Evaluation of the Impact of a Midwife-Led Breastfeeding Group Intervention on Prevention of Postpartum Depression: A Multicentre Randomised Clinical Trial
Abstract
1. Introduction
2. Materials and Methods
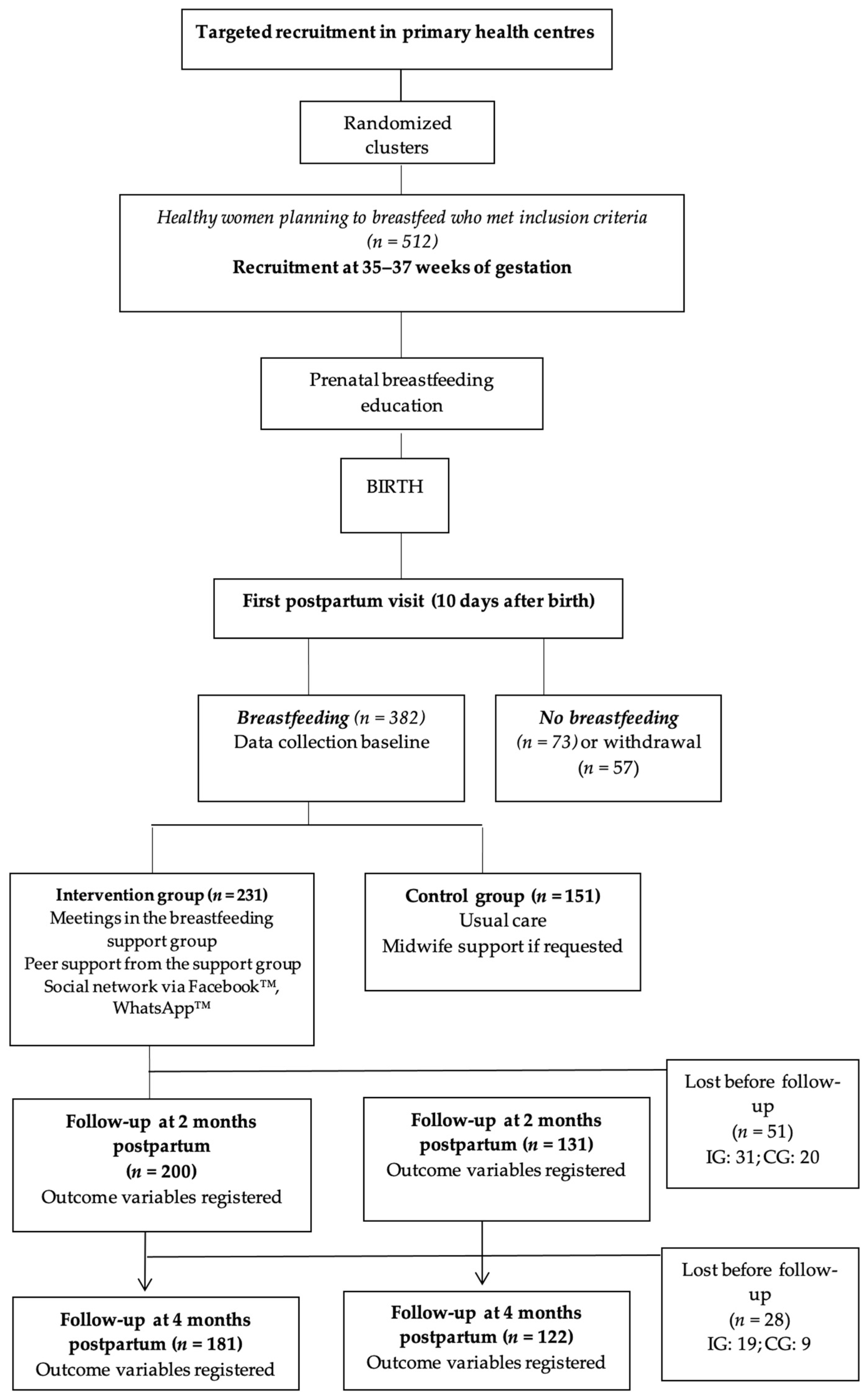
2.1. Study Design
2.2. Participants and Study Area
2.3. Inclusion and Exclusion Criteria
- Healthy women performing exclusive or partial breastfeeding 10 days after birth and who attended antenatal lessons at the primary health center;
- Women over 18 years of age;
- Women who accepted and signed the informed consent form.
- Human immunodeficiency virus-positive;
- Cancer;
- Tuberculosis infection;
- No intention to breastfeed;
- Impossibility or contraindication to breastfeed due to medical conditions;
- Premature and/or complicated labour or newborn in a neonatal intensive care unit during the first month of life;
- Communication difficulties due to language barriers.
2.4. Sample Size
2.5. Randomisation and Recruitment
2.6. Intervention
2.7. Assessment
- Sociodemographic variables: maternal age, country of origin, civil status (single, married, separated, widow), educational level (none, primary school, secondary school, university), employment status (self-employed, employed, unemployed);
- Obstetric variables: parity (primiparous, multiparous), gestational age, labour onset (induction, spontaneous), type of birth (eutocic, instrumental, elective caesarean section, emergent caesarean section), newborn sex, birth weight.
2.8. Data Collection
2.9. Data Analysis
2.10. Ethical Considerations
3. Results
3.1. Characteristics of the Sample
3.2. Sociodemographic and Obstetric–Neonatal Variables
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhao, X.H.; Zhang, Z.H. Risk factors for postpartum depression: An evidence-based systematic review of systematic reviews and meta-analyses. Asian J. Psychiatry 2020, 53, 102353. [Google Scholar] [CrossRef] [PubMed]
- Banti, S.; Mauri, M.; Oppo, A.; Borri, C.; Rambelli, C.; Ramacciotti, D.; Montagnani, M.S.; Camilleri, V.; Cortopassi, S.; Rucci, P.; et al. From the third month of pregnancy to 1 year postpartum. Prevalence, incidence, recurrence, and new onset of depression. Results from the perinatal depression-research & screening unit study. Compr. Psychiatry 2011, 52, 343–351. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Wu, X.; Lai, W.; Long, E.; Zhang, X.; Li, W.; Zhu, Y.; Chen, C.; Zhong, X.; Liu, Z.; et al. Prevalence of depression and depressive symptoms among outpatients: A systematic review and meta-analysis. BMJ Open 2017, 7, e017173. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, TX, USA, 2014; pp. 123–125. [Google Scholar]
- Wang, Z.; Liu, J.; Shuai, H.; Cai, Z.; Fu, X.; Liu, Y.; Xiao, X.; Zhang, W.; Krabbendam, E.; Liu, S.; et al. Mapping global prevalence of depression among postpartum women. Transl. Psychiatry 2021, 11, 543, Erratum in Transl. Psychiatry 2021, 11, 640. [Google Scholar] [CrossRef] [PubMed]
- Payn, J.L.; Maguire, J. Pathophysiological mechanisms implicated in postpartum depression. Front. Neuroendocrinol. 2019, 52, 165–180. [Google Scholar] [CrossRef] [PubMed]
- De la Fe Rodríguez-Muñoz, M.; Le, H.N.; de la Cruz, I.V.; Crespo, M.E.O.; Méndez, N.I. Feasibility of screening and prevalence of prenatal depression in an obstetric setting in Spain. Eur. J. Obstet. Gynecol. Reprod. Biol. 2017, 215, 101–105. [Google Scholar] [CrossRef] [PubMed]
- O’Hara, M.W.; Wisner, K.L. Perinatal mental illness: Definition, description and aetiology. Best Pract. Res. Clin. Obstet. Gynaecol. 2014, 28, 3–12. [Google Scholar] [CrossRef]
- Bruist, A. Perinatal mental health: A guide to the Edinburgh Postnatal Depression Scale. Arch. Women’s Ment. Health 2004, 7, 96. [Google Scholar]
- Mayberry, L.J.; Horowitz, J.A.; Declercq, E. Depression symptom prevalence and demographic risk factors among U.S. women during the first 2 years postpartum. J. Obstet. Gynecol. Neonatal Nurs. 2007, 36, 542–549. [Google Scholar] [CrossRef]
- Department of Health and Human Service Office on Women’s Health. Benefits of breastfeeding. Nutr. Clin. Care 2003, 3, 125–131. [Google Scholar]
- Binns, C.; Lee, M.; Low, W.Y. The Long-Term Public Health Benefits of Breastfeeding. Asia Pac. J. Public Health 2016, 1, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, R.; Sinha, B.; Sankar, M.J.; Taneja, S.; Bhandari, N.; Rollins, N.; Bahl, R.; Martines, J. Breastfeeding and maternal health outcomes: A systematic review and meta-analysis. Acta Paediatry 2015, 467, 96–113. [Google Scholar] [CrossRef]
- Pang, W.W.; Hartmann, P.E. Initiation of human lactation: Secretory differentiation and secretory activation. J. Mammary Gland Biol. Neoplasia 2007, 12, 211–221. [Google Scholar] [CrossRef] [PubMed]
- Stefaniak, M.; Dmoch-Gajzlerska, E.; Jankowska, K.; Rogowski, A.; Kajdy, A.; Maksym, R.B. Progesterone and Its Metabolites Play a Beneficial Role in Affect Regulation in the Female Brain. Pharmaceuticals 2023, 16, 520. [Google Scholar] [CrossRef] [PubMed]
- Figueiredo, B.; Dias, C.C.; Brandão, S.; Canário, C.; Nunes-Costa, R. Breastfeeding and postpartum depression: State of the art review. J. Pediatr. 2013, 89, 332–338. [Google Scholar] [CrossRef]
- Xia, M.; Luo, J.; Wang, J.; Liang, Y. Association between breastfeeding and postpartum depression: A meta-analysis. J. Affect. Disord. 2022, 308, 512–519. [Google Scholar] [CrossRef] [PubMed]
- Dennis, C.L.; Boyce, P. Further psychometric testing of a brief personality scale to measure vulnerability to postpartum depression. J. Psychosom. Obstet. Gynaecol. 2004, 25, 305–311. [Google Scholar] [CrossRef] [PubMed]
- Gillis, B.D.; Parish, A.L. Group-based interventions for postpartum depression: An integrative review and conceptual model. Arch. Psychiatry Nurs. 2019, 33, 290–298. [Google Scholar] [CrossRef]
- Rodríguez-Gallego, I.; Leon-Larios, F.; Corrales-Gutierrez, I.; González-Sanz, J.D. Impact and Effectiveness of Group Strategies for Supporting Breastfeeding after Birth: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 2550. [Google Scholar] [CrossRef]
- Nishioka, E.; Haruna, M.; Ota, E.; Matsuzaki, M.; Murayama, R.; Yoshimura, K.; Murashima, S. A prospective study of the relationship between breastfeeding and postpartum depressive symptoms appearing at 1–5 months after delivery. J. Affect. Disord. 2011, 133, 553–559. [Google Scholar] [CrossRef]
- Pope, C.J.; Mazmanian, D. Breastfeeding and Postpartum Depression: An Overview and Methodological Recommendations for Future Research. Depress. Res. Treat. 2016, 2016, 4765310. [Google Scholar] [CrossRef] [PubMed]
- McCoach, D.B.; Gable, R.K.; Madura, J.P. Instrument Development in the Affective Domain. School and Corporate Applications, 3rd ed.; Springer: New York, NY, USA, 2013. [Google Scholar]
- Bandura, A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol. Rev. 1977, 2, 191–215. [Google Scholar] [CrossRef]
- Han, L.; Zhang, J.; Yang, J.; Yang, X.; Bai, H. Between Personality Traits and Postpartum Depression: The Mediated Role of Maternal Self-Efficacy. Neuropsychiatr. Dis. Treat. 2022, 18, 597–609. [Google Scholar] [CrossRef] [PubMed]
- Henshaw, E.J. Breastfeeding and Postpartum Depression: A Review of Relationships and Potential Mechanisms. Curr. Psychiatry Rep. 2023, 31, 803–808. [Google Scholar] [CrossRef] [PubMed]
- Pezley, L.; Cares, K.; Duffecy, J.; Koenig, M.D.; Maki, P.; Odoms-Young, A.; Clark Withington, M.H.; Lima Oliveira, M.; Loiacono, B.; Prough, J.; et al. Efficacy of behavioral interventions to improve maternal mental health and breastfeeding outcomes: A systematic review. Int. Breastfeed J. 2022, 17, 67. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Hopewell, S.; Schulz, K.F.; Montori, V.; Gøtzsche, P.C.; Devereaux, P.; Elbourne, D.; Egger, M.; Altman, D.G. CONSORT 2010 explanation and elaboration: Updated guidelines for reporting parallel group randomised trials. BMJ 2010, 340, c869. [Google Scholar] [CrossRef]
- Rodríguez-Gallego, I.; Leon-Larios, F.; Ruiz-Ferrón, C.; Lomas-Campos, M.D. Evaluation of the impact of breastfeeding support groups in primary health CENTRES in Andalusia, Spain: A study protocol for a cluster randomized controlled trial (GALMA project). BMC Public Health 2020, 20, 1129, Erratum in BMC Public Health 2020, 20, 1445. [Google Scholar] [CrossRef]
- Instituto Nacional de Estadística. Oficina Estadística Española. Registro INE 2021. Available online: https://www.ine.es/jaxiT3/Datos.htm?t=1433#!tabs-tabla (accessed on 20 July 2023).
- Instituto Nacional de Estadística (INE). Series Detalladas Desde 2002. Población Residente por fecha, Sexo, Grupo de edad y Nacionalidad (Agrupación de Países). Oficina Estadística Española. Registro INE 2022. Available online: https://www.ine.es/jaxiT3/Datos.htm?t=9689 (accessed on 20 July 2023).
- Instituto de Estadística y Cartografía de Andalucía. Movimiento Natural de la Población (MNP) 2022. Available online: https://www.juntadeandalucia.es/institutodeestadisticaycartografia/dega/movimiento-natural-de-la-poblacion-mnp/nota-divulgativa-datos-definitivos-2022 (accessed on 2 January 2024).
- Instituto Nacional de Estadística (INE). Movimiento Natural de la Población: Nacimientos. Fenómenos Demográficos por Comunidades y Ciudades Autónomas y tipo de Fenómeno Demográfico. Oficina Estadística Española. Registro INE 2021. Available online: https://www.ine.es/jaxiT3/Datos.htm?t=6567 (accessed on 20 July 2023).
- Ministerio de Sanidad. Encuesta Nacional de Salud de España 2017 (ENSE 2017). Determinantes de Salud. Tipo de Lactancia. Tabla 3.078. Según Sexo y Clase Social Basada en la Ocupación de la Persona de Referencia. Available online: https://www.sanidad.gob.es/estadEstudios/estadisticas/encuestaNacional/encuestaNac2017/ENSE17_MOD3_REL.pdf (accessed on 20 July 2023).
- Nabulsi, M.; Hamadeh, H.; Tamim, H.; Kabakian, T.; Charafeddine, L.; Yehya, N.; Sinno, D.; Sidani, S. A complex breastfeeding promotion and support intervention in a developing country: Study protocol for a randomized clinical trial. BMC Public Health 2014, 14, 36. [Google Scholar] [CrossRef]
- Rollins, N.C.; Bhandari, N.; Hajeebhoy, N.; Horton, S.; Lutter, C.K.; Martines, J.C.; Piwoz, E.G.; Richter, L.M.; Victora, C.G.; Lancet Breastfeeding Series Group. Why invest, and what it will take to improve breastfeeding practices? Lancet 2016, 387, 491–504. [Google Scholar] [CrossRef]
- Guillaumes, S.; O’Callaghan, C. Versión en español del software gratuito OxMaR para minimización y aleatorización de estudios clínicos. Gac. Sanit. 2019, 33, 395–397. [Google Scholar] [CrossRef]
- Aceituno, L.; Maldonado, J.; Arribas, L.; Caño, A.; Corona, I.; Martín, J.E.; Mora, M.A.; Morales, L.; Ras, J.; Sánchez, T.; et al. Embarazo, Parto y Puerperio. Proceso Asistencial Integrado, 3rd ed.; Consejería De Igualdad, Salud y Políticas Sociales: Junta de Andalucía, Spain, 2014; pp. 24–46. [Google Scholar]
- World Health Organization; UNICEF. Protecting, Promoting, and Supporting Breastfeeding in Facilities Providing Maternity and Newborn Services: The Revised Baby-Friendly Hospital Initiative 2018; Implementation guidance; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- Robinson, A.; Lauckner, C.; Davis, M.; Hall, J.; Anderson, A.K. Facebook support for breastfeeding mothers: A comparison to offline support and associations with breastfeeding outcomes. Digit. Health 2019, 5, 2055207619853397. [Google Scholar] [CrossRef] [PubMed]
- Cox, J.L.; Holden, J.M.; Sagovsky, R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry 1987, 150, 782–786. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Esteve, L.; Ascaso, C.; Ojuel, J.; Navarro, P. Validation of the Edinburgh Postnatal Depression Scale (EPDS) in Spanish mothers. J. Affect. Disord. 2003, 75, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Gutierrez-Zotes, A.; Gallardo-Pujol, D.; Labad, J.; Martín-Santos, R.; García-Esteve, L.; Gelabert, E.; Jover, M.; Guillamat, R.; Mayoral, F.; Gornemann, I.; et al. Factor Structure of the Spanish Version of the Edinburgh Postnatal Depression Scale. Actas Esp. Psiquiatr. 2018, 46, 174–182. [Google Scholar] [PubMed]
- Baessler, J.; Schwarcer, R. Evaluación de la autoeficacia: Adaptación española de la escala de Autoeficacia General. Actas Esp. Psiquiatr. 1996, 2, 174–182. [Google Scholar]
- Sanjuán, P.; Pérez, A.M.; Bermúdez, J. Escala de autoeficacia general: Datos psicométricos de la adaptación para población española. Psicothema 2000, 12, 509–513. [Google Scholar]
- Moore, E.R.; Bergman, N.; Anderson, G.C.; Medley, N. Early skin-to-skin contact for mothers and their healthy newborn infants. Cochrane Database Syst. Rev. 2016, 11, CD003519. [Google Scholar] [CrossRef] [PubMed]
- Niwayama, R.; Nishitani, S.; Takamura, T.; Shinohara, K.; Honda, S.; Miyamura, T.; Nakao, Y.; Oishi, K.; Araki-Nagahashi, M. Oxytocin Mediates a Calming Effect on Postpartum Mood in Primiparous Mothers. Breastfeed Med. 2017, 12, 103–109. [Google Scholar] [CrossRef]
- Nejsum, F.M.; Måstrup, R.; Torp-Pedersen, C.; Løkkegaard, E.C.L.; Wiingreen, R.; Hansen, B.M. Exclusive breastfeeding: Relation to gestational age, birth weight, and early neonatal ward admission. A nationwide cohort study of children born after 35 weeks of gestation. PLoS ONE 2023, 18, e0285476. [Google Scholar] [CrossRef]
- Fan, H.S.L.; Wong, J.Y.H.; Fong, D.Y.T.; Lok, K.Y.W.; Tarrant, M. Association between early-term birth and breastfeeding initiation, duration, and exclusivity: A systematic review. Birth 2019, 46, 24–34. [Google Scholar] [CrossRef]
- Toledo, C.; Cianelli, R.; Villegas Rodriguez, N.; De Oliveira, G.; Gattamorta, K.; Wojnar, D.; Ojukwu, E. The significance of breastfeeding practices on postpartum depression risk. Public Health Nurs. 2022, 39, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Bascom, E.M.E.; Napolitano, M.A. Breastfeeding Duration and Primary Reasons for Breastfeeding Cessation among Women with Postpartum Depressive Symptoms. J. Hum. Lact. 2016, 32, 282–291. [Google Scholar] [CrossRef] [PubMed]
- Franco-Antonio, C.; Santano-Mogena, E.; Sánchez-García, P.; Chimento-Díaz, S.; Cordovilla-Guardia, S. Effect of a brief motivational intervention in the immediate postpartum period on breastfeeding self-efficacy: Randomized controlled trial. Res. Nurs. Health 2021, 44, 295–307. [Google Scholar] [CrossRef] [PubMed]
- Franco-Antonio, C.; Calderón-García, J.F.; Santano-Mogena, E.; Rico-Martín, S.; Cordovilla-Guardia, S. Effectiveness of a brief motivational intervention to increase the breastfeeding duration in the first 6 months postpartum: Randomized controlled trial. J. Adv. Nurs. 2020, 76, 888–902. [Google Scholar] [CrossRef] [PubMed]
- Leon-Larios, F.; Pinero-Pinto, E.; Arnedillo-Sanchez, S.; Ruiz-Ferron, C.; Casado-Mejia, R.; Benitez-Lugo, M. Female employees’ perception of breastfeeding-friendly support in a public university in Spain. Public Health Nurs. 2019, 36, 370–378. [Google Scholar] [CrossRef]
- Oliver-Roig, A.; d’Anglade-González, M.L.; García-García, B.; Silva-Tubio, J.R.; Richart-Martínez, M.; Dennis, C.L. The Spanish version of the Breastfeeding Self-Efficacy Scale-Short Form: Reliability and validity assessment. Int. J. Nurs. Study 2012, 49, 169–173. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, I.M.S.; Kronborg, H.; Rahbek, K.; Strandberg-Larsen, K. The significance of early breastfeeding experiences on breastfeeding self-efficacy one week postpartum. Matern. Child Nutr. 2020, 16, e12986. [Google Scholar] [CrossRef]
- Tseng, J.F.; Chen, S.R.; Au, H.K.; Chipojola, R.; Lee, G.T.; Lee, P.H.; Shyu, M.L.; Kuo, S.Y. Effectiveness of an integrated breastfeeding education program to improve self-efficacy and exclusive breastfeeding rate: A single-blind, randomised controlled study. Int. J. Nurs. Study 2020, 111, 103770. [Google Scholar] [CrossRef]
- Jablotschkin, M.; Binkowski, L.; Markovits Hoopii, R.; Weis, J. Benefits and challenges of cancer peer support groups: A systematic review of qualitative studies. Eur. J. Cancer Care 2022, 31, e13700. [Google Scholar] [CrossRef]
- Grubesic, T.H.; Durbin, K.M. Geodemographies of Breastfeeding Support. J. Hum. Lact. 2021, 37, 301–313. [Google Scholar] [CrossRef]
- Li, R.; Scanlon, K.S.; Serdula, M.K. The validity and reliability of maternal recall of breastfeeding practice. Nutr. Rev. 2005, 63, 103–110. [Google Scholar] [CrossRef] [PubMed]
| Control Group n = 151 (39.5%) | Intervention Group n = 231 (60.5%) | p-Value * | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Country of origin | Spain | 142 | 94 | 215 | 93.1 | 0.709 |
| Foreign | 9 | 6 | 16 | 6.9 | ||
| Civil status | Single | 73 | 48.3 | 95 | 41.1 | 0.326 |
| Married | 76 | 50.3 | 134 | 58 | ||
| Separate | 2 | 1.3 | 2 | 0.9 | ||
| Widow | 0 | 0 | 0 | 0 | ||
| Educational level | None | 0 | 0 | 1 | 0.4 | 0.846 |
| Primary school | 5 | 3.3 | 9 | 3.9 | ||
| Secondary school | 47 | 31.1 | 74 | 32 | ||
| University | 99 | 65.6 | 147 | 63.6 | ||
| Employment status | Self-employed | 11 | 7.3 | 27 | 11.7 | 0.353 |
| Employed | 97 | 64.2 | 138 | 59.7 | ||
| Unemployed | 43 | 28.5 | 66 | 28.6 | ||
| Parity | Primiparous | 87 | 57.6 | 119 | 51.5 | 0.242 |
| Multiparous | 64 | 42.4 | 112 | 48.5 | ||
| Previous BF experience | No | 93 | 61.6 | 128 | 55.4 | 0.232 |
| Yes | 58 | 38.4 | 103 | 44.6 | ||
| Labour onset | Induction | 61 | 40.4 | 89 | 38.5 | 0.715 |
| Spontaneous | 90 | 59.6 | 142 | 61.5 | ||
| Type of birth | Eutocic | 96 | 63.6 | 140 | 60.6 | 0.411 |
| Instrumental | 26 | 17.2 | 51 | 22.1 | ||
| Elective CS | 5 | 3.3 | 12 | 5.2 | ||
| Emergent CS | 24 | 15.9 | 28 | 12.1 | ||
| E-SSC | No | 25 | 16.6 | 21 | 9.1 | 0.028 |
| Yes | 126 | 83.4 | 210 | 90.9 | ||
| Newborn sex | Male | 79 | 52.3 | 116 | 50.2 | 0.688 |
| Female | 72 | 47.7 | 115 | 49.8 | ||
| Type of feeding at discharge (n = 382) | EBF | 121 | 80.1 | 178 | 77.1 | 0.841 |
| BF with OH | 17 | 11.3 | 32 | 13.8 | ||
| Mixed | 13 | 8.6 | 21 | 9.1 | ||
| Formula | - | - | - | - | ||
| Type of feeding T1 (n = 382) | EBF | 118 | 78.1 | 180 | 77.9 | 0.960 |
| BF with OH | 20 | 13.3 | 31 | 13.4 | ||
| Mixed | 13 | 8.6 | 20 | 8.7 | ||
| Formula | - | - | - | - | ||
| Type of feeding T2 (n = 331) | EBF | 84 | 64.1 | 146 | 73 | 0.335 |
| BF with OH | 14 | 10.7 | 18 | 9 | ||
| Mixed | 19 | 14.5 | 23 | 11.5 | ||
| Formula | 14 | 10.7 | 13 | 6.5 | ||
| Type of feeding T3 (n = 303) | EBF | 61 | 50 | 128 | 69.9 | <0.001 |
| BF with OH | 13 | 10.7 | 21 | 11.60 | ||
| Mixed | 22 | 18 | 12 | 6.62 | ||
| Formula | 26 | 21.3 | 20 | 10.9 | ||
| Quantitative Variables | Group | n | Mean | SD | p-value ** | |
| Maternal age (year) | CG | 151 | 33.28 | 5.03 | 0.063 | |
| IG | 231 | 33.50 | 4.41 | |||
| Gestational age (week) | CG | 151 | 39.46 | 1.38 | 0.820 | |
| IG | 231 | 39.45 | 1.14 | |||
| Birth weight (gram) | CG | 151 | 3299 | 430 | 0.819 | |
| IG | 230 | 3253 | 437 | |||
| EPDS T1 (n = 382) | CG | 151 | 12.65 | 3.68 | 0.090 | |
| IG | 231 | 12.11 | 3.26 | |||
| EPDS T2 (n = 331) | CG | 131 | 12.50 | 3.66 | 0.487 | |
| IG | 200 | 12.62 | 3.70 | |||
| EPDS T3 (n = 303) | CG | 122 | 13.39 | 4.00 | 0.116 | |
| IG | 181 | 12.49 | 3.63 | |||
| GSE T1 (n = 382) | CG | 151 | 78.59 | 14.36 | 0.699 | |
| IG | 231 | 79.58 | 13.87 | |||
| GSE T2 (n = 331) | CG | 131 | 75.65 | 14.39 | 0.607 | |
| IG | 200 | 77.73 | 14.81 | |||
| GSE T3 (n = 303) | CG | 122 | 75.36 | 15.17 | 0.881 | |
| IG | 181 | 76.46 | 15.26 | |||
| Group | Total | p-Value * | ||||
|---|---|---|---|---|---|---|
| CG | IG | |||||
| EBF T1 (n = 382) | No | n | 33 | 51 | 84 | 0.959 |
| % | 21.90 | 22.10 | 22.00 | |||
| Yes | n | 118 | 180 | 298 | ||
| % | 78.10 | 77.90 | 78.00 | |||
| EBF T2 (n = 331) | No | n | 47 | 54 | 101 | 0.086 |
| % | 35.90 | 27.00 | 30.50 | |||
| Yes | n | 84 | 146 | 230 | ||
| % | 64.10 | 73.00 | 69.50 | |||
| EBF T3 (n = 303) | No | n | 61 | 53 | 114 | <0.001 |
| % | 50.00 | 29.28 | 37.62 | |||
| Yes | n | 61 | 128 | 189 | ||
| % | 50.00 | 70.72 | 62.38 | |||
| n | Mean | SD | 95% CI | Minimum | Maximum | F | p-Value * | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Upper Limit | Lower Limit | |||||||||
| EPDS T1 | CG | 151 | 12.65 | 3.686 | 12.06 | 13.24 | 6 | 23 | 2.258 | 0.134 |
| IG | 231 | 12.11 | 3.268 | 11.68 | 12.53 | 6 | 23 | |||
| Total | 382 | 12.32 | 3.445 | 11.98 | 12.67 | 6 | 23 | |||
| EPDS T2 | CG | 131 | 12.50 | 3.666 | 11.87 | 13.14 | 6 | 24 | 0.072 | 0.789 |
| IG | 200 | 12.62 | 3.702 | 12.10 | 13.13 | 6 | 22 | |||
| Total | 331 | 12.57 | 3.683 | 12.17 | 12.97 | 6 | 24 | |||
| EPDS T3 | CG | 122 | 13.39 | 4.001 | 12.67 | 14.10 | 6 | 23 | 4.077 | 0.044 |
| IG | 181 | 12.49 | 3.636 | 11.96 | 13.02 | 6 | 24 | |||
| Total | 303 | 12.85 | 3.805 | 12.42 | 13.28 | 6 | 24 | |||
| Levene’s Test for Equality of Variances | t-Test for Equality of Means | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| F | p-Value | t | df | Significance | Mean Difference | Standard Error of Difference | 95% CI | |||||||||
| n | Mean | SD | Standard Error of the Mean | One-Way p-Value | Two-Way p-Value | Lower | Upper | |||||||||
| EBF T1 | EPDS T1 | No | 84 | 12.4 | 3.1 | 0.3 | 1.006 | 0.317 | 0.285 | 380 | 0.388 | 0.776 | 0.121 | 0.426 | −0.716 | 0.959 |
| Yes | 298 | 12.3 | 3.5 | 0.2 | ||||||||||||
| GSE T1 | No | 84 | 80.2 | 12.1 | 1.3 | 1.799 | 0.181 | 0.744 | 380 | 0.229 | 0.457 | 1.293 | 1.738 | −2.123 | 4.709 | |
| Yes | 298 | 78.9 | 14.6 | 0.8 | ||||||||||||
| EBF T2 | EPDS T2 | No | 101 | 13.5 | 3.9 | 0.4 | 2.180 | 0.141 | 3.165 | 329 | 0.001 | 0.002 | 1.373 | 0.434 | 0.519 | 2.226 |
| Yes | 230 | 12.2 | 3.5 | 0.2 | ||||||||||||
| GSE T2 | No | 101 | 74.3 | 15.2 | 1.5 | 0.281 | 0.596 | −2.202 | 329 | 0.014 | 0.028 | −3.831 | 1.740 | −7.253 | −0.408 | |
| Yes | 230 | 78.1 | 14.3 | 0.9 | ||||||||||||
| EBF T3 | EPDS T3 | No | 116 | 14.1 | 3.7 | 0.3 | 0.023 | 0.880 | 4.656 | 303 | <0.001 | <0.001 | 2.015 | 0.433 | 1.163 | 2.867 |
| Yes | 187 | 12.1 | 3.6 | 0.3 | ||||||||||||
| GSE T3 | No | 116 | 72.4 | 15.9 | 1.5 | 1.121 | 0.291 | −3.318 | 303 | <0.001 | <0.001 | −5.587 | 1.809 | −9.331 | −2.384 | |
| Yes | 187 | 78.3 | 14.4 | 1.0 | ||||||||||||
| β | Standard Error | Wald | df | p-Value | Exp (β) | 95% CI | |||
|---|---|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||||
| T1 | E-SSC (No) | −0.839 | 0.341 | 6.047 | 1.000 | 0.014 | 0.432 | 0.221 | 0.843 |
| Gestational age | 0.164 | 0.097 | 2.866 | 1.000 | 0.090 | 1.178 | 0.975 | 1.424 | |
| EPDS T1 | −0.011 | 0.036 | 0.085 | 1.000 | 0.770 | 0.989 | 0.921 | 1.063 | |
| GSE T1 | −0.007 | 0.009 | 0.591 | 1.000 | 0.442 | 0.993 | 0.975 | 1.011 | |
| Intervention (No) | 0.083 | 0.259 | 0.102 | 1.000 | 0.749 | 1.086 | 0.653 | 1.807 | |
| Constant | −4.392 | 3.924 | 1.252 | 1.000 | 0.263 | 0.012 | |||
| T2 | E-SSC (No) | −0.333 | 0.376 | 0.781 | 1.000 | 0.377 | 0.717 | 0.343 | 1.499 |
| Gestational age | 0.043 | 0.101 | 0.177 | 1.000 | 0.674 | 1.044 | 0.856 | 1.273 | |
| EPDS T2 | −0.089 | 0.035 | 6.315 | 1.000 | 0.012 | 0.915 | 0.853 | 0.981 | |
| GSE T2 | 0.009 | 0.009 | 1.028 | 1.000 | 0.311 | 1.009 | 0.992 | 1.026 | |
| Intervention (No) | −0.403 | 0.249 | 2.612 | 1.000 | 0.106 | 0.668 | 0.410 | 1.090 | |
| Constant | −0.187 | 4.044 | 0.002 | 1.000 | 0.963 | 0.829 | |||
| T3 | E-SSC (No) | −0.737 | 0.397 | 3.438 | 1.000 | 0.064 | 0.479 | 0.220 | 1.043 |
| Gestational age | 0.069 | 0.105 | 0.430 | 1.000 | 0.512 | 1.072 | 0.872 | 1.317 | |
| EPDS T3 | −0.120 | 0.039 | 9.406 | 1.000 | 0.002 | 0.887 | 0.822 | 0.958 | |
| GSE T3 | 0.011 | 0.010 | 1.189 | 1.000 | 0.275 | 1.011 | 0.992 | 1.030 | |
| Intervention (No) | −0.746 | 0.255 | 8.566 | 1.000 | 0.003 | 0.474 | 0.288 | 0.782 | |
| Constant | −1.076 | 4.292 | 0.063 | 1.000 | 0.802 | 0.341 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodríguez-Gallego, I.; Vila-Candel, R.; Corrales-Gutierrez, I.; Gomez-Baya, D.; Leon-Larios, F. Evaluation of the Impact of a Midwife-Led Breastfeeding Group Intervention on Prevention of Postpartum Depression: A Multicentre Randomised Clinical Trial. Nutrients 2024, 16, 227. https://doi.org/10.3390/nu16020227
Rodríguez-Gallego I, Vila-Candel R, Corrales-Gutierrez I, Gomez-Baya D, Leon-Larios F. Evaluation of the Impact of a Midwife-Led Breastfeeding Group Intervention on Prevention of Postpartum Depression: A Multicentre Randomised Clinical Trial. Nutrients. 2024; 16(2):227. https://doi.org/10.3390/nu16020227
Chicago/Turabian StyleRodríguez-Gallego, Isabel, Rafael Vila-Candel, Isabel Corrales-Gutierrez, Diego Gomez-Baya, and Fatima Leon-Larios. 2024. "Evaluation of the Impact of a Midwife-Led Breastfeeding Group Intervention on Prevention of Postpartum Depression: A Multicentre Randomised Clinical Trial" Nutrients 16, no. 2: 227. https://doi.org/10.3390/nu16020227
APA StyleRodríguez-Gallego, I., Vila-Candel, R., Corrales-Gutierrez, I., Gomez-Baya, D., & Leon-Larios, F. (2024). Evaluation of the Impact of a Midwife-Led Breastfeeding Group Intervention on Prevention of Postpartum Depression: A Multicentre Randomised Clinical Trial. Nutrients, 16(2), 227. https://doi.org/10.3390/nu16020227









