Efficacy and Tolerability of a Food Supplement Based on Zea mays L., Gymnema sylvestre (Retz.) R.br.ex Sm, Zinc and Chromium for the Maintenance of Normal Carbohydrate Metabolism: A Monocentric, Randomized, Double-Blind, Placebo-Controlled Clinical Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
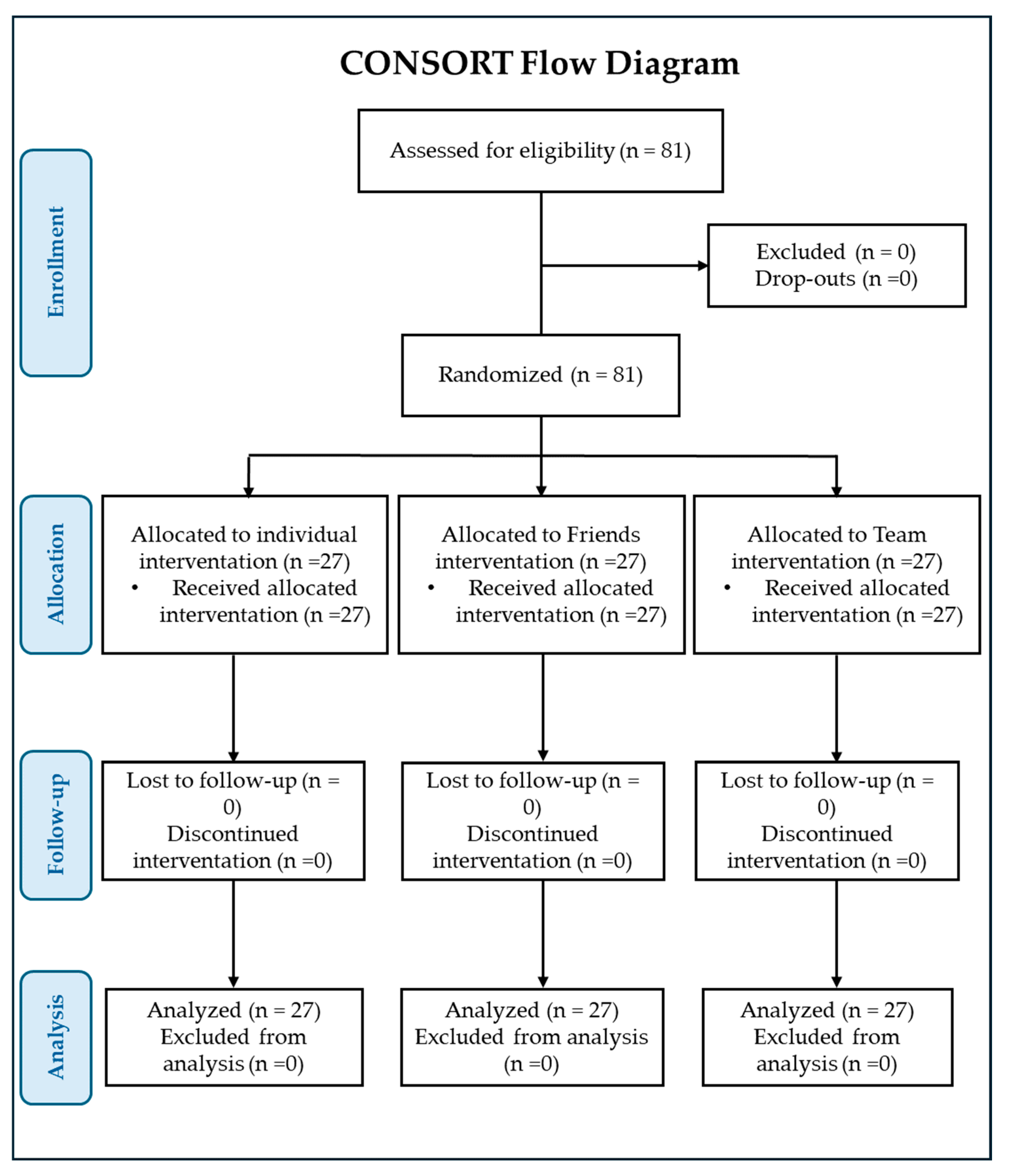
2.2. Clinical Trial Design and Ethical Approval
2.3. Participants and Recruiting Modalities
2.4. Outcome of the Study
2.5. Tolerability
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- De Filippis, A.; Ullah, H.; Baldi, A.; Dacrema, M.; Esposito, C.; Garzarella, E.U.; Santarcangelo, C.; Tantipongpiradet, A.; Daglia, M. Gastrointestinal disorders and metabolic syndrome: Dysbiosis as a key link and common bioactive dietary components useful for their treatment. Int. J. Mol. Sci. 2020, 21, 4929. [Google Scholar] [CrossRef] [PubMed]
- Ullah, H.; De Filippis, A.; Khan, H.; Xiao, J.; Daglia, M. An overview of the health benefits of Prunus species with special reference to metabolic syndrome risk factors. Food Chem. Toxicol. 2020, 144, 111574. [Google Scholar] [CrossRef] [PubMed]
- Ambroselli, D.; Masciulli, F.; Romano, E.; Catanzaro, G.; Besharat, Z.M.; Massari, M.C.; Ferretti, E.; Migliaccio, S.; Izzo, L.; Ritieni, A.; et al. New advances in metabolic syndrome, from prevention to treatment: The role of diet and food. Nutrients 2023, 15, 640. [Google Scholar] [CrossRef]
- Ullah, H.; Sommella, E.; Santarcangelo, C.; D’Avino, D.; Rossi, A.; Dacrema, M.; Minno, A.D.; Di Matteo, G.; Mannina, L.; Campiglia, P.; et al. Hydroethanolic extract of Prunus domestica L.: Metabolite profiling and in vitro modulation of molecular mechanisms associated to cardiometabolic diseases. Nutrients 2022, 14, 340. [Google Scholar] [CrossRef]
- Rochlani, Y.; Pothineni, N.V.; Kovelamudi, S.; Mehta, J.L. Metabolic syndrome: Pathophysiology, management, and modulation by natural compounds. Ther. Adv. Cardiovasc. Dis. 2017, 11, 215–225. [Google Scholar] [CrossRef]
- Castro-Barquero, S.; Ruiz-Leon, A.M.; Sierra-Perez, M.; Estruch, R.; Casas, R. Dietary strategies for metabolic syndrome: A comprehensive review. Nutrients 2020, 12, 2983. [Google Scholar] [CrossRef] [PubMed]
- Harrison, S.; Couture, P.; Lamarche, B. Diet quality, saturated fat and metabolic syndrome. Nutrients 2020, 12, 3232. [Google Scholar] [CrossRef]
- Myers, J.; Kokkinos, P.; Nyelin, E. Physical activity, cardiorespiratory fitness, and the metabolic syndrome. Nutrients 2019, 11, 1652. [Google Scholar] [CrossRef]
- Rask Larsen, J.; Dima, L.; Correll, C.U.; Manu, P. The pharmacological management of metabolic syndrome. Expert. Rev. Clin. Pharmacol. 2018, 11, 397–410. [Google Scholar] [CrossRef]
- Ben Salem, M.; Affes, H.; Ksouda, K.; Dhouibi, R.; Sahnoun, Z.; Hammami, S.; Zeghal, K.M. Pharmacological studies of Artichoke leaf extract and their health benefits. Plant Foods Hum. Nutr. 2015, 70, 441–453. [Google Scholar] [CrossRef]
- Fomenko, E.V.; Chi, Y. Mangiferin modulation of metabolism and metabolic syndrome. Biofactors 2016, 42, 492–503. [Google Scholar] [CrossRef] [PubMed]
- He, L.; Xing, Y.; Ren, X.; Zheng, M.; Yu, S.; Wang, Y.; Xiu, Z.; Dong, Y. Mulberry leaf extract improves metabolic syndrome by alleviating lipid accumulation in vitro and in vivo. Molecules 2022, 27, 5111. [Google Scholar] [CrossRef] [PubMed]
- Roshan, H.; Nikpayam, O.; Sedaghat, M.; Sohrab, G. Effects of green coffee extract supplementation on anthropometric indices, glycaemic control, blood pressure, lipid profile, insulin resistance and appetite in patients with the metabolic syndrome: A randomised clinical trial. Br. J. Nutr. 2018, 119, 250–258. [Google Scholar] [CrossRef] [PubMed]
- Zuniga, L.Y.; Gonzalez-Ortiz, M.; Martinez-Abundis, E. Effect of Gymnema sylvestre administration on metabolic syndrome, insulin sensitivity, and insulin secretion. J. Med. Food 2017, 20, 750–754. [Google Scholar] [CrossRef] [PubMed]
- Panchal, S.K.; Wanyonyi, S.; Brown, L. Selenium, vanadium, and chromium as micronutrients to improve metabolic syndrome. Curr. Hypertens. Rep. 2017, 19, 10. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y.; Zou, Y.; Shen, Z.; Xiong, Y.; Zhang, W.; Liu, C.; Chen, S. Trace elements, PPARs, and metabolic syndrome. Int. J. Mol. Sci. 2020, 21, 2612. [Google Scholar] [CrossRef] [PubMed]
- Ferron, L.; Colombo, R.; Mannucci, B.; Papetti, A. A New Italian purple corn variety (Moradyn) byproduct extract: Antiglycative and hypoglycemic in vitro activities and preliminary bioaccessibility studies. Molecules 2020, 25, 1958. [Google Scholar] [CrossRef] [PubMed]
- Amin, E.; Abdel-Bakky, M.S.; Darwish, M.A.; Mohammed, H.A.; Chigurupati, S.; Qureshi, K.A.; Hassan, M.H.A. The glycemic control potential of some Amaranthaceae plants, with particular reference to in vivo antidiabetic potential of Agathophora alopecuroides. Molecules 2022, 27, 973. [Google Scholar] [CrossRef] [PubMed]
- Qiu, Q.; Zhen, H.S.; Wei, Y.F.; Zhen, D.D. Research progress on effective substance and quality analysis of Gymnema sylvestre(Retz.) schult. Chin. J. Ethnomed. Ethnopharm. 2017, 26, 51–53. [Google Scholar]
- Devangan, S.; Varghese, B.; Johny, E.; Gurram, S.; Adela, R. The effect of Gymnema sylvestre supplementation on glycemic control in type 2 diabetes patients: A systematic review and meta-analysis. Phytother. Res. 2021, 35, 6802–6812. [Google Scholar] [CrossRef]
- Pothuraju, R.; Sharma, R.K.; Chagalamarri, J.; Jangra, S.; Kumar Kavadi, P. A systematic review of Gymnema sylvestre in obesity and diabetes management. J. Sci. Food Agric. 2014, 94, 834–840. [Google Scholar] [CrossRef] [PubMed]
- Muzaffar, H.; Qamar, I.; Bashir, M.; Jabeen, F.; Irfan, S.; Anwar, H. Gymnema sylvestre supplementation restores normoglycemia, corrects dyslipidemia, and transcriptionally modulates pancreatic and hepatic gene expression in alloxan-induced hyperglycemic rats. Metabolites 2023, 13, 516. [Google Scholar] [CrossRef] [PubMed]
- Bhansali, S.; Shafiq, N.; Pandhi, P.; Singh, A.P.; Singh, I.; Singh, P.K.; Sharma, S.; Malhotra, S. Effect of a deacyl gymnemic acid on glucose homeostasis & metabolic parameters in a rat model of metabolic syndrome. Indian J. Med. Res. 2013, 137, 1174–1179. [Google Scholar] [PubMed]
- Tamura, Y. The role of zinc homeostasis in the prevention of diabetes mellitus and cardiovascular diseases. J. Atheroscler. Thromb. 2021, 28, 1109–1122. [Google Scholar] [CrossRef] [PubMed]
- Bjorklund, G.; Dadar, M.; Pivina, L.; Dosa, M.D.; Semenova, Y.; Aaseth, J. The role of zinc and copper in insulin resistance and diabetes mellitus. Curr. Med. Chem. 2020, 27, 6643–6657. [Google Scholar] [CrossRef]
- Cruz, K.J.C.; de Oliveira, A.R.S.; Morais, J.B.S.; Severo, J.S.; Mendes, P.M.V.; de Sousa Melo, S.R.; de Sousa, G.S.; Marreiro, D.D.N. Zinc and insulin resistance: Biochemical and molecular aspects. Biol. Trace Elem. Res. 2018, 186, 407–412. [Google Scholar] [CrossRef]
- Morais, J.B.S.; Severo, J.S.; Beserra, J.B.; de Oiveira, A.R.S.; Cruz, K.J.C.; de Sousa Melo, S.R.; do Nascimento, G.V.R.; de Macedo, G.F.S.; do Nascimento Marreiro, D. Association between cortisol, insulin resistance and zinc in obesity: A mini-review. Biol. Trace Elem. Res. 2019, 191, 323–330. [Google Scholar] [CrossRef]
- Jeejeebhoy, K.N.; Chu, R.C.; Marliss, E.B.; Greenberg, G.R.; Bruce-Robertson, A. Chromium deficiency, glucose intolerance, and neuropathy reversed by chromium supplementation, in a patient receiving long-term total parenteral nutrition. Am. J. Clin. Nutr. 1977, 30, 531–538. [Google Scholar] [CrossRef]
- Vincent, J.B. Effects of chromium supplementation on body composition, human and animal health, and insulin and glucose metabolism. Curr. Opin. Clin. Nutr. Metab. Care 2019, 22, 483–489. [Google Scholar] [CrossRef]
- Directive, E.U. Directive 2002/46/EC of the European Parliament and of the Council of 10 June 2002 on the approximation of the laws of the Member States relating to food supplements. Off. J. Eur. Communities Legis. 2002, 45, 51–57. [Google Scholar]
- Calvert, M.; Blazeby, J.; Altman, D.G.; Revicki, D.A.; Moher, D.; Brundage, M.D.; Group, C.P. Reporting of patient-reported outcomes in randomized trials: The CONSORT PRO extension. JAMA 2013, 309, 814–822. [Google Scholar] [CrossRef] [PubMed]
- Myette-Côté, É.; Durrer, C.; Neudorf, H.; Bammert, T.D.; Botezelli, J.D.; Johnson, J.D.; DeSouza, C.A.; Little, J.P. The effect of a short-term low-carbohydrate, high-fat diet with or without postmeal walks on glycemic control and inflammation in type 2 diabetes: A randomized trial. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2018, 315, R1210–R1219. [Google Scholar] [CrossRef]
- Rosen, E.D. Epigenomic and transcriptional control of insulin resistance. J. Intern. Med. 2016, 280, 443–456. [Google Scholar] [CrossRef] [PubMed]
- Yeh, G.Y.; Eisenberg, D.M.; Kaptchuk, T.J.; Phillips, R.S. Systematic review of herbs and dietary supplements for glycemic control in diabetes. Diabetes Care 2003, 26, 1277–1294. [Google Scholar] [CrossRef] [PubMed]
- El-Shafey, A.; El-Ezabi, M.; Selim, M.; Ouda, H.; Ibrahim, D. Effect of Gymnema sylvestre R. Br. leaves extract on certain physiological parameters of diabetic rats. J. King Saud Univ. Sci. 2013, 25, 135–141. [Google Scholar] [CrossRef]
- Liu, B.; Asare-Anane, H.; Al-Romaiyan, A.; Huang, G.; Amiel, S.A.; Jones, P.M.; Persaud, S.J. Characterisation of the insulinotropic activity of an aqueous extract of Gymnema sylvestre in mouse beta-cells and human islets of Langerhans. Cell. Physiol. Biochem. 2009, 23, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Baskaran, K.; Kizar Ahamath, B.; Radha Shanmugasundaram, K.; Shanmugasundaram, E.R. Antidiabetic effect of a leaf extract from Gymnema sylvestre in non-insulin-dependent diabetes mellitus patients. J. Ethnopharmacol. 1990, 30, 295–300. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.N.; Mani, U.V.; Mani, I. An open label study on the supplementation of Gymnema sylvestre in type 2 diabetics. J. Diet. Suppl. 2010, 7, 273–282. [Google Scholar] [CrossRef]
- Gaytan Martinez, L.A.; Sanchez-Ruiz, L.A.; Zuniga, L.Y.; Gonzalez-Ortiz, M.; Martinez-Abundis, E. Effect of Gymnema sylvestre administration on glycemic control, insulin secretion, and insulin sensitivity in patients with impaired glucose tolerance. J. Med. Food 2021, 24, 28–32. [Google Scholar] [CrossRef]
- Wang, X.; Wu, W.; Zheng, W.; Fang, X.; Chen, L.; Rink, L.; Min, J.; Wang, F. Zinc supplementation improves glycemic control for diabetes prevention and management: A systematic review and meta-analysis of randomized controlled trials. Am. J. Clin. Nutr. 2019, 110, 76–90. [Google Scholar] [CrossRef]
- Hamedifard, Z.; Farrokhian, A.; Reiner, Z.; Bahmani, F.; Asemi, Z.; Ghotbi, M.; Taghizadeh, M. The effects of combined magnesium and zinc supplementation on metabolic status in patients with type 2 diabetes mellitus and coronary heart disease. Lipids Health Dis. 2020, 19, 112. [Google Scholar] [CrossRef] [PubMed]
- Barman, S.; Srinivasan, K. Diabetes and zinc dyshomeostasis: Can zinc supplementation mitigate diabetic complications? Crit. Rev. Food Sci. Nutr. 2022, 62, 1046–1061. [Google Scholar] [CrossRef]
- Bai, J.; Xun, P.; Morris, S.; Jacobs, D.R., Jr.; Liu, K.; He, K. Chromium exposure and incidence of metabolic syndrome among American young adults over a 23-year follow-up: The CARDIA trace element study. Sci. Rep. 2015, 5, 15606. [Google Scholar] [CrossRef] [PubMed]
- Khodavirdipour, A.; Haddadi, F.; Keshavarzi, S. Chromium supplementation; negotiation with diabetes mellitus, hyperlipidemia and depression. J. Diabetes Metab. Disord. 2020, 19, 585–595. [Google Scholar] [CrossRef]
- Luna-Vital, D.; Luzardo-Ocampo, I.; Cuellar-Nunez, M.L.; Loarca-Pina, G.; Gonzalez de Mejia, E. Maize extract rich in ferulic acid and anthocyanins prevents high-fat-induced obesity in mice by modulating SIRT1, AMPK and IL-6 associated metabolic and inflammatory pathways. J. Nutr. Biochem. 2020, 79, 108343. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.H.; Garcia, H.S.; Parkin, K.L. Bioactivities of kernel extracts of 18 strains of maize (Zea mays). J. Food Sci. 2010, 75, C667–C672. [Google Scholar] [CrossRef]
- Luna-Vital, D.; Weiss, M.; Gonzalez de Mejia, E. Anthocyanins from purple corn ameliorated tumor necrosis factor-alpha-induced inflammation and insulin resistance in 3T3-L1 adipocytes via activation of insulin signaling and enhanced GLUT4 translocation. Mol. Nutr. Food Res. 2017, 61, 1700362. [Google Scholar] [CrossRef]
- Luna-Vital, D.A.; Gonzalez de Mejia, E. Anthocyanins from purple corn activate free fatty acid-receptor 1 and glucokinase enhancing in vitro insulin secretion and hepatic glucose uptake. PLoS ONE 2018, 13, e0200449. [Google Scholar] [CrossRef]
- Hong, S.H.; Heo, J.I.; Kim, J.H.; Kwon, S.O.; Yeo, K.M.; Bakowska-Barczak, A.M.; Kolodziejczyk, P.; Ryu, O.H.; Choi, M.K.; Kang, Y.H.; et al. Antidiabetic and beta cell-protection activities of purple corn anthocyanins. Biomol. Ther. 2013, 21, 284–289. [Google Scholar] [CrossRef] [PubMed]
- Kang, M.K.; Li, J.; Kim, J.L.; Gong, J.H.; Kwak, S.N.; Park, J.H.; Lee, J.Y.; Lim, S.S.; Kang, Y.H. Purple corn anthocyanins inhibit diabetes-associated glomerular monocyte activation and macrophage infiltration. Am. J. Physiol. Renal Physiol. 2012, 303, F1060–F1069. [Google Scholar] [CrossRef]
- Colombo, R.; Ferron, L.; Papetti, A. Colored corn: An up-date on metabolites extraction, health implication, and potential use. Molecules 2021, 26, 199. [Google Scholar] [CrossRef] [PubMed]
- Chayati, I.; Sunarti, S.; Marsono, Y.; Astuti, M. Anthocyanin extract of purple corn improves hyperglycemia and insulin resistance of rats fed high fat and fructose diet via GLP1 and GLP1R mechanism. J. Food Nutr. Res. 2019, 7, 303–310. [Google Scholar] [CrossRef]
- Huang, B.; Wang, Z.; Park, J.H.; Ryu, O.H.; Choi, M.K.; Lee, J.Y.; Kang, Y.H.; Lim, S.S. Anti-diabetic effect of purple corn extract on C57BL/KsJ db/db mice. Nutr. Res. Pract. 2015, 9, 22–29. [Google Scholar] [CrossRef] [PubMed]
- Tsuda, T.; Horio, F.; Uchida, K.; Aoki, H.; Osawa, T. Dietary cyanidin 3-O-beta-D-glucoside-rich purple corn color prevents obesity and ameliorates hyperglycemia in mice. J. Nutr. 2003, 133, 2125–2130. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Kang, M.K.; Kim, J.K.; Kim, J.L.; Kang, S.W.; Lim, S.S.; Kang, Y.H. Purple corn anthocyanins retard diabetes-associated glomerulosclerosis in mesangial cells and db/db mice. Eur. J. Nutr. 2012, 51, 961–973. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Lim, S.S.; Lee, J.Y.; Kim, J.K.; Kang, S.W.; Kim, J.L.; Kang, Y.H. Purple corn anthocyanins dampened high-glucose-induced mesangial fibrosis and inflammation: Possible renoprotective role in diabetic nephropathy. J. Nutr. Biochem. 2012, 23, 320–331. [Google Scholar] [CrossRef] [PubMed]
- Thiraphatthanavong, P.; Wattanathorn, J.; Muchimapura, S.; Wipawee, T.M.; Wannanon, P.; Terdthai, T.U.; Suriharn, B.; Lertrat, K. Preventive effect of Zea mays L. (purple waxy corn) on experimental diabetic cataract. Biomed. Res. Int. 2014, 2014, 507435. [Google Scholar] [CrossRef] [PubMed]
- Thiraphatthanavong, P.; Wattanathorn, J.; Muchimapura, S.; Thukham-mee, W.; Lertrat, K.; Suriharn, B. The combined extract of purple waxy corn and ginger prevents cataractogenesis and retinopathy in streptozotocin-diabetic rats. Oxid. Med. Cell. Longev. 2014, 2014, 789406. [Google Scholar] [CrossRef]
- Kang, M.K.; Lim, S.S.; Lee, J.Y.; Yeo, K.M.; Kang, Y.H. Anthocyanin-rich purple corn extract inhibit diabetes-associated glomerular angiogenesis. PLoS ONE 2013, 8, e79823. [Google Scholar] [CrossRef]
- Intuyod, K.; Priprem, A.; Limphirat, W.; Charoensuk, L.; Pinlaor, P.; Pairojkul, C.; Lertrat, K.; Pinlaor, S. Anti-inflammatory and anti-periductal fibrosis effects of an anthocyanin complex in Opisthorchis viverrini-infected hamsters. Food Chem. Toxicol. 2014, 74, 206–215. [Google Scholar] [CrossRef]
- Chuntakaruk, H.; Kongtawelert, P.; Pothacharoen, P. Chondroprotective effects of purple corn anthocyanins on advanced glycation end products induction through suppression of NF-kappaB and MAPK signaling. Sci. Rep. 2021, 11, 1895. [Google Scholar] [CrossRef] [PubMed]
- Tomay, F.; Marinelli, A.; Leoni, V.; Caccia, C.; Matros, A.; Mock, H.P.; Tonelli, C.; Petroni, K. Purple corn extract induces long-lasting reprogramming and M2 phenotypic switch of adipose tissue macrophages in obese mice. J. Transl. Med. 2019, 17, 237. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.; Guo, X.; Zhang, M.; Yang, L.; Liu, R.; Yin, J. Anthocyanins in black rice, soybean and purple corn increase fecal butyric acid and prevent liver inflammation in high fat diet-induced obese mice. Food Funct. 2017, 8, 3178–3186. [Google Scholar] [CrossRef] [PubMed]
- Hyunchae, J.; Chai-hee, K.; Yejoo, L.; Soon-kwon, K.; Myoung-Sool, D. Anti-diabetic and anti-inflammatory effects of purple corn extract in high-fat diet induced obesity mice. Korean J. Food Nutr. 2017, 30, 696–702. [Google Scholar]
- Xu, H.; Liu, M.; Liu, H.; Zhao, B.; Zheng, M.; Liu, J. Anthocyanins from purple corn ameliorated obesity in high fat diet-induced obese mice through activating hepatic AMPK. J. Funct. Foods 2021, 84, 104582. [Google Scholar] [CrossRef]
- Izutani, Y.; Murai, T.; Imoto, T.; Ohnishi, M.; Oda, M.; Ishijima, S. Gymnemic acids inhibit rabbit glyceraldehyde-3-phosphate dehydrogenase and induce a smearing of its electrophoretic band and dephosphorylation. FEBS Lett. 2005, 43, 33–36. [Google Scholar] [CrossRef]
- Di Fabio, G.; Romanucci, V.; De Marco, A.; Zarrelli, A. Triterpenoids from Gymnema sylvestre and their pharmacological activities. Molecules 2014, 19, 10956–10981. [Google Scholar] [CrossRef] [PubMed]
- Renga, B.; Festa, C.; De Marino, S.; Di Micco, S.; D’Auria, M.V.; Bifulco, G.; Fiorucci, S.; Zampella, A. Molecular decodification of gymnemic acids from Gymnema sylvestre. Discovery of a new class of liver X receptor antagonists. Steroids 2015, 96, 121–131. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Sun, M.; Liu, Y.; Liang, J.; Wang, T.; Zhang, Z. Gymnemic acid alleviates type 2 diabetes mellitus and suppresses endoplasmic reticulum stress in vivo and in vitro. J. Agric. Food Chem. 2019, 67, 3662–3669. [Google Scholar] [CrossRef]
- Li, Y.; Xiao, Y.; Gao, W.; Pan, J.; Zhao, Q.; Zhang, Z. Gymnemic acid alleviates inflammation and insulin resistance via PPARδ- and NFκB-mediated pathways in db/db mice. Food Funct. 2019, 10, 5853–5862. [Google Scholar] [CrossRef]

| Characteristics of Enrolled Subjects | Group 1 (n = 27) | Group 2 (n = 27) | Group 3 (n = 27) |
|---|---|---|---|
Ethnicity
| 27 | 27 | 27 |
Gender
| 13 14 | 13 14 | 12 15 |
Age (years)
| 50.5 ± 11.1 54.3 ± 11.5 | 51.6 ± 13.2 53.8 ± 15.6 | 52.8 ± 14.0 57.5 ± 10.8 |
| Mean age (years, range) | 52.5 ± 13.4 (37–69) | 52.5 ± 15.1 (34–68) | 53.5 ± 14.1 (35–68) |
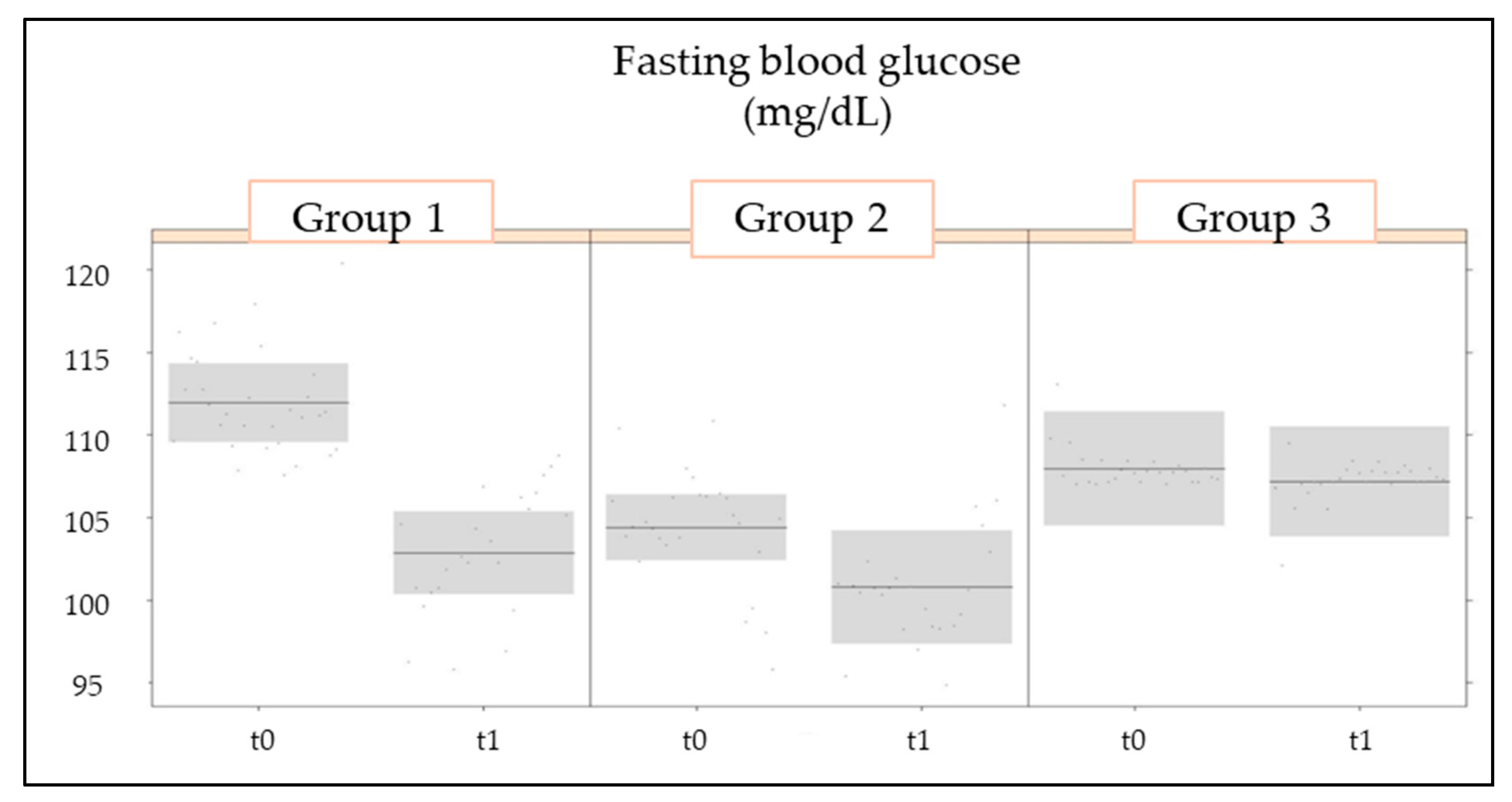
| Fasting glucose (mg/dL) (Range) | 111.9 ± 16.5 (98–125) | 104.4 ± 8.9 (98–121) | 108.9 ± 8.0 (98–122) |
| Variable | Group 1 | Group 2 | Group 3 | |||
|---|---|---|---|---|---|---|
| t0 | t1 | t0 | t1 | t0 | t1 | |
| FBG (mg/dL) | 111.9 ± 16.5 (98–125) | 100.2 ± 12.5 (78–125) | 104.4 ± 8.9 (89–121) | 100 ± 8.8 (92–125) | 108 ± 8 (98–122) | 107.2 ± 8.2 (96–124) |
| HbA1c (%) | 5.9 ± 0.6 (5–8) | 5.7 ± 0.4 (5–6.2) | 5.8 ± 0.3 (5.2–6.4) | 5.8 ± 0.3 (5–6.3) | 5.7 ± 0.3 (5.1–6.2) | 5.7 ± 0.3 (5.1–6.2) |
| INS (pmol/L) | 13.2 ± 7.6 (2.3–42) | 12.6 ± 5.7 (2.3–21.4) | 9.7 ± 5.7 (2.6–22.5) | 8.8 ± 5 (3.2–22.9) | 10.4 ± 5.6 (3.5–21.5) | 10 ± 5.3 (3.5–22) |
| HOMA-IR | 3.6 ± 1.9 (0.6–10.9) | 3.2 ± 1.4 (0.6–5.4) | 2.6 ± 1.7 (0.8–6.4) | 2.2 ± 1.4 (0.8–6) | 2.8 ± 1.6 (0.8–6.5) | 2.7 ± 1.5 (0.8–6.7) |
| BMI (kg/m2) | 24.8 ± 4.6 (18–35.6) | 23.7 ± 4 (18–32.3) | 24.1 ± 3.7 (18–33.3) | 23.6 ± 3.2 (18–30) | 21.8 ± 2.9 (17–26) | 21.7 ± 2.8 (17–26) |
| TC (mg/dL) | 208.1 ± 33.1 (125–261) | 200.2 ± 28.1 (122–254) | 218.8 ± 37.6 (130–280) | 206.4 ± 33 (125–260) | 223.9 ± 21.5 (178–256) | 223.4 ± 21.4 (190–260) |
| LDL-C (mg/dL) | 105.3 ± 22 (60–172) | 99.1 ± 21.2 (79–164) | 105.6 ± 27.9 (73–221) | 96.2 ± 12.2 (63–123) | 105.3 ± 16.1 (79–145) | 107.7 ± 18.9 (83–151) |
| HDL-C (mg/dL) | 45.8 ± 10.4 (23–65) | 48.3 ± 12.6 (24–70) | 54.4 ± 13.4 (34–83) | 56.2 ± 15.1 (35–87) | 50 ± 8.9 (35–67) | 50.7 ± 9.5 (34–69) |
| TG (mg/dL) | 162.6 ± 48.6 (4.8–257) | 180.4 ± 61.3 (67–349) | 146.2 ± 45 (35–190) | 141 ± 45.2 (40–185) | 170.4 ± 14 (143–190) | 167.8 ± 15.9 (139–200) |
| AST (mg/dL) | 22.9 ± 8.3 (5–40) | 23 ± 7.5 (13–38) | 22.6 ± 5.3 (16–33) | 23.7 ± 4.7 (16–32) | 25.6 ± 4.3 (18–37) | 26.6 ± 4.9 (18–40) |
| ALT (U/L) | 27.2 ± 8.2 (12–41) | 28.6 ± 7.5 (11–41) | 27.7 ± 8.8 (11–44) | 30 ± 10.4 (12–45) | 32.3 ± 5.1 (21–41) | 32.1 ± 4.9 (22–41) |
| CRE (mg/dL) | 1 ± 0.2 (0.7–1.3) | 5.4 ± 20.9 (0.8–101.3) | 1 ± 0.2 (0.6–1.3) | 1 ± 0.1 (0.7–1.2) | 1.1 ± 0.1 (0.9–1.2) | 1.1 ± 0.1 (0.9–1.3) |
| Variable | Model | Num | Den | F | p |
|---|---|---|---|---|---|
| FBG | Measurement | 1 | 68 | 44.367 | <0.001 |
| Group | 2 | 76 | 1.507 | 0.228 | |
| Group for measure | 2 | 68 | 13.089 | <0.001 | |
| HbA1c | Measurement | 1 | 70 | 7.850 | 0.007 |
| Group | 2 | 78 | 0.621 | 0.540 | |
| Group for measure | 2 | 70 | 5.565 | 0.006 | |
| INS | Measurement | 1 | 67 | 0.635 | 0.428 |
| Group | 2 | 73 | 3.641 | 0.031 | |
| Group for measure | 2 | 67 | 0.117 | 0.890 | |
| HOMA-IR | Measurement | 1 | 68 | 2.162 | 0.146 |
| Group | 2 | 73 | 3.586 | 0.033 | |
| Group for measure | 2 | 68 | 0.281 | 0.756 | |
| BMI | Measurement | 1 | 71 | 4.811 | 0.032 |
| Group | 2 | 80 | 4.839 | 0.010 | |
| Group for measure | 2 | 71 | 1.632 | 0.203 | |
| TC | Measurement | 1 | 71 | 9.111 | 0.004 |
| Group | 2 | 77 | 4.412 | 0.015 | |
| Group for measure | 2 | 71 | 2.149 | 0.124 | |
| LDL-C | Measurement | 1 | 70 | 3.069 | 0.084 |
| Group | 2 | 76 | 0.654 | 0.523 | |
| Group for measure | 2 | 70 | 2.421 | 0.096 | |
| HDL-C | Measurement | 1 | 72 | 5.778 | 0.019 |
| Group | 2 | 81 | 3.564 | 0.033 | |
| Group for measure | 2 | 72 | 0.672 | 0.514 | |
| TG | Measurement | 1 | 73 | 0.188 | 0.666 |
| Group | 2 | 80 | 3.619 | 0.031 | |
| Group for measure | 2 | 73 | 2.105 | 0.129 | |
| AST | Measurement | 1 | 72 | 0.469 | 0.496 |
| Group | 2 | 80 | 3.336 | 0.041 | |
| Group for measure | 2 | 72 | 1.892 | 0.158 | |
| ALT | Measurement | 1 | 73 | 0.747 | 0.390 |
| Group | 2 | 79 | 3.692 | 0.029 | |
| Group for measure | 2 | 73 | 1.031 | 0.362 | |
| CRE | Measurement | 1 | 82 | 1.324 | 0.253 |
| Group | 2 | 82 | 1.295 | 0.279 | |
| Group for measure | 2 | 82 | 1.313 | 0.275 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Buccato, D.G.; Ullah, H.; De Lellis, L.F.; Morone, M.V.; Larsen, D.S.; Di Minno, A.; Cordara, M.; Piccinocchi, R.; Baldi, A.; Greco, A.; et al. Efficacy and Tolerability of a Food Supplement Based on Zea mays L., Gymnema sylvestre (Retz.) R.br.ex Sm, Zinc and Chromium for the Maintenance of Normal Carbohydrate Metabolism: A Monocentric, Randomized, Double-Blind, Placebo-Controlled Clinical Trial. Nutrients 2024, 16, 2459. https://doi.org/10.3390/nu16152459
Buccato DG, Ullah H, De Lellis LF, Morone MV, Larsen DS, Di Minno A, Cordara M, Piccinocchi R, Baldi A, Greco A, et al. Efficacy and Tolerability of a Food Supplement Based on Zea mays L., Gymnema sylvestre (Retz.) R.br.ex Sm, Zinc and Chromium for the Maintenance of Normal Carbohydrate Metabolism: A Monocentric, Randomized, Double-Blind, Placebo-Controlled Clinical Trial. Nutrients. 2024; 16(15):2459. https://doi.org/10.3390/nu16152459
Chicago/Turabian StyleBuccato, Daniele Giuseppe, Hammad Ullah, Lorenza Francesca De Lellis, Maria Vittoria Morone, Danaé S. Larsen, Alessandro Di Minno, Marcello Cordara, Roberto Piccinocchi, Alessandra Baldi, Agostino Greco, and et al. 2024. "Efficacy and Tolerability of a Food Supplement Based on Zea mays L., Gymnema sylvestre (Retz.) R.br.ex Sm, Zinc and Chromium for the Maintenance of Normal Carbohydrate Metabolism: A Monocentric, Randomized, Double-Blind, Placebo-Controlled Clinical Trial" Nutrients 16, no. 15: 2459. https://doi.org/10.3390/nu16152459
APA StyleBuccato, D. G., Ullah, H., De Lellis, L. F., Morone, M. V., Larsen, D. S., Di Minno, A., Cordara, M., Piccinocchi, R., Baldi, A., Greco, A., Santonastaso, S., Sacchi, R., & Daglia, M. (2024). Efficacy and Tolerability of a Food Supplement Based on Zea mays L., Gymnema sylvestre (Retz.) R.br.ex Sm, Zinc and Chromium for the Maintenance of Normal Carbohydrate Metabolism: A Monocentric, Randomized, Double-Blind, Placebo-Controlled Clinical Trial. Nutrients, 16(15), 2459. https://doi.org/10.3390/nu16152459







