Understanding Health-Promoting Behaviors and Influential Factors in Schizophrenia Patients
Abstract
:1. Introduction
Purpose
2. Participants and Methods
2.1. Measurements
2.2. Statistical Analyses
3. Results
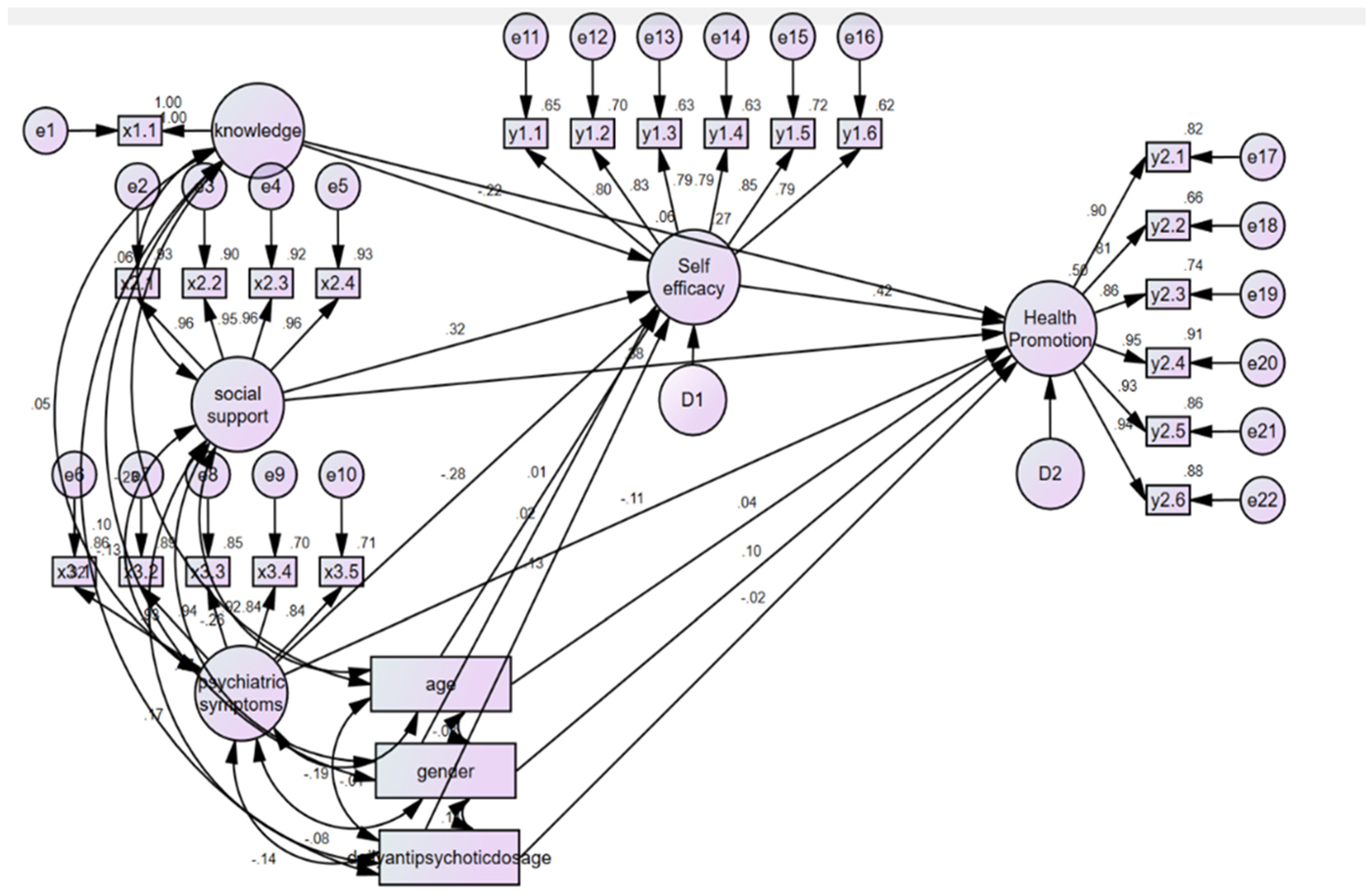
3.1. Analysis of the Finalized Model
3.2. Analysis of the Effect of Finalized Model
3.3. Control Variables of Age, Sex, and Daily Antipsychotic Dosage
4. Discussion
4.1. Health-Promoting Behaviors in Individuals with Schizophrenia
4.2. Factors Related to Health-Promoting Behaviors in Schizophrenia
5. Conclusions and Suggestions for Future Research
Suggestions for Future Research
- (1)
- A multi-site approach is needed when conducting studies related to health-promoting behaviors of individuals with schizophrenia.
- (2)
- Additional research studies are needed that include additional factors explaining health-promoting behaviors.
- (3)
- The development and validation of various intervention studies on enhancing health-promoting behaviors, especially healthy diets and nutrition for schizophrenia, need to be conducted.
- (4)
- Additional intervention programs that enhance self-efficacy need to be created and implemented.
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Mental Disorders Affect One in Four People. 2019. Available online: https://www.who.int/whr/2001/media_centre/press_release/en/ (accessed on 26 January 2024).
- Saha, S.; Chant, D.; Welham, J.; McGrath, J. A systematic review of the prevalence of schizophrenia. PLoS Med. 2005, 2, e141. [Google Scholar] [CrossRef] [PubMed]
- Hainsworth, J.B.; Clow, C.; Welham, J.; Shum, A.; Tse, J. Self-management approaches for people with chronic conditions: A review. Patient Educ. Couns. 2002, 48, 177–187. [Google Scholar]
- Cohen, A.; Griswold, K. Physical health care of people with severe mental illness. In Global Primary Mental Health Care; Routledge: London, UK, 2019; pp. 75–90. [Google Scholar] [CrossRef]
- De Hert, M.; Cohen, D.; Bobes, J.; Cetkovich-Bakmas, M.; Leucht, S.; Ndetei, D.M.; Newcomer, J.W.; Uwakwe, R.; Asai, I.; Möller, H.J.; et al. Physical illness in patients with severe mental disorders. II. Barriers to care, monitoring and treatment guidelines, plus recommendations at the system and individual level. World Psychiatry 2011, 10, 138–151. [Google Scholar] [CrossRef] [PubMed]
- Clow, A.; Edmunds, S. Relationship Between Physical Activity and Mental Health. In Physical Activity and Mental Health; University of Chichester: Chichester, UK, 2014. [Google Scholar] [CrossRef]
- Walker, S.N.; Sechrist, K.R.; Pender, N.J. The Health-Promoting Lifestyle Profile: Development and psychometric characteristics. Nurs. Res. 1987, 36, 76–81. [Google Scholar] [CrossRef] [PubMed]
- Fisher, J.D.; Fisher, W.A. Changing AIDS-risk behavior. Psychol. Bull. 1992, 111, 455–474. [Google Scholar] [CrossRef] [PubMed]
- Fan, Y.; Chen, J.; Shirkey, G.; John, R.; Wu, S.; Park, H.; Shao, C. Applications of structural equation modeling (SEM) in ecological studies: An updated review. Ecol. Process. 2016, 5, 19. [Google Scholar] [CrossRef]
- Fisher, J.D.; Fisher, W.A.; Amico, K.R.; Harman, J.J. An information-motivation-behavioral skills model of adherence to antiretroviral therapy. Health Psychol. 2006, 25, 462–473. [Google Scholar] [CrossRef] [PubMed]
- Wolf, E.J.; Harrington, K.M.; Clark, S.L.; Miller, M.W. Sample Size Requirements for Structural Equation Models: An Evaluation of Power, Bias, and Solution Propriety. Educ. Psychol. Meas. 2013, 76, 913–934. [Google Scholar] [CrossRef] [PubMed]
- Seo, H.M. Construction of Health Promoting Behaviors Model in Elderly. Ph.D. Dissertation, Seoul National University, Seoul, Republic of Korea, 2001. Available online: http://rs2.riss4u.net/search/detail/DetailView.do?p_mat_type=be54d9b8bc7cdb09&control_no=52b673424417dd11&keyword=%EC%84%9C%ED%98%84%EB%AF%B8 (accessed on 1 September 2020).
- Danivas, V.; Venkatasubramanian, G. Current perspectives on chlorpromazine equivalents: Comparing apples and oranges! Indian J. Psychiatry 2013, 55, 207–208. [Google Scholar] [CrossRef]
- Ha, K.Y. Effect of Health Education on Knowledge and Behavior for Elderly in Welfare Facilities. Master’s Thesis, Ewha Woman’s University, Seoul, Republic of Korea, 2005. Available online: http://rs2.riss4u.net/search/detail/DetailView.do?p_mat_type=be54d9b8bc7cdb09&control_no=fbe815e63e743af8&keyword=%ED%95%98%EA%B7%80%EC%97%BC (accessed on 1 September 2020).
- Sherbourne, C.; Stewart, A. The MOS social support survey. Soc. Sci. Med. 1991, 32, 705–714. [Google Scholar] [CrossRef]
- Lim, M.K.; Shin, Y.J.; Yoo, W.S.; Yang, B.M.; Kim, M.H. Social support and self-rated health status in a low-income neighborhood of Seoul, Korea. J. Prev. Med. Public. Health 2003, 36, 54–62. [Google Scholar]
- Becker, H.; Stuifbergen, A.; Oh, H.; Hall, S. Self-rated abilities for health practices: Health Self-Efficacy Measure. Health Values 1993, 17, 43–50. [Google Scholar]
- Lee, J.E.; Hong, H.G.; Park, J.S. Validation study of the Korean Self-Rated Abilities for Health Practices: Health Self-Efficacy Measure (K-SRAHP). Korean J. Adult Nurs. 2018, 26, 140–148. [Google Scholar] [CrossRef]
- Eisen, S.V.; Dill, D.L.; Grob, M.C. Reliability and validity of a brief patient-report instrument for psychiatric outcome evaluation. Hosp. Community Psychiatry 1994, 45, 242–247. [Google Scholar] [CrossRef] [PubMed]
- Bae, A.; Hong, C.; Shin, J. Validation study of the Behavior and Symptom Identification Scale (BASIS-32). Korean J. Clin. Psychol. 2011, 30, 929–941. [Google Scholar]
- Seo, H.M.; Hah, Y.S. A study of factors influencing on health-promoting lifestyle in the elderly: Application of Pender’s Health Promotion Model. J. Korean Acad. Nurs. 2004, 34, 1288. [Google Scholar] [CrossRef] [PubMed]
- Bae, B.R. Structural Equation Modeling with Amos 24; Chung-Nam Publisher: Seoul, Republic of Korea, 2017. [Google Scholar]
- Cain, M.; Zhang, Z.; Yuan, K. Univariate and Multivariate Skewness and Kurtosis for Measuring Nonnormality: Prevalence, Influence, and Estimation. Behav. Res. Methods 2017, 49, 1716–1735. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, N. Detecting Multicollinearity in Regression Analysis. Am. J. Appl. Math. Stat. 2020, 8, 39–42. [Google Scholar] [CrossRef]
- Groenwold, R.H.; Klungel, O.H.; Grobbee, D.E.; Hoes, A.W. Selection of confounding variables should not be based on observed associations with exposure. Eur. J. Epidemiol. 2011, 26, 589–593. [Google Scholar] [CrossRef]
- Ko, J.W.; Kang, H.W. Health Promoting Behavior and Optimism among the Elderly in S City. J. Korean Data Anal. Soc. 2013, 15, 3251–3262. [Google Scholar]
- Baygi, F.; Jensen, O.; Mohammadi-Nasrabadi, F.; Qorbani, M.; Mansourian, M.; Mirkazemi, R.; Farshad, A.; Salehi, S.A.; Roudsari, A.H.; Shidfar, F. Factors affecting health-promoting lifestyle profile in Iranian male seafarers working on tankers. Int. Marit. Health. 2017, 68, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Fashafsheh, I.; Al-Ghabeesh, S.H.; Ayed, A.; Salama, B.; Batran, A.; Bawadi, H. Health-promoting behaviors among nursing students: Palestinian perspective. Inquiry 2021, 58, 3251–3262. [Google Scholar] [CrossRef] [PubMed]
- Kahkonen, O.; Kankkunen, P.; Saaranen, T.; Miettinen, H.; Kyngas, H.; Lamidi, M.L. Motivation is a crucial factor for adherence to a healthy lifestyle among people with coronary heart disease after percutaneous coronary intervention. J. Adv. Nurs. 2015, 71, 2364–2373. [Google Scholar] [CrossRef]
- Winkel, R. Metabolic syndrome in people with schizophrenia. World Psychiatry 2009, 8, 15–20. [Google Scholar]
- Leonard, B.E.; Schwarz, M.; Myint, A.M. The metabolic syndrome in schizophrenia: Is inflammation a contributing cause? J. Psychopharmacol. 2012, 26 (Suppl. S5), 33–41. [Google Scholar] [CrossRef] [PubMed]
- Hong, E. The Mediating Effect of Self-efficacy in the Relationship between Diabetes Knowledge and Health Promoting Behaviors: Focus on Sex Differentiation. J. Korean Acad. Soc. Nurs. Educ. 2015, 21, 509–517. [Google Scholar] [CrossRef]
- Isa, A.; Loke, Y.K.; Smith, J.R.; Papageorgiou, A.; Hunter, P.R. Mediational effects of self-efficacy dimensions in the relationship between knowledge of dengue and dengue preventive behaviour with respect to control of dengue outbreaks: A structural equation model of a cross-sectional survey. PLoS Negl. Trop. Dis. 2013, 7, e2401. [Google Scholar] [CrossRef] [PubMed]
- Arlinghaus, K.R.; Johnston, C.A. Engaging Fathers in the Promotion of Healthy Lifestyle Behaviors. Am. J. Lifestyle Med. 2017, 11, 216–219. [Google Scholar] [CrossRef] [PubMed]
- Kelly, M.P.; Barker, M. Why is changing health-related behaviour so difficult? Public Health 2016, 136, 109–116. [Google Scholar] [CrossRef]
- Lee, G.; Yang, S.J.; Chee, Y.K. Assessment of healthy behaviors for metabolic syndrome among Korean adults: A modified information-motivation-behavioral skills with psychological distress. BMC Public Health 2016, 16, 518. [Google Scholar] [CrossRef]
- Faghri, P.; Buden, J. Health Behavior Knowledge and Self-efficacy as Predictors of Body Weight. J. Nutr. Disorders Ther. 2015, 5, 1000169. [Google Scholar] [CrossRef] [PubMed]
- Raeder, F.; Karbach, L.; Struwe, H.; Margraf, J.; Zlomuzica, A. Low perceived self-efficacy impedes discriminative fear learning. Front. Psychol. 2019, 10, 1191. [Google Scholar] [CrossRef] [PubMed]
- Corrigan, P.; Rao, D. On the Self-Stigma of Mental Illness: Stages, Disclosure, and Strategies for Change. Can. J. Psychiatry 2012, 57, 464–469. [Google Scholar] [CrossRef] [PubMed]
- Aschbrenner, K.A.; Mueser, K.T.; Bartels, S.J.; Pratt, S.I. Perceived social support for diet and exercise among persons with serious mental illness enrolled in a healthy lifestyle intervention. Psychiatr. Rehabil. J. 2013, 36, 65–71. [Google Scholar] [CrossRef]
- Reblin, M.; Uchino, B. Social and emotional support and its implication for health. Curr. Opin. Psychiatry 2008, 21, 201–205. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.Y.; Oh, J.; Lim, M.K.; Yun, E.H.; Kang, Y.H. The association of socioeconomic and psychosocial factors with obesity in a rural community. Korean J. Obes. 2012, 21, 18. [Google Scholar] [CrossRef]
- Oh, J.H. Effects of Social Support on Health Promotion Behavior through the Mediating Effect of Self-efficacy in Older Women Living Alone. J. Korean Gerontol. Nurs. 2018, 20, 177–184. [Google Scholar] [CrossRef]
- Cimpean, D.; Torrey, W.C.; Green, A.I. Schizophrenia and Co-occurring General Medical Illness. Psychiatr. Ann. 2005, 35, 70–81. [Google Scholar] [CrossRef]
- Knaak, S.; Mantler, E.; Szeto, A. Mental illness-related stigma in healthcare: Barriers to access and care and evidence-based solutions. Healthc. Manag. Forum 2017, 30, 111–116. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, M.; Morgan, T.A.; Stanton, K. The severity of psychiatric disorders. World Psychiatry 2018, 17, 258–275. [Google Scholar] [CrossRef]
- Bighelli, I.; Huhn, M.; Schneider-Thoma, J.; Krause, M.; Reitmeir, C.; Wallis, S.; Schwermann, F.; Pitschel-Walz, G.; Barbui, C.; Furukawa, T.A.; et al. Response rates in patients with schizophrenia and positive symptoms receiving cognitive behavioural therapy: A systematic review and single-group meta-analysis. BMC Psychiatry 2018, 18, 380. [Google Scholar] [CrossRef] [PubMed]
- Harvey, A.; Gumport, N. Evidence-based psychological treatments for mental disorders: Modifiable barriers to access and possible solutions. Behav. Res. Ther. 2015, 68, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Soneson, E.; Russo, D.; Knight, C.; Lafortune, L.; Heslin, M.; Stochl, J.; Georgiadis, A.; Galante, J.; Duschinsky, R.; Grey, N.; et al. Psychological interventions for people with psychotic experiences: Protocol for a systematic review and meta-analysis. Syst. Rev. 2019, 8, 124. [Google Scholar] [CrossRef]
- Turner, D.; Van der Gaag, M.; Karyotaki, E.; Cuijpers, P. Psychological interventions for psychosis: A meta-analysis of comparative outcome studies. Am. J. Psychiatry 2014, 171, 523–538. [Google Scholar] [CrossRef]
- Stuifbergen, A.K.; Becker, H.A. Predictors of Health Promoting Lifestyles in Persons with Disabilities. Res. Nurs. Health 1994, 17, 3–13. [Google Scholar] [CrossRef] [PubMed]
- McAuley, E.; Szabo, A.; Gothe, N.; Olson, E.A. Self-efficacy: Implications for Physical Activity, Function, and Functional Limitations in Older Adults. Am. J. Lifestyle Med. 2011, 5, 361–369. [Google Scholar] [CrossRef]
- Bandura, A. Self-efficacy: The Exercise of Control; W H Freeman/Times Books/Henry Holt & Co.: New York, NY, USA, 1997. [Google Scholar]
- Moore, C.D.; Schofield, C.; van Rooyen, D.R.; Andersson, L.M. Development and preliminary validation of a scale to measure self-efficacy in seeking mental health care (SE-SMHC). SpringerPlus 2015, 4, 339. [Google Scholar] [CrossRef]
- Kim, Y. A Study of Relations Between Health Promoting Behaviors and Self-efficacy of Conscripted Policemen. J. Korea Acad-Ind. Coop. Soc. 2013, 14, 778–785. [Google Scholar]
| Characteristics | Categories | n | % |
|---|---|---|---|
| Sex (gender) | Male | 109 | 54 |
| Female | 93 | 46 | |
| Age (years) | 19–29 | 6 | 3 |
| 30–39 | 28 | 13.9 | |
| 40–49 | 59 | 29.2 | |
| 50–59 | 86 | 42.6 | |
| ≥59 | 23 | 10.9 | |
| Mean ± SD | 48.75 ± 9.504 | ||
| Marital status | Married | 24 | 11.9 |
| Single | 142 | 70.3 | |
| Divorced or separated | 32 | 15.8 | |
| Others | 4 | 2 | |
| Education level | Elementary school | 6 | 3 |
| Middle school | 17 | 8.4 | |
| High school | 117 | 57.9 | |
| College or above | 62 | 30.7 | |
| Employment status | Unemployed | 149 | 73.8 |
| Employed | 53 | 26.2 | |
| Smoking status | Current smoker | 75 | 37.1 |
| Nonsmoker | 127 | 62.9 | |
| Alcohol consumption | Current drinker | 35 | 17.3 |
| Nondrinker | 167 | 82.8 | |
| Regular exercise | Yes | 88 | 43.5 |
| No | 114 | 56.5 | |
| First-generation antipsychotics | 27 | 13.37% | |
| Second-generation antipsychotics | 201 | 99.50% | |
| Antipsychotic dosage, chlorpromazine equivalents (mg) | Mean ± SD 596 ± 513 |
| X2 (p) | Normed x2 | GFI | AGFI | RMSEA | TLI | CFI | |
|---|---|---|---|---|---|---|---|
| Criteria | p > 0.10 | ≤3 | ≥0.90 | ≥0.90 | ≤0.80 | ≥0.90 | ≥0.90 |
| Finalized Model | 562.2 (<0.001) | 2.240 | 0.814 | 0.830 | 0.079 | 0.926 | 0.938 |
| Endogenous Variable | Exogenous Variable | Estimate | S.E. | Standardized Estimates | C.R. (p) | SMC |
|---|---|---|---|---|---|---|
| Self-efficacy | Health knowledge | −0.441 | 0.142 | −0.216 | −3.102 (0.002) | 0.274 |
| Social support | 0.235 | 0.053 | 0.317 | 4.478 (<0.001) | ||
| Psychiatric symptoms | −0.248 | 0.060 | −0.283 | −4.126 (<0.001) | ||
| Age | 0.001 | 0.006 | 0.015 | 0.219 (0.827) | ||
| Sex | 0.043 | 0.113 | 0.025 | 0.380 (0.704) | ||
| Daily antipsychotic dosage | 0.000 | 0.000 | 0.125 | 1.798 (0.072) | ||
| Health-promoting behaviors | Health knowledge | 0.092 | 0.091 | 0.059 | 1.006 (0.315) | 0.500 |
| Social support | 0.216 | 0.035 | 0.379 | 6.125 (<0.001) | ||
| Psychiatric symptoms | −0.072 | 0.039 | −0.106 | −1.831 (0.057) | ||
| Self-efficacy | 0.319 | 0.054 | 0.415 | 5.951 (<0.001) | ||
| Age | 0.003 | 0.004 | 0.039 | 0.689 (0.491) | ||
| Sex | 0.129 | 0.071 | 0.097 | 1.805 (0.071) | ||
| Daily antipsychotic dosage | 0.000 | 0.000 | −0.020 | −0.342 (0.732) |
| Endogenous Variable | Exogenous Variable | Direct Effects | p | Indirect Effects | p | Total Effects | p |
|---|---|---|---|---|---|---|---|
| Self-efficacy | Health knowledge | −0.441 (−0.216) | 0.002 | −0.441 (−0.216) | 0.002 | ||
| Social support | 0.235 (0.317) | <0.001 | 0.235 (0.317) | <0.001 | |||
| Psychiatric symptoms | −0.248 (−0.283) | <0.001 | −0.248 (−0.283) | <0.001 | |||
| Age | 0.001 (0.015) | 0.827 | 0.001 (0.015) | 0.827 | |||
| Sex | 0.043 (0.025) | 0.704 | 0.043 (0.025) | 0.704 | |||
| Daily antipsychotic dosage | 0.000 (0.125) | 0.072 | 0.000 (0.125) | 0.072 | |||
| Health-promoting behaviors | Health knowledge | 0.092 (0.059) | 0.315 | −0.141 (−0.090) | 0.005 | −0.049 (−0.031) | 0.606 |
| Social support | 0.216 (0.379) | <0.001 | 0.075 (0.132) | 0.001 | 0.291 (0.510) | 0.001 | |
| Psychiatric symptoms | −0.072 (−0.106) | 0.057 | −0.079 (−0.117) | 0.001 | −0.151 (−0.224) | 0.001 | |
| Self-efficacy | 0.319 (0.415) | <0.001 | 0.319 (0.415) | 0.001 | |||
| Age | 0.003 (0.039) | 0.491 | 0.000 (0.006) | 0.824 | 0.003 (0.045) | 0.483 | |
| Sex | 0.129 (0.097) | 0.071 | 0.014 (0.010) | 0.739 | 0.142 (0.107) | 0.088 | |
| Daily antipsychotic dosage | 0.000 (−0.020) | 0.732 | 0.000 (0.052) | 0.087 | 0.000 (0.032) | 0.601 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yu, H. Understanding Health-Promoting Behaviors and Influential Factors in Schizophrenia Patients. Nutrients 2024, 16, 1490. https://doi.org/10.3390/nu16101490
Yu H. Understanding Health-Promoting Behaviors and Influential Factors in Schizophrenia Patients. Nutrients. 2024; 16(10):1490. https://doi.org/10.3390/nu16101490
Chicago/Turabian StyleYu, Heajin. 2024. "Understanding Health-Promoting Behaviors and Influential Factors in Schizophrenia Patients" Nutrients 16, no. 10: 1490. https://doi.org/10.3390/nu16101490
APA StyleYu, H. (2024). Understanding Health-Promoting Behaviors and Influential Factors in Schizophrenia Patients. Nutrients, 16(10), 1490. https://doi.org/10.3390/nu16101490







