Understanding the Impact of Different Doses of Reducose® Mulberry Leaf Extract on Blood Glucose and Insulin Responses after Eating a Complex Meal: Results from a Double-Blind, Randomised, Crossover Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Participants
2.3. Test Products and Test Meal
2.4. Protocol
2.5. Sample Size and Randomisation
2.6. Statistical Analyses
- (1)
- Reducose® 200 mg dietary supplement;
- (2)
- Reducose® 225 mg dietary supplement;
- (3)
- Reducose® 250 mg dietary supplement;
- (4)
- Placebo.
3. Results
3.1. Physical Characteristics
3.2. Glycaemic Response
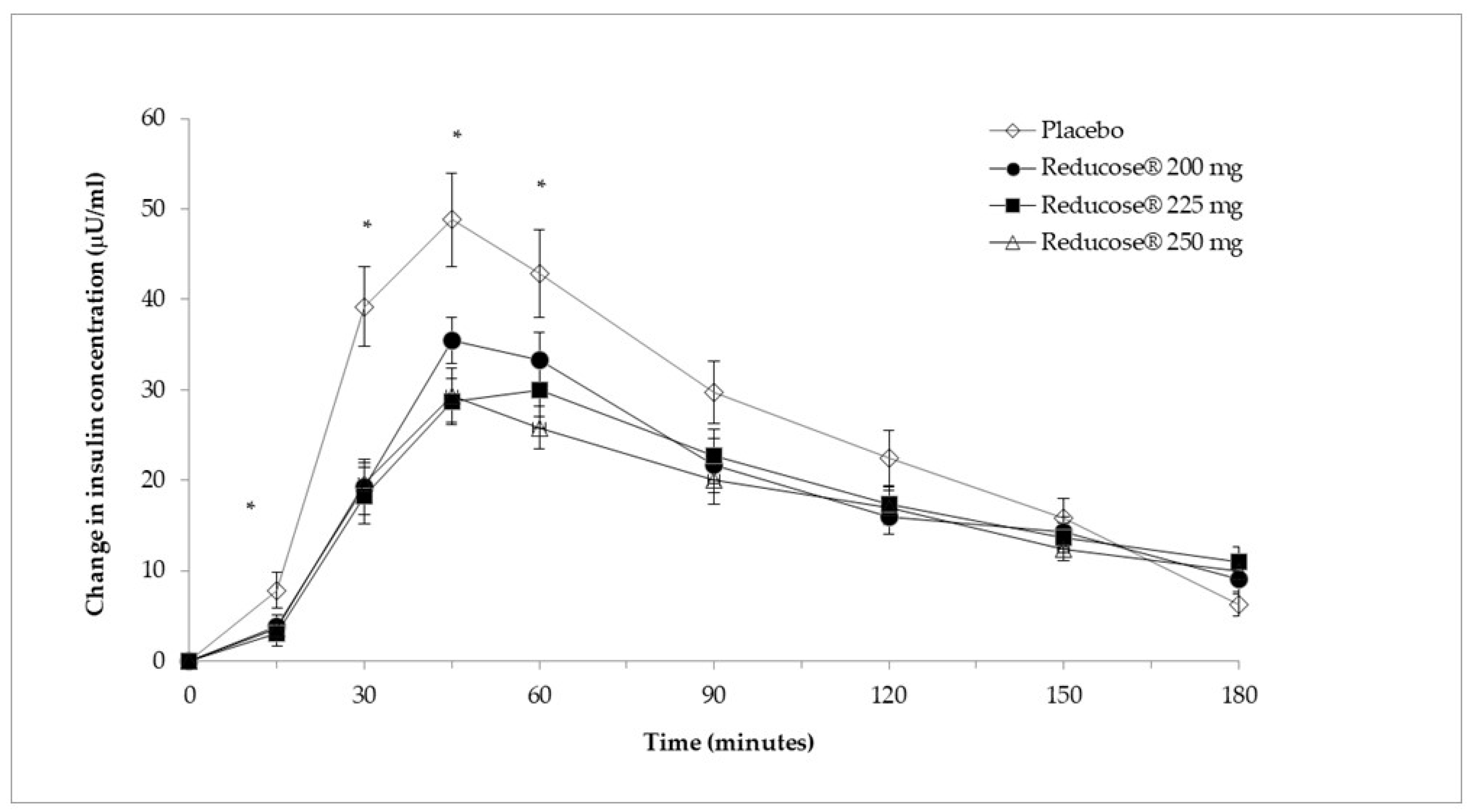
3.3. Insulinaemic Response
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Noncommunicable Diseases; WHO: Geneva, Switzerland, 2023. [Google Scholar]
- Lee, J.T.; Hamid, F.; Pati, S.; Atun, R.; Millett, C. Impact of Noncommunicable Disease Multimorbidity on Healthcare Utilisation and Out-Of-Pocket Expenditures in Middle-Income Countries: Cross Sectional Analysis. PLoS ONE 2015, 10, e0127199. [Google Scholar] [CrossRef] [PubMed]
- Finkelstein, E.A.; Bilger, M.; Baid, D. Effectiveness and cost-effectiveness of incentives as a tool for prevention of non-communicable diseases: A systematic review. Soc. Sci. Med. 2019, 232, 340–350. [Google Scholar] [CrossRef] [PubMed]
- GBD 2021 Diabetes Collaborators. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: A systematic analysis for the Global Burden of Disease Study 2021. Lancet 2023, 402, 203–234. [Google Scholar] [CrossRef]
- American Diabetes Association. Postprandial Blood Glucose. Diabetes Care 2001, 24, 775–778. [Google Scholar] [CrossRef] [PubMed]
- Decode Study Group. Glucose tolerance and mortality: Comparison of WHO and American Diabetes Association diagnostic criteria. The DECODE study group. European Diabetes Epidemiology Group. Diabetes Epidemiology: Collaborative analysis Of Diagnostic criteria in Europe. Lancet 1999, 354, 617–621. [Google Scholar] [CrossRef]
- de Vegt, F.; Dekker, J.M.; Ruhe, H.G.; Stehouwer, C.D.; Nijpels, G.; Bouter, L.M.; Heine, R.J. Hyperglycaemia is associated with all-cause and cardiovascular mortality in the Hoorn population: The Hoorn Study. Diabetologia 1999, 42, 926–931. [Google Scholar] [CrossRef]
- Donahue, R.P.; Abbott, R.D.; Reed, D.M.; Yano, K. Postchallenge glucose concentration and coronary heart disease in men of Japanese ancestry. Honolulu Heart Program. Diabetes 1987, 36, 689–692. [Google Scholar] [CrossRef]
- Orencia, A.J.; Daviglus, M.L.; Dyer, A.R.; Walsh, M.; Greenland, P.; Stamler, J. One-hour postload plasma glucose and risks of fatal coronary heart disease and stroke among nondiabetic men and women: The Chicago Heart Association Detection Project in Industry (CHA) Study. J. Clin. Epidemiol. 1997, 50, 1369–1376. [Google Scholar] [CrossRef]
- Livesey, G.; Taylor, R.; Livesey, H.F.; Buyken, A.E.; Jenkins, D.J.A.; Augustin, L.S.A.; Sievenpiper, J.L.; Barclay, A.W.; Liu, S.; Wolever, T.M.S.; et al. Dietary Glycemic Index and Load and the Risk of Type 2 Diabetes: Assessment of Causal Relations. Nutrients 2019, 11, 1436. [Google Scholar] [CrossRef]
- Livesey, G.; Taylor, R.; Livesey, H.F.; Buyken, A.E.; Jenkins, D.J.A.; Augustin, L.S.A.; Sievenpiper, J.L.; Barclay, A.W.; Liu, S.; Wolever, T.M.S.; et al. Dietary Glycemic Index and Load and the Risk of Type 2 Diabetes: A Systematic Review and Updated Meta-Analyses of Prospective Cohort Studies. Nutrients 2019, 11, 1280. [Google Scholar] [CrossRef]
- Livesey, G.; Livesey, H. Coronary Heart Disease and Dietary Carbohydrate, Glycemic Index, and Glycemic Load: Dose-Response Meta-analyses of Prospective Cohort Studies. Mayo Clin. Proc. Innov. Qual. Outcomes 2019, 3, 52–69. [Google Scholar] [CrossRef] [PubMed]
- Chiavaroli, L.; Di Pede, G.; Dall’Asta, M.; Cossu, M.; Francinelli, V.; Goldoni, M.; Scazzina, F.; Brighenti, F. The importance of glycemic index on post-prandial glycaemia in the context of mixed meals: A randomized controlled trial on pasta and rice. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 615–625. [Google Scholar] [CrossRef] [PubMed]
- Bornhorst, G.M.; Paul Singh, R. Gastric digestion in vivo and in vitro: How the structural aspects of food influence the digestion process. Annu. Rev. Food Sci. Technol. 2014, 5, 111–132. [Google Scholar] [CrossRef] [PubMed]
- Esfahani, A.; Wong, J.M.; Mirrahimi, A.; Srichaikul, K.; Jenkins, D.J.; Kendall, C.W. The glycemic index: Physiological significance. J. Am. Coll. Nutr. 2009, 28 (Suppl. S4), 439S–445S. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D.; Elliott, E.J. Low glycaemic index, or low glycaemic load, diets for diabetes mellitus. Cochrane Database Syst. Rev. 2009, 2009, CD006296. [Google Scholar] [CrossRef] [PubMed]
- Fleming, P.; Godwin, M. Low-glycaemic index diets in the management of blood lipids: A systematic review and meta-analysis. Fam. Pract. 2013, 30, 485–491. [Google Scholar] [CrossRef]
- Solomon, T.P.; Haus, J.M.; Kelly, K.R.; Cook, M.D.; Filion, J.; Rocco, M.; Kashyap, S.R.; Watanabe, R.M.; Barkoukis, H.; Kirwan, J.P. A low-glycemic index diet combined with exercise reduces insulin resistance, postprandial hyperinsulinemia, and glucose-dependent insulinotropic polypeptide responses in obese, prediabetic humans. Am. J. Clin. Nutr. 2010, 92, 1359–1368. [Google Scholar] [CrossRef]
- Mann, E.; Sunni, M.; Bellin, M.D. Secretion of Insulin in Response to Diet and Hormones. In The Pancreapedia: Exocrine Pancreas Knowledge Base; American Pancreatic Association: Prairie Village, KS, USA, 2020. [Google Scholar] [CrossRef]
- Grover, J.K.; Yadav, S.; Vats, V. Medicinal plants of India with anti-diabetic potential. J. Ethnopharmacol. 2002, 81, 81–100. [Google Scholar] [CrossRef]
- Horne, G.; Wilson, F.X.; Tinsley, J.; Williams, D.H.; Storer, R. Iminosugars past, present and future: Medicines for tomorrow. Drug Discov. Today 2011, 16, 107–118. [Google Scholar] [CrossRef]
- Lown, M.; Fuller, R.; Lightowler, H.; Fraser, A.; Gallagher, A.; Stuart, B.; Byrne, C.; Lewith, G. Mulberry-extract improves glucose tolerance and decreases insulin concentrations in normoglycaemic adults: Results of a randomised double-blind placebo-controlled study. PLoS ONE 2017, 12, e0172239. [Google Scholar] [CrossRef]
- Thondre, P.S.; Lightowler, H.; Ahlstrom, L.; Gallagher, A. Mulberry leaf extract improves glycaemic response and insulaemic response to sucrose in healthy subjects: Results of a randomized, double blind, placebo-controlled study. Nutr. Metab. 2021, 18, 41. [Google Scholar] [CrossRef] [PubMed]
- ISO 26642; Food Products—Determination of the Glycaemic Index (GI) and Recommendation for Food Classification. International Organisation for Standardization (ISO): Geneva, Switzerland, 2010.
- Floyd, J.C., Jr.; Fajans, S.S.; Conn, J.W.; Knopf, R.F.; Rull, J. Stimulation of insulin secretion by amino acids. J. Clin. Investig. 1966, 45, 1487–1502. [Google Scholar] [CrossRef] [PubMed]
- Wolpert, H.A.; Atakov-Castillo, A.; Smith, S.A.; Steil, G.M. Dietary fat acutely increases glucose concentrations and insulin requirements in patients with type 1 diabetes: Implications for carbohydrate-based bolus dose calculation and intensive diabetes management. Diabetes Care 2013, 36, 810–816. [Google Scholar] [CrossRef] [PubMed]
- Stanstrup, J.; Schou, S.S.; Holmer-Jensen, J.; Hermansen, K.; Dragsted, L.O. Whey protein delays gastric emptying and suppresses plasma fatty acids and their metabolites compared to casein, gluten, and fish protein. J. Proteome Res. 2014, 13, 2396–2408. [Google Scholar] [CrossRef] [PubMed]
- Gentilcore, D.; Chaikomin, R.; Jones, K.L.; Russo, A.; Feinle-Bisset, C.; Wishart, J.M.; Rayner, C.K.; Horowitz, M. Effects of fat on gastric emptying of and the glycemic, insulin, and incretin responses to a carbohydrate meal in type 2 diabetes. J. Clin. Endocrinol. Metab. 2006, 91, 2062–2067. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Li, X.; Xie, C.; Luo, X.; Bao, Y.; Wu, B.; Hu, Y.; Zhong, Z.; Liu, C.; Li, M. Prevention Effects and Possible Molecular Mechanism of Mulberry Leaf Extract and its Formulation on Rats with Insulin-Insensitivity. PLoS ONE 2016, 11, e0152728. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.; Baek, J.Y.; Choi, Y.J.; Han, M.J.; Kim, S.H.; Kim, T.H.; Lee, S.; Kang, K.S. Glucose-lowering effect of Reducose(R) enriched with 1-deoxynojirimycin and l-leucine: Studies on insulin secretion in INS-1 cells and reduction of blood glucose in diabetic rats. Heliyon 2024, 10, e25499. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, M.; Zagury, R.L.; Bhaskaran, K.; Neutel, J.; Yusof, B.N.M.; Yeo, L.; Kirwan, B.; Aprikian, O.; vo Eynatten, M.; Johansen, O.E. A Randomized, Placebo-Controlled Crossover Study to Evaluate Postprandial Glucometabolic Effects of Mulberry Leaf Extract, Vitamin D, Chromium, and Fiber in People with Type 2 Diabetes. Diabetes Ther. 2023, 14, 749–766. [Google Scholar] [CrossRef] [PubMed]
- Wajchenberg, B.L. Postprandial glycemia and cardiovascular disease in diabetes mellitus. Arq. Bras. Endocrinol. Metabol. 2007, 51, 212–221. [Google Scholar] [CrossRef]
- Schillinger, R.J.; Mwakamui, S.; Mulenga, C.; Tembo, M.; Hodges, P.; Besa, E.; Chandwe, K.; Owino, V.O.; Edwards, C.A.; Kelly, P.; et al. (13)C-sucrose breath test for the non-invasive assessment of environmental enteropathy in Zambian adults. Front. Med. 2022, 9, 904339. [Google Scholar] [CrossRef]

| All Recruited Participants (n = 43) | All Completed Participants (n = 37) | |
|---|---|---|
| Age (y) | 29.4 ± 10.0 | 30.0 ± 10.4 |
| Height (m) | 1.7 ± 0.1 | 1.7 ± 0.1 |
| Weight (kg) | 67.8 ± 11.1 | 67.8 ± 10.6 |
| BMI (kg/m2) | 23.3 ± 2.5 | 23.2 ± 2.4 |
| Fat mass (%) | 24.4 ± 8.0 | 24.8 ± 8.0 |
| Lean body mass (kg) | 51.3 ± 10.2 | 50.9 ± 9.8 |
| Time (min) | Reducose® 200 mg | Reducose® 225 mg | Reducose® 250 mg | Placebo |
|---|---|---|---|---|
| 0 | 4.6 ± 0.3 | 4.6 ± 0.4 | 4.7 ± 0.4 | 4.7 ± 0.4 |
| 15 | 4.5 ± 0.4 * | 4.4 ± 0.4 † | 4.5 ± 0.5 | 4.7 ± 0.5 |
| 30 | 5.2 ± 0.6 § | 5.1 ± 0.7 § | 5.2 ± 0.7 § | 5.9 ± 0.8 |
| 45 | 5.7 ± 0.8 † | 5.6 ± 0.7 § | 5.7 ± 0.7 § | 6.3 ± 0.9 |
| 60 | 5.6 ± 0.7 | 5.5 ± 0.7 * | 5.6 ± 0.8 | 5.9 ± 0.9 |
| 90 | 5.1 ± 0.6 | 5.2 ± 0.7 | 5.2 ± 0.7 | 5.3 ± 0.7 |
| 120 | 5.1 ± 0.5 | 5.1 ± 0.7 | 5.2 ± 0.5 | 5.2 ± 0.8 |
| 150 | 5.1 ± 0.5 | 5.0 ± 0.6 | 5.1 ± 0.5 | 5.1 ± 0.6 |
| 180 | 4.9 ± 0.4 | 4.9 ± 0.6 | 4.9 ± 0.5 | 4.8 ± 0.6 |
| iAUC | Reducose® 200 mg | Reducose® 225 mg | Reducose® 250 mg | Placebo |
|---|---|---|---|---|
| iAUC 60 | 32.6 ± 20.6 § | 27.8 ± 15.8 § | 30.4 ± 15.9 § | 54.6 ± 26.9 |
| iAUC 90 | 55.7 ± 35.5 † | 50.6 ± 30.7 § | 53.1 ± 31.3 § | 83.3 ± 43.1 |
| iAUC 120 | 71.7 ± 47.7 † | 68.5 ± 47.4 † | 69.7 ± 43.7 † | 102.5 ± 57.0 |
| iAUC 150 | 87.2 ± 59.5 † | 83.7 ± 62.7 † | 84.5 ± 52.6 † | 118.8 ± 70.3 |
| iAUC 180 | 99.3 ± 69.2 * | 96.3 ± 78.3 * | 95.5 ± 60.3 * | 129.6 ± 79.4 |
| Reducose® 200 mg | Reducose® 225 mg | Reducose® 250 mg | Placebo | |
|---|---|---|---|---|
| Peak blood glucose | 6.0 ± 0.6 † | 5.9 ± 0.7 § | 6.0 ± 0.7 † | 6.6 ± 0.8 |
| Time of blood glucose peak | 55.1 ± 24.8 | 61.2 ± 37.1 | 53.1 ± 27.1 | 47.4 ± 17.1 |
| Time (min) | Reducose® 200 mg | Reducose® 225 mg | Reducose® 250 mg | Placebo |
|---|---|---|---|---|
| 0 | 9.79 ± 4.94 | 9.30 ± 3.86 | 10.37 ± 3.83 | 10.36 ± 4.76 |
| 15 | 13.58 ± 8.81 | 12.38 ± 9.37 * | 13.98 ± 6.52 | 18.18 ± 12.85 |
| 30 | 29.07 ± 17.34 § | 27.60 ± 20.46 § | 30.05 ± 14.59 † | 49.55 ± 29.20 |
| 45 | 45.25 ± 29.27 * | 38.02 ± 18.11 § | 39.78 ± 19.56 § | 59.16 ± 34.43 |
| 60 | 43.07 ± 28.35 | 39.32 ± 20.42 * | 36.20 ± 15.59 † | 53.20 ± 31.50 |
| 90 | 31.45 ± 16.96 | 31.96 ± 19.76 | 30.41 ± 17.83 | 40.11 ± 22.92 |
| 120 | 25.71 ± 11.70 | 26.69 ± 13.36 | 27.39 ± 13.36 | 32.82 ± 19.64 |
| 150 | 24.05 ± 13.01 | 22.93 ± 11.80 | 22.82 ± 9.84 | 26.18 ± 15.25 |
| 180 | 18.88 ± 10.67 | 20.23 ± 11.93 * | 20.34 ± 10.61 | 16.63 ± 8.46 |
| iAUC | Reducose® 200 mg | Reducose® 225 mg | Reducose® 250 mg | Placebo |
|---|---|---|---|---|
| iAUC 60 | 1136.35 ± 717.61 § | 1002.99 ± 639.23 § | 991.71 ± 532.46 § | 1763.05 ± 991.94 |
| iAUC 90 | 1960.43 ± 1178.94 * | 1769.64 ± 1089.45 § | 1679.62 ± 870.85 § | 2851.81 ± 1604.38 |
| iAUC 120 | 2524.14 ± 1451.71 * | 2393.81 ± 1445.54 † | 2235.56 ± 1194.78 § | 3634.91 ± 2089.11 |
| iAUC 150 | 2977.11 ± 1673.58 * | 2859.19 ± 1643.01 † | 2678.08 ± 1400.30 § | 4209.05 ± 2445.12 |
| iAUC 180 | 3331.52 ± 1868.61 * | 3224.65 ± 1824.11 * | 3016.49 ± 1561.77 § | 4544.78 ± 2616.76 |
| Reducose® 200 mg | Reducose® 225 mg | Reducose® 250 mg | Placebo | |
|---|---|---|---|---|
| Peak plasma insulin | 52.62 ± 31.52 § | 45.74 ± 21.62 § | 45.51 ± 17.55 § | 68.69 ± 33.35 |
| Time of plasma insulin peak | 54.73 ± 26.74 | 63.24 ± 31.05 * | 56.76 ± 26.49 | 44.59 ± 13.46 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thondre, P.S.; Butler, I.; Tammam, J.; Achebe, I.; Young, E.; Lane, M.; Gallagher, A. Understanding the Impact of Different Doses of Reducose® Mulberry Leaf Extract on Blood Glucose and Insulin Responses after Eating a Complex Meal: Results from a Double-Blind, Randomised, Crossover Trial. Nutrients 2024, 16, 1670. https://doi.org/10.3390/nu16111670
Thondre PS, Butler I, Tammam J, Achebe I, Young E, Lane M, Gallagher A. Understanding the Impact of Different Doses of Reducose® Mulberry Leaf Extract on Blood Glucose and Insulin Responses after Eating a Complex Meal: Results from a Double-Blind, Randomised, Crossover Trial. Nutrients. 2024; 16(11):1670. https://doi.org/10.3390/nu16111670
Chicago/Turabian StyleThondre, Pariyarath Sangeetha, Isabel Butler, Jonathan Tammam, Ifunanya Achebe, Elysia Young, Michael Lane, and Andrew Gallagher. 2024. "Understanding the Impact of Different Doses of Reducose® Mulberry Leaf Extract on Blood Glucose and Insulin Responses after Eating a Complex Meal: Results from a Double-Blind, Randomised, Crossover Trial" Nutrients 16, no. 11: 1670. https://doi.org/10.3390/nu16111670
APA StyleThondre, P. S., Butler, I., Tammam, J., Achebe, I., Young, E., Lane, M., & Gallagher, A. (2024). Understanding the Impact of Different Doses of Reducose® Mulberry Leaf Extract on Blood Glucose and Insulin Responses after Eating a Complex Meal: Results from a Double-Blind, Randomised, Crossover Trial. Nutrients, 16(11), 1670. https://doi.org/10.3390/nu16111670






