Development and Rasch Analysis of the 18-Item Health Resilience Profile (HRP)
Abstract
:1. Introduction
2. Materials and Methods
2.1. Rasch Calibration Data Analysis
2.2. Study 1: Instrument Development and Evaluation
Participant Recruitment and Procedure
2.3. Measures
2.4. Profile by Sanford Health Coaching Program
3. Results
3.1. Model Data Fit
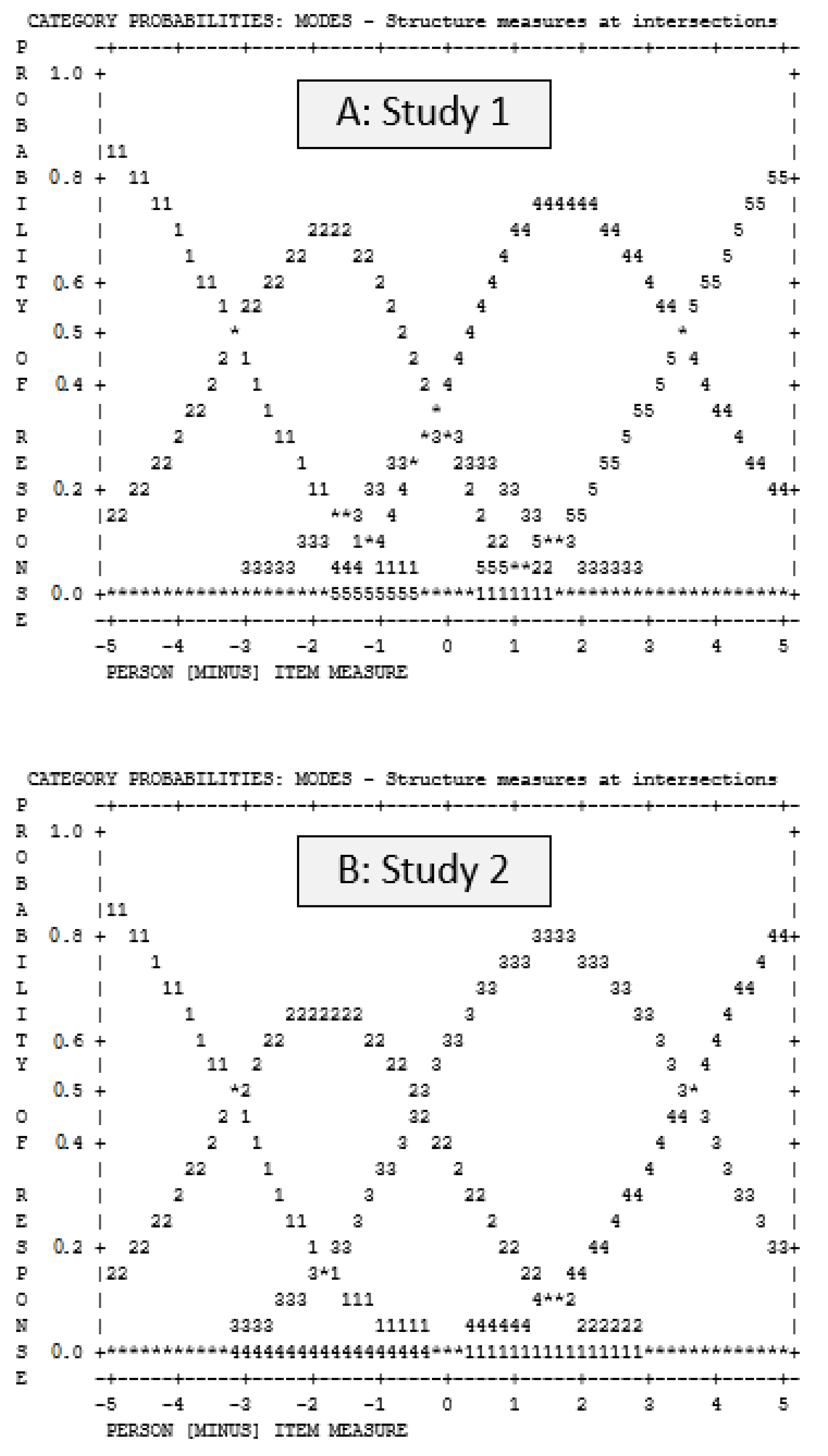
3.2. Rating Scale Functioning
3.3. Item-Person Map
3.4. Item Difficulty and Person Ability
3.5. Differential Item Functioning (DIF)
3.6. HRP Revisions Following Study 1
3.7. Study 2: Rasch Calibration of the HRP
3.7.1. Participant Recruitment and Procedure
3.7.2. Measures
3.8. Study 2: Health Resilience Profile (HRP-18)—Rasch Calibration
3.8.1. Model Data Fit
3.8.2. Rating Scale Function
3.8.3. Item-Person Map
3.8.4. Item Difficulty and Person Ability
3.8.5. Differential Item Functioning (DIF)
3.8.6. Validity Evidence
3.9. HRP Revisions Following Study 2
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Strongly Disagree (1) | Disagree (2) | Agree (3) | Strongly Agree (4) | |
|---|---|---|---|---|
| 1. I enjoy setting health goal(s) that challenge me | ||||
| 2. I can make difficult decisions to reach my health goal(s) when necessary | ||||
| 3. I stay focused on my health goal(s) even when feeling overwhelmed | ||||
| 4. I feel in control of my health goal(s) | ||||
| 5. I work to reach my health goal(s) no matter what roadblocks or challenges I come across in the process | ||||
| 6. Unpleasant feelings like sadness, anger, fear, and boredom get in the way of my health goal(s) | ||||
| 7. I give up on my health goal(s) when the challenges of everyday life get in the way | ||||
| 8. I tend to bounce back after experiencing setbacks | ||||
| 9. I believe I can achieve my health goal(s), even if there are obstacles | ||||
| 10. When I feel overwhelmed, I know how to get the help I need | ||||
| 11. I have confidence from past successes that impacts how I handle challenges and difficulties | ||||
| 12. I give my best effort to reach my health goal(s), no matter what happens | ||||
| 13. I feel a sense of pride when I reach a health goal | ||||
| 14. When unexpected challenges occur while pursuing my health goal(s), I know how to handle them | ||||
| 15. I am able to apply what I’ve learned from past failures | ||||
| 16. I believe past failures contribute to my growth | ||||
| 17. I get discouraged when I’m not making progress toward my health goal(s) | ||||
| 18. Outside factors keep me from pursuing my health goal(s) |
References
- An, S.; Song, R. Effects of health coaching on behavioral modification among adults with cardiovascular risk factors: Systematic review and meta-analysis. Patient Educ. Couns. 2020, 103, 2029–2038. [Google Scholar] [CrossRef] [PubMed]
- Leung, A.W.; Chan, R.S.; Sea, M.M.; Woo, J. An overview of factors associated with adherence to lifestyle modification programs for weight management in adults. Int. J. Environ. Res. Public Health 2017, 14, 922. [Google Scholar] [CrossRef]
- Soutenberg, M.; Stanzilis, K.; Falcon, A. Translation of lifestyle modification programs focused on physical activity and dietary habits delivered in community settings. Int. J. Behav. Med. 2015, 22, 312–327. [Google Scholar] [CrossRef] [PubMed]
- Baekeland, F.; Lundwall, L. Dropping out of treatment: A critical review. Psychol. Bull. 1975, 82, 738. [Google Scholar] [CrossRef]
- Meyerowitz-Katz, G.; Ravi, S.; Arnolda, L.; Feng, X.; Maberly, G.; Astell-Burt, T. Rates of attrition and dropout in app-based interventions for chronic disease: Systematic review and meta-analysis. J. Med. Int. Res. 2020, 22, e20283. [Google Scholar] [CrossRef]
- Silberman, J.M.; Kaur, M.; Sletteland, J.; Vekatesan, A. Outcomes in a digital weight management intervention with one-on-one health coaching. PLoS ONE 2020, 15, e0232221. [Google Scholar] [CrossRef] [PubMed]
- Block, J.; Kremen, A.M. IQ and ego-resiliency: Conceptual and empirical connections and separateness. J. Pers. Soc. Psychol. 1996, 70, 349. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, R.S. From psychological stress to the emotions: A history of changing outlooks. Annu. Rev. Psychol. 1993, 44, 1–21. [Google Scholar] [CrossRef]
- Windle, G. What is resilience? A review and concept analysis. Rev. Clin. Gerontol. 2011, 21, 152–169. [Google Scholar] [CrossRef]
- Green, S.; Spence, G.B. Positive Psychological Intervention. In The Wiley Blackwell Handbook of Positive Psychological Interventions, 1st ed.; Parks, A.C., Schueller, S.M., Eds.; Wiley Blackwell: Malden, MA, USA, 2014; Volume 1, pp. 273–285. [Google Scholar] [CrossRef]
- Karoly, P. Mechanisms of self-regulation: A view. Annu. Rev. Psychol. 1993, 44, 23–52. [Google Scholar] [CrossRef]
- Duckworth, A.L.; Peterson, C.; Matthews, M.D.; Kelly, D.R. Grit: Perseverance and passion for long-term goals. J. Pers. Soc. Psychol. 2007, 92, 1087. [Google Scholar] [CrossRef]
- Duckworth, A.L.; Quinn, P.D. Development and validation of the Short Grit Scale (GRIT–S). J. Pers. Assess. 2009, 91, 166–174. [Google Scholar] [CrossRef]
- Stoffel, J.M.; Cain, J. Review of grit and resilience literature within health professions education. Am. J. Pharm. Educ. 2018, 82, 124–135. [Google Scholar] [CrossRef] [PubMed]
- Grant, A.M.; Curtayne, L.; Burton, G. Executive coaching enhances goal attainment, resilience and workplace well-being: A randomised controlled study. J. Posit. Psychol. 2009, 4, 396–407. [Google Scholar] [CrossRef]
- Sherlock-Storey, M.; Moss, M.; Timson, S. Brief coaching for resilience during organisational change—An exploratory study. Coach. Psychol. 2013, 9, 19–26. [Google Scholar] [CrossRef]
- Lee, J.A.; Heberlein, E.; Pyle, E.; Caughlan, T.; Rahaman, D.; Sabin, M.; Kaar, J.L. Evaluation of a resiliency focused health coaching intervention for middle school students: Building resilience for healthy kids program. Am. J. Health Promot. 2021, 35, 344–351. [Google Scholar] [CrossRef] [PubMed]
- Graziani, G.; Aylward, B.S.; Kunkle, S.; Shih, E. Changes in Resilience Following Engagement with a Virtual Mental Health System: Real-world Observational Study. JMIR Form. Res. 2022, 6, e37169. [Google Scholar] [CrossRef] [PubMed]
- Kleine, H.D.; McCormack, L.A.; Drooger, A.; Meendering, J.R. Barriers to and facilitators of weight management in adults using a meal replacement program that includes health coaching. J. Prim. Care Comm. Health 2019, 10, 2150132719851643. [Google Scholar] [CrossRef] [PubMed]
- Andrich, D. Controversy and the Rasch model: A characteristic of incompatible paradigms? Med. Care 2004, 42, I7–I16. [Google Scholar] [CrossRef] [PubMed]
- Rasch, G. Probabilistic Models for Some Intelligence and Achievement Tests; Danish Institute for Educational Research: Copenhagen, Denmark, 1960. [Google Scholar]
- Tennant, A.; Conaghan, P.G. The Rasch measurement model in rheumatology: What is it and why use it? When should it be applied, and what should one look for in a Rasch paper? Arthritis Care Res. 2007, 57, 1358–1362. [Google Scholar] [CrossRef]
- Bond, T.G.; Yan, Z.; Heene, M. Applying the Rasch Model: Fundamental Measurement in the Human Sciences, 4th ed.; Routledge: New York, NY, USA, 2020. [Google Scholar] [CrossRef]
- Connor, K.M.; Davidson, J.R. Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC). Depress. Anxiety 2003, 18, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Hjemdal, O.; Friborg, O.; Martinussen, M.; Rosenvinge, J.H. Preliminary results from the development and validation of a Norwegian scale for measuring adult resilience. J. Nor. Psychol. Assoc. 2001, 38, 310–317. [Google Scholar]
- Papini, N.M.; Kang, M.; Ryu, S.; Griese, E.; Wingert, T.; Herrmann, S.D. Rasch calibration of the 25-item Connor-Davidson resilience scale. J. Health Psychol. 2020, 26, 1976–1987. [Google Scholar] [CrossRef]
- Arias González, V.B.; Crespo Sierra, M.T.; Arias Martínez, B.; Martínez-Molina, A.; Ponce, F.P. An in-depth psychometric analysis of the Connor-Davidson Resilience Scale: Calibration with Rasch-Andrich model. Health Qual. Life Outcomes 2015, 13, 154. [Google Scholar] [CrossRef]
- Niederberger, M.; Spranger, J. Delphi technique in health sciences: A map. Front. Public Health 2020, 8, 457. [Google Scholar] [CrossRef] [PubMed]
- Linacre, J.M. What do infit and outfit, mean-square and standardized mean. Rasch Meas. Trans. 2002, 16, 878. [Google Scholar]
- Linacre, J.M. Winsteps® Rasch Measurement Computer Program User’s Guide; Winsteps.com: Portland, OR, USA, 2021; Available online: https://www.winsteps.com/ (accessed on 19 February 2007).
- Linacre, J.M. Optimizing rating scale category effectiveness. J. Appl. Meas. 2002, 3, 85–106. [Google Scholar] [PubMed]
- Cohen, S.; Williamson, G. Perceived stress in a probability sample of the United States. In The Social Psychology of Health: Claremont Symposium on Applied Social Psychology; Spacapan, S., Oskamp, S., Eds.; Sage: Newbury Park, CA, USA, 1988; pp. 31–67. [Google Scholar]
- Jackson, A.W.; Morrow, J.R.; Bowles, H.R.; FitzGerald, S.J.; Blair, S.N. Construct validity evidence for single-response items to estimate physical activity levels in large sample studies. Res. Q. Exerc. Sport 2013, 78, 24–31. [Google Scholar] [CrossRef]
- Lee, E.H. Review of the psychometric evidence of the perceived stress scale. Asian Nurs. Res. 2012, 6, 121–127. [Google Scholar] [CrossRef]
- Andreou, E.; Alexopoulos, E.C.; Lionis, C.; Varvogli, L.; Gnardellis, C.; Chrousos, G.P.; Darviri, C. Perceived stress scale: Reliability and validity study in Greece. Int. J. Environ. Res. Public Health 2011, 8, 3287–3298. [Google Scholar] [CrossRef]
- Chen, L.; Zhu, H.; Harshfield, G.A.; Treiber, F.A.; Pollock, J.S.; Pollock, D.; Okereke, O.I.; Shaoyong, S.; Dong, Y. Serum 25-hydroxyvitamin D concentrations are associated with mental health and psychosocial stress in young adults. Nutrients 2020, 12, 1938. [Google Scholar] [CrossRef] [PubMed]
- Katsarou, A.; Panagiotakos, D.; Zafeiropoulou, A.; Vryonis, M.; Skoularigis, I.; Tryposkiadis, F.; Papageorgiou, C. Validation of a Greek version of PSS-14; a global measure of perceived stress. Cent. Eur. J. Public Health 2012, 20, 104–109. [Google Scholar] [CrossRef]
- Bell, M.; Reed, V.; Wernisch, J.; Papini, N.M.; Herrmann, S.D. Effectiveness of profile by Sanford behavioral weight loss program for weight loss following endometrial cancer treatment. Gynecol. Oncol. Rep. 2021, 38, 100897. [Google Scholar] [CrossRef]
- JaKa, M.M.; Dinh, J.M.; Rivard, R.L.; Herrmann, S.D.; Spoonheim, J.; Pronk, N.P.; Ziegenfuss, J.Y. Pragmatic evaluation of a health system-based employee weight management program. Int. J. Environ. Res. Public Health 2021, 18, 5901. [Google Scholar] [CrossRef]
- Morrow, J.R.; Mood, D.P.; Zhu, W.; Kang, M. Measurement and Evaluation in Human Performance, 6th ed.; Human Kinetics Publisher: Champaign, IL, USA, 2023. [Google Scholar]
- García-León, M.Á.; Pérez-Mármol, J.M.; Gonzalez-Pérez, R.; del Carmen García-Ríos, M.; Peralta-Ramírez, M.I. Relationship between resilience and stress: Perceived stress, stressful life events, HPA axis response during a stressful task and hair cortisol. Physiol. Behav. 2019, 202, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Lines, R.L.; Ducker, K.J.; Ntoumanis, N.; Thøgersen-Ntoumani, C.; Fletcher, D.; McGarry, S.; Gucciardi, D.F. Stress, physical activity, and resilience resources: Tests of direct and moderation effects in young adults. Sport Exerc. Perform 2020, 9, 418. [Google Scholar] [CrossRef]
- Salisu, I.; Hashim, N. A critical review of scales used in resilience research. IOSR J. Bus. Manag. 2017, 19, 23–33. [Google Scholar] [CrossRef]
- Goins, R.T.; Gregg, J.J.; Fiske, A. Psychometric properties of the Connor-Davidson resilience scale with older American Indians: The native elder care study. Res. Aging 2013, 35, 123–143. [Google Scholar] [CrossRef]
- Palacio, G.C.; Krikorian, A.; Gómez-Romero, M.J.; Limonero, J.T. Resilience in Caregivers: A Systematic Review. Am. J. Hosp. Care 2020, 37, 648–658. [Google Scholar] [CrossRef]
- Chmitorz, A.; Kunzler, A.; Helmreich, I.; Tüscher, O.; Kalisch, R.; Kubiak, T.; Wessa, M.; Lieb, K. Intervention studies to foster resilience–A systematic review and proposal for a resilience framework in future intervention studies. Clin. Psychol. Rev. 2018, 59, 78–100. [Google Scholar] [CrossRef]
- Southwick, S.M.; Charney, D.S. Resilience: The Science of Mastering Life’s Greatest Challenges. Cambridge University Press: Cambridge, UK, 2018. [Google Scholar]
- Ferreira, M.; Marques, A.; Gomes, P.V. Individual Resilience Interventions: A Systematic Review in Adult Population Samples over the Last Decade. Int. J. Environ. Res. Public Health 2021, 18, 7564. [Google Scholar] [CrossRef] [PubMed]
- Reyes, A.T.; Muthukumar, V.; Bhatta, T.R.; Bombard, J.N.; Gangozo, W.J. Promoting resilience among college student veterans through an acceptance-and-commitment-therapy app: An intervention refinement study. Comm. Ment. Health J. 2020, 56, 1206–1214. [Google Scholar] [CrossRef] [PubMed]
- Vaughan-Horrocks, H.; Reagon, C.; Seymour, A. The experiences of veterans with mental health problems participating in an occupational therapy and resilience workshop intervention: An exploratory study. Br. J. Occup. Ther. 2021, 84, 531–540. [Google Scholar] [CrossRef]
- Cleary, M.; Kornhaber, R.; Thapa, D.K.; West, S.; Visentin, D. The effectiveness of interventions to improve resilience among health professionals: A systematic review. Nurs. Educ. Today 2018, 71, 247–263. [Google Scholar] [CrossRef] [PubMed]
- Shin, J.Y.; Choi, S.W. Online interventions geared toward increasing resilience and reducing distress in family caregivers. Curr. Opin. Support. Palliat. Care 2020, 14, 60–66. [Google Scholar] [CrossRef] [PubMed]
- Ludolph, P.; Kunzler, A.M.; Stoffers-Winterling, J.; Helmreich, I.; Lieb, K. Interventions to promote resilience in cancer patients. Dtsch. Ärzteblatt Int. 2019, 116, 865. [Google Scholar] [CrossRef]
- Lee, J.A.; Heberlein, E.; Pyle, E.; Caughlan, T.; Rahaman, D.; Sabin, M.; Kaar, J.L. Study protocol for a school-based single group pragmatic trial to promote resilience in youth: Building resilience for Healthy Kids. Contemp. Clin. Trials Comm. 2021, 21, 100721. [Google Scholar] [CrossRef]
- Kaye-Kauderer, H.; Feingold, J.H.; Feder, A.; Southwick, S.; Charney, D. Resilience in the age of COVID-19. BJPsych Adv. 2021, 27, 166–178. [Google Scholar] [CrossRef]
- Ungar, M. Resilience across cultures. Br. J. Soc. Work 2008, 38, 218–235. [Google Scholar] [CrossRef]
- Vinkers, C.H.; van Amelsvoort, T.; Bisson, J.I.; Branchi, I.; Cryan, J.F.; Domschke, K.; Howes, O.D.; Manchia, M.; Pinto, L.; de Quervain, D.; et al. Stress resilience during the coronavirus pandemic. Eur. Neuropsychopharmacol. 2020, 35, 12–16. [Google Scholar] [CrossRef]
- Czajkowski, S.M.; Lynch, M.R.; Hall, K.L.; Stipelman, B.A.; Haverkos, L.; Perl, H.; Scott, M.S.; Shirley, M.C. Transdisciplinary translational behavioral (TDTB) research: Opportunities, barriers, and innovations. Transl. Behav. Med. 2016, 6, 32–43. [Google Scholar] [CrossRef] [PubMed]
- Tsai, J.; Freedland, K.E. Introduction to the special section: Resilience for physical and behavioral health. Health Psychol. 2022, 41, 243. [Google Scholar] [CrossRef] [PubMed]
- Kermott, C.A.; Johnson, R.E.; Sood, R.; Jenkins, S.M.; Sood, A. Is higher resilience predictive of lower stress and better mental health among corporate executives? PLoS ONE 2019, 14, e0218092. [Google Scholar] [CrossRef] [PubMed]
- Farewell, C.V.; Jewell, J.; Walls, J.; Leiferman, J.A. A mixed-methods pilot study of perinatal risk and resilience during COVID-19. J. Prim. Care Comm. Health 2020, 11, 2150132720944074. [Google Scholar] [CrossRef]
- Ferreira, R.J.; Buttell, F.; Cannon, C. COVID-19: Immediate predictors of individual resilience. Sustainability 2020, 12, 6495. [Google Scholar] [CrossRef]
- Jacob, C.M.; Briana, D.D.; Di Renzo, G.C.; Modi, N.; Bustreo, F.; Conti, G.; Malamitsi-Puchner, A.; Hanson, M. Building resilient societies after COVID-19: The case for investing in maternal, neonatal, and child health. Lancet Public Health 2020, 5, e624–e627. [Google Scholar] [CrossRef]
- Penkler, M.; Müller, R.; Kenney, M.; Hanson, M. Back to normal? Building community resilience after COVID-19. Lancet Diabetes Endocrinol. 2020, 8, 664–665. [Google Scholar] [CrossRef]

| Characteristics | Study 1 n = 427 | Study 2 n = 493 | ||
|---|---|---|---|---|
| M ± SD | % | M ± SD | % | |
| Age (years) | 44.46 ± 11.93 | 12.2% (52) missing | 49.76 ± 12.53 | |
| Young adults (18–35 years) | 22.2% | 15.6% | ||
| Middle-aged adults (36–55 years) | 45.7% | 48.7% | ||
| Older adults (≥56 years) | 19.9% | 35.7% | ||
| Sex (%) | 12.2% (52) missing | |||
| Male | 4% | 37.7% | ||
| Female | 83.8% | 62.1% | ||
| Prefer not to answer | 0.2% | |||
| BMI (kg/m2) | ||||
| Non-obese (38.3%) | 26.43 ± 2.41 | 26.53 ± 2.52 | ||
| Obese (61.7%) | 37.11 ± 6.28 | 36.46 ± 5.34 | ||
| Alcohol usage | 12.4% (53) missing | |||
| Yes | 37.9% | 44.2% | ||
| No | 49.6% | 55.8% | ||
| Category Score | Counts Used | Average Measure | Outfit MNSQ | Category Thresholds |
|---|---|---|---|---|
| Study 1 | ||||
| 1 | 265 | −2.06 | 1.26 | None |
| 2 | 1462 | −0.81 | 1.02 | −3.16 |
| 3 * | 1154 | 0.26 | 0.86 | 0.01 * |
| 4 * | 3940 | 1.53 | 1.01 | −0.34 * |
| 5 * | 1273 | 3.35 | 1.02 | 3.50 * |
| Study 2 | ||||
| 1 | 331 | −1.85 | 1.64 | None |
| 2 | 1907 | −0.68 | 0.81 | −3.18 |
| 3 | 4760 | 1.54 | 0.98 | −0.41 |
| 4 | 1822 | 3.91 | 1.01 | 3.59 |
| Item | Calibration Logits | SE Logits | Infit MNSQ | Outfit MNSQ |
|---|---|---|---|---|
| Q22. I get discouraged when I’m not making progress toward my health goal(s) | 3.15 | 0.08 | 1.33 | 1.29 |
| Q7. Unpleasant feelings like sadness, anger, fear, and boredom get in the way of my health goal(s) | 2.23 | 0.07 | 1.26 | 1.31 |
| Q4. I stay focused on my health goal(s) even when feeling overwhelmed | 1.19 | 0.06 | 0.97 | 0.99 |
| Q23. Outside factors keep me from pursuing my health goal(s) | 1.18 | 0.06 | 1.05 | 1.10 |
| Q9. I give up on my health goal(s) when the challenges of everyday life get in the way | 0.84 | 0.06 | 0.84 | 0.89 |
| Q6. I work to reach my health goal(s) no matter what roadblocks or challenges I come across in the process | 0.56 | 0.07 | 0.94 | 0.96 |
| Q17. When unexpected challenges occur while pursuing my health goal(s), I know how to handle them | 0.47 | 0.07 | 0.72 | 0.73 |
| Q14. I give my best effort to reach my health goal(s), no matter what happens | 0.27 | 0.07 | 0.94 | 0.98 |
| Q5. I feel in control of my health goal(s) | 0.16 | 0.07 | 0.88 | 0.89 |
| Q12. When I feel overwhelmed, I know how to get the help I need | −0.12 | 0.07 | 1.02 | 1.04 |
| Q3. I can make difficult decisions to reach my health goal(s) when necessary | −0.29 | 0.07 | 0.82 | 0.84 |
| Q10. I tend to bounce back after experiencing setbacks | −0.34 | 0.07 | 1.07 | 1.13 |
| Q13. I have confidence from past successes that impacts how I handle challenges and difficulties | −0.38 | 0.07 | 0.93 | 0.99 |
| Q2. I enjoy setting health goal(s) that challenge me | −0.39 | 0.07 | 1.21 | 1.32 |
| Q11. I believe I can achieve my health goal(s), even if there are obstacles | −0.73 | 0.08 | 0.83 | 0.77 |
| Q19. I am able to apply what I’ve learned from past failures | −0.92 | 0.08 | 0.79 | 0.79 |
| Q20. I believe past failures contribute to my growth | −1.17 | 0.19 | 0.98 | 1.03 |
| Q21. The actions I take daily impact my health | −2.54 | 0.10 | 1.11 | 1.10 |
| Q15. I feel a sense of pride when I reach a health goal | −3.18 | 0.11 | 1.13 | 1.08 |
| Item | Modification | Rationale |
|---|---|---|
| 16. I am my biggest critic when it comes to my health goal(s) | Item removed | Item demonstrated poor infit/outfit statistics in study 1 |
| 1. I am not easily discouraged by failure | Item removed | Item demonstrated poor infit/outfit statistics in study 1 |
| 8. My health goal(s) are connected to my purpose in life | Item removed | Item demonstrated poor infit/outfit statistics in study 1 |
| 18. I have people I can rely on to support me when I need it | Item removed | Item demonstrated poor infit/outfit statistics in study 1 |
| 5-point Likert response | Changed from a 5-point to a 4-point response | The 5-point response did not perform well. As such, the “neither agree nor disagree” response was removed in study 2 to create a 4-point Likert scale. |
| Item # | Item | Calibration Logits (SE) | Infit MNSQ | Outfit MNSQ |
|---|---|---|---|---|
| 18 | I get discouraged when I’m not making progress toward my health goal(s) | 3.40 (0.08) | 1.26 | 1.31 |
| 6 | Unpleasant feelings like sadness, anger, fear, and boredom get in the way of my health goal(s) | 2.32 (0.08) | 1.36 | 1.41 |
| 19 | Outside factors keep me from pursuing my health goal(s) | 1.40 (0.08) | 1.23 | 1.30 |
| 3 | I stay focused on my health goal(s) even when feeling overwhelmed | 1.12 (0.08) | 0.84 | 0.84 |
| 7 | I give up on my health goal(s) when the challenges of everyday life get in the way | 0.82 (0.09) | 0.99 | 1.02 |
| 5 | I work to reach my health goal(s) no matter what roadblocks or challenges I come across in the process | 0.74 (0.09) | 0.90 | 0.89 |
| 12 | I give my best effort to reach my health goal(s), no matter what happens | 0.38 (0.09) | 0.77 | 0.74 |
| 14 | When unexpected challenges occur while pursuing my health goal(s), I know how to handle them | 0.25 (0.09) | 0.59 | 0.59 |
| 4 | I feel in control of my health goal(s) | −0.04 (0.09) | 0.90 | 0.94 |
| 10 | When I feel overwhelmed, I know how to get the help I need | −0.31 (0.09) | 1.07 | 1.03 |
| 8 | I tend to bounce back after experiencing setbacks | −0.53 (0.09) | 1.05 | 1.07 |
| 11 | I have confidence from past successes that impacts how I handle challenges and difficulties | −0.75 (0.09) | 0.86 | 0.80 |
| 2 | I can make difficult decisions to reach my health goal(s) when necessary | −0.85 (0.09) | 0.84 | 0.80 |
| 9 | I believe I can achieve my health goal(s), even if there are obstacles | −0.93 (0.09) | 0.81 | 0.77 |
| 15 | I am able to apply what I’ve learned from past failures | −0.95 (0.09) | 0.75 | 0.74 |
| 1 | I enjoy setting health goal(s) that challenge me | −0.98 (0.09) | 1.45 | 1.47 |
| 16 | I believe past failures contribute to my growth | −1.50 (0.09) | 0.91 | 1.02 |
| 13 | I feel a sense of pride when I reach a health goal | −3.57 (0.09) | 1.29 | 1.39 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Papini, N.M.; Jung, M.; Kang, M.; Lopez, N.V.; Herrmann, S.D. Development and Rasch Analysis of the 18-Item Health Resilience Profile (HRP). Nutrients 2023, 15, 807. https://doi.org/10.3390/nu15040807
Papini NM, Jung M, Kang M, Lopez NV, Herrmann SD. Development and Rasch Analysis of the 18-Item Health Resilience Profile (HRP). Nutrients. 2023; 15(4):807. https://doi.org/10.3390/nu15040807
Chicago/Turabian StylePapini, Natalie M., Myungjin Jung, Minsoo Kang, Nanette V. Lopez, and Stephen D. Herrmann. 2023. "Development and Rasch Analysis of the 18-Item Health Resilience Profile (HRP)" Nutrients 15, no. 4: 807. https://doi.org/10.3390/nu15040807
APA StylePapini, N. M., Jung, M., Kang, M., Lopez, N. V., & Herrmann, S. D. (2023). Development and Rasch Analysis of the 18-Item Health Resilience Profile (HRP). Nutrients, 15(4), 807. https://doi.org/10.3390/nu15040807






