Impact of a Low-Insulin-Stimulating Bread on Weight Development—A Real Life Randomised Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
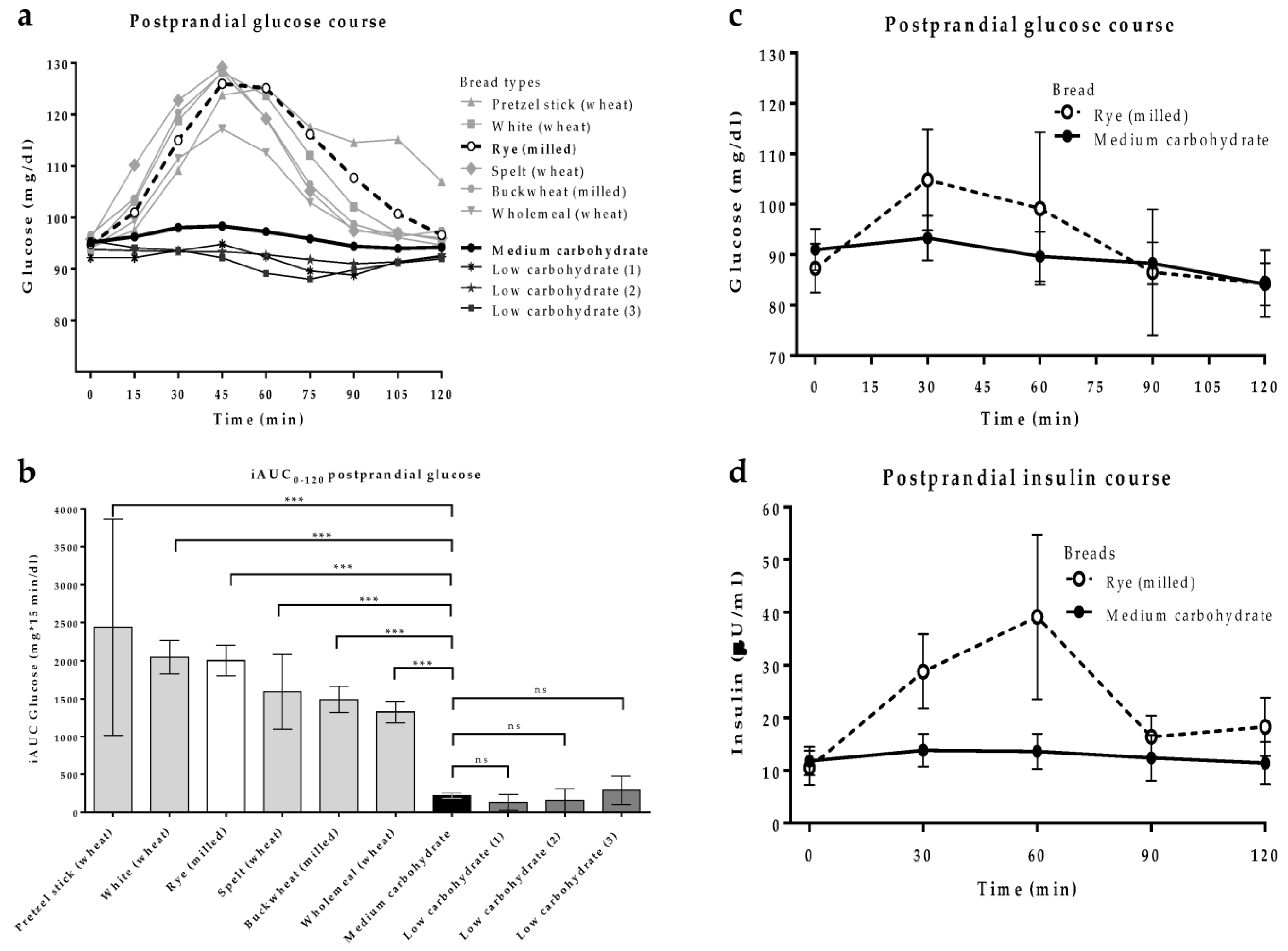
2.2. Pre-Tests
2.3. Randomisation and Masking
2.4. Procedures
2.5. Outcomes
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cust, A.E.; Skilton, M.R.; van Bakel, M.M.; Halkjaer, J.; Olsen, A.; Agnoli, C.; Psaltopoulou, T.; Buurma, E.; Sonestedt, E.; Chirlaque, M.D.; et al. Total dietary carbohydrate, sugar, starch and fibre intakes in the European Prospective Investigation into Cancer and Nutrition. Eur. J. Clin. Nutr. 2009, 63 (Suppl. S4), S37–S60. [Google Scholar] [CrossRef]
- Goletzke, J.; Atkinson, F.S.; Ek, K.L.; Bell, K.; Brand-Miller, J.C.; Buyken, A.E. Glycaemic and insulin index of four common German breads. Eur. J. Clin. Nutr. 2016, 70, 808–811. [Google Scholar] [CrossRef] [PubMed]
- Serra-Majem, L.; Bautista-Castano, I. Relationship between bread and obesity. Br. J. Nutr. 2015, 113 (Suppl S2), S29–S35. [Google Scholar] [CrossRef] [PubMed]
- Fardet, A. A shift toward a new holistic paradigm will help to preserve and better process grain products’ food structure for improving their health effects. Food Funct. 2015, 6, 363–382. [Google Scholar] [CrossRef]
- Bautista-Castano, I.; Serra-Majem, L. Relationship between bread consumption, body weight, and abdominal fat distribution: Evidence from epidemiological studies. Nutr. Rev. 2012, 70, 218–233. [Google Scholar] [CrossRef]
- Bautista-Castano, I.; Sanchez-Villegas, A.; Estruch, R.; Martinez-Gonzalez, M.A.; Corella, D.; Salas-Salvado, J.; Covas, M.I.; Schroder, H.; Alvarez-Perez, J.; Quilez, J.; et al. Changes in bread consumption and 4-year changes in adiposity in Spanish subjects at high cardiovascular risk. Br. J. Nutr. 2013, 110, 337–346. [Google Scholar] [CrossRef] [Green Version]
- Jacob, S.; Hauer, B.; Becker, R.; Artzner, S.; Grauer, P.; Loblein, K.; Nielsen, M.; Renn, W.; Rett, K.; Wahl, H.G.; et al. Lipolysis in skeletal muscle is rapidly regulated by low physiological doses of insulin. Diabetologia 1999, 42, 1171–1174. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kolb, H.; Martin, S. Environmental/lifestyle factors in the pathogenesis and prevention of type 2 diabetes. BMC Med. 2017, 15, 131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kolb, H.; Stumvoll, M.; Kramer, W.; Kempf, K.; Martin, S. Insulin translates unfavourable lifestyle into obesity. BMC Med. 2018, 16, 232. [Google Scholar] [CrossRef] [Green Version]
- Boden, G.; Homko, C.; Barrero, C.A.; Stein, T.P.; Chen, X.; Cheung, P.; Fecchio, C.; Koller, S.; Merali, S. Excessive caloric intake acutely causes oxidative stress, GLUT4 carbonylation, and insulin resistance in healthy men. Sci. Transl. Med. 2015, 7, 304re7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kolb, H.; Kempf, K.; Röhling, M.; Martin, S. Insulin: Too much of a good thing is bad. BMC Med. 2020, 18, 224. [Google Scholar] [CrossRef] [PubMed]
- Röhling, M.; Kempf, K.; Kolb, H.; Martin, T.; Schneider, M.; Martin, S. The Epidemiological Boehringer Ingelheim Employee Study (Part 3): Association of Elevated Fasting Insulin Levels but Not HOMA-IR With Increased Intima Media Thickness and Arteriosclerosis in Middle-Aged Persons. Front. Cardiovasc. Med. 2021, 8, 752789. [Google Scholar] [CrossRef] [PubMed]
- Czech, M.P. Insulin action and resistance in obesity and type 2 diabetes. Nat. Med. 2017, 23, 804–814. [Google Scholar] [CrossRef]
- Zhang, X.; Li, J.; Zheng, S.; Luo, Q.; Zhou, C.; Wang, C. Fasting insulin, insulin resistance, and risk of cardiovascular or all-cause mortality in non-diabetic adults: A meta-analysis. Biosci. Rep. 2017, 37, BSR20170947. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Röhling, M.; Martin, K.; Ellinger, S.; Schreiber, M.; Martin, S.; Kempf, K. Weight Reduction by the Low-Insulin-Method-A Randomized Controlled Trial. Nutrients 2020, 12, 3004. [Google Scholar] [CrossRef]
- Halle, M.; Röhling, M.; Banzer, W.; Braumann, K.M.; Kempf, K.; McCarthy, D.; Schaller, N.; Predel, H.G.; Scholze, J.; Fuhrer-Sakel, D.; et al. Meal replacement by formula diet reduces weight more than a lifestyle intervention alone in patients with overweight or obesity and accompanied cardiovascular risk factors-the ACOORH trial. Eur. J. Clin. Nutr. 2021, 75, 661–669. [Google Scholar] [CrossRef]
- Yang, Q.; Lang, X.; Li, W.; Liang, Y. The effects of low-fat, high-carbohydrate diets vs. low-carbohydrate, high-fat diets on weight, blood pressure, serum liquids and blood glucose: A systematic review and meta-analysis. Eur. J. Clin. Nutr. 2022, 76, 16–27. [Google Scholar] [CrossRef]
- Goldenberg, J.Z.; Day, A.; Brinkworth, G.D.; Sato, J.; Yamada, S.; Jonsson, T.; Beardsley, J.; Johnson, J.A.; Thabane, L.; Johnston, B.C. Efficacy and safety of low and very low carbohydrate diets for type 2 diabetes remission: Systematic review and meta-analysis of published and unpublished randomized trial data. BMJ 2021, 372, m4743. [Google Scholar] [CrossRef]
- Hyde, P.N.; Sapper, T.N.; Crabtree, C.D.; LaFountain, R.A.; Bowling, M.L.; Buga, A.; Fell, B.; McSwiney, F.T.; Dickerson, R.M.; Miller, V.J.; et al. Dietary carbohydrate restriction improves metabolic syndrome independent of weight loss. JCI Insight 2019, 4, e128308. [Google Scholar] [CrossRef] [Green Version]
- Kempf, K.; Röhling, M.; Banzer, W.; Braumann, K.M.; Halle, M.; McCarthy, D.; Predel, H.G.; Schenkenberger, I.; Tan, S.; Toplak, H.; et al. High-Protein, Low-Glycaemic Meal Replacement Decreases Fasting Insulin and Inflammation Markers-A 12-Month Subanalysis of the ACOORH Trial. Nutrients 2021, 13, 1433. [Google Scholar] [CrossRef]
- Kempf, K.; Röhling, M.; Banzer, W.; Braumann, K.M.; Halle, M.; Schaller, N.; McCarthy, D.; Predel, H.G.; Schenkenberger, I.; Tan, S.; et al. Early and Strong Leptin Reduction Is Predictive for Long-Term Weight Loss during High-Protein, Low-Glycaemic Meal Replacement-A Subanalysis of the Randomised-Controlled ACOORH Trial. Nutrients 2022, 14, 2537. [Google Scholar] [CrossRef] [PubMed]
- Ludwig, D.S.; Aronne, L.J.; Astrup, A.; de Cabo, R.; Cantley, L.C.; Friedman, M.I.; Heymsfield, S.B.; Johnson, J.D.; King, J.C.; Krauss, R.M.; et al. The carbohydrate-insulin model: A physiological perspective on the obesity pandemic. Am. J. Clin. Nutr. 2021, 114, 1873–1885. [Google Scholar] [CrossRef]
- Jacobs, D.R., Jr.; Meyer, K.A.; Kushi, L.H.; Folsom, A.R. Whole-grain intake may reduce the risk of ischemic heart disease death in postmenopausal women: The Iowa Women’s Health Study. Am. J. Clin. Nutr. 1998, 68, 248–257. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, S.; Willett, W.C.; Manson, J.E.; Hu, F.B.; Rosner, B.; Colditz, G. Relation between changes in intakes of dietary fiber and grain products and changes in weight and development of obesity among middle-aged women. Am. J. Clin. Nutr. 2003, 78, 920–927. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fuente-Arrillaga, C.; Martinez-Gonzalez, M.A.; Zazpe, I.; Vazquez-Ruiz, Z.; Benito-Corchon, S.; Bes-Rastrollo, M. Glycemic load, glycemic index, bread and incidence of overweight/obesity in a Mediterranean cohort: The SUN project. BMC Public Health 2014, 14, 1091. [Google Scholar] [CrossRef] [Green Version]
- Schutte, S.; Esser, D.; Hoevenaars, F.P.M.; Hooiveld, G.J.E.J.; Priebe, M.G.; Vonk, R.J.; Wopereis, S.; Afman, L.A. A 12-wk whole-grain wheat intervention protects against hepatic fat: The Graandioos study, a randomized trial in overweight subjects. Am. J. Clin. Nutr. 2018, 108, 1264–1274. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cho, S.; Dietrich, M.; Brown, C.J.; Clark, C.A.; Block, G. The effect of breakfast type on total daily energy intake and body mass index: Results from the Third National Health and Nutrition Examination Survey (NHANES III). J. Am. Coll. Nutr. 2003, 22, 296–302. [Google Scholar] [CrossRef]
- Slavin, J. Whole grains and human health. Nutr. Res. Rev. 2004, 17, 99–110. [Google Scholar] [CrossRef] [Green Version]
- Gil, A.; Ortega, R.M.; Maldonado, J. Wholegrain cereals and bread: A duet of the Mediterranean diet for the prevention of chronic diseases. Public Health Nutr. 2011, 14, 2316–2322. [Google Scholar] [CrossRef] [Green Version]
- Röhling, M.; Martin, T.; Wonnemann, M.; Kragl, M.; Klein, H.H.; Heinemann, L.; Martin, S.; Kempf, K. Determination of Postprandial Glycemic Responses by Continuous Glucose Monitoring in a Real-World Setting. Nutrients 2019, 11, 2305. [Google Scholar] [CrossRef] [Green Version]
- Kempf, K.; Kolb, H.; Gartner, B.; Bytof, G.; Stiebitz, H.; Lantz, I.; Lang, R.; Hofmann, T.; Martin, S. Cardiometabolic effects of two coffee blends differing in content for major constituents in overweight adults: A randomized controlled trial. Eur. J. Nutr. 2015, 54, 845–854. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Anton, C.; Artacho, R.; Ruiz-Lopez, M.D.; Gil, A.; Mesa, M.D. Modification of appetite by bread consumption: A systematic review of randomized controlled trials. Crit. Rev. Food Sci. Nutr. 2017, 57, 3035–3050. [Google Scholar] [CrossRef] [PubMed]
- O’Neil, C.E.; Keast, D.R.; Fulgoni, V.L.; Nicklas, T.A. Food sources of energy and nutrients among adults in the US: NHANES 2003–2006. Nutrients 2012, 4, 2097–2120. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Papanikolaou, Y.; Fulgoni, V.L. Grain Foods Are Contributors of Nutrient Density for American Adults and Help Close Nutrient Recommendation Gaps: Data from the National Health and Nutrition Examination Survey, 2009–2012. Nutrients 2017, 9, 873. [Google Scholar] [CrossRef] [Green Version]
- Guo, H.; Wu, H.; Sajid, A.; Li, Z. Whole grain cereals: The potential roles of functional components in human health. Crit. Rev. Food Sci. Nutr. 2022, 62, 8388–8402. [Google Scholar] [CrossRef]
- Kempf, K.; Altpeter, B.; Berger, J.; Reuss, O.; Fuchs, M.; Schneider, M.; Gartner, B.; Niedermeier, K.; Martin, S. Efficacy of the Telemedical Lifestyle intervention Program TeLiPro in Advanced Stages of Type 2 Diabetes: A Randomized Controlled Trial. Diabetes Care 2017, 40, 863–871. [Google Scholar] [CrossRef] [Green Version]
- Page, M.M.; Skovso, S.; Cen, H.; Chiu, A.P.; Dionne, D.A.; Hutchinson, D.F.; Lim, G.E.; Szabat, M.; Flibotte, S.; Sinha, S.; et al. Reducing insulin via conditional partial gene ablation in adults reverses diet-induced weight gain. FASEB J. 2018, 32, 1196–1206. [Google Scholar] [CrossRef] [Green Version]
- Ludwig, D.S.; Ebbeling, C.B. The Carbohydrate-Insulin Model of Obesity: Beyond “Calories In, Calories Out”. East Afr. Med. 2018, 178, 1098–1103. [Google Scholar] [CrossRef]
- Mansoor, N.; Vinknes, K.J.; Veierod, M.B.; Retterstol, K. Effects of low-carbohydrate diets v. low-fat diets on body weight and cardiovascular risk factors: A meta-analysis of randomised controlled trials. Br. J. Nutr. 2016, 115, 466–479. [Google Scholar] [CrossRef]
- Tobias, D.K.; Chen, M.; Manson, J.E.; Ludwig, D.S.; Willett, W.; Hu, F.B. Effect of low-fat diet interventions versus other diet interventions on long-term weight change in adults: A systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2015, 3, 968–979. [Google Scholar] [CrossRef] [Green Version]
- Scazzina, F.; Siebenhandl-Ehn, S.; Pellegrini, N. The effect of dietary fibre on reducing the glycaemic index of bread. Br. J. Nutr. 2013, 109, 1163–1174. [Google Scholar] [CrossRef] [PubMed]
- Akhtar, S.; Layla, A.; Sestili, P.; Ismail, T.; Afzal, K.; Rizvanov, A.A.; Asad, M.H.H.B. Glycemic and Insulinemic Responses of Vegetables and Beans Powders Supplemented Chapattis in Healthy Humans: A Randomized, Crossover Trial. BioMed Res. Int. 2019, 2019, 7425367. [Google Scholar] [CrossRef]
- Ratzmann, K.P.; Strese, J.; Kohnert, K.D.; Jahr, D.; Michaelis, D. Age-dependent relationship of fasting C-peptide concentration and insulin secretion in non-obese subjects with normal glucose tolerance. Exp. Clin. Endocrinol. Diabetes 1986, 88, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, D.J.; Wolever, T.M.; Taylor, R.H.; Barker, H.; Fielden, H.; Baldwin, J.M.; Bowling, A.C.; Newman, H.C.; Jenkins, A.L.; Goff, D.V. Glycemic index of foods: A physiological basis for carbohydrate exchange. Am. J. Clin. Nutr. 1981, 34, 362–366. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Breads (100 g) | Pretzel Stick 1 | White 1 | Rye 2 | Spelt 1 | Buck Wheat 2 | Whole- Meal 1 | MC | LC (1) | LC (2) | LC (3) |
|---|---|---|---|---|---|---|---|---|---|---|
| Energy (kcal) | 264 | 272 | 217 | 233 | 237 | 251 | 237 | 212 | 206 | 199 |
| Energy (kJ) | 1120 | 1153 | 917 | 985 | 998 | 1062 | 989 | 887 | 862 | 830 |
| Carbohydrate (g) | 49 | 54 | 44 | 42 | 49 | 38 | 14 | 3.0 | 4.4 | 3.0 |
| Sugar (g) | 1.2 | 1.4 | 0.8 | 0.8 | 1.2 | 7.0 | 1.9 | 1.7 | 0.9 | 1.6 |
| Total fat (g) | 3.7 | 1.7 | 0.8 | 1.7 | 4.8 | 1.2 | 14.6 | 7.8 | 7.8 | 5.9 |
| Saturated fatty acids (g) | 2.0 | 0.7 | 0.2 | 0.2 | 0.6 | <0.2 | 0.8 | 1.2 | 2.8 | 1.0 |
| Total protein (g) | 7.8 | 8.4 | 5.4 | 9.2 | 8.3 | 6.7 | 8.8 | 28 | 26 | 28 |
| Fiber (g) | 4.0 | 3.0 | 6.0 | 4.0 | 3.0 | 8.0 | 7.8 | 14 | 9.7 | 12.5 |
| Sodium (g) | 3.1 | 1.8 | 1.6 | 1.2 | 1.6 | 2.0 | 0.4 | 1.5 | 1.3 | 1.6 |
| Control Group (n = 40) | Intervention Group (n = 40) | |
|---|---|---|
| Sex (%) ♀/♂ | 62/38 | 45/55 |
| Age (years) | 55 ± 11 | 55 ± 8 |
| Weight (kg) | 98 ± 15 | 102 ± 24 |
| BMI (kg/m2) | 33.1 ± 4.2 | 34.1 ± 6.9 |
| Hip circumference (cm) ♀/♂ | 120 ± 12/115 ± 7 | 120 ± 15/115 ± 11 |
| Waist circumference (cm) ♀/♂ | 107 ± 11/117 ± 8 | 107 ± 12/119 ± 15 |
| Fat mass (%) | 42 ± 7 | 40 ± 8 |
| Fat-free mass (%) | 58 ± 7 | 60 ± 8 |
| Systolic blood pressure (mmHg) | 120 ± 10 | 123 ± 12 |
| Diastolic blood pressure (mmHg) | 68 ± 6 | 68 ± 7 |
| Fasting blood glucose (mg/dl) | 94 ± 12 | 103 ± 24 |
| Fasting insulin (µU/mL) | 12.1 (8.3; 18.2) | 16.1 (8.7; 23.1) |
| HbA1c (%) | 5.6 ± 0.4 | 5.8 ± 0.6 |
| Cholesterol (mg/dl) | 214 ± 36 | 207 ± 41 |
| HDL cholesterol (mg/dl) | 57 ± 15 | 53 ± 13 |
| LDL cholesterol (mg/dl) | 139 ± 35 | 137 ± 35 |
| Triglycerides (mg/dl) | 129 (80; 173) | 134 (97; 198) |
| Antidiabetic drugs (%) | 3 | 5 |
| Antihypertensive drugs (%) | 30 | 33 |
| Statins (%) | 8 | 3 |
| Smoker (none/former/active) (%) | 82/15/3 | 73/21/6 |
| Physical activity (0–1/2–3/4–5/>5 h/week) (%) | 20/42.5/20/17.5 | 12.5/30/32.5/25 |
| Diet (vegetarian/western/mediterranean) (%) | 3/85/12 | 6/87/7 |
| Bread (slices per day) | 3.5 | 3.5 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kempf, K.; Röhling, M.; Kolb, H.; Martin, S. Impact of a Low-Insulin-Stimulating Bread on Weight Development—A Real Life Randomised Controlled Trial. Nutrients 2023, 15, 1301. https://doi.org/10.3390/nu15051301
Kempf K, Röhling M, Kolb H, Martin S. Impact of a Low-Insulin-Stimulating Bread on Weight Development—A Real Life Randomised Controlled Trial. Nutrients. 2023; 15(5):1301. https://doi.org/10.3390/nu15051301
Chicago/Turabian StyleKempf, Kerstin, Martin Röhling, Hubert Kolb, and Stephan Martin. 2023. "Impact of a Low-Insulin-Stimulating Bread on Weight Development—A Real Life Randomised Controlled Trial" Nutrients 15, no. 5: 1301. https://doi.org/10.3390/nu15051301
APA StyleKempf, K., Röhling, M., Kolb, H., & Martin, S. (2023). Impact of a Low-Insulin-Stimulating Bread on Weight Development—A Real Life Randomised Controlled Trial. Nutrients, 15(5), 1301. https://doi.org/10.3390/nu15051301






