Maternal Over- and Malnutrition and Increased Risk for Addictive and Eating Disorders in the Offspring
Abstract
1. Introduction
2. An Overview of the Role of the Dopamine System in Food Overconsumption
3. Peri-Gestation Maternal Overnutrition in Mice: A Robust Neurodevelopmental Animal Model of Several Behavioral Abnormalities
4. Central Nervous System Alterations in An Overnutrition State Drive Addiction-Like Behaviors
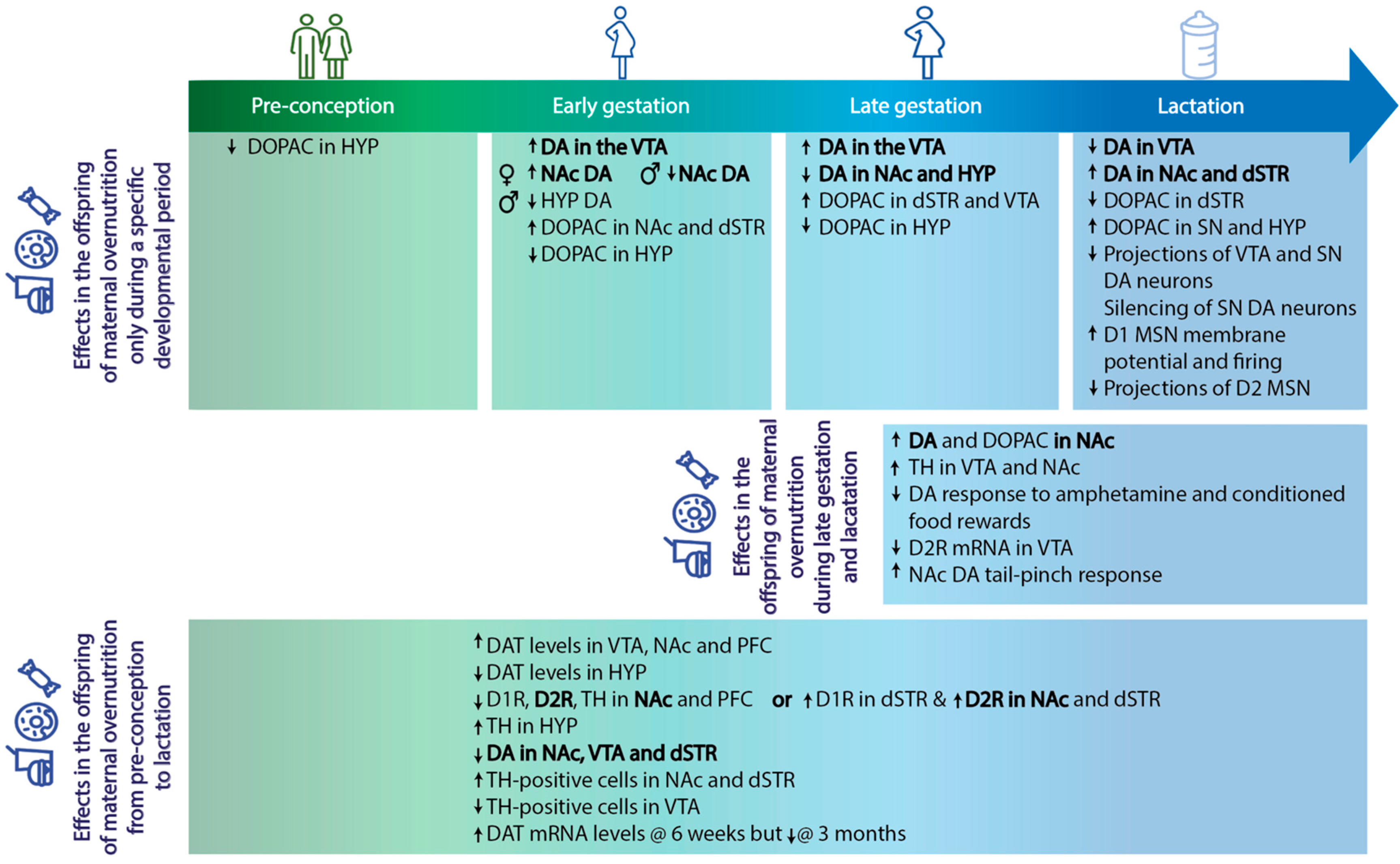
5. Maternal Overnutrition as A Risk Factor for Addiction
6. Fetal Programming by Maternal Overnutrition and Its Impact on Addiction and Overeating in the Offspring
7. The Impact of Maternal Overnutrition on the Risk of Developing Eating Disorders
8. Conclusions
Funding
Conflicts of Interest
References
- Di Cesare, M.; Bentham, J.; Stevens, G.A.; Zhou, B.; Danaei, G.; Lu, Y.; Bixby, H.; Cowan, M.J.; Riley, L.M.; Hajifathalian, K.; et al. Trends in adult body-mass index in 200 countries from 1975 to 2014: A pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet 2016, 387, 1377–1396. [Google Scholar] [CrossRef]
- Hruby, A.; Hu, F.B. The Epidemiology of Obesity: A Big Picture. Pharmacoeconomics 2014, 33, 673–689. [Google Scholar] [CrossRef]
- Yang, W.; Kelly, T.; He, J. Genetic Epidemiology of Obesity. Epidemiologic Rev. 2007, 29, 49–61. (In English) [Google Scholar] [CrossRef]
- Catalano, P.M.; Shankar, K. Obesity and pregnancy: Mechanisms of short term and long term adverse consequences for mother and child. BMJ 2017, 356, j1. [Google Scholar] [CrossRef]
- Barker, D.J.P. The origins of the developmental origins theory. J. Intern. Med. 2007, 261, 412–417. (In English) [Google Scholar]
- Kominiarek, M.A.; Peaceman, A.M. Gestational weight gain. Am. J. Obstet. Gynecol. 2017, 217, 642–651. (In English) [Google Scholar] [CrossRef]
- Ruager-Martin, R.; Hyde, M.J.; Modi, N. Maternal obesity and infant outcomes. Early Hum. Dev. 2010, 86, 715–722. [Google Scholar] [CrossRef]
- Birch, L.L.; Davison, K.K. Family Environmental Factors Influencing the Developing Behavioral Controls of Food Intake and Childhood Overweight. Pediatri. Clin. N. Am. 2001, 48, 893–907. (In English) [Google Scholar] [CrossRef]
- Contento, I.R.; Basch, C.; Shea, S.; Gutin, B.; Zybert, P.; Michela, J.L.; Rips, J. Relationship of mothers’ food choice criteria to food intake of preschool children: Identification of family sub-groups. Health Educ. Q 1993, 20, 243–259. (In English) [Google Scholar] [CrossRef]
- Yang, Y.; Smith, D.L.; Keating, K.D.; Allison, D.B.; Nagy, T.R. Variations in body weight, food intake and body composition after long-term high-fat diet feeding in C57BL/6J mice. Obesity 2014, 22, 2147–2155. [Google Scholar] [CrossRef]
- Nutt, D.J.; Lingford-Hughes, A.; Erritzoe, D.; Stokes, P. The dopamine theory of addiction: 40 years of highs and lows. Nat. Rev. Neurosci. 2015, 16, 305–312. (In English) [Google Scholar] [CrossRef]
- Koob, G.F.; Volkow, N.D. Neurocircuitry of Addiction. Neuropsychopharmacology 2010, 35, 217–238. (In English) [Google Scholar] [CrossRef]
- Koob, G.F.; Le Moal, M. Drug addiction, dysregulation of reward, and allostasis. Neuropsychopharmacology 2001, 24, 97–129. [Google Scholar] [CrossRef]
- Ong, Z.Y.; Muhlhausler, B.S. Maternal “junk-food” feeding of rat dams alters food choices and development of the mesolimbic re-ward pathway in the offspring. FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 2011, 25, 2167–2179. (In English) [Google Scholar]
- Naef, L.; Srivastava, L.; Gratton, A.; Hendrickson, H.; Owens, S.M.; Walker, C.-D. Maternal high fat diet during the perinatal period alters mesocorticolimbic dopamine in the adult rat offspring: Reduction in the behavioral responses to repeated amphetamine administration. Psychopharmacology 2007, 197, 83–94. (In English) [Google Scholar] [CrossRef]
- Vucetic, Z.; Kimmel, J.; Totoki, K.; Hollenbeck, E.; Reyes, T.M. Maternal high-fat diet alters methylation and gene expression of dopa-mine and opioid-related genes. Endocrinology 2010, 151, 4756–4764. (In English) [Google Scholar] [CrossRef]
- Naef, L.; Moquin, L.; Bo, G.D.; Giros, B.; Gratton, A.; Walker, C.-D. Maternal high-fat intake alters presynaptic regulation of dopamine in the nucleus accumbens and increases motivation for fat rewards in the offspring. Neuroscience 2011, 176, 225–236. (In English) [Google Scholar] [CrossRef]
- Naef, L.; Gratton, A.; Walker, C.-D. Exposure to high fat during early development impairs adaptations in dopamine and neuroendocrine responses to repeated stress. Stress 2013, 16, 540–548. [Google Scholar] [CrossRef]
- Naef, L.; Moquin, L.; Gratton, A.; Walker, C.-D. Reduced anticipatory dopamine responses to food in rats exposed to high fat during early development. Int. J. Obes. 2012, 37, 885–888. [Google Scholar] [CrossRef]
- Peleg-Raibstein, D.; Sarker, G.; Litwan, K.; Krämer, S.D.; Ametamey, S.M.; Schibli, R.; Wolfrum, C. Enhanced sensitivity to drugs of abuse and palatable foods following maternal overnutrition. Transl. Psychiatry 2016, 6, e911. (In English) [Google Scholar] [CrossRef]
- Sarker, G.; Berrens, R.; von Arx, J.; Pelczar, P.; Reik, W.; Wolfrum, C.; Peleg-Raibstein, D. Transgenerational transmission of hedonic behaviors and metabolic phenotypes induced by maternal overnutrition. Transl. Psychiatry 2018, 8, 195. (In English) [Google Scholar] [CrossRef]
- Sarker, G.; Litwan, K.; Kastli, R.; Peleg-Raibstein, D. Maternal overnutrition during critical developmental periods leads to different health adversities in the offspring: Relevance of obesity, addiction and schizophrenia. Sci. Rep. 2019, 9, 17322. (In English) [Google Scholar] [CrossRef]
- Lippert, R.; Hess, S.; Klemm, P.; Burgeno, L.; Jahans-Price, T.; Walton, M.; Kloppenburg, P.; Brüning, J. Maternal high-fat diet during lactation reprograms the dopaminergic circuitry in mice. J. Clin. Investig. 2020, 130, 3761–3776. [Google Scholar] [CrossRef]
- Stice, E.; Yokum, S.; Burger, K.S.; Epstein, L.H.; Small, D.M. Youth at Risk for Obesity Show Greater Activation of Striatal and Somatosensory Regions to Food. J. Neurosci. 2011, 31, 4360–4366. (In English) [Google Scholar] [CrossRef]
- Berthoud, H.-R.; Morrison, C. The Brain, Appetite, and Obesity. Annu. Rev. Psychol. 2008, 59, 55–92. [Google Scholar] [CrossRef]
- Baik, J.-H. Dopaminergic Control of the Feeding Circuit. Endocrinol. Metab. 2021, 36, 229–239. (In English) [Google Scholar] [CrossRef]
- Finlayson, G.; Dalton, M. Hedonics of Food Consumption: Are Food ‘Liking’ and ‘Wanting’ Viable Targets for Appetite Control in the Obese? Curr. Obes. Rep. 2012, 1, 42–49. (In English) [Google Scholar] [CrossRef]
- Lutter, M.; Nestler, E.J. Homeostatic and Hedonic Signals Interact in the Regulation of Food Intake. J. Nutr. 2009, 139, 629–632. (In English) [Google Scholar] [CrossRef]
- Berthoud, H.-R. Multiple neural systems controlling food intake and body weight. Neurosci. Biobehav. Rev. 2002, 26, 393–428. (In English) [Google Scholar] [CrossRef]
- Kelley, A.E. Ventral striatal control of appetitive motivation: Role in ingestive behavior and reward-related learning. Neurosci. Biobehav. Rev. 2004, 27, 765–776. (In English) [Google Scholar] [CrossRef]
- Volkow, N.D.; Wise, R.A.; Baler, R. The dopamine motive system: Implications for drug and food addiction. Nat. Rev. Neurosci. 2017, 18, 741–752. (In English) [Google Scholar] [CrossRef]
- Russo, S.J.; Nestler, E.J. The brain reward circuitry in mood disorders. Nat. Rev. Neurosci. 2013, 14, 609–625. [Google Scholar] [CrossRef]
- Volkow, N.D.; Wang, G.J.; Fowler, J.S.; Telang, F. Overlapping neuronal circuits in addiction and obesity: Evidence of systems pathol-ogy. Philos. Trans. R. Soc. B Biol. Sci. 2008, 363, 3191–3200. (In English) [Google Scholar] [CrossRef]
- Wang, G.J.; Volkow, N.D.; Logan, J.; Pappas, N.R.; Wong, C.T.; Zhu, W.; Netusll, N.; Fowler, J.S. Brain dopamine and obesity. Lancet 2001, 357, 354–357. (In English) [Google Scholar] [CrossRef]
- Volkow, N.D.; Wang, G.-J.; Baler, R.D. Reward, dopamine and the control of food intake: Implications for obesity. Trends Cogn. Sci. 2011, 15, 37–46. [Google Scholar] [CrossRef]
- Goldstein, R.Z.; Volkow, N.D. Drug Addiction and Its Underlying Neurobiological Basis: Neuroimaging Evidence for the Involvement of the Frontal Cortex. Am. J. Psychiatry 2002, 159, 1642–1652. (In English) [Google Scholar] [CrossRef]
- Volkow, N.D.; Wang, G.J.; Fowler, J.S.; Logan, J.; Gatley, S.J.; Gifford, A.; Hitzemann, R.; Ding, Y.S.; Pappas, N. Prediction of reinforcing responses to psychostimulants in humans by brain dopamine D2 receptor levels. Am. J. Psychiatry 1999, 156, 1440–1443. (In English) [Google Scholar] [CrossRef]
- Volkow, N.D.; Wang, G.J.; Tomasi, D.; Baler, R.D. Obesity and addiction: Neurobiological overlaps. Obesity reviews: An offi-cial journal of the International Association for the Study of Obesity. J. Artic. Rev. 2013, 14, 2–18. (In English) [Google Scholar]
- Ziauddeen, H.; Farooqi, I.S.; Fletcher, P.C. Obesity and the brain: How convincing is the addiction model? Nat. Rev. Neurosci. 2012, 13, 279–286. (In English) [Google Scholar] [CrossRef]
- Alfaradhi, M.Z.; Ozanne, S.E. Developmental Programming in Response to Maternal Overnutrition. Front. Genet. 2011, 2, 27. [Google Scholar] [CrossRef]
- Vogt, M.C.; Paeger, L.; Hess, S.; Steculorum, S.M.; Awazawa, M.; Hampel, B.; Neupert, S.; Nicholls, H.T.; Mauer, J.; Hausen, A.C.; et al. Neonatal Insulin Action Impairs Hypothalamic Neurocircuit Formation in Response to Maternal High-Fat Feeding. Cell 2014, 156, 495–509. [Google Scholar] [CrossRef]
- Ainge, H.; Thompson, C.; Ozanne, S.; Rooney, K. A systematic review on animal models of maternal high fat feeding and offspring glycaemic control. Int. J. Obes. 2010, 35, 325–335. [Google Scholar] [CrossRef]
- Dunn, G.A.; Bale, T.L. Maternal High-Fat Diet Promotes Body Length Increases and Insulin Insensitivity in Second-Generation Mice. Endocrinology 2009, 150, 4999–5009. (In English) [Google Scholar] [CrossRef]
- Peleg-Raibstein, D. Understanding the Link between Maternal Overnutrition, Cardio-Metabolic Dysfunction and Cognitive Aging. Front. Neurosci. 2021, 15, 645569. (In English) [Google Scholar] [CrossRef]
- Kereliuk, S.M.; Dolinsky, V.W. Recent Experimental Studies of Maternal Obesity, Diabetes during Pregnancy and the Developmental Origins of Cardiovascular Disease. Int. J. Mol. Sci. 2022, 23, 4467. [Google Scholar] [CrossRef]
- Salter, A.; Tarling, E.; Langley-Evans, S. Influence of maternal nutrition on the metabolic syndrome and cardiovascular risk in the off-spring. Clin. Lipidol. 2009, 4, 145–158. [Google Scholar] [CrossRef]
- Mitra, A.; Alvers, K.M.; Crump, E.M.; Rowland, N.E. Effect of high-fat diet during gestation, lactation, or postweaning on physiological and behavioral indexes in borderline hypertensive rats. Am. J. Physiol. Integr. Comp. Physiol. 2009, 296, R20–R28. (In English) [Google Scholar] [CrossRef]
- Peleg-Raibstein, D.; Luca, E.; Wolfrum, C. Maternal high-fat diet in mice programs emotional behavior in adulthood. Behav. Brain Res. 2012, 233, 398–404. (In English) [Google Scholar] [CrossRef]
- Tozuka, Y.; Kumon, M.; Wada, E.; Onodera, M.; Mochizuki, H.; Wada, K. Maternal obesity impairs hippocampal BDNF production and spatial learning performance in young mouse offspring. Neurochem. Int. 2010, 57, 235–247. (In English) [Google Scholar] [CrossRef]
- Wolfrum, C.; Peleg-Raibstein, D. Maternal overnutrition leads to cognitive and neurochemical abnormalities in C57BL/6 mice. Nutr. Neurosci. 2018, 22, 688–699. (In English) [Google Scholar] [CrossRef]
- Sarker, G.; Peleg-Raibstein, D. Maternal Overnutrition Induces Long-Term Cognitive Deficits across Several Generations. Nutrients 2018, 11, 7. (In English) [Google Scholar] [CrossRef]
- Rivera, H.M.; Christiansen, K.J.; Sullivan, E.L. The role of maternal obesity in the risk of neuropsychiatric disorders. Front. Neurosci. 2015, 9, 194. [Google Scholar] [CrossRef]
- Bayol, S.A.; Farrington, S.J.; Stickland, N.C. A maternal ‘junk food’ diet in pregnancy and lactation promotes an exacerbated taste for ‘junk food’ and a greater propensity for obesity in rat offspring. Br. J. Nutr. 2007, 98, 843–851. (In English) [Google Scholar] [CrossRef]
- Howie, G.J.; Sloboda, D.M.; Kamal, T.; Vickers, M.H. Maternal nutritional history predicts obesity in adult offspring independent of postnatal diet. J. Physiol. 2009, 587, 905–915. (In English) [Google Scholar] [CrossRef]
- Grissom, N.; Bowman, N.; Reyes, T.M. Epigenetic programming of reward function in offspring: A role for maternal diet. Mamm. Genome 2013, 25, 41–48. (In English) [Google Scholar] [CrossRef]
- Andersen, S.L. Trajectories of brain development: Point of vulnerability or window of opportunity? Neurosci. Biobehav. Rev. 2003, 27, 3–18. (In English) [Google Scholar] [CrossRef]
- Sullivan, E.L.; Grayson, B.; Takahashi, D.; Robertson, N.; Maier, A.; Bethea, C.L.; Smith, M.S.; Coleman, K.; Grove, K.L. Chronic consumption of a high-fat diet during pregnancy causes perturbations in the serotonergic system and in-creased anxiety-like behavior in nonhuman primate offspring. J. Neurosci. Off. J. Soc. Neurosci. 2010, 30, 3826–3830. (In English) [Google Scholar] [CrossRef]
- Erlanson-Albertsson, C. Fat-Rich Food Palatability and Appetite Regulation. In Fat Detection: Taste, Texture, and Post Ingestive Effects; Montmayeur, J.P., le Coutre, J., Eds.; Frontiers in Neuroscience: Boca Raton, FL, USA, 2010. [Google Scholar]
- Di Chiara, G. Dopamine in disturbances of food and drug motivated behavior: A case of homology? Physiol. Behav. 2005, 86, 9–10. (In English) [Google Scholar] [CrossRef]
- Schultz, W. Dopamine reward prediction error coding. Dialogues Clin. Neuro. 2016, 18, 23–32. [Google Scholar] [CrossRef]
- Tomasi, D.; Wang, G.-J.; Wang, R.; Caparelli, E.C.; Logan, J.; Volkow, N.D. Overlapping patterns of brain activation to food and cocaine cues in cocaine abusers: Association to striatal D2/D3 receptors. Hum. Brain Mapp. 2014, 36, 120–136. (In English) [Google Scholar] [CrossRef]
- Devoto, F.; Coricelli, C.; Paulesu, E.; Zapparoli, L. Neural circuits mediating food cue-reactivity: Toward a new model shaping the interplay of internal and external factors. Front. Nutr. 2022, 9, 954523. (In English) [Google Scholar] [CrossRef]
- Kalivas, P.W.; Volkow, N.D. The Neural Basis of Addiction: A Pathology of Motivation and Choice. Am. J. Psychiatry 2005, 162, 1403–1413. (In English) [Google Scholar] [CrossRef]
- Montalvo-Martínez, L.; Ruiz, R.M.; Cardenas-Tueme, M.; Reséndez-Pérez, D.; Camacho, A. Maternal Overnutrition Programs Central Inflammation and Addiction-Like Behavior in Offspring. BioMed. Res. Int. 2018, 2018, 1–11. (In English) [Google Scholar] [CrossRef]
- Kim, K.-S.; Seeley, R.J.; Sandoval, D.A. Signalling from the periphery to the brain that regulates energy homeostasis. Nat. Rev. Neurosci. 2018, 19, 185–196. (In English) [Google Scholar] [CrossRef]
- Avena, N.M. The study of food addiction using animal models of binge eating. Appetite 2010, 55, 734–737. (In English) [Google Scholar] [CrossRef]
- Han, W.; Tellez, L.A.; Niu, J.; Medina, S.; Ferreira, T.L.; Zhang, X.; Su, J.; Tong, J.; Schwartz, G.J.; Pol, A.V.D.; et al. Striatal Dopamine Links Gastrointestinal Rerouting to Altered Sweet Appetite. Cell Metab. 2015, 23, 103–112. (In English) [Google Scholar] [CrossRef]
- Avena, N.M.; Gearhardt, A.N.; Gold, M.S.; Wang, G.-J.; Potenza, M.N. Tossing the baby out with the bathwater after a brief rinse? The potential downside of dismissing food addiction based on limited data. Nat. Rev. Neurosci. 2012, 13, 514. (In English) [Google Scholar] [CrossRef]
- Rogers, P.J.; Smit, H.J. Food Craving and Food “Addiction”: A Critical Review of the Evidence From a Biopsychosocial Perspective. Pharmacol. Biochem. Behav. 2000, 66, 3–14. (In English) [Google Scholar] [CrossRef]
- Das, U. Is obesity an inflammatory condition? Nutrition 2001, 17, 953–966. (In English) [Google Scholar] [CrossRef]
- Bolton, J.L.; Bilbo, S.D. Developmental programming of brain and behavior by perinatal diet: Focus on inflammatory mechanisms. Dialogues Clin. Neuro. 2014, 16, 307–320. [Google Scholar] [CrossRef]
- Bouret, S.G. Developmental programming of hypothalamic melanocortin circuits. Exp. Mol. Med. 2022, 54, 403–413. (In English) [Google Scholar] [CrossRef]
- Proulx, K.; Richard, D.; Walker, C.-D. Leptin Regulates Appetite-Related Neuropeptides in the Hypothalamus of Developing Rats without Affecting Food Intake. Endocrinology 2002, 143, 4683–4692. (In English) [Google Scholar] [CrossRef]
- Florio, L.; Lassi, D.L.; Perico, C.D.A.M.; Vignoli, N.G.; Torales, J.; Ventriglio, A.; Castaldelli-Maia, J.M. Food Addiction: A Comprehensive Review. J. Nerv. Ment. Dis. 2022, 210. (In English) [Google Scholar] [CrossRef]
- Vasiliu, O. Current Status of Evidence for a New Diagnosis: Food Addiction-A Literature Review. Front. Psychiatry 2022, 12, 824936. (In English) [Google Scholar] [CrossRef]
- Behnke, M.; Smith, V.C.; Abuse, C.S.; Newborn, C.F. Prenatal Substance Abuse: Short- and Long-term Effects on the Exposed Fetus. Pediatrics 2013, 131, e1009–e1024. (In English) [Google Scholar] [CrossRef]
- Jutras-Aswad, D.; DiNieri, J.A.; Harkany, T.; Hurd, Y.L. Neurobiological consequences of maternal cannabis on human fetal development and its neuropsychiatric outcome. Eur. Arch. Psy. Clin. N 2009, 259, 395–412. (In English) [Google Scholar] [CrossRef]
- Bocarsly, M.; Barson, J.R.; Hauca, J.M.; Hoebel, B.G.; Leibowitz, S.F.; Avena, N.M. Effects of perinatal exposure to palatable diets on body weight and sensitivity to drugs of abuse in rats. Physiol. Behav. 2012, 107, 568–575. (In English) [Google Scholar] [CrossRef]
- Morganstern, I.; Lukatskaya, O.; Moon, S.-H.; Guo, W.-R.; Shaji, J.; Karatayev, O.; Leibowitz, S.F. Stimulation of nicotine reward and central cholinergic activity in Sprague–Dawley rats exposed perinatally to a fat-rich diet. Psychopharmacology 2013, 230, 509–524. (In English) [Google Scholar] [CrossRef]
- Rising, R.; Lifshitz, F. Relationship between maternal obesity and infant feeding-interactions. Nutr. J. 2005, 4, 17. (In English) [Google Scholar] [CrossRef]
- Brekke, H.K.; van Odijk, J.; Ludvigsson, J. Predictors and dietary consequences of frequent intake of high-sugar, low-nutrient foods in 1-year-old children participating in the ABIS study. Br. J. Nutr. 2007, 97, 176–181. (In English) [Google Scholar] [CrossRef]
- Gross, R.S.; Mendelsohn, A.L.; Fierman, A.H.; Hauser, N.R.; Messito, M.J. Maternal Infant Feeding Behaviors and Disparities in Early Child Obesity. Child. Obes. 2014, 10, 145–152. (In English) [Google Scholar] [CrossRef]
- Barker, D. In utero programming of chronic disease. Clin. Sci. 1998, 95, 115. (In English) [Google Scholar] [CrossRef]
- Seneviratne, S.N.; Rajindrajith, S. Fetal programming of obesity and type 2 diabetes. World J. Diabetes 2022, 13, 482–497. (In English) [Google Scholar] [CrossRef]
- Camacho, A.; Montalvo-Martinez, L.; Cardenas-Perez, R.E.; Fuentes-Mera, L.; Garza-Ocañas, L. Obesogenic diet intake during pregnancy programs aberrant synaptic plasticity and addiction-like behavior to a palatable food in offspring. Behav. Brain Res. 2017, 330, 46–55. (In English) [Google Scholar] [CrossRef]
- de Heredia, F.P.; Gómez-Martínez, S.; Marcos, A. Obesity, inflammation and the immune system. Proc. Nutr. Soc. 2012, 71, 332–338. (In English) [Google Scholar] [CrossRef]
- Ghnenis, A.B.; Odhiambo, J.F.; McCormick, R.J.; Nathanielsz, P.; Ford, S.P. Maternal obesity in the ewe increases cardiac ventricular expression of glucocorticoid receptors, proinflammatory cytokines and fibrosis in adult male offspring. PLoS ONE 2017, 12, e0189977. (In English) [Google Scholar] [CrossRef]
- Hannibal, K.E.; Bishop, M. Chronic Stress, Cortisol Dysfunction, and Pain: A Psychoneuroendocrine Rationale for Stress Management in Pain Rehabilitation. Phys. Ther. 2014, 94, 1816–1825. (In English) [Google Scholar] [CrossRef]
- Carobbio, S.; Pellegrinelli, V.; Vidal-Puig, A. Adipose Tissue Function and Expandability as Determinants of Lipotoxicity and the Meta-bolic Syndrome. Adv. Exp. Med. Biol. 2017, 960, 161–196. (In English) [Google Scholar] [CrossRef]
- Fox, H.C.; D’Sa, C.; Kimmerling, A.; Siedlarz, K.M.; Tuit, K.L.; Stowe, R.; Sinha, R. Immune system inflammation in cocaine dependent individuals: Implications for medications development. Hum. Psychopharmacol. Clin. Exp. 2012, 27, 156–166. (In English) [Google Scholar] [CrossRef]
- Harricharan, R.; Abboussi, O.; Daniels, W.M. Addiction: A dysregulation of satiety and inflammatory processes. Prog. Brain Res. 2017, 235, 65–91. (In English) [Google Scholar] [CrossRef]
- Goran, M.I.; Plows, J.F.; Ventura, E.E. Effects of consuming sugars and alternative sweeteners during pregnancy on maternal and child health: Evidence for a secondhand sugar effect. Proc. Nutr. Soc. 2018, 78, 262–271. (In English) [Google Scholar] [CrossRef]
- Silverman, B.L.; Metzger, B.E.; Cho, N.H.; Loeb, C.A. Impaired Glucose Tolerance in Adolescent Offspring of Diabetic Mothers: Relationship to fetal hyperinsulinism. Diabetes Care 1995, 18, 611–617. (In English) [Google Scholar] [CrossRef]
- Magnusson, A.L.; Waterman, I.J.; Wennergren, M.; Jansson, T.; Powell, T. Triglyceride Hydrolase Activities and Expression of Fatty Acid Binding Proteins in the Human Placenta in Pregnancies Complicated by Intrauterine Growth Restriction and Diabetes. J. Clin. Endocrinol. Metab. 2004, 89, 4607–4614. (In English) [Google Scholar] [CrossRef]
- Gauster, M.; Hiden, U.; van Poppel, M.; Frank, S.; Wadsack, C.; Mouzon, S.H.-D.; Desoye, G. Dysregulation of Placental Endothelial Lipase in Obese Women with Gestational Diabetes Mellitus. Diabetes 2011, 60, 2457–2464. (In English) [Google Scholar] [CrossRef]
- Newsholme, P.; Gaudel, C.; Krause, M. Mitochondria and Diabetes. An Intriguing Pathogenetic Role. Adv. Mitochondrial Med. 2011, 942, 235–247. (In English) [Google Scholar] [CrossRef]
- Alexander, J.; Teague, A.M.; Chen, J.; Aston, C.E.; Leung, Y.-K.; Chernausek, S.; Simmons, R.; Pinney, S.E. Offspring sex impacts DNA methylation and gene expression in placentae from women with diabetes during pregnancy. PLoS ONE 2018, 13, e0190698. (In English) [Google Scholar] [CrossRef]
- Martini, M.G.; Barona-Martinez, M.; Micali, N. Eating disorders mothers and their children: A systematic review of the literature. Arch. Women’s Ment. Health 2020, 23, 449–467. (In English) [Google Scholar] [CrossRef]
- Micali, N.; Treasure, J. Biological effects of a maternal ED on pregnancy and foetal development: A review. Eur. Eat. Disord. Rev. 2009, 17, 448–454. (In English) [Google Scholar] [CrossRef]
- Cvitic, S.; Desoye, G.; Hiden, U. Glucose, Insulin, and Oxygen Interplay in Placental Hypervascularisation in Diabetes Mellitus. BioMed. Res. Int. 2014, 2014, 12. (In English) [Google Scholar] [CrossRef]
- Morgan, J.F.; Lacey, J.H.; Sedgwick, P.M. Impact of pregnancy on bulimia nervosa. Br. J. Psychiatry 1999, 174, 135–140. (In English) [Google Scholar] [CrossRef]
- Correa, A.; Gilboa, S.M.; Besser, L.M.; Botto, L.D.; Moore, C.A.; Hobbs, C.A.; Cleves, M.A.; Riehle-Colarusso, T.J.; Waller, D.K.; Reece, E.A. Diabetes mellitus and birth defects. Am. J. Obstet. Gynecol. 2008, 199, 237.e1–237.e9. (In English) [Google Scholar] [CrossRef]
- Watson, H.J.; Zerwas, S.; Torgersen, L.; Gustavson, K.; Diemer, E.W.; Knudsen, G.P.; Reichborn-Kjennerud, T.; Bulik, C.M. Maternal eating disorders and perinatal outcomes: A three-generation study in the Norwegian Mother and Child Cohort Study. J. Abnorm. Psychol. 2017, 126, 552–564. (In English) [Google Scholar] [CrossRef]
- Stice, E.; Agras, W.S.; Hammer, L.D. Risk factors for the emergence of childhood eating disturbances: A five-year prospective study. Int J Eat Disord. 1999, 25, 375–387. (In English) [Google Scholar] [CrossRef]
- Watson, H.; Torgersen, L.; Zerwas, S.; Reichborn-Kjennerud, T.; Knoph, C.; Stoltenberg, C.; Siega-Riz, A.M.; Von Holle, A.; Hamer, R.M.; Meltzer, H.M.; et al. Eating Disorders, Pregnancy, and the Postpartum Period: Findings from the Norwegian Mother and Child Cohort Study (MoBa). Nor. Epidemiol. 2014, 24, 51–62. [Google Scholar] [CrossRef]
- Reba-Harrelson, L.; Von Holle, A.; Hamer, R.M.; Torgersen, L.; Reichborn-Kjennerud, T.; Bulik, C.M. Patterns of maternal feeding and child eating associated with eating disorders in the Norwegian Mother and Child Cohort Study (MoBa). Eat. Behav. 2010, 11, 54–61. (In English) [Google Scholar] [CrossRef]
- Drewnowski, A. Metabolic determinants of binge eating. Addict. Behav. 1995, 20, 733–745. (In English) [Google Scholar] [CrossRef]
- Cimino, S.; Cerniglia, L.; Porreca, A.; Ballarotto, G.; Marzilli, E.; Simonelli, A. Impact of Parental Binge Eating Disorder: Exploring Children’s Emotional/Behavioral Problems and the Quality of Parent-Child Feeding Interactions. Infant Ment. Health J. 2018, 39, 552–568. (In English) [Google Scholar] [CrossRef]
- Bulik, C.M.; Reba, L.; Siega-Riz, A.-M.; Reichborn-Kjennerud, T. Anorexia nervosa: Definition, epidemiology, and cycle of risk. Int. J. Eat. Disord. 2005, 37, S2–S9. (In English) [Google Scholar] [CrossRef]
- Siega-Riz, A.M.; Haugen, M.; Meltzer, H.M.; Von Holle, A.; Hamer, R.; Torgersen, L.; Knopf-Berg, C.; Reichborn-Kjennerud, T.; Bulik, C.M. Nutrient and food group intakes of women with and without bulimia nervosa and binge eating disorder during pregnancy. Am. J. Clin. Nutr. 2008, 87, 1346–1355. (In English) [Google Scholar] [CrossRef]
- Mathes, W.F.; Brownley, K.A.; Mo, X.; Bulik, C.M. The biology of binge eating. Appetite 2009, 52, 545–553. (In English) [Google Scholar] [CrossRef]
- Avena, N.M.; Rada, P.; Hoebel, B.G. Evidence for sugar addiction: Behavioral and neurochemical effects of intermittent, excessive sugar intake. Neurosci. Biobehav. Rev. 2008, 32, 20–39. (In English) [Google Scholar] [CrossRef]
- Rogers, P.J.; Hill, A.J. Breakdown of dietary restraint following mere exposure to food stimuli: Interrelationships between restraint, hunger, salivation, and food intake. Addict. Behav. 1989, 14, 387–397. (In English) [Google Scholar] [CrossRef]
- Pang, M.D.; Goossens, G.H.; Blaak, E.E. The Impact of Artificial Sweeteners on Body Weight Control and Glucose Homeostasis. Front. Nutr. 2021, 7, 598340. (In English) [Google Scholar] [CrossRef]
- Wang, Q.-P.; Lin, Y.Q.; Zhang, L.; Wilson, Y.A.; Oyston, L.J.; Cotterell, J.; Qi, Y.; Khuong, T.M.; Bakhshi, N.; Planchenault, Y.; et al. Sucralose Promotes Food Intake through NPY and a Neuronal Fasting Response. Cell Metab. 2016, 24, 75–90. (In English) [Google Scholar] [CrossRef]
- Cnattingius, S.; Villamor, E.; Lagerros, Y.T.; Wikström, A.-K.; Granath, F. High birth weight and obesity—A vicious circle across generations. Int. J. Obes. 2011, 36, 1320–1324. (In English) [Google Scholar] [CrossRef]
- Bleker, L.S.; de Rooij, S.R.; Painter, R.C.; Ravelli, A.C.; Roseboom, T.J. Cohort profile: The Dutch famine birth cohort (DFBC)—A prospective birth cohort study in the Netherlands. BMJ Open 2021, 11, e042078. (In English) [Google Scholar] [CrossRef]
- Painter, R.C.; de Rooij, S.R.; Bossuyt, P.M.; Simmers, T.A.; Osmond, C.; Barker, D.J.; Bleker, O.P.; Roseboom, T.J. Early onset of coronary artery disease after prenatal exposure to the Dutch famine1–3. Am. J. Clin. Nutr. 2006, 84, 322–327. (In English) [Google Scholar] [CrossRef]
- Ravelli, A.; van der Meulen, J.; Michels, R.; Osmond, C.; Barker, D.; Hales, C.; Bleker, O. Glucose tolerance in adults after prenatal exposure to famine. Lancet 1998, 351, 173–177. (In English) [Google Scholar] [CrossRef]
- Lussana, F.; Painter, R.C.; Ocke, M.C.; Buller, H.R.; Bossuyt, P.M.; Roseboom, T.J. Prenatal exposure to the Dutch famine is associated with a preference for fatty foods and a more atherogenic lipid profile. Am. J. Clin. Nutr. 2008, 88, 1648–1652. (In English) [Google Scholar] [CrossRef]
- Ravelli, A.C.; van der Meulen, J.H.; Osmond, C.; Barker, D.J.; Bleker, O.P. Obesity at the age of 50 y in men and women exposed to famine prenatally. Am. J. Clin. Nutr. 1999, 70, 811–816. (In English) [Google Scholar] [CrossRef]
- Painter, R.; Osmond, C.; Gluckman, P.; Hanson, M.; Phillips, D.; Roseboom, T. Transgenerational effects of prenatal exposure to the Dutch famine on neonatal adiposity and health in later life. BJOG: Int. J. Obstet. Gynaecol. 2008, 115, 1243–1249. (In English) [Google Scholar] [CrossRef]
- Veenendaal, M.; Painter, R.; de Rooij, S.; Bossuyt, P.; van der Post, J.; Gluckman, P.; Hanson, M.; Roseboom, T. Transgenerational effects of prenatal exposure to the 1944-45 Dutch famine. BJOG: Int. J. Obstet. Gynaecol. 2013, 120, 548–554. (In English) [Google Scholar] [CrossRef]
- Jantsch, J.; Tassinari, I.D.; Giovenardi, M.; Bambini-Junior, V.; Guedes, R.P.; de Fraga, L.S. Mood Disorders Induced by Maternal Overnutrition: The Role of the Gut-Brain Axis on the Development of Depression and Anxiety. Front. Cell Dev. Biol. 2022, 10, 795384. [Google Scholar] [CrossRef]

| Offspring Phenotypes | |||||
|---|---|---|---|---|---|
| Diet | Period | Changes in Central Dopaminergic Pathways | Changes in Addictive and Eating Behaviors | Species | References |
| STUDIES IN RODENTS | |||||
| HFD (30% fat) | Last week of gestation and whole of lactation. | ↑ TH expression in the VTA & NAc. ↑ in DA and DOPAC (i.e., elevated DA tone) in the NAc. No significant changes in D1R, D2R or DAT levels. | ↓ amphetamine-induced locomotion. | Rats | [15] |
| HFD (60% fat) | During pregnancy and lactation (introduction of HFD 60% 3 months before mating). | 3-to-10-fold upregulation of the DA transporter (DAT) in the VTA, NAc and prefrontal cortex (PFC). Downregulation of DAT in the hypothalamus (HYP). Downregulation of D1R, D2R and TH in the NAc and PFC. Upregulation of TH in the HYP. DNA hypomethylation of the DAT gene promoter. | ↑ preference for sucrose and fat. | Mice | [16] |
| HFD (30% fat) | Last week of gestation and whole of lactation. | Attenuated DA response to amphetamine in the NAc. ↑ activity of NAc synaptosomal DA transpoter sites. ↓ in VTA D2R mRNA levels. ↑ locomotor response to D2/3R activation. | ↑ operant responding to obtain a fat-rich reward (but not a sugar-rich reward) in an FR/PR task. | Rats | [17] |
| ‘Cafeteria junk-food diet’ (mix of sweet and fatty ingredients) | 4 weeks pre-conception, gestation and lactation. | ↓ NAc DAT mRNA levels during juvenile period (6 weeks of age). ↑ NAc DAT mRNA levels at adulthood (3 months of age). = VTA DAT mRNA levels. = TH, D1R or D2R mRNA levels in the NAc or VTA. | ↑ fat and protein intake during the juvenile period. ↑ fat intake during adulthood. | Rats | [14] |
| HFD (30% fat) | Last week of gestation and whole of lactation. | ↑ NAc DA response to acute tail-pinch. Alteration in DA response to both acute and repeated stress exposure. | Rats | [18] | |
| HFD (30% fat) | Last week of gestation and whole of lactation. | ↓ NAc DA response to food-reward-paired tone in a Pavlovian conditioning task. No difference in NAc DA levels between HFD and control offspring during food consumption in an unconditioned protocol. | Rats | [19] | |
| HFD (60% fat) | 3 weeks before conception, during gestation and during lactation. | ↓ DA in the NAc, VTA and dorsal striatum. ↑ D2R levels in the NAc (core and shell) and dorsal striatum. ↑ D1R levels in the dorsal striatum. ↑ DAT levels in the medial prefrontal cortex. ↑ number of TH-positive neurons in the NAc (core and shell) and dorsal striatum. ↓ number of TH-positive neurons in the VTA. | ↑ alcohol consumption. ↑ amphetamine-induced locomotion. ↑ cocaine-conditioned place preference. ↑ preference for sucrose and HFD. | Mice | [20] |
| HFD (60% fat) | 3 weeks before conception, during gestation and during lactation. | ↓ number of TH-positive cells in the VTA in F2 and F3 female offspring. ↓ levels of TH in the dorsal striatum (dSTR), NAc shell and VTA in F3 offspring. ↓ DAT expression in the NAc in F2 and F3 female offspring. ↓ D1R expression in the dSTR and mPFC in F2 female offspring. ↑ D1R expression in the dSTR and NAc in F3 offspring. ↑ D2R expression in the dSTR, NAc and mPFC of F2 offspring. ↑ D2R expression in the NAc (but decreased in the mPFC) of F3 offspring. ↓ DA levels in the VTA, NAc and dSTR in F2 and F3 offspring. ↓ levels of DOPAC in the NAc of F2 offspring and in the VTA of F3 female offspring. | 3rd generation females show addictive-like behaviors. ↑ alcohol consumption, amphetamine-induced locomotion and cocaine-conditioned place preference in F2 and F3 generations (F3 males only showed ↑sensitivity to cocaine). F1 offspring showed ↑ sensitivity to both drugs of abuse and natural rewards. | Mice | [21] |
| HFD (60% fat) | Pre-conception (3 weeks prior to mating). | ↓ DOPAC levels in the hypothalamus. | Mice | [22] | |
| HFD (60% fat) | Early gestation (G0-G11). | ↑ DA levels in the VTA. Females: ↑ NAc DA levels/ Males: ↓ NAc DA levels. ↓ DA levels in the Hypothalamus (males only). ↑ DOPAC levels in the NAc and dSTR. ↓ DOPAC levels in the hypothalamus. | ↑ amphetamine-induced locomotion. | Mice | [22] |
| HFD (60% fat) | Late gestation (G12-G21). | ↑ DA levels in the VTA. ↓ DA levels in the hypothalamus (females only) and NAc. ↑ DOPAC levels in the dSTR and VTA. ↓ DOPAC levels in the hypothalamus. | ↑ alcohol preference. ↑ amphetamine-induced locomotion. | Mice | [22] |
| HFD (60% fat) | Lactation (3 weeks after birth, P0-P21). | ↑ DA levels in the NAc and dSTR. ↓ DOPAC levels in the dSTR. ↑ DOPAC levels in the SN and hypothalamus. | ↑ amphetamine-induced locomotion. | Mice | [22] |
| HFD (60% fat) | During lactation only. | ↓ in projections of SN and VTA DA neurons. ↓ in DA release in the VTA. Silencing of SN DA neurons. ↑ in striatal D1 MSN membrane potential and firing. ↓ in projections of striatal D2 MSNs. | Females: ↑ in sucrose preference. Males: ↑ in novelty-induced locomotion. | Mice | [23] |
| STUDY IN HUMANS | |||||
| 2 parents with BMI>27. | Not specified. | ↑ activation of dorsal striatum in response to palatable food rewards. ↑ activation of striatum in response to monetary rewards. | ↑ oral somatosensory response to palatable food rewards. | Humans | [24] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guillaumin, M.C.C.; Peleg-Raibstein, D. Maternal Over- and Malnutrition and Increased Risk for Addictive and Eating Disorders in the Offspring. Nutrients 2023, 15, 1095. https://doi.org/10.3390/nu15051095
Guillaumin MCC, Peleg-Raibstein D. Maternal Over- and Malnutrition and Increased Risk for Addictive and Eating Disorders in the Offspring. Nutrients. 2023; 15(5):1095. https://doi.org/10.3390/nu15051095
Chicago/Turabian StyleGuillaumin, Mathilde C. C., and Daria Peleg-Raibstein. 2023. "Maternal Over- and Malnutrition and Increased Risk for Addictive and Eating Disorders in the Offspring" Nutrients 15, no. 5: 1095. https://doi.org/10.3390/nu15051095
APA StyleGuillaumin, M. C. C., & Peleg-Raibstein, D. (2023). Maternal Over- and Malnutrition and Increased Risk for Addictive and Eating Disorders in the Offspring. Nutrients, 15(5), 1095. https://doi.org/10.3390/nu15051095






