GLIM Criteria for Assessment of Malnutrition in Saudi Patients with Type 2 Diabetes
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample Selection and Study Design
2.2. Nutrition Screening and Assessment
2.2.1. Subjective Global Assessment
2.2.2. Nutrition Risk Screening 2002
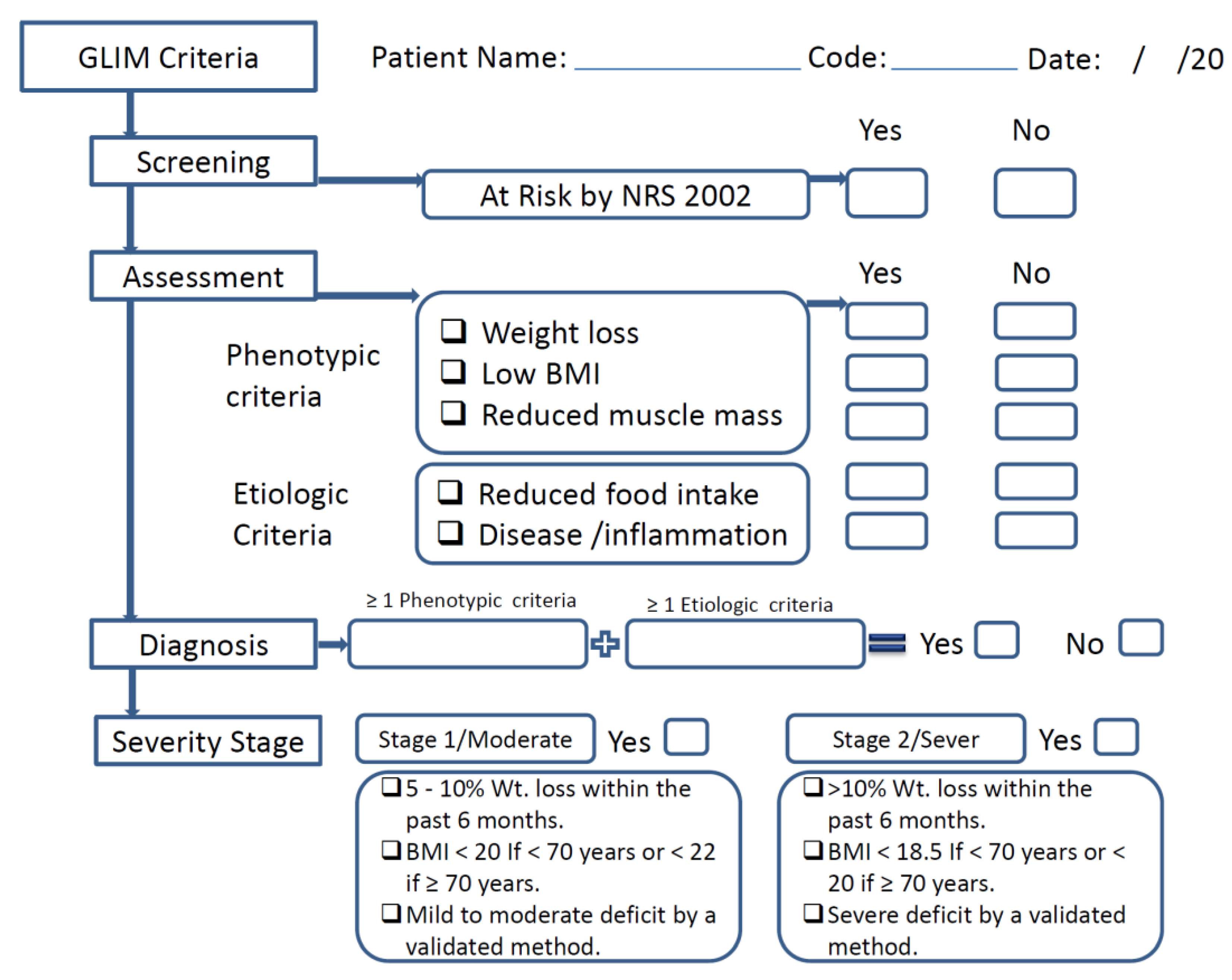
2.2.3. GLIM Criteria
2.3. Body Mass Index, Fat Mass, and Muscle Mass
2.4. Biochemical Data and Information Related to T2DM
2.5. Statistical Analysis
3. Results
3.1. Characteristics and Nutritional Status of Patients with T2DM
3.2. Anthropometric Characteristics of Patients with T2DM According to the GLIM and SGA
3.3. Comorbidities, Complications, and Medication of Patients with T2DM According to the GLIM Criteria and the SGA
3.4. Concurrent Validity of GLIM Criteria
3.5. Prevalence of GLIM Criteria in Patients with T2DM
3.6. GLIM Criteria and T2DM Complications
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sun, H.; Saeedi, P.; Karuranga, S.; Pinkepank, M.; Ogurtsova, K.; Duncan, B.B.; Stein, C.; Basit, A.; Chan, J.C.N.; Mbanya, J.C.; et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res. Clin. Pract. 2022, 183, 109119. [Google Scholar] [CrossRef]
- Whiting, D.R.; Guariguata, L.; Weil, C.; Shaw, J. IDF Diabetes Atlas: Global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res. Clin. Pract. 2011, 94, 311–321. [Google Scholar] [CrossRef] [PubMed]
- Harding, J.L.; Pavkov, M.E.; Magliano, D.J.; Shaw, J.E.; Gregg, E.W. Global trends in diabetes complications: A review of current evidence. Diabetologia 2019, 62, 3–16. [Google Scholar] [CrossRef]
- World Health Organization. Malnutrition Fact Sheets. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/malnutritio (accessed on 12 March 2022).
- Armstrong, D.G.; Hanft, J.R.; Driver, V.R.; Smith, A.P.S.; Lazaro-Martinez, J.L.; Reyzelman, A.M.; Furst, G.J.; Vayser, D.J.; Cervantes, H.L.; Snyder, R.J.; et al. Effect of oral nutritional supplementation on wound healing in diabetic foot ulcers: A prospective randomized controlled trial. Diabet. Med. 2014, 31, 1069–1077. [Google Scholar] [CrossRef] [PubMed]
- Kondrup, J.; Ramussen, H.H.; Hamberg, O.; Stanga, Z.; Camilo, M.; Richardson, R.; Elia, M.; Allison, S.; Meier, R.; Plauth, M. Nutritional risk screening (NRS 2002): A new method based on an analysis of controlled clinical trials. Clin. Nutr. 2003, 22, 321–336. [Google Scholar] [CrossRef] [PubMed]
- Tran, Q.C.; Banks, M.; Hannan-Jones, M.; Do, T.N.D.; Gallegos, D. Validity of four nutritional screening tools against subjective global assessment for inpatient adults in a low-middle income country in Asia. Eur. J. Clin. Nutr. 2018, 72, 979–985. [Google Scholar] [CrossRef]
- Bolayir, B.; Arik, G.; Yeşil, Y.; Kuyumcu, M.E.; Varan, H.D.; Kara, Ö.; Güngör, A.E.; Yavuz, B.B.; Cankurtaran, M.; Halil, M.G. Validation of Nutritional Risk Screening-2002 in a Hospitalized Adult Population. Nutr. Clin. Pract. 2019, 34, 297–303. [Google Scholar] [CrossRef]
- Cuong, T.Q.; Banks, M.; Hannan-Jones, M.; Thi Ngoc Diep, D.; Gallegos, D. Validity, reliability and feasibility of nutrition screening tools NRS-2002 and MST administered by trained medical doctors in routine practice. Hosp. Pract. 2019, 47, 259–266. [Google Scholar] [CrossRef]
- Detsky, A.S.; Mclaughlin, J.; Baker, J.P.; Johnston, N.; Whittaker, S.; Mendelson, R.A.; Jeejeebhoy, K.N. What is subjective global assessment of nutritional status? J. Parenter. Enter. Nutr. 1987, 11, 8–13. [Google Scholar] [CrossRef]
- Barbosa-Silva, M.C.G.; Barros, A.J.D. Indications and limitations of the use of subjective global assessment in clinical practice: An update. Curr. Opin. Clin. Nutr. Metab. Care 2006, 9, 263–269. [Google Scholar] [CrossRef]
- Cederholm, T.; Jensen, G.L.; Correia, M.I.T.D.; Gonzalez, M.C.; Fukushima, R.; Higashiguchi, T.; Baptista, G.; Barazzoni, R.; Blaauw, R.; Coats, A.; et al. GLIM criteria for the diagnosis of malnutrition—A consensus report from the global clinical nutrition community. Clin. Nutr. 2019, 38, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Zugasti-Murillo, A.; Estrella Petrina-Jáuregui, M.; Ripa-Ciáurriz, C.; Sánchez-Sánchez, R.; Villazón-González, F.; González-Díaz Faes, Á.; Fernández-López, C.; Calles-Romero, L.; Martín-Palmero, Á.; Riestra-Fernández, M.; et al. Nutrición Hospitalaria Trabajo Original Valoración nutricional SeDREno study-Prevalence of hospital malnutrition according to GLIM criteria, ten years after the PREDyCES study Estudio SeDREno: Prevalencia de la desnutrición hospitalaria según los criterios GLIM, diez años después del estudio PREDyCES. Nutr. Hosp. 2021, 38, 1016–1025. [Google Scholar] [CrossRef] [PubMed]
- Barazzoni, R.; Jensen, G.L.; Correia, M.I.T.D.; Gonzalez, M.C.; Higashiguchi, T.; Shi, H.P.; Bischoff, S.C.; Boirie, Y.; Carrasco, F.; Cruz-Jentoft, A.; et al. Guidance for assessment of the muscle mass phenotypic criterion for the Global Leadership Initiative on Malnutrition (GLIM) diagnosis of malnutrition. Clin. Nutr. 2022, 41, 1425–1433. [Google Scholar] [CrossRef]
- Zahorec, R. Neutrophil-to-lymphocyte ratio, past, present and future perspectives. Bratisl. Med. J. 2021, 122, 474–488. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Baeyens, J.P.; Bauer, J.M.; Boirie, Y.; Cederholm, T.; Landi, F.; Martin, F.C.; Michel, J.P.; Rolland, Y.; Schneider, S.M.; et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 2010, 39, 412–423. [Google Scholar] [CrossRef]
- de van der Schueren, M.A.E.; Keller, H.; Cederholm, T.; Barazzoni, R.; Compher, C.; Correia, M.I.T.D.; Gonzalez, M.C.; Jager-Wittenaar, H.; Pirlich, M.; Steiber, A.; et al. Global Leadership Initiative on Malnutrition (GLIM): Guidance on validation of the operational criteria for the diagnosis of protein-energy malnutrition in adults. Clin. Nutr. 2020, 39, 2872–2880. [Google Scholar] [CrossRef]
- Vural Keskinler, M.; Feyİzoglu, G.; Yildiz, K.; Oguz, A. The Frequency of Malnutrition in Patients with Type 2 Diabetes. Medeni. Med. J. 2021, 36, 117–122. [Google Scholar] [CrossRef]
- Sharma, K.; Mogensen, K.M.; Robinson, M.K. Under-Recognizing Malnutrition in Hospitalized Obese Populations: The Real Paradox. Curr. Nutr. Rep. 2019, 8, 317–322. [Google Scholar] [CrossRef]
- Cederholm, T.; Barazzoni, R.; Austin, P.; Ballmer, P.; Biolo, G.; Bischoff, S.C.; Compher, C.; Correia, I.; Higashiguchi, T.; Holst, M.; et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin. Nutr. 2017, 36, 49–64. [Google Scholar] [CrossRef]
- Balci, C.; Bolayir, B.; Eşme, M.; Arik, G.; Kuyumcu, M.E.; Yeşil, Y.; Varan, H.D.; Kara, Ö.; Güngör, A.E.; Doğu, B.B.; et al. Comparison of the Efficacy of the Global Leadership Initiative on Malnutrition Criteria, Subjective Global Assessment, and Nutrition Risk Screening 2002 in Diagnosing Malnutrition and Predicting 5-Year Mortality in Patients Hospitalized for Acute Illnesses. J. Parenter. Enter. Nutr. 2021, 45, 1172–1180. [Google Scholar] [CrossRef] [PubMed]
- Shahbazi, S.; Hajimohammadebrahim-Ketabforoush, M.; Vahdat Shariatpanahi, M.; Shahbazi, E.; Vahdat Shariatpanahi, Z. The validity of the global leadership initiative on malnutrition criteria for diagnosing malnutrition in critically ill patients with COVID-19: A prospective cohort study. Clin. Nutr. ESPEN 2021, 43, 377–382. [Google Scholar] [CrossRef] [PubMed]
- Brito, J.E.; Burgel, C.F.; Lima, J.; Chites, V.S.; Saragiotto, C.B.; Rabito, E.I.; Silva, F.M. GLIM criteria for malnutrition diagnosis of hospitalized patients presents satisfactory criterion validity: A prospective cohort study. Clin. Nutr. 2021, 40, 4366–4372. [Google Scholar] [CrossRef] [PubMed]
- Allard, J.P.; Keller, H.; Gramlich, L.; Jeejeebhoy, K.N.; Laporte, M.; Duerksen, D.R. GLIM criteria has fair sensitivity and specificity for diagnosing malnutrition when using SGA as comparator. Clin. Nutr. 2020, 39, 2771–2777. [Google Scholar] [CrossRef] [PubMed]
- Huo, Z.; Chong, F.; Yin, L.; Lu, Z.; Liu, J.; Xu, H. Accuracy of the GLIM criteria for diagnosing malnutrition: A systematic review and meta-analysis. Clin. Nutr. 2022, 41, 1208–1217. [Google Scholar] [CrossRef]
- Sanz-París, A.; Martín-Palmero, A.; Gomez-Candela, C.; García-Almeida, J.M.; Burgos-Pelaez, R.; Sanz-Arque, A.; Espina, S.; Arbones-Mainar, J.M. GLIM Criteria at Hospital Admission Predict 8-Year All-Cause Mortality in Elderly Patients With Type 2 Diabetes Mellitus: Results From VIDA Study. J. Parenter. Enter. Nutr. 2020, 44, 1492–1500. [Google Scholar] [CrossRef]
- Lauwers, P.; Hendriks, J.M.H.; Van Bouwel, S.; Verrijken, A.; Van Dessel, K.; Van Gils, C.; Peiffer, F.; Yogeswaran, K.; De Block, C.; Dirinck, E. Malnutrition according to the 2018 GLIM criteria is highly prevalent in people with a diabetic foot ulcer but does not affect outcome. Clin. Nutr. ESPEN 2021, 43, 335–341. [Google Scholar] [CrossRef]
- Klip, A.; Pâquet, M.R. Glucose Transport and Glucose Transporters in Muscle and Their Metabolic Regulation. Diabetes Care 1990, 13, 228–243. [Google Scholar] [CrossRef]
- Kalyani, R.R.; Corriere, M.; Ferrucci, L. Age-related and disease-related muscle loss: The effect of diabetes, obesity, and other diseases. Lancet Diabetes Endocrinol. 2014, 2, 819–829. [Google Scholar] [CrossRef]
- Kim, H.; Kwon, O. Higher Diet Quality is Associated with Lower Odds of Low Hand Grip Strength in the Korean Elderly Population. Nutrients 2019, 11, 1487. [Google Scholar] [CrossRef]
- Seo, D.H.; Suh, Y.J.; Cho, Y.; Ahn, S.H.; Seo, S.; Hong, S.; Lee, Y.H.; Choi, Y.J.; Lee, E.; Kim, S.H. Effect of low skeletal muscle mass and sarcopenic obesity on chronic kidney disease in patients with type 2 diabetes. Obesity 2022, 30, 2034–2043. [Google Scholar] [CrossRef]
- Suyoto, P.S.T.; Aulia, B. Low muscle mass and inflammation among patients with type 2 diabetes mellitus in Indonesia. Diabetol. Int. 2018, 10, 219–224. [Google Scholar] [CrossRef]
- Romanello, V.; Sandri, M. Mitochondria quality control and muscle mass maintenance. Front Physiol. 2016, 6, 422. [Google Scholar] [CrossRef] [PubMed]
- Buckinx, F.; Landi, F.; Cesari, M.; Fielding, R.A.; Visser, M.; Engelke, K.; Maggi, S.; Dennison, E.; Al-Daghri, N.M.; Allepaerts, S.; et al. Pitfalls in the measurement of muscle mass: A need for a reference standard. J. Cachexia Sarcopenia Muscle. 2018, 9, 269–278. [Google Scholar] [CrossRef] [PubMed]
- Stevens, D.E.; Smith, C.B.; Harwood, B.; Rice, C.L. In vivo measurement of fascicle length and pennation of the human anconeus muscle at several elbow joint angles. J. Anat. 2014, 225, 502–509. [Google Scholar] [CrossRef] [PubMed]
- Sbrignadello, S.; Göbl, C.; Tura, A. Bioelectrical Impedance Analysis for the Assessment of Body Composition in Sarcopenia and Type 2 Diabetes. Nutrients 2022, 14, 1864. [Google Scholar] [CrossRef]
- Sachin, C.; Deep, D.; Zahran, Q.; Vineet, S.; Sagar, K.; Nath, D.T. Neutrophil-lymphocyte Ratio is a Novel Reliable Predictor of Nephropathy, Retinopathy, and Coronary Artery Disease in Indians with Type-2 Diabetes. Indian J. Endocrinol. Metab. 2017, 21, 864–870. [Google Scholar] [CrossRef]
- Lowe, G.; Woodward, M.; Hillis, G.; Rumley, A.; Li, Q.; Harrap, S.; Marre, M.; Hamet, P.; Patel, A.; Poulter, N.; et al. Circulating Inflammatory Markers and the Risk of Vascular Complications and Mortality in People With Type 2 Diabetes and Cardiovascular Disease or Risk Factors: The ADVANCE Study. Diabetes 2014, 63, 1115–1123. [Google Scholar] [CrossRef]
- Zheng, N.; Shi, X.; Chen, X.; Lv, W. Associations Between Inflammatory Markers, Hemostatic Markers, and Microvascular Complications in 182 Chinese Patients With Type 2 Diabetes Mellitus. Lab. Med. 2015, 46, 214–220. [Google Scholar] [CrossRef]
| GLIM | ||||
|---|---|---|---|---|
| Variable | All n = 101 | Well-Nourished (n = 85) | Malnourished (n = 16) | p Value |
| Anthropometric | ||||
| BMI | 28.4 ± 4.8 | 29.07 ± 4.61 | 24.86 ± 4.7 | 0.001 |
| Muscle mass | 49.7 ± 8.56 | 50.54 ± 8.4 | 45.27 ± 8.2 | 0.023 |
| Fat mass | 23.89 ± 10.6 | 25.16 ± 10.5 | 17.13 ± 8.6 | 0.005 |
| ASMM | 22.07 ± 4.36 | 22.5 ± 4.26 | 19.73 ± 4.28 | 0.019 |
| ASMMI | 8.19 (2) | 8.40 (1) | 7.45 (1) | 0.008 |
| SGA | ||||
|---|---|---|---|---|
| Variable | All n = 101 | Well-Nourished (n = 83) | Malnourished (n = 18) | p Value |
| Anthropometrics | ||||
| BMI | 28.4 ± 4.8 | 28.83 ± 4.6 | 26.45 ± 5.3 | 0.060 |
| Muscle mass | 49.7 ± 8.56 | 50.41 ± 8.35 | 46.45 ± 9.0 | 0.075 |
| Fat mass | 23.89 ± 10.6 | 24.77 ± 10.7 | 19.83 ± 9.32 | 0.075 |
| ASMM | 22.07 ± 4.36 | 22.47 ± 4.22 | 20.24 ± 4.64 | 0.049 |
| ASMMI | 8.19 (2) | 8.40 (2) | 7.90 (2) | 0.112 |
| GLIM | ||||
|---|---|---|---|---|
| Variable | All n = 101 | Well-Nourished (n = 85) | Malnourished (n = 16) | p Value |
| Comorbidities | ||||
| HTN | 63 (62.4%) | (60%) 51 | 12 (75%) | 0.399 |
| DLP | 78 (77.2%) | (76.5%) 65 | (81.3%) 13 | 1.00 |
| Hypothyroidism | 12 (11.9%) | 8 (9.4%) | 4 (25%) | 0.095 |
| IDA | 7 (6.9%) | 6 (7.1%) | 1 (6.3%) | 1.00 |
| Asthma | 5 (5%) | 4 (4.7%) | 1 (6.3%) | 0.586 |
| Other | 39 (38.6%) | 33 (38.8%) | 6 (37.5%) | 1.00 |
| Macrovascular complications | 19 (18.8%) | 15 (17.6%) | 4 (25%) | 0.495 |
| Microvascular complications | 50 (49.5%) | 41 (48.2%) | 9 (56.3%) | 0.596 |
| Neuropathy | 27 (26.7%) | 24 (28.2%) | 3 (18.8%) | 0.548 |
| Nephropathy | 15 (14.9%) | 11 (12.9%) | 4 (25%) | 0.250 |
| Retinopathy | 27 (26.7%) | 22 (25.9%) | 5 (31.3%) | 0.759 |
| Medication | ||||
| Oral antidiabetic | 98 (97.0%) | 82 (96.5%) | 16 (100%) | 1.00 |
| Insulin | 54 (53.5%) | 48 (56.5%) | 6 (37.5%) | 0.163 |
| Both | 50 (49.5%) | 44 (51.8%) | 6 (37.5%) | 0.295 |
| SGA | ||||
|---|---|---|---|---|
| Variable | All n = 101 | Well-Nourished (n = 83) | Malnourished (n = 18) | p Value |
| Comorbidities | ||||
| HTN | 63 (62.4%) | 49 (59.0%) | 14 (77.8%) | 0.183 |
| DLP | 78 (77.2%) | 63 (75.9%) | 15 (83.3%) | 0.757 |
| Hypothyroidism | 12 (11.9%) | 7 (8.4%) | 5 (27.8%) | 0.021 |
| IDA | 7 (6.9%) | 6 (7.2%) | 1 (5.6%) | 1.00 |
| Asthma | 5 (5%) | 4 (4.8%) | 1 (5.6%) | 1.00 |
| Other | 39 (38.6%) | 32 (38.6%) | 7 (38.9%) | 0.979 |
| Macrovascular complications | 19 (18.8%) | 16 (19.3%) | 3 (16.7%) | 1.00 |
| Microvascular complications | 50 (49.5%) | 39 (47.0%) | 11 (61.1%) | 0.277 |
| Neuropathy | 27 (26.7%) | 23 (27.7%) | 4 (22.2%) | 0.774 |
| Nephropathy | 15 (14.9%) | 11 (13.3%) | 4 (22.2%) | 0.462 |
| Retinopathy | 27 (26.7%) | 20 (24.1%) | 7 (38.9%) | 0.199 |
| Medication | ||||
| Oral antidiabetic | 98 (97.0%) | 80 (96.4%) | 18 (100%) | 1.00 |
| Insulin | 54 (53.5%) | 48 (57.8%) | 6 (33.3%) | 0.059 |
| Both | 50 (49.5%) | 45 (54.2%) | 5 (27.8%) | 0.042 |
| Statistical Parameters of Concurrent Validity | |||
|---|---|---|---|
| Kappa (κ) | 0.788 | (p = 0.001) | |
| AUC (95% CI) | 0.877 | (0.760–0.993) | (p = 0.001) |
| Sensitivity | 77.8% | ||
| Specificity | 97.6% | ||
| Predictive positive value | 87.5% | ||
| Predictive negative value | 95.3% | ||
| Youden’s index | 0.754 |
| All n = 101 | Well-Nourished (n = 85) | Malnourished (n = 16) | p Value | |
|---|---|---|---|---|
| Phenotypic criteria | ||||
| Weight loss | 17 (16.8%) | 3 (3.5%) | 14 (87.5%) | 0.001 |
| Low BMI | 1 (1%) | 0 | (6.3%) 1 | 0.158 |
| Reduce muscle mass | 6 (5.9%) | 3 (3.5%) | 3 (18.8%) | 0.049 |
| Etiologic Criteria | ||||
| Low food intake | 37 (36.6%) | 22 (25.9%) | 15 (93.8%) | 0.001 |
| Disease/inflammation | 45 (44.6%) | 34 (40%) | 11 (68.8%) | 0.034 |
| Model 1 | Model 2 | |||
|---|---|---|---|---|
| Variable | OR (95% CI) | p Value | OR (95% CI) | p Value |
| Weight loss | 2.08 (0.633–6.85) | 0.227 | 1.563 (0.38–6.44) | 0.536 |
| Low BMI | 0.92 (0.824–1.03) | 0.160 | 0.941 (0.83–1.07) | 0.349 |
| Reduce muscle mass | 0.86 (0.094–7.78) | 0.890 | 0.744 (0.06–9.97) | 0.824 |
| Reduce food intake | 1.74 (0.632–4.76) | 0.284 | 0.898 (0.25–3.16) | 0.867 |
| Disease burden/inflammation | 4.606 (1.511–14.04) | 0.007 | 4.266 (1.29–14.11) | 0.017 |
| Model 1 | Model 2 | |||
|---|---|---|---|---|
| Variable | OR (95% CI) | p Value | OR (95% CI) | p Value |
| Weight loss | 1.57 (0.546–4.52) | 0.402 | 1.22 (0.38–3.96) | 0.737 |
| Low BMI | 0.98 (0.905–1.06) | 0.652 | 0.99 (0.90–1.08) | 0.767 |
| Reduce muscle mass | 0.49 (0.086–2.80) | 0.422 | 0.43 (0.07–2.79) | 0.378 |
| Reduce food intake | 1.58 (0.701–3.58) | 0.269 | 1.37 (0.53–3.51) | 0.515 |
| Disease burden/inflammation | 1.82 (0.82–4.03) | 0.138 | 1.58 (0.68–3.68) | 0.289 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Albukhari, S.; Abulmeaty, M.M.A.; Alguwaihes, A.M.; Shoqeair, M.; Aldisi, D.; Alhamdan, A. GLIM Criteria for Assessment of Malnutrition in Saudi Patients with Type 2 Diabetes. Nutrients 2023, 15, 897. https://doi.org/10.3390/nu15040897
Albukhari S, Abulmeaty MMA, Alguwaihes AM, Shoqeair M, Aldisi D, Alhamdan A. GLIM Criteria for Assessment of Malnutrition in Saudi Patients with Type 2 Diabetes. Nutrients. 2023; 15(4):897. https://doi.org/10.3390/nu15040897
Chicago/Turabian StyleAlbukhari, Sondos, Mahmoud M. A. Abulmeaty, Abdullah M. Alguwaihes, Mustafa Shoqeair, Dara Aldisi, and Adel Alhamdan. 2023. "GLIM Criteria for Assessment of Malnutrition in Saudi Patients with Type 2 Diabetes" Nutrients 15, no. 4: 897. https://doi.org/10.3390/nu15040897
APA StyleAlbukhari, S., Abulmeaty, M. M. A., Alguwaihes, A. M., Shoqeair, M., Aldisi, D., & Alhamdan, A. (2023). GLIM Criteria for Assessment of Malnutrition in Saudi Patients with Type 2 Diabetes. Nutrients, 15(4), 897. https://doi.org/10.3390/nu15040897








