Real-World Evaluation of Once-Weekly Subcutaneous Semaglutide in Patients with Type 2 Diabetes Mellitus in Spain (SEMA-RW Study)
Abstract
1. Introduction
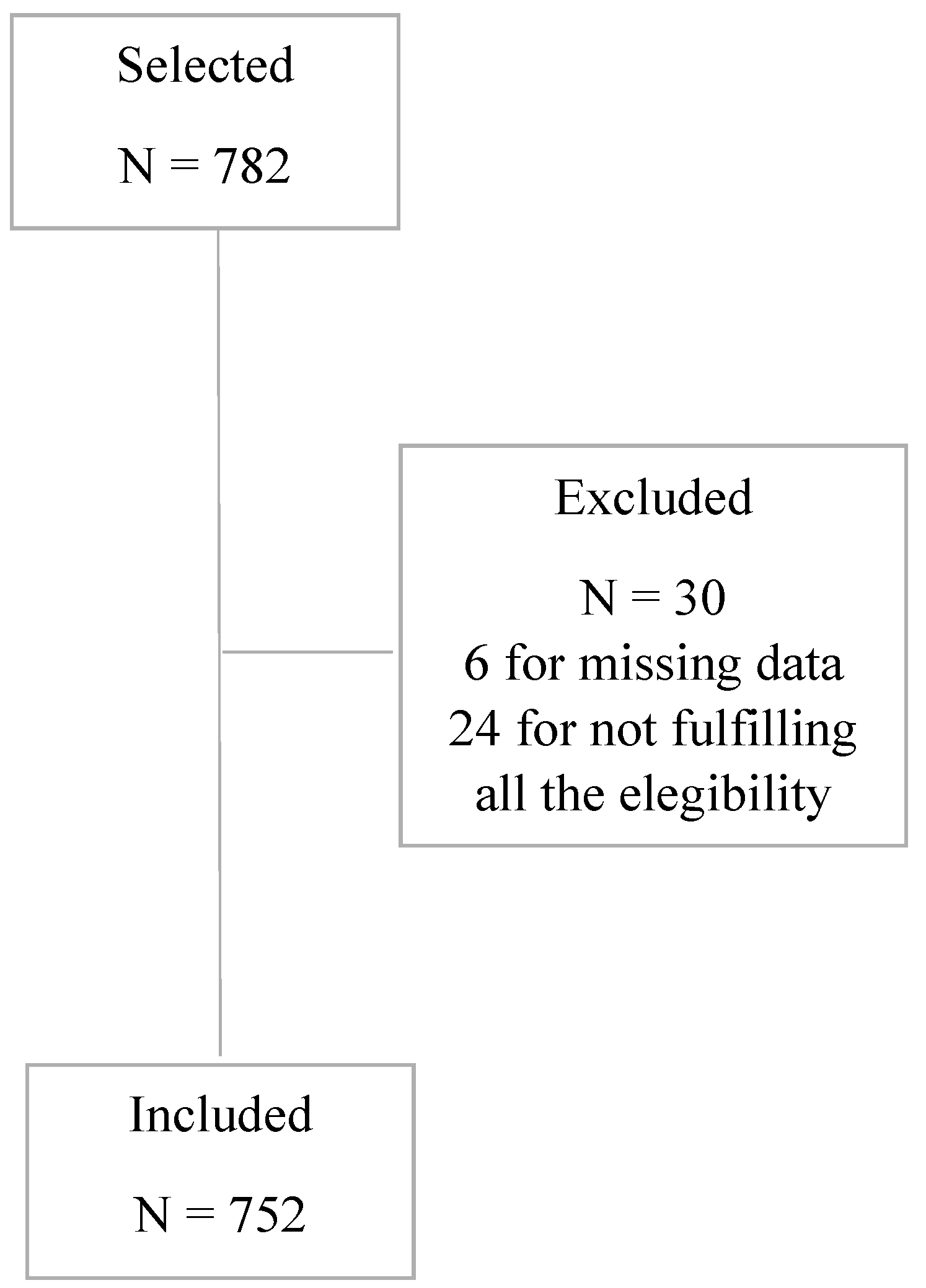
2. Materials and Methods
2.1. Design
2.2. Study Endpoints and Outcome Measures
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- ElSayed, N.A.; Aleppo, G.; Aroda, V.R.; Bannuru, R.R.; Brown, F.M.; Bruemmer, D.; Collins, B.S.; Gaglia, J.L.; Hilliard, M.E.; Isaacs, D.; et al. 2. Classification and diagnosis of diabetes: Standards of care in diabetes-2023. Diabetes Care 2023, 46, S19–S40. [Google Scholar] [CrossRef]
- Khan, M.A.B.; Hashim, M.J.; King, J.K.; Govender, R.D.; Mustafa, H.; Al Kaabi, J. Epidemiology of type 2 diabetes—Global burden of disease and forecasted trends. J. Epidemiol. Glob. Health 2020, 10, 107–111. [Google Scholar] [CrossRef] [PubMed]
- European Commission. Diabetes. Available online: https://research-and-innovation.ec.europa.eu/research-area/health/diabetes_en (accessed on 3 July 2024).
- Davies, M.J.; Aroda, V.R.; Collins, B.S.; Gabbay, R.A.; Green, J.; Maruthur, N.M.; Rosas, S.E.; Del Prato, S.; Mathieu, C.; Mingrone, G.; et al. Management of hyperglycemia in type 2 diabetes, 2022. A consensus report by the American diabetes association (ADA) and the European association for the study of diabetes (EASD). Diabetes Care 2022, 45, 2753–2786. [Google Scholar] [CrossRef]
- Gomez-Peralta, F.; Martín, F.J.E.S.; Torre, E.M.; Cases, M.M.; García, J.C.F.; Loiola, P.E.; Lachica, L.; Pérez, J.A.F.; Menéndez, S.A.; Álvarez-Guisasola, F.; et al. Spanish diabetes society (SED) recommendations for the pharmacologic treatment of hyperglycemia in type 2 diabetes: 2018 update. Endocrinol. Diabetes Nutr. (Engl. Ed.) 2018, 65, 611–624. [Google Scholar] [CrossRef] [PubMed]
- Reyes-García, R.; Moreno-Pérez, O.; Tejera-Pérez, C.; Fernández-García, D.; Bellido-Castañeda, V.; Casares, M.L.d.l.T.; Rozas-Moreno, P.; Fernández-García, J.C.; Martínez, A.M.; Martín, J.E.-S.; et al. A comprehensive approach to type 2 diabetes mellitus–a recommendation document. Endocrinol. Diabetes Nutr. (Engl. Ed.) 2019, 66, 443–458. [Google Scholar] [CrossRef] [PubMed]
- Nadkarni, P.; Chepurny, O.G.; Holz, G.G. Regulation of glucose homeostasis by GLP-1. Prog. Mol. Biol. Transl. Sci. 2014, 121, 23–65. [Google Scholar] [CrossRef] [PubMed]
- Nauck, M.A.; Quast, D.R.; Wefers, J.; Meier, J.J. GLP-1 receptor agonists in the treatment of type 2 diabetes—State-of-the-art. Mol. Metab. 2021, 46, 101102. [Google Scholar] [CrossRef] [PubMed]
- Caruso, I.; Cignarelli, A.; Sorice, G.P.; Natalicchio, A.; Perrini, S.; Laviola, L.; Giorgino, F. Cardiovascular and renal effectiveness of GLP-1 receptor agonists vs. other glucose-lowering drugs in type 2 diabetes: A systematic review and meta-analysis of real-world studies. Metabolites 2022, 12, 183. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Rosenblit, P.D. Glucagon-like peptide-1 receptor agonists and cardiovascular risk reduction in type 2 diabetes mellitus: Is it a class effect? Curr. Cardiol. Rep. 2018, 20, 113. [Google Scholar] [CrossRef] [PubMed]
- Näslund, E.; Bogefors, J.; Skogar, S.; Grybäck, P.; Jacobsson, H.; Holst, J.J.; Hellström, P.M.; Hart, N.J.; Weber, C.; Papas, K.K.; et al. GLP-1 slows solid gastric emptying and inhibits insulin, glucagon, and PYY release in humans. Am. J. Physiol. 1999, 277, R910–R916. [Google Scholar] [CrossRef] [PubMed]
- Shah, M.; Vella, A. Effects of GLP-1 on appetite and weight. Rev. Endocr. Metab. Disord. 2014, 15, 181–187. [Google Scholar] [CrossRef] [PubMed]
- Chun, J.H.; Butts, A. Long-acting GLP-1RAs: An overview of efficacy, safety, and their role in type 2 diabetes management. Jaapa 2020, 33, 3–18. [Google Scholar] [CrossRef] [PubMed]
- Patel, D. Glycaemic and non-glycaemic efficacy of once-weekly GLP-1 receptor agonists in people with type 2 diabetes. J. Clin. Pharm. Ther. 2020, 45 (Suppl. S1), 28–42. [Google Scholar] [CrossRef] [PubMed]
- Annex i Summary of Product Characteristics. Available online: https://www.ema.europa.eu/en/documents/product-information/ozempic-epar-product-information_en.pdf (accessed on 3 July 2024).
- European Medicines Agencys Science Medicines Health. Rybelsus. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/rybelsus (accessed on 3 July 2024).
- Aroda, V.R.; Ahmann, A.; Cariou, B.; Chow, F.; Davies, M.J.; Jódar, E.; Mehta, R.; Woo, V.; Lingvay, I. Comparative efficacy, safety, and cardiovascular outcomes with once-weekly subcutaneous semaglutide in the treatment of type 2 diabetes: Insights from the SUSTAIN 1-7 trials. Diabetes Metab. 2019, 45, 409–418. [Google Scholar] [CrossRef] [PubMed]
- Marso, S.P.; Bain, S.C.; Consoli, A.; Eliaschewitz, F.G.; Jódar, E.; Leiter, L.A.; Lingvay, I.; Rosenstock, J.; Seufert, J.; Warren, M.L.; et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N. Engl. J. Med. 2016, 375, 1834–1844. [Google Scholar] [CrossRef] [PubMed]
- Bueno, B.A.; Soler, M.J.; Perez-Belmonte, L.; Jimenez Millan, A.; Rivas Ruiz, F.; De Lucas, M.D.G. Semaglutide in type 2 diabetes with chronic kidney disease at high risk progression-real-world clinical practice. Clin. Kidney J. 2022, 15, 1593–1600. [Google Scholar] [CrossRef] [PubMed]
- Bellido, V.; Padín, C.A.; Catarig, A.M.; Clark, A.; Pittol, S.B.; Delgado, E. Once-weekly semaglutide use in patients with type 2 diabetes: Results from the sure spain multicentre, prospective, observational study. J. Clin. Med. 2022, 11, 4938. [Google Scholar] [CrossRef] [PubMed]
- De Lucas, M.D.G.; PÉRez-Belmonte, L.M.; Aviles, B.; Jimenez, A.I.; Fernandez, J.M.; Ruiz, F.R. 676-P: Semaglutide achieves better metabolic and weight control than other GLP-1 RA in real life after 12 months of follow-up. Diabetes 2021, 70, 676. [Google Scholar] [CrossRef]
- Ferrer-García, J.C.; Galera, R.A.; Arribas, L.; Torrens, M.T.; Lorente, A.S.; Portilla, A.J.; Artero, A.; Sánchez-Juan, C. 947-P: Semaglutide added to treatment or changed from other GLP-1 receptor agonist in type 2 diabetes: A study to evaluate real-world effectiveness. Diabetes 2020, 69, 947. [Google Scholar] [CrossRef]
- De Lucas, M.D.G.; Miramontes-González, J.P.; Avilés-Bueno, B.; Jiménez-Millán, A.I.; Rivas-Ruiz, F.; Pérez-Belmonte, L.M. Real-world use of once-weekly semaglutide in patients with type 2 diabetes at an outpatient clinic in Spain. Front. Endocrinol. (Lausanne) 2022, 13, 995646. [Google Scholar] [CrossRef]
- De Lucas, M.D.G.; Perez-Belmonte, L.; Aviles-Bueno, B.; Jimenez-Millan, A.; Ruiz, F.R.; Miramontes-González, J.P. Results of semaglutide in patients older than 70 years, a real-world study of efficacy and safety. Minerva Endocrinol. (Torino) 2023. [Google Scholar] [CrossRef]
- Pérez-Belmonte, L.M.; Sanz-Cánovas, J.; de Lucas, M.D.G.; Ricci, M.; Avilés-Bueno, B.; Cobos-Palacios, L.; Pérez-Velasco, M.A.; López-Sampalo, A.; Bernal-López, M.R.; Jansen-Chaparro, S.; et al. Efficacy and safety of semaglutide for the management of obese patients with type 2 diabetes and chronic heart failure in real-world clinical practice. Front. Endocrinol. (Lausanne) 2022, 13, 851035. [Google Scholar] [CrossRef] [PubMed]
- Cardenas, S.J.J.; Poyatos, R.M.S.; Luiza, L.B.; Sanchez, L.B.; Modrono, M.N.; Montoya, A.T.; GoMez, M.M.D.L.P.; Sanchez-Lopez, R.; Casado, C.; Vazquez, M.C. Real life study of SEMaglutide in patients with type 2 diabetes in Spain (REALSEM-SP): Retrospective clinical study on the efficacy, adherence, and safety with semaglutide. Endocr. Abstr. 2022, 81, P333. [Google Scholar] [CrossRef]
- Brown, R.E.; Bech, P.G.; Aronson, R. Semaglutide once weekly in people with type 2 diabetes: Real-world analysis of the Canadian LMC diabetes registry (SPARE study). Diabetes Obes. Metab. 2020, 22, 2013–2020. [Google Scholar] [CrossRef] [PubMed]
- Di Loreto, C.; Minarelli, V.; Nasini, G.; Norgiolini, R.; Del Sindaco, P. Effectiveness in real world of once weekly semaglutide in people with type 2 diabetes: Glucagon-like peptide receptor agonist naïve or switchers from other glucagon-like peptide receptor agonists: Results from a retrospective observational study in Umbria. Diabetes Ther. 2022, 13, 551–567. [Google Scholar] [CrossRef] [PubMed]
- Hansen, K.B.; Svendstrup, M.; Lund, A.; Knop, F.K.; Vilsbøll, T.; Vestergaard, H. Once-weekly subcutaneous semaglutide treatment for persons with type 2 diabetes: Real-world data from a diabetes out-patient clinic. Diabet. Med. 2021, 38, e14655. [Google Scholar] [CrossRef] [PubMed]
- Holmes, P.; Bell, H.E.; Bozkurt, K.; Catarig, A.-M.; Clark, A.; Machell, A.; Sathyapalan, T. Real-world use of once-weekly semaglutide in type 2 diabetes: Results from the sure UK multicentre, prospective, observational study. Diabetes Ther. 2021, 12, 2891–2905. [Google Scholar] [CrossRef]
- Jain, A.B.; Kanters, S.; Khurana, R.; Kissock, J.; Severin, N.; Stafford, S.G. Real-world effectiveness analysis of switching from liraglutide or dulaglutide to semaglutide in patients with type 2 diabetes mellitus: The retrospective realise-DM study. Diabetes Ther. 2021, 12, 527–536. [Google Scholar] [CrossRef] [PubMed]
- Lingvay, I.; Kirk, A.R.; Lophaven, S.; Wolden, M.L.; Shubrook, J.H. Outcomes in GLP-1 RA-experienced patients switching to once-weekly semaglutide in a real-world setting: The retrospective, observational expert study. Diabetes Ther. 2021, 12, 879–896. [Google Scholar] [CrossRef] [PubMed]
- Marzullo, P.; Daffara, T.; Mele, C.; Zavattaro, M.; Ferrero, A.; Caputo, M.; Prodam, F.; Aimaretti, G. Real-world evaluation of weekly subcutaneous treatment with semaglutide in a cohort of Italian diabetic patients. J. Endocrinol. Investig. 2022, 45, 1587–1598. [Google Scholar] [CrossRef] [PubMed]
- Menzen, M.; Berentzen, T.L.; Catarig, A.M.; Pieperhoff, S.; Simon, J.; Jacob, S. Real-world use of once-weekly semaglutide in type 2 diabetes: Results from semaglutide real-world evidence (SURE) Germany. Exp. Clin. Endocrinol. Diabetes 2023, 131, 205–215. [Google Scholar] [CrossRef]
- Mohammedi, K.; Belhatem, N.; Berentzen, T.L.; Catarig, A.M.; Potier, L. Once-weekly semaglutide use in patients with type 2 diabetes: Results from the SURE France multicentre, prospective, observational study. Diabetes Obes. Metab. 2023, 25, 1855–1864. [Google Scholar] [CrossRef] [PubMed]
- Napoli, R.; Berra, C.; Catarig, A.M.; Di Loreto, C.; Donatiello, E.; Berentzen, T.L. Once-weekly semaglutide use in patients with type 2 diabetes: Real-world data from the SURE Italy observational study. Diabetes Obes. Metab. 2023, 25, 1658–1667. [Google Scholar] [CrossRef] [PubMed]
- Ekberg, N.R.; Bodholdt, U.; Catarig, A.-M.; Catrina, S.-B.; Grau, K.; Holmberg, C.N.; Klanger, B.; Knudsen, S.T. Real-world use of once-weekly semaglutide in patients with type 2 diabetes: Results from the SURE Denmark/Sweden multicentre, prospective, observational study. Prim. Care Diabetes 2021, 15, 871–878. [Google Scholar] [CrossRef]
- Vilsbøll, T.; Lindahl, C.; Nielsen, N.F.; Tikkanen, C.K. Real-world impact of once-weekly subcutaneous semaglutide after 2 years of follow-up: Results from a nationwide observational study in people with type 2 diabetes. Diabetes Obes. Metab. 2023, 25, 1740–1749. [Google Scholar] [CrossRef] [PubMed]
- Volpe, S.; Lisco, G.; Fanelli, M.; Racaniello, D.; Colaianni, V.; Triggiani, D.; Donghia, R.; Crudele, L.; Rinaldi, R.; Sabbà, C.; et al. Once-weekly subcutaneous semaglutide improves fatty liver disease in patients with type 2 diabetes: A 52-week prospective real-life study. Nutrients 2022, 14, 4673. [Google Scholar] [CrossRef] [PubMed]
- Yale, J.; Catarig, A.; Grau, K.; Harris, S.; Klimek-Abercrombie, A.; Rabasa-Lhoret, R.; Reardon, L.; Woo, V.; Liutkus, J. Use of once-weekly semaglutide in patients with type 2 diabetes in routine clinical practice: Results from the SURE Canada multicentre, prospective, observational study. Diabetes Obes. Metab. 2021, 23, 2269–2278. [Google Scholar] [CrossRef] [PubMed]

| Variable | |
|---|---|
| N | 753 |
| Age, years, mean (±SD) | 60.71 (±11.18) |
| Female, n (%) | 355 (47.2%) |
| Time since diabetes diagnosis, years, median (IQR) | 11.00 (5.00, 17.00) |
| HbA1c, %, mean (±SD) | 8.53 (±1.84) |
| HbA1c ≥ 7.5%, n (%) | 510 (67.8%) |
| HbA1c ≥ 7.0%, n (%) | 615 (81.8%) |
| Body weight, kg, mean (±SD) | 101.62 (±19.77) |
| Height, cm, mean (±SD) | 165.18 (±9.5) |
| Body mass index, kg/m2 mean (±SD) | 37.11 (±6.55) |
| SBP, mm Hg, mean (±SD) | 135.99 (±17.97) |
| DBP, mm Hg, mean (±SD) | 78.18 (±11.18) |
| Waist circumference, cm, mean (±SD) | 119.11 (±14.25) |
| Fasting plasma glucose, mg/dL, mean (±SD) | 169.45 (±67.82) |
| Severe hypoglycemic episodes, n (%) | 10 (1.3%) |
| Diabetic retinopathy, n (%) | 98 (13.1%) |
| 67 (8.9%) |
| 17 (2.3%) |
| 14 (1.9%) |
| Hypertension, n (%) | 542 (72.1%) |
| Dyslipidemia, n (%) | 554 (73.7%) |
| CKD, n (%) | 134 (17.8%) |
| OSAHS, n (%) | 144 (19.1%) |
| NASH, n (%) | 126 (16.8%) |
| IHD, n (%) | 121 (16.1%) |
| Established cerebrovascular disease, n (%) | 22 (2.9%) |
| PAD, n (%) | 65 (8.6%) |
| CHF, n (%) | 45 (6.0%) |
| Smoking status, n (%) | |
| 115 (15.3%) |
| 246 (32.7%) |
| Albumin, mg/dL, mean (±SD) | 5.48 (±23.29) |
| Creatinine, mg/dL, mean (±SD) | 1.27 (±5.59) |
| UAE, mg/dL, mean (±SD) | 78.19 (±279.38) |
| eGFR, mL/min, mean (±SD) | 81.21 (±24.52) |
| FIB4 score (0–6), mean (±SD) | 1.24 (±0.65) |
| GOT, units/L, mean (±SD) | 29.21 (±21.64) |
| GPT, units/L, mean (±SD) | 34.10 (±29.13) |
| Blood platelet count, units/µL, mean (±SD) | 1220.86 (±17,116.13) |
| Uric acid, mg/dL, mean (±SD) | 13.63 (±190.10) |
| TC, mg/dL, mean (±SD) | 173.94 (±41.4) |
| HDL-C, mg/dL, mean (±SD) | 42.51 (±10.41) |
| LDL-C, mg/dL, mean (±SD) | 95.17 (±35.85) |
| TG, mg/dL, mean (±SD) | 213.41 (±234.121) |
| Variable | N = 752 |
|---|---|
| Creatinine, mg/dL, mean (±SD) | 1.2 (5.5) |
| UAE, mg/dL, mean (±SD) | 78.1 (±79.3) |
| eGFR, mL/min, mean (±SD) | 81.2 (24.5) |
| TC, mg/dL, mean (±SD) | 173.9 (41.4) |
| HDL-C, mg/dL, mean (±SD) | 42.5 (10.4) |
| LDL-C, mg/dL, mean (±SD) | 95.1 (35.8) |
| TG, mg/dL, mean (±SD) | 213.4 (234.1) |
| Medication | |
|---|---|
| N | 753 |
| Semaglutide dose (s.c., OAW), n (%) | |
| 511 (68.00%) |
| 154 (20.50%) |
| 87 (11.60%) |
| Concomitant antidiabetic medication, n (%): | |
| 251 (33.40%) |
| 342 (45.50%) |
| 342 (45.50%) |
| 157 (20.90%) |
| 15 (2.00%) |
| 80 (10.60%) |
| |
| 305 (40.6%) |
| 173 (23.0%) |
| Other concomitant medication, n (%): | |
| 493 (65.60%) |
| 173 (23.00%) |
| 29 (3.90%) |
| 196 (26.10%) |
| 705 (93.80%) |
| 22 (2.90%) |
| 463 (61.60%) |
| 2 (0.30%) |
| 52 (6.90%) |
| 86 (11.40%) |
| 53 (7.00%) |
| 234 (31.10%) |
| Semaglutide Plus Noninsulin Monotherapy | Semaglutide Plus Noninsulin Double or Triple Therapy | Semaglutide Plus Basal Insulin Therapy | Semaglutide Plus Basal-Bolus Insulin Therapy | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 12-Months-Baseline Mean Difference (95% CI) | N | p Value * | 12-Months-Baseline Mean Difference (95% CI) | N | p Value * | 12-Months-Baseline Mean Difference (95% CI) | N | p Value * | 12-Months-Baseline Mean Difference (95% CI) | N | p Value * | |
| HbA1C (%) | −2.3 (−2.6, −2.0) | 184 | <0.001 | −1.8 (−2.0, −1.6) | 236 | <0.001 | −1.2 (−1.5, −0.9) | 84 | <0.001 | −1.3 (−1.7, −0.8) | 35 | <0.001 |
| Weight (kg) | −10.0 (−11.2, −8.7) | 186 | <0.001 | −8.3 (−9.2, −7.4) | 238 | <0.001 | −6.2 (−7.3, −5.2) | 85 | <0.001 | −6.9 (−8.6, −5.3) | 36 | <0.001 |
| Adverse Event | N (%) |
|---|---|
| Severe hypoglycemia *$ | 7 (0.9) |
| Lower limb amputation | 3 (0.4) |
| Gastro-intestinal overall | 72 (9.6) |
| 15 (2.0) |
| 57 (7.6) |
| MACE ** | 4 (0.6) |
| MARE *** | 3 (0.4) |
| Retinopathy overall | 4 (0.6) |
| 2 (0.3) |
| 2 (0.3) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Caballero Mateos, I.; García de Lucas, M.D.; Doulatram-Gamgaram, V.K.; Moreno-Moreno, P.; Jimenez-Millan, A.I.; Botana-López, M.; Merino-Torres, J.F.; Soto-Gónzalez, A.; Fernández-García, J.C.; Morales-Portillo, C. Real-World Evaluation of Once-Weekly Subcutaneous Semaglutide in Patients with Type 2 Diabetes Mellitus in Spain (SEMA-RW Study). Nutrients 2024, 16, 2545. https://doi.org/10.3390/nu16152545
Caballero Mateos I, García de Lucas MD, Doulatram-Gamgaram VK, Moreno-Moreno P, Jimenez-Millan AI, Botana-López M, Merino-Torres JF, Soto-Gónzalez A, Fernández-García JC, Morales-Portillo C. Real-World Evaluation of Once-Weekly Subcutaneous Semaglutide in Patients with Type 2 Diabetes Mellitus in Spain (SEMA-RW Study). Nutrients. 2024; 16(15):2545. https://doi.org/10.3390/nu16152545
Chicago/Turabian StyleCaballero Mateos, Irene, María Dolores García de Lucas, Viyey Kishore Doulatram-Gamgaram, Paloma Moreno-Moreno, Ana Isabel Jimenez-Millan, Manuel Botana-López, Juan Francisco Merino-Torres, Alfonso Soto-Gónzalez, José Carlos Fernández-García, and Cristóbal Morales-Portillo. 2024. "Real-World Evaluation of Once-Weekly Subcutaneous Semaglutide in Patients with Type 2 Diabetes Mellitus in Spain (SEMA-RW Study)" Nutrients 16, no. 15: 2545. https://doi.org/10.3390/nu16152545
APA StyleCaballero Mateos, I., García de Lucas, M. D., Doulatram-Gamgaram, V. K., Moreno-Moreno, P., Jimenez-Millan, A. I., Botana-López, M., Merino-Torres, J. F., Soto-Gónzalez, A., Fernández-García, J. C., & Morales-Portillo, C. (2024). Real-World Evaluation of Once-Weekly Subcutaneous Semaglutide in Patients with Type 2 Diabetes Mellitus in Spain (SEMA-RW Study). Nutrients, 16(15), 2545. https://doi.org/10.3390/nu16152545







