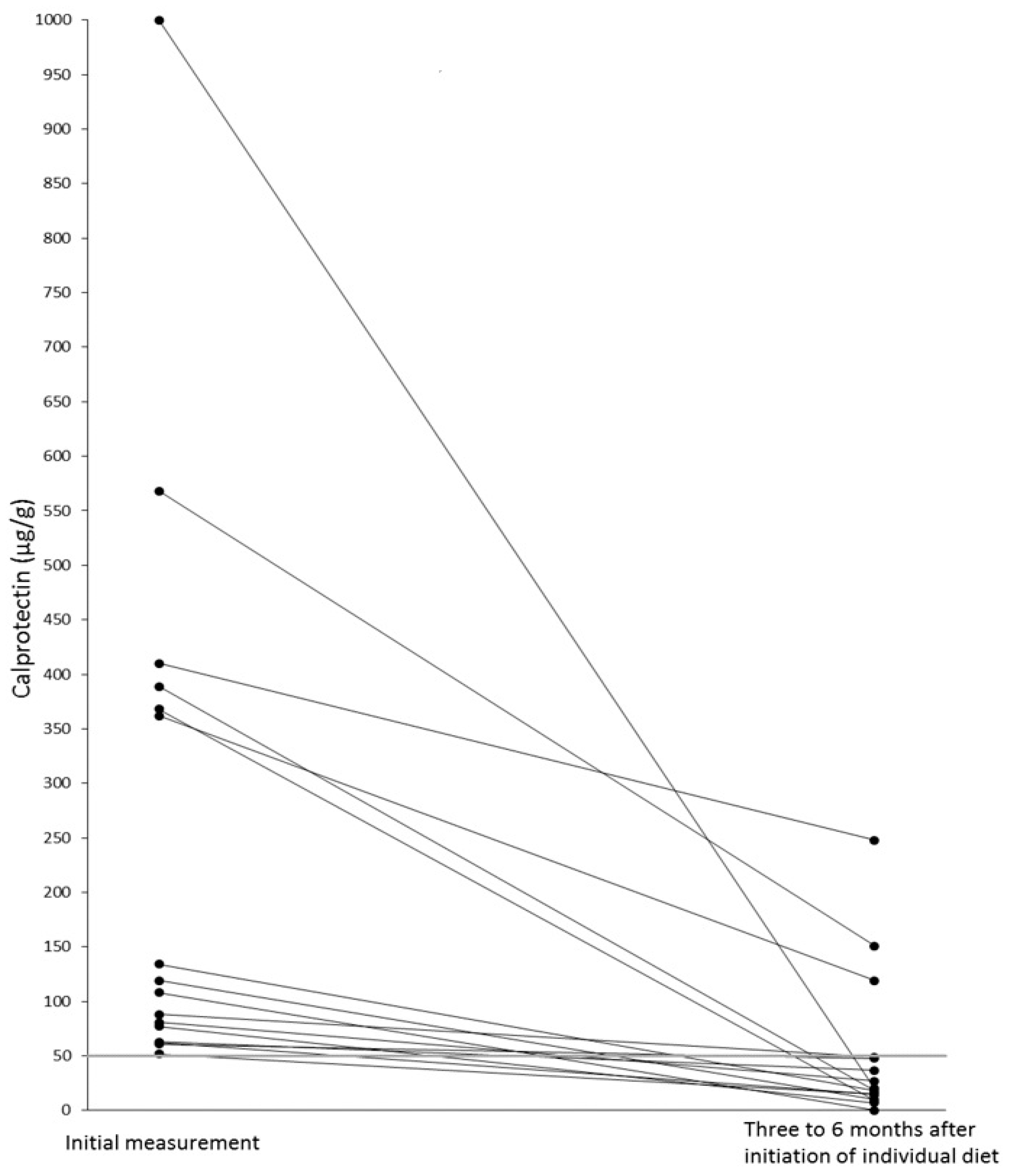
Fecal Calprotectin Elevations Associated with Food Intolerance/Malabsorption Are Significantly Reduced with Targeted Diets
Abstract
1. Introduction
2. Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Deputy, M.; Devanaboina, R.; Al Bakir, I.; Burns, E.; Faiz, O. The role of faecal calprotectin in the diagnosis of inflammatory bowel disease. BMJ 2023, 380, e068947. [Google Scholar] [CrossRef] [PubMed]
- Adolph, T.; Meyer, M.; Schwärzler, J.; Mayr, L.; Grabherr, F.; Tilg, H. The metabolic nature of inflammatory bowel diseases. Nat. Rev. Gastroenterol. Hepatol. 2022, 19, 753–767. [Google Scholar] [CrossRef] [PubMed]
- Manceau, H.; Chicha-Cattoir, V.; Puy, H.; Peoc’h, K. Faecal calprotectin in inflammatory bowel diseases: Update and perspectives. Clin. Chem. Lab. Med. 2017, 55, 474–483. [Google Scholar] [CrossRef]
- Campbell, J.P.; Zierold, C.; Rode, A.; Blocki, F.A.; Vaughn, B.P. Clinical performance of a novel LIAISON fecal calprotectin assay for differentiation of inflammatory bowel disease from irritable bowel syndrome. J. Clin. Gastroenterol. 2021, 55, 239–243. [Google Scholar] [CrossRef] [PubMed]
- Camilleri, M. Diagnosis and treatment of irritable bowel syndrome. A review. JAMA 2021, 325, 865–877. [Google Scholar] [CrossRef]
- Schnedl, W.J.; Meier-Allard, N.; Lackner, S.; Enko, D.; Mangge, H.; Holasek, S.J. Increasing expiratory hydrogen in lactose intolerance is associated with additional food intolerance/malabsorption. Nutrients 2020, 12, 3690. [Google Scholar] [CrossRef]
- Schulz, C.; Kupčinskas, J. Review—Helicobacter pylori and non-malignant upper gastrointestinal diseases. Helicobacter 2020, 25 (Suppl. S1), e12738. [Google Scholar] [CrossRef] [PubMed]
- Storhaug, C.L.; Fosse, S.K.; Fadnes, L.T. Country, regional, and global estimates for lactose malabsorption in adults: A systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 2017, 2, 738–746. [Google Scholar] [CrossRef]
- Lasson, A.; Stotzer, P.O.; Öhman, L.; Isaksson, S.; Sapnara, M.; Strid, H. The intra-individual variability of faecal calprotectin: A prospective study in patients with active ulcerative colitis. J. Crohns Colitis 2015, 9, 26–32. [Google Scholar] [CrossRef]
- Wenzel, R.R.; Datz, C. Association of sprue-like enteropathy and angiotensin receptor-1 antagonists. Wien. Klin. Wochenschr. 2019, 131, 493–501. [Google Scholar] [CrossRef]
- Camilleri, M. Irritable bowel syndrome: Straightening the road from the Rome criteria. Neurogastroenterol. Motil. 2020, 32, e13957. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, A.; Shah, A.; Jones, M.P.; Koloski, N.; Talley, N.J.; Morrison, M.; Holtmann, G. Methane positive small intestinal bacterial overgrowth in inflammatory bowel disease and irritable bowel syndrome: A systematic review and meta-analysis. Gut Microbes 2021, 13, 1933313. [Google Scholar] [CrossRef] [PubMed]
- Savarino, E.; Zingone, F.; Barberio, B.; Marasco, G.; Akyuz, F.; Akpinar, H.; Barboi, O.; Bodini, G.; Bor, S.; Chiarioni, G.; et al. Functional bowel disorders with diarrhoea: Clinical guidelines of the United European Gastroenterology and European Society for Neurogastroenterology and Motility. United Eur. Gastroenterol. J. 2022, 10, 556–584. [Google Scholar] [CrossRef] [PubMed]
- Carrasco-Labra, A.; Lytvyn, L.; Falck-Ytter, Y.; Surawicz, C.M.; Chey, W.D. AGA technical review on the evaluation of functional diarrhea and diarrhea-predominant irritable bowel syndrome in adults (IBS-D). Gastroenterology 2019, 157, 859–880. [Google Scholar] [CrossRef] [PubMed]
- Zollner, A.; Schmiderer, A.; Reider, S.; Oberhuber, G.; Pfister, A.; Texler, B.; Watschinger, C.; Koch, R.; Effenberger, M.; Raine, T.; et al. Faecal biomarkers in inflammatory bowel diseases: Calprotectin versus lipocalin-2-a comparative study. J. Crohns Colitis 2021, 15, 43–54. [Google Scholar] [CrossRef]
- Xiang, B.J.; Jiang, M.; Sun, M.J.; Dai, C. Optimal range of fecal calprotectin for predicting mucosal healing in patients with inflammatory bowel disease: A systematic review and meta-analysis. Visc. Med. 2021, 37, 338–348. [Google Scholar] [CrossRef] [PubMed]
- Jansson-Knodell, C.L.; Krajicek, E.J.; Ramakrishnan, M.; Rogers, N.A.; Siwiec, R.; Bohm, M.; Nowak, T.; Wo, J.; Lockett, C.; Xu, H.; et al. Relationships of intestinal lactase and the small intestinal microbiome with symptoms of lactose intolerance and intake in adults. Dig. Dis. Sci. 2022, 67, 5617–5627. [Google Scholar] [CrossRef]
- Sánchez-Pérez, S.; Comas-Basté, O.; Duelo, A.; Veciana-Nogués, M.T.; Berlanga, M.; Latorre-Moratalla, M.L.; Vidal-Carou, M.C. Intestinal dysbiosis in patients with histamine intolerance. Nutrients 2022, 14, 1774. [Google Scholar] [CrossRef]
- Basu, S.; Liu, C.; Zhou, X.K.; Nishiguchi, R.; Ha, T.; Chen, J.; Johncilla, M.; Yantiss, R.K.; Montrose, D.C.; Dannenberg, A.J. GLUT5 is a determinant of dietary fructose-mediated exacerbation of experimental colitis. Am. J. Physiol. Gastrointest. Liver Physiol. 2021, 321, G232–G242. [Google Scholar] [CrossRef]
- Perets, T.T.M.; Ben Simon, S.; Ashoro, O.; Hamouda, D.; Dickman, R.; Turjeman, S. Lasting effects of helicobacter pylori infection on the microbial communities of patients with and without small intestinal bacterial overgrowth. New Microbiol. 2022, 45, 193–198. [Google Scholar]
- Schnedl, W.J.; Meier-Allard, N.; Schenk, M.; Lackner, S.; Enko, D.; Mangge, H.; Holasek, S.J. Helicobacter pylori infection and lactose intolerance increase expiratory hydrogen. EXCLI J. 2022, 21, 426–435. [Google Scholar] [PubMed]
- Deng, Y.; Misselwitz, B.; Dai, N.; Fox, M. Lactose intolerance in adults: Biological mechanism and dietary management. Nutrients 2015, 7, 8020–8035. [Google Scholar] [CrossRef] [PubMed]
- Enko, D.; Meinitzer, A.; Mangge, H.; Kriegshäuser, G.; Halwachs-Baumann, G.; Reininghaus, E.Z.; Bengesser, S.A.; Schnedl, W.J. Concomitant prevalence of low serum diamine oxidase activity and carbohydrate malabsorption. Can. J. Gastroenterol. Hepatol. 2016, 2016, 4893501. [Google Scholar]
- Jukic, A.; Bakiri, L.; Wagner, E.F.; Tilg, H.; Adolph, T.E. Calprotectin: From biomarker to biological function. Gut 2021, 70, 1978–1988. [Google Scholar] [CrossRef]
- Dolovich, C.; Shafer, L.A.; Vagianos, K.; Witges, K.; Targownik, L.E.; Bernstein, C.N. The complex relationship between diet, symptoms, and intestinal inflammation in persons with inflammatory bowel disease: The Manitoba living with IBD study. JPEN J. Parenter. Enteral Nutr. 2022, 46, 867–877. [Google Scholar] [CrossRef] [PubMed]
- Burns, G.L.; Talley, N.J.; Keely, S. Immune responses in the irritable bowel syndromes: Time to consider the small intestine. BMC Med. 2022, 20, 115. [Google Scholar] [CrossRef]
- Forget, P.; Grandfils, C.; van Cutsem, J.L.; Dandrifosse, G. Diamine oxidase and disaccharidase activities in small intestinal biopsies of children. Pediatr. Res. 1984, 18, 647–649. [Google Scholar] [CrossRef]
- Schnedl, W.J.; Meier-Allard, N.; Michaelis, S.; Lackner, S.; Enko, D.; Mangge, H.; Holasek, S.J. Serum diamine oxidase values, indicating histamine intolerance, influence lactose tolerance breath test results. Nutrients 2022, 14, 2026. [Google Scholar] [CrossRef] [PubMed]
- Kerimi, A.; Gauer, J.S.; Crabbe, S.; Cheah, J.W.; Lau, J.; Walsh, R.; Cancalon, P.F.; Williamson, G. Effect of the flavonoid hesperidin on glucose and fructose transport, sucrase activity and glycaemic response to orange juice in a crossover trial on healthy volunteers. Br. J. Nutr. 2019, 121, 782–792. [Google Scholar] [CrossRef]
| Food Intolerance/Malabsorption | Number (n) of Patients | Percent (%) of Patients | Number (n) of Patients with High FCAL | Percent (%) of Patients with High FCAL |
|---|---|---|---|---|
| Number of patients | 228 | 100 | 39 | 17.1 |
| LIT-only | 49 | 21.5 | 14 | 28.6 |
| FM-only | 22 | 9.6 | 3 | 13.6 |
| HIT-only | 29 | 12.7 | 6 | 20.7 |
| H. pylori-only | 10 | 4.4 | 0 | 0 |
| LIT + FM | 18 | 7.9 | 2 | 11.1 |
| LIT + FM + HIT | 21 | 9.2 | 1 | 4.8 |
| LIT + HIT | 34 | 14.9 | 5 | 14.7 |
| LIT + H. pylori | 14 | 6.1 | 4 | 28.6 |
| LIT + HIT + H. pylori | 4 | 1.7 | 0 | 0 |
| LIT + FM + H. pylori | 5 | 2.2 | 0 | 0 |
| LIT + FM + HIT + H. pylori | 2 | 0.9 | 0 | 0 |
| FM + HIT | 11 | 4.8 | 1 | 9.1 |
| FM + HIT + H. pylori | 5 | 2.2 | 0 | 0 |
| FM + H. pylori | 1 | 0.4 | 1 | 100 |
| HIT + H. pylori | 2 | 0.9 | 1 | 50 |
| Candesartan | 1 | 0.4 | 1 | 100 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schnedl, W.J.; Michaelis, S.; Enko, D.; Mangge, H. Fecal Calprotectin Elevations Associated with Food Intolerance/Malabsorption Are Significantly Reduced with Targeted Diets. Nutrients 2023, 15, 1179. https://doi.org/10.3390/nu15051179
Schnedl WJ, Michaelis S, Enko D, Mangge H. Fecal Calprotectin Elevations Associated with Food Intolerance/Malabsorption Are Significantly Reduced with Targeted Diets. Nutrients. 2023; 15(5):1179. https://doi.org/10.3390/nu15051179
Chicago/Turabian StyleSchnedl, Wolfgang J., Simon Michaelis, Dietmar Enko, and Harald Mangge. 2023. "Fecal Calprotectin Elevations Associated with Food Intolerance/Malabsorption Are Significantly Reduced with Targeted Diets" Nutrients 15, no. 5: 1179. https://doi.org/10.3390/nu15051179
APA StyleSchnedl, W. J., Michaelis, S., Enko, D., & Mangge, H. (2023). Fecal Calprotectin Elevations Associated with Food Intolerance/Malabsorption Are Significantly Reduced with Targeted Diets. Nutrients, 15(5), 1179. https://doi.org/10.3390/nu15051179







