Body Size Measurements Grouped Independently of Common Clinical Measures of Metabolic Health: An Exploratory Factor Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Demographics
2.3. Metabolic Health Measures
2.4. Body Size Measures
2.5. Statistical Analysis
3. Results
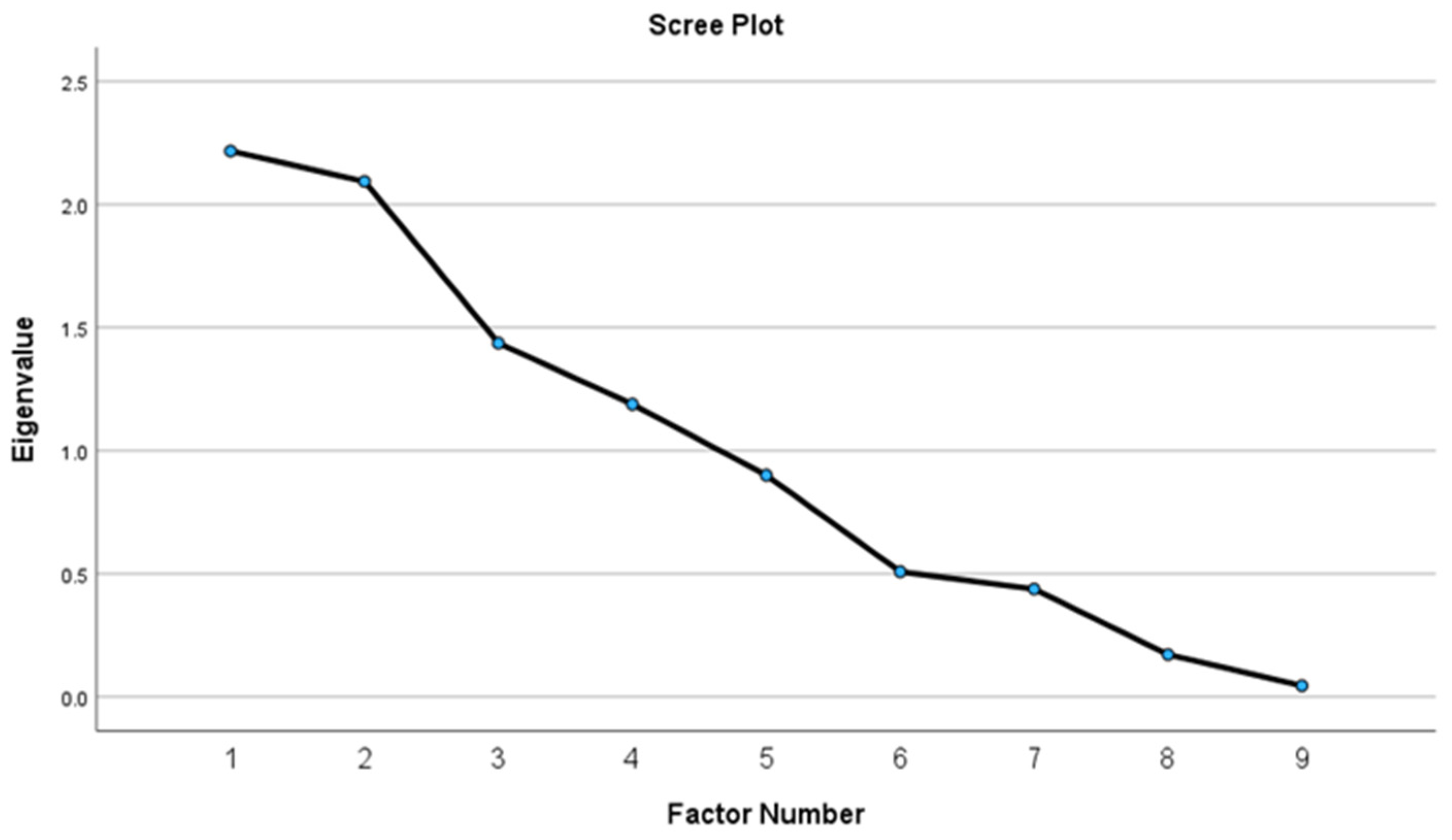
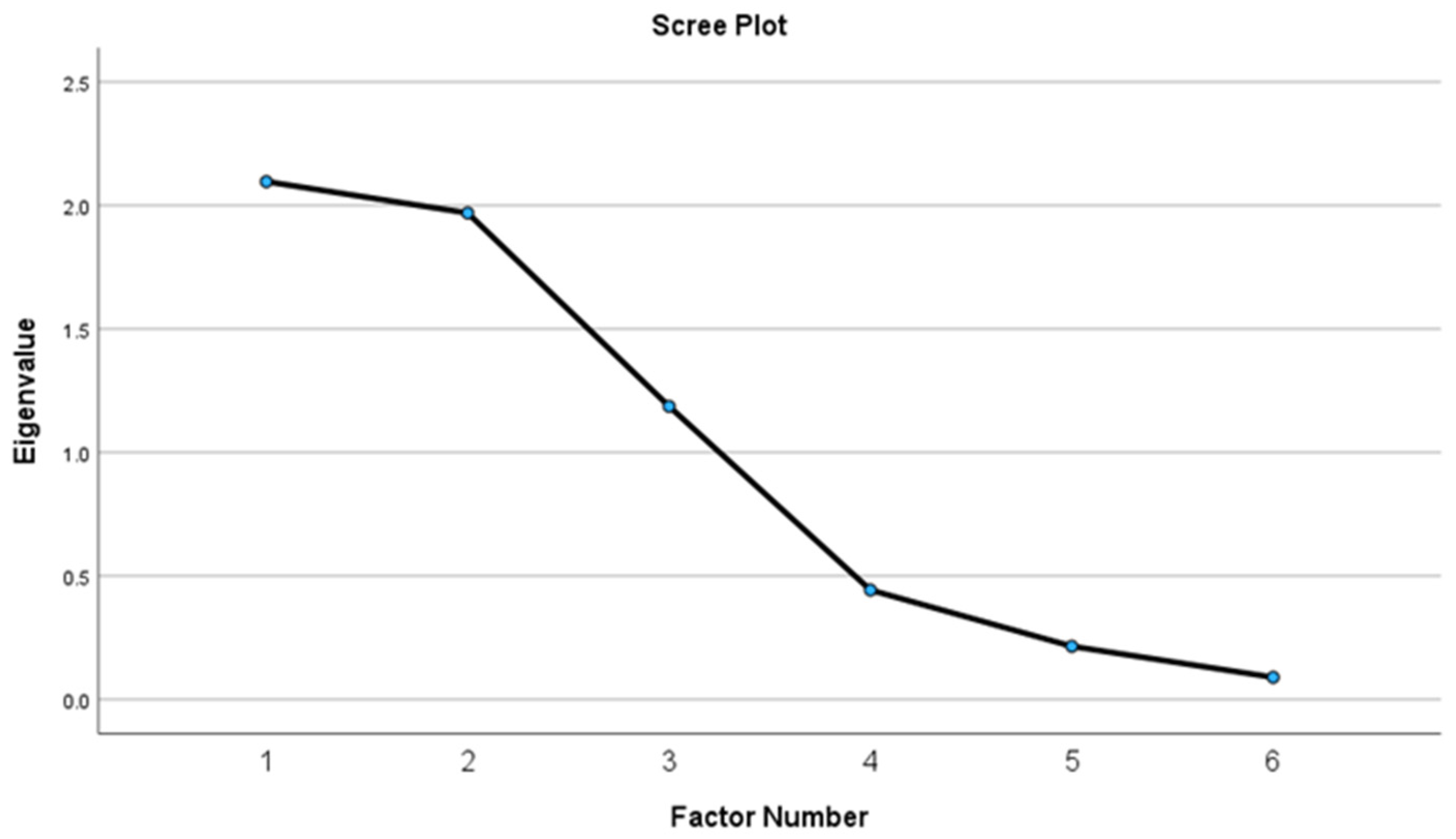
3.1. Exploratory Factor Analysis
3.2. Item Total Correlations
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- National Academies of Sciences, Engineering, and Medicine; Division of Behavioral and Social Sciences and Education; Committee on National Statistics; Committee on Population; Committee on Rising Midlife Mortality Rates and Socioeconomic Disparities. Cardiometabolic Diseases. In High and Rising Mortality Rates among Working-Age Adults; Harris, K.M., Majmundar, M.K., Becker, T., Eds.; National Academies Press (US): Washington, DC, USA, 2021. [Google Scholar]
- Wing, R.R.; Lang, W.; Wadden, T.A.; Safford, M.; Knowler, W.C.; Bertoni, A.G.; Hill, J.O.; Brancati, F.L.; Peters, A.; Wagenknecht, L. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care 2011, 34, 1481–1486. [Google Scholar] [CrossRef] [PubMed]
- Garvey, W.T.; Mechanick, J.I.; Brett, E.M.; Garber, A.J.; Hurley, D.L.; Jastreboff, A.M.; Nadolsky, K.; Pessah-Pollack, R.; Plodkowski, R. American Association of Clinical Endocrinologists and American College of Endocrinology Comprehensive Clinical Practice Guidelines for Medical Care of Patients with Obesity. Endocr. Pract. 2016, 22, 1–203. [Google Scholar] [PubMed]
- Ryan, D.H.; Yockey, S.R. Weight Loss and Improvement in Comorbidity: Differences at 5%, 10%, 15%, and Over. Curr. Obes. Rep. 2017, 6, 187–194. [Google Scholar] [CrossRef]
- The Association for Size Diversity and Health (ASDAH). Health at Every Size®. Available online: https://asdah.org/haes/ (accessed on 23 May 2024).
- Ulian, M.D.; Benatti, F.B.; de Campos-Ferraz, P.L.; Roble, O.J.; Unsain, R.F.; de Morais Sato, P.; Brito, B.C.; Murakawa, K.A.; Modesto, B.T.; Aburad, L.; et al. The Effects of a “Health at Every Size®”-Based Approach in Obese Women: A Pilot-Trial of the “Health and Wellness in Obesity” Study. Front. Nutr. 2015, 2, 34. [Google Scholar] [CrossRef] [PubMed]
- Bacon, L.; Aphramor, L. Weight science: Evaluating the evidence for a paradigm shift. Nutr. J. 2011, 10, 9. [Google Scholar] [CrossRef]
- Hagen, S.J.; Henningfield, M.F. Health at Every Size Principles: Clinician Perspectives to Limit Weight Stigma in Medical Care. WMJ 2023, 122, 277–279. [Google Scholar]
- Penney, T.L.; Kirk, S.F. The Health at Every Size paradigm and obesity: Missing empirical evidence may help push the reframing obesity debate forward. Am. J. Public Health 2015, 105, e38–e42. [Google Scholar] [CrossRef]
- Morsali, M.; Poorolajal, J.; Shahbazi, F.; Vahidinia, A.; Doosti-Irani, A. Diet Therapeutics Interventions for Obesity: A Systematic Review and Network Meta-Analysis. J. Res. Health Sci. 2021, 21, e00521. [Google Scholar] [CrossRef]
- Hall, K.D. Metabolic Adaptations to Weight Loss. Obesity 2018, 26, 790–791. [Google Scholar] [CrossRef]
- Martins, C.; Roekenes, J.; Gower, B.A.; Hunter, G.R. Metabolic adaptation is associated with less weight and fat mass loss in response to low-energy diets. Nutr. Metab. 2021, 18, 60. [Google Scholar] [CrossRef]
- Hales, C.M.; Fryar, C.D.; Ogden, C.L. Prevalence of Obesity and Severe Obesity among Adults: United States, 2017–2018; National Center for Health Statistics: Hyattsville, MD, USA, 2020.
- Clina, J.G.; Sayer, R.D.; Pan, Z.; Cohen, C.W.; McDermott, M.T.; Catenacci, V.A.; Wyatt, H.R.; Hill, J.O. High- and normal-protein diets improve body composition and glucose control in adults with type 2 diabetes: A randomized trial. Obesity 2023, 31, 2021–2030. [Google Scholar] [CrossRef]
- Whitehead, S.J.; Ford, C.; Gama, R. A combined laboratory and field evaluation of the Cholestech LDX and CardioChek PA point-of-care testing lipid and glucose analysers. Ann. Clin. Biochem. 2014, 51, 54–67. [Google Scholar] [CrossRef] [PubMed]
- Shephard, M.D.; Mazzachi, B.C.; Shephard, A.K. Comparative performance of two point-of-care analysers for lipid testing. Clin. Lab. 2007, 53, 561–566. [Google Scholar] [PubMed]
- Panz, V.R.; Raal, F.J.; Paiker, J.; Immelman, R.; Miles, H. Performance of the CardioChek PA and Cholestech LDX point-of-care analysers compared to clinical diagnostic laboratory methods for the measurement of lipids. Cardiovasc. J. S. Afr. 2005, 16, 112–117. [Google Scholar] [PubMed]
- Arnold, W.D.; Kupfer, K.; Little, R.R.; Amar, M.; Horowitz, B.; Godbole, N.; Hvidsten Swensen, M.; Li, Y.; San George, R.C. Accuracy and Precision of a Point-of-Care HbA1c Test. J. Diabetes Sci. Technol. 2020, 14, 883–889. [Google Scholar] [CrossRef] [PubMed]
- D’Hondt, J.; Waterplas, J.; Chapelle, L.; Clarys, P.; D’Hondt, E. A Comparative and Sex-Specific Study of Bio-Electrical Impedance Analysis and Dual Energy X-ray Absorptiometry for Estimating Whole-Body and Segmental Body Composition in Healthy Young Adults. Appl. Sci. 2022, 12, 7686. [Google Scholar] [CrossRef]
- Ng, B.K.; Liu, Y.E.; Wang, W.; Kelly, T.L.; Wilson, K.E.; Schoeller, D.A.; Heymsfield, S.B.; Shepherd, J.A. Validation of rapid 4-component body composition assessment with the use of dual-energy X-ray absorptiometry and bioelectrical impedance analysis. Am. J. Clin. Nutr. 2018, 108, 708–715. [Google Scholar] [CrossRef]
- Suida, A.; Chomentowski, P.J., III; Salacinski, A.J.; Broeder, C. Validity of Whole and Regional Body Composition Testing Devices: 986 Board #165 May 31 3: 30 PM–5: 00 PM. Med. Sci. Sports Exerc. 2017, 49, 264–265. [Google Scholar]
- Ellison, K.M.; Ehrlicher, S.E.; El Zein, A.; Sayer, R.D. Fat and fat-free mass measurement agreement by dual-energy X-ray absorptiometry versus bioelectrical impedance analysis: Effects of posture and waist circumference. Obes. Sci. Pract. 2024, 10, e744. [Google Scholar] [CrossRef]
- Office of Public Health and Science, Health and Human Services Department. The Practical Guide: Identification, Evaluation, and Treatment of Overweight and Obesity in Adults; Office of Public Health and Science, Health and Human Services Department: Washington, DC, USA, 2000.
- Taber, K.S. The Use of Cronbach’s Alpha When Developing and Reporting Research Instruments in Science Education. Res. Sci. Educ. 2018, 48, 1273–1296. [Google Scholar] [CrossRef]
- Zijlmans, E.A.O.; Tijmstra, J.; van der Ark, L.A.; Sijtsma, K. Item-Score Reliability in Empirical-Data Sets and Its Relationship With Other Item Indices. Educ. Psychol. Meas. 2018, 78, 998–1020. [Google Scholar] [CrossRef]
- Bays, H.E.; Chapman, R.H.; Grandy, S. The relationship of body mass index to diabetes mellitus, hypertension and dyslipidaemia: Comparison of data from two national surveys. Int. J. Clin. Pract. 2007, 61, 737–747. [Google Scholar] [CrossRef]
- Blüher, M. Metabolically Healthy Obesity. Endocr. Rev. 2020, 41, bnaa004. [Google Scholar] [CrossRef] [PubMed]
- Taylor, R.; Holman, R.R. Normal weight individuals who develop type 2 diabetes: The personal fat threshold. Clin. Sci. 2015, 128, 405–410. [Google Scholar] [CrossRef] [PubMed]
- Batsis, J.A.; Sahakyan, K.R.; Rodriguez-Escudero, J.P.; Bartels, S.J.; Somers, V.K.; Lopez-Jimenez, F. Normal weight obesity and mortality in United States subjects ≥ 60 years of age (from the Third National Health and Nutrition Examination Survey). Am. J. Cardiol. 2013, 112, 1592–1598. [Google Scholar] [CrossRef] [PubMed]
- Romero-Corral, A.; Somers, V.K.; Sierra-Johnson, J.; Korenfeld, Y.; Boarin, S.; Korinek, J.; Jensen, M.D.; Parati, G.; Lopez-Jimenez, F. Normal weight obesity: A risk factor for cardiometabolic dysregulation and cardiovascular mortality. Eur. Heart J. 2010, 31, 737–746. [Google Scholar] [CrossRef]
- Stefan, N.; Schick, F.; Häring, H.-U. Causes, Characteristics, and Consequences of Metabolically Unhealthy Normal Weight in Humans. Cell Metab. 2017, 26, 292–300. [Google Scholar] [CrossRef]
- Ekelund, U.; Besson, H.; Luan, J.A.; May, A.M.; Sharp, S.J.; Brage, S.; Travier, N.; Agudo, A.; Slimani, N.; Rinaldi, S.; et al. Physical activity and gain in abdominal adiposity and body weight: Prospective cohort study in 288,498 men and women. Am. J. Clin. Nutr. 2011, 93, 826–835. [Google Scholar] [CrossRef]
- Strasser, B. Physical activity in obesity and metabolic syndrome. Ann. N. Y. Acad. Sci. 2013, 1281, 141–159. [Google Scholar] [CrossRef]
- Diels, S.; Vanden Berghe, W.; Van Hul, W. Insights into the multifactorial causation of obesity by integrated genetic and epigenetic analysis. Obes. Rev. 2020, 21, e13019. [Google Scholar] [CrossRef]
- Anna, B.; Costello, J.O. Best practices in explor actices in exploratory factor analysis: Four or analysis: Four recommendations for getting the most from your analysis. Pract. Assess. Res. Eval. 2005, 10, 1–9. [Google Scholar]
- Ellison, K.; Smith, K.; Hill, J.; Wyatt, H.; Sayer, D. PTFS04-06-23 An Exploratory Factor Analysis of Common Cardiometabolic Measures in People With Obesity for Building a Parsimonious Health Assessment. Curr. Dev. Nutr. 2023, 7, 101649. [Google Scholar] [CrossRef]
| Study | NCT04014296 1 | NCT04745572 1 | NCT04392284 1 | NCT03832933 [14] |
|---|---|---|---|---|
| Purpose | To compare the separate and combined effects of a high-protein diet and resistance training on retention of fat-free mass during weight loss in older adults. | To compare a high and reduced carbohydrate diet with or without individual counseling for time-restricted eating or exercise. | To investigate the feasibility of an adaptive biobehavioral intervention for improving insulin sensitivity among patients with Stage 1 obesity. | To compare a high-protein diet with ≥4 weekly servings of lean beef and a normal-protein diet without any red meat for weight loss, body composition changes, and glucose control in individuals with T2D. |
| Study design | SMART | SMART | SMART | RT |
| Original study N | 89 | 83 | 40 | 106 |
| n for present analysis | 52 | 53 | 40 | 104 |
| Age | ≥50 years old | 18–75 years old | 18–65 years old | ≥18 years old |
| BMI | ≥30 kg/m2 | 27 kg/m2 | ≥27 kg/m2 | ≥27 kg/m2 |
| Main inclusion criteria | Must be postmenopausal if female (≥1 year since last menstrual period). | Must have prediabetes (A1c ≥ 5.7% and/or fasting glucose ≥ 100 mg/dL). | Must have one or more mild-to-moderate obesity-related complication such as prediabetes, type 2 diabetes, metabolic syndrome, dyslipidemia, hypertension, non-alcoholic fatty liver disease, etc. | Must have a diagnosis of T2D within the previous 6 years by either a documented physician diagnosis, use of antidiabetic medication, or fasting glucose ≥ 126 mg/dL, and/or HbA1c ≥ 6.5%. |
| Additional criteria | Participants could not have a pacemaker or other battery-operated implant, no use or stable use (≥3 months on same dosage) of medications affecting body weight, and were not taking insulin. | Participants could not have a pacemaker or other battery-operated implant, no use or stable use (≥3 months on same dosage) of medications affecting body weight, and were not taking insulin. | Participants could not have a pacemaker or other battery-operated implant, no use or stable use (≥3 months on same dosage) of medications affecting body weight, and were not taking insulin. | No use or stable use (≥3 months on same dosage) of medications affecting body weight and were not taking insulin. |
| Characteristic | Mean ± SD or n (%) | ||||
|---|---|---|---|---|---|
| Present Study | NCT04014296 | NCT04745572 | NCT04392284 | NCT03832933 [14] | |
| Age (years) | 55.7 ± 11.3 | 62.0 ± 7.3 | 52.9 ± 12.7 | 53.1 ± 12.2 | 54.8 ± 10.9 |
| Race/Ethnicity | |||||
| Non-Hispanic White | 123 (49.2) | 31 (59.6) | 16 (30.2) | 10 (25.0) | 66 (63.5) |
| Non-Hispanic Black | 111 (44.6) | 19 (36.5) | 34 (64.2) | 29 (72.5) | 29 (27.9) |
| Asian | 6 (2.4) | 1 (1.9) | 1 (2.5) | 4 (3.8) | |
| Native Hawaiian or Pacific Islander | 1 (0.4) | 1 (1.0) | |||
| Other | 8 (3.2) | 2 (3.8) | 2 (3.8) | 4 (3.8) | |
| Sex | |||||
| Male | 63 (25.3) | 23 (44.2) | 8 (15.1) | 7 (17.5) | 25 (24.0) |
| Female | 186 (74.7) | 29 (55.8) | 45 (84.9) | 33 (82.5) | 79 (76.0) |
| Height (cm) | 166.9 ± 9.1 | 170.1 ± 9.9 | 164.3 ± 7.1 | 166.4 ± 9.7 | |
| Weight (kg) | 107.8 ± 23.1 | 111.8 ± 19.5 | 108.6 ± 24.9 | 106.0 ± 28.2 | 106.1 ± 21.7 |
| BMI (kg/m2) | 38.5 ± 6.7 | 38.5 ± 5.0 | 39.6 ± 7.6 | 37.6 ± 8.0 | 38.3 ± 6.4 |
| 25th percentile | 33.4 | 34.2 | 33.9 | 30.5 | 33.3 |
| 50th percentile | 37.3 | 38.2 | 39.4 | 35.2 | 37.0 |
| 75th percentile | 43.3 | 41.9 | 44.1 | 43.3 | 43.2 |
| WC (cm) | 117.8 ± 15.3 | 121.7 ± 13.1 | 118.4 ± 17.6 | 114.4 ± 18.8 | 117.0 ± 13.3 |
| n = 249 | Mean | SD |
|---|---|---|
| SBP | 134.3 | 15.4 |
| DBP | 85.2 | 9.7 |
| A1c | 6.4 | 1.1 |
| HDL-C | 49.7 | 13.4 |
| LDL-C | 103.1 | 34.8 |
| TC | 172.7 | 39.9 |
| BMI (kg/m2) | 38.5 | 6.7 |
| BF% | 45.8 | 9.0 |
| WC (cm) | 117.8 | 15.3 |
| Kaiser–Meyer–Olkin Measure of Sampling Adequacy | 0.528 |
| Approx. Chi-Square | 781.805 |
| df | 15 |
| Sig. | <0.001 |
| Factor | 1 | 2 | 3 |
|---|---|---|---|
| SBP | .864 | ||
| DBP | .643 | ||
| LDL | .991 | ||
| TC | .916 | ||
| BMI | .805 | ||
| WC | .974 |
| Factor | Corrected Item/Total Correlation | Cronbach’s Alpha |
|---|---|---|
| LDL-C | 0.91 | 0.95 |
| TC | ||
| BMI | 0.79 | 0.74 |
| WC | ||
| SBP | 0.56 | 0.67 |
| DBP |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ellison, K.M.; El Zein, A.; Reynolds, C.; Ehrlicher, S.E.; Clina, J.G.; Chui, T.-K.; Smith, K.A.; Hill, J.O.; Wyatt, H.R.; Sayer, R.D. Body Size Measurements Grouped Independently of Common Clinical Measures of Metabolic Health: An Exploratory Factor Analysis. Nutrients 2024, 16, 2874. https://doi.org/10.3390/nu16172874
Ellison KM, El Zein A, Reynolds C, Ehrlicher SE, Clina JG, Chui T-K, Smith KA, Hill JO, Wyatt HR, Sayer RD. Body Size Measurements Grouped Independently of Common Clinical Measures of Metabolic Health: An Exploratory Factor Analysis. Nutrients. 2024; 16(17):2874. https://doi.org/10.3390/nu16172874
Chicago/Turabian StyleEllison, Katie M., Aseel El Zein, Chelsi Reynolds, Sarah E. Ehrlicher, Julianne G. Clina, Tsz-Kiu Chui, Kimberly A. Smith, James O. Hill, Holly R. Wyatt, and R. Drew Sayer. 2024. "Body Size Measurements Grouped Independently of Common Clinical Measures of Metabolic Health: An Exploratory Factor Analysis" Nutrients 16, no. 17: 2874. https://doi.org/10.3390/nu16172874
APA StyleEllison, K. M., El Zein, A., Reynolds, C., Ehrlicher, S. E., Clina, J. G., Chui, T.-K., Smith, K. A., Hill, J. O., Wyatt, H. R., & Sayer, R. D. (2024). Body Size Measurements Grouped Independently of Common Clinical Measures of Metabolic Health: An Exploratory Factor Analysis. Nutrients, 16(17), 2874. https://doi.org/10.3390/nu16172874






