The Mediating Role of the Muscle Quality Index in the Relation of Screen Time and Abdominal Obesity with Health-Related Quality of Life in Chilean Schoolchildren
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Main Outcomes
2.2.1. Health-Related Quality of Life
2.2.2. Muscle Quality Index
2.2.3. Abdominal Obesity
2.2.4. Screen Time and Physical Activity
2.2.5. Cardiorespiratory Fitness
2.2.6. Anthropometric Parameters
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Frisén, A. Measuring health-related quality of life in adolescence. Acta Paediatr. 2007, 96, 963–968. [Google Scholar] [CrossRef] [PubMed]
- Stenman, U.; Hakama, M.; Knekt, P.; Aromaa, A.; Teppo, L.; Leinonen, J.; Zhang, B.; Yang, B.; Tang, Z. Measurement and modeling of health-related quality of life. Epidem. Demog. Public Health 2010, 195, 130–135. [Google Scholar]
- Jonsson, U.; Alaie, I.; Löfgren Wilteus, A.; Zander, E.; Marschik, P.B.; Coghill, D.; Bölte, S. Annual Research Review: Quality of life and childhood mental and behavioural disorders–a critical review of the research. J. Child Psychol. Psychiatry 2017, 58, 439–469. [Google Scholar] [CrossRef] [PubMed]
- Marker, A.; Steele, R.; Noser, A. Physical activity and health-related quality of life in children and adolescents: A systematic review and meta-analysis. Health Psychol. 2018, 37, 893–903. [Google Scholar] [CrossRef] [PubMed]
- Pfeifer, J.H.; Berkman, E.T. The Development of Self and Identity in Adolescence: Neural Evidence and Implications for a Value-Based Choice Perspective on Motivated Behavior. Child Dev. Perspect. 2018, 12, 158–164. [Google Scholar] [CrossRef]
- World Health Organization. Promoting Mental Health: Concepts, Emerging Evidence, Practice: A Report of the World Health Organization, Department of Mental Health and Substance Abuse in Collaboration with the Victorian Health Promotion Foundation and the University of Melbourne; World Health Organization: Geneve, Switzerland, 2005. [Google Scholar]
- Cheung, M.-C.; Yip, J.; Cheung, J.P.Y. Influence of Screen Time during COVID-19 on Health-Related Quality of Life of Early Adolescents. Int. J. Environ. Res. Public Health 2022, 19, 10498. [Google Scholar] [CrossRef]
- Stiglic, N.; Viner, R.M. Effects of screentime on the health and well-being of children and adolescents: A systematic review of reviews. BMJ Open 2019, 9, e023191. [Google Scholar] [CrossRef]
- Gopinath, B.; Hardy, L.L.; Baur, L.A.; Burlutsky, G.; Mitchell, P. Physical activity and sedentary behaviors and health-related quality of life in adolescents. Pediatrics 2012, 130, e167–e174. [Google Scholar] [CrossRef] [PubMed]
- Després, J.-P.; Lemieux, I. Abdominal obesity and metabolic syndrome. Nature 2006, 444, 881–887. [Google Scholar] [CrossRef]
- Wu, S.; Wang, R.; Jiang, A.; Ding, Y.; Wu, M.; Ma, X.; Zhao, Y.; He, J. Abdominal obesity and its association with health-related quality of life in adults: A population-based study in five Chinese cities. Health Qual. Life Outcomes 2014, 12, 100. [Google Scholar] [CrossRef]
- Kesztyüs, D.; Wirt, T.; Kobel, S.; Schreiber, A.; Kettner, S.; Dreyhaupt, J.; Kilian, R.; Steinacker, J.M. Is central obesity associated with poorer health and health-related quality of life in primary school children? Cross-sectional results from the Baden-Württemberg Study. BMC Public Health 2013, 13, 260. [Google Scholar] [CrossRef] [PubMed]
- Perez-Sousa, M.A.; Olivares, P.R.; Garcia-Hermoso, A.; Gusi, N. Does anthropometric and fitness parameters mediate the effect of exercise on the HRQoL of overweight and obese children/adolescents? Qual. Life Res. 2018, 27, 2305–2312. [Google Scholar] [CrossRef]
- Delgado-Floody, P.; Soto-García, D.; Caamaño-Navarrete, F.; Carter-Thuillier, B.; Guzmán-Guzmán, I.P. Negative Physical Self-Concept Is Associated to Low Cardiorespiratory Fitness, Negative Lifestyle and Poor Mental Health in Chilean Schoolchildren. Nutrients 2022, 14, 2771. [Google Scholar] [CrossRef] [PubMed]
- Andersen, J.R.; Natvig, G.K.; Aadland, E.; Moe, V.F.; Kolotkin, R.L.; Anderssen, S.A.; Resaland, G.K. Associations between health-related quality of life, cardiorespiratory fitness, muscle strength, physical activity and waist circumference in 10-year-old children: The ASK study. Qual. Life Res. 2017, 26, 3421–3428. [Google Scholar] [CrossRef]
- Evaristo, S.; Moreira, C.; Lopes, L.; Oliveira, A.; Abreu, S.; Agostinis-Sobrinho, C.; Oliveira-Santos, J.; Póvoas, S.; Santos, R.; Mota, J. Muscular fitness and cardiorespiratory fitness are associated with health-related quality of life: Results from labmed physical activity study. J. Exerc. Sci. Fit. 2019, 17, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Gerber, M.; Endes, K.; Brand, S.; Herrmann, C.; Colledge, F.; Donath, L.; Faude, O.; Hanssen, H.; Pühse, U.; Zahner, L. In 6- to 8-year-old children, cardiorespiratory fitness moderates the relationship between severity of life events and health-related quality of life. Qual. Life Res. 2016, 26, 695–706. [Google Scholar] [CrossRef]
- Lawman, H.G.; Troiano, R.P.; Perna, F.M.; Wang, C.-Y.; Fryar, C.D.; Ogden, C.L. Associations of relative handgrip strength and cardiovascular disease biomarkers in US adults, 2011–2012. Am. J. Prev. Med. 2016, 50, 677–683. [Google Scholar] [CrossRef]
- Kwak, Y.; Kim, Y. Quality of life and subjective health status according to handgrip strength in the elderly: A cross-sectional study. Aging Ment. Health 2019, 23, 107–112. [Google Scholar] [CrossRef]
- Yi, D.; Khang, A.R.; Lee, H.W.; Son, S.M.; Kang, Y.H. Relative handgrip strength as a marker of metabolic syndrome: The Korea National Health and Nutrition Examination Survey (KNHANES) VI (2014–2015). Diabetes Metab. Syndr. Obes. Targets Ther. 2018, 11, 227. [Google Scholar] [CrossRef]
- Steffl, M.; Chrudimsky, J.; Tufano, J.J. Using relative handgrip strength to identify children at risk of sarcopenic obesity. PLoS ONE 2017, 12, e0177006. [Google Scholar] [CrossRef]
- Zaccagni, L.; Toselli, S.; Bramanti, B.; Gualdi-Russo, E.; Mongillo, J.; Rinaldo, N. Handgrip Strength in Young Adults: Association with Anthropometric Variables and Laterality. Int. J. Environ. Res. Public Health 2020, 17, 4273. [Google Scholar] [CrossRef] [PubMed]
- Norman, K.; Stobäus, N.; Gonzalez, M.C.; Schulzke, J.D.; Pirlich, M. Hand grip strength: Outcome predictor and marker of nutritional status. Clin. Nutr. 2011, 30, 135–142. [Google Scholar] [CrossRef] [PubMed]
- Dumuid, D.; Olds, T.; Lewis, L.K.; Martin-Fernández, J.A.; Katzmarzyk, P.T.; Barreira, T.; Broyles, S.T.; Chaput, J.-P.; Fogelholm, M.; Hu, G.; et al. Health-related quality of life and lifestyle behavior clusters in school-aged children from 12 countries. J. Pediatr. 2017, 183, 178–183.e172. [Google Scholar] [CrossRef] [PubMed]
- Sepúlveda, R.; Molina, T.; Molina, R.; Martínez, V.; González, E.; George, M.; Montaño, R.; Hidalgo-Rasmussen, C. Validation of an instrument to measure health-related quality of life in Chilean children and adolescents. Rev. Méd. Chile 2013, 141, 1283–1292. [Google Scholar]
- Molina, G.; Montaño, E.; González, A.; Sepúlveda, P.; Hidalgo-Rasmussen, C.; Martínez, N.; Molina, C.; George, L. Psychometric properties of the quality of life questionnaire health related KIDSCREEN-27 in Chilean adolescents. Rev. Med. Chile 2014, 142, 1415–1421. [Google Scholar]
- Caamaño-Navarrete, F.; Angel Latorre-Roman, P.; Guzmán-Guzmán, I.P.; Parraga Montilla, J.; Jerez-Mayorga, D.; Delgado-Floody, P. Lifestyle mediates the relationship between self-esteem and health-related quality of life in Chilean schoolchildren. Psychol. Health Med. 2022, 27, 638–648. [Google Scholar] [CrossRef]
- Zulic-Agramunt, C.M.; Guzmán-Guzmán, I.P.; Delgado-Floody, P.; Saavedra, M.B.C.; De La Fuente, P.G.; Solano, M.M.; Berrios, C.S.; Testor, C.P. Psychosocial factors and sociodemographic characteristics associated with suicidality risk in Chilean adolescents. Children 2022, 9, 1185. [Google Scholar] [CrossRef]
- Ravens-Sieberer, U.; Erhart, M.; Rajmil, L.; Herdman, M.; Auquier, P.; Bruil, J.; Power, M.; Duer, W.; Abel, T.; Czemy, L. Reliability, construct and criterion validity of the KIDSCREEN-10 score: A short measure for children and adolescents’ well-being and health-related quality of life. Qual. Life Res. 2010, 19, 1487–1500. [Google Scholar] [CrossRef]
- Fess, F. Grip strength. In Casanova JS Clinical Assessment Recommendations, 2nd ed.; American Society of Hand Therapists: Mount Laurel, NJ, USA, 1992; pp. 41–45. [Google Scholar]
- Ruiz, J.R.; Espana Romero, V.; Castro Pinero, J.; Artero, E.G.; Ortega, F.B.; Cuenca, M.; Jimenez, D.; Chillon, P.; Girela, M.J.; Mora, J.; et al. Bateria ALPHA-Fitness: Test de campo para la evaluacion de la condicion fisica relacionada con la salud en ninos y adolescentes. Nutr. Hosp. 2011, 26, 1210–1214. [Google Scholar]
- Schröder, H.; Ribas, L.; Koebnick, C.; Funtikova, A.; Gomez, S.F.; Fíto, M.; Perez-Rodrigo, C.; Serra-Majem, L. Prevalence of abdominal obesity in Spanish children and adolescents. Do we need waist circumference measurements in pediatric practice? PLoS ONE 2014, 9, e87549. [Google Scholar] [CrossRef]
- Chung, I.H.; Park, S.; Park, M.J.; Yoo, E.-G. Waist-to-height ratio as an index for cardiometabolic risk in adolescents: Results from the 1998–2008 KNHANES. Yonsei Med. J. 2016, 57, 658–663. [Google Scholar] [CrossRef] [PubMed]
- Majem, L.S.; Barba, L.R.; Bartrina, J.A.; Rodrigo, C.P.; Santana, P.S.; Quintana, L.P. Obesidad infantil y juvenil en España. Resultados del Estudio enKid (1998–2000). Med. Clin. 2003, 121, 725–732. [Google Scholar] [CrossRef] [PubMed]
- Caamaño-Navarrete, F.; Latorre-Román, P.Á.; Párraga-Montilla, J.A.; Álvarez, C.; Delgado-Floody, P. Association between Creativity and Memory with Cardiorespiratory Fitness and Lifestyle among Chilean Schoolchildren. Nutrients 2021, 13, 1799. [Google Scholar] [CrossRef] [PubMed]
- Leger, L.A.; Mercier, D.; Gadoury, C.; Lambert, J. The multistage 20 metre shuttle run test for aerobic fitness. J. Sport. Sci. 1988, 6, 93–101. [Google Scholar] [CrossRef]
- MINEDUC. SIMCE 2015 Educación Física, Resultados para Docentes y Directivos; Santiago, Chile, 2015.
- Silva, D.A.S.; Lang, J.J.; Barnes, J.D.; Tomkinson, G.R.; Tremblay, M.S. Cardiorespiratory fitness in children: Evidence for criterion-referenced cut-points. PLoS ONE 2018, 13, e0201048. [Google Scholar] [CrossRef]
- Karnik, S.; Kanekar, A. Childhood obesity: A global public health crisis. Int. J. Prev. Med. 2012, 3, 1–7. [Google Scholar]
- Preacher, K.; Hayes, A. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav. Res. Methods Instrum. Comput. 2004, 36, 717–731. [Google Scholar] [CrossRef]
- Wu, X.; Tao, S.; Zhang, Y.; Zhang, S.; Tao, F. Low physical activity and high screen time can increase the risks of mental health problems and poor sleep quality among Chinese college students. PLoS ONE 2015, 10, e0119607. [Google Scholar] [CrossRef]
- Lacy, K.E.; Allender, S.E.; Kremer, P.J.; de Silva-Sanigorski, A.M.; Millar, L.M.; Moodie, M.L.; Mathews, L.B.; Malakellis, M.; Swinburn, B.A. Screen time and physical activity behaviours are associated with health-related quality of life in Australian adolescents. Qual. Life Res. 2012, 21, 1085–1099. [Google Scholar] [CrossRef]
- Saunders, T.J.; Vallance, J.K. Screen Time and Health Indicators Among Children and Youth: Current Evidence, Limitations and Future Directions. Appl. Health Econ. Health Policy 2017, 15, 323–331. [Google Scholar] [CrossRef]
- Aoki, A.; Togoobaatar, G.; Tseveenjav, A.; Nyam, A.; Zuunnast, K.; Lkhagvasuren, G.; Shagdar, B.-E.; Mori, R.; Kikuchi, A.; Soya, H.; et al. Socioeconomic and lifestyle factors associated with mental health problems among Mongolian elementary school children. Soc. Psychiatry Psychiatr. Epidemiol. 2022, 57, 791–803. [Google Scholar] [CrossRef] [PubMed]
- Babic, M.J.; Smith, J.J.; Morgan, P.J.; Eather, N.; Plotnikoff, R.C.; Lubans, D.R. Longitudinal associations between changes in screen-time and mental health outcomes in adolescents. Ment. Health Phys. Act. 2017, 12, 124–131. [Google Scholar] [CrossRef]
- Evaristo, O.S.; Moreira, C.; Lopes, L.; Abreu, S.; Agostinis-Sobrinho, C.; Oliveira-Santos, J.; Póvoas, S.; Oliveira, A.; Santos, R.; Mota, J. Associations between physical fitness and adherence to the Mediterranean diet with health-related quality of life in adolescents: Results from the LabMed Physical Activity Study. Eur. J. Public Health 2018, 28, 631–635. [Google Scholar] [CrossRef] [PubMed]
- Solera-Sanchez, A.; Adelantado-Renau, M.; Moliner-Urdiales, D.; Beltran-Valls, M.R. Individual and combined impact of physical fitness on health-related quality of life during adolescence: DADOS Study. Eur. J. Sport Sci. 2021, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Pastor, R.; Bouzas, C.; Albertos, I.; García, C.; García, Á.; Prieto, T.; Velázquez, J.; Sánchez-Jiménez, E.; Rodríguez, R.; Martín, F.J. Health-Related Quality of Life in Spanish Schoolchildren and Its Association with the Fitness Status and Adherence to the Mediterranean Diet. Nutrients 2022, 14, 2322. [Google Scholar] [CrossRef]
- Gu, X.; Chang, M.; Solmon, M.A. Physical activity, physical fitness, and health-related quality of life in school-aged children. J. Teach. Phys. Educ. 2016, 35, 117–126. [Google Scholar] [CrossRef]
- Janssen, A.; Leahy, A.A.; Diallo, T.M.; Smith, J.J.; Kennedy, S.G.; Eather, N.; Mavilidi, M.F.; Wagemakers, A.; Babic, M.J.; Lubans, D.R. Cardiorespiratory fitness, muscular fitness and mental health in older adolescents: A multi-level cross-sectional analysis. Prev. Med. 2020, 132, 105985. [Google Scholar] [CrossRef]
- Tapia-Serrano, M.A.; Jorge, M.-L.; David, S.-O.; Mikel, V.-S.; Sánchez-Miguel, P.A. Mediating effect of fitness and fatness on the association between lifestyle and body dissatisfaction in Spanish youth. Physiol. Behav. 2021, 232, 113340. [Google Scholar]
- Bermejo-Cantarero, A.; Álvarez-Bueno, C.; Martínez-Vizcaino, V.; Redondo-Tébar, A.; Pozuelo-Carrascosa, D.P.; Sánchez-López, M. Relationship between both cardiorespiratory and muscular fitness and health-related quality of life in children and adolescents: A systematic review and meta-analysis of observational studies. Health Qual. Life Outcomes 2021, 19, 127. [Google Scholar] [CrossRef]
- Appelqvist-Schmidlechner, K.; Vaara, J.P.; Vasankari, T.; Häkkinen, A.; Mäntysaari, M.; Kyröläinen, H. Muscular and cardiorespiratory fitness are associated with health-related quality of life among young adult men. BMC Public Heal. 2020, 20, 842. [Google Scholar] [CrossRef]
- Marković, L.; Jocić, J.T.; Horvatin, M.; Pekas, D.; Trajković, N. Cardiorespiratory Fitness and Health-Related Quality of Life in Secondary School Children Aged 14 to 18 Years: A Cross-Sectional Study. Healthcare 2022, 10, 660. [Google Scholar] [CrossRef] [PubMed]
- Kesztyüs, D.; Schreiber, A.; Kobel, S.; Wartha, O.; Kesztyüs, T.; Kilian, R.; Steinacker, J.M. Illness and determinants of health-related quality of life in a cross-sectional sample of schoolchildren in different weight categories. Ger. Med. Sci. 2014, 12, Doc04. [Google Scholar] [PubMed]
- Perez-Sousa, M.A.; Olivares, P.R.; Escobar-Alvarez, J.A.; Parraça, J.A.; Gusi, N. Fitness as mediator between weight status and dimensions of health-related quality of life. Health Qual. Life Outcomes 2018, 16, 155. [Google Scholar] [CrossRef]
- Griffiths, L.J.; Parsons, T.J.; Hill, A.J. Self-esteem and quality of life in obese children and adolescents: A systematic review. Int. J. Pediatr. Obes. 2010, 5, 282–304. [Google Scholar] [CrossRef]
- Mastorci, F.; Piaggi, P.; Doveri, C.; Trivellini, G.; Marinaro, I.; Casu, A.; Pingitore, A.; Vassalle, C. Relationship between weight status and health-related quality of life in a sample of early adolescents from Central and Northern Italy: A cross-sectional study of the AVATAR project participants. Int. J. Environ. Res. Public Health 2021, 18, 8782. [Google Scholar] [CrossRef]
- Arnaoutis, G.; Georgoulis, M.; Psarra, G.; Milkonidou, A.; Panagiotakos, D.B.; Kyriakou, D.; Bellou, E.; Tambalis, K.D.; Sidossis, L.S. Association of Anthropometric and Lifestyle Parameters with Fitness Levels in Greek Schoolchildren: Results from the EYZHN Program. Front. Nutr. 2018, 5, 10. [Google Scholar] [CrossRef] [PubMed]
- Palacio-Agüero, A.; Díaz-Torrente, X.; Quintiliano Scarpelli Dourado, D. Relative handgrip strength, nutritional status and abdominal obesity in Chilean adolescents. PLoS ONE 2020, 15, e0234316. [Google Scholar] [CrossRef]
- Gerber, M.; Ayekoé, S.; Bonfoh, B.; Coulibaly, J.T.; Daouda, D.; Gba, B.C.; Kouassi, B.; Traoré, S.G.; du Randt, R.; Nqweniso, S. Is grip strength linked to body composition and cardiovascular risk markers in primary schoolchildren? Cross-sectional data from three African countries. BMJ Open 2022, 12, e052326. [Google Scholar] [CrossRef]
- Kang, S.Y.; Lim, J.; Park, H.S. Relationship between low handgrip strength and quality of life in Korean men and women. Qual. Life Res. 2018, 27, 2571–2580. [Google Scholar] [CrossRef]
- Basterfield, L.; Burn, N.L.; Galna, B.; Karoblyte, G.; Weston, K.L. The association between physical fitness, sports club participation and body mass index on health-related quality of life in primary school children from a socioeconomically deprived area of England. Prev. Med. Rep. 2021, 24, 101557. [Google Scholar] [CrossRef]


| Total (n = 750) | Girls (n = 332) | Boys (n = 418) | p Value (F-value) | |
|---|---|---|---|---|
| Age (years) | 11.65 ± 1.13 | 11.62 ± 1.08 | 11.66 ± 1.16 | 0.637 (0.22) |
| Height (cm) | 155 ± 0.11 | 154 ± 0.09 | 156 ± 0.11 | 0.090 (7.13) |
| Body mass (kg) | 53.23 ± 14.40 | 52.82 ± 13.49 | 53.55 ± 15.09 | 0.494(0.47) |
| BMI (kg/m2) | 21.89 ± 4.63 | 22.10 ± 4.68 | 21.73 ± 4.59 | 0.273 (1.20) |
| WC (cm) | 74.21 ± 12.08 | 73.32 ± 11.44 | 74.92 ± 12.53 | 0.093 (2.83) |
| WtHR (WC/size) | 0.48 ± 0.07 | 0.48 ± 0.07 | 0.48 ± 0.07 | 0.443 (0.59) |
| Abdominal obesity | ||||
| No | 602 (80.3%) | 274 (82.5%) | 328 (78.5%) | p = 0.097 |
| Yes | 148 (19.7%) | 58 (17.5%) | 90 (21.5%) | |
| VO2max (ml/kg/min) | 44.34 ± 5.57 | 42.77 ± 4.63 | 45.57 ± 5.93 | p < 0.001 (49.94) |
| HGS (kg) | 23.84 ± 7.94 | 22.76 ± 7.91 | 24.71 ± 7.88 | p = 0.001 (11.33) |
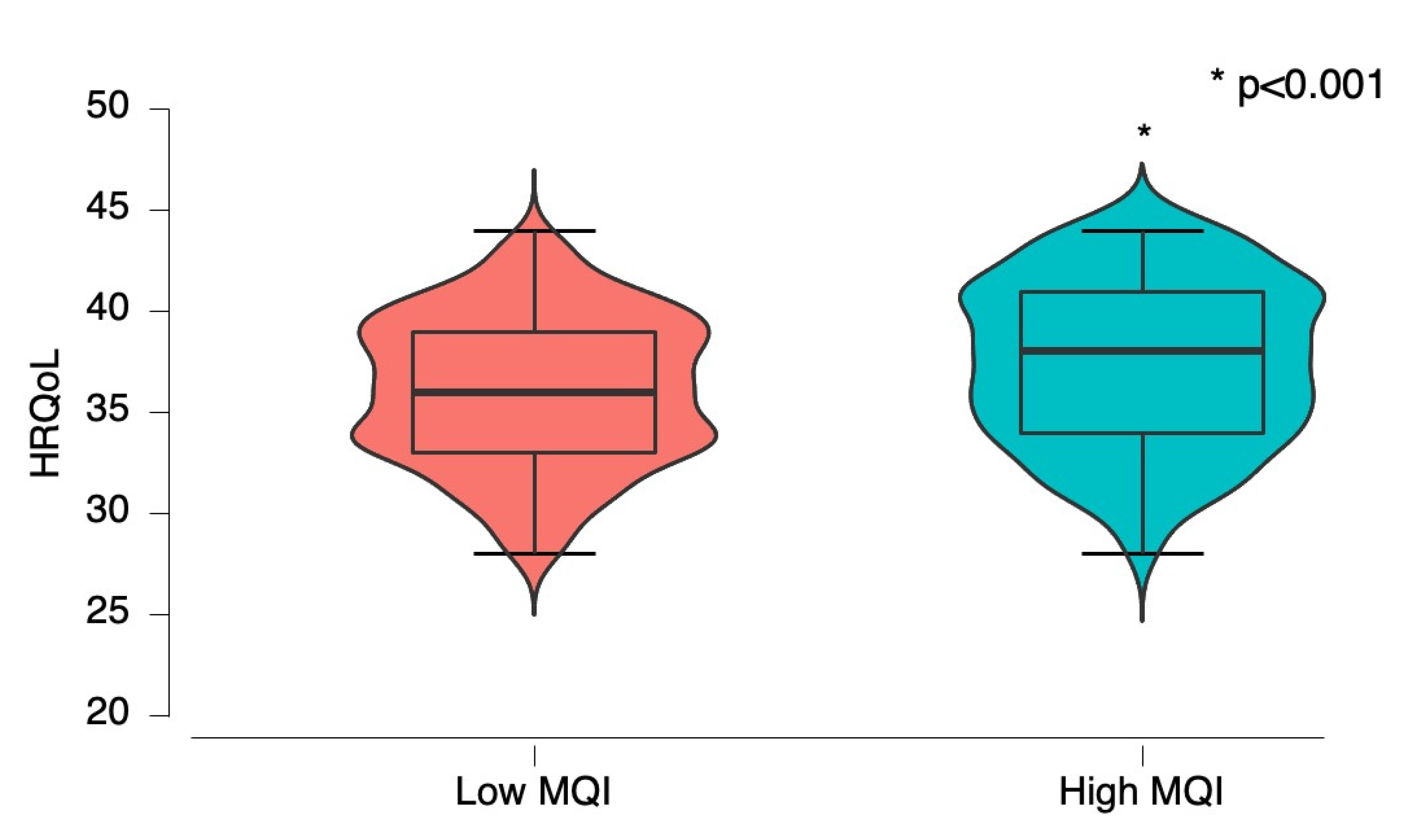
| MQI (HGS/BMI) | 1.14 ± 0.44 | 1.07 ± 0.42 | 1.19 ± 0.45 | p < 0.001 (13.00) |
| Low MQI | 373 (49.7%) | 184 (55.4%) | 189 (45.2%) | p = 0.003 |
| High MQI | 377 (50.3%) | 148 (44.6%) | 229 (54.8%) | |
| Screen time (h/day) | 3.39 ± 1.12 | 3.45 ± 1.14 | 3.34 ± 1.11 | 0.221 (1.50) |
| PA after school (h/week) | 2.45 ± 1.38 | 2.36 ± 1.32 | 2.51 ± 1.42 | 0.139 (2.19) |
| HRQoL (score) | 36.77 ± 3.87 | 36.76 ± 3.83 | 36.78 ± 3.91 | 0.940 (0.01) |
| BMI (kg/m2) | WtHR (WC/size) | VO2max (ml/kg/min) | Screen Time (h/day) | PA after School (h/week) | MQI (Ratio) | HRQoL (Score) | |
|---|---|---|---|---|---|---|---|
| BMI (kg/m2) | - | ||||||
| WtHR (WC/size) | 0.70 ** | ||||||
| VO2max (ml/kg/min) | −0.33 ** | −0.26 ** | |||||
| Screen time (h/day) | 0.20 ** | 0.15 ** | −0.14 ** | ||||
| PA after school (h/week) | −0.26 ** | −0.25 ** | 0.29 ** | −0.63 ** | |||
| MQI (ratio) | −0.50 ** | −0.30 ** | 0.31 ** | −0.10 ** | 0.17 ** | ||
| HRQoL (score) | −0.14 ** | −0.19 ** | 0.20 ** | −0.25 ** | 0.26 ** | 0.14 ** | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Delgado-Floody, P.; Gómez-López, M.; Caamaño-Navarrete, F.; Valdés-Badilla, P.; Jerez-Mayorga, D. The Mediating Role of the Muscle Quality Index in the Relation of Screen Time and Abdominal Obesity with Health-Related Quality of Life in Chilean Schoolchildren. Nutrients 2023, 15, 714. https://doi.org/10.3390/nu15030714
Delgado-Floody P, Gómez-López M, Caamaño-Navarrete F, Valdés-Badilla P, Jerez-Mayorga D. The Mediating Role of the Muscle Quality Index in the Relation of Screen Time and Abdominal Obesity with Health-Related Quality of Life in Chilean Schoolchildren. Nutrients. 2023; 15(3):714. https://doi.org/10.3390/nu15030714
Chicago/Turabian StyleDelgado-Floody, Pedro, Manuel Gómez-López, Felipe Caamaño-Navarrete, Pablo Valdés-Badilla, and Daniel Jerez-Mayorga. 2023. "The Mediating Role of the Muscle Quality Index in the Relation of Screen Time and Abdominal Obesity with Health-Related Quality of Life in Chilean Schoolchildren" Nutrients 15, no. 3: 714. https://doi.org/10.3390/nu15030714
APA StyleDelgado-Floody, P., Gómez-López, M., Caamaño-Navarrete, F., Valdés-Badilla, P., & Jerez-Mayorga, D. (2023). The Mediating Role of the Muscle Quality Index in the Relation of Screen Time and Abdominal Obesity with Health-Related Quality of Life in Chilean Schoolchildren. Nutrients, 15(3), 714. https://doi.org/10.3390/nu15030714











