Resveratrol Propionate Ester Supplement Exerts Antihypertensive Effect in Juvenile Rats Exposed to an Adenine Diet via Gut Microbiota Modulation
Abstract
:1. Introduction
2. Materials and Methods
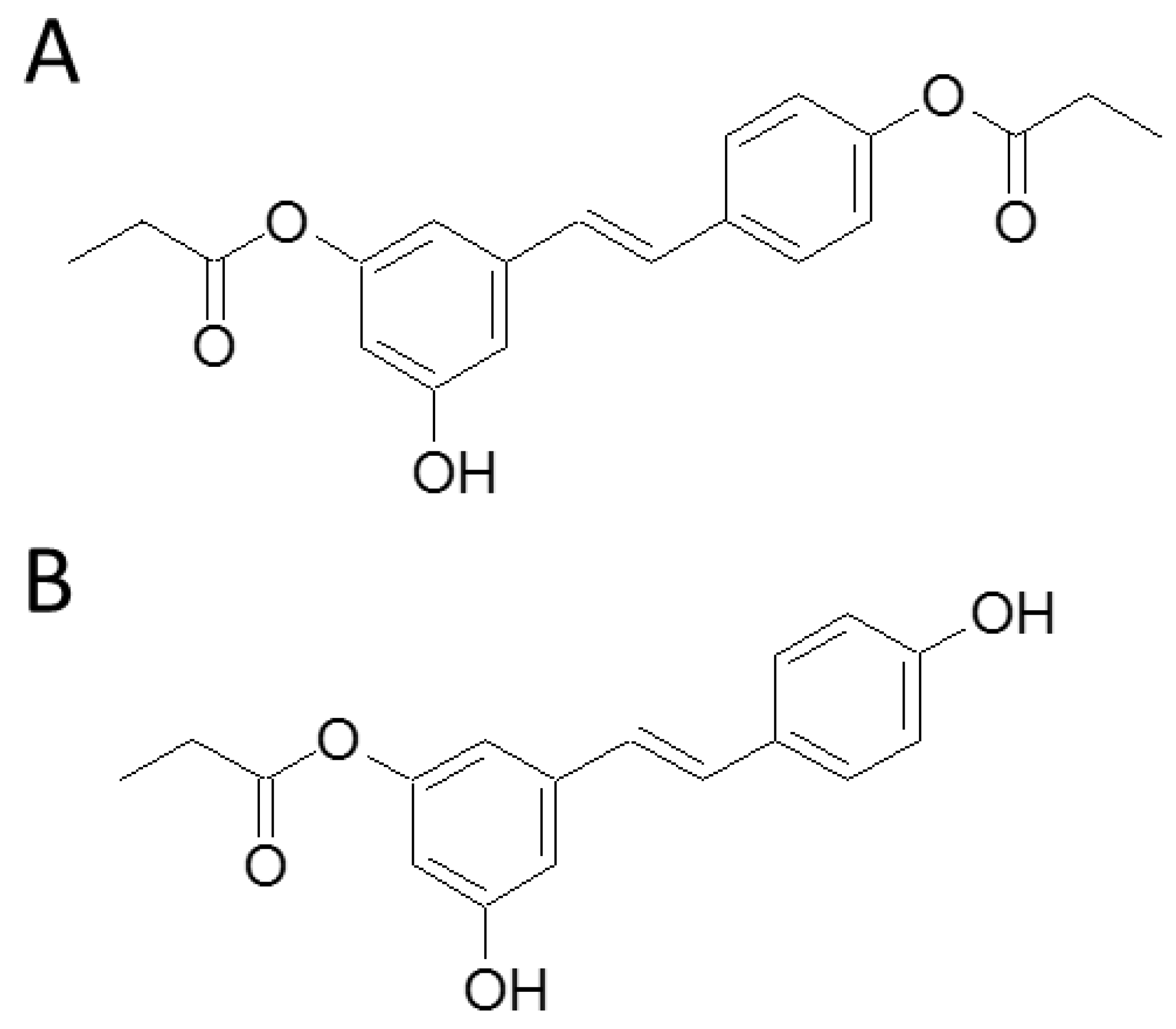
2.1. Synthesis of Resveratrol Propionate Esters
2.2. Purification of RPE Esters
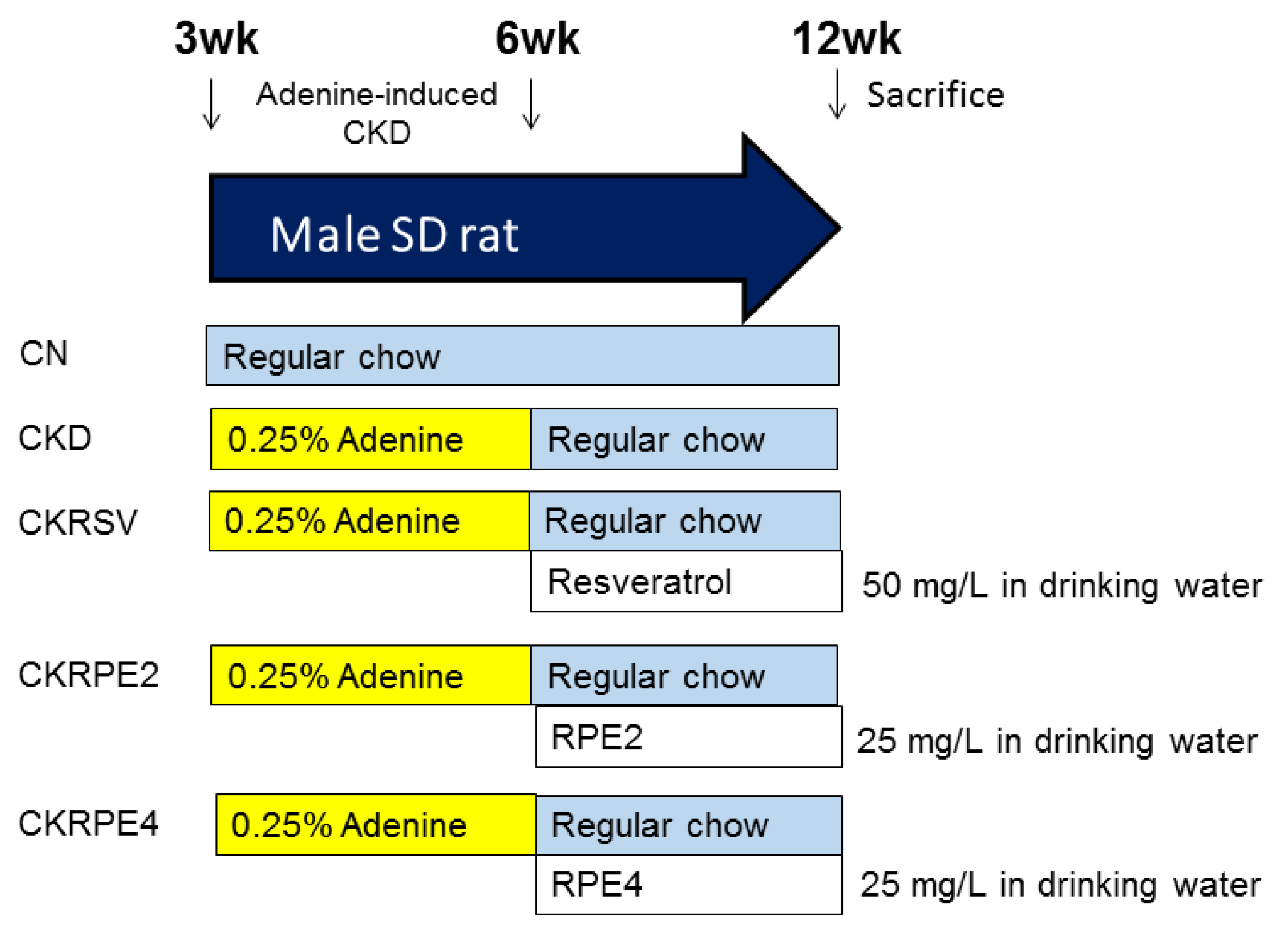
2.3. Animal Model
2.4. Measurement of SCFAs by GC-MS
2.5. Measurement of NO Elements by HPLC
2.6. Quantitative Real-Time Polymerase Chain Reaction
2.7. Microbiome Analysis
2.8. Statistics
3. Results
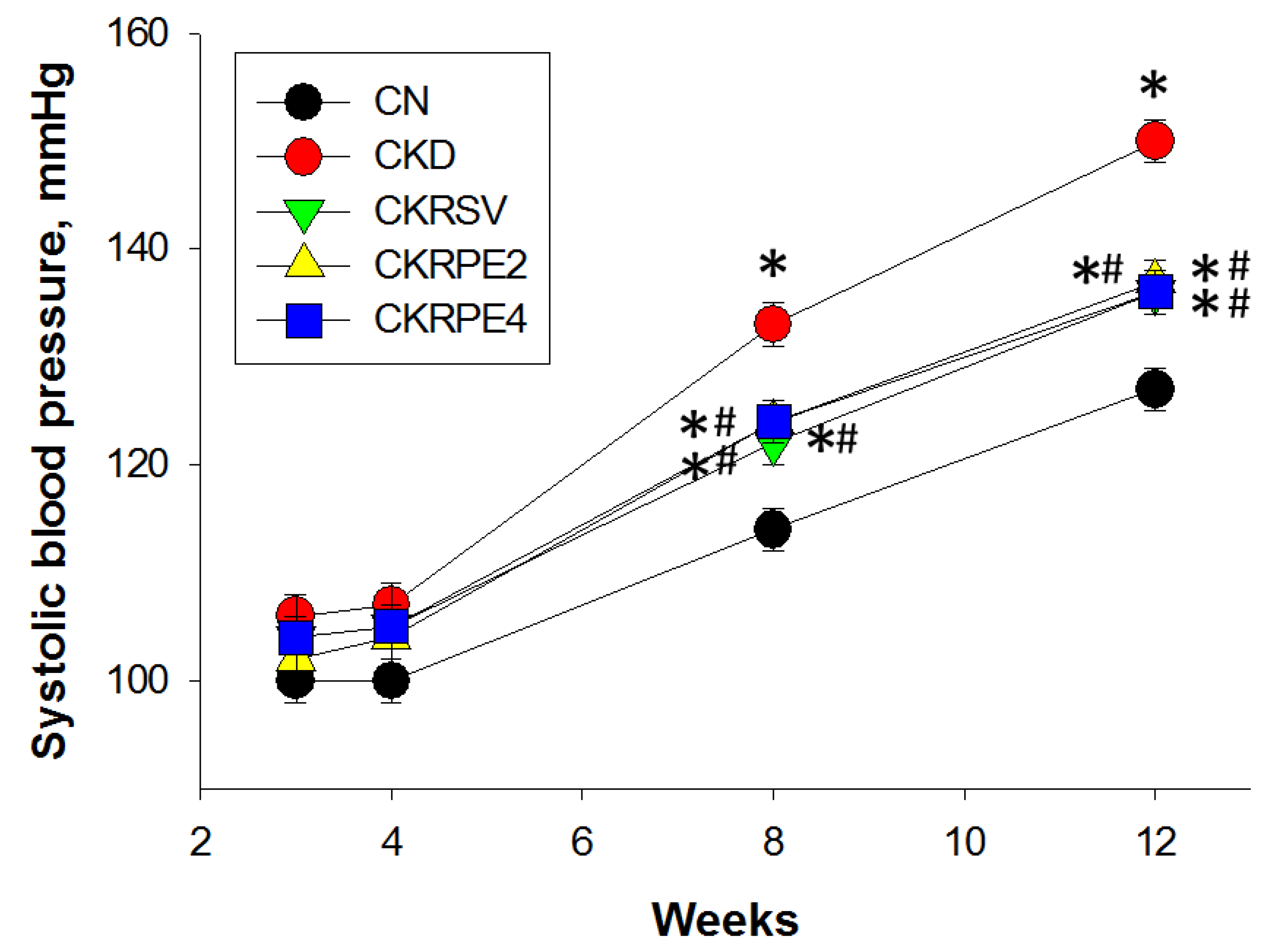
3.1. Body Weight, BP, and Renal Function
3.2. NO Pathway
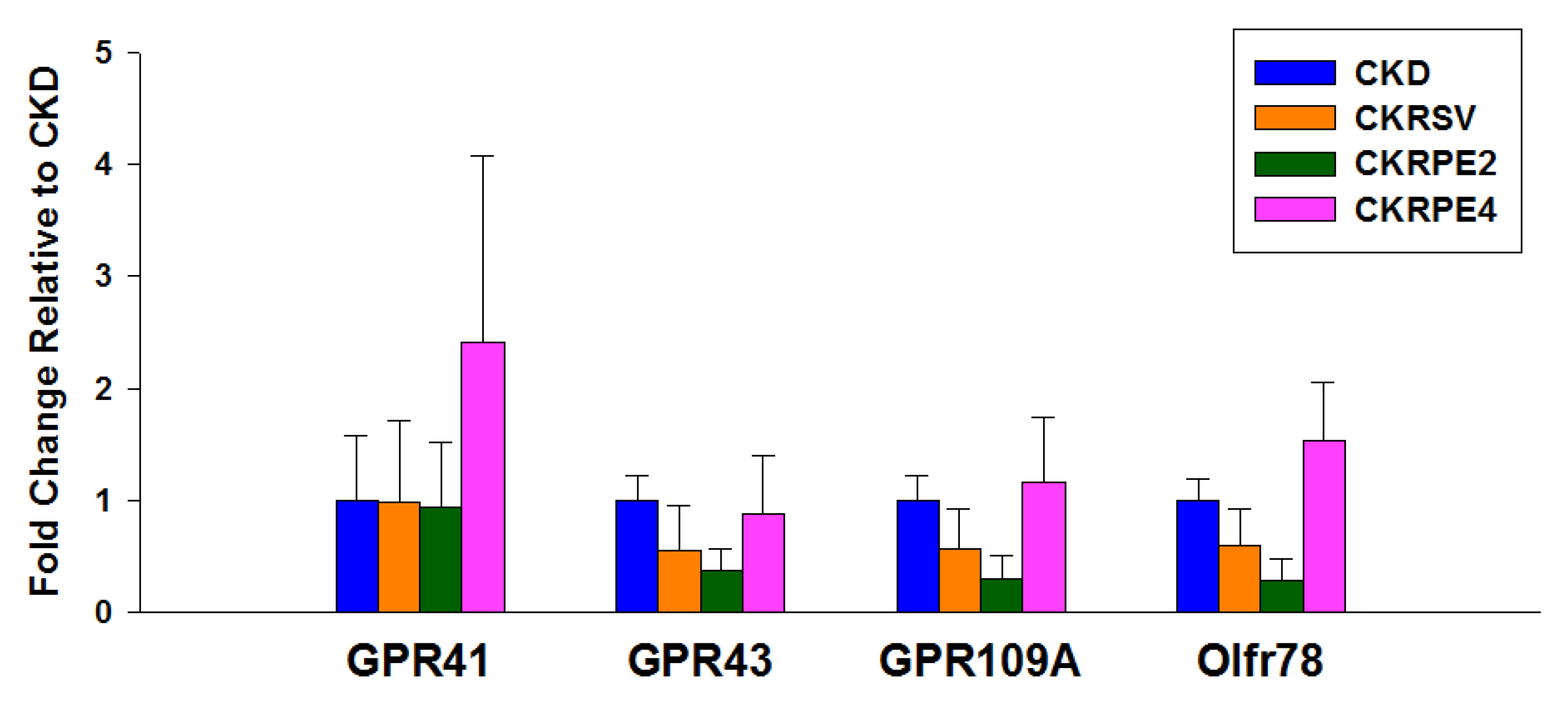
3.3. SCFAs and Their Receptors
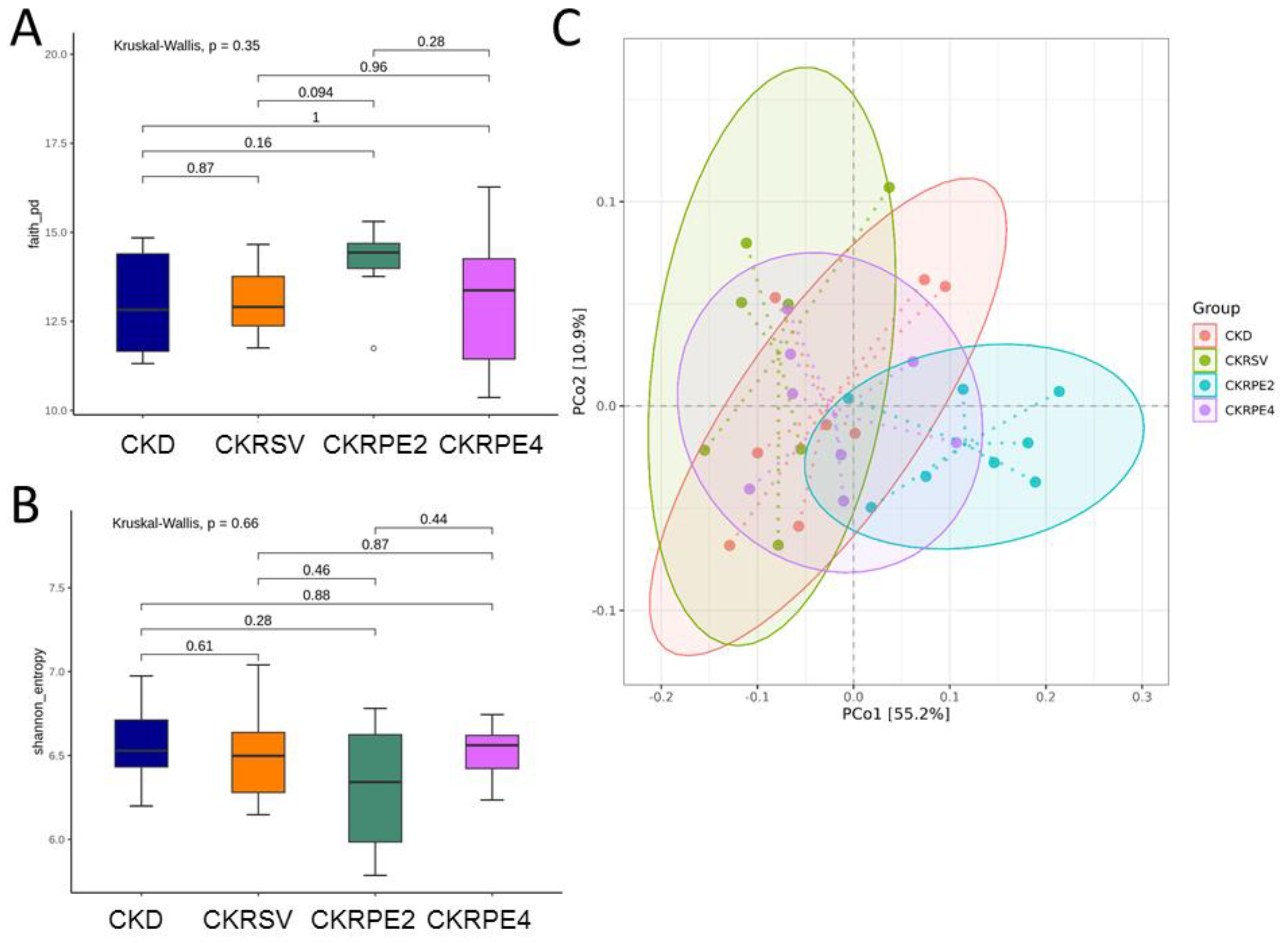
3.4. Gut Microbiota Compositions
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vidi, S.R. Role of hypertension in progression of chronic kidney disease in children. Curr. Opin. Pediatr. 2018, 30, 247–251. [Google Scholar] [CrossRef] [PubMed]
- Yang, T.; Richards, E.M.; Pepine, C.J.; Raizada, M.K. The gut microbiota and the brain-gut-kidney axis in hypertension and chronic kidney disease. Nat. Rev. Nephrol. 2018, 14, 442–456. [Google Scholar] [CrossRef]
- Claramunt, D.; Gil-Peña, H.; Fuente, R.; Hernández-Frías, O.; Santos, F. Animal models of pediatric chronic kidney disease. Is adenine intake an appropriate model? Nefrologia 2015, 35, 517–522. [Google Scholar] [CrossRef]
- Hsu, C.N.; Yang, H.W.; Hou, C.Y.; Chang-Chien, G.P.; Lin, S.; Tain, Y.L. Melatonin Prevents Chronic Kidney Disease-Induced Hypertension in Young Rat Treated with Adenine: Implications of Gut Microbiota-Derived Metabolites. Antioxidants 2021, 10, 1211. [Google Scholar] [CrossRef]
- Sanders, M.E.; Merenstein, D.J.; Reid, G.; Gibson, G.R.; Rastall, R.A. Probiotics and prebiotics in intestinal health and disease: From biology to the clinic. Nat. Rev. Gastroenterol. Hepatol. 2019, 16, 605–616. [Google Scholar] [CrossRef]
- Peluzio, M.D.C.G.; Martinez, J.A.; Milagro, F.I. Postbiotics: Metabolites and mechanisms involved in microbiota-host interactions. Trends Food Sci. Technol. 2021, 108, 11–26. [Google Scholar] [CrossRef]
- Diaz-Gerevini, G.T.; Repossi, G.; Dain, A.; Tarres, M.C.; Das, U.N.; Eynard, A.R. Beneficial action of resveratrol: How and why? Nutrition 2016, 32, 174–178. [Google Scholar] [CrossRef]
- Kursvietiene, L.; Staneviciene, I.; Mongirdiene, A.; Bernatoniene, J. Multiplicity of effects and health benefits of resveratrol. Medicina 2016, 52, 148–155. [Google Scholar] [CrossRef]
- Moorthy, M.; Chaiyakunapruk, N.; Jacob, S.A.; Palanisamy, U.D. Prebiotic potential of polyphenols, its effect on gut microbiota and anthropometric/clinical markers: A systematic review of randomised controlled trials. Trends Food Sci. Technol. 2020, 99, 634–649. [Google Scholar] [CrossRef]
- Moorthy, M.; Sundralingam, U.; Palanisamy, U.D. Polyphenols as Prebiotics in the Management of High-Fat Diet-Induced Obesity: A Systematic Review of Animal Studies. Foods 2021, 10, 299. [Google Scholar] [CrossRef]
- Rodríguez-Daza, M.C.; Pulido-Mateos, E.C.; Lupien-Meilleur, J.; Guyonnet, D.; Desjardins, Y.; Roy, D. Polyphenol-Mediated Gut Microbiota Modulation: Toward Prebiotics and Further. Front. Nutr. 2021, 8, 689456. [Google Scholar] [CrossRef]
- Hsu, C.N.; Hou, C.Y.; Tain, Y.L. Preventive Aspects of Early Resveratrol Supplementation in Cardiovascular and Kidney Disease of Developmental Origins. Int. J. Mol. Sci. 2021, 22, 4210. [Google Scholar] [CrossRef]
- Cottart, C.H.; Nivet-Antoine, V.; Laguillier-Morizot, C.; Beaudeux, J.L. Resveratrol bioavailability and toxicity in humans. Mol. Nutr. Food Res. 2010, 54, 7–16. [Google Scholar] [CrossRef]
- Xu, J.; Moore, B.N.; Pluznick, J.L. Short-Chain Fatty Acid Receptors and Blood Pressure Regulation: Council on Hypertension Mid-Career Award for Research Excellence 2021. Hypertension 2022, 79, 2127–2137. [Google Scholar] [CrossRef] [PubMed]
- Scott, E.; De Paepe, K.; Van de Wiele, T. Postbiotics and Their Health Modulatory Biomolecules. Biomolecules 2022, 12, 1640. [Google Scholar] [CrossRef]
- Hosseini, E.; Grootaert, C.; Verstraete, W.; Van de Wiele, T. Propionate as a health-promoting microbial metabolite in the human gut. Nutr. Rev. 2011, 69, 245–258. [Google Scholar] [CrossRef] [PubMed]
- Tain, Y.L.; Hou, C.Y.; Chang-Chien, G.P.; Lin, S.F.; Hsu, C.N. Perinatal Propionate Supplementation Protects Adult Male Offspring from Maternal Chronic Kidney Disease-Induced Hypertension. Nutrients 2022, 14, 3435. [Google Scholar] [CrossRef] [PubMed]
- Tain, Y.L.; Hou, C.Y.; Chang-Chien, G.P.; Lin, S.; Tzeng, H.T.; Lee, W.C.; Wu, K.L.H.; Yu, H.R.; Chan, J.Y.H.; Hsu, C.N. Reprogramming Effects of Postbiotic Butyrate and Propionate on Maternal High-Fructose Diet-Induced Offspring Hypertension. Nutrients 2023, 15, 1682. [Google Scholar] [CrossRef]
- Tain, Y.L.; Chang, S.K.C.; Liao, J.X.; Chen, Y.W.; Huang, H.T.; Li, Y.L.; Hou, C.Y. Synthesis of Short-Chain-Fatty-Acid Resveratrol Esters and Their Antioxidant Properties. Antioxidants 2021, 10, 420. [Google Scholar] [CrossRef]
- Oh, W.Y.; Shahidi, F. Antioxidant activity of resveratrol ester derivatives in food and biological model systems. Food Chem. 2018, 261, 267–273. [Google Scholar] [CrossRef]
- Carrero, J.J.; González-Ortiz, A.; Avesani, C.M.; Bakker, S.J.L.; Bellizzi, V.; Chauveau, P.; Clase, C.M.; Cupisti, A.; Espinosa-Cuevas, A.; Molina, P.; et al. Plant-based diets to manage the risks and complications of chronic kidney disease. Nat. Rev. Nephrol. 2020, 16, 525–542. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, C.B.; Glisson, J.K.; Minor, D.S. Dietary supplements and hypertension: Potential benefits and precautions. J. Clin. Hypertens. 2012, 14, 467–471. [Google Scholar] [CrossRef] [PubMed]
- Gohari, S.; Ghobadi, S.; Jafari, A.; Ahangar, H.; Gohari, S.; Mahjani, M. The effect of dietary approaches to stop hypertension and ketogenic diets intervention on serum uric acid concentration: A systematic review and meta-analysis of randomized controlled trials. Sci. Rep. 2023, 13, 10492. [Google Scholar] [CrossRef]
- Hsu, C.N.; Hou, C.Y.; Chang, C.I.; Tain, Y.L. Resveratrol Butyrate Ester Protects Adenine-Treated Rats against Hypertension and Kidney Disease by Regulating the Gut-Kidney Axis. Antioxidants 2021, 11, 83. [Google Scholar] [CrossRef] [PubMed]
- Reckelhoff, J.F. Gender differences in the regulation of blood pressure. Hypertension 2001, 37, 1199–1208. [Google Scholar] [CrossRef] [PubMed]
- Bode-Böger, S.M.; Scalera, F.; Ignarro, L.J. The L-arginine paradox: Importance of the L-arginine/asymmetrical dimethylarginine ratio. Pharmacol. Ther. 2007, 114, 295–306. [Google Scholar] [CrossRef] [PubMed]
- Bolyen, E.; Rideout, J.R.; Dillon, M.R.; Bokulich, N.A.; Abnet, C.C.; Al-Ghalith, G.A.; Alexander, H.; Alm, E.J.; Arumugam, M.; Asnicar, F.; et al. Reproducible, interactive, scalable and extensible microbiome data science using QIIME 2. Nat. Biotechnol. 2019, 37, 852–857. [Google Scholar] [CrossRef]
- Price, M.N.; Dehal, P.S.; Arkin, A.P. FastTree 2—Approximately maximum-likelihood trees for large alignments. PLoS ONE 2010, 5, e9490. [Google Scholar] [CrossRef]
- Sahebkar, A.; Serban, C.; Ursoniu, S.; Wong, N.D.; Muntner, P.; Graham, I.M.; Mikhailidis, D.P.; Rizzo, M.; Rysz, J.; Sperling, L.S.; et al. Lack of efficacy of resveratrol on C-reactive protein and selected cardiovascular risk factors—Results from a systematic review and meta-analysis of randomized controlled trials. Int. J. Cardiol. 2015, 189, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Fogacci, F.; Tocci, G.; Presta, V.; Fratter, A.; Borghi, C.; Cicero, A.F.G. Effect of resveratrol on blood pressure: A systematic review and meta-analysis of randomized, controlled, clinical trials. Crit. Rev. Food Sci. Nutr. 2019, 59, 1605–1618. [Google Scholar] [CrossRef]
- Baylis, C. Nitric oxide synthase derangements and hypertension in kidney disease. Curr. Opin. Nephrol. Hypertens. 2012, 21, 1–6. [Google Scholar] [CrossRef] [PubMed]
- DiNatale, J.C.; Crowe-White, K.M. Effects of resveratrol supplementation on nitric oxide-mediated vascular outcomes in hypertension: A systematic review. Nitric Oxide 2022, 129, 74–81. [Google Scholar] [CrossRef] [PubMed]
- R Muralitharan, R.; Marques, F.Z. Diet-related gut microbial metabolites and sensing in hypertension. J. Hum. Hypertens. 2021, 35, 162–169. [Google Scholar] [CrossRef]
- Zhang, H.; Duan, Y.; Cai, F.; Cao, D.; Wang, L.; Qiao, Z.; Hong, Q.; Li, N.; Zheng, Y.; Su, M.; et al. Next-Generation Probiotics: Microflora Intervention to Human Diseases. Biomed. Res. Int. 2022, 2022, 5633403. [Google Scholar] [CrossRef]
- Guerrero Sanchez, M.; Passot, S.; Campoy, S.; Olivares, M.; Fonseca, F. Ligilactobacillus salivarius functionalities, applications, and manufacturing challenges. Appl. Microbiol. Biotechnol. 2022, 106, 57–80. [Google Scholar] [CrossRef]
- Mukohda, M.; Yano, T.; Matsui, T.; Nakamura, S.; Miyamae, J.; Toyama, K.; Mitsui, R.; Mizuno, R.; Ozaki, H. Treatment with Ligilactobacillus murinus lowers blood pressure and intestinal permeability in spontaneously hypertensive rats. Sci. Rep. 2023, 13, 15197. [Google Scholar] [CrossRef] [PubMed]
- Palmu, J.; Lahti, L.; Niiranen, T. Targeting Gut Microbiota to Treat Hypertension: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 1248. [Google Scholar] [CrossRef]
- Yan, D.; Sun, Y.; Zhou, X.; Si, W.; Liu, J.; Li, M.; Wu, M. Regulatory effect of gut microbes on blood pressure. Animal Model Exp. Med. 2022, 5, 513–531. [Google Scholar]
- Tomova, A.; Bukovsky, I.; Rembert, E.; Yonas, W.; Alwarith, J.; Barnard, N.D.; Kahleova, H. The Effects of Vegetarian and Vegan Diets on Gut Microbiota. Front. Nutr. 2019, 6, 47. [Google Scholar] [CrossRef]
- Thandapilly, S.J.; Louis, X.L.; Behbahani, J.; Movahed, A.; Yu, L.; Fandrich, R.; Zhang, S.; Kardami, E.; Anderson, H.D.; Netticadan, T. Reduced hemodynamic load aids low-dose resveratrol in reversing cardiovascular defects in hypertensive rats. Hypertens. Res. 2013, 36, 866–872. [Google Scholar]
- Huang, P.H.; Chen, D.Q.; Chen, Y.W.; Shih, M.K.; Lee, B.H.; Tain, Y.L.; Hsieh, C.W.; Hou, C.Y. Evaluation of the Feasibility of In Vitro Metabolic Interruption of Trimethylamine with Resveratrol Butyrate Esters and Its Purified Monomers. Molecules 2024, 29, 429. [Google Scholar] [CrossRef]
- Zhang, L.X.; Li, C.X.; Kakar, M.U.; Khan, M.S.; Wu, P.F.; Amir, R.M.; Dai, D.F.; Naveed, M.; Li, Q.Y.; Saeed, M.; et al. Resveratrol (RV): A pharmacological review and call for further research. Biomed. Pharmacother. 2021, 143, 112164. [Google Scholar] [CrossRef]


| Groups | CN | CKD | CKRSV | CKRPE2 | CKRPE4 |
|---|---|---|---|---|---|
| Mortality (%) | 0 | 0 | 12.5 | 0 | 0 |
| Body weight (BW) (g) | 334 ± 7 | 243 ± 13 * | 289 ± 5 * | 307 ± 7 # | 286 ± 6 * |
| Left kidney weight (KW) (g) | 1.14 ± 0.04 | 2.12 ± 0.07 * | 1.70 ± 0.06 #* | 1.98 ± 0.1 * | 1.67 ± 0.05 *# |
| KW-to-BW ratio (g/kg) | 3.4 ± 0.1 | 8.9 ± 0.1 * | 5.9 ± 0.1 *# | 6.4 ± 0.1 *# | 5.8 ± 0.1 *# |
| Systolic BP (mmHg) | 127 ± 1 | 150 ± 2 * | 136 ± 1 # | 137 ± 1 # | 136 ± 1 # |
| Diastolic BP (mmHg) | 86 ± 2 | 99 ± 2 * | 86 ± 3 # | 91 ± 2 # | 87 ± 2 # |
| Creatinine (μM) | 16.4 ± 0.5 | 23.2 ± 1.2 * | 21.5 ± 0.8 * | 19.1 ± 1 *# | 20.8 ± 0.8 * |
| Groups | CKD | CKRSV | CKRPE2 | CKRPE4 |
|---|---|---|---|---|
| Arginine, μM | 203.4 ± 15.1 | 202.6 ± 8.3 | 227.1 ± 9.4 | 233.2 ± 21.5 |
| ADMA, μM | 2.71 ± 0.08 | 2.42 ± 0.07 * | 2.12 ± 0.1 * | 2.3 ± 0.04 * |
| SDMA, μM | 2.84 ± 0.1 | 2.58 ± 0.09 | 2.38 ± 0.08 * | 2.47 ± 0.06 * |
| Ratio of arginine-to-ADMA | 75.6 ± 5.3 | 82.1 ± 2 | 105.4 ± 8.5 * | 100.8 ± 12 * |
| Groups | CKD | CKRSV | CKRPE2 | CKRPE4 |
|---|---|---|---|---|
| Acetic acid, ng/mL | 561.1 ± 31.3 | 643.5 ± 19.4 | 779.5 ± 41.6 * | 584.2 ± 34.5 |
| Propionic acid, ng/mL | 4.92 ± 0.17 | 4.61 ± 0.14 | 7.16 ± 0.23 * | 7.46 ± 0.52 * |
| Butyric acid, ng/mL | 9.79 ± 1.21 | 8.14 ± 0.41 | 10.81 ± 0.92 | 18.04 ± 0.78 * |
| Valeric acid, ng/mL | 1.93 ± 0.08 | 1.94 ± 0.03 | 2.11 ± 0.07 | 1.92 ± 0.04 |
| Hexanoic acid, ng/mL | 16.14 ± 0.73 | 17.34 ± 0.43 | 21.07 ± 0.87 * | 19.67 ± 0.73 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tain, Y.-L.; Chang, C.-I.; Hou, C.-Y.; Chang-Chien, G.-P.; Lin, S.-F.; Hsu, C.-N. Resveratrol Propionate Ester Supplement Exerts Antihypertensive Effect in Juvenile Rats Exposed to an Adenine Diet via Gut Microbiota Modulation. Nutrients 2024, 16, 2131. https://doi.org/10.3390/nu16132131
Tain Y-L, Chang C-I, Hou C-Y, Chang-Chien G-P, Lin S-F, Hsu C-N. Resveratrol Propionate Ester Supplement Exerts Antihypertensive Effect in Juvenile Rats Exposed to an Adenine Diet via Gut Microbiota Modulation. Nutrients. 2024; 16(13):2131. https://doi.org/10.3390/nu16132131
Chicago/Turabian StyleTain, You-Lin, Chi-I Chang, Chih-Yao Hou, Guo-Ping Chang-Chien, Shu-Fen Lin, and Chien-Ning Hsu. 2024. "Resveratrol Propionate Ester Supplement Exerts Antihypertensive Effect in Juvenile Rats Exposed to an Adenine Diet via Gut Microbiota Modulation" Nutrients 16, no. 13: 2131. https://doi.org/10.3390/nu16132131






