Typical Guidelines for Well-Balanced Diet and Science Communication in Japan and Worldwide
Abstract
1. Introduction
2. Methods
3. Dietary Reference Intake
3.1. Overview
3.2. DRIs from Japan and Other Countries
3.3. Brief Summary
4. Food-Based Guidelines
4.1. Overview
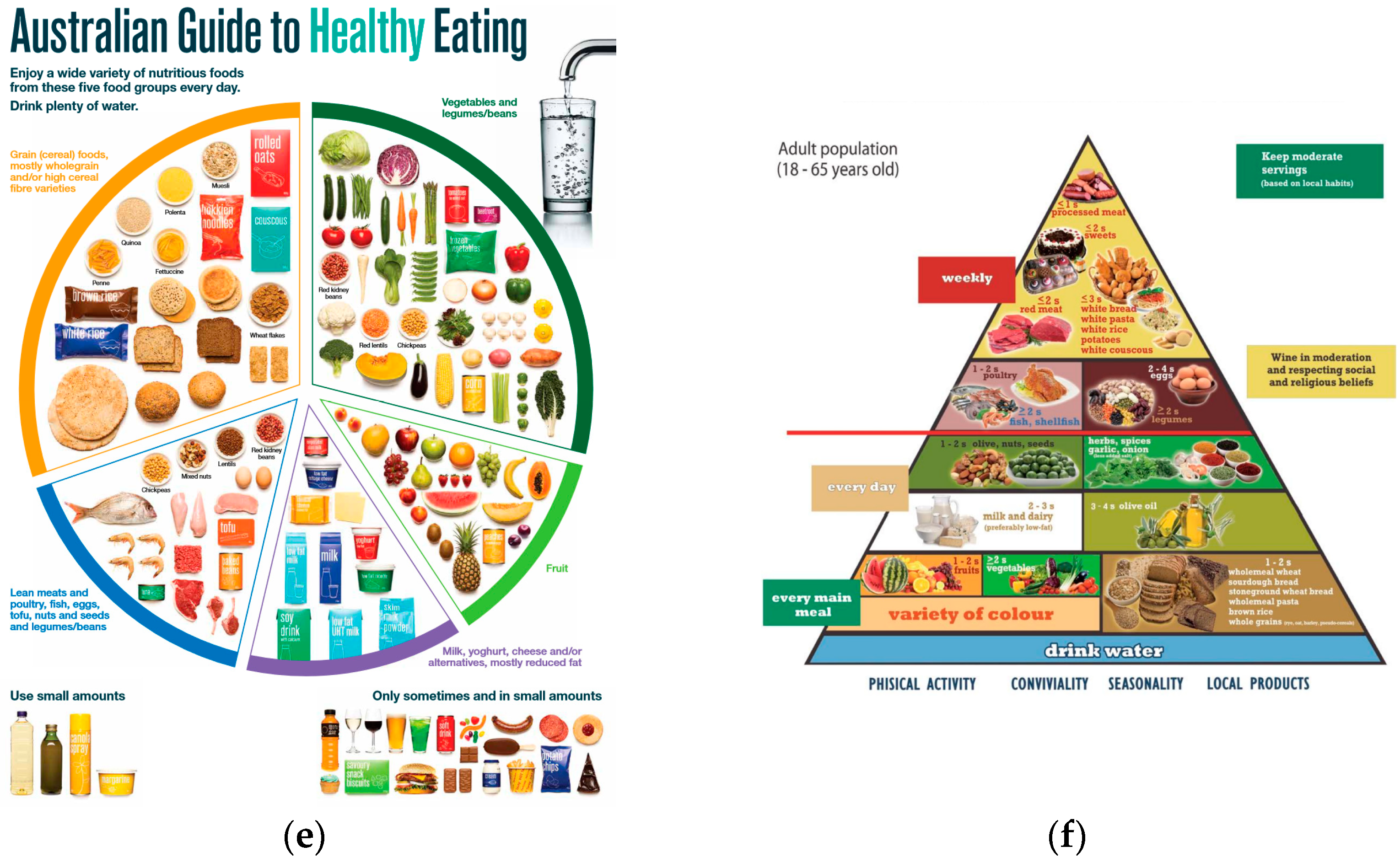
4.2. Food Balance Guides from Japan and Other Countries
4.3. DASH Diet
4.4. The Mediterranean Diet
4.5. Nordic Diet
4.6. Japanese Traditional Diet (Washoku)
4.7. The EAT-Lancet Guideline
4.8. Brief Summary
5. Recent Notable Consumer Communications
6. Conclusions and Further Perspective
7. Limitation
Author Contributions
Funding
Conflicts of Interest
References
- Ministry of Health Labour and Welfare Dietary Reference Intakes for Japanese (2020). Available online: https://www.mhlw.go.jp/content/001151422.pdf (accessed on 20 June 2024).
- The Ministry of Agriculture Forestry and Fishers. The Ministry of Health Labor and Welfare Japanese Food Guide Spinning Top. Available online: https://www.maff.go.jp/j/balance_guide/b_use/pdf/eng_reiari.pdf (accessed on 29 March 2024).
- Maruyama, C.; Shijo, Y.; Kameyama, N.; Umezawa, A.; Sato, A.; Nishitani, A.; Ayaori, M.; Ikewaki, K.; Waki, M.; Teramoto, T. Effects of Nutrition Education Program for the Japan Diet on Serum Ldl-Cholesterol Concentration in Patients with Dyslipidemia: A Randomized Controlled Trial. J. Atheroscler. Thromb. 2021, 28, 1035–1051. [Google Scholar] [CrossRef]
- Abarca-Gómez, L.; Abdeen, Z.A.; Hamid, Z.A.; Abu-Rmeileh, N.M.; Acosta-Cazares, B.; Acuin, C.; Adams, R.J.; Aekplakorn, W.; Afsana, K.; Aguilar-Salinas, C.A.; et al. Worldwide Trends in Body-Mass Index, Underweight, Overweight, and Obesity from 1975 to 2016: A Pooled Analysis of 2416 Population-Based Measurement Studies in 128·9 Million Children, Adolescents, and Adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, N.; Nishi, N.; Noda, H.; Noda, M. Trends in Prevalence and Management of Diabetes and Related Vascular Risks in Japanese Adults: Japan National Health and Nutrition Surveys 2003–2012. Diabetes Res. Clin. Pract. 2017, 127, 115–122. [Google Scholar] [CrossRef]
- Ogawa, W.; Gupta, P. The Humanistic and Societal Impact of Obesity in Japan: A Targeted Literature Review. Endocr. J. 2024, 71, 273–284. [Google Scholar] [CrossRef]
- Iizuka, K.; Sato, H.; Kobae, K.; Yanagi, K.; Yamada, Y.; Ushiroda, C.; Hirano, K.; Ichimaru, S.; Seino, Y.; Ito, A.; et al. Young Japanese Underweight Women with “Cinderella Weight” Are Prone to Malnutrition, Including Vitamin Deficiencies. Nutrients 2023, 15, 2216. [Google Scholar] [CrossRef] [PubMed]
- Powell, J.; Pring, T. The Impact of Social Media Influencers on Health Outcomes: Systematic Review. Soc. Sci. Med. 2024, 340, 116472. [Google Scholar] [CrossRef] [PubMed]
- The National Nutrition Survey, Japan: NNS-J. Available online: https://www.mhlw.go.jp/content/000711006.pdf (accessed on 18 June 2024).
- World Health Statistics 2022: Monitoring Health for the SDGs, Sustainable Development Goals; World Health Organization: Geneva, Switzerland, 2022.
- Dietary Reference Intakes for Energy; National Academies Press: Washington, DC, USA, 2023; ISBN 9780309697231.
- EFSA (European Food Safety Authority). Dietary Reference Values for Nutrients Summary Report. EFSA Support. Publ. 2017, 14, e15121E. [Google Scholar] [CrossRef]
- Maitin-Shepard, M.; Flaxman, M. Use of Meta-Analyses in Nutrition Research and Policy: Best Practices of Conducting Meta-Analysis: Proceedings of a Workshop in Brief; National Academies Press: Washington, DC, USA, 2024; ISBN 9780309715393. [Google Scholar]
- US Department of Health and Human Services Dietary Reference Intake. Available online: https://nap.nationalacademies.org/topic/380/food-and-nutrition/nutrition-dietary-reference-intakes (accessed on 29 March 2024).
- The French Food Safety Agency Références Nutritionnelles. Available online: https://www.anses.fr/fr/content/avis-du-ces-nutrition-humaine (accessed on 29 March 2024).
- National Health and Medical Research Council (Australia); New Zealand Ministry of Health. Nutrient Reference Values. Available online: https://www.eatforhealth.gov.au/nutrient-reference-values (accessed on 29 March 2024).
- Ascherio, A.; Katan, M.B.; Zock, P.L.; Stampfer, M.J.; Willett, W.C. Trans Fatty Acids and Coronary Heart Disease. N. Engl. J. Med. 1999, 340, 1994–1998. [Google Scholar] [CrossRef] [PubMed]
- Ohkubo, T. The Importance of Dietary Choline Intake. Vitamins 2020, 94, 539–544. [Google Scholar] [CrossRef]
- Mills, C.A. Thiamine Overdosage and Toxicity. JAMA J. Am. Med. Assoc. 1941, 116, 2101. [Google Scholar] [CrossRef]
- McKenney, J.M. A Comparison of the Efficacy and Toxic Effects of Sustained- vs Immediate-Release Niacin in Hypercholesterolemic Patients. JAMA J. Am. Med. Assoc. 1994, 271, 672. [Google Scholar] [CrossRef]
- WHO. Guideline: Potassium Intake for Adults and Children. Available online: https://www.who.int/publications/i/item/9789241504829 (accessed on 22 January 2024).
- Vinceti, M.; Filippini, T.; Crippa, A.; de Sesmaisons, A.; Wise, L.A.; Orsini, N. Meta-Analysis of Potassium Intake and the Risk of Stroke. J. Am. Heart Assoc. 2016, 5, e004210. [Google Scholar] [CrossRef] [PubMed]
- Jéquier, E.; Constant, F. Water as an Essential Nutrient: The Physiological Basis of Hydration. Eur. J. Clin. Nutr. 2010, 64, 115–123. [Google Scholar] [CrossRef]
- Ohno, K.; Ohno, K.; Asami, M.; Matsui, Y. Is the Default of 2 Liters for Daily Per-Capita Water Consumption Appropriate? A Nationwide Survey Reveals Water Intake in Japan. J. Water Health 2018, 16, 562–573. [Google Scholar] [CrossRef] [PubMed]
- Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients); National Academies Press: Washington, DC, USA, 2005; ISBN 030908525X.
- French Agency for Food Safety. Apport en Protéines: Consommation, Qualité, Besoins et Recommandations. Available online: https://www.anses.fr/fr/system/files/NUT-Sy-Proteines.pdf (accessed on 20 June 2024).
- U.S. Department of Agriculture; U.S. Department of Health and Human Services. Dietary Guidelines for Americans 2020–2025 (9th Edition). 2020. Available online: https://www.dietaryguidelines.gov/sites/default/files/2020-12/Dietary_Guidelines_for_Americans_2020-2025.pdf (accessed on 29 March 2024).
- Public Health England. Government Dietary Recommendations: Government Recommendations for Energy and Nutrients for Males and Females Aged 1–18 Years and 19+ Years. 2016. Available online: https://assets.publishing.service.gov.uk/media/5a749fece5274a44083b82d8/government_dietary_recommendations.pdf (accessed on 26 June 2024).
- Koshida, E.; Okada, C.; Okada, E.; Matsumoto, M.; Takimoto, H. Comparison of Dietary Reference Intakes and Their Applications between Japan and Other Countries. Jpn. J. Nutr. Diet. 2021, 79, 14–26. [Google Scholar] [CrossRef]
- US Department of Agriculture. Food and Drug Administration My Plate. Available online: https://www.myplate.gov/ (accessed on 29 March 2024).
- D’Alessandro, A.; Lampignano, L.; De Pergola, G. Mediterranean Diet Pyramid: A Proposal for Italian People. A Systematic Review of Prospective Studies to Derive Serving Sizes. Nutrients 2019, 11, 1296. [Google Scholar] [CrossRef]
- National Health Services. The Eatwell Guide. Available online: https://www.nhs.uk/live-well/eat-well/food-guidelines-and-food-labels/the-eatwell-guide/#:~:text=Aim%20to%20eat%20at%20least,of%20vitamins%2C%20minerals%20and%20fibre (accessed on 29 March 2024).
- Hamad Al-Dkheel, M. Dietary Guidelines for Saudis: The Healthy Food Palm; Saudi Ministry of Health, General Directorate of Nutrition: Riyadh, Saudi Arabia, 2012. [Google Scholar]
- Halawani, R.; Jaceldo-Siegl, K.; Bahjri, K.; Heskey, C. Saudi Population’s Adherence to the Healthy Food Palm: A Cross-Sectional Study (P16-066-19). Curr. Dev. Nutr. 2019, 3, 3131618. [Google Scholar] [CrossRef]
- National Health and Medical Council. Australian Guide to Healthy Eating. Available online: https://www.eatforhealth.gov.au/guidelines/australian-guide-healthy-eating (accessed on 29 March 2024).
- McCarthy, W.J.; Rico, M.; Chandler, M.; Herman, D.R.; Chang, C.; Belin, T.R.; Love, S.; Ramirez, E.; Gelberg, L. Randomized Comparative Effectiveness Trial of 2 Federally Recommended Strategies to Reduce Excess Body Fat in Overweight, Low-Income Patients: Myplate.Gov vs Calorie Counting. Ann. Fam. Med. 2023, 21, 213–219. [Google Scholar] [CrossRef]
- Fuller, N.R.; Fong, M.; Gerofi, J.; Leung, L.; Leung, C.; Denyer, G.; Caterson, I.D. A Randomized Controlled Trial to Determine the Efficacy of a High Carbohydrate and High Protein Ready-to-Eat Food Product for Weight Loss. Clin. Obes. 2016, 6, 108–116. [Google Scholar] [CrossRef]
- Filippou, C.D.; Tsioufis, C.P.; Thomopoulos, C.G.; Mihas, C.C.; Dimitriadis, K.S.; Sotiropoulou, L.I.; Chrysochoou, C.A.; Nihoyannopoulos, P.I.; Tousoulis, D.M. Dietary Approaches to Stop Hypertension (DASH) Diet and Blood Pressure Reduction in Adults with and without Hypertension: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Adv. Nutr. 2020, 11, 1150–1160. [Google Scholar] [CrossRef]
- Theodoridis, X.; Chourdakis, M.; Chrysoula, L.; Chroni, V.; Tirodimos, I.; Dipla, K.; Gkaliagkousi, E.; Triantafyllou, A. Adherence to the DASH Diet and Risk of Hypertension: A Systematic Review and Meta-Analysis. Nutrients 2023, 15, 3261. [Google Scholar] [CrossRef] [PubMed]
- Ibsen, D.B.; Levitan, E.B.; Åkesson, A.; Gigante, B.; Wolk, A. The DASH Diet Is Associated with a Lower Risk of Heart Failure: A Cohort Study. Eur. J. Prev. Cardiol. 2022, 29, 1114–1123. [Google Scholar] [CrossRef]
- Lari, A.; Sohouli, M.H.; Fatahi, S.; Cerqueira, H.S.; Santos, H.O.; Pourrajab, B.; Rezaei, M.; Saneie, S.; Rahideh, S.T. The Effects of the Dietary Approaches to Stop Hypertension (DASH) Diet on Metabolic Risk Factors in Patients with Chronic Disease: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 2766–2778. [Google Scholar] [CrossRef]
- Soltani, S.; Shirani, F.; Chitsazi, M.J.; Salehi-Abargouei, A. The Effect of Dietary Approaches to Stop Hypertension (DASH) Diet on Weight and Body Composition in Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Clinical Trials. Obes. Rev. 2016, 17, 442–454. [Google Scholar] [CrossRef] [PubMed]
- Struijk, E.A.; Hagan, K.A.; Fung, T.T.; Hu, F.B.; Rodríguez-Artalejo, F.; Lopez-Garcia, E. Diet Quality and Risk of Frailty among Older Women in the Nurses’ Health Study. Am. J. Clin. Nutr. 2020, 111, 877–883. [Google Scholar] [CrossRef] [PubMed]
- Saharkhiz, M.; Khorasanchi, Z.; Karbasi, S.; Jafari-Nozad, A.M.; Naseri, M.; Mohammadifard, M.; Siami Ali Abad, M.; Ayadilord, M.; Ferns, G.A.; Bahrami, A. The Association between Adherence to a Dietary Approaches to Stop Hypertension (DASH) Diet and Neuro-Psychological Function in Young Women. BMC Nutr. 2021, 7, 21. [Google Scholar] [CrossRef]
- Kwan, M.W.M.; Wong, M.C.S.; Wang, H.H.X.; Liu, K.Q.L.; Lee, C.L.S.; Yan, B.P.Y.; Yu, C.M.; Griffiths, S.M. Compliance with the Dietary Approaches to Stop Hypertension (DASH) Diet: A Systematic Review. PLoS ONE 2013, 8, e78412. [Google Scholar] [CrossRef] [PubMed]
- Kawamura, A.; Kajiya, K.; Kishi, H.; Inagaki, J.; Mitarai, M.; Oda, H.; Umemoto, S.; Kobayashi, S. Effects of the DASH-JUMP Dietary Intervention in Japanese Participants with High-Normal Blood Pressure and Stage 1 Hypertension: An Open-Label Single-Arm Trial. Hypertens. Res. 2016, 39, 777–785. [Google Scholar] [CrossRef]
- Menotti, A.; Puddu, P.E. How the Seven Countries Study Contributed to the Definition and Development of the Mediterranean Diet Concept: A 50-Year Journey. Nutr. Metab. Cardiovasc. Dis. 2015, 25, 245–252. [Google Scholar] [CrossRef]
- Shai, I.; Schwarzfuchs, D.; Henkin, Y.; Shahar, D.R.; Witkow, S.; Greenberg, I.; Golan, R.; Fraser, D.; Bolotin, A.; Vardi, H.; et al. Weight Loss with a Low-Carbohydrate, Mediterranean, or Low-Fat Diet. N. Engl. J. Med. 2008, 359, 229–241. [Google Scholar] [CrossRef]
- Estruch, R.; Ngel Martínez-Gonzá Lez, M.A.; Corella, D.; Salas-Salvadó, J.; Ruiz-Gutié Rrez, V.; Covas, M.I.; Covas, I.; Fiol, M.; Gó Mez-Gracia, E.; López-Sabater, M.C.; et al. Effects of a Mediterranean-Style Diet on Cardiovascular Risk Factors: A Randomized Trial. Ann. Intern. Med. 2006, 145, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Marseglia, A.; Xu, W.; Fratiglioni, L.; Fabbri, C.; Berendsen, A.A.M.; Bialecka-Debek, A.; Jennings, A.; Gillings, R.; Meunier, N.; Caumon, E.; et al. Effect of the NU-AGE Diet on Cognitive Functioning in Older Adults: A Randomized Controlled Trial. Front. Physiol. 2018, 9, 349. [Google Scholar] [CrossRef] [PubMed]
- Delgado-Lista, J.; Alcala-Diaz, J.F.; Torres-Peña, J.D.; Quintana-Navarro, G.M.; Fuentes, F.; Garcia-Rios, A.; Ortiz-Morales, A.M.; Gonzalez-Requero, A.I.; Perez-Caballero, A.I.; Yubero-Serrano, E.M.; et al. Long-Term Secondary Prevention of Cardiovascular Disease with a Mediterranean Diet and a Low-Fat Diet (CORDIOPREV): A Randomised Controlled Trial. Lancet 2022, 399, 1876–1885. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Lapiscina, E.H.; Clavero, P.; Toledo, E.; Estruch, R.; Salas-Salvadó, J.; San Julián, B.; Sanchez-Tainta, A.; Ros, E.; Valls-Pedret, C.; Martinez-Gonzalez, M.Á. Mediterranean Diet Improves Cognition: The PREDIMED-NAVARRA Randomised Trial. J. Neurol. Neurosurg. Psychiatry 2013, 84, 1318–1325. [Google Scholar] [CrossRef]
- Salas-Salvadó, J.; Bulló, M.; Babio, N.; Martínez-González, M.Á.; Ibarrola-Jurado, N.; Basora, J.; Estruch, R.; Covas, M.I.; Corella, D.; Arós, F.; et al. Reduction in the Incidence of Type 2 Diabetes with the Mediterranean Diet: Results of the PREDIMED-Reus Nutrition Intervention Randomized Trial. Diabetes Care 2011, 34, 14–19. [Google Scholar] [CrossRef]
- Dernini, S.; Berry, E.M.; Serra-Majem, L.; La Vecchia, C.; Capone, R.; Medina, F.X.; Aranceta-Bartrina, J.; Belahsen, R.; Burlingame, B.; Calabrese, G.; et al. Med Diet 4.0: The Mediterranean Diet with Four Sustainable Benefits. Public Health Nutr. 2017, 20, 1322–1330. [Google Scholar] [CrossRef] [PubMed]
- Serra-Majem, L.; Tomaino, L.; Dernini, S.; Berry, E.M.; Lairon, D.; de la Cruz, J.N.; Bach-Faig, A.; Donini, L.M.; Medina, F.X.; Belahsen, R.; et al. Updating the Mediterranean Diet Pyramid towards Sustainability: Focus on Environmental Concerns. Int. J. Environ. Res. Public Health 2020, 17, 8758. [Google Scholar] [CrossRef]
- Krznarić, Ž.; Karas, I.; Ljubas Kelečić, D.; Vranešić Bender, D. The Mediterranean and Nordic Diet: A Review of Differences and Similarities of Two Sustainable, Health-Promoting Dietary Patterns. Front. Nutr. 2021, 8, 683678. [Google Scholar] [CrossRef] [PubMed]
- Kanerva, N.; Harald, K.; Männistö, S.; Kaartinen, N.E.; Maukonen, M.; Haukkala, A.; Jousilahti, P. Adherence to the Healthy Nordic Diet Is Associated with Weight Change during 7 Years of Follow-Up. Br. J. Nutr. 2018, 120, 101–110. [Google Scholar] [CrossRef]
- Kolehmainen, M.; Ulven, S.M.; Paananen, J.; De Mello, V.; Schwab, U.; Carlberg, C.; Myhrstad, M.; Pihlajamäki, J.; Dungner, E.; Sjöolin, E.; et al. Healthy Nordic Diet Downregulates the Expression of Genes Involved in Inflammation in Subcutaneous Adipose Tissue in Individuals with Features of the Metabolic Syndrome. Am. J. Clin. Nutr. 2015, 101, 228–239. [Google Scholar] [CrossRef]
- Poulsen, S.K.; Due, A.; Jordy, A.B.; Kiens, B.; Stark, K.D.; Stender, S.; Holst, C.; Astrup, A.; Larsen, T.M. Health Effect of the New Nordic Diet in Adults with Increased Waist Circumference: A 6-Mo Randomized Controlled Trial. Am. J. Clin. Nutr. 2014, 99, 35–45. [Google Scholar] [CrossRef]
- Hanbali, S.; Avgerinou, C. Association between Adherence to the Nordic Diet and Frailty in Older Adults: A Systematic Review of Observational Studies. Maturitas 2024, 182, 107923. [Google Scholar] [CrossRef] [PubMed]
- Sorensen, L.B.; Damsgaard, C.T.; Dalskov, S.M.; Petersen, R.A.; Egelund, N.; Dyssegaard, C.B.; Stark, K.D.; Andersen, R.; Tetens, I.; Astrup, A.; et al. Diet-Induced Changes in Iron and n-3 Fatty Acid Status and Associations with Cognitive Performance in 8–11-Year-Old Danish Children: Secondary Analyses of the Optimal Well-Being, Development and Health for Danish Children through a Healthy New Nordic Diet School Meal Study. Br. J. Nutr. 2015, 114, 1623–1637. [Google Scholar] [CrossRef] [PubMed]
- Sabet, J.A.; Ekman, M.S.; Sofia Lundvall, A.; Risérus, U.; Johansson, U.; Öström, Å.; Adamsson, V.; Cao, Y.; Msghina, M.; Brummer, R.J. Feasibility and Acceptability of a Healthy Nordic Diet Intervention for the Treatment of Depression: A Randomized Controlled Pilot Trial. Nutrients 2021, 13, 902. [Google Scholar] [CrossRef] [PubMed]
- Mithril, C.; Dragsted, L.O.; Meyer, C.; Blauert, E.; Holt, M.K.; Astrup, A. Guidelines for the New Nordic Diet. Public Health Nutr. 2012, 15, 1941–1947. [Google Scholar] [CrossRef]
- Nordic Council of Ministers Nordic Nutrition Recommendations. 2023. Available online: https://norden.diva-portal.org/smash/record.jsf?pid=diva2%3A1769986&dswid=8186 (accessed on 26 June 2024).
- Imai, T.; Miyamoto, K.; Sezaki, A.; Kawase, F.; Shirai, Y.; Abe, C.; Fukaya, A.; Kato, T.; Sanada, M.; Shimokata, H. Traditional Japanese Diet Score—Association with Obesity, Incidence of Ischemic Heart Disease, and Healthy Life Expectancy in a Global Comparative Study. J. Nutr. Health Aging 2019, 23, 717–724. [Google Scholar] [CrossRef]
- Imamoto, M.; Takada, T.; Sasaki, S.; Kato, K.; Onishi, Y. Salt Intake per Dish in the Japanese Diet: A Clue to Help Establish Dietary Goals at Home. J. Nutr. Sci. 2021, 10, e107. [Google Scholar] [CrossRef]
- Sakane, N.; Osaki, N.; Takase, H.; Suzuki, J.; Suzukamo, C.; Nirengi, S.; Suganuma, A.; Shimotoyodome, A. The Study of Metabolic Improvement by Nutritional Intervention Controlling Endogenous GIP (Mini Egg Study): A Randomized, Cross-over Study. Nutr. J. 2019, 18, 52. [Google Scholar] [CrossRef] [PubMed]
- Honma, T.; Kitano, Y.; Kijima, R.; Jibu, Y.; Kawakami, Y.; Tsuduki, T.; Nakagawa, K.; Miyazawa, T. Comparison of the Health Benefits of Different Eras of Japanese Foods: Lipid and Carbohydrate Metabolism Focused Research. Nippon Shokuhin Kagaku Kogaku Kaishi 2013, 60, 541–553. [Google Scholar] [CrossRef]
- Suthutvoravut, U.; Takahashi, K.; Murayama, H.; Tanaka, T.; Akishita, M.; Iijima, K. Association Between Traditional Japanese Diet Washoku and Sarcopenia in Community-Dwelling Older Adults: Findings from the Kashiwa Study. J. Nutr. Health Aging 2020, 24, 282–289. [Google Scholar] [CrossRef]
- Kobayashi, M.; Sasazuki, S.; Shimazu, T.; Sawada, N.; Yamaji, T.; Iwasaki, M.; Mizoue, T.; Tsugane, S. Association of Dietary Diversity with Total Mortality and Major Causes of Mortality in the Japanese Population: JPHC Study. Eur. J. Clin. Nutr. 2020, 74, 54–66. [Google Scholar] [CrossRef] [PubMed]
- Sugawara, S.; Kushida, M.; Iwagaki, Y.; Asano, M.; Yamamoto, K.; Tomata, Y.; Tsuji, I.; Tsuduki, T. The 1975 Type Japanese Diet Improves Lipid Metabolic Parameters in Younger Adults: A Randomized Controlled Trial. J. Oleo Sci. 2018, 67, 599–607. [Google Scholar] [CrossRef]
- Willett, W.; Rockström, J.; Loken, B.; Springmann, M.; Lang, T.; Vermeulen, S.; Garnett, T.; Tilman, D.; DeClerck, F.; Wood, A.; et al. Food in the Anthropocene: The EAT–Lancet Commission on Healthy Diets from Sustainable Food Systems. Lancet 2019, 393, 447–492. [Google Scholar] [CrossRef]
- Langmann, F.; Ibsen, D.B.; Tjønneland, A.; Olsen, A.; Overvad, K.; Dahm, C.C. Adherence to the EAT-Lancet Diet Is Associated with a Lower Risk of Type 2 Diabetes: The Danish Diet, Cancer and Health Cohort. Eur. J. Nutr. 2023, 62, 1493–1502. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Stubbendorff, A.; Olsson, K.; Ericson, U.; Niu, K.; Qi, L.; Borné, Y.; Sonestedt, E. Adherence to the EAT-Lancet Diet, Genetic Susceptibility, and Risk of Type 2 Diabetes in Swedish Adults. Metabolism 2023, 141, 155401. [Google Scholar] [CrossRef]
- Tonstad, S.; Butler, T.; Yan, R.; Fraser, G.E. Type of Vegetarian Diet, Body Weight, and Prevalence of Type 2 Diabetes. Diabetes Care 2009, 32, 791–796. [Google Scholar] [CrossRef] [PubMed]
- Berthy, F.; Brunin, J.; Allès, B.; Fezeu, L.K.; Touvier, M.; Hercberg, S.; Galan, P.; Pointereau, P.; Lairon, D.; Baudry, J.; et al. Association between Adherence to the EAT-Lancet Diet and Risk of Cancer and Cardiovascular Outcomes in the Prospective NutriNet-Sante Cohort. Am. J. Clin. Nutr. 2022, 116, 980–991. [Google Scholar] [CrossRef]
- Young, H.A. Adherence to the EAT–Lancet Diet: Unintended Consequences for the Brain? Nutrients 2022, 14, 4254. [Google Scholar] [CrossRef]
- Borthwick, F.; Edgar, D.; Eltholth, M.; McNeill, G.; Tulloch, A.I.T.; Grech, A.; Boylan, S.; Perkins Centre, C.; Tulloch, A.I.T.; Borthwick, F.; et al. How the EAT-Lancet Commission on Food in the Anthropocene Influenced Discourse and Research on Food Systems: A Systematic Review Covering the First 2 Years Post-Publication. Lancet Glob. Health 2023, 11, e1125–e1136. [Google Scholar]
- Hirvonen, K.; Bai, Y.; Headey, D.; Masters, W.A. Affordability of the EAT–Lancet Reference Diet: A Global Analysis. Lancet Glob. Health 2020, 8, e59–e66. [Google Scholar] [CrossRef]
- Tayyem, R.; Allehdan, S.S.; Al-Awwad, N.j.; Alatrash, R.M.; Mahfouz, I.A. Food Group Intake of Pregnant Jordanian Women Based on the Three Pregnancy Trimesters. Prev. Nutr. Food Sci. 2020, 25, 346–352. [Google Scholar] [CrossRef]
- Yukie, M.; Akira, K.; Hironori, Y. Study on Management Strategy of Olive Production and Business in Jappan. Jpn. J. Farm Manag. 2021, 58, 21–26. [Google Scholar] [CrossRef]
- High Price of Olive Oil Due to Poor Raw Material Crop; Spotlight for Blended Oils. The Nikkei Newspaper, 2 April 2024.
- Shahid, M.; Neal, B.; Jones, A. Uptake of Australia’s Health Star Rating System 2014–2019. Nutrients 2020, 12, 1791. [Google Scholar] [CrossRef] [PubMed]
- Jones, A.; Thow, A.M.; Ni Mhurchu, C.; Sacks, G.; Neal, B. The Performance and Potential of the Australasian Health Star Rating System: A Four-Year Review Using the RE-AIM Framework. Aust. N. Z. J. Public Health 2019, 43, 355–365. [Google Scholar] [CrossRef]
- Egnell, M.; Seconda, L.; Neal, B.; Mhurchu, C.N.; Rayner, M.; Jones, A.; Touvier, M.; Kesse-Guyot, E.; Hercberg, S.; Julia, C. Prospective Associations of the Original Food Standards Agency Nutrient Profiling System and Three Variants with Weight Gain, Overweight and Obesity Risk: Results from the French NutriNet-Santé Cohort. Br. J. Nutr. 2021, 125, 902–914. [Google Scholar] [CrossRef]
- Pan, X.-F.; Magliano, D.J.; Zheng, M.; Shahid, M.; Taylor, F.; Julia, C.; Ni Mhurchu, C.; Pan, A.; Shaw, J.E.; Neal, B.; et al. Seventeen-Year Associations between Diet Quality Defined by the Health Star Rating and Mortality in Australians: The Australian Diabetes, Obesity and Lifestyle Study (AusDiab). Curr. Dev. Nutr. 2020, 4, nzaa157. [Google Scholar] [CrossRef] [PubMed]
- Maganja, D.; Davies, T.; Sanavio, L.; Louie, J.C.Y.; Huffman, M.D.; Trieu, K.; Wu, J.H.Y. Current Food Labelling Practices in Online Supermarkets in Australia. Int. J. Behav. Nutr. Phys. Act. 2023, 20, 105. [Google Scholar] [CrossRef]
- Shobako, N.; Goto, C.; Nakagawa, T.; Yamato, T.; Kondo, S.; Nakamura, F.; Nakazeko, T.; Hirano, Y.; Honda, K. Hypotensive and HbA1c Reducing Effect of Novel Dietary Intervention Program “COMB Meal Program”: Two Randomized Clinical Trials. J. Funct Foods 2022, 98, 105279. [Google Scholar] [CrossRef]
- Nakazeko, T.; Shobako, N.; Shioya, N.; Iwama, Y.; Hirano, Y.; Fujii, S.; Nakamura, F.; Honda, K. Frailty-Preventing Effect of an Intervention Program Using a Novel Complete Nutritional “COMB-FP Meal”: A Pilot Randomized Control Trial. Nutrients 2023, 15, 4317. [Google Scholar] [CrossRef]
- Nakazeko, T.; Shobako, N.; Hirano, Y.; Nakamura, F.; Honda, K. Novel Dietary Intervention Program “COMB Meal Program” Approaching Health and Presenteeism: Two Pilot Studies. J. Funct. Foods 2022, 92, 105050. [Google Scholar] [CrossRef]
- Murayama, H.; Takagi, Y.; Tsuda, H.; Kato, Y. Applying Nudge to Public Health Policy: Practical Examples and Tips for Designing Nudge Interventions. Int. J. Environ. Res. Public Health 2023, 20, 3962. [Google Scholar] [CrossRef]
- Edmondson, E.K.; Roberto, C.A.; Gregory, E.F.; Mitra, N.; Virudachalam, S. Association of a Sweetened Beverage Tax With Soda Consumption in High School Students. JAMA Pediatr. 2021, 175, 1261–1268. [Google Scholar] [CrossRef]
- Teng, A.M.; Jones, A.C.; Mizdrak, A.; Signal, L.; Genç, M.; Wilson, N. Impact of Sugar-Sweetened Beverage Taxes on Purchases and Dietary Intake: Systematic Review and Meta-Analysis. Obes. Rev. 2019, 20, 1187–1204. [Google Scholar] [CrossRef]
- Chatelan, A.; Rouche, M.; Dzielska, A.; Fismen, A.S.; Kelly, C.; Pedroni, C.; Desbouys, L.; Castetbon, K. Sixteen-Year Trends in Adolescent Consumption of Sugar-Sweetened Soda in Six European Countries with a Soda Tax and Comparison Countries: A Repeated Cross-Sectional Survey Analysis. Public Health Nutr. 2023, 26, 519–530. [Google Scholar] [CrossRef]
- Wright, A.; Smith, K.E.; Hellowell, M. Policy Lessons from Health Taxes: A Systematic Review of Empirical Studies. BMC Public Health 2017, 17, 583. [Google Scholar] [CrossRef]
- Momin, S.R.; Wood, A.C. Sugar-Sweetened Beverages and Child Health: Implications for Policy. Curr. Nutr. Rep. 2018, 7, 286–293. [Google Scholar] [CrossRef]
- Niederdeppe, J.; Heley, K.; Barry, C.L. Inoculation and Narrative Strategies in Competitive Framing of Three Health Policy Issues. J. Commun. 2015, 65, 838–862. [Google Scholar] [CrossRef]
- Chavasit, V.; Photi, J.; Dunkum, P.; Krassanairawiwong, T.; Ditmetharoj, M.; Preecha, S.; Martinez, F. Evolution of Trans-Fatty Acid Consumption in Thailand and Strategies for Its Reduction. J. Clin. Hypertens. 2020, 22, 1347–1354. [Google Scholar] [CrossRef]
- Banker, M.; Miller, M.; Voichek, G.; Goor, D.; Makov, T. Prosocial Nudges and Visual Indicators Increase Social Distancing, but Authoritative Nudges Do Not. Proc. Natl. Acad. Sci. USA 2022, 119, e2116156119. [Google Scholar] [CrossRef]
- Vyth, E.L.; Steenhuis, I.H.M.; Vlot, J.A.; Wulp, A.; Hogenes, M.G.; Looije, D.H.; Brug, J.; Seidell, J.C. Actual Use of a Front-of-Pack Nutrition Logo in the Supermarket: Consumers Motives in Food Choice. Public Health Nutr. 2010, 13, 1882–1889. [Google Scholar] [CrossRef]
- Vyth, E.L.; Steenhuis, I.H.M.; Mallant, S.F.; Mol, Z.L.; Brug, J.; Temminghoff, M.; Feunekes, G.I.; Jansen, L.; Verhagen, H.; Seidell, J.C. A Front-of-Pack Nutrition Logo: A Quantitative and Qualitative Process Evaluation in the Netherlands. J. Health Commun. 2009, 14, 631–645. [Google Scholar] [CrossRef] [PubMed]
- Dai, H.; Saccardo, S.; Han, M.A.; Roh, L.; Raja, N.; Vangala, S.; Modi, H.; Pandya, S.; Sloyan, M.; Croymans, D.M. Behavioural Nudges Increase COVID-19 Vaccinations. Nature 2021, 597, 404–409. [Google Scholar] [CrossRef] [PubMed]
- Ainuson-Quampah, J.; Amuna, N.; Holdsworth, M.; Aryeetey, R. A Review of Food-Based Dietary Guidelines in Africa: Opportunities to Enhance the Healthiness and Environmental Sustainability of Population Diets. Agric. Nutr. Dev. 2022, 22, 19471–19495. [Google Scholar] [CrossRef]
- Petrikova, I.; Bhattacharjee, R.; Fraser, P.D. The ‘Nigerian Diet’ and Its Evolution: Review of the Existing Literature and Household Survey Data. Foods 2023, 12, 443. [Google Scholar] [CrossRef]



| Nutrients | Japan | U.S. | EU | UK | France * | Australia/New Zealand | |
|---|---|---|---|---|---|---|---|
| Energy | BMI | EER | AR | EAR | EER | EER | |
| Protein | 〇 | 〇 (+Amino Acids) | 〇 | 〇 | 〇 (+Amino Acids) | 〇 | |
| Fats | Total fats | 〇 | 〇 | 〇 | 〇 | 〇 | 〇 (Infants only) |
| SFA | 〇 | 〇 | 〇 **** | 〇 | 〇 | × ** | |
| Mono unsaturated fatty acids | × | × | × | 〇 | × | × | |
| Poly unsaturated fatty acids | × | × | × | 〇 | × | × | |
| n6 | 〇 | 〇 | × | × | × | 〇 (0–12 month) | |
| n3 | 〇 | 〇 | × | × | × | 〇 (0–12 month) | |
| Linoleic acid | × | 〇 | 〇 | 〇 | 〇 | 〇 (age 1 or more) | |
| α-linolenic acid | × | 〇 | 〇 | 〇 | 〇 | 〇 (age 1 or more) | |
| DHA, EPA | × | × | 〇 | × | 〇 | 〇 † | |
| Cholesterol | 〇 *** | 〇 **** | × | × | × | × | |
| Trans | × | 〇 **** | 〇 **** | 〇 | 〇 | × ** | |
| Carbohydrate | Carbohydrate | 〇 | 〇 | 〇 | 〇 | 〇 | 〇 (Infants only) |
| Fiber | 〇 | 〇 | 〇 | 〇 | 〇 | 〇 | |
| Sugars | × | 〇 (Added sugars) | × | 〇 (Free sugars) | 〇 (Total sugars) | × | |
| Vitamin | A | 〇 | 〇 | 〇 | 〇 | 〇 | 〇 |
| D | 〇 | 〇 | 〇 | 〇 | 〇 | 〇 | |
| E | 〇 | 〇 | 〇 | 〇 | 〇 | 〇 | |
| K | 〇 | 〇 | 〇 | 〇 | 〇 | 〇 | |
| B1 | 〇 | 〇 | 〇 | 〇 | 〇 | 〇 | |
| B2 | 〇 | 〇 | 〇 | 〇 | 〇 | 〇 | |
| Nia | 〇 | 〇 | 〇 | 〇 | 〇 | 〇 | |
| B6 | 〇 | 〇 | 〇 | 〇 | 〇 | 〇 | |
| B12 | 〇 | 〇 | 〇 | 〇 | 〇 | 〇 | |
| FA | 〇 | 〇 | 〇 | 〇 | 〇 | 〇 | |
| PA | 〇 | 〇 | 〇 | 〇 | 〇 | 〇 | |
| Biotin | 〇 | 〇 | 〇 | 〇 | 〇 | 〇 | |
| Choline | × | 〇 | 〇 | × | 〇 | 〇 | |
| C | 〇 | 〇 | 〇 | 〇 | 〇 | 〇 | |
| Minerals | Na | 〇 | 〇 | 〇 | 〇 | 〇 | 〇 |
| K | 〇 | 〇 | 〇 | 〇 | 〇 | 〇 | |
| Ca | 〇 | 〇 | 〇 | 〇 | 〇 | 〇 | |
| Mg | 〇 | 〇 | 〇 | 〇 | 〇 | 〇 | |
| P | 〇 | 〇 | 〇 | 〇 | 〇 | 〇 | |
| Fe | 〇 | 〇 | 〇 | 〇 | 〇 | 〇 | |
| Zn | 〇 | 〇 | 〇 | 〇 | 〇 | 〇 | |
| Cu | 〇 | 〇 | 〇 | 〇 | 〇 | 〇 | |
| Mn | 〇 | 〇 | 〇 | 〇 | 〇 | 〇 | |
| I | 〇 | 〇 | 〇 | 〇 | 〇 | 〇 | |
| Se | 〇 | 〇 | 〇 | 〇 | 〇 | 〇 | |
| Cr | 〇 | 〇 | × | 〇 | 〇 | 〇 | |
| Mo | 〇 | 〇 | 〇 | 〇 | 〇 | 〇 | |
| F | × | 〇 | 〇 | 〇 | 〇 | 〇 | |
| B | × | 〇 | × | 〇 | × | × | |
| Ni | × | 〇 | × | × | 〇 | × | |
| V | × | 〇 | × | × | × | × | |
| Cl | × | 〇 | 〇 | 〇 | 〇 | × | |
| As | × | × | × | × | 〇 | × | |
| Water | × | 〇 | 〇 | × | 〇 | 〇 | |
| Food Guidelines | Japan | U.S. | UK | Saudi Arabia | Australia | DASH | The Mediterranean Diet ** | The Japan Diet *** | The EAT-LANCET | |
|---|---|---|---|---|---|---|---|---|---|---|
| Kcal | 2200 | 2200 | 2200 | 2500 | ||||||
| Units | serve | cups | portion | serve | serve | serve | serve | grams | grams | |
| Grains | 5–7 | 7 (ounce) | 6–11 | 6 | 6–8 | |||||
| Whole grain | 3.5 (ounce) | 1–2/meal | 232 | |||||||
| Refined grain | 3.5 (ounce) | ≤3/week | 440 (mixed with rolled oats) 250 (if “soba” choosed) | |||||||
| Vegetable | 5–6 | 3 | 5 | 3–5 | 5–6 | 4–5 | 2-/meal | 170 (green and yellow) 230 (others) | 300 (200-600) | |
| Dark-green | 2/week | |||||||||
| Red and orange | 6/week | |||||||||
| Beans | 2/week | |||||||||
| Starchy | 6/week | 110 | 50 (0–100) | |||||||
| Other | 5/week | 60 (seaweed and mushroom) | ||||||||
| Protein | 3–5 | 6 (ounce) | 2–3 | 2.5–3 | 6 or less | |||||
| Meats, poultry, eggs | 28 (ounce) /week | eggs: 2–4/week poultry: 1–2/week red meat: ≤2/week processed meat: ≤1/week | eggs: 10 meats (without chicken skin and fat): 80 | meat: 43 (0–86) eggs: 13 (0–25) | ||||||
| Seafood | 9 (ounce) /week | 2/week * | 2-/week | 100 | 28 (0–100) | |||||
| Nuts, seeds, soyproducts | 5 (ounce) /week | 4–5/week | legumes: 2-/week olive, nuts, seeds: 1–2 | soy: 100 | nuts: 125 (0–175) | |||||
| Dairy products | 2 | 3 | 2–4 | 2.5 | 2–3 (low fat) | 2–3/meal (low fat preferably) | 210 | 250 (0–500) | ||
| Fruits | 2 | 2 | 2–4 | 2 | 4–5 | 1–2/meal | 275 | 200 (100–300) | ||
| Oils | 29 (grams) | the least amount | 27 | Unsaturated: 40 (20–80) Saturated: 11.8 (0–11.8) | ||||||
| Extra virgin olive oil | 3–4 | |||||||||
| Fluids | 6–8 | 6 (cups) | ||||||||
| Sodium (mg) | 2300 | 2300 /1500 | 22 (salt + miso + soysauce) | |||||||
| Sweets | sugar: the least amount | 5 or less/week | ≤2/week | sugar:12 | Sugar: 31 (0–31) |
| Nutrients | Lower Limit | Upper Limit | Nutrients | Lower Limit | Upper Limit |
|---|---|---|---|---|---|
| Protein | Niacin | ||||
| Fats | Vitamin B6 | ||||
| n-3 fatty acid | Vitamin B12 | ||||
| Carbohydrate | Folic acid | ||||
| Sodium | Pantothenic acid | ||||
| Potassium | Biotin | ||||
| Calcium | Vitamin C | ||||
| Magnesium | Isoleucine | ||||
| Iron | Leucine | ||||
| Zinc | Lysine | ||||
| Copper | Sulfur-containing amino acid | ||||
| Vitamin A | Aromatic amino acid | ||||
| Vitamin D | Threonine | ||||
| Vitamin E | Tryptophan | ||||
| Vitamin K | Valine | ||||
| Vitamin B1 | Histidine | ||||
| Vitamin B2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shobako, N.; Itoh, H.; Honda, K. Typical Guidelines for Well-Balanced Diet and Science Communication in Japan and Worldwide. Nutrients 2024, 16, 2112. https://doi.org/10.3390/nu16132112
Shobako N, Itoh H, Honda K. Typical Guidelines for Well-Balanced Diet and Science Communication in Japan and Worldwide. Nutrients. 2024; 16(13):2112. https://doi.org/10.3390/nu16132112
Chicago/Turabian StyleShobako, Naohisa, Hiroshi Itoh, and Keiko Honda. 2024. "Typical Guidelines for Well-Balanced Diet and Science Communication in Japan and Worldwide" Nutrients 16, no. 13: 2112. https://doi.org/10.3390/nu16132112
APA StyleShobako, N., Itoh, H., & Honda, K. (2024). Typical Guidelines for Well-Balanced Diet and Science Communication in Japan and Worldwide. Nutrients, 16(13), 2112. https://doi.org/10.3390/nu16132112






