Energy Costs of 37 Physical Activities in Chinese Children and Adolescents Aged 9–17 Years with Obesity
Abstract
1. Introduction
2. Methods
2.1. Participants
2.2. Anthropometric Indicator Measurements
2.3. Bioelectrical Impedance Analysis
2.4. Indirect Calorimetry
2.5. Heart Rate and Motion Monitoring
2.6. Physical Activity Tests
2.6.1. Resting Energy Expenditure (REE)
2.6.2. Exercise Tests: Continuous PAs
Field and Treadmill Walking and Running
Elliptical Trainer
2.6.3. Conditioning PAs
2.6.4. Individual, Sport, and Fitness PAs
2.6.5. Sitting Sedentary Behaviors
2.6.6. Standing Sedentary Behavior and PAs
2.7. Data Processing and Statistical Analysis
2.7.1. Data Processing
- (1)
- TEE or REE (kcal/min) = 3.9 × VO2 (L/min) + 1.1 × VCO2 (L/min);
- (2)
- PAEE (kcal/kg/min) = TEE (kcal/kg/min) − REE (kcal/kg/min);
- (3)
- Estimated HRmax = 220 − age (year);
- (4)
- % estimated HRmax = HRPA/estimated HRmax × 100%;
- (5)
- METs = Exercise VO2 (mL/min)/resting VO2 (mL/min) [36].
2.7.2. Statistical Analysis
3. Results
3.1. Basic Characteristics of the Participants
3.2. Energy Expenditure and Oxygen Uptake Characteristics of the Resting State
3.3. Energy Expenditure Characteristics of PAs
3.3.1. Energy Expenditure Characteristics of Continuous PAs
3.3.2. Energy Expenditure Characteristics of Conditioning PAs
3.4. Energy Expenditure Characteristics of Sitting Sedentary Behaviors
3.5. Energy Expenditure Characteristics of Standing Sedentary Behavior and PAs
3.6. Energy Expenditure Characteristics of Individual, Sport, and Fitness PAs
3.7. Factors Affecting the Energy Expenditure of PAs
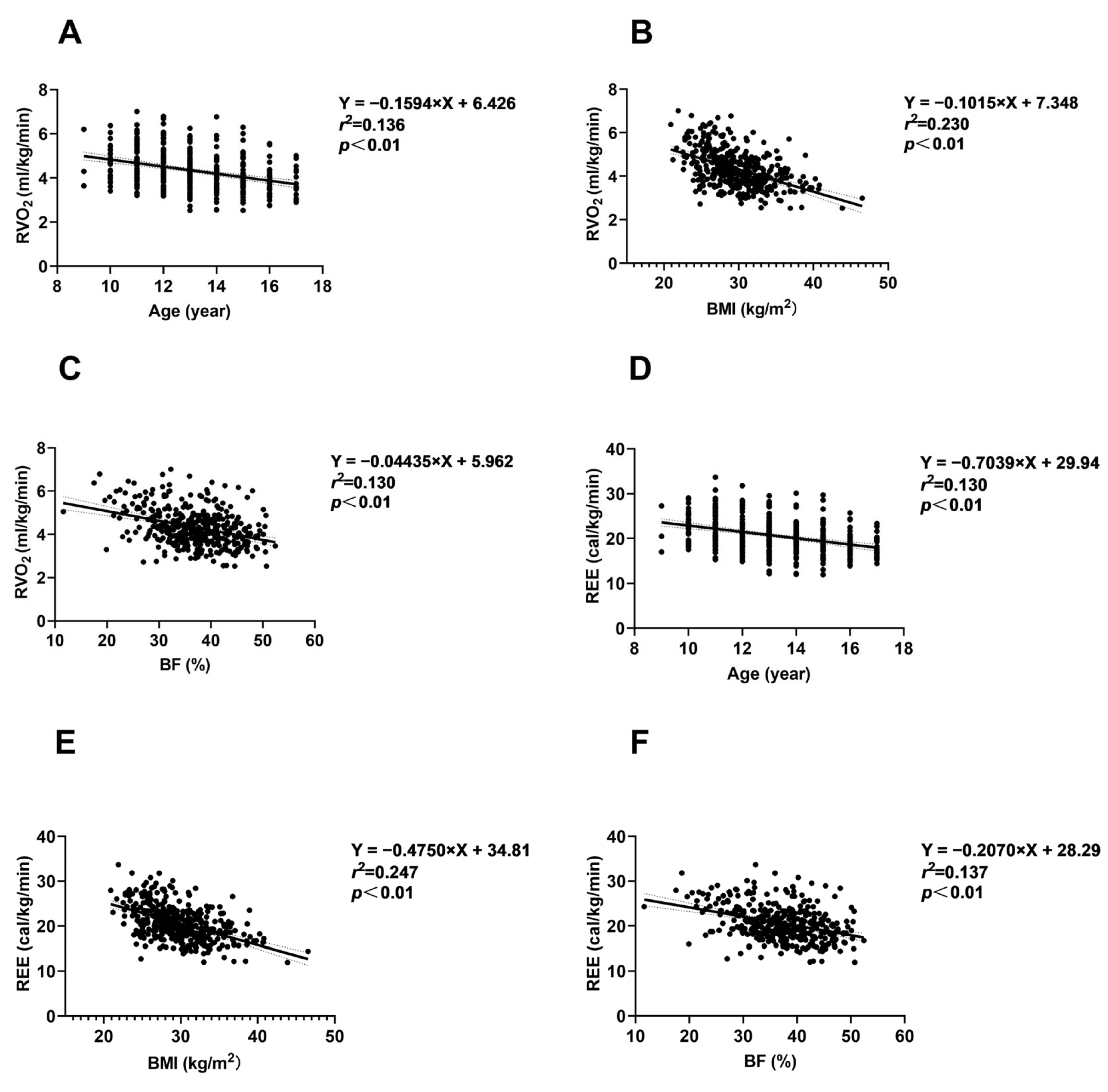
3.7.1. Relationships Between Age, Obesity Degree, and REE
3.7.2. Relationships Between Age, Obesity Degree, and Energy Expenditure for PAs
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight#:~:text=In%202022%2C%2043%25%20of%20adults,who%20were%20living%20with%20obesity (accessed on 1 March 2024).
- Wang, Y.; Sun, M.; Yang, Y. Blue Paper on Obesity Prevention and Control in China; Peking University Medical Press: Beijing, China, 2019. [Google Scholar]
- Balasundaram, P.; Krishna, S. Obesity Effects on Child Health. Available online: https://www.ncbi.nlm.nih.gov/books/NBK570613/ (accessed on 10 April 2023).
- Simmonds, M.; Llewellyn, A.; Owen, C.G.; Woolacott, N. Predicting adult obesity from childhood obesity: A systematic review and meta-analysis. Obes. Rev. 2016, 17, 95–107. [Google Scholar] [CrossRef] [PubMed]
- Patton, G.C.; Coffey, C.; Carlin, J.B.; Sawyer, S.M.; Williams, J.; Olsson, C.A.; Wake, M. Overweight and obesity between adolescence and young adulthood: A 10-year prospective cohort study. J. Adolesc. Health 2011, 48, 275–280. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Kelly, A.S. Review of Childhood Obesity: From Epidemiology, Etiology, and Comorbidities to Clinical Assessment and Treatment. Mayo Clin. Proc. 2017, 92, 251–265. [Google Scholar] [CrossRef]
- Bull, F.C. Physical Activity Guidelines in the UK: Review and Recommendations; Loughborough University: Loughborough, UK, 2010. [Google Scholar]
- Kelley, G.A.; Kelley, K.S.; Pate, R.R. Exercise and BMI in Overweight and Obese Children and Adolescents: A Systematic Review and Trial Sequential Meta-Analysis. Biomed. Res. Int. 2015, 2015, 704539. [Google Scholar] [CrossRef]
- Chang, Y.H.; Yang, H.Y.; Shun, S.C. Effect of exercise intervention dosage on reducing visceral adipose tissue: A systematic review and network meta-analysis of randomized controlled trials. Int. J. Obes. 2021, 45, 982–997. [Google Scholar] [CrossRef]
- Chen, L.; Liu, Q.; Xu, F.; Wang, F.; Luo, S.; An, X.; Chen, J.; Tang, N.; Jiang, X.; Liang, X. Effect of physical activity on anxiety, depression and obesity index in children and adolescents with obesity: A meta-analysis. J. Affect. Disord. 2024, 354, 275–285. [Google Scholar] [CrossRef]
- Husøy, A.; Kolle, E.; Steene-Johannessen, J.; Andersen, L.B.; Anderssen, S.A.; Ekelund, U. Prospective associations of physical activity and sedentary time in adolescence with cardiometabolic risk in young adulthood. Med. Sci. Sports Exerc. 2024. [Google Scholar] [CrossRef]
- Sriram, K.; Mulder, H.S.; Frank, H.R.; Santanam, T.S.; Skinner, A.C.; Perrin, E.M.; Armstrong, S.C.; Peterson, E.D.; Pencina, M.J.; Wong, C.A. The Dose-Response Relationship Between Physical Activity and Cardiometabolic Health in Adolescents. Am. J. Prev. Med. 2021, 60, 95–103. [Google Scholar] [CrossRef]
- Chen, Z.; Zhu, L. Dose-response relationship between physical activity and cardiometabolic risk in obese children and adolescents: A pre-post quasi-experimental study. Front. Physiol. 2023, 14, 1070653. [Google Scholar] [CrossRef]
- Eskandari, M.; Hooshmand Moghadam, B.; Bagheri, R.; Ashtary-Larky, D.; Eskandari, E.; Nordvall, M.; Dutheil, F.; Wong, A. Effects of Interval Jump Rope Exercise Combined with Dark Chocolate Supplementation on Inflammatory Adipokine, Cytokine Concentrations, and Body Composition in Obese Adolescent Boys. Nutrients 2020, 12, 3011. [Google Scholar] [CrossRef]
- Gil-Cosano, J.J.; Plaza-Florido, A.; Gracia-Marco, L.; Migueles, J.H.; Cadenas-Sanchez, C.; Olvera-Rojas, M.; Ubago-Guisado, E.; Labayen, I.; Lucia, A.; Ortega, F.B. Effects of combined aerobic and resistance training on the inflammatory profile of children with overweight/obesity: A randomized clinical trial. Pediatr. Obes. 2024, 19, e13152. [Google Scholar] [CrossRef] [PubMed]
- Seo, Y.G.; Lim, H.; Kim, Y.; Ju, Y.S.; Lee, H.J.; Jang, H.B.; Park, S.I.; Park, K.H. The Effect of a Multidisciplinary Lifestyle Intervention on Obesity Status, Body Composition, Physical Fitness, and Cardiometabolic Risk Markers in Children and Adolescents with Obesity. Nutrients 2019, 11, 137. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Ma, H.; Zhang, W.; Zhang, Y.; Youssef, L.; Carneiro, M.A.S.; Chen, C.; Wang, D.; Wang, D. Effects of Functional Strength Training Combined with Aerobic Training on Body Composition, Physical Fitness, and Movement Quality in Obese Adolescents. Nutrients 2024, 16, 1434. [Google Scholar] [CrossRef] [PubMed]
- Composing Editorial Board of Physical Activity Guidelines for Chinese. Physical Activity Guidelines for Chinese (2021). Biomed. Environ. Sci. 2022, 35, 1–3. [Google Scholar] [CrossRef]
- Zhu, Z.; Tang, Y.; Zhuang, J.; Liu, Y.; Wu, X.; Cai, Y.; Wang, L.; Cao, Z.B.; Chen, P. Physical activity, screen viewing time, and overweight/obesity among Chinese children and adolescents: An update from the 2017 physical activity and fitness in China-the youth study. BMC Public Health 2019, 19, 197. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Butte, N.F.; Watson, K.B.; Ridley, K.; Zakeri, I.F.; McMurray, R.G.; Pfeiffer, K.A.; Crouter, S.E.; Herrmann, S.D.; Bassett, D.R.; Long, A.; et al. A Youth Compendium of Physical Activities: Activity Codes and Metabolic Intensities. Med. Sci. Sports Exerc. 2018, 50, 246–256. [Google Scholar] [CrossRef]
- Herrmann, S.D.; Willis, E.A.; Ainsworth, B.E.; Barreira, T.V.; Hastert, M.; Kracht, C.L.; Schuna, J.M., Jr.; Cai, Z.; Quan, M.; Tudor-Locke, C.; et al. 2024 Adult Compendium of Physical Activities: A third update of the energy costs of human activities. J. Sport Health Sci. 2024, 13, 6–12. [Google Scholar] [CrossRef]
- Willis, E.A.; Herrmann, S.D.; Hastert, M.; Kracht, C.L.; Barreira, T.V.; Schuna, J.M., Jr.; Cai, Z.; Quan, M.; Conger, S.A.; Brown, W.J.; et al. Older Adult Compendium of Physical Activities: Energy costs of human activities in adults aged 60 and older. J. Sport. Health Sci. 2024, 13, 13–17. [Google Scholar] [CrossRef]
- Peyrot, N.; Thivel, D.; Isacco, L.; Morin, J.B.; Duche, P.; Belli, A. Do mechanical gait parameters explain the higher metabolic cost of walking in obese adolescents? J. Appl. Physiol. (1985) 2009, 106, 1763–1770. [Google Scholar] [CrossRef]
- Lazzer, S.; O’Malley, G.; Vermorel, M. Metabolic and Mechanical Cost of Sedentary and Physical Activities in Obese Children and Adolescents. Available online: https://ecogobesity.wpenginepowered.com/wp-content/uploads/2015/02/ECOG-Obesity-eBook-Metabolic-And-Mechanical-Cost-Of-Sedentary-And-Physical-Activities-In-Obese-Children-And-Adolescents.pdf (accessed on 1 February 2015).
- Lazzer, S.; Boirie, Y.; Bitar, A.; Montaurier, C.; Vernet, J.; Meyer, M.; Vermorel, M. Assessment of energy expenditure associated with physical activities in free-living obese and nonobese adolescents. Am. J. Clin. Nutr. 2003, 78, 471–479. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Chen, P.; Zhuang, J.; Walt, S. Metabolic cost, mechanical work, and efficiency during normal walking in obese and normal-weight children. Res. Q. Exerc. Sport. 2013, 84 (Suppl. S2), S72–S79. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Zong, X.N.; Ji, C.Y.; Mi, J. Body mass index cut-offs for overweight and obesity in Chinese children and adolescents aged 2–18 years. Zhonghua Liu Xing Bing. Xue Za Zhi 2010, 31, 616–620. [Google Scholar] [PubMed]
- Oshima, T.; Graf, S.; Heidegger, C.P.; Genton, L.; Pugin, J.; Pichard, C. Can calculation of energy expenditure based on CO(2) measurements replace indirect calorimetry? Crit. Care 2017, 21, 13. [Google Scholar] [CrossRef] [PubMed]
- Shaw, P.A.; McMurray, R.; Butte, N.; Sotres-Alvarez, D.; Sun, H.; Stoutenberg, M.; Evenson, K.R.; Wong, W.W.; Moncrieft, A.E.; Sanchez-Johnsen, L.A.P.; et al. Calibration of activity-related energy expenditure in the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). J. Sci. Med. Sport. 2019, 22, 300–306. [Google Scholar] [CrossRef]
- Trost, S.G.; Way, R.; Okely, A.D. Predictive validity of three ActiGraph energy expenditure equations for children. Med. Sci. Sports Exerc. 2006, 38, 380–387. [Google Scholar] [CrossRef]
- Freedson, P.; Pober, D.; Janz, K.F. Calibration of accelerometer output for children. Med. Sci. Sports Exerc. 2005, 37, S523–S530. [Google Scholar] [CrossRef]
- Tamini, S.; Caroli, D.; Bondesan, A.; Abbruzzese, L.; Sartorio, A. Measured vs estimated resting energy expenditure in children and adolescents with obesity. Sci. Rep. 2023, 13, 13178. [Google Scholar] [CrossRef]
- Reis, V.M.; Vianna, J.M.; Barbosa, T.M.; Garrido, N.; Vilaça Alves, J.; Carneiro, A.L.; Aidar, F.J.; Novaes, J. Are wearable heart rate measurements accurate to estimate aerobic energy cost during low-intensity resistance exercise? PLoS ONE 2019, 14, e0221284. [Google Scholar] [CrossRef]
- Weir, J.B. New methods for calculating metabolic rate with special reference to protein metabolism. J. Physiol. 1949, 109, 1–9. [Google Scholar] [CrossRef]
- Jetté, M.; Sidney, K.; Blümchen, G. Metabolic equivalents (METS) in exercise testing, exercise prescription, and evaluation of functional capacity. Clin. Cardiol. 1990, 13, 555–565. [Google Scholar] [CrossRef] [PubMed]
- Hibbing, P.R.; Bassett, D.R.; Coe, D.P.; Lamunion, S.R.; Crouter, S.E. Youth Metabolic Equivalents Differ Depending on Operational Definitions. Med. Sci. Sports Exerc. 2020, 52, 1846–1853. [Google Scholar] [CrossRef] [PubMed]
- Roemmich, J.N.; Clark, P.A.; Walter, K.; Patrie, J.; Weltman, A.; Rogol, A.D. Pubertal alterations in growth and body composition. V. Energy expenditure, adiposity, and fat distribution. Am. J. Physiol. Endocrinol. Metab. 2000, 279, E1426–E1436. [Google Scholar] [CrossRef] [PubMed]
- Byrne, N.M.; Hills, A.P.; Hunter, G.R.; Weinsier, R.L.; Schutz, Y. Metabolic equivalent: One size does not fit all. J. Appl. Physiol. (1985) 2005, 99, 1112–1119. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L. A Methodological Study on the Measurement of Energy Expenditure for Common Physical Activities in Adolescents aged 11–14 Years. Ph.D. Thesis, Shanghai University of Sport, Shanghai, China, 2012. [Google Scholar]
- Sasaki, J.E.; Howe, C.; John, D.; Hickey, A.; Steeves, J.; Conger, S.; Lyden, K.; Kozey-Keadle, S.; Burkart, S.; Alhassan, S.; et al. Energy Expenditure for 70 Activities in Children and Adolescents. J. Phys. Act. Health 2016, 13, S24–S28. [Google Scholar] [CrossRef][Green Version]
- Ekelund, U.; Sanchez-Lastra, M.A.; Dalene, K.E.; Tarp, J. Dose-response associations, physical activity intensity and mortality risk: A narrative review. J. Sport. Health Sci. 2024, 13, 24–29. [Google Scholar] [CrossRef]
- Dempsey, P.C.; Rowlands, A.V.; Strain, T.; Zaccardi, F.; Dawkins, N.; Razieh, C.; Davies, M.J.; Khunti, K.K.; Edwardson, C.L.; Wijndaele, K.; et al. Physical activity volume, intensity, and incident cardiovascular disease. Eur. Heart J. 2022, 43, 4789–4800. [Google Scholar] [CrossRef]
- Piercy, K.L.; Troiano, R.P.; Ballard, R.M.; Carlson, S.A.; Fulton, J.E.; Galuska, D.A.; George, S.M.; Olson, R.D. The Physical Activity Guidelines for Americans. JAMA 2018, 320, 2020–2028. [Google Scholar] [CrossRef]
- Chen, P.; Wang, D.; Shen, H.; Yu, L.; Gao, Q.; Mao, L.; Jiang, F.; Luo, Y.; Xie, M.; Zhang, Y.; et al. Physical activity and health in Chinese children and adolescents: Expert consensus statement (2020). Br. J. Sports Med. 2020, 54, 1321–1331. [Google Scholar] [CrossRef]
- Pfeiffer, K.A.; Watson, K.B.; McMurray, R.G.; Bassett, D.R.; Butte, N.F.; Crouter, S.E.; Herrmann, S.D.; Trost, S.G.; Ainsworth, B.E.; Fulton, J.E.; et al. Energy Cost Expression for a Youth Compendium of Physical Activities: Rationale for Using Age Groups. Pediatr. Exerc. Sci. 2018, 30, 142–149. [Google Scholar] [CrossRef]
- Harrell, J.S.; McMurray, R.G.; Baggett, C.D.; Pennell, M.L.; Pearce, P.F.; Bangdiwala, S.I. Energy costs of physical activities in children and adolescents. Med. Sci. Sports Exerc. 2005, 37, 329–336. [Google Scholar] [CrossRef] [PubMed]
- Soares, M.J.; Müller, M.J. Resting energy expenditure and body composition: Critical aspects for clinical nutrition. Eur. J. Clin. Nutr. 2018, 72, 1208–1214. [Google Scholar] [CrossRef] [PubMed]
- Leibel, R.L.; Rosenbaum, M.; Hirsch, J. Changes in energy expenditure resulting from altered body weight. N. Engl. J. Med. 1995, 332, 621–628. [Google Scholar] [CrossRef]
- Maffeis, C.; Schutz, Y.; Schena, F.; Zaffanello, M.; Pinelli, L. Energy expenditure during walking and running in obese and nonobese prepubertal children. J. Pediatr. 1993, 123, 193–199. [Google Scholar] [CrossRef]
- Balcı, S.S. Comparison of substrate oxidation during walking and running in normal-weight and overweight/obese men. Obes. Facts 2012, 5, 327–338. [Google Scholar] [CrossRef]
- Heymsfield, S.B.; Thomas, D.M.; Bosy-Westphal, A.; Müller, M.J. The anatomy of resting energy expenditure: Body composition mechanisms. Eur. J. Clin. Nutr. 2019, 73, 166–171. [Google Scholar] [CrossRef]
- Heymsfield, S.B.; Peterson, C.M.; Bourgeois, B.; Thomas, D.M.; Gallagher, D.; Strauss, B.; Müller, M.J.; Bosy-Westphal, A. Human energy expenditure: Advances in organ-tissue prediction models. Obes. Rev. 2018, 19, 1177–1188. [Google Scholar] [CrossRef]
- Thivel, D.; Ennequin, G.; Lambert, C.; Siroux, J.; Ratel, S.; Boscaro, A.; Pelissier, L.; Julian, V.; Cardenoux, C.; Duclos, M.; et al. Improved walking energy efficiency might persist in presence of simulated full weight regain after multidisciplinary weight loss in adolescents with obesity: The POWELL study. Int. J. Obes. 2024, 48, 384–393. [Google Scholar] [CrossRef]
- Gould, L.M.; Hirsch, K.R.; Blue, M.N.M.; Cabre, H.E.; Brewer, G.J.; Smith-Ryan, A.E. Effects of adiposity and body composition on adjusted resting energy expenditure in women. Am. J. Hum. Biol. 2022, 34, e23610. [Google Scholar] [CrossRef]
- Elbelt, U.; Schuetz, T.; Hoffmann, I.; Pirlich, M.; Strasburger, C.J.; Lochs, H. Differences of energy expenditure and physical activity patterns in subjects with various degrees of obesity. Clin. Nutr. 2010, 29, 766–772. [Google Scholar] [CrossRef]
- Group of China Obesity Task Force. Body mass index reference norm for screening overweight and obesity in Chinese children and adolescents. Chin. J. Epidemiol. 2004, 25, 97–102. [Google Scholar]
- Ebbeling, C.B.; Pawlak, D.B.; Ludwig, D.S. Childhood obesity: Public-health crisis, common sense cure. Lancet 2002, 360, 473–482. [Google Scholar] [CrossRef] [PubMed]
- Hermand, E.; Cassirame, J.; Ennequin, G.; Hue, O. Validation of a Photoplethysmographic Heart Rate Monitor: Polar OH1. Int. J. Sports Med. 2019, 40, 462–467. [Google Scholar] [CrossRef] [PubMed]
- Borg, G.A. Psychophysical bases of perceived exertion. Med. Sci. Sports Exerc. 1982, 14, 377–381. [Google Scholar] [CrossRef]
- Eston, R.G.; Williams, J.G. Reliability of ratings of perceived effort regulation of exercise intensity. Br. J. Sports Med. 1988, 22, 153–155. [Google Scholar] [CrossRef]


| Continuous PAs (n = 15) | Conditioning PAs (n = 8) | Individual, Sport, and Fitness PAs (n = 7) |
|---|---|---|
| Field walking | Self-weighted | Rhythmic gymnastics |
| 3.0 km/h | Squat | Stretching |
| 4.0 km/h | Jumping jacks | Basketball |
| 5.0 km/h | Walking lunge | Circuit training |
| Field running | Kneeling push-ups | Flag football |
| 6.0 km/h | Quantitively loaded | Badminton |
| 7.0 km/h | Dumbbell squat (5 kg) | Elliptical trainer (self-selected pace and load) |
| Treadmill walking | Dumbbell rowing (5 kg) | |
| 3.0 km/h | Dumbbell press (2.5 kg) | |
| 4.0 km/h | Bicep curls (2.5 kg) | |
| 5.0 km/h | ||
| Treadmill running | ||
| 6.0 km/h | ||
| 7.0 km/h | ||
| Elliptical trainer | ||
| Level 1 | ||
| Level 2 | ||
| Level 3 | ||
| Level 4 | ||
| Level 5 | ||
| Sitting Sedentary Behaviors (n = 4) | Standing Sedentary Behavior and PAs(n = 3) | |
| Writing | Standing quietly | |
| Reading | Step up and down | |
| Listening to music | Horse Stance | |
| Playing video game |
| Indicators | Total (n = 397) | Boys (n = 231) | Girls (n = 166) |
|---|---|---|---|
| Age (year) | 13.00 (12.00–15.00) | 13.00 (12.00–14.00) | 13.00 (12.00–15.00) * |
| Height (cm) | 163.45 ± 9.28 | 165.06 ± 10.35 | 161.22 ± 6.97 ** |
| BM (kg) | 80.24 ± 16.21 | 82.65 ± 17.86 | 76.90 ± 12.90 ** |
| BMI (kg/m2) | 29.30 (26.85–32.37) | 29.70 (26.80–32.60) | 29.02 (27.08–31.91) |
| FM (kg) | 29.61 ± 9.00 | 29.07 ± 9.09 | 30.30 ± 8.87 |
| BF (%) | 36.86 ± 6.85 | 35.59 ± 6.98 | 38.68 ± 6.25 ** |
| Indicators | Total (n = 397) | Boys (n = 231) | Girls (n = 166) |
|---|---|---|---|
| VO2 (L/min) | 0.34 ± 0.07 | 0.36 ± 0.07 | 0.31 ± 0.05 ** |
| VO2 (mL/kg/min) | 4.23 (3.72–4.84) | 4.38 (3.82–5.01) | 4.05 (3.59–4.48) ** |
| REE (kcal/kg/min) | 0.020 (0.018–0.023) | 0.021 (0.018–0.024) | 0.019 (0.018–0.022) ** |
| HRrest (bpm) | 80 (72–87) | 79.00 (71.15–85.00) | 81 (73–89) * |
| % predicted HRmax | 38.53 (34.78–42.01) | 37.92 (34.46–41.06) | 39.46 (35.67–42.68) ** |
| Physical Activity | VO2 (L/min) | VO2 (mL/kg/min) | MET Values | TEE (kcal/kg/min) | PAEE (kcal/kg/min) | HRPA (bpm) | % Estimated HRmax |
|---|---|---|---|---|---|---|---|
| Continuous PAs | |||||||
| Field walking and running | |||||||
| 3 km/h (n = 244) | 0.94 ± 0.23 ## | 11.51 (10.23–12.68) # | 2.67 (2.35–2.98) | 0.055 (0.050–0.060) ## | 0.033 (0.029–0.038) | 118 ± 14 ## | 57.25 ± 6.76 ## |
| 4 km/h (n = 244) | 1.09 ± 0.24 # | 13.64 ± 2.06 | 3.09 (2.74–3.52) | 0.065 ± 0.009 | 0.044 ± 0.008 | 126 ± 14 | 60.97 ± 6.60 # |
| 5 km/h (n = 244) | 1.39 ± 0.31 | 17.26 ± 2.64 | 3.90 (3.47–4.40) | 0.082 ± 0.012 | 0.061 ± 0.011 # | 139 ± 15 | 67.30 ± 7.03 |
| 6 km/h (n = 232) | 2.07 ± 0.52 ## | 25.65 ± 4.97 ## | 6.00 ± 1.44 | 0.127 ± 0.024 ## | 0.106 ± 0.023 ## | 168 ± 17 | 84.09 ± 11.41 ## |
| 7 km/h (n = 212) | 2.37 ± 0.52 # | 29.98 ± 5.07 | 6.70 (5.92–7.70) | 0.147 ± 0.025 # | 0.126 ± 0.023 | 180 ± 15 | 87.20 ± 6.91 |
| Treadmill walking and running | |||||||
| 3 km/h (n = 74) | 0.86 ± 0.17 | 11.15 ± 1.56 | 2.71 ± 0.49 | 0.053 ± 0.007 | 0.033 ± 0.006 | 112 ± 13 | 54.16 ± 6.18 |
| 4 km/h (n = 74) | 1.04 ± 0.19 | 13.39 ± 1.76 | 3.26 ± 0.57 | 0.064 ± 0.009 | 0.043 ± 0.007 | 122 ± 14 | 59.15 ± 6.84 |
| 5 km/h (n = 74) | 1.36 ± 0.24 | 17.67 ± 2.26 | 4.30 ± 0.76 | 0.084 ± 0.011 | 0.065 ± 0.010 | 139 (131–148) | 67.23 (63.50–72.01) |
| 6 km/h (n = 68) | 1.86 ± 0.29 | 24.25 ± 2.40 | 5.85 ± 0.92 | 0.118 ± 0.012 | 0.098 ± 0.011 | 165 ± 14 | 79.47 ± 6.68 |
| 7 km/h (n = 61) | 2.24 ± 0.39 | 29.13 ± 2.42 | 7.03 ± 1.05 | 0.143 ± 0.012 | 0.123 ± 0.011 | 181 (171–188) | 87.39 (82.73–91.15) |
| Elliptical Trainer | |||||||
| Level 1 (n = 50) | 1.09 ± 0.21 | 13.25 ± 1.93 | 3.22 ± 0.55 | 0.063 ± 0.009 | 0.043 ± 0.009 | 128 ± 15 | 62.04 ± 7.40 |
| Level 2 (n = 50) | 1.13 ± 0.20 | 13.79 ± 1.92 | 3.35 ± 0.54 | 0.066 ± 0.009 | 0.046 ± 0.009 | 132 ± 16 | 63.83 ± 7.66 |
| Level 3 (n = 50) | 1.19 ± 0.21 | 14.60 ± 2.16 | 3.54 ± 0.58 | 0.070 ± 0.011 | 0.050 ± 0.009 | 135 ± 16 | 65.33 ± 7.77 |
| Level 4 (n = 50) | 1.26 ± 0.20 | 15.40 ± 2.22 | 3.74 ± 0.61 | 0.073 ± 0.011 | 0.054 ± 0.010 | 139 ± 17 | 67.10 ± 8.05 |
| Level 5 (n = 50) | 1.34 ± 0.20 | 16.47 ± 2.41 | 4.00 ± 0.70 | 0.079 ± 0.012 | 0.059 ± 0.011 | 144 ± 17 | 69.50 ± 8.24 |
| Conditioning PAs | |||||||
| 1 min squat (n = 126) | 2.51 (2.00–3.26) | 33.68 ± 8.69 | 8.00 ± 2.37 | 0.166 (0.137–0.195) | 0.146 (0.116–0.174) | 151 ± 18 | 72.87 ± 8.71 |
| 1 min jumping jacks (n = 131) | 2.56 (2.19–3.23) | 34.89 ± 8.57 | 8.14 ± 2.15 | 0.172 ± 0.043 | 0.151 ± 0.042 | 151 (140–161) | 73.03 ± 8.45 |
| 1 min dumbbell squat (n = 32) | 0.85 ± 0.17 | 12.97 ± 2.33 | 2.91 ± 0.51 | 0.056 ± 0.009 | 0.036 ± 0.009 | 116 ± 12 | 56.00 ± 5.61 |
| 1 min dumbbell press (n = 32) | 0.40 ± 0.08 | 6.16 ± 1.25 | 1.38 ± 0.27 | 0.027 ± 0.006 | 0.008 ± 0.005 | 101 ± 11 | 48.76 ± 5.45 |
| 1 min bicep curls (n = 32) | 0.41 ± 0.08 | 6.19 ± 1.07 | 1.43 ± 0.28 | 0.027 ± 0.005 | 0.008 ± 0.005 | 97 ± 11 | 46.75 ± 5.47 |
| 1 min kneeling push-ups (n = 50) | 0.70 ± 0.15 | 8.51 ± 1.35 | 2.07 ± 0.64 | 0.041 ± 0.006 | 0.021 ± 0.006 | 110 ± 11 | 53.22 ± 5.67 |
| 1 min dumbbell rowing (n = 50) | 0.60 ± 0.14 | 7.36 ± 1.39 | 1.78 ± 0.34 | 0.035 ± 0.006 | 0.015 ± 0.006 | 112 ± 11 | 53.89 ± 5.38 |
| 1 min walking lunge (n = 50) | 0.90 ± 0.23 | 10.88 ± 2.08 | 2.66 ± 0.68 | 0.052 ± 0.010 | 0.032 ± 0.010 | 119 ± 12 | 57.68 ± 5.76 |
| Individual, Sport, and Fitness PAs *** | |||||||
| Rhythmic gymnastics (n = 25) | 3.62 ± 0.96 | 0.065 ± 0.021 | 127 ± 15 | 61.73 ± 7.47 | |||
| Stretching (n = 17) | 2.98 ± 0.92 | 0.037 ± 0.019 | 116 ± 16 | 55.97 ± 7.72 | |||
| Basketball (n = 7) | 3.28 ± 0.46 | 0.043 ± 0.008 | 140 ± 9 | 67.44 ± 4.48 | |||
| Circuit training (n = 22) | 3.52 ± 0.54 | 0.056 ± 0.012 | 134 ± 9 | 64.99 ± 4.53 | |||
| Flag football (n = 16) | 4.86 ± 1.01 | 0.073 ± 0.018 | 125 ± 15 | 60.04 ± 7.51 | |||
| Badminton (n = 17) | 3.63 ± 0.83 | 0.059 ± 0.016 | 134 ± 15 | 64.95 ± 7.24 | |||
| Elliptical trainer (self-selected pace, load) (n = 16) | 3.13 ± 0.55 | 0.057 ± 0.015 | 127 ± 7 | 61.54 ± 3.29 | |||
| Sitting sedentary behaviors | |||||||
| Writing (n = 25) | 0.33 ± 0.06 | 4.57 ± 0.90 | 1.17 ± 0.15 | 0.022 ± 0.003 | 0.003 ± 0.002 | 84 ± 9 | 40.71 ± 4.38 |
| Reading (n = 16) | 0.31 ± 0.04 | 4.27 ± 0.55 | 1.15 ± 0.11 | 0.022 ± 0.003 | 0.003 ± 0.002 | 83 ± 9 | 40.20 ± 4.15 |
| Listening to music (n = 13) | 0.31 ± 0.06 | 4.36 ± 0.49 | 1.12 ± 0.09 | 0.021 ± 0.002 | 0.002 (0.001–0.003) | 86 ± 6 | 41.26 ± 2.94 |
| Playing video game (n = 46) | 0.45 ± 0.10 | 5.29 ± 0.87 | 1.25 (1.16–1.49) | 0.026 ± 0.004 | 0.005 (0.004–0.009) | 95 ± 11 | 45.57 ± 5.27 |
| Standing sedentary behavior and PAs | |||||||
| Standing quietly (n = 19) | 0.35 ± 0.04 | 4.78 ± 0.70 | 1.22 ± 0.12 | 0.020 ± 0.004 | 0.001 ± 0.002 | 97 ± 11 | 46.95 ± 5.13 |
| Step up and down (n = 32) | 0.92 ± 0.19 | 12.97 ± 1.56 | 3.18 ± 0.59 | 0.060 ± 0.007 | 0.041 ± 0.008 | 117 ± 13 | 56.60 ± 6.11 |
| 1 min horse stance (n = 47) | 0.63 ± 0.15 | 7.59 ± 1.30 | 1.85 ± 0.34 | 0.040 ± 0.006 | 0.020 ± 0.006 | 111 ± 11 | 53.84 ± 5.30 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhu, L.; Chen, Z.; Liu, J.; Cao, Y.; Liao, J.; Xie, W. Energy Costs of 37 Physical Activities in Chinese Children and Adolescents Aged 9–17 Years with Obesity. Nutrients 2024, 16, 3966. https://doi.org/10.3390/nu16223966
Zhu L, Chen Z, Liu J, Cao Y, Liao J, Xie W. Energy Costs of 37 Physical Activities in Chinese Children and Adolescents Aged 9–17 Years with Obesity. Nutrients. 2024; 16(22):3966. https://doi.org/10.3390/nu16223966
Chicago/Turabian StyleZhu, Lin, Zekai Chen, Jingxin Liu, Youxiang Cao, Jing Liao, and Weijun Xie. 2024. "Energy Costs of 37 Physical Activities in Chinese Children and Adolescents Aged 9–17 Years with Obesity" Nutrients 16, no. 22: 3966. https://doi.org/10.3390/nu16223966
APA StyleZhu, L., Chen, Z., Liu, J., Cao, Y., Liao, J., & Xie, W. (2024). Energy Costs of 37 Physical Activities in Chinese Children and Adolescents Aged 9–17 Years with Obesity. Nutrients, 16(22), 3966. https://doi.org/10.3390/nu16223966







