Exploring the Preventive Potential of Vitamin D against Respiratory Infections in Preschool-Age Children: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Ethical Considerations
2.2. Inclusion and Exclusion Criteria
2.3. Laboratory Analysis
2.4. Statistical Analysis
3. Results
Background Characteristics
4. Discussion
4.1. Literature Findings
4.2. Limitations and Future Perspectives
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sizar, O.; Khare, S.; Goyal, A.; Givler, A. Vitamin D Deficiency. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar] [PubMed]
- Dominguez, L.J.; Farruggia, M.; Veronese, N.; Barbagallo, M. Vitamin D Sources, Metabolism, and Deficiency: Available Compounds and Guidelines for Its Treatment. Metabolites 2021, 11, 255. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ao, T.; Kikuta, J.; Ishii, M. The Effects of Vitamin D on Immune System and Inflammatory Diseases. Biomolecules 2021, 11, 1624. [Google Scholar] [CrossRef] [PubMed]
- Martens, P.J.; Gysemans, C.; Verstuyf, A.; Mathieu, A.C. Vitamin D’s Effect on Immune Function. Nutrients 2020, 12, 1248. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dahma, G.; Craina, M.; Dumitru, C.; Neamtu, R.; Popa, Z.L.; Gluhovschi, A.; Citu, C.; Bratosin, F.; Bloanca, V.; Alambaram, S.; et al. A Prospective Analysis of Vitamin D Levels in Pregnant Women Diagnosed with Gestational Hypertension after SARS-CoV-2 Infection. J. Pers. Med. 2023, 13, 317. [Google Scholar] [CrossRef]
- Raju, A.; Luthra, G.; Shahbaz, M.; Almatooq, H.; Foucambert, P.; Esbrand, F.D.; Zafar, S.; Panthangi, V.; Cyril Kurupp, A.R.; Khan, S. Role of Vitamin D Deficiency in Increased Susceptibility to Respiratory Infections Among Children: A Systematic Review. Cureus 2022, 14, e29205. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hughes, D.A.; Norton, R. Vitamin D and respiratory health. Clin. Exp. Immunol. 2009, 158, 20–25. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Taha, R.; Abureesh, S.; Alghamdi, S.; Hassan, R.Y.; Cheikh, M.M.; Bagabir, R.A.; Almoallim, H.; Abdulkhaliq, A. The Relationship Between Vitamin D and Infections Including COVID-19: Any Hopes? Int. J. Gen. Med. 2021, 14, 3849–3870. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- de Hoog, M.L.; Venekamp, R.P.; van der Ent, C.K.; Schilder, A.; Sanders, E.A.; Damoiseaux, R.A.; Bogaert, D.; Uiterwaal, C.S.; Smit, H.A.; Bruijning-Verhagen, P. Impact of early daycare on healthcare resource use related to upper respiratory tract infections during childhood: Prospective WHISTLER cohort study. BMC Med. 2014, 12, 107. [Google Scholar] [CrossRef] [PubMed]
- Schuez-Havupalo, L.; Toivonen, L.; Karppinen, S.; Kaljonen, A.; Peltola, V. Daycare attendance and respiratory tract infections: A prospective birth cohort study. BMJ Open 2017, 7, e014635. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shi, C.; Wang, X.; Ye, S.; Deng, S.; Cong, B.; Lu, B.; Li, Y. Understanding the risk of transmission of respiratory viral infections in childcare centres: Protocol for the DISeases TrANsmission in ChildcarE (DISTANCE) multicentre cohort study. BMJ Open Respir. Res. 2023, 10, e001617. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Al Rajeh, A.M.; Naser, A.Y.; Siraj, R.; Alghamdi, A.; Alqahtani, J.; Aldabayan, Y.; Aldhahir, A.; Al Haykan, A.; Elmosaad, Y.M. Acute upper respiratory infections admissions in England and Wales. Medicine 2023, 102, e33616. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hon, K.L.; Leung, A.K. Severe childhood respiratory viral infections. Adv. Pediatr. 2009, 56, 47–73. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Grimwood, K.; Chang, A.B. Long-term effects of pneumonia in young children. Pneumonia 2015, 6, 101–114. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Grant, W.B.; Lahore, H.; McDonnell, S.L.; Baggerly, C.A.; French, C.B.; Aliano, J.L.; Bhattoa, H.P. Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths. Nutrients 2020, 12, 988. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gunville, C.F.; Mourani, P.M.; Ginde, A.A. The role of vitamin D in prevention and treatment of infection. Inflamm. Allergy Drug Targets 2013, 12, 239–245. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wimalawansa, S.J. Controlling Chronic Diseases and Acute Infections with Vitamin D Sufficiency. Nutrients 2023, 15, 3623. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jolliffe, D.A.; Camargo, C.A., Jr.; Sluyter, J.D.; Aglipay, M.; Aloia, J.F.; Ganmaa, D.; Bergman, P.; Bischoff-Ferrari, H.A.; Borzutzky, A.; Damsgaard, C.T.; et al. Vitamin D supplementation to prevent acute respiratory infections: A systematic review and meta-analysis of aggregate data from randomised controlled trials. Lancet Diabetes Endocrinol. 2021, 9, 276–292. [Google Scholar] [CrossRef] [PubMed]
- Fang, Q.; Wu, Y.; Lu, J.; Zheng, H. A meta-analysis of the association between vitamin D supplementation and the risk of acute respiratory tract infection in the healthy pediatric group. Front. Nutr. 2023, 10, 1188958. [Google Scholar] [CrossRef] [PubMed]
- Esposito, S.; Lelii, M. Vitamin D and respiratory tract infections in childhood. BMC Infect. Dis. 2015, 15, 487. [Google Scholar] [CrossRef] [PubMed]
- Aranow, C. Vitamin D and the immune system. J. Investig. Med. 2011, 59, 881–886. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Liu, Y.; Clare, S.; D’Erasmo, G.; Heilbronner, A.; Dash, A.; Krez, A.; Zaworski, C.; Haseltine, K.; Serota, A.; Miller, A.; et al. Vitamin D and SARS-CoV-2 Infection: SERVE Study (SARS-CoV-2 Exposure and the Role of Vitamin D among Hospital Employees). J. Nutr. 2023, 153, 1420–1426. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kearns, M.D.; Alvarez, J.A.; Seidel, N.; Tangpricha, V. Impact of vitamin D on infectious disease. Am. J. Med. Sci. 2015, 349, 245–262. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Calvo, M.S.; Whiting, S.J. Perspective: School Meal Programs Require Higher Vitamin D Fortification Levels in Milk Products and Plant-Based Alternatives-Evidence from the National Health and Nutrition Examination Surveys (NHANES 2001–2018). Adv. Nutr. 2022, 13, 1440–1449. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- JaBaay, N.R.; Nel, N.H.; Comstock, S.S. Dietary Intake by Toddlers and Preschool Children: Preliminary Results from a Michigan Cohort. Children 2023, 10, 190. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Vargas Buonfiglio, L.G.; Cano, M.; Pezzulo, A.A.; Vanegas Calderon, O.G.; Zabner, J.; Gerke, A.K.; Comellas, A.P. Effect of vitamin D3 on the antimicrobial activity of human airway surface liquid: Preliminary results of a randomised placebo-controlled double-blind trial. BMJ Open Respir. Res. 2017, 4, e000211. [Google Scholar] [CrossRef] [PubMed]
- Gombart, A.F. The vitamin D-antimicrobial peptide pathway and its role in protection against infection. Future Microbiol. 2009, 4, 1151–1165. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Amrein, K.; Scherkl, M.; Hoffmann, M.; Neuwersch-Sommeregger, S.; Köstenberger, M.; Tmava Berisha, A.; Martucci, G.; Pilz, S.; Malle, O. Vitamin D deficiency 2.0: An update on the current status worldwide. Eur. J. Clin. Nutr. 2020, 74, 1498–1513. [Google Scholar] [CrossRef] [PubMed]
- Balan, K.V.; Babu, U.S.; Godar, D.E.; Calvo, M.S. Vitamin D and respiratory infections in infants and toddlers: A nutri-shine perspective. In Handbook of Vitamin D in Human Health; Wageningen Academic: Wageningen, The Netherlands, 2013; Volume 4, pp. 276–297. [Google Scholar] [PubMed Central]
- Şişmanlar, T.; Aslan, A.T.; Gülbahar, Ö.; Özkan, S. The effect of vitamin D on lower respiratory tract infections in children. Türk Pediatri Arşivi 2016, 51, 94–99. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nicolae, M.; Mihai, C.M.; Chisnoiu, T.; Balasa, A.L.; Frecus, C.E.; Mihai, L.; Lupu, V.V.; Ion, I.; Pantazi, A.C.; Nelson Twakor, A.; et al. Immunomodulatory Effects of Vitamin D in Respiratory Tract Infections and COVID-19 in Children. Nutrients 2023, 15, 3430. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Xiao, J.; He, W. The immunomodulatory effects of vitamin D drops in children with recurrent respiratory tract infections. Am. J. Transl. Res. 2021, 13, 1750–1756. [Google Scholar] [PubMed] [PubMed Central]
- Abioye, A.I.; Bromage, S.; Fawzi, W. Effect of micronutrient supplements on influenza and other respiratory tract infections among adults: A systematic review and meta-analysis. BMJ Glob. Health 2021, 6, e003176. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Martineau, A.R.; Jolliffe, D.A.; Hooper, R.L.; Greenberg, L.; Aloia, J.F.; Bergman, P.; Dubnov-Raz, G.; Esposito, S.; Ganmaa, D.; Ginde, A.A.; et al. Vitamin D supplementation to prevent acute respiratory tract infections: Systematic review and meta-analysis of individual participant data. BMJ 2017, 356, i6583. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jat, K.R. Vitamin D deficiency and lower respiratory tract infections in children: A systematic review and meta-analysis of observational studies. Trop. Dr. 2017, 47, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Buendía, J.A.; Patiño, D.G. Cost-utility of vitamin D supplementation to prevent acute respiratory infections in children. Cost Eff. Resour. Alloc. 2023, 21, 23. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
| Variables | Recurrent Respiratory Infections (n = 141) | No Recurrent Respiratory Infections (n = 74) | p-Value |
|---|---|---|---|
| Age (mean ± SD) | 3.78 ± 0.95 | 3.67 ± 1.03 | 0.483 |
| Age category, n (%) | 0.675 | ||
| 2–3 years | 68 (48.23%) | 32 (43.24%) | |
| 4–5 years | 73 (51.77%) | 42 (56.76%) | |
| BMI (mean ± SD) | 16.3 ± 1.6 | 16.5 ± 1.3 | 0.389 |
| Development, n (%) | |||
| Normal | 108 (76.60%) | 56 (75.68%) | 0.847 |
| Underweight | 16 (11.35%) | 12 (16.22%) | 0.423 |
| Overweight | 11 (7.80%) | 5 (6.76%) | 0.765 |
| Low weight for height | 4 (2.84%) | 1 (1.35%) | 0.621 |
| Low height for age | 2 (1.42%) | 0 (0.00%) | 0.486 |
| Place of living | 0.822 | ||
| Rural | 58 (41.13%) | 29 (39.19%) | |
| Urban | 83 (58.87%) | 45 (60.81%) | |
| Daily calorie intake, n (%) | |||
| Low (< 1400 kcal) | 29 (20.57%) | 16 (21.62%) | 0.922 |
| Moderate (1400–1600 kcal) | 68 (48.23%) | 36 (48.65%) | 0.966 |
| High (>1600 kcal) | 44 (31.21%) | 22 (29.73%) | 0.882 |
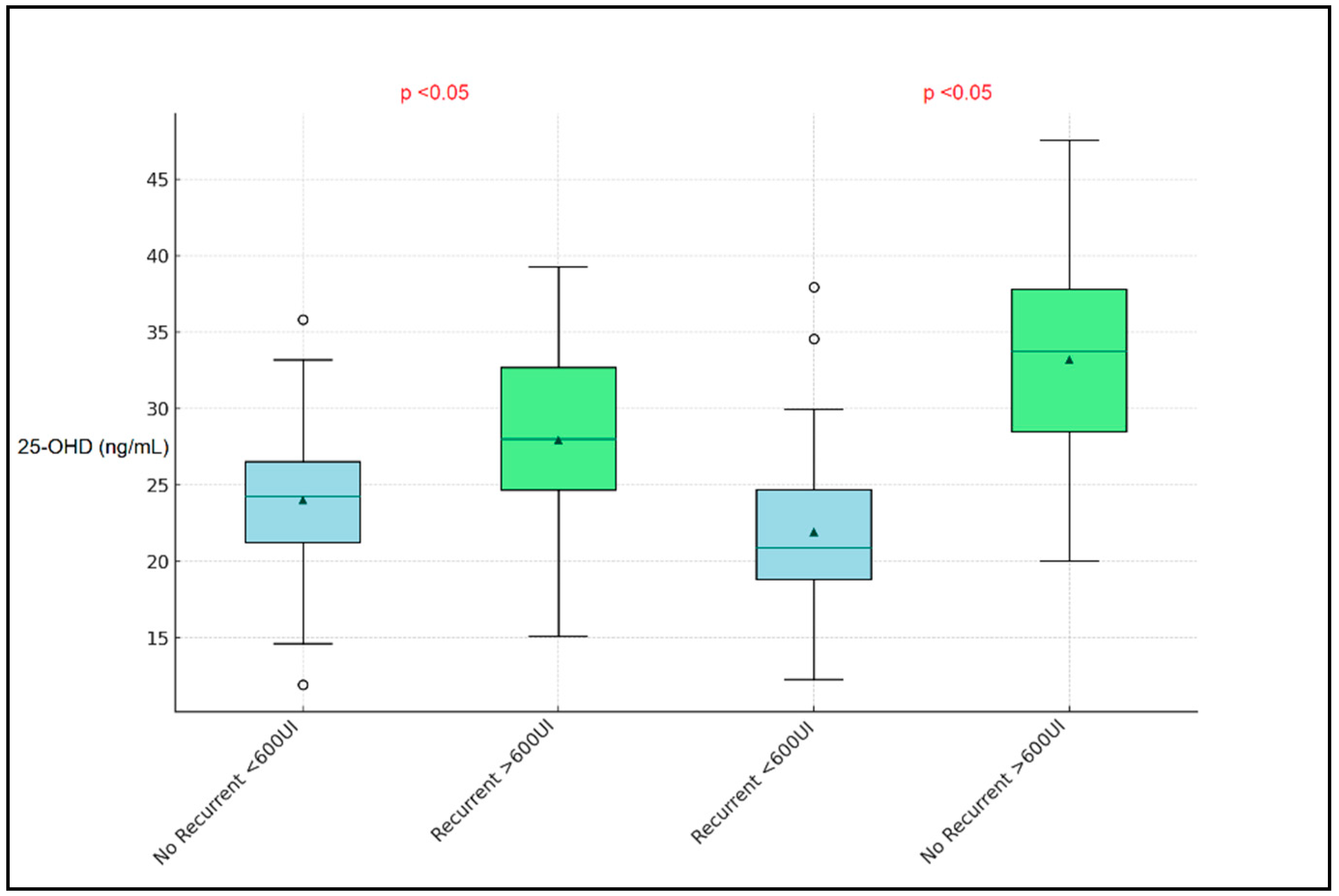
| Vitamin D supplementation (>600 UI/week), n (%) | 4.8 × 10−5 | ||
| Yes | 32 (22.70%) | 44 (59.46%) | |
| No | 109 (77.30%) | 30 (40.54%) | |
| Number of respiratory infections in the past 12 months, n (%) | 3.2 × 10−5 | ||
| 1 | 0 (0.00%) | 74 (100.00%) | |
| 2–3 | 89 (63.12%) | 0 (0.00%) | |
| >3 | 52 (36.88%) | 0 (0.00%) | |
| Type of respiratory infection | 0.503 | ||
| Upper tract infection | 117 (83.00%) | 64 (86.49%) | |
| Lower tract infection | 24 (17.00%) | 10 (13.51%) | |
| Sun exposure per day, n (%) | |||
| 5–15 min | 52 (36.88%) | 25 (33.78%) | 0.744 |
| 15–30 min | 59 (41.84%) | 34 (45.95%) | 0.679 |
| >30 min | 30 (21.28%) | 15 (20.27%) | 0.888 |
| Daily sunscreen use, n (%) | |||
| Frequently | 23 (16.31%) | 10 (13.51%) | 0.648 |
| Often | 44 (31.21%) | 28 (37.84%) | 0.556 |
| Rarely | 58 (41.13%) | 26 (35.14%) | 0.419 |
| Never | 16 (11.35%) | 10 (13.51%) | 0.764 |
| Antibiotic use in the past 6 months, n (%) | 0.257 | ||
| Yes | 81 (57.45%) | 37 (50.00%) | |
| No | 60 (42.55%) | 37 (50.00%) |
| Variables (Mean ± SD) | Normal Range | Recurrent Respiratory Infections (n = 141) | No Recurrent Respiratory Infections (n = 74) | p-Value |
|---|---|---|---|---|
| 25-OHD (ng/mL) | 30–55.5 | 24.5 ± 5.3 | 29.7 ± 6.1 | 3.9 × 10−4 |
| PTH (pg/mL) | 15–65 | 55.2 ± 15.3 | 48.7 ± 14.8 | 0.023 |
| Calcitonin (pg/mL) | <10 | 7.3 ± 2.5 | 6.9 ± 2.2 | 0.311 |
| Calcium (mg/dL) | 8.8–10.8 | 9.4 ± 0.8 | 9.5 ± 0.7 | 0.542 |
| Phosphate (mg/dL) | 3.4–5.5 | 4.2 ± 0.5 | 4.3 ± 0.4 | 0.376 |
| Creatinine (mg/dL) | 0.3–0.7 | 0.5 ± 0.1 | 0.5 ± 0.1 | 0.890 |
| CRP (mg/L) | <5 | 6.8 ± 2.3 | 3.1 ± 1.2 | 6.1 × 10−6 |
| Ferritin (ng/mL) | 15–150 | 60.3 ± 25.4 | 55.1 ± 22.3 | 0.148 |
| ESR (mm/h) | 0–20 | 18.5 ± 8.3 | 14.7 ± 7.9 | 0.037 |
| Iron (µg/dL) | 50–120 | 85.2 ± 23.7 | 91.3 ± 25.1 | 0.153 |
| WBC (×109/L) | 4.0–10.0 | 8.3 ± 2.1 | 7.2 ± 1.8 | 0.004 |
| RBC (×1012/L) | 4.5–5.5 | 4.8 ± 0.6 | 4.9 ± 0.5 | 0.272 |
| Lymphocytes (%) | 20–40 | 35.2 ± 8.4 | 37.1 ± 7.9 | 0.154 |
| Neutrophils (%) | 40–60 | 54.6 ± 7.5 | 52.8 ± 6.9 | 0.088 |
| Hemoglobin (g/dL) | 11.0–14.0 | 12.3 ± 1.2 | 12.5 ± 1.1 | 0.229 |
| Platelets (×109/L) | 150–450 | 310.5 ± 80.2 | 325.3 ± 75.4 | 0.197 |
| Vitamin D assessment, n (%) | ||||
| Optimal | 30–55.5 ng/mL | 18 (12.77%) | 25 (33.78%) | 5.0 × 10−4 |
| Insufficient | 21–29 ng/mL | 63 (44.68%) | 34 (45.95%) | 0.881 |
| Deficient | 20–16 ng/mL | 52 (36.88%) | 12 (16.22%) | 6.6 × 10−5 |
| Severe deficiency | <16 ng/mL | 8 (5.67%) | 3 (4.05%) | 0.717 |
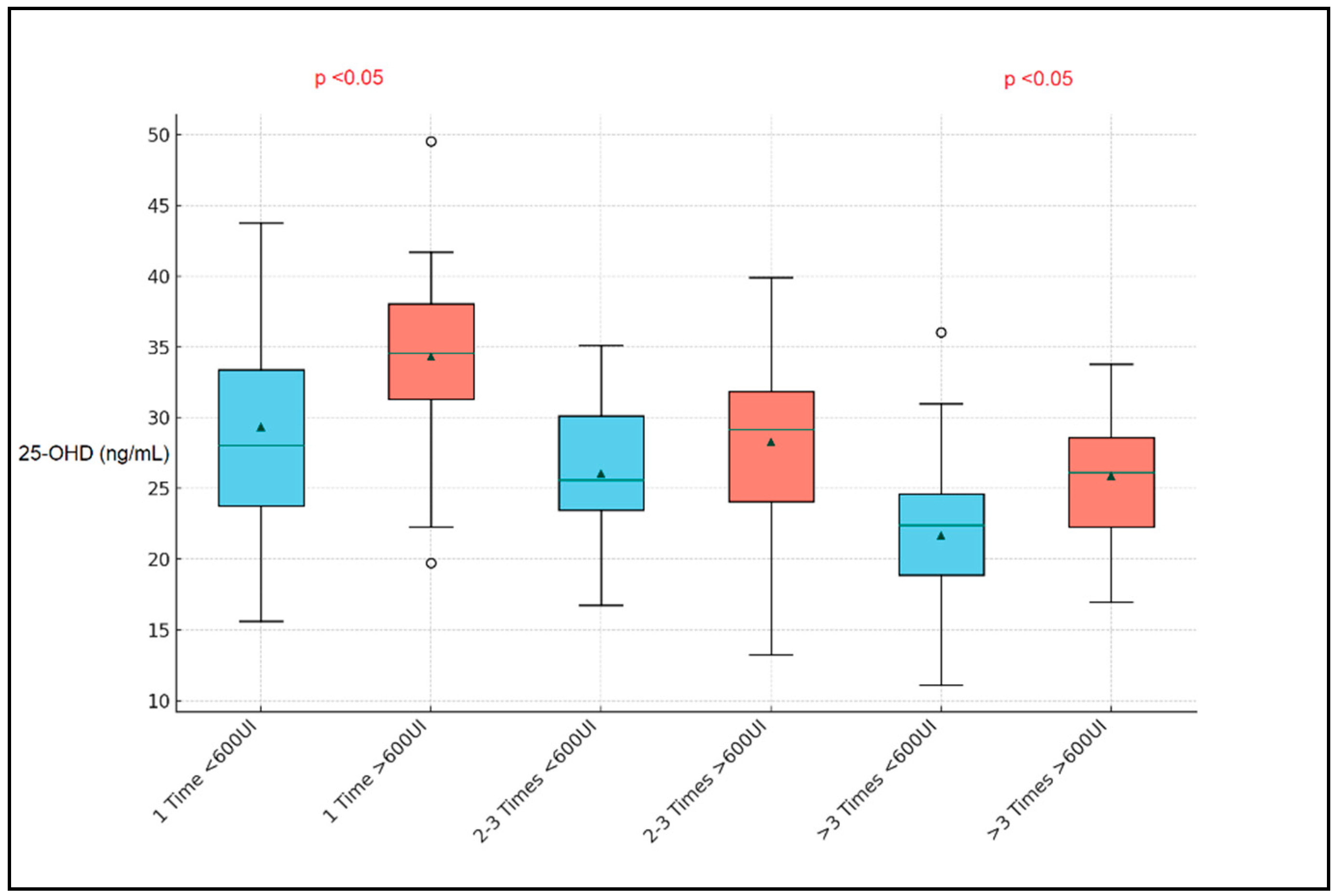
| Variables (Mean ± SD) | 1 Time (n = 74) | 2–3 Times (n = 89) | >3 Times (n = 52) | p-Value |
|---|---|---|---|---|
| 25-OHD (ng/mL) | 29.7 ± 6.1 | 25.2 ± 5.4 | 22.8 ± 4.9 | 4.8 × 10−4 |
| PTH (pg/mL) | 48.7 ± 14.8 | 54.9 ± 15.1 | 58.3 ± 16.2 | 0.004 |
| Calcitonin (pg/mL) | 6.9 ± 2.2 | 7.1 ± 2.3 | 7.5 ± 2.4 | 0.218 |
| Calcium (mg/dL) | 9.5 ± 0.7 | 9.3 ± 0.8 | 9.2 ± 0.9 | 0.076 |
| Phosphate (mg/dL) | 4.3 ± 0.4 | 4.1 ± 0.5 | 4.0 ± 0.6 | 0.037 |
| Creatinine (mg/dL) | 0.5 ± 0.1 | 0.5 ± 0.1 | 0.6 ± 0.1 | 0.019 |
| CRP (mg/L) | 3.1 ± 1.2 | 6.5 ± 2.1 | 8.7 ± 3.3 | 4.2 × 10−5 |
| Ferritin (ng/mL) | 55.1 ± 22.3 | 61.7 ± 25.1 | 67.9 ± 27.5 | 0.031 |
| ESR (mm/hr) | 14.7 ± 7.9 | 18.4 ± 8.2 | 21.6 ± 9.4 | 0.002 |
| Iron (µg/dL) | 91.3 ± 25.1 | 86.4 ± 24.8 | 82.1 ± 23.6 | 0.053 |
| WBC (×109/L) | 7.2 ± 1.8 | 8.4 ± 2.0 | 9.1 ± 2.3 | 3.9 × 10−5 |
| RBC (×1012/L) | 4.9 ± 0.5 | 4.8 ± 0.6 | 4.7 ± 0.7 | 0.127 |
| Lymphocytes (%) | 37.1 ± 7.9 | 34.5 ± 8.2 | 32.3 ± 8.5 | 0.010 |
| Neutrophils (%) | 52.8 ± 6.9 | 55.4 ± 7.2 | 58.2 ± 7.5 | 0.003 |
| Hemoglobin (g/dL) | 12.5 ± 1.1 | 12.2 ± 1.2 | 11.9 ± 1.3 | 0.017 |
| Platelets (×109/L) | 325.3 ± 75.4 | 308.2 ± 80.1 | 296.7 ± 82.3 | 0.044 |
| Vitamin D assessment, n (%) | ||||
| Optimal | 25 (33.78%) | 12 (13.48%) | 5 (9.62%) | 3.6 × 10−4 |
| Insufficient | 34 (45.95%) | 41 (46.07%) | 22 (42.31%) | 0.912 |
| Deficient | 12 (16.22%) | 28 (31.46%) | 20 (38.46%) | 0.001 |
| Severe deficiency | 3 (4.05%) | 8 (8.99%) | 5 (9.62%) | 0.258 |
| Predictor | B (Coefficients) | Standard Error | Wald | df | p-Value | Exp(B) (Odds Ratio) |
|---|---|---|---|---|---|---|
| Vitamin D Status (Reference: Optimal) | ||||||
| Insufficient | 0.143 | 0.193 | 0.549 | 1 | 0.469 | 1.154 |
| Deficient | 0.289 | 0.218 | 1.756 | 1 | 0.185 | 1.335 |
| Severe Deficiency | 1.087 | 0.304 | 12.785 | 1 | <0.001 | 2.967 |
| Vitamin D Supplementation (>600 IU/week) | −0.648 | 0.176 | 13.519 | 1 | <0.001 | 0.523 |
| Sun Exposure (Reference: >30 min) | ||||||
| 5–15 min | 0.132 | 0.251 | 0.276 | 1 | 0.599 | 1.141 |
| 15–30 min | 0.098 | 0.205 | 0.228 | 1 | 0.633 | 1.103 |
| Daily Sunscreen Use (Reference: Never) | ||||||
| Frequently | 0.061 | 0.265 | 0.053 | 1 | 0.817 | 1.063 |
| Often | 0.034 | 0.184 | 0.034 | 1 | 0.853 | 1.035 |
| Rarely | −0.017 | 0.147 | 0.013 | 1 | 0.909 | 0.983 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sarau, O.S.; Rachabattuni, H.C.; Gadde, S.T.; Daruvuri, S.P.; Marusca, L.M.; Horhat, F.G.; Fildan, A.P.; Tanase, E.; Prodan-Barbulescu, C.; Horhat, D.I. Exploring the Preventive Potential of Vitamin D against Respiratory Infections in Preschool-Age Children: A Cross-Sectional Study. Nutrients 2024, 16, 1595. https://doi.org/10.3390/nu16111595
Sarau OS, Rachabattuni HC, Gadde ST, Daruvuri SP, Marusca LM, Horhat FG, Fildan AP, Tanase E, Prodan-Barbulescu C, Horhat DI. Exploring the Preventive Potential of Vitamin D against Respiratory Infections in Preschool-Age Children: A Cross-Sectional Study. Nutrients. 2024; 16(11):1595. https://doi.org/10.3390/nu16111595
Chicago/Turabian StyleSarau, Oana Silvana, Hari Charan Rachabattuni, Sai Teja Gadde, Sai Praveen Daruvuri, Larisa Mihaela Marusca, Florin George Horhat, Ariadna Petronela Fildan, Elena Tanase, Catalin Prodan-Barbulescu, and Delia Ioana Horhat. 2024. "Exploring the Preventive Potential of Vitamin D against Respiratory Infections in Preschool-Age Children: A Cross-Sectional Study" Nutrients 16, no. 11: 1595. https://doi.org/10.3390/nu16111595
APA StyleSarau, O. S., Rachabattuni, H. C., Gadde, S. T., Daruvuri, S. P., Marusca, L. M., Horhat, F. G., Fildan, A. P., Tanase, E., Prodan-Barbulescu, C., & Horhat, D. I. (2024). Exploring the Preventive Potential of Vitamin D against Respiratory Infections in Preschool-Age Children: A Cross-Sectional Study. Nutrients, 16(11), 1595. https://doi.org/10.3390/nu16111595






