Food Avoidance beyond the Gluten-Free Diet and the Association with Quality of Life and Eating Attitudes and Behaviors in Adults with Celiac Disease
Abstract
1. Introduction
Background
2. Materials and Methods
2.1. Recruitment
2.2. Study Measures
2.3. Statistical Analysis
2.4. Ethical Approval
3. Results
3.1. Overall Survey Results
3.2. Avoiding Food
3.3. Avoiding Food and Specific Variables
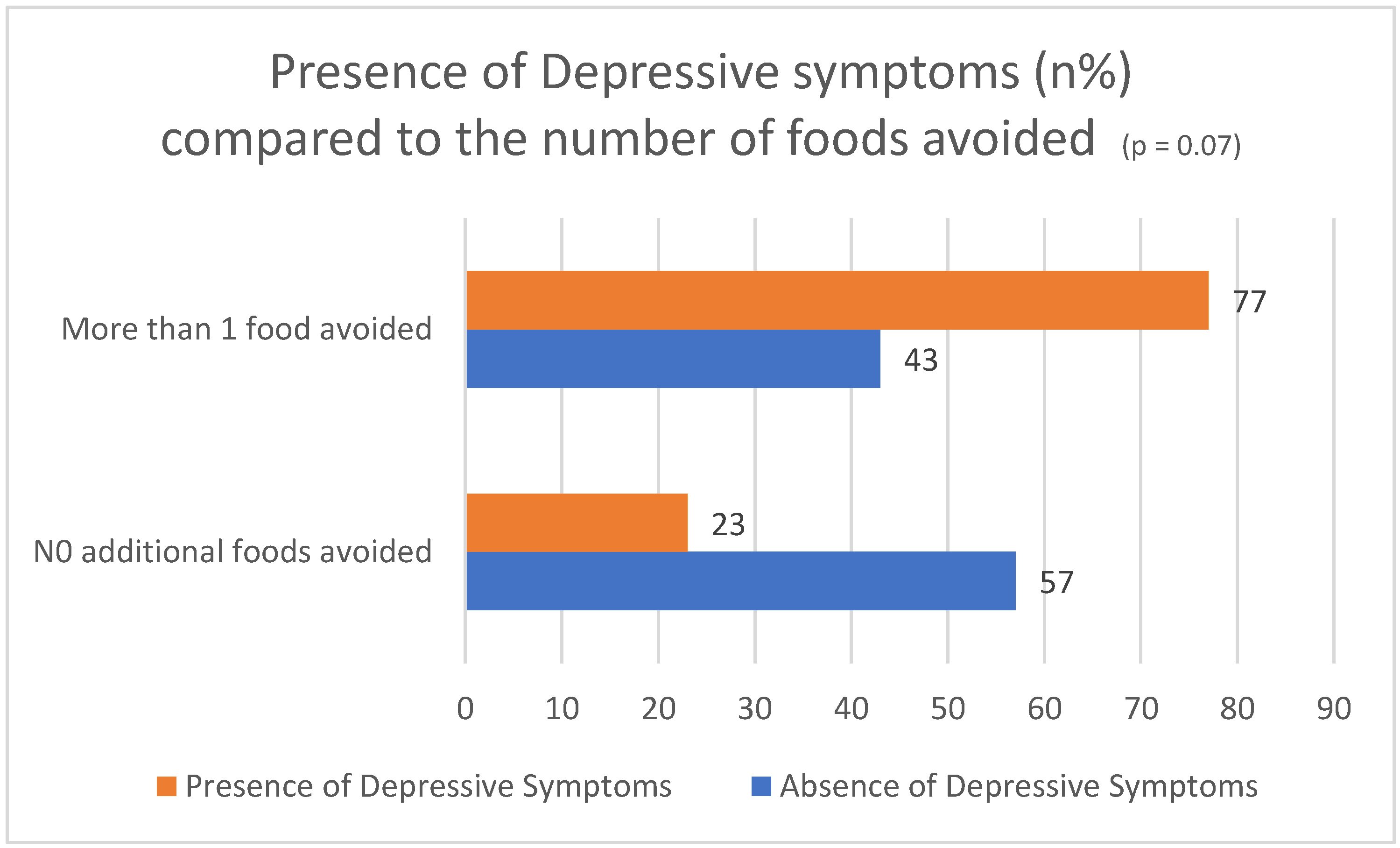
3.4. Thinking about Weight
3.5. Thinking about Food
4. Discussions
4.1. Limitations
4.2. Strengths
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Green, P.H.R.; Krishnareddy, S.; Lebwohl, B. Clinical manifestations of celiac disease. Dig. Dis. 2015, 33, 137–140. [Google Scholar] [CrossRef] [PubMed]
- Abu Daya, H.; Lebwohl, B.; Lewis, S.K.; Green, P.H. Celiac disease patients presenting with anemia have more severe disease than those presenting with diarrhea. Clin. Gastroenterol. Hepatol. 2013, 11, 14721477. [Google Scholar] [CrossRef] [PubMed]
- Green, P.H.R.; Jabri, B. Celiac Disease. Annu. Rev. Med. 2006, 57, 207–221. [Google Scholar] [CrossRef] [PubMed]
- Cellier, C.; Flobert, C.; Cormier, C.; Roux, C.; Schmitz, J. Severe osteopenia in symptom-free adults with a childhood diagnosis of coeliac disease. Lancet 2000, 355, 806. [Google Scholar] [CrossRef]
- Murray, J. The widening spectrum of celiac disease. Am. J. Clin. Nutr. 1999, 69, 354–365. [Google Scholar] [CrossRef]
- Rubio-Tapia, A.; Ludvigsson, J.F.; Brantner, T.L.; Murray, J.A.; Everhart, J.E. The prevalence of celiac disease in the United States. Am. J. Gastroenterol. 2012, 107, 1538–1545. [Google Scholar] [CrossRef]
- Lohi, S.; Mustalahti, K.; Kaukinen, K.; Laurila, K.; Collin, P.; Rissanen, H.; Lohi, O.; Bravi, E.; Gasparin, M.; Reunanen, A.; et al. Increasing prevalence of coeliac disease over time. Aliment. Pharmacol. Ther. 2007, 26, 1217–1225. [Google Scholar] [CrossRef]
- Ludvigsson, J.F.; Bai, J.C.; Biagi, F.; Card, T.R.; Ciacci, C.; Ciclitira, P.J.; Green, P.H.R.; Hadjivassiliou, M.; Holdoway, A.; van Heel, D.A.; et al. Diagnosis and management of adult coeliac disease: Guidelines from the British Society of Gastroenterology. Gut 2014, 63, 1210–1228. [Google Scholar] [CrossRef]
- Hornell, A. Effects of a gluten-free diet on gastrointestinal symptoms in celiac disease. Am. J. Clin. Nutr. 2005, 81, 1452–1453. [Google Scholar] [CrossRef][Green Version]
- Fabiani, E.; Catassi, C. The serum IgA class anti-tissue transglutaminase antibodies in the diagnosis and follow up of coeliac disease. Results of an international multi-centre study. International WorkingGroup on Eu-tTG. Eur. J. Gastroenterol. Hepatol. 2001, 13, 659–665. [Google Scholar] [CrossRef]
- Catassi, C.; Fabiani, E.; Iacono, G.; D’Agate, C.; Francavilla, R.; Biagi, F.; Volta, U.; Accomando, S.; Picarelli, A.; De Vitis, I.; et al. A prospective, double-blind, placebo-controlled trial to establish a safe gluten threshold for patients with celiac disease. Am. J. Clin. Nutr. 2007, 85, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.; Akbari, M.; Vanga, R.; Kelly, C.P.; Hansen, J.; Theethira, T.; Tariq, S.; Dennis, M.; A Leffler, D. Patient perception of treatment burden is high in celiac disease compared with other common conditions. Am. J. Gastroenterol. 2014, 109, 1304–1311. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.R.; Ng, D.L.; Diamond, B.; Ciaccio, E.J.; Green, P.H. Living with coeliac disease: Survey results from the U.S.A. J. Hum. Nutr. Diet. 2012, 25, 233–238. [Google Scholar] [CrossRef] [PubMed]
- Cranney, A.; Zarkadas, M.; Graham, I.D.; Butzner, J.D.; Rashid, M.; Warren, R.; Molloy, M.; Case, S.; Burrows, V.; Switzer, C. The Canadian Celiac Health Survey. Dig. Dis. Sci. 2007, 52, 1087–1095. [Google Scholar] [CrossRef] [PubMed]
- Black, J.L.; Orfila, C. Impact of celiac disease on dietary habits and quality of life. J. Hum. Nutr. Diet. 2011, 24, 582–587. [Google Scholar] [CrossRef] [PubMed]
- Gray, A.M.; Papanicolas, I.N. Impact of symptoms on quality of life before and after diagnosis of celiac disease: Results from a UK population survey. BMC Health Serv. Res. 2010, 10, 105. [Google Scholar] [CrossRef]
- Cadenhead, J.W.; Wolf, R.L.; Lebwohl, B.; Lee, A.R.; Zybert, P.; Reilly, N.R.; Schebendach, J.; Satherley, R.; Green, P.H.R. Diminished quality of life among adolescents with coeliac disease using maladaptive eating behaviours to manage a gluten-free diet: A cross-sectional, mixed-methods study. J. Hum. Nutr. Diet. 2019, 32, 311–320. [Google Scholar] [CrossRef]
- Sverker, A.; Hensing, G.; Hallert, C. ‘Controlled by food’-lived experiences of coeliac disease. J. Hum. Nutr. Diet. 2005, 18, 171–180. [Google Scholar] [CrossRef]
- Santonicola, A.; Gagliardi, M.; Guarino, M.P.L.; Siniscalchi, M.; Ciacci, C.; Iovino, P. Eating Disorders and Gastrointestinal Diseases. Nutrients 2019, 11, 3038. [Google Scholar] [CrossRef]
- Leffler, D.A.; Dennis, M.; Edwards George, J.B.; Kelly, C.P. The interaction between eating disorders and celiac disease: An exploration of 10 cases. Eur. J. Gastroenterol. Hepatol. 2007, 19, 251–255. [Google Scholar] [CrossRef]
- Mårild, K.; Størdal, K.; Bulik, C.M.; Rewers, M.; Ekbom, A.; Liu, E.; Ludvigsson, J.F. Celiac Disease and Anorexia Nervosa: A Nationwide Study. Pediatrics 2017, 139, e20164367. [Google Scholar] [CrossRef] [PubMed]
- Alkalay, M.J. Nutrition in Patients with Lactose Malabsorption, Celiac Disease, and Rel ated Disorders. Nutrients 2021, 14, 2. [Google Scholar] [CrossRef] [PubMed]
- Nacinovich, R.; Tremolizzo, L.; Corbetta, F.; Conti, E.; Neri, F.; Bomba, M. Anorexia nervosa of the restrictive type and celiac disease in adolescence. Neuropsychiatr. Dis. Treat. 2017, 13, 1211–1214. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Satherley, R.M.; Higgs, S.; Howard, R. Disordered eating patterns in coeliac disease: A framework analysis. J. Hum. Nutr. Diet. 2017, 30, 724–736. [Google Scholar] [CrossRef] [PubMed]
- Grilo, C. Eating and Weight Disorders; Psychology Press: New York, NY, USA, 2012. [Google Scholar]
- Arigo, D.; Anskis, A.M.; Smyth, J.M. Psychiatric comorbidities in women with celiac disease. Chronic Illn. 2012, 8, 45–55. [Google Scholar] [CrossRef]
- Rosen, J.C.; Ramirez, E. A comparison of eating disorders and body dysmorphic disorder on body image and psychological adjustment. J. Psychosom. Res. 1998, 44, 441–449. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- Gładyś, K.; Dardzińska, J.; Guzek, M.; Adrych, K.; Kochan, Z.; Małgorzewicz, S. Expanded Role of a Dietitian in Monitoring a Gluten-Free Diet in Patients with Celiac Disease: Implications for Clinical Practice. Nutrients 2021, 13, 1859. [Google Scholar] [CrossRef]
- Satherley, R.M.; Howard, R.; Higgs, S. The prevalence and predictors of disordered eating in women with coeliac disease. Appetite 2016, 107, 260–267. [Google Scholar] [CrossRef]
- Gholmie, Y.; Lee, A.R.; Satherley, R.M.; Schebendach, J.; Zybert, P.; Green, P.H.R.; Lebwohl, B.; Wolf, R. Maladaptive Food Attitudes and Behaviors in Individuals with Celiac Disease and Their Association with Quality of Life. Dig. Dis. Sci. 2023, 68, 2899–2907. [Google Scholar] [CrossRef]
- Leffler, D.A.; Dennis, M.; Edwards George, J.; Jamma, S.; Cook, E.F.; Schuppan, D.; Kelly, C.P. A validated disease-specific symptom index for adults with celiac disease. Clin. Gastroenterol. Hepatol. 2009, 7, 1328–1334.e3. [Google Scholar] [CrossRef]
- Dorn, S.D.; Hernandez, L.; Minayas, M.T.; Morris, C.B.; Hu, Y.; Leserman, J.; Lewis, S.; Lee, A.; Bangdiwala, S.I.; Green, P.H.R.; et al. The development and validation of a new coeliac disease quality of life survey (CD-QOL). Aliment. Pharmacol. Ther. 2009, 31, 666–675. [Google Scholar] [CrossRef] [PubMed]
- Radloff, L.S. The CES-D scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Spielberger, C.D.; Gorsuch, R.L.; Lushene, R.; Vagg, P.R. Manual for the State-Trait Anxiety Inventory; Consulting Psychologists Press: Palo Alto, CA, USA, 1983. [Google Scholar]
- Forbush, K.T.; Wildes, J.E.; Hunt, T.K. Gender norms, psychometric properties, and validity for the Eating Pathology Symptoms Inventory. Int. J. Eat. Disord. 2014, 47, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Satherley, R.M.; Howard, R.; Higgs, S. Development and Validation of the Coeliac Disease Food Attitudes and Behaviours Scale. Gastroenterol. Res. Pract. 2018, 2018, 6930269. [Google Scholar] [CrossRef]
- Latzer, I.T.; Lerner-Geva, L.; Stein, D.; Weiss, B.; Pinhas-Hamiel, O. Disordered eating behaviors in adolescents with celiac disease. Eat. Weight. Disord. 2018, 25, 365–371. [Google Scholar] [CrossRef]
- Lee, A.R.; Lebwohl, B.; Lebovits, J.; Wolf, R.L.; Ciaccio, E.J.; Green, P.H.R. Factors Associated with Maladaptive Eating Behaviors, Social Anxiety, and Quality of Life in Adults with Celiac Disease. Nutrients 2021, 13, 4494. [Google Scholar] [CrossRef]
- Lebovits, J.; Lee, A.R.; Ciaccio, E.J.; Wolf, R.L.; Davies, R.H.; Cerino, C.; Lebwohl, B.; Green, P.H.R. Impact of Celiac Disease on Dating. Dig. Dis. Sci. 2022, 67, 5158–5167. [Google Scholar] [CrossRef]
- Joelson, A.M.; Geller, M.G.; Zylberberg, H.M.; Green, P.H.R.; Lebwohl, B. The Effect of Depressive Symptoms on the Association between Gluten-Free Diet Adherence and Symptoms in Celiac Disease: Analysis of a Patient Powered Research Network. Nutrients 2018, 10, 538. [Google Scholar] [CrossRef]
- Fisher, M.; Zimmerman, J.; Bucher, C.; Yadlosky, L. ARFID at 10 years: A Review of Medical, Nutritional and Psychological Evaluation and Management. Curr. Gastroenterol. Rep. 2023, 25, 421–429. [Google Scholar] [CrossRef]
| Demographics | N (%) | |
|---|---|---|
| Gender | Female | 35 (70.0) |
| Male | 15 (30.0) | |
| Race | Asian | 2 (4.0) |
| Black | 1 (2.0) | |
| White | 47 (94.0) | |
| Education | Some college | 8 (16.0) |
| College graduate | 32 (64.0) | |
| Postgraduate | 10 (20.0) | |
| Household income | <USD 50,000/year | 4 (8.0) |
| USD 50–100,000/year | 11 (22.0) | |
| >USD 100,000/year | 31 (62) | |
| Did not disclose | 4 (8.0) | |
| Mean (SD) | ||
| Age at enrollment | 29.6 (7.4) | |
| Age at diagnosis | 22.8 (9.3) | |
| Years since diagnosis | 7.2 (5.3) | |
| BMI (kg/m2) | 23.2 (4.0) |
| 0 Foods Avoided N = 21 | 1+ Foods Avoided N = 29 | |||
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | t-Test | p | |
| Age at enrollment (yrs) | 30.1 (7.2) | 29.2 (7.7) | 0.4 | 0.664 |
| Years since CD diagnosis | 8.9 (6.0) | 6.0 (4.5) | 1.9 | 0.060 |
| BMI (kg/m2) | 23.5 (4.0) | 22.9 (4.1) | 0.6 | 0.559 |
| # GI symptoms past 24 h (CDSD) | 1.7 (1.5) | 2.1 (1.5) | −0.8 | 0.405 |
| Gluten-free diet adherence (CDAT) | 11.3 (2.6) | 12.3 (3.7) | −1.1 | 0.263 |
| # other dietary patterns followed | 0.1 (0.3) | 0.9 (1.1) | −3.2 | 0.002 |
| OVERALL quality of life (CD-QOL) | 70.2 (15.9) | 57.4 (23.2) | 2.2 | 0.034 |
| Dysphoria subscale | 82.7 (20.4) | 68.1 (28.5) | 2.0 | 0.050 |
| Limitations subscale | 66.8 (17.1) | 54.8 (25.1) | 1.9 | 0.064 |
| Health concerns subscale | 63.3 (22.2) | 52.5 (27.4) | 1.5 | 0.142 |
| Inadequate treatment subscale | 77.4 (31.3) | 59.5 (32.5) | 2.0 | 0.057 |
| Depression (CESD) | 13.6 (4.0) | 16.0 (4.9) | −1.8 | 0.078 |
| Anxiety state (STAI Adults) | 32.0 (11.6) | 41.2 (12.9) | −2.6 | 0.012 |
| Anxiety trait (STAI Adults) | 36.2 (9.2) | 42.3 (11.1) | −2.1 | 0.043 |
| Body dissatisfaction (EPSI) | 7.3 (7.1) | 11.7 (7.9) | −2.0 | 0.052 |
| Binge eating (EPSI) | 6.2 (6.1) | 9.5 (6.6) | −1.8 | 0.083 |
| Cognitive restraint (EPSI) | 4.0 (2.5) | 5.0 (2.9) | −1.3 | 0.200 |
| Purging (EPSI) | 0.1 (0.3) | 0.3 (1.0) | −1.1 | 0.294 |
| Restricting (EPSI) | 3.1 (4.7) | 6.1 (5.5) | −2.0 | 0.053 |
| Excessive exercise (EPSI) | 5.3 (5.7) | 5.8 (4.4) | −0.3 | 0.734 |
| Negative attitude toward obesity (EPSI) | 3.2 (4.8) | 3.9 (5.0) | −0.5 | 0.636 |
| Muscle building (EPSI) | 1.7 (2.6) | 2.5 (3.0) | −1.0 | 0.299 |
| CD-FAB TOTAL | 33.0 (13.7) | 39.9 (16.0) | −1.6 | 0.116 |
| Food attitude subscale | 13.1 (7.3) | 15.4 (7.4) | −1.1 | 0.271 |
| Fear response subscale | 7.4 (3.4) | 8.7 (4.5) | −1.1 | 0.274 |
| Adaptive response subscale | 12.4 (5.5) | 15.7 (6.0) | −2.0 | 0.055 |
| Thinking about eating and/or food | 2.7 (0.8) | 3.2 (1.0) | −1.9 | 0.068 |
| Thinking about your weight | 1.8 (1.1) | 2.6 (1.1) | −2.6 | 0.013 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, A.R.; Zybert, P.; Chen, Z.; Lebovits, J.; Wolf, R.L.; Lebwohl, B.; Green, P.H.R. Food Avoidance beyond the Gluten-Free Diet and the Association with Quality of Life and Eating Attitudes and Behaviors in Adults with Celiac Disease. Nutrients 2024, 16, 3411. https://doi.org/10.3390/nu16193411
Lee AR, Zybert P, Chen Z, Lebovits J, Wolf RL, Lebwohl B, Green PHR. Food Avoidance beyond the Gluten-Free Diet and the Association with Quality of Life and Eating Attitudes and Behaviors in Adults with Celiac Disease. Nutrients. 2024; 16(19):3411. https://doi.org/10.3390/nu16193411
Chicago/Turabian StyleLee, Anne R., Patricia Zybert, Zhijun Chen, Jessica Lebovits, Randi L. Wolf, Benjamin Lebwohl, and Peter H. R. Green. 2024. "Food Avoidance beyond the Gluten-Free Diet and the Association with Quality of Life and Eating Attitudes and Behaviors in Adults with Celiac Disease" Nutrients 16, no. 19: 3411. https://doi.org/10.3390/nu16193411
APA StyleLee, A. R., Zybert, P., Chen, Z., Lebovits, J., Wolf, R. L., Lebwohl, B., & Green, P. H. R. (2024). Food Avoidance beyond the Gluten-Free Diet and the Association with Quality of Life and Eating Attitudes and Behaviors in Adults with Celiac Disease. Nutrients, 16(19), 3411. https://doi.org/10.3390/nu16193411






