Prognostic Value of New Sarcopenia Screening Tool in the Elderly—SARC-GLOBAL
Abstract
:1. Introduction
2. Materials and Methods
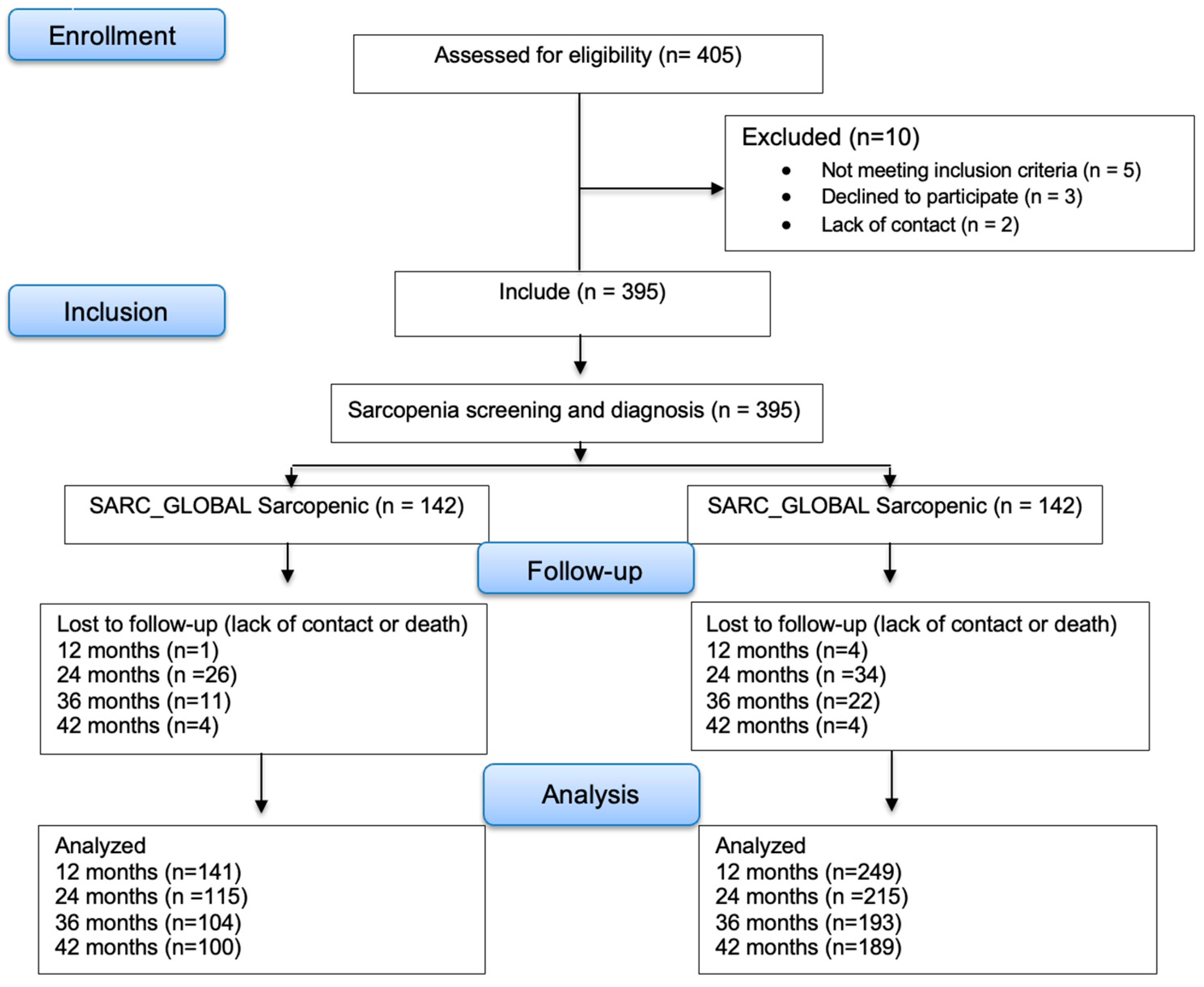
2.1. Study Design and Participants
2.2. Participant Information
2.3. Anthropometric Measurements
2.4. Sarcopenia Screening
2.5. Diagnosis of Sarcopenia
Muscle Mass, Strength, and Performance
2.6. Follow-Up for Adverse Outcomes
2.7. Statistical Analysis
3. Results
3.1. Study Population Characteristics
3.2. Predictive Performance of the of SARC-GLOBAL, SARC-F, and SARC-CalF Sarcopenia Screening Tools for Clinical Outcomes According to Logistic Regression
3.3. Predictive Performance of the of SARC-GLOBAL, SARC-F, and SARC-CalF Sarcopenia Screening Tools for Clinical Outcomes according to Poisson Regression
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Azzolino, D.; Arosio, B.; Marzetti, E.; Calvani, R.; Cesari, M. Nutritional Status as a Mediator of Fatigue and Its Underlying Mechanisms in Older People. Nutrients 2020, 12, 444. [Google Scholar] [CrossRef] [PubMed]
- Silva Neto, L.S.; Karnikowiski, M.G.O.; Tavares, A.B.; Lima, R.M. Associação entre sarcopenia, obesidade sarcopênica e força muscular com variáveis relacionadas de qualidade de vida em idosas. Braz. J. Phys. Ther. 2012, 16, 360–367. [Google Scholar] [CrossRef]
- St-Onge, M.-P.; Gallagher, D. Body composition changes with aging: The cause or the result of alterations in metabolic rate and macronutrient oxidation? Nutrition 2010, 26, 152–155. [Google Scholar] [CrossRef] [PubMed]
- JafariNasabian, P.; Inglis, J.E.; Reilly, W.; Kelly, O.J.; Ilich, J.Z. Aging human body: Changes in bone, muscle and body fat with consequent changes in nutrient intake. J. Endocrinol. 2017, 234, R37–R51. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, I.H. Summary comments. Am. J. Clin. Nutr. 1989, 50, 1231–1233. [Google Scholar] [CrossRef]
- Cao, L.; Morley, J.E. Sarcopenia Is Recognized as an Independent Condition by an International Classification of Disease, Tenth Revision, Clinical Modification (ICD-10-CM) Code. J. Am. Med. Dir. Assoc. 2016, 17, 675–677. [Google Scholar] [CrossRef] [PubMed]
- Shafiee, G.; Keshtkar, A.; Soltani, A.; Ahadi, Z.; Larijani, B.; Heshmat, R. Prevalence of sarcopenia in the world: A systematic review and meta- analysis of general population studies. J. Diabetes Metab. Disord. 2017, 16, 21. [Google Scholar] [CrossRef] [PubMed]
- Chang, K.-V.; Hsu, T.-H.; Wu, W.-T.; Huang, K.-C.; Han, D.-S. Association Between Sarcopenia and Cognitive Impairment: A Systematic Review and Meta-Analysis. J. Am. Med. Dir. Assoc. 2016, 17, 1164.e7–1164.e15. [Google Scholar] [CrossRef] [PubMed]
- Chang, K.-V.; Hsu, T.-H.; Wu, W.-T.; Huang, K.-C.; Han, D.-S. Is sarcopenia associated with depression? A systematic review and meta-analysis of observational studies. Age Ageing 2017, 46, 738–746. [Google Scholar] [CrossRef]
- Yeung, S.S.Y.; Reijnierse, E.M.; Pham, V.K.; Trappenburg, M.C.; Lim, W.K.; Meskers, C.G.M.; Maier, A.B. Sarcopenia and its association with falls and fractures in older adults: A systematic review and meta-analysis. J. Cachexia Sarcopenia Muscle 2019, 10, 485–500. [Google Scholar] [CrossRef]
- Beaudart, C.; Zaaria, M.; Pasleau, F.; Reginster, J.-Y.; Bruyère, O. Health Outcomes of Sarcopenia: A Systematic Review and Meta-Analysis. PLoS ONE 2017, 12, e0169548. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jentoft, A.J.; Sayer, A.A. Sarcopenia. Lancet 2019, 393, 2636–2646. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef]
- Di Lenarda, L.; Buoite Stella, A.; Ratti, C.; Ruggiero, L.; Bernard, M.; Cavarzerani, L.P.; Canton, G.; Murena, L. Assessing Muscle Mass in the Orthopedic Clinical Setting: Application of the Ultrasound Sarcopenia Index in Elderly Subjects with a Recent Femoral Fracture. Nutrients 2024, 16, 711. [Google Scholar] [CrossRef] [PubMed]
- Malmstrom, T.K.; Morley, J.E. SARC-F: A simple questionnaire to rapidly diagnose sarcopenia. J. Am. Med. Dir. Assoc. 2013, 14, 531–532. [Google Scholar] [CrossRef] [PubMed]
- Barbosa-Silva, T.G.; Menezes, A.M.B.; Bielemann, R.M.; Malmstrom, T.K.; Gonzalez, M.C.; Grupo de Estudos em Composição Corporal e Nutrição (COCONUT). Enhancing SARC-F: Improving Sarcopenia Screening in the Clinical Practice. J. Am. Med. Dir. Assoc. 2016, 17, 1136–1141. [Google Scholar] [CrossRef] [PubMed]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, N.C.L. Development of a new sarcopenia screening tool in the elderly. In Mestrado em Ciências em Gastroenterologia; Universidade de São Paulo: São Paulo, Brazil, 2023. [Google Scholar]
- Deschenes, M.R. Effects of aging on muscle fibre type and size. Sports Med. 2004, 34, 809–824. [Google Scholar] [CrossRef]
- Araújo, A.H.D.; Patrício, A.C.F.D.A.; Ferreira, M.A.M.; Rodrigues, B.F.L.; Santos, T.D.D.; Rodrigues, T.D.D.B.; Silva, R.A.R.D. Falls in institutionalized older adults: Risks, consequences and antecedents. Rev. Bras. Enferm. 2017, 70, 719–725. [Google Scholar] [CrossRef]
- English, K.L.; Paddon-Jones, D. Protecting muscle mass and function in older adults during bed rest. Curr. Opin. Clin. Nutr. Metab. Care 2010, 13, 34–39. [Google Scholar] [CrossRef]
- Bijlsma, A.Y.; Pasma, J.H.; Lambers, D.; Stijntjes, M.; Blauw, G.J.; Meskers, C.G.M.; Maier, A.B. Muscle strength rather than muscle mass is associated with standing balance in elderly outpatients. J. Am. Med. Dir. Assoc. 2013, 14, 493–498. [Google Scholar] [CrossRef] [PubMed]
- Liguori, I.; Russo, G.; Aran, L.; Bulli, G.; Curcio, F.; Della-Morte, D.; Gargiulo, G.; Testa, G.; Cacciatore, F.; Bonaduce, D.; et al. Sarcopenia: Assessment of disease burden and strategies to improve outcomes. Clin. Interv. Aging 2018, 13, 913–927. [Google Scholar] [CrossRef]
- Ogawa, S.; Yakabe, M.; Akishita, M. Age-related sarcopenia and its pathophysiological bases. Inflamm. Regen. 2016, 36, 17. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, A.D.B.; Filho, R.R.D.S.; Rodrigues, L.P.; de Souza, G.V.; Noll, M.; Silveira, E.A. Association between sarcopenia and hospitalization in community-dwelling older adults, using the SARC-F and SARC-CalF methods: A systematic review protocol. Phys. Ther. Rev. 2021, 26, 391–397. [Google Scholar] [CrossRef]
- Schoevaerdts, D.; Sibille, F.-X.; Gavazzi, G. Infections in the older population: What do we know? Aging Clin. Exp. Res. 2021, 33, 689–701. [Google Scholar] [CrossRef]
- Yang, M.; Liu, Y.; Zuo, Y.; Tang, H. Sarcopenia for predicting falls and hospitalization in community-dwelling older adults: EWGSOP versus EWGSOP2. Sci. Rep. 2019, 9, 17636. [Google Scholar] [CrossRef] [PubMed]
- Schene, M.R.; Willems, H.C.; Driessen, J.H.M.; Vranken, L.; Heersprink, F.O.; Janzing, H.M.J.; van der Velde, R.Y.; van den Bergh, J.P.; Wyers, C.E. Physical performance and sarcopenia assessment in patients with a recent fracture visiting the Fracture Liaison Service. Osteoporos. Int. 2024, 35, 851–862. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Data Finder—Health, United States. 2022. Available online: https://www.cdc.gov/nchs/hus/data-finder.htm (accessed on 30 May 2023).
- Fu, A.Z.; Liu, G.G.; Christensen, D.B. Inappropriate medication use and health outcomes in the elderly. J. Am. Geriatr. Soc. 2004, 52, 1934–1939. [Google Scholar] [CrossRef] [PubMed]
- Bhaskaran, K.; dos-Santos-Silva, I.; Leon, D.A.; Douglas, I.J.; Smeeth, L. Association of BMI with overall and cause-specific mortality: A population-based cohort study of 3·6 million adults in the UK. Lancet Diabetes Endocrinol. 2018, 6, 944–953. [Google Scholar] [CrossRef]
- Martone, A.M.; Bianchi, L.; Abete, P.; Bellelli, G.; Bo, M.; Cherubini, A.; Corica, F.; Di Bari, M.; Maggio, M.; Manca, G.M.; et al. The incidence of sarcopenia among hospitalized older patients: Results from the Glisten study. J. Cachexia Sarcopenia Muscle 2017, 8, 907–914. [Google Scholar] [CrossRef]
- Ishida, Y.; Maeda, K.; Ueshima, J.; Shimizu, A.; Nonogaki, T.; Kato, R.; Matsuyama, R.; Yamanaka, Y.; Mori, N. The SARC-F Score on Admission Predicts Falls during Hospitalization in Older Adults. J. Nutr. Health Aging 2021, 25, 399–404. [Google Scholar] [CrossRef] [PubMed]
- Nozoe, M.; Kubo, H.; Kanai, M.; Yamamoto, M. Relationships between Pre-Stroke SARC-F Scores, Disability, and Risk of Malnutrition and Functional Outcomes after Stroke—A Prospective Cohort Study. Nutrients 2021, 13, 3586. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Jiang, J.; Zeng, Y.; Tang, H. Sarcopenia for predicting mortality among elderly nursing home residents: SARC-F versus SARC-CalF. Medicine 2019, 98, e14546. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, F.W.; Burgel, C.F.; Brito, J.E.; Baumgardt, E.; de Araújo, B.E.; Silva, F.M. SARC-CalF tool has no significant prognostic value in hospitalized patients: A prospective cohort study. Nutr. Clin. Pract. 2021, 36, 1072–1079. [Google Scholar] [CrossRef] [PubMed]
| Variables | Total (n = 395) | SARC-GLOBAL Sarcopenic | SARC-GLOBAL Non-Sarcopenic | p-Value 1 |
|---|---|---|---|---|
| Sex | ||||
| Female, n (%) | 320 (81) | 107 (75.3) | 214 (84.6) | |
| Male, n (%) | 75 (19) | 35 (24.7) | 39 (15.4) | 0.031 2 |
| Age, years | 70.7 ± 7.5 | 74.6 ± 8.2 | 68.5 ± 6.1 | <0.001 3 |
| Comorbidities 4, n (%) | 57 (14.4) | 35 (14.7) | 34 (24.6) | <0.001 5 |
| Medications 6, n (%) | 199 (50.4) | 102 (40.3) | 97 (68.3) | <0.001 5 |
| Anthropometric data | ||||
| Weight, kg | 67.8 ± 14.2 | 65.4 ± 15.3 | 69.2 ± 13.5 | 0.013 7 |
| BMI 8, kg/m2 | 27.6 ± 5.3 | 26.9 ± 5.9 | 28.0 ± 4.9 | 0.070 3 |
| Arm circumference, cm | 32.0 ± 4.5 | 30.8 ± 4.9 | 32.9 ± 4.1 | <0.001 3 |
| Calf circumference, cm | 35.9 ± 3.6 | 34.9 ± 4.0 | 36.5 ± 3.1 | <0.001 3 |
| ASMI 9, kg/m2 | 6.6 ± 0.2 | 6.4 ± 1.7 | 6.7 ± 1.6 | 0.003 7 |
| HGS 10 | 17.1 ± 7.2 | 12.9 ± 5.0 | 19.5 ± 7.1 | <0.001 3 |
| EWGSOP2 11 | ||||
| Sarcopenic, n (%) | 85 (21.5) | 22 (8.7) | 63 (44.4) | 0.736 2 |
| Non-sarcopenic, n (%) | 310 (78.5) | 231 (91.3) | 79 (55.6) | |
| SARC-GLOBAL, n (%) | NA 12 | 142 (35.9) | 253 (64.1) | <0.001 5 0.001 2 |
| Physical practice, IPAC 13 | ||||
| Sedentary, n (%) | 53 (13.7) | 24 (9.6) | 29 (20.9) | |
| Irregularly active a, n (%) | 121 (3.2) | 73 (29.3) | 48 (34.5) | |
| Irregularly active b, n (%) | 146 (37.6) | 98 (39.4) | 48 (34.5) | |
| Active, n (%) | 58 (15.0) | 44 (17.7) | 14 (10.1) | |
| Very active, n (%) | 10 (2.6) | 10 (4.0) | 0 (0.0) |
| Follow-Up Time (Months) | SARC-GLOBAL Sarcopenic | SARC-GLOBAL Non-Sarcopenic | ||||||
|---|---|---|---|---|---|---|---|---|
| 12 | 24 | 36 | 42 | 12 | 24 | 36 | 42 | |
| Clinical Outcomes | ||||||||
| Falls | 34 (24.1) | 47 (40.9) | 47 (45.2) | 49 (49.0) | 33 (12.3) | 46 (21.4) | 49 (25.4) | 53 (28.0) |
| Factures | 3 (2.1) | 4 (3.6) | 5 (5.2) | 7 (7.9) | 0 (0.0) | 8 (3.8) | 10 (5.4) | 13 (7.4) |
| Infections | 25 (17.7) | 35 (30.4) | 38 (35.9) | 42 (42.0) | 44 (17.7) | 55 (25.0) | 60 (30.2) | 65 (33.9) |
| Hospitalizations | 22 (15.6) | 32 (28.1) | 37 (35.6) | 40 (40.4) | 24 (9.6) | 38 (17.8) | 42 (21.9) | 44 (23.8) |
| Death | 3 (2.1) | 6 (5.1) | 8 (7.8) | 9 (9.5) | 4 (1.6) | 1 (0.5) | 2 (1.1) | 2 (1.2) |
| Total | 141 | 115 | 104 | 100 | 249 | 215 | 193 | 189 |
| Follow-Up (Months) | SARC-GLOBAL | EWGSOP2 1 | SARC-F | SARC-CalF | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | OR (CI 95%) | p-Value 2 | β | OR (CI 95%) | p-Value 2 | β | OR (CI 95%) | p-Value 2 | β | OR (CI 95%) | p-Value 2 | |
| Falls | ||||||||||||
| 12 | 0.73 | 2.07 (1.22–3.54) | 0.007 | −0.06 | 0.94 (0.49–1.79) | 0.845 | 1.48 | 4.40 (2.45–7.88) | <0.001 | −0.02 | 0.98 (0.46–2.13) | 0.967 |
| 24 | 0.93 | 2.54 (1.55–4.16) | <0.001 | 0.02 | 1.02 (0.57–1.84) | 0.935 | 1.16 | 0.98 (0.48–2.01) | 0.966 | −0.02 | 0.98 (0.48–2.01) | 0.966 |
| 36 | 0.97 | 2.64 (1.58–4.38) | <0.001 | 0.00 | 1.00 (0.55–1.81) | 0.990 | 1.10 | 3.02 (1.68–5.41) | <0.001 | −0.03 | 0.97 (0.47–2.01) | 0.937 |
| 42 | 0.69 | 1.99 (1.26–3.15) | 0.003 | −0.08 | 0.93 (0.53–1.61) | 0.791 | 1.09 | 2.98 (1.74–5.09) | <0.001 | −0.20 | 0.82 (0.41–1.63) | 0.570 |
| Fractures | ||||||||||||
| 12 | 18.73 | >1000 (0-inf) | 0.995 | 0.59 | 1.80 (0.16–20.13) | 0.632 | 0.83 | 2.30 (0.21–25.77) | 0.498 | 2.58 | 13.18 (1.17–147.9) | 0.037 |
| 24 | −0.07 | 0.93 (0.27–3.16) | 0.908 | −1.13 | 0.32 (0.04–2.54) | 0.282 | −0.95 | 0.39 (0.05–3.04) | 0.366 | 0.27 | 1.31 (0.28–6.18) | 0.735 |
| 36 | 0.06 | 1.06 (0.34–3.25) | 0.923 | −0.55 | 0.58 (0.13–2.64) | 0.477 | −1.19 | 0.30 (0.04–2.37) | 0.255 | 0.56 | 1.75 (0.47–6.58) | 0.407 |
| 42 | −0.04 | 0.96 (0.37–2.46) | 0.928 | −0.94 | 0.39 (0.09–1.72) | 0.214 | −0.71 | 0.49 (0.11–2.17) | 0.350 | 0.51 | 1.66 (0.53–5.18) | 0.380 |
| Infections | ||||||||||||
| 12 | 0.00 | 1.00 (0.58–1.73) | 0.988 | 0.10 | 1.10 (0.59–2.05) | 0.757 | −0.05 | 0.95 (0.48–1.89) | 0.894 | 0.09 | 1.10 (0.52–2.30) | 0.809 |
| 24 | 0.27 | 1.31 (0.80–2.17) | 0.287 | −1.13 | 0.32 (0.04–2.54) | 0.282 | 0.13 | 1.14 (0.62–2.10) | 0.670 | 0.40 | 1.49 (0.76–2.93) | 0.248 |
| 36 | 0.28 | 1.33 (0.80–2.19) | 0.269 | −0.55 | 0.58 (0.13–2.64) | 0.477 | 0.05 | 1.06 (0.57–1.94) | 0.862 | 0.25 | 1.28 (0.64–2.54) | 0.481 |
| 42 | 0.19 | 1.21 (0.77–1.92) | 0.405 | 0.00 | 1.00 (0.58–1.71) | 0.994 | 0.07 | 1.07 (0.60–1.89) | 0.821 | 0.07 | 1.07 (0.56–2.04) | 0.831 |
| Hospitalizations | ||||||||||||
| 12 | 0.55 | 1.73 (0.93–3.22) | 0.082 | 0.27 | 0.13 (0.09–0.18) | 0.454 | 0.81 | 2.25 (1.13–4.49) | 0.021 | 0.51 | 1.66 (0.75–3.67) | 0.212 |
| 24 | 0.59 | 1.81 (1.06–3.10) | 0.031 | 0.29 | 1.34 (0.72–2.48) | 0.353 | 0.98 | 2.65 (1.44–4.89) | 0.002 | 0.51 | 1.67 (0.82–3.40) | 0.157 |
| 36 | 0.60 | 1.82 (1.07–3.10) | 0.027 | 0.13 | 1.14 (0.62–2.10) | 0.666 | 0.81 | 2.25 (1.23–4.13) | 0.009 | 0.55 | 1.73 (0.86–3.46) | 0.121 |
| 42 | 0.62 | 1.86 (1.14–3.04) | 0.013 | 0.25 | 1.29 (0.73–2.26) | 0.382 | 0.97 | 2.65 (1.51- 4.64) | 0.001 | 0.66 | 1.94 (1.03–3.66) | 0.041 |
| Follow-Up (Months) | SARC-GLOBAL | EWGSOP2 1 | SARC-F | SARC-CalF | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | RR (CI 95%) | p-Value 2 | β | RR (CI 95%) | p-Value 2 | β | RR (CI 95%) | p-Value 2 | β | RR (CI 95%) | p-Value 2 | |
| Fall | ||||||||||||
| 12 | 0.61 | 1.84 (1.23–2.76) | 0.003 | −0.38 | 0.68 (0.39–1.18) | 0.173 | 1.39 | 4.02 (2.68–6.03) | <0.001 | −0.40 | 0.67 (0.34–1.34) | 0.259 |
| 24 | 0.70 | 2.01 (1.44–2.81) | <0.001 | −0.17 | 0.84 (0.55–1.29) | 0.434 | 0.87 | 2.38 (1.68–3.37) | <0.001 | −0.24 | 0.78 (0.46–1.34) | 0.376 |
| 36 | 0.64 | 1.90 (1.35–2.66) | <0.001 | −0.06 | 0.94 (0.62–1.42) | 0.767 | 0.81 | 2.26 (1.59–3.21) | <0.001 | −0.25 | 0.78 (0.46–1.33) | 0.363 |
| 42 | 0.57 | 1.76 (1.32–2.36) | <0.001 | 0.18 | 1.19 (0.80–1.78) | 0.386 | 0.97 | 2.65 (1.86–3.78) | <0.001 | −0.01 | 0.99 (0.59–1.65) | 0.966 |
| Fractures | ||||||||||||
| 12 | 18.74 | >1000 (0-inf) | 0.994 | 0.18 | 1.20 (0.12–11.50) | 0.877 | 1.52 | 4.57 (0.64–32.45) | 0.129 | 1.85 | 6.36 (0.90–45.14) | 0.064 |
| 24 | 0.34 | 1.40 (0.49–4.03) | 0.534 | −1.27 | 0.28 (0.04–2.15) | 0.221 | −0.32 | 0.73 (0.16–3.24) | 0.674 | 0.07 | 1.08 (0.24–4.81) | 0.922 |
| 36 | 0.37 | 1.44 (0.50–4.16) | 0.496 | −0.56 | 0.57 (0.13–2.56) | 0.465 | −16.54 | 0.00 (0.00–inf) | 0.990 | 0.04 | 1.04 (0.23–4.64) | 0.960 |
| 42 | 0.34 | 1.40 (0.64–3.08) | 0.404 | −0.82 | 0.44 (0.10–1.92) | 0.275 | −1.41 | 0.24 (0.03–1.84) | 0.171 | 0.24 | 1.27 (0.37–4.40) | 0.702 |
| Infections | ||||||||||||
| 12 | 0.36 | 1.43 (0.95–2.14) | 0.087 | 0.52 | 1.68 (1.09–2.60) | 0.019 | −0.06 | 0.94 (0.55–1.61) | 0.815 | 0.34 | 1.40 (0.83–2.37) | 0.206 |
| 24 | 0.64 | 1.90 (1.31–2.76) | <0.001 | 0.44 | 1.55 (1.03–2.32) | 0.036 | 0.01 | 1.01 (0.63–1.63) | 0.951 | 0.47 | 1.60 (1.00–2.55) | 0.049 |
| 36 | 0.67 | 1.95 (1.34–2.85) | <0.001 | 0,59 | 1.81 (1.21–2.69) | 0.004 | 0.16 | 1.18 (0.75–1.86) | 0.480 | 0.53 | 1.70 (1.07–2.70) | 0.024 |
| 42 | 0.53 | 1.70 (1.25–2.31) | <0.001 | 0.53 | 1.71 (1.16–2.50) | 0.006 | 0.24 | 1.27 (0.83–1.94) | 0.265 | 0.42 | 1.52 (0.96–2.39) | 0.072 |
| Hospitalizations | ||||||||||||
| 12 | 0.77 | 2.15 (1.35–3.43) | 0.001 | 0.48 | 1.61 (0.97–2.66) | 0.063 | 0.65 | 1.92 (1.15–3.20) | 0.012 | 0.84 | 2.32 (1.37–3.93) | 0.002 |
| 24 | 0.73 | 2.08 (1.39–3.12) | <0.001 | 0.32 | 1.38 (0.88–2.17) | 0.160 | 0.84 | 2.32 (1.52–3.55) | <0.001 | 0.79 | 2.19 (1.38–3.48) | <0.001 |
| 36 | 0.58 | 1.79 (1.17–2.72) | 0.007 | 0.02 | 1.02 (0.62–1.68) | 0.936 | 0.91 | 2.49 (1.61–3.84) | <0.001 | 0.55 | 1.74 (1.04–2.89) | 0.034 |
| 42 | 0.67 | 1.95 (1.39–2.75) | <0.001 | 0.05 | 1.05 (0.64–1.73) | 0.840 | 0.86 | 2.36 (1.53–3.65) | <0.001 | 0.58 | 1.78 (1.07–2.96) | 0.026 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vicedomini, A.C.C.; Waitzberg, D.L.; Lopes, N.C.; Magalhães, N.; Prudêncio, A.P.A.; Jacob Filho, W.; Busse, A.L.; Ferdinando, D.; Alves, T.P.; Pereira, R.M.R.; et al. Prognostic Value of New Sarcopenia Screening Tool in the Elderly—SARC-GLOBAL. Nutrients 2024, 16, 1717. https://doi.org/10.3390/nu16111717
Vicedomini ACC, Waitzberg DL, Lopes NC, Magalhães N, Prudêncio APA, Jacob Filho W, Busse AL, Ferdinando D, Alves TP, Pereira RMR, et al. Prognostic Value of New Sarcopenia Screening Tool in the Elderly—SARC-GLOBAL. Nutrients. 2024; 16(11):1717. https://doi.org/10.3390/nu16111717
Chicago/Turabian StyleVicedomini, Ana Carolina Costa, Dan L. Waitzberg, Natalia Correia Lopes, Natalia Magalhães, Ana Paula A. Prudêncio, Wilson Jacob Filho, Alexandre Leopold Busse, Douglas Ferdinando, Tatiana Pereira Alves, Rosa Maria Rodrigues Pereira, and et al. 2024. "Prognostic Value of New Sarcopenia Screening Tool in the Elderly—SARC-GLOBAL" Nutrients 16, no. 11: 1717. https://doi.org/10.3390/nu16111717





