Oxidative Stress in Children with Autism Spectrum Disorders. Ind. J. Clin. Biochem. 2018, 33, 196–201. [Google Scholar] [CrossRef]
- Mostafa, G.A.; AL-Ayadhi, L.Y. Reduced Serum Concentrations of 25-Hydroxy Vitamin D in Children with Autism: Relation to Autoimmunity. J. Neuroinflammation 2012, 9, 686. [Google Scholar] [CrossRef] [Green Version]
- Mostafa, G.A.; El-Khashab, H.Y.; AL-Ayadhi, L.Y. A Possible Association between Elevated Serum Levels of Brain-Specific Auto-Antibodies and Reduced Plasma Levels of Docosahexaenoic Acid in Autistic Children. J. Neuroimmunol. 2015, 280, 16–20. [Google Scholar] [CrossRef]
- Mostafa, G.A.; AL-Ayadhi, L.Y. Reduced Levels of Plasma Polyunsaturated Fatty Acids and Serum Carnitine in Autistic Children: Relation to Gastrointestinal Manifestations. Behav. Brain Funct. 2015, 11, 4. [Google Scholar] [CrossRef] [Green Version]
- Murshid, E.Z. Diet, Oral Hygiene Practices and Dental Health in Autistic Children in Riyadh, Saudi Arabia. Oral Health Dent. Manag. 2014, 13, 6. [Google Scholar]
- Salehi, H.; Aghanoori, M.R.; Shahmohammadlu, S.; Hooseini, B.; Mitchell, S.E.; Mahmudi, M.; Djafarian, K. Body Composition in Iranian Boys with Autism Spectrum Disorders. Paediatr. Croat. 2015, 59, 159–165. [Google Scholar] [CrossRef] [Green Version]
- Shaaban, S.Y.; El Gendy, Y.G.; Mehanna, N.S.; El-Senousy, W.M.; El-Feki, H.S.A.; Saad, K.; El-Asheer, O.M. The Role of Probiotics in Children with Autism Spectrum Disorder: A Prospective, Open-Label Study. Nutr. Neurosci. 2018, 21, 676–681. [Google Scholar] [CrossRef] [PubMed]
- Wtwt, E.T.; Farhood, H.F. Feeding Problems and Nutritional Assessment in Children with Autism. 2015. Available online: https://iraqjournals.com/article_102620_0.html (accessed on 8 June 2021).
- Esteban-Figuerola, P.; Canals, J.; Fernández-Cao, J.C.; Arija Val, V. Differences in Food Consumption and Nutritional Intake between Children with Autism Spectrum Disorders and Typically Developing Children: A Meta-Analysis. Autism 2019, 23, 1079–1095. [Google Scholar] [CrossRef] [PubMed]
- Kral, T.V.E.; Souders, M.C.; Tompkins, V.H.; Remiker, A.M.; Eriksen, W.T.; Pinto-Martin, J.A. Child Eating Behaviors and Caregiver Feeding Practices in Children with Autism Spectrum Disorders. Public Health Nurs. 2015, 32, 488–497. [Google Scholar] [CrossRef] [PubMed]
- Marí-Bauset, S.; Zazpe, I.; Marí-Sanchis, A.; Llopis-González, A.; Suárez-Varela, M.M. Anthropometric Measurements and Nutritional Assessment in Autism Spectrum Disorders: A Systematic Review. Res. Autism Spectr. Disord. 2015, 9, 130–143. [Google Scholar] [CrossRef]
- Li, Y.-J.; Xie, X.-N.; Lei, X.; Li, Y.-M.; Lei, X. Global Prevalence of Obesity, Overweight and Underweight in Children, Adolescents and Adults with Autism Spectrum Disorder, Attention-Deficit Hyperactivity Disorder: A Systematic Review and Meta-Analysis. Obes. Rev. 2020, 21, e13123. [Google Scholar] [CrossRef]
- Curtin, C.; Anderson, S.E.; Must, A.; Bandini, L. The Prevalence of Obesity in Children with Autism: A Secondary Data Analysis Using Nationally Representative Data from the National Survey of Children’s Health. BMC Pediatr. 2010, 10, 11. [Google Scholar] [CrossRef]
- de Vinck-Baroody, O.; Shui, A.; Macklin, E.A.; Hyman, S.L.; Leventhal, J.M.; Weitzman, C. Overweight and Obesity in a Sample of Children With Autism Spectrum Disorder. Acad. Pediatr. 2015, 15, 396–404. [Google Scholar] [CrossRef]
- Mills, J.L.; Hediger, M.L.; Molloy, C.A.; Chrousos, G.P.; Manning-Courtney, P.; Yu, K.F.; Brasington, M.; England, L.J. Elevated Levels of Growth-Related Hormones in Autism and Autism Spectrum Disorder. Clin. Endocrinol. 2007, 67, 230–237. [Google Scholar] [CrossRef]
- Must, A.; Phillips, S.M.; Curtin, C.; Anderson, S.E.; Maslin, M.; Lividini, K.; Bandini, L.G. Comparison of Sedentary Behaviors between Children with Autism Spectrum Disorders and Typically Developing Children. Autism 2014, 18, 376–384. [Google Scholar] [CrossRef] [Green Version]
- Goyal, R.K.; Shah, V.N.; Saboo, B.D.; Phatak, S.R.; Shah, N.N.; Gohel, M.C.; Raval, P.B.; Patel, S.S. Prevalence of Overweight and Obesity in Indian Adolescent School Going Children: Its Relationship with Socioeconomic Status and Associated Lifestyle Factors. J. Assoc. Physicians India 2010, 58, 151–158. [Google Scholar]
- Lamerz, A.; Kuepper-Nybelen, J.; Wehle, C.; Bruning, N.; Trost-Brinkhues, G.; Brenner, H.; Hebebrand, J.; Herpertz-Dahlmann, B. Social Class, Parental Education, and Obesity Prevalence in a Study of Six-Year-Old Children in Germany. Int. J. Obes. 2005, 29, 373–380. [Google Scholar] [CrossRef] [Green Version]
- Lee, A.; Cardel, M.; Donahoo, W.T. Social and Environmental Factors Influencing Obesity. In Endotext; Feingold, K.R., Anawalt, B., Boyce, A., Chrousos, G., de Herder, W.W., Dhatariya, K., Dungan, K., Grossman, A., Hershman, J.M., Hofland, J., et al., Eds.; MDText.com, Inc.: South Dartmouth, MA, USA, 2000. [Google Scholar]
- Sahoo, K.; Sahoo, B.; Choudhury, A.K.; Sofi, N.Y.; Kumar, R.; Bhadoria, A.S. Childhood Obesity: Causes and Consequences. J. Fam. Med. Prim. Care 2015, 4, 187–192. [Google Scholar] [CrossRef]
- Cannell, J.J.; Grant, W.B. What Is the Role of Vitamin D in Autism? Derm. Endocrinol. 2013, 5, 199–204. [Google Scholar] [CrossRef] [Green Version]
- Kittana, M.; Ahmadani, A.; Stojanovska, L.; Attlee, A. The Role of Vitamin D Supplementation in Children with Autism Spectrum Disorder: A Narrative Review. Nutrients 2021, 14, 26. [Google Scholar] [CrossRef]
- Guo, B.-Q.; Li, H.-B.; Ding, S.-B. Blood Homocysteine Levels in Children with Autism Spectrum Disorder: An Updated Systematic Review and Meta-Analysis. Psychiatry Res. 2020, 291, 113283. [Google Scholar] [CrossRef]
- Puig-Alcaraz, C.; Fuentes-Albero, M.; Calderón, J.; Garrote, D.; Cauli, O. Increased Homocysteine Levels Correlate with the Communication Deficit in Children with Autism Spectrum Disorder. Psychiatry Res. 2015, 229, 1031–1037. [Google Scholar] [CrossRef]
- Gunes, S.; Ekinci, O.; Celik, T. Iron Deficiency Parameters in Autism Spectrum Disorder: Clinical Correlates and Associated Factors. Ital. J. Pediatr. 2017, 43, 86. [Google Scholar] [CrossRef]
- Faber, S.; Zinn, G.M.; Kern II, J.C.; Skip Kingston, H.M. The Plasma Zinc/Serum Copper Ratio as a Biomarker in Children with Autism Spectrum Disorders. Biomarkers 2009, 14, 171–180. [Google Scholar] [CrossRef]
- Saldanha Tschinkel, P.F.; Bjørklund, G.; Conón, L.Z.Z.; Chirumbolo, S.; Nascimento, V.A. Plasma Concentrations of the Trace Elements Copper, Zinc and Selenium in Brazilian Children with Autism Spectrum Disorder. Biomed. Pharmacother. 2018, 106, 605–609. [Google Scholar] [CrossRef]
- Sweetman, D.U.; O’Donnell, S.M.; Lalor, A.; Grant, T.; Greaney, H. Zinc and Vitamin A Deficiency in a Cohort of Children with Autism Spectrum Disorder. Child. Care Health Dev. 2019, 45, 380–386. [Google Scholar] [CrossRef]
- Monteiro, M.A.; dos Santos, A.A.A.; Gomes, L.M.M.; Rito, R.V.V.F. Autism Spectrum Disorder: A Systematic Review about Nutritional Interventions. Rev. Paul. Pediatr. 2020, 38, e2018262. [Google Scholar] [CrossRef] [PubMed]
- Zulkifli, F.N.A.; Rahman, P.A. Relationships Between Sensory Processing Disorders with Feeding Behavior Problems Among Children with Autism Spectrum Disorder. Mal. J. Med. Health Sci. 2021, 17 (Suppl. 3), 230–236. [Google Scholar]
- Silverman, A.H. Behavioral Management of Feeding Disorders of Childhood. ANM 2015, 66, 33–42. [Google Scholar] [CrossRef] [PubMed]
- Elamin, A.; Garemo, M.; Gardner, A. Dental Caries and Their Association with Socioeconomic Characteristics, Oral Hygiene Practices and Eating Habits among Preschool Children in Abu Dhabi, United Arab Emirates—The NOPLAS Project. BMC Oral Health 2018, 18, 104. [Google Scholar] [CrossRef] [Green Version]
- Sayegh, A.; Dini, E.L.; Holt, R.D.; Bedi, R. Food and Drink Consumption, Sociodemographic Factors and Dental Caries in 4–5-Year-Old Children in Amman, Jordan. Br. Dent. J. 2002, 193, 37–42. [Google Scholar] [CrossRef] [Green Version]
- Kutbi, H.A. Picky Eating in School-Aged Children: Sociodemographic Determinants and the Associations with Dietary Intake. Nutrients 2021, 13, 2518. [Google Scholar] [CrossRef]
- Mouallem, R.E.; Malaeb, D.; Akel, M.; Hallit, S.; Khalife, M.-C.F. Food Neophobia in Lebanese Children: Scale Validation and Correlates. Public Health Nutr. 2021, 24, 5015–5023. [Google Scholar] [CrossRef]
- Qazaryan, K.S.; Karim, S. The Clinical Link of Preschoolers’ Picky Eating Behavior with Their Growth, Development, Nutritional Status, and Physical Activity in Iraq/Kurdistan Region. Highlights Med. Med. Sci. 2019, 5, 119–132. [Google Scholar] [CrossRef]
- Ashley, K.; Steinfeld, M.B.; Young, G.S.; Ozonoff, S. Onset, Trajectory, and Pattern of Feeding Difficulties in Toddlers Later Diagnosed with Autism. J. Dev. Behav. Pediatr. 2020, 41, 165–171. [Google Scholar] [CrossRef]

Child Terms | Autism Terms | Countries † | Nutritional Status Terms | Eating Behavior Terms |
|---|---|---|---|---|
| Infant Infancy Baby Babies Newborn Toddler Preschool Pre-school Children Child Kindergar * Schoolchild Teen * Youth | Autism Autism, early infantile Autism, infantile Kanner’s syndrome Autistic Autistics disorder | Algeria, Djibouti, Egypt, Bahrain, United Arab Emirates, Qatar, Kuwait, and the Kingdom of Saudi Arabia, Iran, Iraq, Jordan, Lebanon, Libya, Morocco, Oman, Palestine, Sudan, Syria, Tunisia, Tunisia, Yemen, Arab, West Bank, Gaza, Middle East, North Africa, MENA, Middle East North Africa | Nutrition Nutritional status Anthropom * Energy Calorie * Weight * Height * Circumference BMI Body Mass Index Nutrient * Micronutrient Macronutrient Protein Fat * Carbohydrate * Vitamin Mineral Iron Zinc Folate Folic acid | Food intake Ingestion Feeding behavior Diet habits Dietary habits Eating behavior Eating habits Feeding pattern Eating pattern Food habits Food Fussiness Picky eating Meal Snack |
| # | First Author (Year) | Country | Aim | Study Design | Cases | n | Controls | n | Recruitment |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Aghaeinejad (2013) [24] | Iran | Compare nutritional intake with TD-C | Cross-sectional | Male 6–11 years | 62 | TD-C Male 6–11 years | 62 | Cases: Elementary schools in Tehran Controls: Elementary schools in Tehran |
| 2 | Al-Ali (2014) [25] | Palestine | Investigate iron deficiency association with ASD and compare food selectivity indices | Case-control | Both genders 3–13 years | 30 | Both genders 3–13 years Group 1: Children with other mental disorders Group 2: TD-C | Group 1: 30 Group 2: 30 | Cases: Rehabilitation centers from the North West Bank Control 1: Same rehabilitation centers Control 2: from the general population |
| 3 | Al-Bazzaz (2020) [26] | Jordan | Measure fasting levels of glucose, zinc, copper, and zinc/copper ratio, as well as their correlations to the lipid profile | Cross-sectional | Both genders 4–12 years | 35 | TD-C Both genders 4–12 years | 35 | Cases: Autism Academy of Jordan Controls: NR |
| 4 | Al-Farsi (2011) [9] | Oman | Assess the prevalence of malnutrition indicators | Cross-sectional | Both genders 3–5 years | 128 | N/A | N/A | Cases: Various social centers and a child psychiatry clinic in Oman Controls: N/A |
| 5 | Al-Farsi (2013a) [27] | Oman | Assess the dietary and serum folate and vitamin B12 statuses | Case-control | Both genders 3–5 years | 40 | TD-C Both genders 3–5 years | 40 | Cases: Sultan Qaboos University Hospital (SQUH) Controls: Outpatients—Child Health Department at SQUH |
| 6 | Al-Farsi (2013b) [28] | Oman | Evaluate the serum levels and dietary intake of docosahexaenoic acid | Case-control | Both genders <5 years | 40 | TD-C Both genders <5 years | 40 | Cases: Child and Adolescent Psychiatry—SQUH Controls: Outpatients from the Child Health Department at SQUH |
| 7 | Ali (2011) [29] | Oman | Compare serum homo-cysteine, folate, and vitamin B12 | Case-control | Both genders 3–5 years | 40 | TD-C Both genders 3–5 years | 40 | Cases: NR, Assumed SQUH Controls: Outpatients from the Child Health Department at SQUH |
| 8 | Alkazemi (2016) [30] | Kuwait | Evaluate obesity and investigate dietary habits and mealtime behavior | Cross-sectional | Both genders 5–27 years (subgroup: <19 years) | 33 (<19 years) | N/A | N/A | Cases: Reach School at Kuwait Center for Autism Controls: N/A |
| 9 | Al-Kindi (2016) [31] | Oman | Evaluate the nutritional status through BMI and nutritional intake | Cross-sectional | Both genders 4–13 years | 163 | TD-C Both genders 4–13 years | 212 | Cases: SQUH, Developmental Medicine Clinic, Muscat Autism Center, Early Intervention Center for Children with Disabilities, and Al-Waffa Rehabilitation Centers. Controls: Same provinces |
| 10 | Al-Kindi (2020) [32] | Oman | Assess food selection criteria, and preferences | Cross-sectional | Both genders 4–13 years | 163 | TD-C Both genders 4–13 years | 212 | Same as Al-Kindi 2016 |
| 11 | Alzghoul (2019) [33] | Jordan | Assess correlation between vitamin D and ASD | Case-control | Male <8 years | 83 | TD-C Male <8 years | 106 | Cases: pediatric clinics and healthcare centers Controls: Jordan University Hospital |
| 12 | Arastoo (2018) [34] | Iran | Evaluate vitamin D status | Cross-sectional | Both genders 5–12 years | 31 | TD-C Both genders 5–12 years | 31 | Cases: Special schools in Ahvaz city Controls: Regular schools in Ahvaz city |
| 13 | Ashour (2018) [35] | Saudi Arabia | Investigate the association between dental carries and obesity | Cross-sectional | Females only 6–17 years | 41 | Other physical or developmental disabilities Females only 6–17 years | 234 | Cases: various special need schools in Makkah City Controls: Same as cases |
| 14 | Attlee (2015) [36] | UAE | Assess the physical status and feeding behavior | Cross-sectional | Both genders 5–16 years | 23 | N/A | N/A | Cases: Sharjah Autism Center-Sharjah City Controls: N/A |
| 15 | Bener (2014) [37] | Qatar | Investigate the association between vitamin D and ASD | Case-control | Both genders <9 years | 254 | TD-C Both genders <9 years | 254 | Cases: Pediatrics Clinics and School Health Controls: Primary Health Care centers |
| 16 | Bener (2017) [38] | Qatar | Investigate iron and vitamin D deficiency and to assess risk factors | Case-control | Both genders <8 years | 308 | TD-C Both genders <8 years | 308 | Cases: Pediatrics Clinic and School Health Controls: Primary Health Care centers |
| 17 | Cherif (2018) [39] | Tunisia | Evaluate the frequency and the types of feeding problems | Cross-sectional | Both genders 2–12 years | 57 | TD-C Both genders Age: NR, but age-matched with cases. | 57 | Cases: Department of child psychiatry of Sfax Controls: Two Kindergartens from the same area |
| 18 | Desoky (2017) [40] | Egypt | Assess thyroid profile, vitamin D levels, and CD5 expression levels, and evaluate correlation with ASD severity | Cross-sectional | Both genders Age range NR. Mean age: 7.03 ± 2.34 years | 60 | TD-C Both genders Age range NR. Mean age: 7.91 ± 3.21 years | 40 | Cases: Neuropsychiatric and Pediatric Departments of Qena University Hospital Controls: NR |
| 19 | El-Ansary (2010) [41] | Saudi Arabia | Clarify the role of selected ions related to energy metabolism in the deterioration accompanied autism | Cross-sectional | Both genders 3–15 years | 30 | TD-C Both genders 3–15 years | 30 | Cases: NR Controls: NR |
| 20 | El-Ansary (2011) [42] | Saudi Arabia | Compare the concentrations of essential fatty acids (FAs), polyunsaturated FAs, and phospholipids | Cross-sectional | Both genders 4–12 years | 25 | TD-C Both genders 4–11 years | 16 | Cases: Autism Research and Treatment Center Clinic—King Saud University Controls: Well Baby clinic-King Khaled University Hospital |
| 21 | El-Ansary (2018) [43] | Saudi Arabia | Determine if there is any relationship between vitamin D levels and ASD presence and severity | Cross-sectional | Male only 3–12 years | 28 | TD-C Male only Age range NR. Mean age: 7.2 ± 2.14 years | 27 | Cases: Autism Research and Treatment Center Clinic—King Saud University Controls: siblings of infants from the Well Baby Clinic-King Khalid University Hospital |
| 22 | Elbaz (2014) [44] | Egypt | Study plasma essential and non-essential amino acid levels, protein electrophoresis, serum ammonia, and urea | Cross-sectional | Both genders 2–7 years | 20 | TD-C Both genders 2–7 years | 20 | Cases: Psychiatric clinic—Children’s Hospital, and Institute of Postgraduate Childhood Studies—Ain Shams University Controls: Pediatrics Outpatient Clinic—Children’s Hospital |
| 23 | El-Khatib (2014) [45] | Egypt | Assess the oral health status and behaviors of children | Cross-sectional | Both genders 3–13 years | 100 | TD-C Both genders 3–13 years | 100 | Cases: Private and governmental institutions—Alexandria Controls: Private and governmental schools |
| 24 | Fahmy (2016) [46] | Egypt | Determine vitamin D dietary intake and sun exposure | Cross-sectional | Both genders 3–15 years | 42 | TD-C Both genders 3–15 years | 40 | Cases: Autism clinic—Ain Shams University hospital Controls: Cases siblings |
| 25 | Ghodsi (2019) [47] | Iran | Examine carnosine supplementation effects on the advanced glycation end products and the precursors of advanced lipoxidation end products | Randomized controlled trial | ASD-C—with carnosine supplements Both genders 4–14 years | 18 | ASD-C—without carnosine supplements Both genders 4–14 years | 18 | Cases: NR Controls: NR |
| 26 | Hammouda (2018) [48] | Saudi Arabia | Identify nutritional risk factors that predispose to autism | Case-control | Both genders 2.4–9 years | 30 | TD-C Both genders 2–9 years | 36 | Cases: Pediatric psychiatry outpatient clinic and autism day care center—Al-Amal psychiatric hospital. Controls: University and Nabaa AL-Maref Nursery (2–6 years) and researchers’ family members (7–10 years) |
| 27 | Hashemzadeh (2015) [49] | Iran | Compare the vitamin D serum levels | Case-control | Both genders 3–12 years | 13 | TD-C Both genders Age: NR, but matched with cases | 14 | Cases: Outpatient clinic of Ibn-e-Sina psychiatric hospital Controls: NR |
| 28 | Hawari (2020) [50] | Syria | Investigate the levels of lead, manganese, and zinc | Case-control | Group 1: ASD only Both genders 3–12 years Group 2: ASD and ADHD Both genders 3–12 years | Group 1: 31 Group 2: 11 | Group 1: ADHD only Both genders 3–12 years Group 2: TD-C Both genders 3–12 years | Group 1: 29 Group 2: 30 | Cases: Children Hospital and from related associations Controls: Children Hospital and from related associations |
| 29 | Javadfar (2020) [51] | Iran | Evaluate the effect of vitamin D on core symptoms and serum serotonin and IL-6 | Randomized controlled trial | ASD-C and vitamin D supplements Both genders 3–13 years | 26 | ASD-C, but without vitamin D supplements Both genders 3–13 years | 26 | Cases: Autism clinic of Kermanshah University of Medical Sciences Controls: Autism clinic of Kermanshah University of Medical Sciences |
| 30 | Meguid (2008) [52] | Egypt | Estimate free PUFAs in blood and evaluate behavior of children before and after taking fish oil | Before/after trial | Both genders 3–11 years | 30 | TD-C Both genders 3–11 years | 30 | Cases: Department of the Children with Special Needs, National Research Center Controls: NR |
| 31 | Meguid (2010) [53] | Egypt | Investigate the potential role of vitamin D in autism | Cross-sectional | Gender NR Age range NR. Mean age 5.3 ± 2.8 years | 70 | TD-C Gender NR Age range NR. Mean age 6.1 ± 1.8 years | 42 | Cases: Department of the Children with Special Needs, National Research Center Controls: Other clinics at the same facility |
| 32 | Meguid (2015) [54] | Egypt | Assess the nutritional status of autistic children | Cross-sectional study | Both genders 3–9 years | 80 | N/A | N/A | Same as Meguid 2014 |
| 33 | Meguid (2017) [55] | Egypt | Comparing dietary regimens and habits | Cross-sectional | Both genders 4–6 years | 80 | TD-C Both genders Age range NR. Age mean 3.7 ± 0.52 years | 80 | Cases: Department of the Children with Special Needs, National Research Center Controls: NR |
| 34 | Meguid (2019) [56] | Egypt | Elucidate the role of zinc supplementation on plasma concentration, gene expression, and cognitive-motor performance | Before/after trial | Both genders 3–8 years | 30 | N/A | N/A | Same as Meguid 2014 |
| 35 | Metwally (2018) [57] | Egypt | Assess the concentration of serum BPA and 8-oxodG levels | Cross-sectional | Both genders 5–12 years | 49 | TD-C Both genders Age range NR. Age mean 5.333 ± 2.279 years | 40 | Cases: Learning Disability and Neuro-Rehabilitation at Medical Excellence Centre, National Research Centre Controls: NR |
| 36 | Mostafa (2012) [58] | Saudi Arabia | Investigate the relationship between vitamin D and anti-myelin-associated glycoprotein auto-antibodies | Cross-sectional | Both genders 5–12 years | 50 | TD-C Both genders 5–12 years | 30 | Cases: Autism Research and Treatment Center—King Saud University Controls: Siblings of infants from the Well Baby Clinic—King Khalid University Hospital |
| 37 | Mostafa (2015a) [59] | Egypt | Investigate the relationship between serum levels of anti-myelin basic protein auto-antibodies and plasma levels of PUFAs | Cross-sectional | Both genders 4–12 years | 80 | TD-C Both genders 4–12 years | 80 | Cases: Pediatric Neuropsychiatric Clinic—Children’s Hospital Controls: Outpatients Clinic—Children’s Hospital, |
| 38 | Mostafa (2015b) [60] | Saudi Arabia | Investigate plasma levels of PUFAs and serum carnitine in relation to GI manifestations | Cross-sectional | Both genders 3–10 years | 100 | TD-C Both genders 3–10 years | 80 | Same as Mostafa (2012) |
| 39 | Murshid (2014) [61] | Saudi Arabia | Report baseline information about the diet, oral hygiene, and dental health of a group of autistic children | Cross-sectional | Both genders 3–14 years | 344 | N/A | N/A | Cases: 3 autistic rehabilitation centers registered with the Saudi Autistic Society Controls: N/A |
| 40 | Saad (2016) [20] | Egypt | Assess vitamin D status compared with controls and the relationship between vitamin D deficiency and autism severity | Cross sectional, followed by a trial | Both genders 3–9 years | 122 | TD-C Both genders Age range NR. Mean age: 4.88 ± 1.30 years | 100 | Cases: Assiut university hospitals and five private centers Controls: Assiut university hospitals and siblings of cases |
| 41 | Salehi (2014) [62] | Iran | Assess body composition and association of demographic factors, autism severity, and drug therapy | Cross-sectional | Males only 7–14 years | 85 | N/A | N/A | Cases: Four autism specific schools in Tehran, Controls: N/A |
| 42 | Shaaban (2018) [63] | Egypt | Evaluate the efficacy and tolerability of probiotics | prospective, open-label study | Both genders 5–9 years | 30 | TD-C Both genders Age range not provided, but controls are age-matched | 30 | Cases: Ain Shams University Hospitals, and The Developmental Pediatric Clinic—National Research Center, Controls: patients’ relatives |
| 43 | Wtwt (2015) [64] | Iraq | Assess common feeding problems and nutritional status | Cross-sectional | Both genders Age: >3 years | 70 | N/A | N/A | Cases: Al Rehma Institute of Autism, Babil Specialized Institute of Autism, and Al Imam Al Husien Institute Controls: N/A |
| First Author (Year) | Age (Year) | Height (cm) | Weight (kg) | BMI (kg/m2)/BMI z-Score | BMI Categories n (%) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| UWT | NWT | OWT | Obese | p | |||||||||||||||
| A | C | p | A | C | p | A | C | p | A | C | A | C | A | C | A | C | |||
| Aghaeinejad (2013) [24] | 6–11 | 133.45 ± 8.26 | 130.57 ± 8.35 | 0.05 | 33.14 ± 8.02 | 30.09 ± 8.18 | 0.03 | 6 (10) | 8 (13) | 29 (47) | 31 (50) | 7 (11) | 13 (21) | 20 (32) | 10 (16) | 0.14 | |||
| Al-Farsi (2013a) [27] | 3–5 | 15.8 ± 3.1 | 18.34 ± 2.4 | ||||||||||||||||
| Alkazemi (2016) [30] | 5–19 | (6) | N/A | (36) | N/A | O/O (58) | N/A | N/A | |||||||||||
| Al-Kindi (2016) [31] | 4–13 | 15.4 ± 2.5 | 15.4 ± 2.6 | 0.816 | 47 (28.8) | 67 (31.6) | 91 (55.8) | 126 (59.4) | 22 (13.5) | 17 (8.0) | 3 (1.8) | 2 (0.9) | 0.301 | ||||||
| Arastoo (2018) [34] | 5–12 | 142.35 ± 14.23 | 137.06 ± 12.52 | 0.12 | 42.37 ± 19.55 | 36.13 ± 12.53 | 0.14 | ||||||||||||
| Ashour (2018) [35] | 6–17 | 2 (4.8) | 23 (56.1) | 7 (17.1) | 9 (21.9) | N/A | |||||||||||||
| Attlee (2015) [36] | 5–16 | 148.8 ± 20.2 | N/A | N/A | 78.15 ± 43.7 | N/A | N/A | 25.5 ± 10.3 | N/A | N/A | 0 (0) | N/A | 6 (26) | N/A | 5 (22) | N/A | 12 (52) | N/A | N/A |
| Bener (2014) [37] | <9 | U + N 227 (89.4) | U + N 204 (80.3) | 22 (8.7) | 41 (16.1) | 5 (2.0) | 9 (3.5) | <0.001 | |||||||||||
| Bener (2017) [38] | <8 | U + N 248 (89.4) | U + N 255 (80.3) | 39 (8.7) | 34 (16.1) | 21 (2.0) | 15 (3.5) | <0.001 | |||||||||||
| Fahmy (2016) [46] | 3–15 | 120 ± 14.9 | 123.5 ± 20.1 | 0.385 | 27.7 ± 9.3 | 26.4 ± 12.5 | 0.613 | ||||||||||||
| Ghodsi (2019) [47] | 4–14 | 134.93 | N/A | N/A | 31.94 | N/A | N/A | 6 (16.7) | N/A | 23 (63.9) | N/A | 7 (19.4) | N/A | 0 | N/A | N/A | |||
| Hammouda (2018) [48] | 2.4–9 | The prevalence of overweight and underweight was higher among ASD-C (Data not presented) | 0.098 | ||||||||||||||||
| Javadfar (2020) [51] | 3–13 | 33.55 | N/A | N/A | |||||||||||||||
| Meguid (2015) [54] | 3–5 | 108.32 ± 1.20 | N/A | N/A | 21.15 ± 1.14 | N/A | N/A | F:18.89 ± 1.42/0.4 ± 0.3 M:19.06 ± 2.57/0.95 ± 0.04 | N/A | N/A | |||||||||
| Meguid (2015) [54] | 6–9 | 131.08 ± 0.87 | N/A | N/A | 37.17 ± 1.02 | N/A | N/A | F:19.02 ± 1.05/1.6 ± 0.5 M:19.71 ± 1.70/0.9 ± 0.05 | N/A | N/A | |||||||||
| Meguid (2017) [55] | 4–6 | 98.5 ± 6.6 | 97.7 ± 5.7 | 0.43 | 16.0 ± 2.3 | 15.2 ± 1.7 | 0.02 | ||||||||||||
| Metwally (2018) [57] | 5–12 | 17.713 ± 4.228 | 15.994 ± 0.691 | 0.007 | |||||||||||||||
| Mostafa (2012) [58] | 5–12 | All studied subjects had normal body weight (BMI was between the 5th and 85th percentiles based on age and sex) | N/A | ||||||||||||||||
| Mostafa (2015b) [60] | 3–10 | All studied subjects had normal body weight (BMI was between the 5th and 85th percentiles based on age and sex) | N/A | ||||||||||||||||
| Salehi (2014) [62] | 7–14 | 138.56 ± 11.41 | N/A | N/A | 37.48 + 12.12 | N/A | N/A | 19.14 + 4.23/NR | N/A | N/A | (9.40) | N/A | (43.50) | N/A | (24.70) | N/A | (22.40) | N/A | N/A |
| Shaaban (2018) [63] | 5–9 | 122.48 ± 8.27 | N/A | N/A | 25.91 ± 5.32 | N/A | N/A | 17.043 ± 1.36/0.80 ± 0.56 | N/A | N/A | (0) | N/A | (40) | N/A | (60) | N/A | (0) | N/A | N/A |
| Wtwt (2015) [64] | 3–6 | 0(0) | N/A | 20 (45.5) | N/A | O/O 24 (54.5) | N/A | N/A | |||||||||||
| Wtwt (2015) [64] | >6 | 4 (15.4) | N/A | 8 (30.8) | N/A | O/O 14 (53.8) | N/A | N/A | |||||||||||
| First Author | Serum Iron (ug/dL) | Vitamin B12 (pg/mL) | Folate (μg/L) | HCY (μmol/L) | ||||||||
| A | C | p | A | C | p | A | C | p | A | C | p | |
| Al-Ali (2014) [25] | ||||||||||||
| Al-Farsi (2013a) [27] | 183.6 ± 12.3 | 341.2 ± 27.4 | 0.001 | 2.1 ± 0.3 | 7.3 ± 0.4 | 0.001 | 6.59 ± 0.6 | 3.92 ± 0.5 | 0.004 | |||
| Ali (2011) [29] | 191.1 ± 0.9 | 288.9 ± 1.3 | <0.05 | 1.8 ± 0.4 | 6.1 ± 0.6 | <0.05 | 20.1 ± 3.3 | 9.64 ± 2.1 | <0.01 | |||
| Bener (2017) [38] | 74.13 ± 21.61 | 87.59 ± 23.36 | 0.003 | |||||||||
| Meguid (2017) [55] | Lower | Higher | Sig. | Lower | Higher | Sig. | Lower | Higher | Sig. | |||
| First Author | Hb (g/dL) | HCT (%) | MCV (fL) | Ferritin (ng/mL) | ||||||||
| A | C | p | A | C | p | A | C | p | A | C | p | |
| Al-Ali (2014) [25] | 11.543 | MD: 11.960 TD: 12.250 | 0.016 | 34.32 | MD: 36.453 TD: 35.707 | 0.016 | 76.597 | MD: 80.243 TD: 78.213 | 0.052 | 29.63 | MD: 29.513 TD: 35.880 | 0.316 |
| Al-Farsi (2013a) [27] | 11.3 ± 0.7 | 12.4 ± 0.8 | 0.43 | 92 ± 6 | 83 ± 9 | 0.21 | ||||||
| Bener (2017) [38] | 12.03 ± 2.13 | 12.86 ± 2.02 | <0.001 | 36.32 ± 2.81 | 39.07 ± 2.66 | <0.001 | 77.23 ± 5.92 | 85.24 ± 6.53 | <0.001 | 36.57 ± 5.12 | 38.49 ± 5.73 | <0.001 |
| First Author (Year) | Energy (kcal/Day) | Carbohydrates (g/Day) | Protein (g/Day) | Fat (g/Day) | Fiber (g/Day) | ||||||||||
| A | C | p | A | C | p | A | C | p | A | C | p | A | C | p | |
| Aghaeinejad (2013) [24] | 1926.27 ± 460.07 | 1647.66 ± 317.14 | 0.001 | 240.20 ± 74.59 | 235.86 ± 48.40 | 0.7 | 69.30 ± 21.52 | 64.08 ± 17.57 | 0.14 | 80.48 ± 24.13 | 52.36 ± 16.07 | 0.001 | |||
| Al-Farsi (2013b) [28] | 1323 ± 117.8 | 1684 ± 101.3 | 0.001 | ||||||||||||
| Al-Kindi (2016) [31] | 1389.6 (56.6) | 1594.9 (43.2) | 0.005 | 229.2 (11.1) | 248.0 (7.8) | 0.16 | 47.5 (1.8) | 55.4 (1.6) | 0.002 | 38.9 (3.3) | 47.4 (1.8) | 0.015 | 9.8 (0.7) | 12.5 (0.7) | 0.017 |
| Hammouda (2018) [48] | 1330 ± 541 | 1576 ± 463 | 0.051 | 199 ± 87 | 234 ± 67 | 0.076 | 38 ± 20 | 48 ± 25 | 0.091 | 46 ± 24 | 54 ± 21 | 0.159 | |||
| Javadfar (2020) [51] | 1765.65 | NA | 246.05 | NA | 56.65 | NA | 61.65 | NA | |||||||
| Meguid (2015) (age 3–5) [54] | 1490.98 ± 58.51 | NA | 202.23 ± 7.51 | NA | 32.77 ± 3.69 | NA | 61.22 ± 4.61 | NA | 19.56 ± 2.33 | NA | |||||
| Meguid (2015) (age 6–9) [54] | 1875.82 ± 55.32 | NA | 297.79 ± 32.54 | NA | 35.58 ± 7.95 | NA | 60.26 ± 11.80 | NA | 23.57 ± 2.85 | NA | |||||
| Meguid (2017) [55] | 1116.2 ± 271.6 | 1136.5 ± 269.4 | 0.317 | 145.3 ± 22.3 | 143.0 ± 32.4 | 0.303 | 36.6 ± 10.3 | 39.7 ± 8.7 | 0.021 | 43.2 ± 12.8 | 45.0 ± 11.1 | 0.233 | 1.4 ± 0.4 | 0.715 ± 0.2 | 0.001 |
| Author (Year) | Omega-3 (g/day) | Saturated fat (g/day) | MUFA (g/day) | PUFA (g/day) | Cholesterol (mg/day) | ||||||||||
| A | C | p | A | C | p | A | C | p | A | C | p | A | C | p | |
| Al-Farsi (2013b) [28] | 0.8 ± 0.2 | 1.2 ± 0.4 | 0.001 | ||||||||||||
| Al-Kindi (2016) [31] | 9.4 (0.9) | 14.4 (0.7) | <0.001 | 122.2 (12.7) | 153.3 (10.0) | 0.057 | |||||||||
| Hammouda (2018) [48] | 0.029 ± 0.036 | 0.268 ± 0.498 | 0.011 | ||||||||||||
| Javadfar (2020) [51] | 0.0065 | NA | |||||||||||||
| Meguid (2015) (age 3–5) [54] | 21.27 ± 1.45 | NA | 17.25 ± 1.57 | NA | 9.35 ± 1.69 | NA | 289.19 ± 14.75 | NA | |||||||
| Meguid (2015) (age 6–9) [54] | 29.63 ± 11.30 | NA | 23.61 ± 2.21 | NA | 12.35 ± 1.02 | NA | 258.03 ± 21.05 | NA | |||||||
| First Author (Year) | Vitamin A (μg/Day) | Riboflavin (mg/Day) | Niacin (mg/Day) | Pyridoxine (mg/Day) | Vitamin C (mg/Day) | Vitamin E (mg/Day) | ||||||||||||
| A | C | p | A | C | p | A | C | p | A | C | p | A | C | p | A | C | p | |
| Al-Kindi (2016) [31] | 281.6 ± 65.2 | 306.6 ± 29.5 | 0.689 | 1.4 ± 0.2 | 1.5 ± 0.1 | 0.615 | 15.4 ± 0.9 | 15.2 ± 0.8 | 0.861 | 1.2 ± 0.19 | 1.3 ± 0.1 | 0.416 | 47.2 ± 4.6 | 61.0 ± 4.7 | 0.057 | 1.9 ± 0.3 | 2.2 ± 0.2 | 0.361 |
| Javadfar (2020) [51] | 738.25 | NA | 1.25 | NA | 18.15 | NA | 1.3 | NA | 119.25 | NA | 2.4 | |||||||
| Meguid (2015) (age 3–5) [54] | 560.19 ± 35.58 | NA | 0.88 ± 0.10 | NA | 10.09 ± 5.23 | NA | 0.91 ± 0.49 | NA | 39.89 ± 5.41 | NA | 5.99 ± 0.55 (TR) | |||||||
| Meguid (2015) (age 6–9) [54] | 789.25 ± 32.5 | NA | 1.28 ± 0.14 | NA | 13.96 ± 4.35 | NA | 1.51 ± 0.27 | NA | 35.99 ± 3.09 | NA | 7.21 ± 1.01 (TR) | |||||||
| Meguid (2017) [55] | 159.6 ± 30.9 mg | 161.8 ± 46.7 mg | 0.359 | 0.47 ± 0.12 | 0.5 ± 0.13 | 0.052 | 0.91 ± 0.16 | 0.6 ± 0.15 | 0.001 | 23.2 ± 6.8 | 17.7 ± 4.7 | 0.001 | ||||||
| First Author (Year) | Thiamin (mg/day) | Phosphorus (mg/day) | Folic acid (μg/day) | vitamin B12 (μg/day) | vitamin D (μg/day) | |||||||||||||
| A | C | p | A | C | p | A | C | p | A | C | p | A | C | p | ||||
| Al-Farsi (2013a) [27] | 136.3 (5.2) | 230.5 (3.7) | 0.04 | 1.3 (0.9) | 2.2 (0.8) | 0.02 | ||||||||||||
| Al-Kindi (2016) [31] | 1.2 (0.1) | 1.2 (0.1) | 0.913 | 297.9 (16.1) | 297.2 (14.8) | 0.977 | 1.9 (0.7) | 1.9 (0.1) | 0.993 | 1.9 (0.2) | 3.0 (0.2) | 0.0001 | ||||||
| Fahmy (2016) [46] | 164.7 ± 71.5 (IU) | 177.9 ± 75.9 (IU) | 0.42 | |||||||||||||||
| Hammouda (2018) [48] | 173 ± 128 | 203 ± 97.9 | 0.44 | 0.45 ± 2.27 | 0.55 ± 1.9 | 0.365 | 1.31 ± 1.91 | 1.60 ± 1.60 | 0.515 | |||||||||
| Javadfar (2020) [51] | 1.45 | NA | 209.2 | NA | 3.5 | NA | 0.95 (IU) | NA | ||||||||||
| Meguid (2015) (age 3–5) [54] | 0.89 ± 0.60 | NA | 434.28 ± 35.11 | NA | 195.55 ± 27.21 | NA | 1.75 ± 1.26 | NA | 2.34 ± 0.68 | NA | ||||||||
| Meguid (2015) (age 6–9) [54] | 1.40 ± 1.07 | NA | 1195.25 ± 68.96 | NA | 231.03 ± 16.97 | NA | 2.29 ± 0.97 | NA | 1.95 ± 0.37 | NA | ||||||||
| Meguid (2017) [55] | 0.27 ± 0.08 | 0.28 ± 0.07 | 0.27 | 468.2 ± 119.9 | 469.7 ± 122.7 | 0.467 | 197.75 ± 34.22 | 269.48 ± 20.90 | 0.001 | 0.39 ± 0.12 | 0.85 ± 0.15 | 0.001 | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kittana, M.; Ahmadani, A.; Williams, K.E.; Attlee, A. Nutritional Status and Feeding Behavior of Children with Autism Spectrum Disorder in the Middle East and North Africa Region: A Systematic Review. Nutrients 2023, 15, 711. https://doi.org/10.3390/nu15030711
Kittana M, Ahmadani A, Williams KE, Attlee A. Nutritional Status and Feeding Behavior of Children with Autism Spectrum Disorder in the Middle East and North Africa Region: A Systematic Review. Nutrients. 2023; 15(3):711. https://doi.org/10.3390/nu15030711
Chicago/Turabian StyleKittana, Monia, Asma Ahmadani, Keith E. Williams, and Amita Attlee. 2023. "Nutritional Status and Feeding Behavior of Children with Autism Spectrum Disorder in the Middle East and North Africa Region: A Systematic Review" Nutrients 15, no. 3: 711. https://doi.org/10.3390/nu15030711