Phenylalanine-Free Infant Formula in Patients with Phenylketonuria: A Retrospective Study
Abstract
1. Introduction
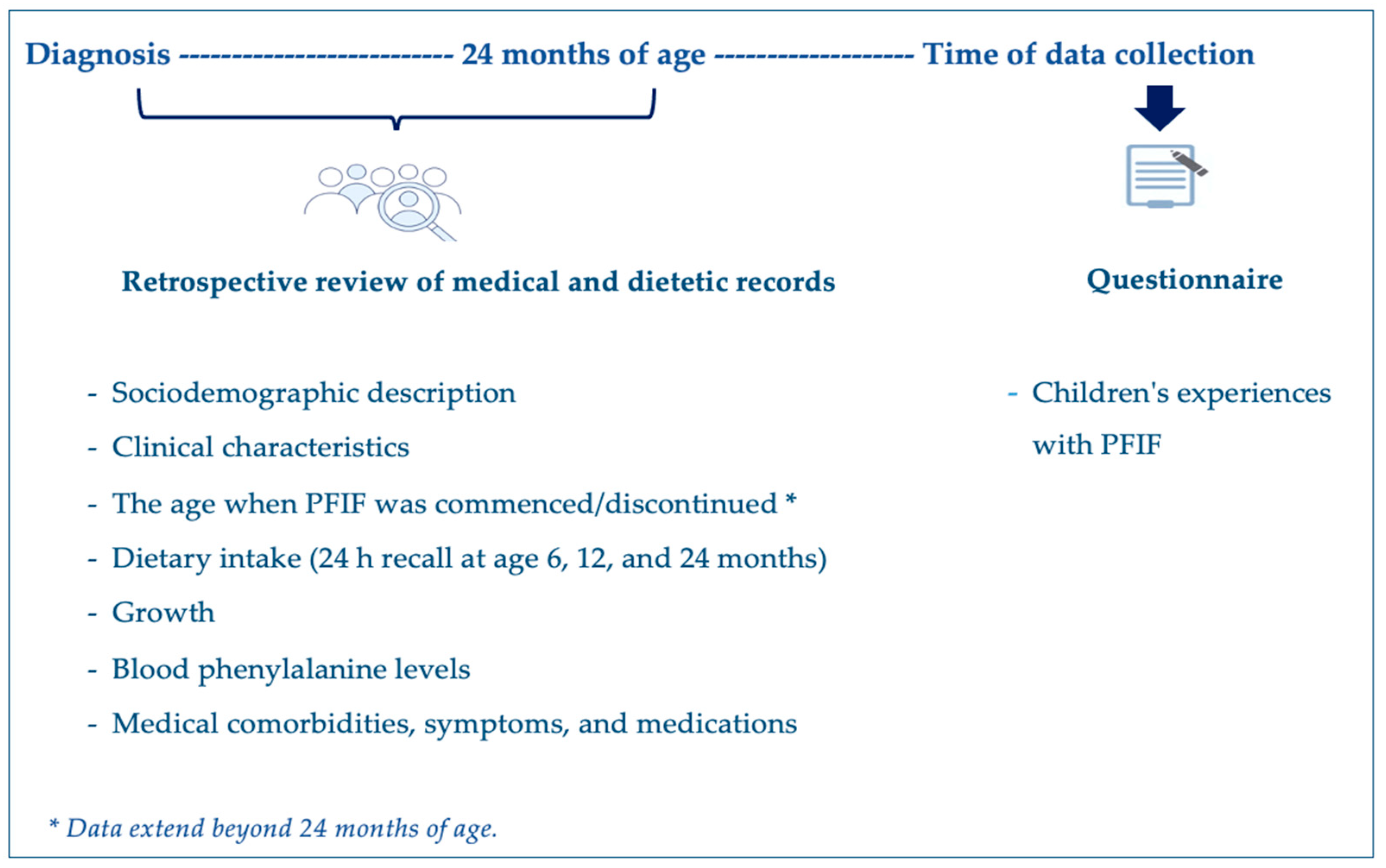
2. Materials and Methods
2.1. Project Design
2.2. Data Collection
2.3. Blood Phenylalanine Control
2.4. Anthropometry
2.5. Dietary Assessment
2.6. Study Formula
2.7. Statistical Analysis
2.8. Ethical Approval
3. Results
3.1. Subjects
3.2. Introduction of PFIF and Transition to Weaning Protein Substitute and Solid Foods
3.3. Metabolic Control
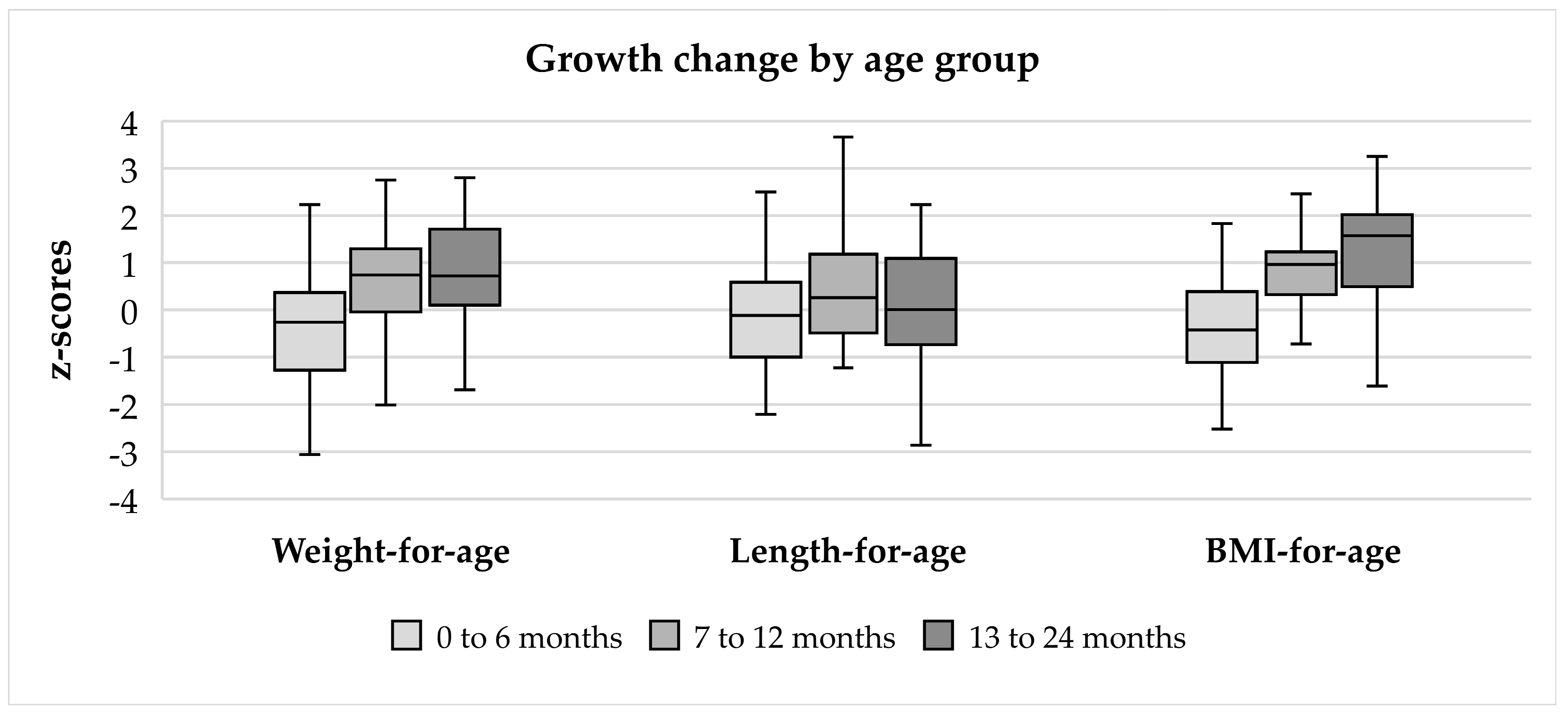
3.4. Anthropometric Changes
3.5. Dietary Intake
3.6. Metabolic Control—PFIF Discontinuation before vs. after 24 Months of Age
3.7. Growth—Male vs. Female
3.8. Growth—PFIF Discontinuation before vs. after 24 Months of Age
3.9. Dietary Intake—PFIF Discontinuation before vs. after 24 Months of Age
3.10. Socioeconomic Factors—PFIF Discontinuation before vs. after 24 Months of Age
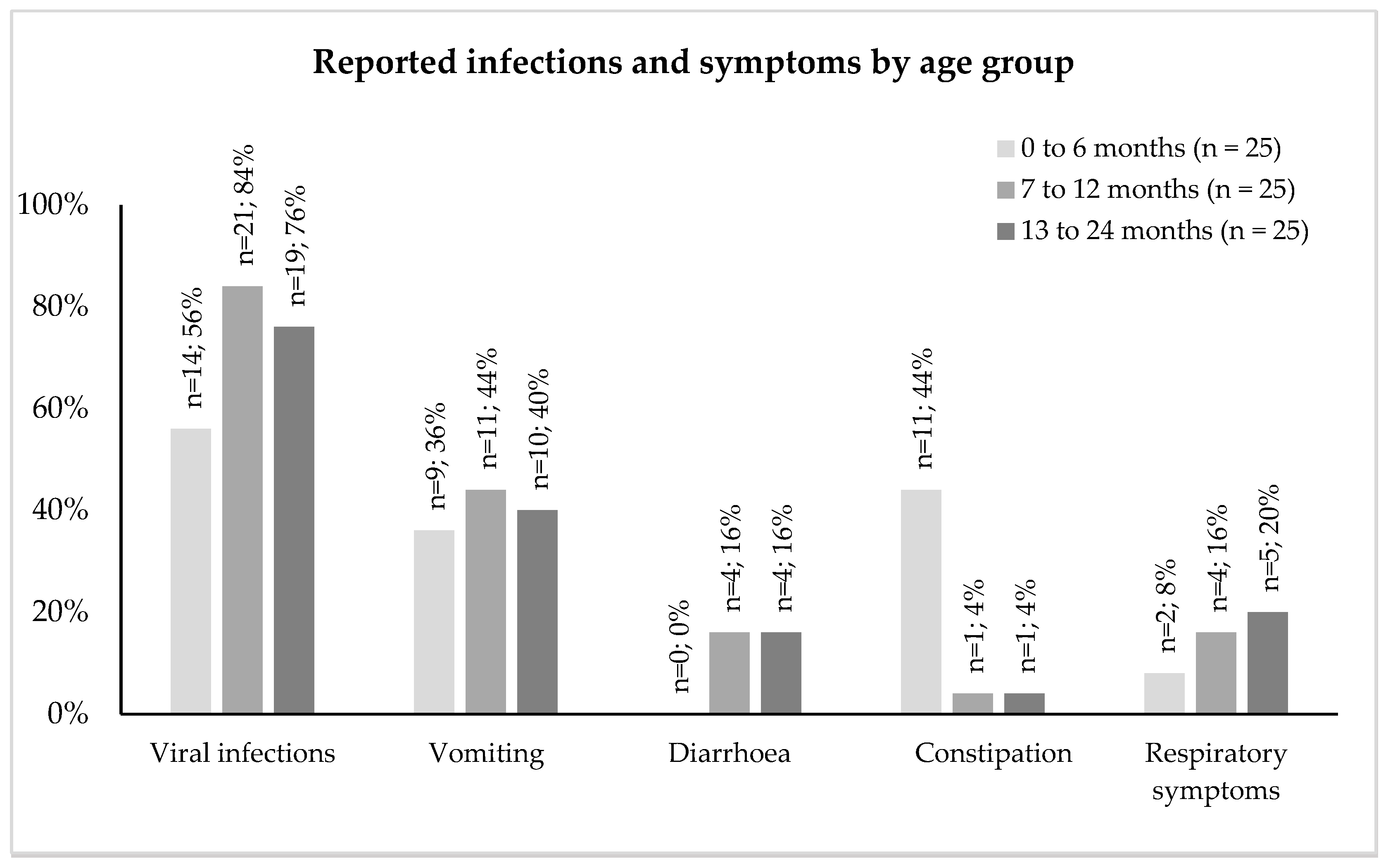
3.11. Symptoms and Medications
3.12. Experience with the PFIF
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- van Wegberg, A.M.J.; MacDonald, A.; Ahring, K.; Bélanger-Quintana, A.; Blau, N.; Bosch, A.M.; Burlina, A.; Campistol, J.; Feillet, F.; Giżewska, M.; et al. The complete European guidelines on phenylketonuria: Diagnosis and treatment. Orphanet J. Rare Dis. 2017, 12, 162. [Google Scholar] [CrossRef]
- Blau, N.; Van Spronsen, F.J.; Levy, H.L. Phenylketonuria. Lancet 2010, 376, 1417–1427. [Google Scholar] [CrossRef]
- Brown, C.S.; Lichter-Konecki, U. Phenylketonuria (PKU): A problem solved? Mol. Genet. Metab. 2016, 6, 8–12. [Google Scholar] [CrossRef]
- Hillert, A.; Anikster, Y.; Belanger-Quintana, A.; Burlina, A.; Burton, B.K.; Carducci, C.; Chiesa, A.E.; Christodoulou, J.; Đorđević, M.; Desviat, L.R. The genetic landscape and epidemiology of phenylketonuria. Am. J. Hum. Genet. 2020, 107, 234–250. [Google Scholar] [CrossRef]
- Blanchard, E.; Zhu, P.; Schuck, P. Infant formula powders. In Handbook of Food Powders; Elsevier: Amsterdam, The Netherlands, 2024; pp. 375–386. [Google Scholar]
- Nutten, S. Proteins, peptides and amino acids: Role in infant nutrition. In Protein in Neonatal and Infant Nutrition: Recent Updates; Karger Publishers: Basel, Switzerland, 2016; Volume 86, pp. 1–10. [Google Scholar]
- European Commission. Commission Delegated Regulation (EU) 2016/127 of 25 September 2015 supplementing Regulation (EU) No 609/2013 of the European Parliament and of the Council as regards the specific compositional and information requirements for infant formula and follow-on formula and as regards requirements on information relating to infant and young child feeding. OJEC 2016, 59, 1–29. [Google Scholar]
- MacDonald, A.; Cochrane, B.; Wopereis, H.; Loveridge, N. Specific prebiotics in a formula for infants with Phenylketonuria. Mol. Genet. Metab. 2011, 104, S55–S59. [Google Scholar] [CrossRef]
- Bakshi, S.; Paswan, V.K.; Yadav, S.P.; Bhinchhar, B.K.; Kharkwal, S.; Rose, H.; Kanetkar, P.; Kumar, V.; Al-Zamani, Z.A.S.; Bunkar, D.S. A comprehensive review on infant formula: Nutritional and functional constituents, recent trends in processing and its impact on infants’ gut microbiota. Front. Nutr. 2023, 10, 1194679. [Google Scholar] [CrossRef]
- Francisquini, J.A.; Nunes, L.; Martins, E.; Stephani, R.; Perrone, Í.T.; Carvalho, A.F. How the heat treatment affects the constituents of infant formulas: A review. Braz. J. Food Technol. 2020, 23, e2019272. [Google Scholar] [CrossRef]
- Masum, A.; Chandrapala, J.; Adhikari, B.; Huppertz, T.; Zisu, B. Effect of lactose-to-maltodextrin ratio on emulsion stability and physicochemical properties of spray-dried infant milk formula powders. J. Food Eng. 2019, 254, 34–41. [Google Scholar] [CrossRef]
- Miraglia Del Giudice, M.; D’Auria, E.; Peroni, D.; Palazzo, S.; Radaelli, G.; Comberiati, P.; Galdo, F.; Maiello, N.; Riva, E. Flavor, relative palatability and components of cow’s milk hydrolysed formulas and amino acid-based formula. Ital. J. Pediatr. 2015, 41, 42. [Google Scholar] [CrossRef]
- Kumar Dalei, S.; Adlakha, N. Food Regime for Phenylketonuria: Presenting Complications and Possible Solutions. J. Multidiscip. Healthc. 2022, 15, 125–136. [Google Scholar] [CrossRef]
- Acosta, P.; Yannicelli, S. Protein intake affects phenylalanine requirements and growth of infants with phenylketonuria. Acta Paediatr. 1994, 83, 66–67. [Google Scholar] [CrossRef]
- Daly, A.; Evans, S.; Pinto, A.; Ashmore, C.; MacDonald, A. Protein substitutes in PKU; their historical evolution. Nutrients 2021, 13, 484. [Google Scholar] [CrossRef]
- Yilmaz, O.; Cochrane, B.; Wildgoose, J.; Pinto, A.; Evans, S.; Daly, A.; Ashmore, C.; MacDonald, A. Phenylalanine free infant formula in the dietary management of phenylketonuria. Orphanet J. Rare Dis. 2023, 18, 16. [Google Scholar] [CrossRef]
- Van Spronsen, F.J.; van Wegberg, A.M.; Ahring, K.; Bélanger-Quintana, A.; Blau, N.; Bosch, A.M.; Burlina, A.; Campistol, J.; Feillet, F.; Giżewska, M. Key European guidelines for the diagnosis and management of patients with phenylketonuria. Lancet Diabetes Endocrinol. 2017, 5, 743–756. [Google Scholar] [CrossRef]
- World Health Organization. WHO Anthro Survey Analyser: Software for Analysing Survey Anthropometric Data for Children under 5 Years of Age; Built-in Software Edition; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- World Health Organization. WHO Child Growth Standards: Training Course on Child Growth Assessment; WHO: Geneva, Switzerland, 2008. [Google Scholar]
- Nutritics. Research Edition (v5. 09) [Computer Software]. Available online: https://www.nutritics.com (accessed on 26 May 2024).
- Scientific Advisory Committee on Nutrition. Dietary Reference Values for Energy; The Stationery Office: London, UK, 2012.
- Microsoft Excel, version 16.71 (Build 23031200); Microsoft Corporation: Redmond, WA, USA, 2023.
- IBM SPSS Statistics for Macintosh, version 26.0; IBM Corp: Armonk, NY, USA, 2019.
- Evans, S.; Daly, A.; Wildgoose, J.; Cochrane, B.; Chahal, S.; Ashmore, C.; Loveridge, N.; MacDonald, A. How does feeding development and progression onto solid foods in PKU compare with non-PKU children during weaning? Nutrients 2019, 11, 529. [Google Scholar] [CrossRef]
- MacDonald, A.; Evans, S.; Cochrane, B.; Wildgoose, J. Weaning infants with phenylketonuria: A review. J. Hum. Nutr. Diet. 2012, 25, 103–110. [Google Scholar] [CrossRef]
- Gooze, R.A.; Anderson, S.E.; Whitaker, R.C. Prolonged bottle use and obesity at 5.5 years of age in US children. J. Pediatr. 2011, 159, 431–436. [Google Scholar] [CrossRef]
- Bonuck, K.; Kahn, R.; Schechter, C. Is late bottle-weaning associated with overweight in young children? Analysis of NHANES III data. Clin. Pediatr. 2004, 43, 535–540. [Google Scholar] [CrossRef] [PubMed]
- Kristiansen, A.L.; Lande, B.; Øverby, N.C.; Andersen, L.F. Factors associated with exclusive breast-feeding and breast-feeding in Norway. Public Health Nutr. 2010, 13, 2087–2096. [Google Scholar] [CrossRef]
- Kim, J.; Gallien, T.L. Childcare arrangements and infant feeding practices by family structure and household income among US children aged 0 to 2 years. Matern. Child Nutr. 2016, 12, 591–602. [Google Scholar] [CrossRef]
- Ballikaya, E.; Yildiz, Y.; Sivri, H.S.; Tokatli, A.; Dursun, A.; Olmez, S.; Coskun, T.; Uzamis Tekcicek, M. Oral health status of children with phenylketonuria. J. Pediatr. Endocrinol. Metab. 2020, 33, 361–365. [Google Scholar] [CrossRef]
- Ābola, I.; Emuliņa, D.E.; Skadiņš, I.; Brinkmane, A.; Gailīte, L.; Auzenbaha, M. Dental Status and Periodontal Health of Patients with Phenylketonuria in Latvia. Acta Stomatol. Croat. 2022, 56, 109. [Google Scholar] [CrossRef]
- da Costa Silveira, A.; dos Santos, E.d.S.C.; Pires, D.; da Silva, W.B.; Correa, A.R.B.; da Costa Silveira, E.; de Alencar Menezes, T.O.; Pinheiro, H.H.C.; de Menezes, S.A.F. Evaluation of oral health status in children with phenylketonuria. Int. J. Clin. Dent. 2015, 43, 43–50. [Google Scholar]
- Singh-Hüsgen, P.; Meissner, T.; Bizhang, M.; Henrich, B.; Raab, W.H. Investigation of the oral status and microorganisms in children with phenylketonuria and type 1 diabetes. Clin. Oral Investig. 2016, 20, 841–847. [Google Scholar] [CrossRef]
- Cheng, H.; Chen, R.; Milosevic, M.; Rossiter, C.; Arora, A.; Denney-Wilson, E. Interventions targeting bottle and formula feeding in the prevention and treatment of early childhood caries, overweight and obesity: An integrative review. Int. J. Environ. Res. Public Health 2021, 18, 12304. [Google Scholar] [CrossRef]
- Brecher, E.A.; Lewis, C.W. Infant oral health. Pediatr. Clin. 2018, 65, 909–921. [Google Scholar] [CrossRef]
- Green, M. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents; National Maternal and Child Health Clearinghouse: McLean, VA, USA, 1994.
- American Academy of Pediatric Dentistry. Policy on Early Childhood Caries (ECC): Consequences and Preventive Strategies; The Reference Manual of Pediatric Dentistry; American Academy of Pediatric Dentistry: Chicago, IL, USA, 2023; pp. 88–91. [Google Scholar]
- Weaver, L.; Lucas, A. Development of bowel habit in preterm infants. Arch. Dis. Child. 1993, 68, 317–320. [Google Scholar] [CrossRef]
- Weaver, L.T.; Ewing, G.; Taylor, L.C. The bowel habit of milk-fed infants. J. Pediatr. Gastroenterol. Nutr. 1988, 7, 568–571. [Google Scholar] [CrossRef] [PubMed]
- Quinlan, P.; Lockton, S.; Irwin, J.; Lucas, A. The relationship between stool hardness and stool composition in breast-and formula-fed infants. J. Pediatr. Gastroenterol. Nutr. 1995, 20, 81–90. [Google Scholar] [CrossRef] [PubMed]
- Turco, R.; Miele, E.; Russo, M.; Mastroianni, R.; Lavorgna, A.; Paludetto, R.; Pensabene, L.; Greco, L.; Campanozzi, A.; Borrelli, O. Early-life factors associated with pediatric functional constipation. J. Pediatr. Gastroenterol. Nutr. 2014, 58, 307–312. [Google Scholar] [CrossRef] [PubMed]
- Mehrotra, V.; Sehgal, S.K.; Bangale, N.R. Fat structure and composition in human milk and infant formulas: Implications in infant health. Clin. Epidemiol. Glob. Health 2019, 7, 153–159. [Google Scholar] [CrossRef]
- Carnielli, V.P.; Luijendijk, I.H.; Van Goudoever, J.B.; Sulkers, E.J.; Boerlage, A.A.; Degenhart, H.J.; Sauer, P.J. Structural position and amount of palmitic acid in infant formulas: Effects on fat, fatty acid, and mineral balance. J. Pediatr. Gastroenterol. Nutr. 1996, 23, 553–560. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, K.; Fewtrell, M.S.; Morley, R.; Abbott, R.; Quinlan, P.T.; Wells, J.C.; Bindels, J.G.; Lucas, A. Double-blind, randomized trial of a synthetic triacylglycerol in formula-fed term infants: Effects on stool biochemistry, stool characteristics, and bone mineralization. Am. J. Clin. Nutr. 1999, 70, 920–927. [Google Scholar] [CrossRef]
- Yao, M.; Lien, E.L.; Capeding, M.R.; Fitzgerald, M.; Ramanujam, K.; Yuhas, R.; Northington, R.; Lebumfacil, J.; Wang, L.; DeRusso, P.A. Effects of term infant formulas containing high sn-2 palmitate with and without oligofructose on stool composition, stool characteristics, and bifidogenicity. J. Pediatr. Gastroenterol. Nutr. 2014, 59, 440. [Google Scholar] [CrossRef] [PubMed]
- Béghin, L.; Marchandise, X.; Lien, E.; Bricout, M.; Bernet, J.-P.; Lienhardt, J.-F.; Jeannerot, F.; Menet, V.; Requillart, J.-C.; Marx, J. Growth, stool consistency and bone mineral content in healthy term infants fed sn-2-palmitate-enriched starter infant formula: A randomized, double-blind, multicentre clinical trial. Clin. Nutr. 2019, 38, 1023–1030. [Google Scholar] [CrossRef] [PubMed]
- Nowacki, J.; Lee, H.-C.; Lien, R.; Cheng, S.-W.; Li, S.-T.; Yao, M.; Northington, R.; Jan, I.; Mutungi, G. Stool fatty acid soaps, stool consistency and gastrointestinal tolerance in term infants fed infant formulas containing high sn-2 palmitate with or without oligofructose: A double-blind, randomized clinical trial. Nutr. J. 2014, 13, 105. [Google Scholar] [CrossRef]
- Litmanovitz, I.; Bar-Yoseph, F.; Lifshitz, Y.; Davidson, K.; Eliakim, A.; Regev, R.H.; Nemet, D. Reduced crying in term infants fed high beta-palmitate formula: A double-blind randomized clinical trial. BMC Pediatr. 2014, 14, 152. [Google Scholar] [CrossRef]

| Nutritional Information (per 100 mL) | Units | PKU Start (Vitaflo) | Standard Infant Formula 1 |
|---|---|---|---|
| Energy | kcal | 68 | 66 |
| kj | 287 | 276 | |
| Protein Equivalent | g | 2.0 | 1.3 |
| Carbohydrate | g | 7.2 | 7.3 |
| of which sugars | g | 0.7 | 7.2 |
| Fat | g | 3.5 | 3.4 |
| Saturated fat | g | 0.9 | 1.1 |
| Polyunsaturated fat | g | 0.6 | 0.6 |
| Linoleic acid | mg | 536 | N/A |
| Docosahexaenoic acid (DHA) | mg | 14 | 16.5 |
| Arachidonic acid (ARA) | mg | 28 | 16.5 |
| Alpha linolenic acid | mg | 48 | N/A |
| Monounsaturated fat | g | 1.8 | 1.7 |
| Vitamins | |||
| Vitamin A | µg | 65 (RE) | 58 |
| Vitamin D | µg | 1.6 | 1.44 |
| Vitamin E | mg αTE | 0.99 | 1.3 |
| Vitamin C | mg | 8.6 | 9.2 |
| Vitamin K | µg | 5.6 | 5.5 |
| Thiamin | mg | 0.06 | 0.07 |
| Riboflavin | mg | 0.07 | 0.13 |
| Niacin | mg | 0.47 | 0.43 |
| Vitamin B6 | mg | 0.06 | 0.05 |
| Folate | µg | 18 | 14 |
| Vitamin B12 | µg | 0.17 | 0.16 |
| Biotin | µg | 2.7 | 1.9 |
| Pantothenic acid | mg | 0.35 | 0.53 |
| Choline | mg | 21 | N/A |
| Minerals | |||
| Sodium | mg | 27 | 23 |
| Potassium | mg | 71 | 86 |
| Chloride | mg | 51 | 51 |
| Calcium | mg | 56 | 50 |
| Phosphorus | mg | 42 | 36 |
| Magnesium | mg | 6.3 | 5.4 |
| Trace Elements | |||
| Iron | mg | 0.82 | 0.53 |
| Copper | mg | 0.06 | 0.05 |
| Zinc | mg | 0.49 | 0.48 |
| Manganese | mg | 0.04 | 0.003 |
| Iodine | µg | 15 | 13 |
| Molybdenum | µg | 2.3 | N/A |
| Selenium | µg | 3.0 | 2.5 |
| Chromium | µg | 2.0 | N/A |
| Amino acids | |||
| Essential amino acids | |||
| Histidine | mg | 80 | 34 |
| Isoleucine | mg | 150 | 75 |
| Leucine | mg | 230 | 136 |
| Lysine | mg | 150 | 119 |
| Methionine | mg | 40 | 33 |
| Phenylalanine | mg | 0 | 55 |
| Threonine | mg | 150 | 64 |
| Tryptophan | mg | 50 | 22 |
| Tyrosine 2 | mg | 220 | 56 |
| Valine | mg | 170 | 81 |
| Non-essential amino acids | |||
| Alanine | mg | 80 | 55 |
| Arginine | mg | 140 | 40 |
| Aspartic acid | mg | 220 | 123 3 |
| Cystine | mg | 50 | 21 |
| Glutamine | mg | 160 | 282 4 |
| Glycine | mg | 210 | 25 |
| Proline | mg | 150 | 116 |
| Serine | mg | 100 | 76 |
| Age | Weight-for-Age z-Scores | Length-for-Age z-Scores | BMI-for-Age z-Scores | |||
|---|---|---|---|---|---|---|
| n | Median (Q1–Q3) | n | Median (Q1–Q3) | n | Median (Q1–Q3) | |
| 0 to 6 months | 224 | −0.3 (−1.3–0.4) | 67 | −0.1 (−1.0–0.5) | 67 | −0.4 (−1.1–0.4) |
| 7 to 12 months | 91 | 0.7 (0.0–1.3) | 38 | 0.3 (−0.5–1.2) | 37 | 1.0 (0.4–1.2) |
| 13 to 24 months | 108 | 0.7 (0.1–1.7) | 56 | 0.0 (−0.7–1.1) | 55 | 1.6 (0.5–2.0) |
| 6 Months (n = 21) 1 Median (Q1–Q3) | 12 Months (n = 24) 1 Median (Q1–Q3) | 24 Months (n = 25) Median (Q1–Q3) | |
|---|---|---|---|
| Energy | |||
| kcal/day | 671 (622–680) | 935 (834–1056) | 1000 (932–1099) |
| EAR % | 105 (98–125) | 126 (114–141) | 106 (94–114) |
| Carbohydrate | |||
| g/day | 77 (73–88) | 117 (102–140) | 138 (123–153) |
| g/kg/day | 11 (10–12) | 11 (10–14) | 10 (9–12) |
| % of energy | 46 (45–47) | 50 (48–54) | 55 (51–59) |
| Fat | |||
| g/day | 30 (26–36) | 33 (28–39) | 31 (27–36) |
| g/kg/day | 4.1 (3.6–5.1) | 3.4 (2.6–4.2) | 2.3 (2.1–2.9) |
| % of energy | 40 (39–42) | 33 (30–36) | 27 (25–34) |
| Total protein | |||
| g/day | 24 (22–25) | 39 (33–42) | 42 (40–45) |
| g/kg/day | 3.3 (3.0–3.5) | 3.8 (3.4–4.1) | 3.3 (3.0–3.6) |
| % of energy | 14 (12–15) | 16 (14–18) | 16 (16–19) |
| Natural protein | |||
| g/day | 4 (4–5) | 5 (5–6) | 6 (5–6) |
| g/kg/day | 0.6 (0.5–0.6) | 0.5 (0.4–0.7) | 0.4 (0.4–0.5) |
| % of energy | 2.5 (1.9–2.8) | 2.1 (2.0–2.7) | 2.2 (1.8–2.6) |
| % of total protein | 19 (15–20) | 14 (11–18) | 13 (11–16) |
| Total protein equivalent from infant and weaning protein substitute | |||
| g/day | 19 (18–22) | 33 (27–36) | 37 (34–41) |
| g/kg/day | 2.7 (2.4–3.0) | 3.3 (2.9–3.6) | 2.8 (2.6–3.2) |
| % of energy | 12 (10–12) | 14 (12–16) | 14 (13–16) |
| % of total protein | 81 (79–85) | 86 (83—89) | 87 (84–89) |
| Recommended intakes (g/kg/day) [1] | 2.0–3.0 | 2.0–3.0 | 1.5–2.0 |
| Contribution from PFIF | |||
| protein equivalent (g/day) | 13 (10–16) | 12 (8–15) | 0 (0–8) |
| protein equivalent (g/kg/day) | 1.8 (1.5–2.2) | 1.2 (0.8–1.6) | 0.0 (0.0–0.6) |
| % of energy | 66 (60–72) | 40 (31–50) | 0 (0–22) |
| % of total protein | 57 (48–66) | 31 (19–41) | 0 (0–17) |
| Contribution from weaning PS | |||
| protein equivalent (g/day) | 6 (4–8) | 22 (15–26) | 32 (30–37) |
| protein equivalent (g/kg/day) | 0.8 (0.6–1.1) | 2.1 (1.5–2.4) | 2.7 (2.3–2.9) |
| % of energy | 6 (5–11) | 19 (16–25) | 29 (24–33) |
| % of total protein | 22 (18–33) | 55 (44–64) | 83 (73–86) |
| Variable | PFIF Discontinued < 24 Months of Age (n = 16) | PFIF Discontinued ≥ 24 Months of Age (n = 9) | p | ||
|---|---|---|---|---|---|
| n | Mean ± SD | n | Mean ± SD | ||
| Blood phenylalanine (µmol/L) | |||||
| 0 to 6 months | 743 | 144 ± 123 | 422 | 159 ± 121 | <0.05 * |
| 7 to 12 months | 624 | 172 ± 117 | 346 | 180 ± 131 | >0.05 |
| 13 to 24 months | 855 | 205 ± 136 | 507 | 178 ± 139 | <0.05 * |
| Variable | Male (n = 12) | Female (n = 13) | p | ||
|---|---|---|---|---|---|
| n | Mean ± SD | n | Mean ± SD | ||
| Weight-for-age z-score | |||||
| 0 to 6 months | 94 | −0.7 + 1.3 | 130 | −0.3 + 1.1 | <0.05 * |
| 7 to 12 months | 44 | 0.5 + 1.4 | 47 | 0.4 + 0.9 | >0.05 |
| 13 to 24 months | 48 | 0.4 + 1.3 | 60 | 0.9 + 0.9 | <0.05 * |
| Length-for-age z-score | |||||
| 0 to 6 months | 30 | −0.2 + 1.1 | 37 | −0.1 + 1.2 | >0.05 |
| 7 to 12 months | 20 | 0.6 + 1.4 | 18 | 0.0 + 1.1 | >0.05 |
| 13 to 24 months | 25 | 0.0 + 1.4 | 31 | −0.1 + 1.2 | >0.05 |
| BMI-for-age z-score | |||||
| 0 to 6 months | 30 | −0.3 + 1.0 | 37 | −0.4 + 1.0 | >0.05 |
| 7 to 12 months | 20 | 0.9 + 1.0 | 17 | 0.3 + 1.1 | >0.05 |
| 13 to 24 months | 25 | 0.9 + 0.9 | 30 | 1.4 + 1.1 | >0.05 |
| Variable | PFIF Discontinued < 24 Months of Age (n = 16) | PFIF Discontinued ≥ 24 Months of Age (n = 9) | p | ||
|---|---|---|---|---|---|
| Number of Assessments | Mean ± SD | Number of Assessments | Mean ± SD | ||
| Weight-for-age z-score | |||||
| 0 to 6 months | 123 | −0.1 ± 1.1 | 101 | −0.9 ± 1.1 | <0.05 * |
| 7 to 12 months | 53 | 0.5 ± 1.2 | 38 | 0.4 ± 1.1 | >0.05 |
| 13 to 24 months | 68 | 0.4 ± 1.1 | 40 | 1.1 ± 1.0 | <0.05 * |
| Length-for-age z-score | |||||
| 0 to 6 months | 34 | 0.0 ± 1.1 | 33 | −0.4 ± 1.2 | >0.05 |
| 7 to 12 months | 24 | 0.3 ± 1.2 | 14 | 0.4 ±1.5 | >0.05 |
| 13 to 24 months | 35 | −0.1 ± 1.2 | 21 | 0.1 ± 1.5 | >0.05 |
| BMI-for-age z-score | |||||
| 0 to 6 months | 34 | −0.1 ± 1.1 | 33 | −0.5 ± 1.3 | >0.05 |
| 7 to 12 months | 23 | 0.5 ± 1.3 | 14 | 0.9 ± 0.5 | >0.05 |
| 13 to 24 months | 35 | 1.0 ± 1.0 | 20 | 1.6 ± 0.9 | <0.05 * |
| Variable | PFIF Discontinued < 24 Months of Age (n = 16) | PFIF Discontinued ≥ 24 Months of Age (n = 9) | p |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| Energy (kcal/day) | |||
| 6 months | 653 ± 86 | 734 ± 101 | >0.05 |
| 12 months | 899 ± 145 | 1013 ± 139 | >0.05 |
| 24 months | 966 ± 79 | 1148 ± 192 | <0.05 * |
| EAR % for energy | |||
| 6 months | 103 ± 13 | 117 ± 17 | >0.05 |
| 12 months | 121 ± 19 | 138 ± 21 | >0.05 |
| 24 months | 100 ± 10 | 120 ± 22 | <0.05 * |
| Carbohydrate (g/day) | |||
| 6 months | 76 ± 8 | 83 ± 10 | >0.05 |
| 12 months | 117 ± 25 | 129 ± 23 | >0.05 |
| 24 months | 136 ± 20 | 147 ± 24 | >0.05 |
| Carbohydrate (g/kg/day) | |||
| 6 months | 10.5 ± 1.4 | 11.3 ± 1.8 | >0.05 |
| 12 months | 11.8 ± 3.3 | 13.8 ± 3.6 | >0.05 |
| 24 months | 10.6 ± 2.2 | 11.4 ± 2.2 | >0.05 |
| Fat (g/day) | |||
| 6 months | 29 ± 5 | 34 ± 6 | >0.05 |
| 12 months | 30 ± 7 | 39 ± 7 | <0.05 * |
| 24 months | 28 ± 5 | 41 ± 13 | <0.05 * |
| Fat (g/kg/day) | |||
| 6 months | 4.0 ± 0.8 | 4.6 ± 0.9 | >0.05 |
| 12 months | 3.1 ± 0.8 | 4.2 ± 1.1 | <0.05 * |
| 24 months | 2.2 ± 0.5 | 3.2 ± 1.1 | <0.05 * |
| Total protein (g/day) | |||
| 6 months | 23 + 4 | 24 + 2 | >0.05 |
| 12 months | 39 ± 5 | 35 ± 5 | >0.05 |
| 24 months | 42 + 7 | 45 + 4 | >0.05 |
| Total protein (g/kg/day) | |||
| 6 months | 3.2 + 0.6 | 3.3 + 0.3 | >0.05 |
| 12 months | 3.9 ± 0.6 | 3.7 ± 0.5 | >0.05 |
| 24 months | 3.3 + 0.5 | 3.5 + 0.5 | >0.05 |
| Natural protein (g/kg/day) | |||
| 6 months | 0.5 + 0.1 | 0.6 + 0.2 | >0.05 |
| 12 months | 0.5 ± 0.1 | 0.6 ± 0.1 | >0.05 |
| 24 months | 0.5 + 0.1 | 0.4 + 0.1 | >0.05 |
| Protein Equivalent (g/kg/day) | |||
| 6 months | 2.7 + 0.6 | 2.7 + 0.4 | >0.05 |
| 12 months | 3.4 ± 0.5 | 3.1 ± 0.5 | >0.05 |
| 24 months | 2.8 + 0.4 | 3.1 + 0.5 | >0.05 |
| Variables | Total | PFIF Discontinued ≥ 24 Months of Age | p |
|---|---|---|---|
| n | n (%) | ||
| Sex | >0.05 | ||
| Male | 12 | 3 (25) | |
| Female | 13 | 6 (46) | |
| Siblings | >0.05 | ||
| 0 | 5 | 2 (40) | |
| 1–2 | 13 | 3 (23) | |
| 3–4 | 7 | 4 (57) | |
| Family size (parents included) | >0.05 | ||
| 2–3 | 5 | 2 (40) | |
| 4–5 | 14 | 5 (36) | |
| 6–7 | 6 | 2 (33) | |
| Parental marital status (n, %) | <0.05 * | ||
| Two parents | 18 | 4 (22) | |
| Single parent 1 | 7 | 5 (71) | |
| Maternal education | >0.05 | ||
| Up to 16 years old only | 13 | 7 (54) | |
| Diploma/Degree | 12 | 2 (17) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yilmaz Nas, O.; Ashmore, C.; Evans, S.; Pinto, A.; Daly, A.; Yabancı Ayhan, N.; MacDonald, A. Phenylalanine-Free Infant Formula in Patients with Phenylketonuria: A Retrospective Study. Nutrients 2024, 16, 2204. https://doi.org/10.3390/nu16142204
Yilmaz Nas O, Ashmore C, Evans S, Pinto A, Daly A, Yabancı Ayhan N, MacDonald A. Phenylalanine-Free Infant Formula in Patients with Phenylketonuria: A Retrospective Study. Nutrients. 2024; 16(14):2204. https://doi.org/10.3390/nu16142204
Chicago/Turabian StyleYilmaz Nas, Ozlem, Catherine Ashmore, Sharon Evans, Alex Pinto, Anne Daly, Nurcan Yabancı Ayhan, and Anita MacDonald. 2024. "Phenylalanine-Free Infant Formula in Patients with Phenylketonuria: A Retrospective Study" Nutrients 16, no. 14: 2204. https://doi.org/10.3390/nu16142204
APA StyleYilmaz Nas, O., Ashmore, C., Evans, S., Pinto, A., Daly, A., Yabancı Ayhan, N., & MacDonald, A. (2024). Phenylalanine-Free Infant Formula in Patients with Phenylketonuria: A Retrospective Study. Nutrients, 16(14), 2204. https://doi.org/10.3390/nu16142204







