Adherence to the Mediterranean Diet Mitigates Inflammation and Hospital Stay in Frail Elderly Patients: A Moderation Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Biochemical Analysis and Data Collection
2.3. Assessment of Nutritional Status and Adherence to the Mediterranean Diet
2.4. Frailty Assessment
- Weight Loss: The unintentional loss of more than 4.5 kg in the last year or a ≥5% loss of body weight in the previous year.
- Exhaustion: Measured using the CES-D Depression Scale, identified by the answers, “I felt that everything I did was an effort” and “I could not get going”.
- Physical Activity: Evaluated using the short version of the Minnesota Leisure Time Activity questionnaire, with a weighted physical activity score calculated for each gender and kilocalories expended per week determined.
- Walking Time: Based on the time required to walk 4.57 m (15 feet), adjusted for gender and standing height.
- Grip Strength: Stratified by gender and BMI quartiles.
2.5. Statistical Analysis
3. Results
3.1. Characteristics of the Population
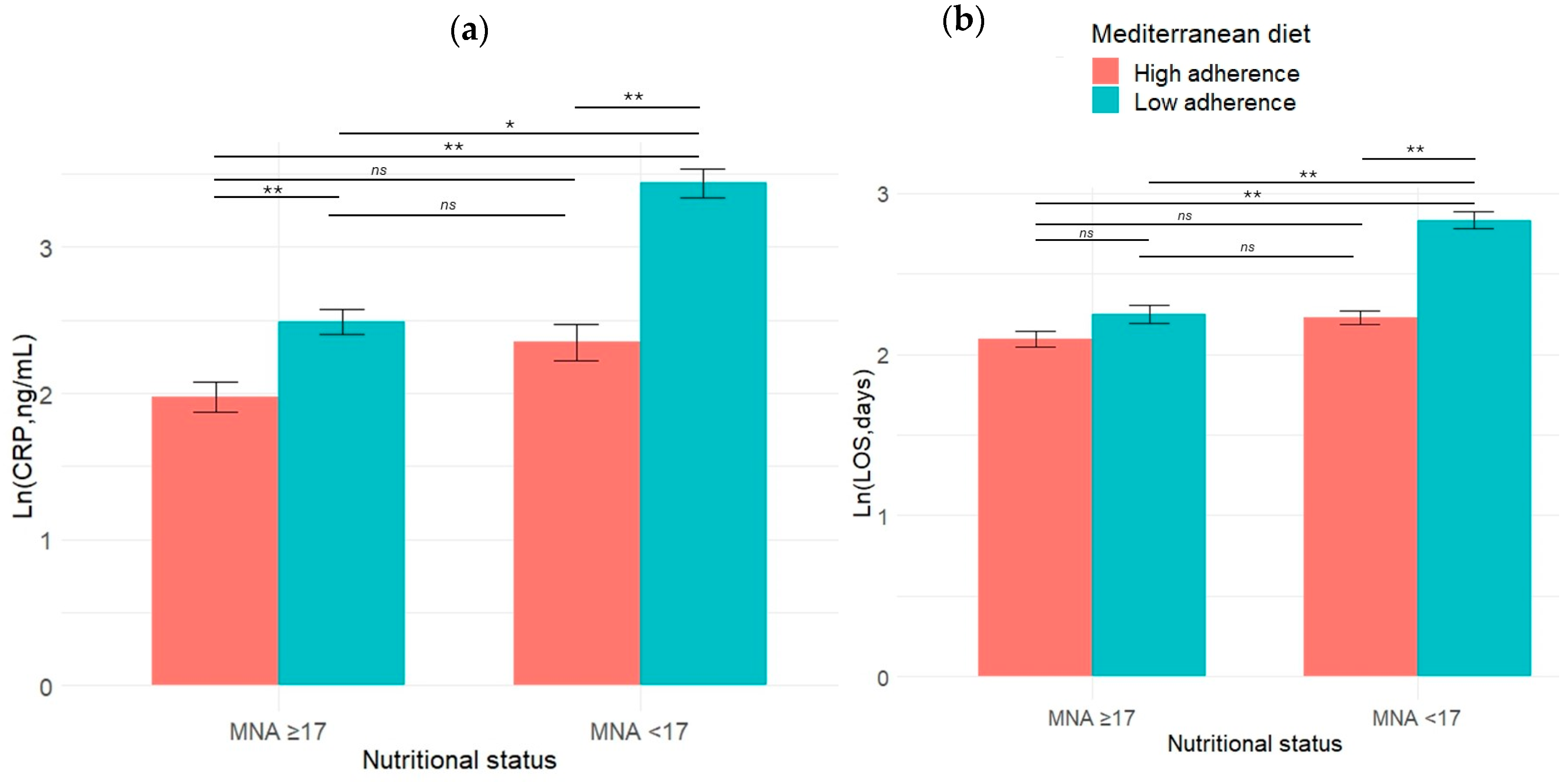
3.2. Two-Way ANOVA Analysis: Impact of Nutritional Status and Mediterranean Diet Adherence
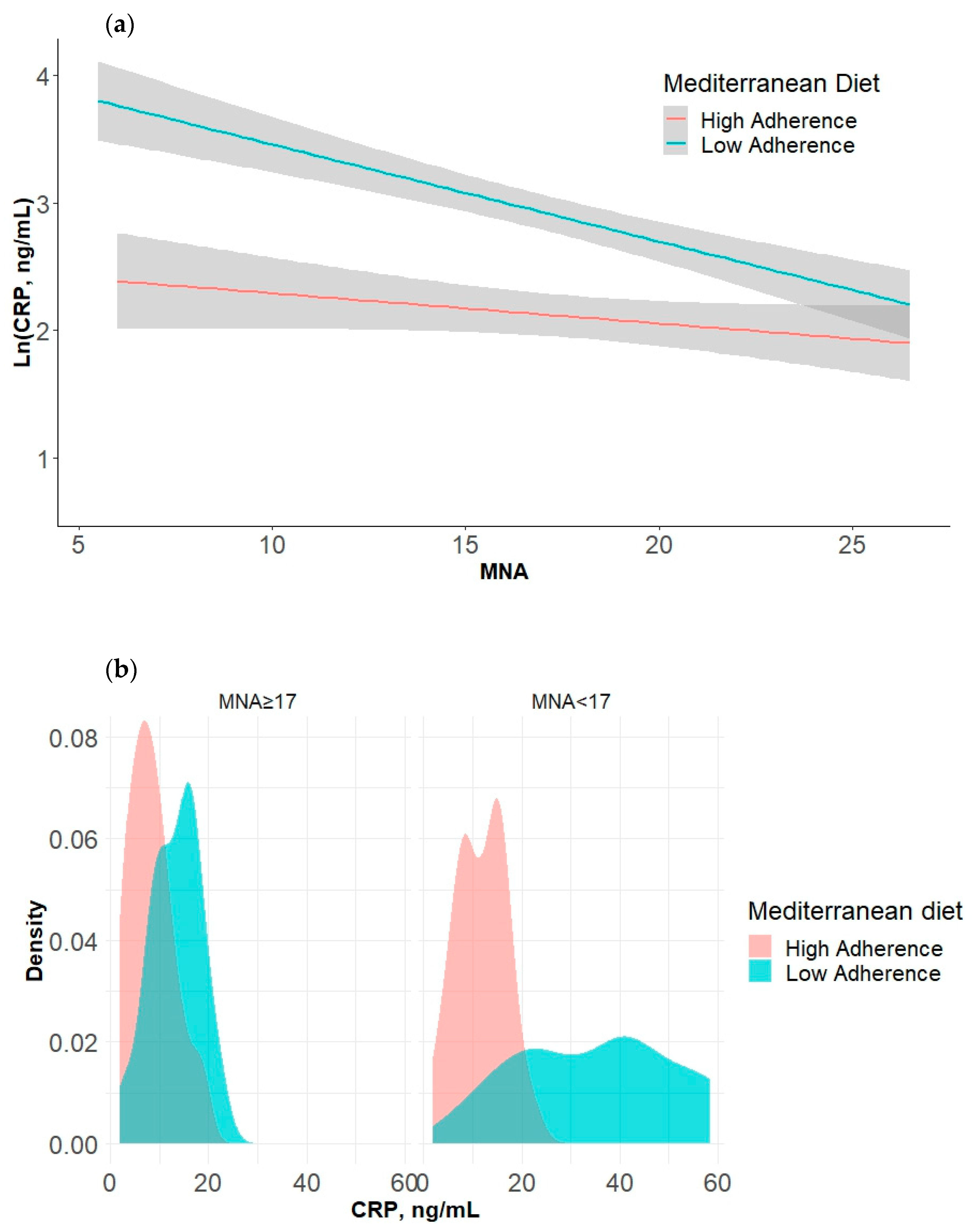
3.3. Moderation Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Norman, K.; Haß, U.; Pirlich, M. Malnutrition in Older Adults—Recent Advances and Remaining Challenges. Nutrients 2021, 13, 2764. [Google Scholar] [CrossRef] [PubMed]
- Kabashneh, S.; Alkassis, S.; Shanah, L.; Ali, H. A Complete Guide to Identify and Manage Malnutrition in Hospitalized Patients. Cureus 2020, 12, e8486. [Google Scholar] [CrossRef] [PubMed]
- Dent, E.; Wright, O.R.L.; Woo, J.; Hoogendijk, E.O. Malnutrition in Older Adults. Lancet 2023, 401, 951–966. [Google Scholar] [CrossRef] [PubMed]
- Lo Buglio, A.; Bellanti, F.; Capurso, C.; Vendemiale, G. Controlling Nutritional Status (CONUT) Score as a Predictive Marker in Hospitalized Frail Elderly Patients. J. Pers. Med. 2023, 13, 1119. [Google Scholar] [CrossRef] [PubMed]
- Lengfelder, L.; Mahlke, S.; Moore, L.; Zhang, X.; Williams, G.; Lee, J. Prevalence and Impact of Malnutrition on Length of Stay, Readmission, and Discharge Destination. J. Parenter. Enter. Nutr. 2022, 46, 1335–1342. [Google Scholar] [CrossRef] [PubMed]
- Lo Buglio, A.; Bellanti, F.; Capurso, C.; Paglia, A.; Vendemiale, G. Adherence to Mediterranean Diet, Malnutrition, Length of Stay and Mortality in Elderly Patients Hospitalized in Internal Medicine Wards. Nutrients 2019, 11, 790. [Google Scholar] [CrossRef] [PubMed]
- Fan, Y.; Yao, Q.; Liu, Y.; Jia, T.; Zhang, J.; Jiang, E. Underlying Causes and Co-Existence of Malnutrition and Infections: An Exceedingly Common Death Risk in Cancer. Front. Nutr. 2022, 9, 814095. [Google Scholar] [CrossRef] [PubMed]
- Lo Buglio, A.; Bellanti, F.; Serviddio, G.; Vendemiale, G. Impact of Nutritional Status on Muscle Architecture in Elderly Patients Hospitalized in Internal Medicine Wards. J. Nutr. Health Aging 2020, 24, 717–722. [Google Scholar] [CrossRef] [PubMed]
- Xie, L.; Jiang, J.; Fu, H.; Zhang, W.; Yang, L.; Yang, M. Malnutrition in Relation to Muscle Mass, Muscle Quality, and Muscle Strength in Hospitalized Older Adults. J. Am. Med. Dir. Assoc. 2022, 23, 722–728. [Google Scholar] [CrossRef]
- Çalapkorur, S.; Bakır, B.; Toklu, H.; Akın, S. The Effect of the Nutritional Status and Dietary Inflammatory Index on Frailty and Activities of Daily Living in Geriatric Outpatients. Ir. J. Med. Sci. (1971-) 2024, 193, 1671–1680. [Google Scholar] [CrossRef]
- Padilha de Lima, A.; Macedo Rogero, M.; Araujo Viel, T.; Garay-Malpartida, H.M.; Aprahamian, I.; Lima Ribeiro, S.M. Interplay between Inflammaging, Frailty and Nutrition in Covid-19: Preventive and Adjuvant Treatment Perspectives. J. Nutr. Health Aging 2022, 26, 67–76. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Zeng, X.; He, F.; Huang, X. Inflammatory Biomarkers of Frailty: A Review. Exp. Gerontol. 2023, 179, 112253. [Google Scholar] [CrossRef]
- Stumpf, F.; Keller, B.; Gressies, C.; Schuetz, P. Inflammation and Nutrition: Friend or Foe? Nutrients 2023, 15, 1159. [Google Scholar] [CrossRef] [PubMed]
- Di Giosia, P.; Stamerra, C.A.; Giorgini, P.; Jamialahamdi, T.; Butler, A.E.; Sahebkar, A. The Role of Nutrition in Inflammaging. Ageing Res. Rev. 2022, 77, 101596. [Google Scholar] [CrossRef] [PubMed]
- Baylis, D.; Syddall, H.E.; Jameson, K.A.; Cooper, C.; Lord, J.M.; Roberts, H.C.; Sayer, A.A. Cachexia, Sarcopenia, Inflammaging and Outcomes in Hospitalised Older People (the CaSIO Study): Study Protocol and Preliminary Results. Eur. Geriatr. Med. 2015, 6, 495–501. [Google Scholar] [CrossRef]
- Sabbatinelli, J.; Matacchione, G.; Giuliani, A.; Ramini, D.; Rippo, M.R.; Procopio, A.D.; Bonafè, M.; Olivieri, F. Circulating Biomarkers of Inflammaging as Potential Predictors of COVID-19 Severe Outcomes. Mech. Ageing Dev. 2022, 204, 111667. [Google Scholar] [CrossRef] [PubMed]
- Ghone, R.A. A Study of Oxidative Stress Biomarkers and Effect of Oral Antioxidant Supplementation in Severe Acute Malnutrition. J. Clin. Diagn. Res. 2013, 7, 2146–2148. [Google Scholar] [CrossRef]
- Bellanti, F.; Lo Buglio, A.; Vendemiale, G. Redox Homeostasis and Immune Alterations in Coronavirus Disease-19. Biology 2022, 11, 159. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Wang, Z.; Song, M.; Liu, T.; Ding, J.; Deng, L.; Zhang, X.; Qian, L.; Ge, Y.; Xie, H.; et al. Effects of Systemic Inflammation and Frailty on Survival in Elderly Cancer Patients: Results from the INSCOC Study. Front. Immunol. 2023, 14, 936904. [Google Scholar] [CrossRef]
- Lee, H.Y.; Lee, J.; Jung, Y.S.; Kwon, W.Y.; Oh, D.K.; Park, M.H.; Lim, C.-M.; Lee, S.-M. Preexisting Clinical Frailty Is Associated with Worse Clinical Outcomes in Patients with Sepsis. Crit. Care Med. 2022, 50, 780–790. [Google Scholar] [CrossRef]
- Santamaría-Ulloa, C.; Lehning, A.J.; Cortés-Ortiz, M.V.; Méndez-Chacón, E. Frailty as a Predictor of Mortality: A Comparative Cohort Study of Older Adults in Costa Rica and the United States. BMC Public Health 2023, 23, 1960. [Google Scholar] [CrossRef] [PubMed]
- Lo Buglio, A.; Bellanti, F.; Carmignano, D.F.P.; Serviddio, G.; Vendemiale, G. Association between Controlling Nutritional Status (CONUT) Score and Body Composition, Inflammation and Frailty in Hospitalized Elderly Patients. Nutrients 2024, 16, 576. [Google Scholar] [CrossRef] [PubMed]
- Custodero, C.; Mankowski, R.T.; Lee, S.A.; Chen, Z.; Wu, S.; Manini, T.M.; Hincapie Echeverri, J.; Sabbà, C.; Beavers, D.P.; Cauley, J.A.; et al. Evidence-Based Nutritional and Pharmacological Interventions Targeting Chronic Low-Grade Inflammation in Middle-Age and Older Adults: A Systematic Review and Meta-Analysis. Ageing Res. Rev. 2018, 46, 42–59. [Google Scholar] [CrossRef] [PubMed]
- Costamagna, D.; Costelli, P.; Sampaolesi, M.; Penna, F. Role of Inflammation in Muscle Homeostasis and Myogenesis. Mediat. Inflamm. 2015, 2015, 805172. [Google Scholar] [CrossRef]
- Webster, J.M.; Kempen, L.J.A.P.; Hardy, R.S.; Langen, R.C.J. Inflammation and Skeletal Muscle Wasting During Cachexia. Front. Physiol. 2020, 11, 597675. [Google Scholar] [CrossRef] [PubMed]
- Londhe, P.; Guttridge, D.C. Inflammation Induced Loss of Skeletal Muscle. Bone 2015, 80, 131–142. [Google Scholar] [CrossRef]
- Davis, C.; Bryan, J.; Hodgson, J.; Murphy, K. Definition of the Mediterranean Diet; A Literature Review. Nutrients 2015, 7, 9139–9153. [Google Scholar] [CrossRef]
- Martini, D. Health Benefits of Mediterranean Diet. Nutrients 2019, 11, 1802. [Google Scholar] [CrossRef]
- Finicelli, M.; Di Salle, A.; Galderisi, U.; Peluso, G. The Mediterranean Diet: An Update of the Clinical Trials. Nutrients 2022, 14, 2956. [Google Scholar] [CrossRef]
- Trichopoulou, A.; Costacou, T.; Bamia, C.; Trichopoulos, D. Adherence to a Mediterranean Diet and Survival in a Greek Population. N. Engl. J. Med. 2003, 348, 2599–2608. [Google Scholar] [CrossRef]
- Gantenbein, K.V.; Kanaka-Gantenbein, C. Mediterranean Diet as an Antioxidant: The Impact on Metabolic Health and Overall Wellbeing. Nutrients 2021, 13, 1951. [Google Scholar] [CrossRef]
- Dinu, M.; Pagliai, G.; Casini, A.; Sofi, F. Mediterranean Diet and Multiple Health Outcomes: An Umbrella Review of Meta-Analyses of Observational Studies and Randomised Trials. Eur. J. Clin. Nutr. 2018, 72, 30–43. [Google Scholar] [CrossRef]
- Mantzorou, M.; Tolia, M.; Poultsidi, A.; Vasios, G.K.; Papandreou, D.; Theocharis, S.; Kavantzas, N.; Troumbis, A.Y.; Giaginis, C. Adherence to Mediterranean Diet and Nutritional Status in Women with Breast Cancer: What Is Their Impact on Disease Progression and Recurrence-Free Patients’ Survival? Curr. Oncol. 2022, 29, 7482–7497. [Google Scholar] [CrossRef]
- Lengelé, L.; Grande de França, N.A.; Rolland, Y.; Guyonnet, S.; de Souto Barreto, P. Body Composition, Physical Function, and Dietary Patterns in People from 20 to Over 80 Years Old. J. Nutr. Health Aging 2023, 27, 1047–1055. [Google Scholar] [CrossRef]
- Dominguez, L.J.; Donat-Vargas, C.; Sayon-Orea, C.; Barberia-Latasa, M.; Veronese, N.; Rey-Garcia, J.; Rodríguez-Artalejo, F.; Guallar-Castillón, P.; Martínez-González, M.À.; Barbagallo, M. Rationale of the Association between Mediterranean Diet and the Risk of Frailty in Older Adults and Systematic Review and Meta-Analysis. Exp. Gerontol. 2023, 177, 112180. [Google Scholar] [CrossRef]
- Sam-Yellowe, T.Y. Nutritional Barriers to the Adherence to the Mediterranean Diet in Non-Mediterranean Populations. Foods 2024, 13, 1750. [Google Scholar] [CrossRef] [PubMed]
- Sureda, A.; Bibiloni, M.; Julibert, A.; Bouzas, C.; Argelich, E.; Llompart, I.; Pons, A.; Tur, J. Adherence to the Mediterranean Diet and Inflammatory Markers. Nutrients 2018, 10, 62. [Google Scholar] [CrossRef] [PubMed]
- Rosenkranz, S.; Channick, R.; Chin, K.M.; Jenner, B.; Gaine, S.; Galiè, N.; Ghofrani, H.; Hoeper, M.M.; McLaughlin, V.V.; Du Roure, C.; et al. The Impact of Comorbidities on Selexipag Treatment Effect in Patients with Pulmonary Arterial Hypertension: Insights from the GRIPHON Study. Eur. J. Heart Fail. 2022, 24, 205–214. [Google Scholar] [CrossRef] [PubMed]
- Vellas, B.; Guigoz, Y.; Garry, P.J.; Nourhashemi, F.; Bennahum, D.; Lauque, S.; Albarede, J.-L. The Mini Nutritional Assessment (MNA) and Its Use in Grading the Nutritional State of Elderly Patients. Nutrition 1999, 15, 116–122. [Google Scholar] [CrossRef]
- Power, L.; Mullally, D.; Gibney, E.R.; Clarke, M.; Visser, M.; Volkert, D.; Bardon, L.; de van der Schueren, M.A.E.; Corish, C.A. A Review of the Validity of Malnutrition Screening Tools Used in Older Adults in Community and Healthcare Settings—A MaNuEL Study. Clin. Nutr. ESPEN 2018, 24, 1–13. [Google Scholar] [CrossRef]
- Martínez-González, M.A.; García-Arellano, A.; Toledo, E.; Salas-Salvadó, J.; Buil-Cosiales, P.; Corella, D.; Covas, M.I.; Schröder, H.; Arós, F.; Gómez-Gracia, E.; et al. A 14-Item Mediterranean Diet Assessment Tool and Obesity Indexes among High-Risk Subjects: The PREDIMED Trial. PLoS ONE 2012, 7, e43134. [Google Scholar] [CrossRef] [PubMed]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.-I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet Supplemented with Extra-Virgin Olive Oil or Nuts. N. Engl. J. Med. 2018, 378, e34. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in Older Adults: Evidence for a Phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M146–M157. [Google Scholar] [CrossRef] [PubMed]
- van Sleen, Y.; Shetty, S.A.; van der Heiden, M.; Venema, M.C.A.; Gutiérrez-Melo, N.; Toonen, E.J.M.; van Beek, J.; Buisman, A.-M.; van Baarle, D.; Sauce, D. Frailty Is Related to Serum Inflammageing Markers: Results from the VITAL Study. Immun. Ageing 2023, 20, 68. [Google Scholar] [CrossRef] [PubMed]
- Alberro, A.; Iribarren-Lopez, A.; Sáenz-Cuesta, M.; Matheu, A.; Vergara, I.; Otaegui, D. Inflammaging Markers Characteristic of Advanced Age Show Similar Levels with Frailty and Dependency. Sci. Rep. 2021, 11, 4358. [Google Scholar] [CrossRef] [PubMed]
- Romano, A.D.; Lo Buglio, A.; Bellanti, F.; Villani, R.; Serviddio, G.; Vendemiale, G. Diagnostic Reliability of the Procalcitonin Serum Marker in Septic Frail Patient. Aging Clin. Exp. Res. 2019, 31, 727–732. [Google Scholar] [CrossRef] [PubMed]
- Bagheri, A.; Babaei, M.; Rezaei, S.; Motallebnejad, Z.A.; Ganjalikhani, M.; Malekahmadi, M.; Esmaillzadeh, A. The Effect of Mediterranean Diet on Nutritional Status, Muscle Mass and Strength, and Inflammatory Factors in Patients with Colorectal Cancer-Induced Cachexia: Study Protocol for a Randomized Clinical Trial. Trials 2022, 23, 1015. [Google Scholar] [CrossRef] [PubMed]
- Ratajczak, A.E.; Festa, S.; Aratari, A.; Papi, C.; Dobrowolska, A.; Krela-Kaźmierczak, I. Should the Mediterranean Diet Be Recommended for Inflammatory Bowel Diseases Patients? A Narrative Review. Front. Nutr. 2023, 9, 1088693. [Google Scholar] [CrossRef] [PubMed]
- Tsigalou, C.; Konstantinidis, T.; Paraschaki, A.; Stavropoulou, E.; Voidarou, C.; Bezirtzoglou, E. Mediterranean Diet as a Tool to Combat Inflammation and Chronic Diseases. An Overview. Biomedicines 2020, 8, 201. [Google Scholar] [CrossRef]
- Koelman, L.; Egea Rodrigues, C.; Aleksandrova, K. Effects of Dietary Patterns on Biomarkers of Inflammation and Immune Responses: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Adv. Nutr. 2022, 13, 101–115. [Google Scholar] [CrossRef]
- Ecarnot, F.; Maggi, S. The Impact of the Mediterranean Diet on Immune Function in Older Adults. Aging Clin. Exp. Res. 2024, 36, 117. [Google Scholar] [CrossRef]
- Wu, D.; Lewis, E.D.; Pae, M.; Meydani, S.N. Nutritional Modulation of Immune Function: Analysis of Evidence, Mechanisms, and Clinical Relevance. Front. Immunol. 2019, 9, 3160. [Google Scholar] [CrossRef]
- Barrea, L.; Muscogiuri, G.; Laudisio, D.; Pugliese, G.; de Alteriis, G.; Colao, A.; Savastano, S. Influence of the Mediterranean Diet on 25-Hydroxyvitamin D Levels in Adults. Nutrients 2020, 12, 1439. [Google Scholar] [CrossRef] [PubMed]
- Massimino, E.; Izzo, A.; Castaldo, C.; Amoroso, A.P.; Rivellese, A.A.; Capaldo, B.; Della Pepa, G. Dietary Micronutrient Adequacies and Adherence to the Mediterranean Diet in a Population of Older Adults with Type 2 Diabetes: A Cross-Sectional Study. Clin. Nutr. ESPEN 2023, 57, 337–345. [Google Scholar] [CrossRef] [PubMed]
- Casas, R.; Urpi-Sardà, M.; Sacanella, E.; Arranz, S.; Corella, D.; Castañer, O.; Lamuela-Raventós, R.-M.; Salas-Salvadó, J.; Lapetra, J.; Portillo, M.P.; et al. Anti-Inflammatory Effects of the Mediterranean Diet in the Early and Late Stages of Atheroma Plaque Development. Mediat. Inflamm. 2017, 2017, 3674390. [Google Scholar] [CrossRef] [PubMed]
- Boucher, E.L.; Gan, J.M.; Rothwell, P.M.; Shepperd, S.; Pendlebury, S.T. Prevalence and Outcomes of Frailty in Unplanned Hospital Admissions: A Systematic Review and Meta-Analysis of Hospital-Wide and General (Internal) Medicine Cohorts. eClinicalMedicine 2023, 59, 101947. [Google Scholar] [CrossRef]
- Lampropoulos, C.E.; Konsta, M.; Dradaki, V.; Roumpou, A.; Dri, I.; Papaioannou, I. Effects of Mediterranean Diet on Hospital Length of Stay, Medical Expenses, and Mortality in Elderly, Hospitalized Patients: A 2-Year Observational Study. Nutrition 2020, 79–80, 110868. [Google Scholar] [CrossRef]
- Bonaccio, M.; Costanzo, S.; Di Castelnuovo, A.; Gialluisi, A.; Ruggiero, E.; De Curtis, A.; Persichillo, M.; Cerletti, C.; Donati, M.B.; de Gaetano, G.; et al. Increased Adherence to a Mediterranean Diet Is Associated With Reduced Low-Grade Inflammation after a 12.7-Year Period: Results From the Moli-Sani Study. J. Acad. Nutr. Diet. 2023, 123, 783–795.e7. [Google Scholar] [CrossRef]



| High-Level Adherence (Score ≥10) n. 52 (44.4%) | Low-Level Adherence (Score < 10) n. 65 (55.6%) | p Value | |
|---|---|---|---|
| Age, years | 79.0 ± 6.6 | 80.0 ± 6.4 | 0.573 |
| Genre F, n (%) | 42 (80.8) | 36 (55.4) | 0.004 |
| Comorbidities, ≥3 | 29 (55.8) | 50 (76.9) | 0.015 |
| BMI, Kg/m2 | 26.0 [19.1–31.2] | 29. 0 [20.1–33.0] | 0.189 |
| Hemoglobin, g/dL | 11.2 ± 1.9 | 12.1 ± 1.3 | 0.006 |
| WBC, n/mm3 | 6568 [5019–8544] | 6547 [5192–7719] | 0.677 |
| Neutrophils, n/mm3 | 4348 [3244–5703] | 4496 [3543–5722] | 0.598 |
| Lymphocytes, n/mm3 | 1045 [828–1481] | 932 [663–1124] | 0.062 |
| Platelet, 103/μL | 227 [170–349] | 190 [128–242] | <0.001 |
| Glucose, mg/dL | 117.3 ± 24.5 | 116.0 ± 32.5 | 0.820 |
| Albumin, g/dL | 3.6 ± 0.3 | 3.1 ± 0.6 | <0.001 |
| Creatinine, mg/dL | 0.80 [0.67–0.80] | 1.20 [1.00–2.36] | 0.015 |
| Total cholesterol, mg/dL | 155 [129–159] | 158 [122–208] | 0.168 |
| LDL, mg/dL | 88 [67–109] | 88 [65–137] | 0.540 |
| HDL, mg/dL | 50 [45–61] | 41 [35–60] | 0.040 |
| Triglycerides, mg/dL | 74 [57–88] | 125 [113–141] | <0.001 |
| Ferritin, ng/mL | 20 [6–308] | 115 [27–817] | 0.002 |
| CRP, ng/mL | 8.8 [6.0–14.0] | 17.4 [11.7–39.1] | <0.001 |
| MNA score | 17.9 ± 5.8 | 17.0 ± 5.8 | 0.361 |
| LOS, days | 9 [7–11] | 12 [9–18] | <0.001 |
| Inflammatory Status | ||||
| Adherence to MD | n(%) | Mean | Standard Deviation | |
| MNA < 17 | Low | 30 (25.6) | 3.44 | ±0.5 |
| MNA < 17 | High | 17 (14.5) | 2.35 | ±0.5 |
| MNA ≥ 17 | Low | 35 (29.9) | 2.49 | ±0.5 |
| MNA ≥ 17 | High | 35 (29.9) | 1.97 | ±0.6 |
| Length of Stay | ||||
| Adherence to MD | n(%) | Mean | Standard Deviation | |
| MNA < 17 | Low | 30 (25.6) | 2.83 | ±0.3 |
| MNA < 17 | High | 17 (14.5) | 2.23 | ±0.2 |
| MNA ≥ 17 | Low | 35 (29.9) | 2.25 | ±0.3 |
| MNA ≥ 17 | High | 35 (29.9) | 2.10 | ±0.3 |
| Dependent Variable: Inflammatory Status | ||||
| b | SEB | t | p Value | |
| Constant | 2.53 [2.02, 3.04] | 0.26 | 9.76 | <0.001 |
| MNA | −0.02 [−0.05, 0.01] | 0.01 | −1.72 | 0.880 |
| Adherence to the MD | 1.68 [1.01, 2.36] | 0.34 | 4.94 | <0.001 |
| MNA x Adherence to the MD | −0.05 [−0.09, −0.02] | 0.02 | −2.82 | 0.006 |
| Dependent Variable: Length of Stay | ||||
| b | SEB | t | p Value | |
| Constant | 2.15 [2.07, 2.23] | 0.04 | 55.5 | <0.001 |
| MNA | −0.01 [−0.02, 0.01] | 0.01 | −1.68 | 0.095 |
| Adherence to the MD | 0.35 [0.24, 0.45] | 0.05 | 6.68 | <0.001 |
| MNA x Adherence to the MD | −0.05 [−0.06, −0.03] | 0.01 | −5.02 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lo Buglio, A.; Bellanti, F.; Carapellese, R.M.; Capurso, C.; Serviddio, G.; Vendemiale, G. Adherence to the Mediterranean Diet Mitigates Inflammation and Hospital Stay in Frail Elderly Patients: A Moderation Analysis. Nutrients 2024, 16, 2482. https://doi.org/10.3390/nu16152482
Lo Buglio A, Bellanti F, Carapellese RM, Capurso C, Serviddio G, Vendemiale G. Adherence to the Mediterranean Diet Mitigates Inflammation and Hospital Stay in Frail Elderly Patients: A Moderation Analysis. Nutrients. 2024; 16(15):2482. https://doi.org/10.3390/nu16152482
Chicago/Turabian StyleLo Buglio, Aurelio, Francesco Bellanti, Rosanna Maria Carapellese, Cristiano Capurso, Gaetano Serviddio, and Gianluigi Vendemiale. 2024. "Adherence to the Mediterranean Diet Mitigates Inflammation and Hospital Stay in Frail Elderly Patients: A Moderation Analysis" Nutrients 16, no. 15: 2482. https://doi.org/10.3390/nu16152482
APA StyleLo Buglio, A., Bellanti, F., Carapellese, R. M., Capurso, C., Serviddio, G., & Vendemiale, G. (2024). Adherence to the Mediterranean Diet Mitigates Inflammation and Hospital Stay in Frail Elderly Patients: A Moderation Analysis. Nutrients, 16(15), 2482. https://doi.org/10.3390/nu16152482








