Atractylodes macrocephala Koidz Alleviates Symptoms in Zymosan-Induced Irritable Bowel Syndrome Mouse Model through TRPV1, NaV1.5, and NaV1.7 Channel Modulation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Analysis of AMK Targets
2.2. Preparation of AMK Extract and High-Performance Liquid Chromatography (HPLC) Analysis
2.3. Animal Experiments
2.4. Measurement of Body Weight Change and Food Intake
2.5. Observation of Changes in Colon and Stool Conditions
2.6. Histological Examination of the Colon
2.7. Tumor Necrosis Factor (TNF)-α Gene Expression Evaluation by Quantitative RT-qPCR
2.8. Pain-Related Behavior Measurement
2.9. Plasmid Transfection
2.10. Electrophysiological Experiments
2.11. Statistical Analysis
3. Results
3.1. Active Compounds of AMK
3.2. Identification of 35 Compounds Related to GI Diseases in AMK
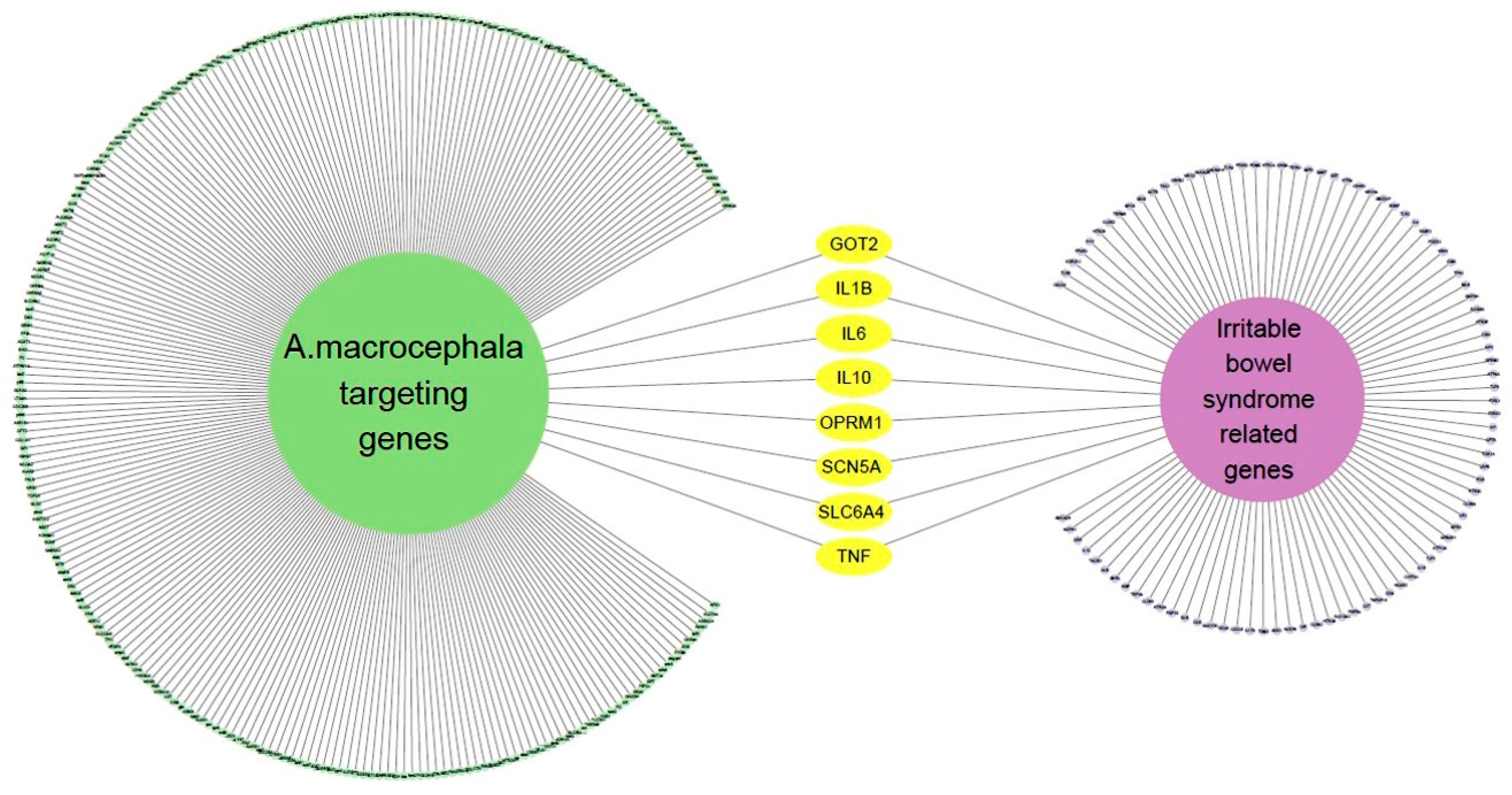
3.3. Eight Genes Are Included in Both IBS-Related Genes and AMK Target Genes
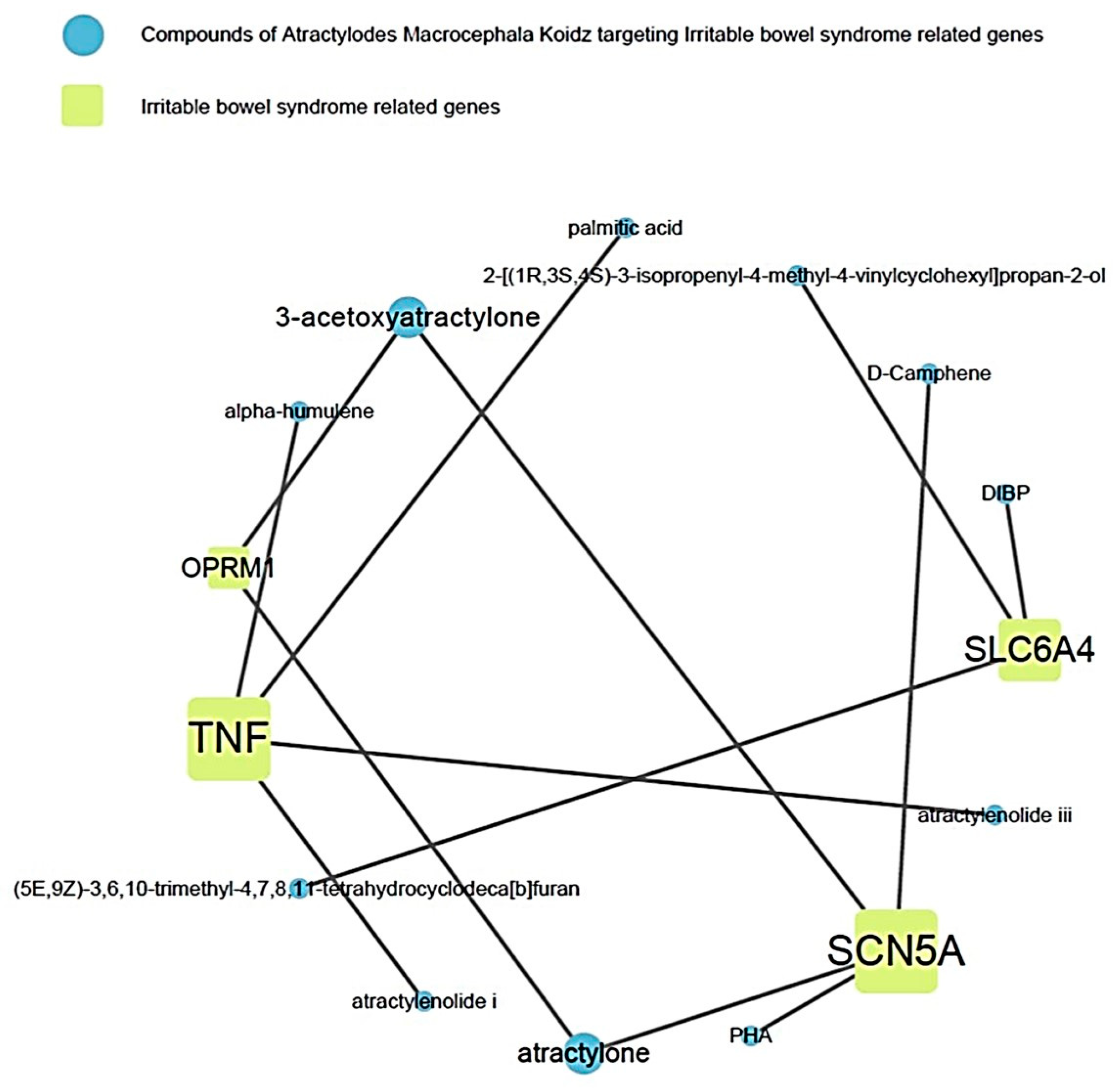
3.4. Relevance of AMK Compounds and IBS-Related Genes
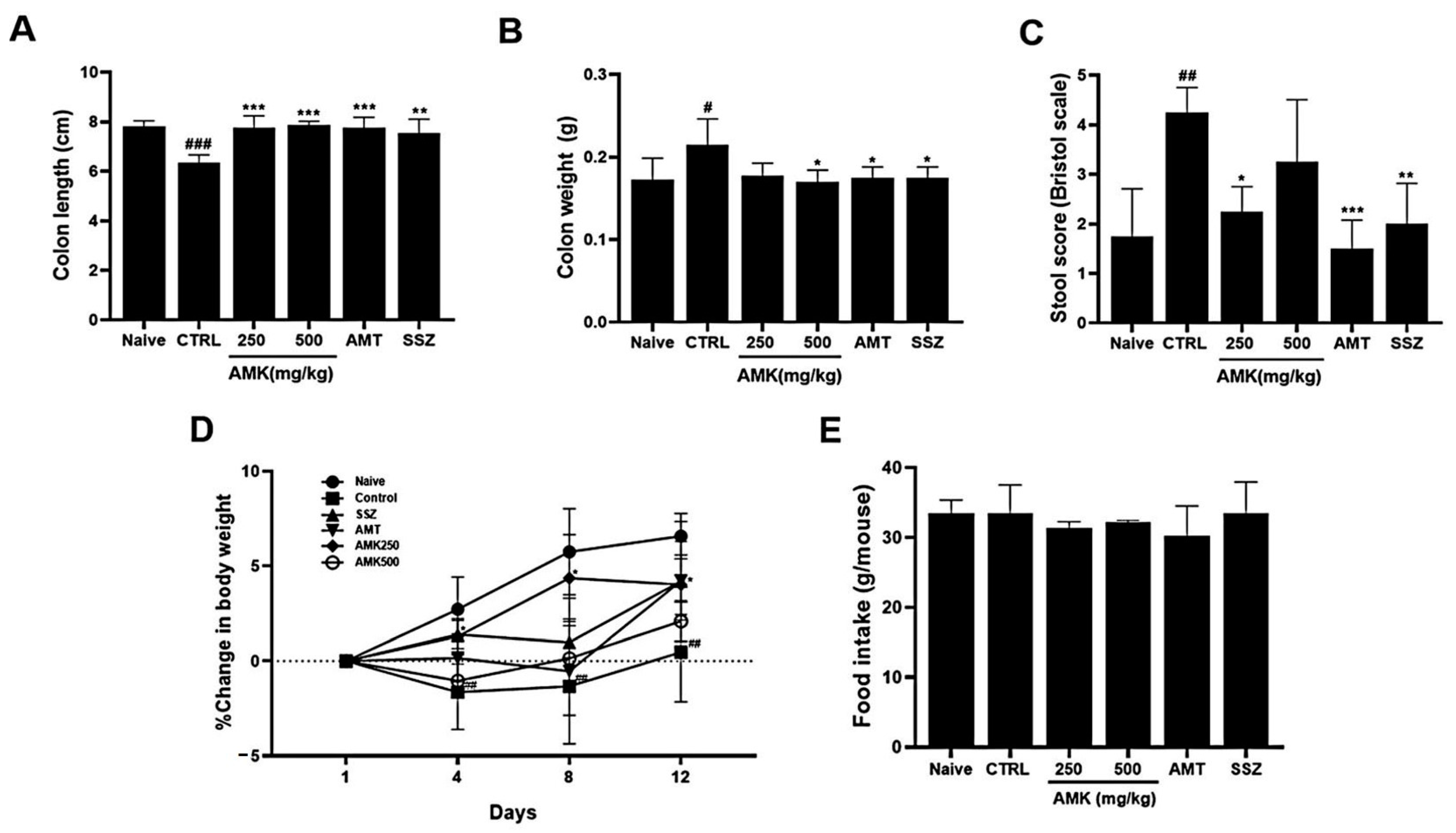
3.5. Effects of AMK Extract on Zymosan-Induced Colonic Changes
3.6. Effects of AMK Extract on Body Weight Change and Food Intake
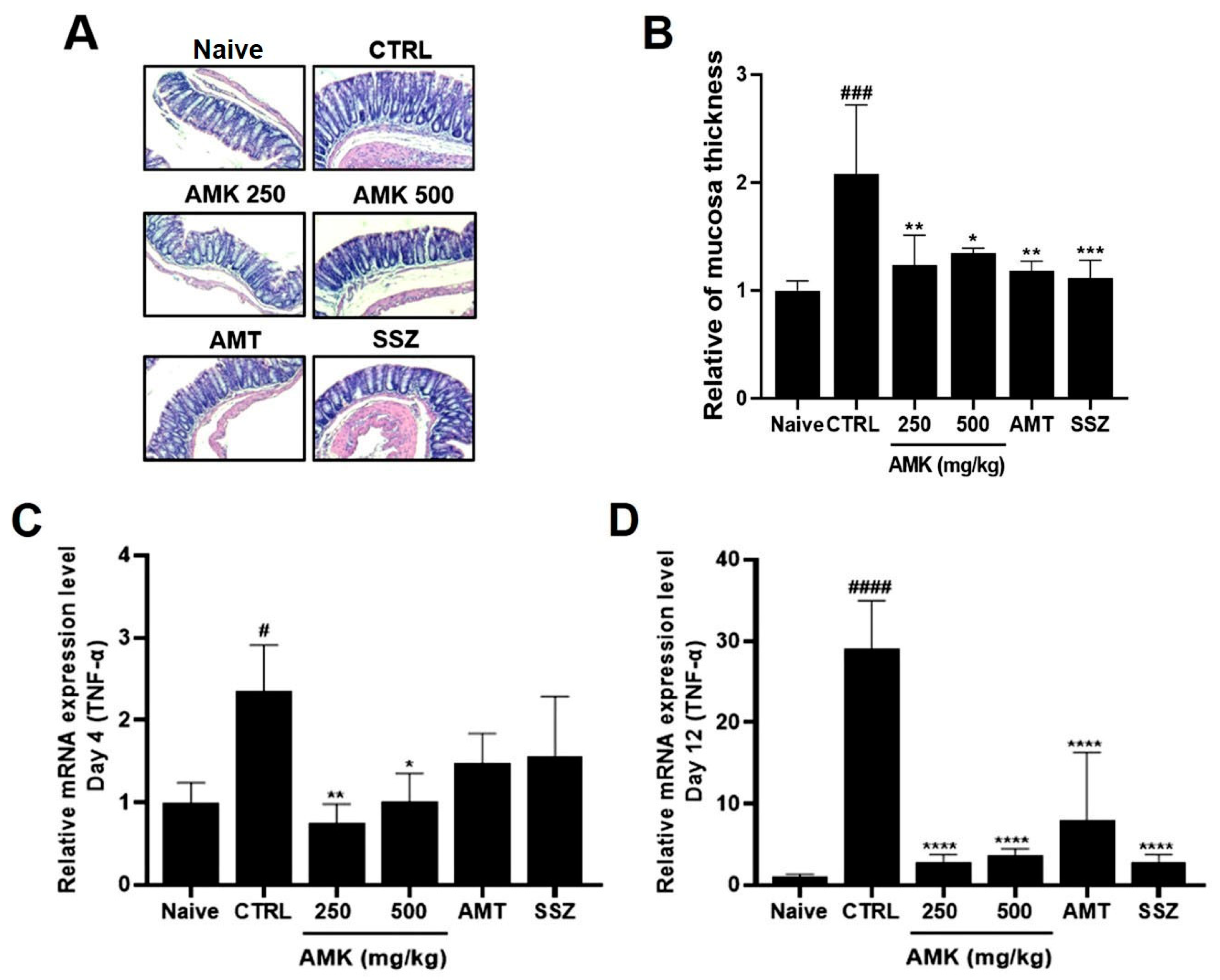
3.7. Effect of AMK Extract on Tissue Changes and TNF-α Expression Levels
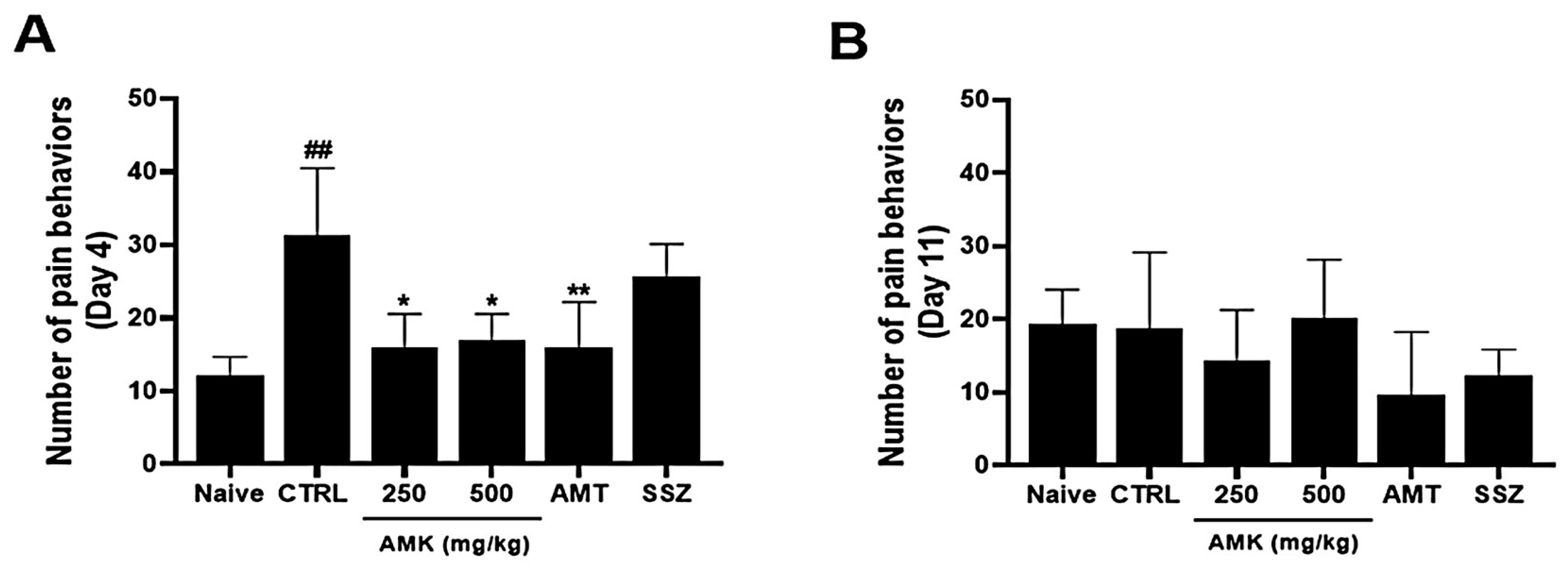
3.8. Effects of AMK Extract on Pain-Related Behaviors
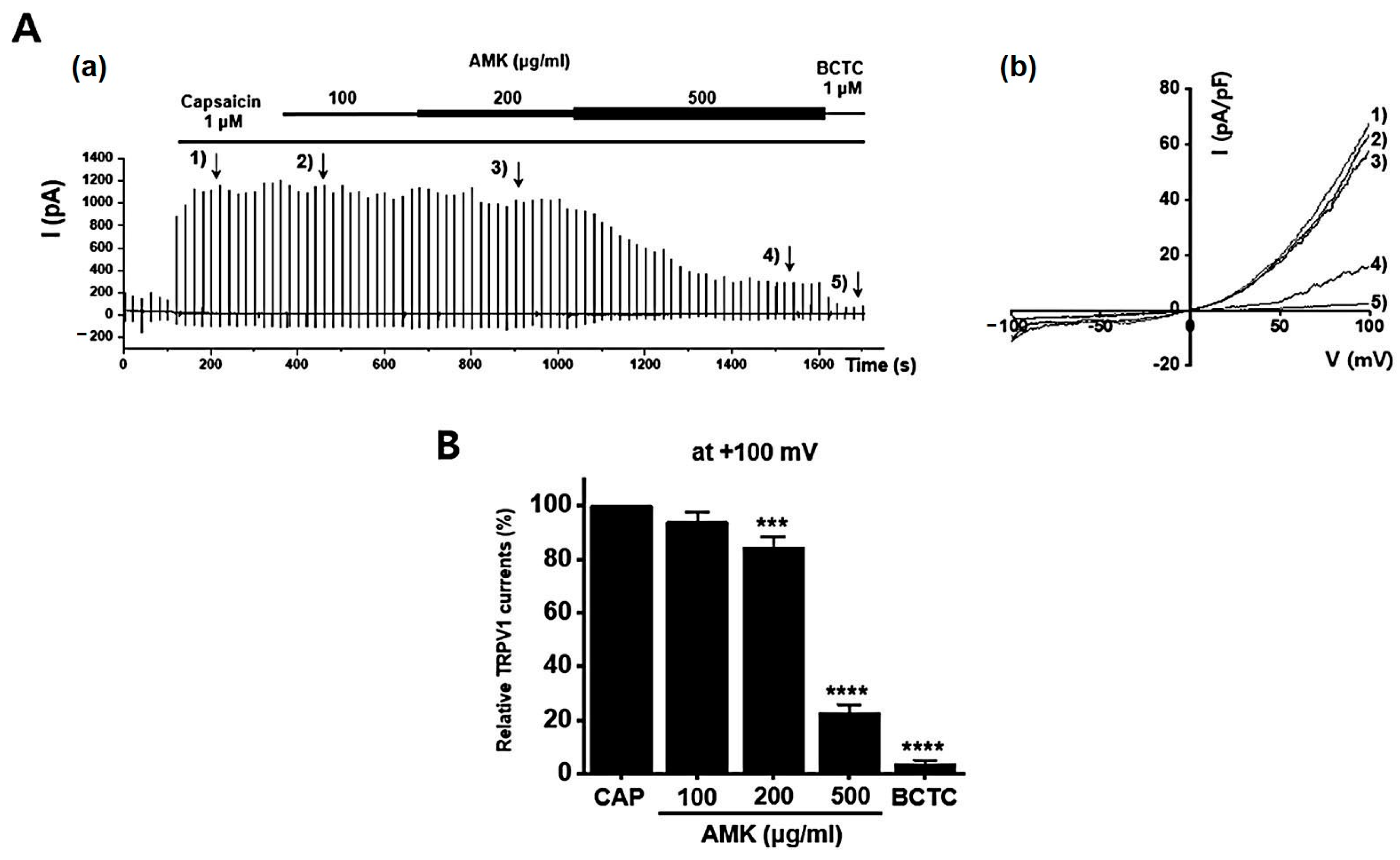
3.9. Effects of AMK Extract on TRP Channel Currents
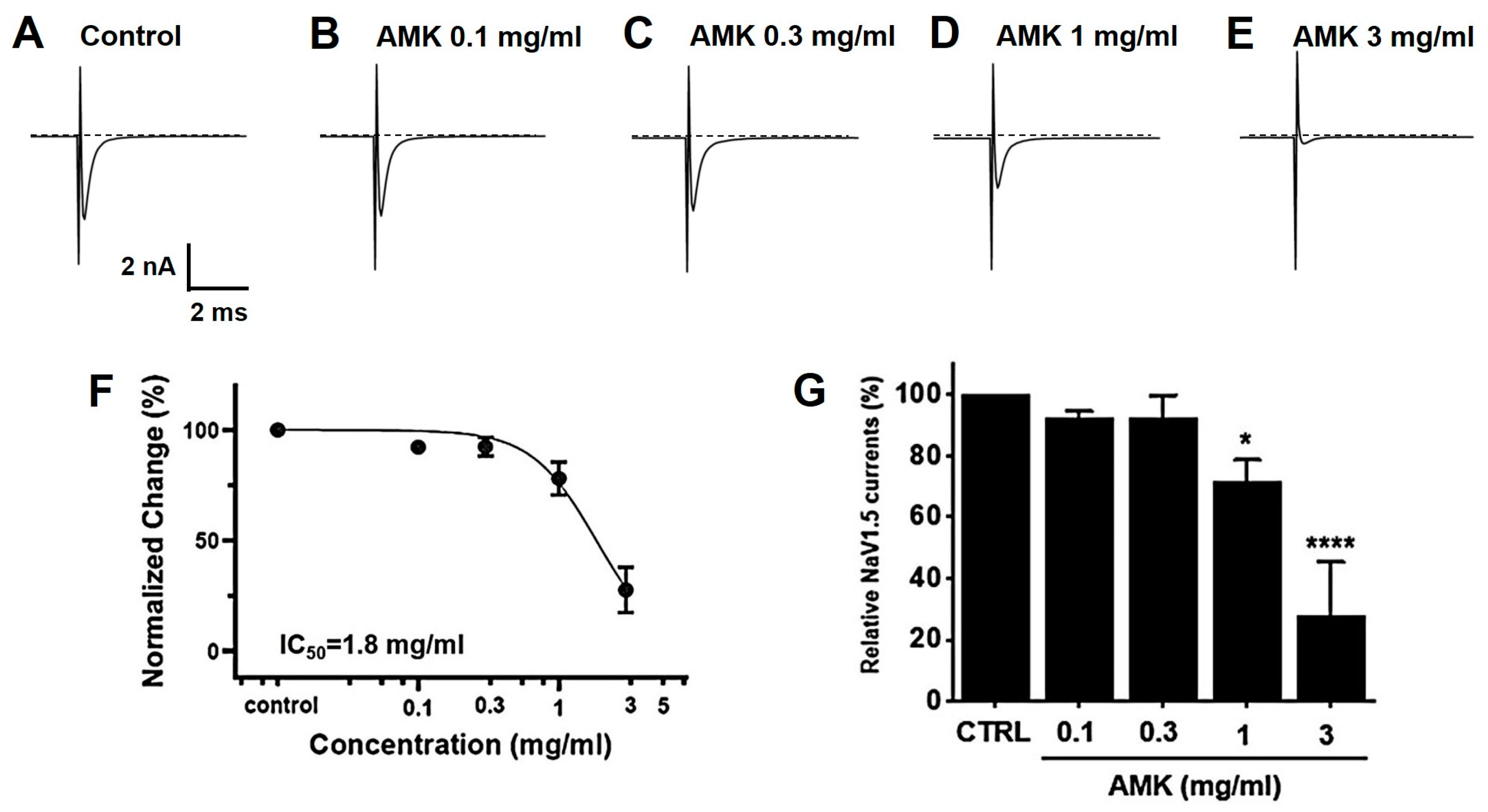
3.10. Effects of AMK Extract on NaV1.5 and NaV1.7 Currents
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhu, B.; Zhang, Q.L.; Hua, J.W.; Cheng, W.L.; Qin, L.P. The traditional uses, phytochemistry, and pharmacology of Atractylodes macrocephala Koidz.: A review. J. Ethnopharmacol. 2018, 226, 143–167. [Google Scholar] [CrossRef] [PubMed]
- Song, H.P.; Li, R.L.; Chen, X.; Wang, Y.Y.; Cai, J.Z.; Liu, J.; Chen, W.W. Atractylodes macrocephala Koidz promotes intestinal epithelial restitution via the polyamine—Voltage-gated K+ channel pathway. J. Ethnopharmacol. 2014, 152, 163–172. [Google Scholar] [CrossRef] [PubMed]
- Song, H.P.; Li, R.L.; Zhou, C.; Cai, X.; Huang, H.Y. Atractylodes macrocephala Koidz stimulates intestinal epithelial cell migration through a polyamine dependent mechanism. J. Ethnopharmacol. 2015, 159, 23–35. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Zhou, G.; Wang, M.; Peng, Y.; Li, X. The Metabolism of Polysaccharide from Atractylodes macrocephala Koidz and Its Effect on Intestinal Microflora. Evid. Based Complement. Altern. Med. 2014, 2014, 926381. [Google Scholar] [CrossRef]
- Wang, Z.; Li, R.L.; Xu, S.F.; Chen, W.W. Effects of Atractylodes macrocephala monosaccharide composition on cytodifferentiation and villin expression of IEC-6 cells in vitro. J. Chin. Med. Mater 2010, 33, 938–944. [Google Scholar]
- Zhang, Y.Q.; Xu, S.B.; Lin, Y.C. Gastrointestinal inhibitory effects of sesquiterpene lactones from Atractylodes macrocephala. J. Chin. Med. Mater 1999, 22, 636–640. [Google Scholar]
- Cashman, M.D.; Martin, D.K.; Dhillon, S.; Puli, S.R. Irritable Bowel Syndrome: A Clinical Review. Curr. Rheumatol. Rev. 2016, 12, 13–26. [Google Scholar] [CrossRef]
- Chiarioni, G.; Popa, S.L.; Ismaiel, A.; Pop, C.; Dumitrascu, D.I.; Brata, V.D.; Duse, T.A.; Incze, V.; Surdea-Blaga, T. Herbal Remedies for Constipation-Predominant Irritable Bowel Syndrome: A Systematic Review of Randomized Controlled Trials. Nutrients 2013, 15, 4216. [Google Scholar] [CrossRef] [PubMed]
- Xie, P.; Luo, M.; Deng, X.; Fan, J.; Xiong, L. Outcome-Specific Efficacy of Different Probiotic Strains and Mixtures in Irritable Bowel Syndrome: A Systematic Review and Network Meta-Analysis. Nutrients 2023, 15, 3856. [Google Scholar] [CrossRef]
- Choi, N.R.; Kwon, M.J.; Choi, W.G.; Kim, S.C.; Park, J.W.; Nam, J.H.; Kim, B.J. The traditional herbal medicines mixture, Banhasasim-tang, relieves the symptoms of irritable bowel syndrome via modulation of TRPA1, NaV1.5 and NaV1.7 channels. J. Ethnopharmacol. 2023, 312, 116499. [Google Scholar] [CrossRef]
- Park, B.K.; Chun, E.; Choi, J.J.; Shin, Y.; Kho, Y.T.; Oh, S.H.; Kim, S.Y.; Lee, T.H.; Kim, T.W.; Shin, E.; et al. Administration of Wasabia koreana Ameliorates Irritable Bowel Syndrome-Like Symptoms in a Zymosan-Induced Mouse Model. J. Med. Food 2017, 20, 474–484. [Google Scholar] [CrossRef]
- Yu, S.; Chun, E.; Ji, Y.; Lee, Y.J.; Jin, M. Effects of red ginseng on gut, microbiota, and brain in a mouse model of post-infectious irritable bowel syndrome. J. Ginseng Res. 2012, 45, 706–716. [Google Scholar] [CrossRef] [PubMed]
- Coutinho, S.V.; Meller, S.T.; Gebhart, G.F. Intracolonic zymosan produces visceral hyperalgesia in the rat that is mediated by spinal NMDA and non-NMDA receptors. Brain Res. 1996, 736, 7–15. [Google Scholar] [CrossRef] [PubMed]
- UniProt Consortium. UniProt: A worldwide hub of protein knowledge. Nucleic Acids Res. 2019, 47, D506–D515. [Google Scholar] [CrossRef] [PubMed]
- Choi, N.R.; Choi, W.G.; Zhu, A.; Park, J.; Kim, Y.T.; Hong, J.; Kim, B.J. Exploring Therapeutic Effects of Atractylodes macrocephala Koidz against Human Gastric cancer. Nutrients 2024, 16, 965. [Google Scholar] [CrossRef] [PubMed]
- Laird, J.M.A.; Martinez-Caro, L.; Garcia-Nicas, E.; Cervero, F. A new model of visceral pain and referred hyperalgesia in the mouse. Pain 2001, 92, 335–342. [Google Scholar] [CrossRef] [PubMed]
- Morgan, V.; Pickens, D.; Gautam, S.; Kessler, R.; Mertz, H. Amitriptyline reduces rectal pain related activation of the anterior cingulate cortex in patients with irritable bowel syndrome. Gut 2005, 54, 601–607. [Google Scholar] [CrossRef] [PubMed]
- Pruzanski, W.; Stefanski, E.; Vadas, P.; Ramamurthy, N.S. Inhibition of extracellular release of proinflammatory secretory phospholipase A2 (sPLA2) by sulfasalazine: A novel mechanism of anti-inflammatory activity. Biochem. Pharmacol. 1997, 53, 1901–1907. [Google Scholar] [CrossRef] [PubMed]
- Nishiyama, Y.; Kataoka, T.; Yamato, K.; Taguchi, T.; Yamaoka, K. Suppression of dextran sulfate sodium-induced colitis in mice by radon inhalation. Mediat. Inflamm. 2012, 2012, 239617. [Google Scholar] [CrossRef]
- Heber, S.; Ciotu, C.I.; Hartner, G.; Gold-Binder, M.; Ninidze, N.; Gleiss, A.; Kress, H.G.; Fischer, M.J.M. TRPV1 antagonist BCTC inhibits pH 6.0-induced pain in human skin. Pain 2020, 161, 1532–1541. [Google Scholar] [CrossRef]
- Zhang, C.; Huang, Y.; Li, P.; Chen, X.; Liu, F.; Hou, Q. Ginger relieves intestinal hypersensitivity of diarrhea predominant irritable bowel syndrome by inhibiting proinflammatory reaction. BMC Complement. Med. Ther. 2020, 20, 279. [Google Scholar] [CrossRef]
- Ueda, T.; Shikano, M.; Kamiya, T.; Joh, T.; Ugawa, S. The TRPV4 channel is a novel regulator of intracellular Ca2+ in human esophageal epithelial cells. Am. J. Physiol. Gastrointest. Liver Physiol. 2011, 301, G138–G147. [Google Scholar] [CrossRef] [PubMed]
- Jin, M.; Wu, Z.; Chen, L.; Jaimes, J.; Collins, D.; Walters, E.T.; O’Neil, R.G. Determinants of TRPV4 activity following selective activation by small molecule agonist GSK1016790A. PLoS ONE 2011, 6, e16713. [Google Scholar] [CrossRef]
- Gyamfi, O.A.; Bortey-Sam, N.; Donkor, A.B.; White, C.W.; Logue, B.A. Analysis of TRPA1 antagonist, A-967079, in plasma using high-performance liquid chromatography tandem mass-spectrometry. J. Pharm. Anal. 2020, 10, 157–163. [Google Scholar] [CrossRef]
- Sandor, Z.; Dekany, A.; Kelemen, D.; Bencsik, T.; Papp, R.; Bartho, L. The TRPA1 Activator Allyl Isothiocyanate (AITC) Contracts Human Jejunal Muscle: Pharmacological Analysis. Basic Clin. Pharmacol. Toxicol. 2016, 119, 341–342. [Google Scholar] [CrossRef] [PubMed]
- Canavan, C.; West, J.; Card, T. The epidemiology of irritable bowel syndrome. Clin. Epidemiol. 2014, 6, 71–80. [Google Scholar]
- Defrees, D.N.; Bailey, J. Irritable Bowel Syndrome: Epidemiology, Pathophysiology, Diagnosis, and Treatment. Prim. Care 2017, 44, 655–671. [Google Scholar] [CrossRef] [PubMed]
- Chaudhury, D.; Liu, H.; Han, M.H. Neuronal correlates of depression. Cell. Mol. Life Sci. 2015, 72, 4825–4848. [Google Scholar] [CrossRef]
- Drossman, D.A.; Hasler, W.L. Rome IV-Functional GI Disorders: Disorders of Gut-Brain Interaction. Gastroenterology 2016, 150, 1257–1261. [Google Scholar] [CrossRef]
- Marchesi, J.R. Prokaryotic and eukaryotic diversity of the human gut. Adv. Appl. Microbiol. 2010, 72, 43–62. [Google Scholar]
- Liu, Y.H.; Chen, B.L.; Zhou, X.L.; Li, P.; Qiu, Y.X.; Fu, C.X. Studies on genetic diversity in cultivated populations of Atractylodes macrocephala. Zhongguo Zhong Yao Za Zhi 2008, 33, 2756–2760. [Google Scholar] [PubMed]
- Kim, J.H.; Doh, E.J.; Lee, G. Evaluation of Medicinal Categorization of Atractylodes japonica Koidz. by Using Internal Transcribed Spacer Sequencing Analysis and HPLC Fingerprinting Combined with Statistical Tools. Evid. Based Complement. Altern. Med. 2016, 2016, 2926819. [Google Scholar]
- Le, S.H.; Tran, M.H.; Lee, J.S.; Ngo, Q.M.; Woo, M.H.; Min, B.S. Inflammatory Inhibitory Activity of Sesquiterpenoids from Atractylodes macrocephala Rhizomes. Chem. Pharm. Bull. 2016, 64, 507–511. [Google Scholar]
- Shu, Y.T.; Kao, K.T.; Weng, C.S. In vitro antibacterial and cytotoxic activities of plasma-modified polyethylene terephthalate nonwoven dressing with aqueous extract of Rhizome Atractylodes macrocephala. Mater. Sci. Eng. C Mater. Biol. Appl. 2017, 77, 606–612. [Google Scholar] [CrossRef] [PubMed]
- Beckers, A.B.; Weerts, Z.; Helyes, Z.; Masclee, A.A.M.; Keszthelyi, D. Review article: Transient receptor potential channels as possible therapeutic targets in irritable bowel syndrome. Aliment. Pharmacol. Ther. 2017, 46, 938–952. [Google Scholar] [CrossRef] [PubMed]
- Emery, E.C.; Luiz, A.P.; Wood, J.N. Nav1.7 and other voltage-gated sodium channels as drug targets for pain relief. Expert Opin. Ther. Targets 2016, 20, 975–983. [Google Scholar] [CrossRef] [PubMed]
- Zielinska, M.; Jarmuz, A.; Wasilewski, A.; Salaga, M.; Fichna, J. Role of transient receptor potential channels in intestinal inflammation and visceral pain: Novel targets in inflammatory bowel diseases. Inflamm. Bowel Dis. 2015, 21, 419–427. [Google Scholar] [CrossRef] [PubMed]
- Stucky, C.L.; Dubin, A.E.; Jeske, N.A.; Malin, S.A.; McKemy, D.D.; Story, G.M. Roles of transient receptor potential channels in pain. Brain Res. Rev. 2009, 60, 2–23. [Google Scholar] [CrossRef]
- Wang, J.; Ou, S.W.; Bai, Y.F.; Wang, Y.J.; Xu, Z.D.; Luan, G.M. Downregulation of adult and neonatal Nav1.5 in the dorsal root ganglia and axon of peripheral sensory neurons of rats with spared nerve injury. Int. J. Mol. Med. 2018, 41, 2225–2232. [Google Scholar] [CrossRef]





| Molecule Name | Structure | MW * | OB (%) * | Caco-2 * | DL * |
|---|---|---|---|---|---|
| 12-senecioyl-2E,8E,10E-atractylentriol | 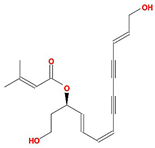 | 312.39 | 62.4 | 0.01 | 0.22 |
| 14-acetyl-12-senecioyl-2E,8E,10E-atractylentriol |  | 355.44 | 60.31 | 0.33 | 0.31 |
| 14-acetyl-12-senecioyl-2E,8Z,10E-atractylentriol |  | 356.45 | 63.37 | 0.42 | 0.3 |
| α-Longipinene | 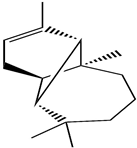 | 204.39 | 53.26 | 1.83 | 0.12 |
| α-Amyrin |  | 426.8 | 39.51 | 1.42 | 0.76 |
| (3S,8S,9S,10R,13R,14S,17R)-10,13-dimethyl-17-[(2R,5S)-5-propan-2-yloctan-2-yl]-2,3,4,7,8,9,11,12,14,15,16,17-dodecahydro-1H-cyclopenta[a]phenanthren-3-ol |  | 428.82 | 36.23 | 1.45 | 0.78 |
| Akridin | 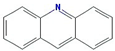 | 179.23 | 33.71 | 1.63 | 0.1 |
| Atractylenolide I | 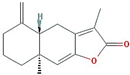 | 230.33 | 37.37 | 1.3 | 0.15 |
| Atractylenolide II |  | 232.35 | 47.5 | 1.3 | 0.15 |
| Atractylenolide III | 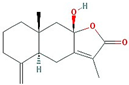 | 248.35 | 68.11 | 0.75 | 0.17 |
| atractylone | 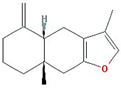 | 216.35 | 41.1 | 1.76 | 0.13 |
| Juniper camphor |  | 222.41 | 33.3 | 1.44 | 0.1 |
| (5E,9Z)-3,6,10-trimethyl-4,7,8,11-tetrahydrocyclodeca[b]furan | 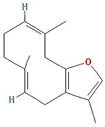 | 216.35 | 43.17 | 1.77 | 0.1 |
| 3β-acetoxyatractylone |  | 274.39 | 54.07 | 1.13 | 0.22 |
| DIBP | 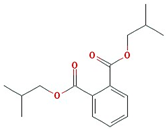 | 278.38 | 49.63 | 0.85 | 0.13 |
| Selina-4(14),7(11)-dien-8-one |  | 218.37 | 32.31 | 1.42 | 0.1 |
| Alloaromadedrene |  | 204.39 | 53.46 | 1.83 | 0.1 |
| 8β-ethoxy atractylenolide Ⅲ | 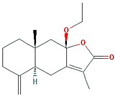 | 276.41 | 35.95 | 1.08 | 0.21 |
| Molecular Name | Gene Name | Disease Name |
|---|---|---|
| (+/−)−Isoborneol | PTGS2 | Adenomatous polyposis |
| Colorectal cancer | ||
| Peutz–Jeghers syndrome | ||
| (3S)−3−[(1R)−1,5−dimethylhex−4−enyl]−6− methylenecyclohexene | PTGS2 | Adenomatous polyposis |
| Colorectal cancer | ||
| Peutz–Jeghers syndrome | ||
| (5E,9Z)−3,6,10−trimethyl−4,7,8,11−tetrahydrocyclodeca[b]furan | NOS3 | Colon cancer |
| PTGS2 | Adenomatous polyposis | |
| Colorectal cancer | ||
| Peutz–Jeghers syndrome | ||
| SLC6A4 | * Irritable bowel syndrome | |
| 14−acetyl−12−senecioyl−2E,8Z,10E−atractylentriol | PTGS2 | Adenomatous polyposis |
| Colorectal cancer | ||
| Peutz–Jeghers syndrome | ||
| 2−[(1R,3S,4S)−3−isopropenyl−4−methyl−4−vinylcyclohexyl]propan−2−ol | SLC6A4 | * Irritable bowel syndrome |
| 3β−acetoxyatractylone | OPRM1 | Diarrhea |
| Opioid-induced bowel dysfunction | ||
| * Irritable bowel syndrome | ||
| NOS3 | Colon cancer | |
| Adenomatous polyposis | ||
| PTGS2 | Colorectal cancer | |
| Peutz–Jeghers syndrome | ||
| SCN5A | * Irritable bowel syndrome | |
| 8β−ethoxy atractylenolide Ⅲ | PTGS2 | Adenomatous polyposis |
| Colorectal cancer | ||
| Peutz–Jeghers syndrome | ||
| Akridin | PTGS2 | Adenomatous polyposis |
| Colorectal cancer | ||
| Peutz–Jeghers syndrome | ||
| Alpha−Curcumene | PTGS2 | Adenomatous polyposis |
| Colorectal cancer | ||
| Peutz–Jeghers syndrome | ||
| Alpha−humulene | PTGS2 | Adenomatous polyposis |
| Colorectal cancer | ||
| Peutz–Jeghers syndrome | ||
| TNF | * Irritable bowel syndrome | |
| ASI | ALOX5 | Gastrointestinal Cancers |
| Inflammatory Bowel Disease | ||
| Pancreatic Cancer | ||
| Ulcerative colitis | ||
| Atractylenolide i | TNF | * Irritable bowel syndrome |
| Atractylenolide iii | TNF | * Irritable bowel syndrome |
| Atractylone | Diarrhea | |
| OPRM1 | Opioid-induced bowel dysfunction | |
| * Irritable bowel syndrome | ||
| NOS3 | Colon cancer | |
| SCN5A | * Irritable bowel syndrome | |
| Beta−caryophyllene | PTGS2 | Adenomatous polyposis |
| Colorectal cancer | ||
| Peutz–Jeghers syndrome | ||
| Beta−Humulene | PTGS2 | Adenomatous polyposis |
| Colorectal cancer | ||
| Peutz–Jeghers syndrome | ||
| Beta−Selinene | PTGS2 | Adenomatous polyposis |
| Colorectal cancer | ||
| Peutz–Jeghers syndrome | ||
| D−Camphene | Adenomatous polyposis | |
| PTGS2 | Colorectal cancer | |
| Peutz–Jeghers syndrome | ||
| SCN5A | * Irritable bowel syndrome | |
| DIBP | SLC6A4 | * Irritable bowel syndrome |
| DTY | NOS3 | Colon cancer |
| Adenomatous polyposis | ||
| PTGS2 | Colorectal cancer | |
| Peutz–Jeghers syndrome | ||
| GLY | CTNNB1 | Colorectal cancer |
| LTA4H | Esophageal cancer | |
| Crohns’s Disease, unspecified | ||
| MMP12 | Gastro-intestinal ulcers | |
| Ulcerative colitis | ||
| AMY2A | Pancreatic disease | |
| Adenomatous polyposis | ||
| PTGS2 | Colorectal cancer | |
| Peutz–Jeghers syndrome | ||
| RRM1 | Pancreatic Neoplasms | |
| Gulutamine | LTA4H | Esophageal cancer |
| Adenomatous polyposis | ||
| PTGS2 | Colorectal cancer | |
| Peutz–Jeghers syndrome | ||
| Hemo−sol | PTGS2 | Adenomatous polyposis |
| Colorectal cancer | ||
| Peutz–Jeghers syndrome | ||
| Istidina | PTGS2 | Adenomatous polyposis |
| Colorectal cancer | ||
| Peutz–Jeghers syndrome | ||
| Juniper camphor | PTGS2 | Adenomatous polyposis |
| Colorectal cancer | ||
| Peutz–Jeghers syndrome | ||
| L−Arginin | PTGS2 | Adenomatous polyposis |
| Colorectal cancer | ||
| Peutz–Jeghers syndrome | ||
| LPG | Crohns’s Disease, unspecified | |
| MMP12 | Gastro-intestinal ulcers | |
| Ulcerative colitis | ||
| RRM1 | Pancreatic Neoplasms | |
| L−Valin | PTGS2 | Adenomatous polyposis |
| Colorectal cancer | ||
| Peutz–Jeghers syndrome | ||
| Palmitic acid | PTGS2 | Adenomatous polyposis |
| Colorectal cancer | ||
| Peutz–Jeghers syndrome | ||
| TNF | * Irritable bowel syndrome | |
| PHA | NOS3 | Colon cancer |
| Adenomatous polyposis | ||
| PTGS2 | Colorectal cancer | |
| Peutz–Jeghers syndrome | ||
| SCN5A | * Irritable bowel syndrome | |
| Prolinum | PTGS2 | Adenomatous polyposis |
| Colorectal cancer | ||
| Peutz–Jeghers syndrome | ||
| Scopoletol | CA1 | Pancreatic cancer |
| LTA4H | Esophageal cancer | |
| Adenomatous polyposis | ||
| PTGS2 | Colorectal cancer | |
| Peutz–Jeghers syndrome | ||
| Selina−4(14),7(11)−dien−8−one | PTGS2 | Adenomatous polyposis |
| Colorectal cancer | ||
| Peutz–Jeghers syndrome | ||
| α−Longipinene | PTGS2 | Adenomatous polyposis |
| Colorectal cancer | ||
| Peutz–Jeghers syndrome | ||
| γ−elemene | PTGS2 | Adenomatous polyposis |
| Colorectal cancer | ||
| Peutz–Jeghers syndrome |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, N.-R.; Choi, W.-G.; Lee, J.-H.; Park, J.; Kim, Y.-T.; Das, R.; Woo, J.-H.; Kim, B.-J. Atractylodes macrocephala Koidz Alleviates Symptoms in Zymosan-Induced Irritable Bowel Syndrome Mouse Model through TRPV1, NaV1.5, and NaV1.7 Channel Modulation. Nutrients 2024, 16, 1683. https://doi.org/10.3390/nu16111683
Choi N-R, Choi W-G, Lee J-H, Park J, Kim Y-T, Das R, Woo J-H, Kim B-J. Atractylodes macrocephala Koidz Alleviates Symptoms in Zymosan-Induced Irritable Bowel Syndrome Mouse Model through TRPV1, NaV1.5, and NaV1.7 Channel Modulation. Nutrients. 2024; 16(11):1683. https://doi.org/10.3390/nu16111683
Chicago/Turabian StyleChoi, Na-Ri, Woo-Gyun Choi, Jong-Hwan Lee, Joon Park, Yun-Tai Kim, Raju Das, Joo-Han Woo, and Byung-Joo Kim. 2024. "Atractylodes macrocephala Koidz Alleviates Symptoms in Zymosan-Induced Irritable Bowel Syndrome Mouse Model through TRPV1, NaV1.5, and NaV1.7 Channel Modulation" Nutrients 16, no. 11: 1683. https://doi.org/10.3390/nu16111683







