Kaempferol, a Phytoprogestin, Induces a Subset of Progesterone-Regulated Genes in the Uterus
Abstract
1. Introduction
2. Materials and Methods
2.1. Animal Study and Chemicals
2.2. Immunohistochemical Staining
2.3. RNA Isolation and RNA Sequencing Profiling
2.4. Statistical and Bioinformatics Analysis
3. Results
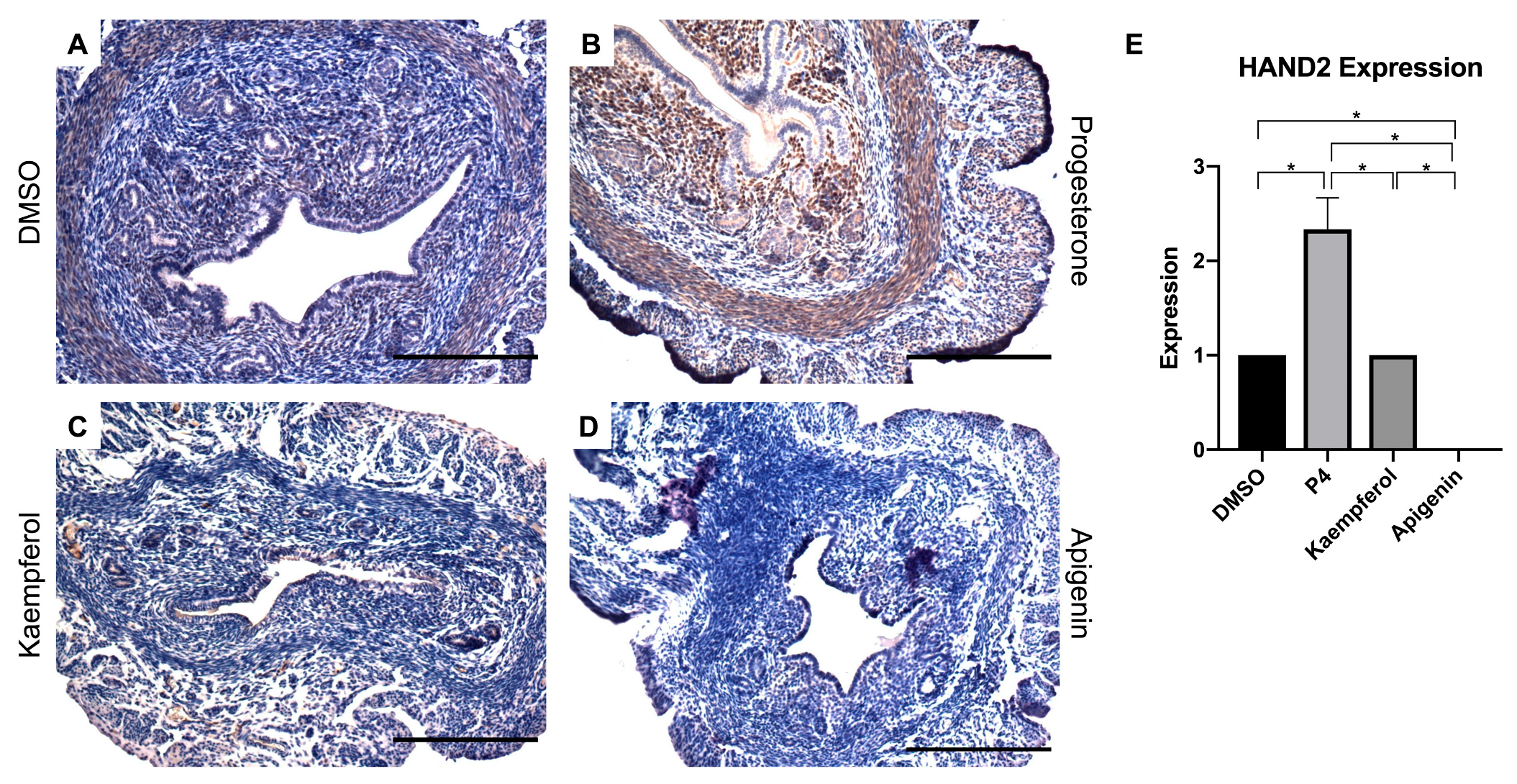
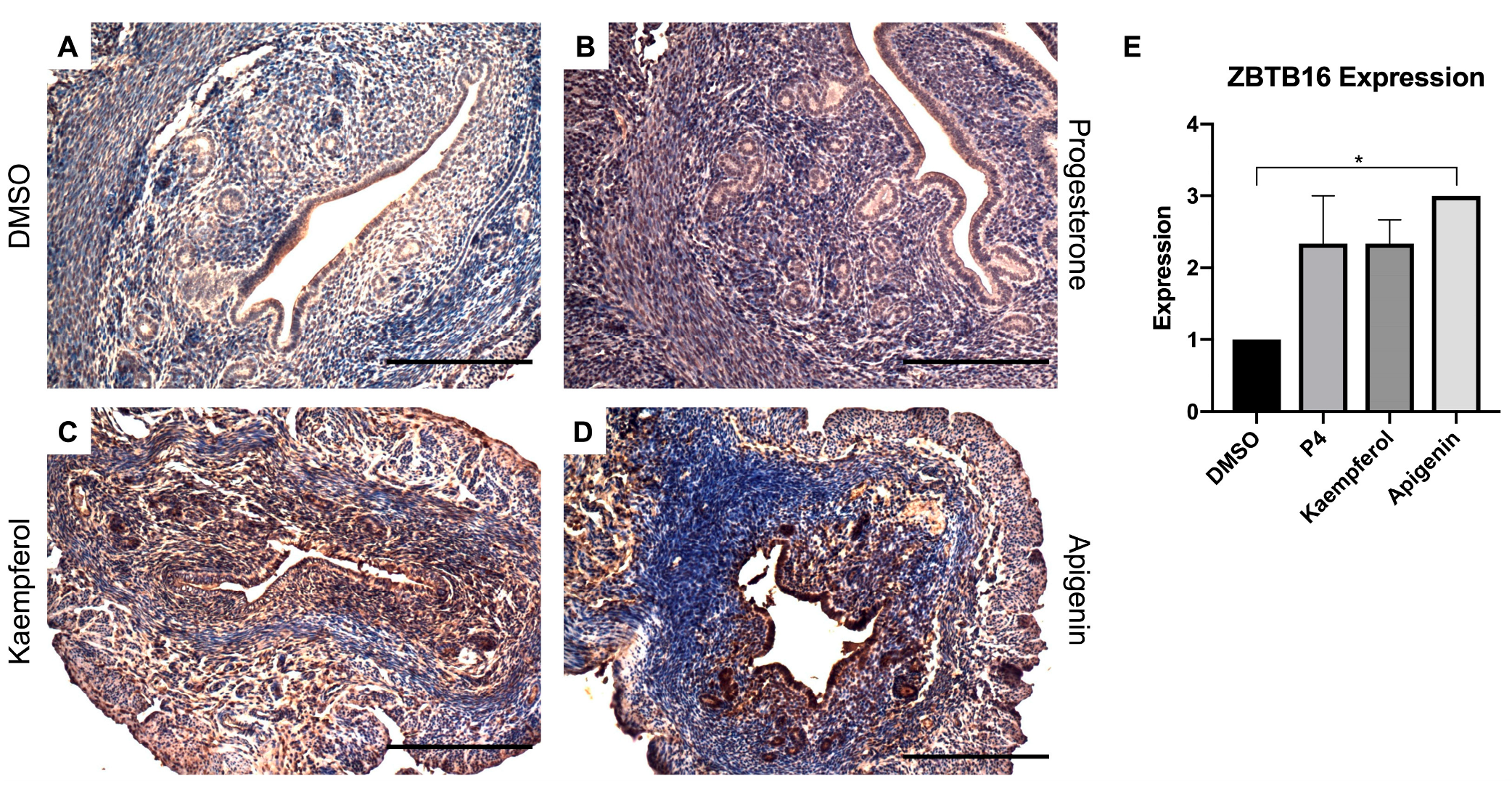
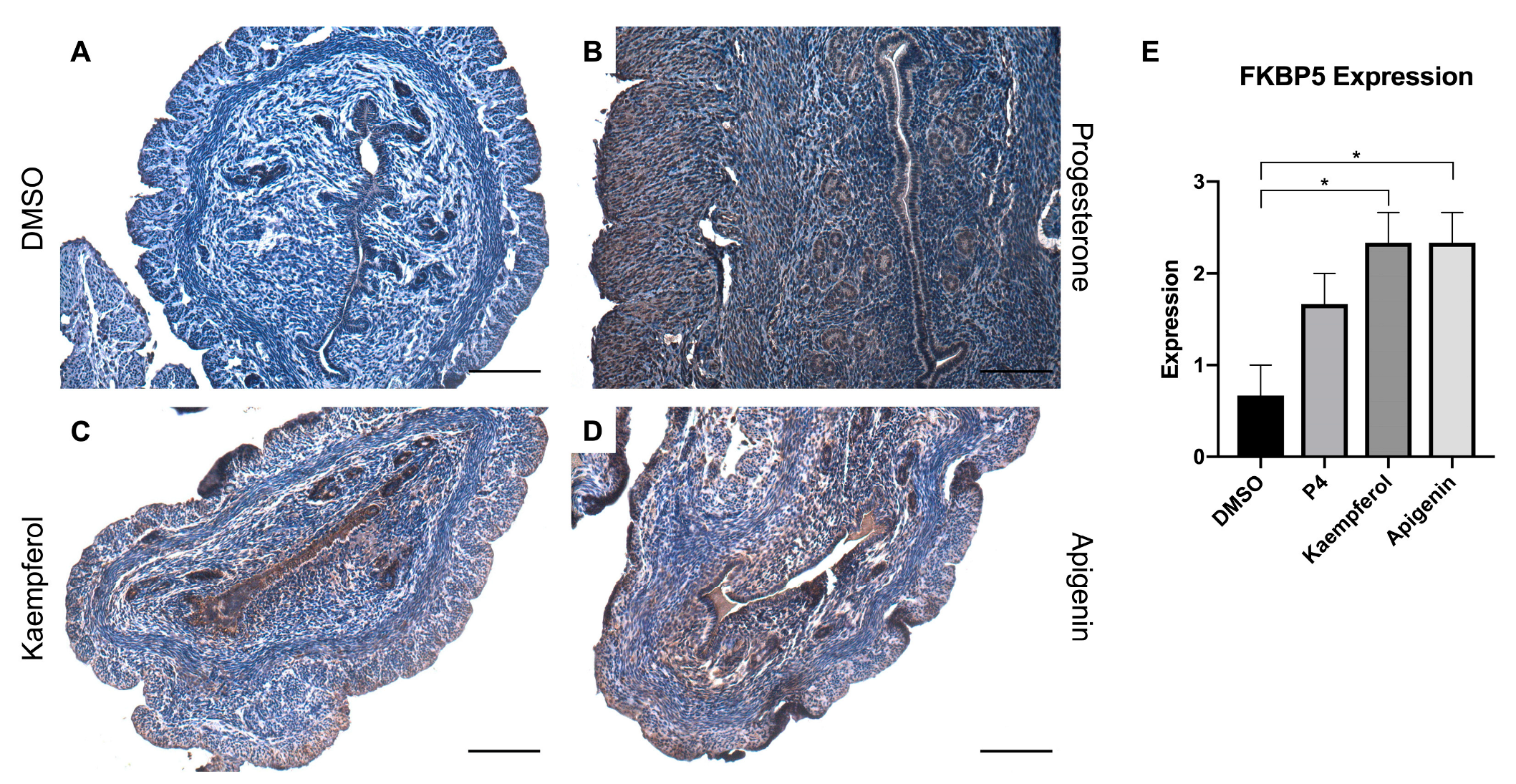
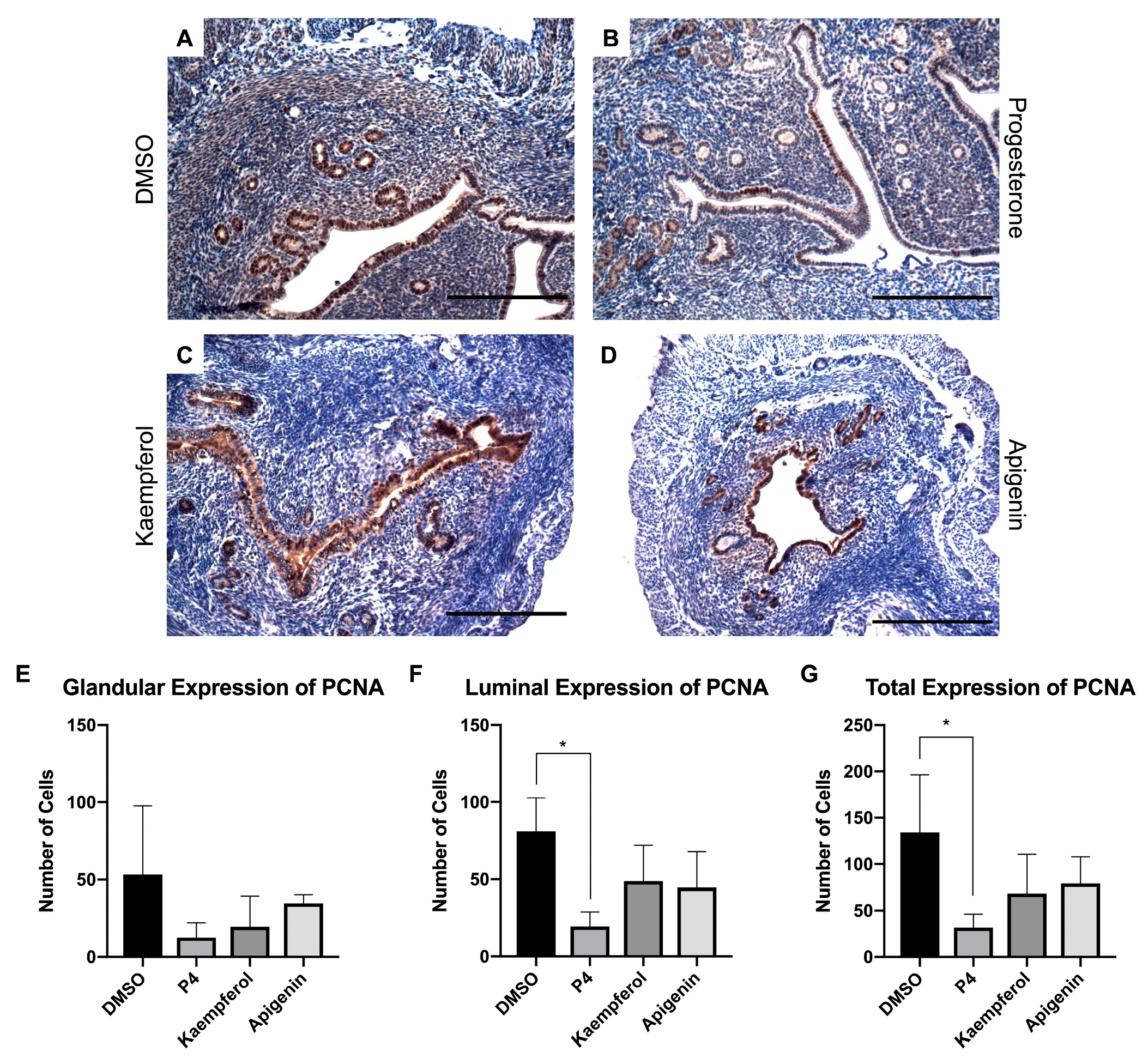
3.1. Kaempferol and Apigenin Have Progestogenic Activity In Vivo
3.2. Kaempferol and Progesterone Effects on mRNA Transcripts
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gronemeyer, H.; Meyer, M.E.; Bocquel, M.T.; Kastner, P.; Turcotte, B.; Chambon, P. Progestin receptors: Isoforms and antihormone action. J. Steroid Biochem. Mol. Biol. 1991, 40, 271–278. [Google Scholar] [CrossRef]
- Scarpin, K.M.; Graham, J.D.; Mote, P.A.; Clarke, C.L. Progesterone action in human tissues: Regulation by progesterone receptor (PR) isoform expression, nuclear positioning and coregulator expression. Nucl. Recept. Signal. 2009, 7, e009. [Google Scholar] [CrossRef] [PubMed]
- Diep, C.H.; Daniel, A.R.; Mauro, L.J.; Knutson, T.P.; Lange, C.A. Progesterone action in breast, uterine, and ovarian cancers. J. Mol. Endocrinol. 2015, 54, R31–R53. [Google Scholar] [CrossRef] [PubMed]
- Practice Committee of the American Society for Reproductive Medicine. Treatment of pelvic pain associated with endometriosis: A committee opinion. Fertil. Steril. 2014, 101, 927–935. [Google Scholar] [CrossRef]
- Dennehy, C.E. The use of herbs and dietary supplements in gynecology: An evidence-based review. J. Midwifery Womens Health 2006, 51, 402–409. [Google Scholar] [CrossRef]
- Dietz, B.M.; Hajirahimkhan, A.; Dunlap, T.L.; Bolton, J.L. Botanicals and Their Bioactive Phytochemicals for Women’s Health. Pharmacol. Rev. 2016, 68, 1026–1073. [Google Scholar] [CrossRef] [PubMed]
- Smith, T.; Majid, F.; Eckl, V.; Reynolds, C.M. Herbal Supplement Sales in US Increase by Record-Breaking 17.3% in 2020. HerbalGram 2021, 131, 52–65. [Google Scholar]
- Nie, Q.; Xing, M.; Hu, J.; Hu, X.; Nie, S.; Xie, M. Metabolism and health effects of phyto-estrogens. Crit. Rev. Food Sci. Nutr. 2017, 57, 2432–2454. [Google Scholar] [CrossRef]
- Dean, M.; Murphy, B.T.; Burdette, J.E. Phytosteroids beyond estrogens: Regulators of reproductive and endocrine function in natural products. Mol. Cell. Endocrinol. 2017, 442, 98–105. [Google Scholar] [CrossRef]
- Calderon-Montano, J.M.; Burgos-Moron, E.; Perez-Guerrero, C.; Lopez-Lazaro, M. A review on the dietary flavonoid kaempferol. Mini Rev. Med. Chem. 2011, 11, 298–344. [Google Scholar] [CrossRef]
- Ross, J.A.; Kasum, C.M. Dietary flavonoids: Bioavailability, metabolic effects, and safety. Annu. Rev. Nutr. 2002, 22, 19–34. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.K.; Kim, H.J.; Choi, S.E.; Park, K.H.; Choi, H.K.; Lee, M.W. Anti-oxidative and inhibitory activities on nitric oxide (NO) and prostaglandin E2 (COX-2) production of flavonoids from seeds of Prunus tomentosa Thunberg. Arch. Pharm. Res. 2008, 31, 424–428. [Google Scholar] [CrossRef] [PubMed]
- Hamalainen, M.; Nieminen, R.; Vuorela, P.; Heinonen, M.; Moilanen, E. Anti-inflammatory effects of flavonoids: Genistein, kaempferol, quercetin, and daidzein inhibit STAT-1 and NF-kappaB activations, whereas flavone, isorhamnetin, naringenin, and pelargonidin inhibit only NF-kappaB activation along with their inhibitory effect on iNOS expression and NO production in activated macrophages. Mediat. Inflamm. 2007, 2007, 45673. [Google Scholar]
- Luo, H.; Jiang, B.H.; King, S.M.; Chen, Y.C. Inhibition of cell growth and VEGF expression in ovarian cancer cells by flavonoids. Nutr. Cancer 2008, 60, 800–809. [Google Scholar] [CrossRef]
- Dean, M.; Austin, J.; Jinhong, R.; Johnson, M.E.; Lantvit, D.D.; Burdette, J.E. The Flavonoid Apigenin Is a Progesterone Receptor Modulator with In Vivo Activity in the Uterus. Horm. Cancer 2018, 9, 265–277. [Google Scholar] [CrossRef] [PubMed]
- Toh, M.F.; Mendonca, E.; Eddie, S.L.; Endsley, M.P.; Lantvit, D.D.; Petukhov, P.A.; Burdette, J.E. Kaempferol Exhibits Progestogenic Effects in Ovariectomized Rats. J. Steroids Horm. Sci. 2014, 5, 136. [Google Scholar]
- Li, K.; Diakite, D.; Austin, J.; Lee, J.-H.; Lantvit, D.D.; Murphy, B.T.; Burdette, J.E. The Flavonoid Baicalein Negatively Regulates Progesterone Target Genes in the Uterus in Vivo. J. Nat. Prod. 2022, 85, 237–247. [Google Scholar] [CrossRef]
- Wu, X.; Howard, M.J. Transcripts encoding HAND genes are differentially expressed and regulated by BMP4 and GDNF in developing avian gut. Gene Expr. 2002, 10, 279–293. [Google Scholar] [CrossRef]
- Li, Q.; Kannan, A.; DeMayo, F.J.; Lydon, J.P.; Cooke, P.S.; Yamagishi, H.; Srivastava, D.; Bagchi, M.K.; Bagchi, I.C. The antiproliferative action of progesterone in uterine epithelium is mediated by Hand2. Science 2011, 331, 912–916. [Google Scholar] [CrossRef]
- Fahnenstich, J.; Nandy, A.; Milde-Langosch, K.; Schneider-Merck, T.; Walther, N.; Gellersen, B. Promyelocytic leukaemia zinc finger protein (PLZF) is a glucocorticoid- and progesterone-induced transcription factor in human endometrial stromal cells and myometrial smooth muscle cells. Mol. Hum. Reprod. 2003, 9, 611–623. [Google Scholar] [CrossRef]
- Binder, E.B. The role of FKBP5, a co-chaperone of the glucocorticoid receptor in the pathogenesis and therapy of affective and anxiety disorders. Psychoneuroendocrinology 2009, 34 (Suppl. 1), S186–S195. [Google Scholar] [CrossRef] [PubMed]
- Wan, Y.; Nordeen, S.K. Identification of genes differentially regulated by glucocorticoids and progestins using a Cre/loxP-mediated retroviral promoter-trapping strategy. J. Mol. Endocrinol. 2002, 28, 177–192. [Google Scholar] [CrossRef] [PubMed]
- Kester, H.A.; van der Leede, B.M.; van der Saag, P.T.; van der Burg, B. Novel progesterone target genes identified by an improved differential display technique suggest that progestin-induced growth inhibition of breast cancer cells coincides with enhancement of differentiation. J. Biol. Chem. 1997, 272, 16637–16643. [Google Scholar] [CrossRef] [PubMed]
- Hubler, T.R.; Denny, W.B.; Valentine, D.L.; Cheung-Flynn, J.; Smith, D.F.; Scammell, J.G. The FK506-binding immunophilin FKBP51 is transcriptionally regulated by progestin and attenuates progestin responsiveness. Endocrinology 2003, 144, 2380–2387. [Google Scholar] [CrossRef]
- Hubler, T.R.; Scammell, J.G. Intronic hormone response elements mediate regulation of FKBP5 by progestins and glucocorticoids. Cell Stress Chaperones 2004, 9, 243–252. [Google Scholar] [CrossRef]
- Amler, L.C.; Agus, D.B.; LeDuc, C.; Sapinoso, M.L.; Fox, W.D.; Kern, S.; Lee, D.; Wang, V.; Leysens, M.; Higgins, B.; et al. Dysregulated expression of androgen-responsive and nonresponsive genes in the androgen-independent prostate cancer xenograft model CWR22-R1. Cancer Res. 2000, 60, 6134–6141. [Google Scholar]
- Mousses, S.; Wagner, U.; Chen, Y.; Kim, J.W.; Bubendorf, L.; Bittner, M.; Pretlow, T.; Elkahloun, A.G.; Trepel, J.B.; Kallioniemi, O.-P. Failure of hormone therapy in prostate cancer involves systematic restoration of androgen responsive genes and activation of rapamycin sensitive signaling. Oncogene 2001, 20, 6718–6723. [Google Scholar] [CrossRef]
- Zhu, W.; Zhang, J.S.; Young, C.Y. Silymarin inhibits function of the androgen receptor by reducing nuclear localization of the receptor in the human prostate cancer cell line LNCaP. Carcinogenesis 2001, 22, 1399–1403. [Google Scholar] [CrossRef]
- Subramanian, A.; Tamayo, P.; Mootha, V.K.; Mukherjee, S.; Ebert, B.L.; Gillette, M.A.; Paulovich, A.; Pomeroy, S.L.; Golub, T.R.; Lander, E.S.; et al. Gene set enrichment analysis: A knowledge-based approach for interpreting genome-wide expression profiles. Proc. Natl. Acad. Sci. USA 2005, 102, 15545–15550. [Google Scholar] [CrossRef]
- Mootha, V.K.; Lindgren, C.M.; Eriksson, K.-F.; Subramanian, A.; Sihag, S.; Lehar, J.; Puigserver, P.; Carlsson, E.; Ridderstråle, M.; Laurila, E.; et al. PGC-1alpha-responsive genes involved in oxidative phosphorylation are coordinately downregulated in human diabetes. Nat. Genet. 2003, 34, 267–273. [Google Scholar] [CrossRef]
- Park, H.-J.; Park, S.-J.; Koo, D.-B.; Lee, S.-R.; Kong, I.-K.; Ryoo, J.-W.; Park, Y.-I.; Chang, K.-T.; Lee, D.-S. Progesterone production is affected by unfolded protein response (UPR) signaling during the luteal phase in mice. Life Sci. 2014, 113, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Carambula, S.F.; Matikainen, T.; Lynch, M.P.; Flavell, R.A.; Dias Gonçalves, P.B.; Tilly, J.L.; Rueda, B.R. Caspase-3 is a pivotal mediator of apoptosis during regression of the ovarian corpus luteum. Endocrinology 2002, 143, 1495–1501. [Google Scholar] [CrossRef] [PubMed]
- Erzurumlu, Y.; Dogan, H.K.; Catakli, D. Progesterone regulates the endoplasmic reticulum-associated degradation and Unfolded Protein Response axis by mimicking the androgenic stimulation in prostate cancer cells. Mol. Biol. Rep. 2022, 50, 1253–1265. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.Y.; Jo, M.W.; Lee, E.Y.; Lee, D.Y.; Choi, D.S. Ovarian steroid dependence of endoplasmic reticulum stress involvement in endometrial cell apoptosis during the human endometrial cycle. Reproduction 2018, 155, 493–503. [Google Scholar] [CrossRef]
- Ghatge, R.P.; Jacobsen, B.M.; Schittone, S.A.; Horwitz, K.B. The progestational and androgenic properties of medroxyprogesterone acetate: Gene regulatory overlap with dihydrotestosterone in breast cancer cells. Breast Cancer Res. 2005, 7, R1036–R1050. [Google Scholar] [CrossRef]
- Toit, R.L.-d.; Perkins, M.S.; Hapgood, J.P.; Africander, D. Comparing the androgenic and estrogenic properties of progestins used in contraception and hormone therapy. Biochem. Biophys. Res. Commun. 2017, 491, 140–146. [Google Scholar] [CrossRef]
- Zhu, G.; Kang, L.; Wei, Q.; Cui, X.; Wang, S.; Chen, Y.; Jiang, Y. Expression and regulation of MMP1, MMP3, and MMP9 in the chicken ovary in response to gonadotropins, sex hormones, and TGFB1. Biol. Reprod. 2014, 90, 57. [Google Scholar] [CrossRef]
- Cornet, P.B.; Picquet, C.; Lemoine, P.; Osteen, K.G.; Bruner-Tran, K.L.; Tabibzadeh, S.; Courtoy, P.J.; Eeckhout, Y.; Marbaix, E.; Henriet, P. Regulation and function of LEFTY-A/EBAF in the human endometrium. mRNA expression during the menstrual cycle, control by progesterone, and effect on matrix metalloprotineases. J. Biol. Chem. 2002, 277, 42496–42504. [Google Scholar] [CrossRef]
- Tang, M.; Xu, Y.; Julian, J.; Carson, D.; Tabibzadeh, S. Lefty is expressed in mouse endometrium in estrous cycle and peri-implantation period. Hum. Reprod. 2005, 20, 872–880. [Google Scholar] [CrossRef]
- Cheng, X.; Liu, J.; Shan, H.; Sun, L.; Huang, C.; Yan, Q.; Jiang, R.; Ding, L.; Jiang, Y.; Zhou, J.; et al. Activating transcription factor 3 promotes embryo attachment via up-regulation of leukemia inhibitory factor in vitro. Reprod. Biol. Endocrinol. 2017, 15, 42. [Google Scholar] [CrossRef]
- Wang, Z.; Liu, Y.; Liu, J.; Kong, N.; Jiang, Y.; Jiang, R.; Zhen, X.; Zhou, J.; Li, C.; Sun, H.; et al. ATF3 deficiency impairs the proliferative-secretory phase transition and decidualization in RIF patients. Cell Death Dis. 2021, 12, 387. [Google Scholar] [CrossRef]
- Fujita, M.; Ogawa, S.; Fukuoka, H.; Tsukui, T.; Nemoto, N.; Tsutsumi, O.; Ouchi, Y.; Inoue, S. Differential expression of secreted frizzled-related protein 4 in decidual cells during pregnancy. J. Mol. Endocrinol. 2002, 28, 213–223. [Google Scholar] [CrossRef] [PubMed]
- Fitzgerald, H.C.; Evans, J.; Johnson, N.; Infusini, G.; Webb, A.; Rombauts, L.J.R.; Vollenhoven, B.J.; Salamonsen, A.L.; Edgell, A.T. Idiopathic infertility in women is associated with distinct changes in proliferative phase uterine fluid proteins. Biol. Reprod. 2018, 98, 752–764. [Google Scholar] [CrossRef] [PubMed]
- Pan, H.; Zhu, L.; Deng, Y.; Pollard, J.W. Microarray analysis of uterine epithelial gene expression during the implantation window in the mouse. Endocrinology 2006, 147, 4904–4916. [Google Scholar] [CrossRef] [PubMed]
- Hu, S.; Yao, G.; Wang, Y.; Xu, H.; Ji, X.; He, Y.; Zhu, Q.; Chen, Z.-J.; Sun, Y. Transcriptomic changes during the pre-receptive to receptive transition in human endometrium detected by RNA-Seq. J. Clin. Endocrinol. Metab. 2014, 99, E2744–E2753. [Google Scholar] [CrossRef]
- D’Aurora, M.; Romani, F.; Franchi, S.; Diomede, F.; Merciaro, I.; Impicciatore, G.G.; Trubiani, O.; Stuppia, L.; Tiboni, G.M.; Gatta, V. MRAP2 regulates endometrial receptivity and function. Gene 2019, 703, 7–12. [Google Scholar] [CrossRef]
- Carroll, J.S.; Meyer, C.A.; Song, J.; Li, W.; Geistlinger, T.R.; Eeckhoute, J.; Brodsky, A.S.; Keeton, E.K.; Fertuck, K.C.; Hall, G.F.; et al. Genome-wide analysis of estrogen receptor binding sites. Nat. Genet. 2006, 38, 1289–1297. [Google Scholar] [CrossRef]
- Frasor, J.; Danes, J.M.; Komm, B.; Chang, K.C.; Lyttle, C.R.; Katzenellenbogen, B.S. Profiling of estrogen up- and down-regulated gene expression in human breast cancer cells: Insights into gene networks and pathways underlying estrogenic control of proliferation and cell phenotype. Endocrinology 2003, 144, 4562–4574. [Google Scholar] [CrossRef]
- Gomez, H.L.; Felipe-Medina, N.; Sánchez-Martín, M.; Davies, O.R.; Ramos, I.; García-Tuñón, I.; De Rooij, D.G.; Dereli, I.; Tóth, A.; Barbero, J.L.; et al. C14ORF39/SIX6OS1 is a constituent of the synaptonemal complex and is essential for mouse fertility. Nat. Commun. 2016, 7, 13298. [Google Scholar] [CrossRef]
- Townley-Tilson, W.H.D.; Wu, Y.; Ferguson, J.E., 3rd; Patterson, C. The ubiquitin ligase ASB4 promotes trophoblast differentiation through the degradation of ID2. PLoS ONE 2014, 9, e89451. [Google Scholar] [CrossRef]
- Zhang, C.; Large, M.; Duggavathi, R.; DeMayo, F.J.; Lydon, J.P.; Schoonjans, K.; Kovanci, E.; Murphy, B.D. Liver receptor homolog-1 is essential for pregnancy. Nat. Med. 2013, 19, 1061–1066. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Cheng, D.; Liu, T.; Zhang, Y.; Chen, Z.J.; Zhang, C. Dysfunction of Liver Receptor Homolog-1 in Decidua: Possible Relevance to the Pathogenesis of Preeclampsia. PLoS ONE 2015, 10, e0145968. [Google Scholar] [CrossRef] [PubMed]
- Shen, F.; Zong, Z.H.; Liu, Y.; Chen, S.; Sheng, X.J.; Zhao, Y. CEMIP promotes ovarian cancer development and progression via the PI3K/AKT signaling pathway. Biomed. Pharmacother. 2019, 114, 108787. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Li, H.; Wang, Y.; Cao, L.; Zhan, X. Quantitative proteomics revealed energy metabolism pathway alterations in human epithelial ovarian carcinoma and their regulation by the antiparasite drug ivermectin: Data interpretation in the context of 3P medicine. EPMA J. 2020, 11, 661–694. [Google Scholar] [CrossRef] [PubMed]
- Tang, F.H.; Chang, W.A.; Tsai, E.M.; Tsai, M.J.; Kuo, P.L. Investigating Novel Genes Potentially Involved in Endometrial Adenocarcinoma using Next-Generation Sequencing and Bioinformatic Approaches. Int. J. Med. Sci. 2019, 16, 1338–1348. [Google Scholar] [CrossRef]
- Shi, S.; Tan, Q.; Feng, F.; Huang, H.; Liang, J.; Cao, D.; Wang, Z. Identification of core genes in the progression of endometrial cancer and cancer cell-derived exosomes by an integrative analysis. Sci. Rep. 2020, 10, 9862. [Google Scholar] [CrossRef] [PubMed]
- Cabrera-Cruz, H.; Orostica, L.; Plaza-Parrochia, F.; Torres-Pinto, I.; Romero, C.; Vega, M. The insulin-sensitizing mechanism of myo-inositol is associated with AMPK activation and GLUT-4 expression in human endometrial cells exposed to a PCOS environment. Am. J. Physiol. Endocrinol. Metab. 2020, 318, E237–E248. [Google Scholar] [CrossRef]
- Wang, J.; Chu, K.; Wang, Y.; Li, J.; Fu, J.; Zeng, Y.A.; Li, W. Procr-expressing granulosa cells are highly proliferative and are important for follicle development. iScience 2021, 24, 102065. [Google Scholar] [CrossRef]
- Qi, J.; Li, J.; Wang, Y.; Wang, W.; Zhu, Q.; He, Y.; Lu, Y.; Wu, H.; Li, X.; Zhu, Z.; et al. Novel role of CXCL14 in modulating STAR expression in luteinized granulosa cells: Implication for progesterone synthesis in PCOS patients. Transl. Res. 2021, 230, 55–67. [Google Scholar] [CrossRef]
- Scotti, L.; Parborell, F.; Irusta, G.; De Zuñiga, I.; Bisioli, C.; Pettorossi, H.; Tesone, M.; Abramovich, D. Platelet-derived growth factor BB and DD and angiopoietin1 are altered in follicular fluid from polycystic ovary syndrome patients. Mol. Reprod. Dev. 2014, 81, 748–756. [Google Scholar] [CrossRef]
- Zheng, Q.; Zhou, F.; Cui, X.; Liu, M.; Li, Y.; Liu, S.; Tan, J.; Yan, Q. Novel Serum Biomarkers Detected by Protein Array in Polycystic Ovary Syndrome with Low Progesterone Level. Cell Physiol. Biochem. 2018, 46, 2297–2310. [Google Scholar] [CrossRef] [PubMed]
- Di Pietro, M.; Parborell, F.; Irusta, G.; Pascuali, N.; Bas, D.; Bianchi, M.S.; Tesone, M.; Abramovich, D. Metformin regulates ovarian angiogenesis and follicular development in a female polycystic ovary syndrome rat model. Endocrinology 2015, 156, 1453–1463. [Google Scholar] [CrossRef] [PubMed]
- Lewis, R.D.; Narayanaswamy, A.K.; Farewell, D.; Rees, D.A. Complement activation in polycystic ovary syndrome occurs in the postprandial and fasted state and is influenced by obesity and insulin sensitivity. Clin. Endocrinol. 2021, 94, 74–84. [Google Scholar] [CrossRef] [PubMed]
- Khichar, A.; Gupta, S.; Mishra, S.; Meena, M. Assessment of Inflammatory Markers in Women with PCOS and their Correlation with Insulin Resistance. Clin. Lab. 2021, 67. [Google Scholar] [CrossRef] [PubMed]

| Gene Symbol | Kaempferol Log2 Fold Change | Kaempferol p Value | Upregulated by P4 |
|---|---|---|---|
| Lefty1 | 2.61 | 4.83 × 10−21 | No |
| Padi4 | 2.08 | 3.06 × 10−17 | Yes |
| Sdr9c7 | 1.89 | 8.53 × 10−12 | No |
| Gm5148 | 1.77 | 1.41 × 10−10 | No |
| Muc5b | 1.71 | 8.04 × 10−10 | No |
| Syt8 | 1.41 | 4.27 × 10−7 | No |
| Mmp3 | 1.38 | 5.92 × 10−7 | No |
| Msr1 | 1.34 | 1.35 × 10−6 | No |
| Ceacam19 | 1.29 | 1.68 × 10−6 | No |
| Atf3 | 1.27 | 1.61 × 10−6 | Yes |
| Fam83c | 1.25 | 6.64 × 10−6 | No |
| Mrap2 | 1.22 | 5.30 × 10−6 | Yes |
| Prss27 | 1.21 | 7.34 × 10−6 | No |
| Sfrp4 | 1.21 | 1.19 × 10−7 | Yes |
| Galnt6 | 1.15 | 3.31 × 10−5 | No |
| Hk3 | 1.12 | 4.21 × 10−5 | No |
| Rarb | 1.12 | 3.36 × 10−5 | No |
| Pstpip2 | 1.07 | 1.12 × 10−4 | No |
| Sulf2 | 1.05 | 8.77 × 10−6 | Yes |
| Fabp5 | 1.05 | 1.62 × 10−4 | No |
| Brinp3 | 1.05 | 5.10 × 10−5 | No |
| Atp6v0d2 | 1.03 | 1.80 × 10−4 | No |
| Lrp2 | 0.99 | 4.56 × 10−5 | Yes |
| Slamf8 | 0.96 | 2.20 × 10−4 | No |
| Car12 | 0.94 | 4.12 × 10−6 | No |
| Padi3 | 0.93 | 2.29 × 10−4 | No |
| Noct | 0.88 | 7.37 × 10−5 | Yes |
| AI467606 | 0.85 | 1.73 × 10−5 | No |
| Ptgr1 | 0.82 | 7.65 × 10−5 | No |
| Rhbdl2 | 0.81 | 2.88 × 10−4 | No |
| Palm3 | 0.80 | 3.00 × 10−4 | Yes |
| Kdm8 | 0.74 | 2.60 × 10−4 | Yes |
| Ada | 0.74 | 2.20 × 10−4 | No |
| Rab27a | 0.72 | 9.16 × 10−5 | Yes |
| Gene Symbol | Kaempferol Log2 Fold Change | Kaempferol p Value | Downregulated by P4 |
|---|---|---|---|
| Cemip | −1.43 | 6.93 × 10−14 | Yes |
| Tcte2 | −1.42 | 5.16 × 10−8 | Yes |
| 2700054A10Rik | −1.42 | 5.16 × 10−8 | Yes |
| Egfl6 | −1.29 | 4.04 × 10−9 | Yes |
| C1s1 | −1.27 | 9.21 × 10−9 | No |
| Wif1 | −1.27 | 1.96 × 10−6 | Yes |
| Lepr | −1.26 | 1.87 × 10−7 | No |
| Bpifb5 | −1.25 | 9.14 × 10−8 | Yes |
| A330023F24Rik | −1.22 | 1.10 × 10−5 | No |
| Wnt9b | −1.20 | 6.24 × 10−6 | Yes |
| 4930447C04Rik | −1.14 | 2.24 × 10−5 | No |
| Lrrtm1 | −1.12 | 2.45 × 10−5 | Yes |
| Alox12e | −1.11 | 6.04 × 10−6 | No |
| Gm525 | −1.11 | 6.75 × 10−5 | No |
| Nkain4 | −1.04 | 1.20 × 10−4 | No |
| Rnase1 | −1.03 | 2.11 × 10−4 | Yes |
| Kcne2 | −1.03 | 2.15 × 10−4 | Yes |
| Rsad2 | −1.03 | 8.44 × 10−5 | Yes |
| Erich3 | −1.00 | 2.76 × 10−4 | Yes |
| Slc5a3 | −0.99 | 7.65 × 10−6 | No |
| Car4 | −0.99 | 1.39 × 10−4 | Yes |
| Cyp4b1 | −0.98 | 2.00 × 10−5 | No |
| C1s2 | −0.98 | 6.63 × 10−6 | No |
| Edil3 | −0.97 | 7.49 × 10−6 | Yes |
| Mycn | −0.97 | 1.23 × 10−4 | Yes |
| Wipf3 | −0.96 | 4.71 × 10−5 | No |
| Asb4 | −0.95 | 2.25 × 10−10 | Yes |
| Kctd4 | −0.93 | 2.05 × 10−5 | No |
| Ubc | −0.92 | 4.22 × 10−6 | No |
| Procr | −0.91 | 1.36 × 10−6 | Yes |
| C3 | −0.91 | 1.59 × 10−4 | Yes |
| Abcb1a | −0.87 | 9.87 × 10−5 | No |
| Selp | −0.86 | 2.79 × 10−4 | No |
| Creb5 | −0.85 | 2.07 × 10−4 | No |
| Enkur | −0.85 | 3.66 × 10−6 | Yes |
| Grb14 | −0.85 | 1.47 × 10−5 | Yes |
| Gmpr | −0.85 | 2.77 × 10−4 | Yes |
| Nr5a2 | −0.83 | 9.12 × 10−5 | No |
| Car8 | −0.83 | 2.85 × 10−5 | Yes |
| Osr2 | −0.77 | 4.65 × 10−8 | No |
| Ogdhl | −0.77 | 9.33 × 10−7 | Yes |
| Cyp46a1 | −0.75 | 2.33 × 10−4 | No |
| Cxcl14 | −0.74 | 5.47 × 10−5 | Yes |
| 2700046A07Rik | −0.72 | 2.10 × 10−4 | Yes |
| Nrep | −0.71 | 5.24 × 10−6 | Yes |
| Usp2 | −0.69 | 2.17 × 10−4 | No |
| Prdm1 | −0.69 | 4.33 × 10−5 | Yes |
| Pdgfd | −0.69 | 2.62 × 10−4 | No |
| 3632451O06Rik | −0.68 | 2.72 × 10−4 | No |
| C130074G19Rik | −0.67 | 1.68 × 10−4 | Yes |
| Zhx3 | −0.66 | 1.29 × 10−4 | No |
| Csrp2 | −0.63 | 9.08 × 10−6 | No |
| Afap1l1 | −0.62 | 2.67 × 10−9 | Yes |
| Rapgef4 | −0.61 | 1.42 × 10−4 | No |
| Pfkfb3 | −0.61 | 2.89 × 10−5 | No |
| Grrp1 | −0.59 | 9.37 × 10−6 | Yes |
| Gimap6 | −0.59 | 1.31 × 10−4 | No |
| Kank3 | −0.58 | 1.31 × 10−6 | No |
| Ly6c1 | −0.56 | 1.40 × 10−6 | Yes |
| Sox18 | −0.55 | 1.16 × 10−4 | No |
| Esam | −0.53 | 1.30 × 10−5 | Yes |
| Pdgfc | −0.52 | 8.70 × 10−5 | Yes |
| Zfp503 | −0.51 | 2.87 × 10−4 | No |
| Casp4 | −0.51 | 4.23 × 10−5 | Yes |
| Palmd | −0.50 | 1.84 × 10−4 | No |
| Cdc42ep1 | −0.47 | 1.35 × 10−4 | No |
| Ushbp1 | −0.43 | 1.26 × 10−4 | No |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bergsten, T.M.; Li, K.; Lantvit, D.D.; Murphy, B.T.; Burdette, J.E. Kaempferol, a Phytoprogestin, Induces a Subset of Progesterone-Regulated Genes in the Uterus. Nutrients 2023, 15, 1407. https://doi.org/10.3390/nu15061407
Bergsten TM, Li K, Lantvit DD, Murphy BT, Burdette JE. Kaempferol, a Phytoprogestin, Induces a Subset of Progesterone-Regulated Genes in the Uterus. Nutrients. 2023; 15(6):1407. https://doi.org/10.3390/nu15061407
Chicago/Turabian StyleBergsten, Tova M., Kailiang Li, Daniel D. Lantvit, Brian T. Murphy, and Joanna E. Burdette. 2023. "Kaempferol, a Phytoprogestin, Induces a Subset of Progesterone-Regulated Genes in the Uterus" Nutrients 15, no. 6: 1407. https://doi.org/10.3390/nu15061407
APA StyleBergsten, T. M., Li, K., Lantvit, D. D., Murphy, B. T., & Burdette, J. E. (2023). Kaempferol, a Phytoprogestin, Induces a Subset of Progesterone-Regulated Genes in the Uterus. Nutrients, 15(6), 1407. https://doi.org/10.3390/nu15061407






