Stunting and Underweight among Adolescent Girls of Indigenous Communities in Telangana, India: A Cross-Sectional Study
Abstract
:1. Introduction
2. Methodology
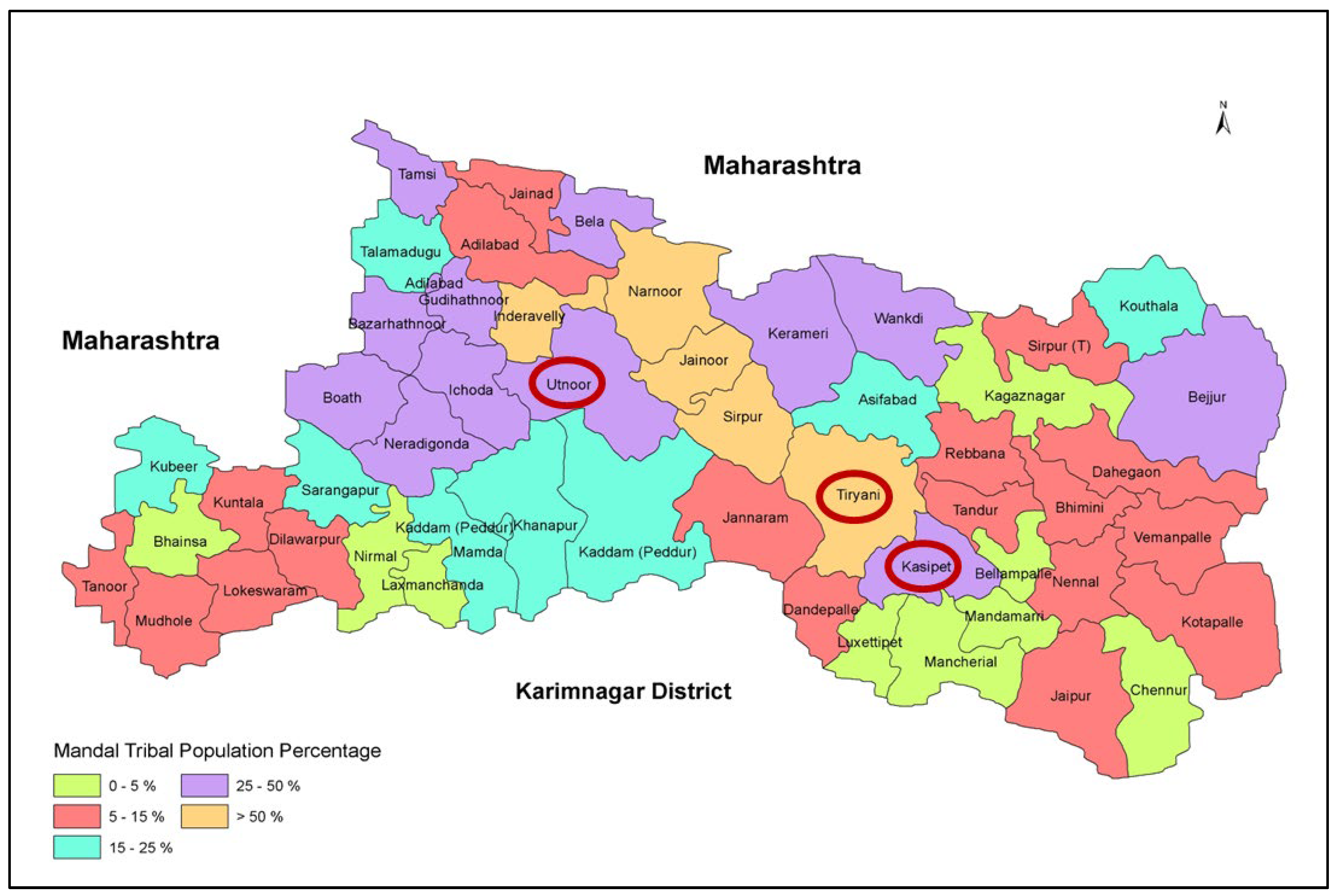
2.1. Study Sites and Participants
2.2. Data and Methods
3. Results
3.1. Socio-Demographic Characteristics
3.2. Nutritional Status
3.3. Determinants of Malnutrition—A Statistical Analysis
3.4. Qualitative Insights
3.5. Socio-Cultural Norms around Dietary Decisions and Behaviours
3.6. Government Programs for Adolescent Girls
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Adolescent Nutrition: A Review of the Situation in Selected South-East Asian Countries; WHO: Geneva, Switzerland, 2006. [Google Scholar]
- UNICEF. Adolescence: A Time That Matters; UNICEF: New York, NY, USA, 2002. [Google Scholar]
- Cordeiro, L.; Lamstein, S.; Mahmud, Z.; Levinson, F.J. Adolescent malnutrition in developing countries: A close look at the problem and at two national experiences. SCN News 2006, 31, 6–13. [Google Scholar]
- Pal, A.; Pari, A.K.; Sinha, A.; Dhara, P.C. Prevalence of undernutrition and associated factors: A cross-sectional study among rural adolescents in West Bengal, India. Int. J. Pediatr. Adolesc. Med. 2017, 4, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Bej, P. Adolescent health problems in India: A review from 2001 to 2015. Indian J. Community Health 2015, 27, 418–428. [Google Scholar]
- Caleyachetty, R.; Thomas, G.N.; Kengne, A.P.; Echouffo-Tcheugui, J.B.; Schilsky, S.; Khodabocus, J.; Uauy, R. The double burden of malnutrition among adolescents: Analysis of data from the Global School-Based Student Health and Health Behavior in School-Aged Children surveys in 57 low- and middle-income countries. Am. J. Clin. Nutr. 2018, 108, 414–424. [Google Scholar] [CrossRef]
- United Nations Children’s Fund. Improving Child Nutrition: The Achievable Imperative for Global Progress; United Nations Children’s Fund: New York, NY, USA, 2013. [Google Scholar]
- NCD Risk Factor Collaboration. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef] [PubMed]
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, Z.A.; Christian, P.; de Onis, M.; Ezzati, M.; Grantham-McGregor, S.; Katz, J.; Martorell, R.; et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef]
- Darling, A.M.; Fawzi, W.W.; Barik, A.; Chowdhury, A.; Rai, R.K. Double burden of malnutrition among adolescents in rural West Bengal, India. Nutrition 2020, 79, 110809. [Google Scholar] [CrossRef]
- Bhargava, M.; Bhargava, A.; Ghate, S.D.; Rao, R.S.P. Nutritional status of Indian adolescents (15–19 years) from National Family Health Surveys 3 and 4: Revised estimates using WHO 2007 Growth reference. PLoS ONE 2020, 15, e0234570. [Google Scholar]
- Schott, W.; Aurino, E.; Penny, M.E.; Behrman, J.R. The double burden of malnutrition among youth: Trajectories and inequalities in four emerging economies. Econ. Hum. Biol. 2019, 34, 80–91. [Google Scholar] [CrossRef]
- Faizi, N.; Khan, Z.; Khan, I.M.; Amir, A.; Azmi, S.A.; Khalique, N. A study on nutritional status of school-going adolescents in Aligarh, India. Trop. Dr. 2017, 47, 212–216. [Google Scholar] [CrossRef]
- MoHFW. Health and Family Welfare Statistics in India; Statistics Division, Ministry of Health: New Delhi, India, 2020. Available online: https://main.mohfw.gov.in/sites/default/files/rhs20-21_1.pdf (accessed on 11 December 2023).
- Santhya, K.; Acharya, R.; Pandey, N.; Singh, S.K.; Rampal, S.; Zavier, A.; Gupta, A.K. Executive Summary—Understanding the Lives of Adolescents and Young Adults (UDAYA) in Bihar, India; Population Council: New York, NY, USA, 2017. [Google Scholar]
- Santhya, K.; Acharya, R.; Pandey, N.; Gupta, A.K.; Rampal, S.; Singh, S.K.; Zavier, A. Understanding the Lives of Adolescents and Young adults (UDAYA) in Uttar Pradesh, India (2015–2016); Population Council: New York, NY, USA, 2017. [Google Scholar]
- Sethi, V.; Lahiri, A.; Bhanot, A.; Kumar, A.; Chopra, M.; Mishra, R. Adolescents, Diets and Nutrition: Growing Well in a Changing World; The Comprehensive National Nutrition Survey, Thematic Reports; 2019; pp. 1–4. Available online: https://www.unicef.org/india/media/2631/file/CNNS-Thematic-Report-Adolescents-Diets-and-Nutrition.pdf (accessed on 11 December 2023).
- Chandramouli, C.; General, R. Census of India 2011. In Provisional Population Totals; Government of India: New Delhi, India, 2011; pp. 409–413. [Google Scholar]
- Bhasin, M.; Jain, S. Biology of the Tribal Groups of Rajasthan, India: 3. Assessment of Nutritional Status Using Heights and Weights. Anthropologist 2007, 9, 189–197. [Google Scholar] [CrossRef]
- Rao, V.; Aggrawal, M.; Yadav, R.; Das, S.; Sahare, L.; Bondley, M.; Minocha, R. Intestinal parasitic infections, anaemia and undernutrition among tribal adolescents of Madhya Pradesh. Indian J. Community Med. 2003, 28, 26. [Google Scholar]
- Kulkarni, R.; Surve, S.; Patil, S.; Sankhe, L.; Gupta, P.; Toteja, G. Nutritional status of adolescent girls in tribal blocks of Maharashtra. Indian J. Community Med. Off. Publ. Indian Assoc. Prev. Soc. Med. 2019, 44, 281. [Google Scholar] [CrossRef]
- Rajaretnam, T.; Hallad, J.S. Nutritional status of adolescents in northern Karnataka, India. J. Fam. Welf. 2012, 58, 55–67. [Google Scholar]
- Jeyakumar, A.; Ghugre, P.; Gadhave, S. Mid-upper-arm circumference (MUAC) as a simple measure to assess the nutritional status of adolescent girls as compared with BMI. ICAN Infant Child Adolesc. Nutr. 2013, 5, 22–25. [Google Scholar] [CrossRef]
- Ghosh, S.; Varerkar, S.A. Undernutrition among tribal children in Palghar district, Maharashtra, India. PLoS ONE 2019, 14, e0212560. [Google Scholar] [CrossRef] [PubMed]
- Savanur, M.S.; Sathye, A.; Udawant, A.; Udipi, S.A.; Ghugre, P.; Haas, J.; Boy, E.; Bhatnagar, A. Nutritional status and physical fitness of tribal adolescents in ahmednagar district of Maharashtra. Ecol. Food Nutr. 2017, 56, 552–566. [Google Scholar] [CrossRef] [PubMed]
- Bharthi, K.; Ghritlahre, M.; Das, S.; Bose, K. Nutritional status among children and adolescents aged 6–18 years of Kolam tribe of Andhra Pradesh, India. AnthropologicAl Rev. 2017, 80, 153–163. [Google Scholar] [CrossRef]
- Dey, U.; Bisai, S. The prevalence of under-nutrition among the tribal children in India: A systematic review. Anthropol. Rev. 2019, 82, 203–217. [Google Scholar] [CrossRef]
- Ingole, A.B. Pragmatic Influence of Anthropometry and Dietary Position in Tribal Region: Critical Micro Analysys. IJRBAT 2017, V, 1105–1110. [Google Scholar]
- Rao, K.M.; Kumar, R.H.; Krishna, K.S.; Bhaskar, V.; Laxmaiah, A. Diet & nutrition profile of Chenchu population—A vulnerable tribe in Telangana & Andhra Pradesh, India. Indian J. Med. Res. 2015, 141, 688. [Google Scholar] [PubMed]
- Chakma, T.; Rao, P.V.; Meshram, P.; Singh, S. Health and nutrition profile of tribals of Madhya Pradesh and Chhattisgarh. In Proceedings of the National Symposium on Tribal Health, Jaipur, India, 19–20 October 2006; Available online: https://www.nirth.res.in/publications/nsth/26.T.Chakma.pdf (accessed on 10 December 2023).
- Mitra, A.; Rao, N. Gender Differences in Adolescent Nutrition: Evidence from Two Indian Districts; Institute of Development Studies: Falmer, UK, 2017; Available online: https://opendocs.ids.ac.uk/opendocs/handle/20.500.12413/13467 (accessed on 12 December 2023).
- Parimalavalli, R. A study of socio-economic and nutritional status of the tribal children. Stud. Tribes Tribals 2012, 10, 183–187. [Google Scholar] [CrossRef]
- Rao, B.D.; Busi, B. A study of physical growth and nutritional status among Jatapu tribal girls of Andhra Pradesh. J. Hum. Ecol. 1997, 8, 355–359. [Google Scholar] [CrossRef]
- Ahankari, A.; Hayter, M.; Whitfield, C.; Ali, P.; Giridhari, S.; Tambe, S.; Kabra, P.; Rayamane, K.; Ovseiko, P. aDolescents gEnder surVey, rEsponsible coupLes evaluatiOn, and capacity building Project in India (DEVELOP): A study protocol. F1000Research 2019, 8, 958. [Google Scholar] [CrossRef] [PubMed]
- Ahankari, A.S.; Tata, L.J.; Fogarty, A.W. Weight, height, and midupper arm circumference are associated with haemoglobin levels in adolescent girls living in rural India: A cross-sectional study. Matern. Child Nutr. 2020, 16, e12908. [Google Scholar] [CrossRef]
- Saha, S.; Pandya, A.; Kandre, Y.; Raval, D.; Saxena, D. Cross-Sectional Analysis of Nutritional Status, Knowledge and Uptake of Nutritional Services Among Adolescent Girls in Western India. Adolesc. Health Med. Ther. 2021, 12, 117–125. [Google Scholar] [CrossRef]
- Wells, J.C.; Sawaya, A.L.; Wibaek, R.; Mwangome, M.; Poullas, M.S.; Yajnik, C.S.; Demaio, A. The double burden of malnutrition: Aetiological pathways and consequences for health. Lancet 2020, 395, 75–88. [Google Scholar] [CrossRef]
- Rao, K.M.; Balakrishna, N.; Laxmaiah, A.; Venkaiah, K.; Brahmam, G. Diet and nutritional status of adolescent tribal population in nine states of India. Asia Pac. J. Clin. Nutr. 2006, 15, 64–71. [Google Scholar]
- Sridhar, D.; Gauthami, N. Menstrual health status and cultural practices of tribal adolescent girls. Int. J. Commun. Med. Public Health 2017, 4, 4120–4124. [Google Scholar]
- Müller, O.; Krawinkel, M. Malnutrition and health in developing countries. Cmaj 2005, 173, 279–286. [Google Scholar] [CrossRef]
- Kumar, P.; Srivastava, S.; Chauhan, S.; Patel, R.; Marbaniang, S.P.; Dhillon, P. Associated factors and socio-economic inequality in the prevalence of thinness and stunting among adolescent boys and girls in Uttar Pradesh and Bihar, India. PLoS ONE 2021, 16, e0247526. [Google Scholar] [CrossRef]
- Kahssay, M.; Mohamed, L.; Gebre, A. Nutritional status of school going adolescent girls in Awash Town, Afar Region, Ethiopia. J. Environ. Public Health 2020, 2020, 7367139. [Google Scholar] [CrossRef]
- Gagebo, D.D.; Kerbo, A.A.; Thangavel, T. Undernutrition and associated factors among adolescent girls in Damot Sore District, Southern Ethiopia. J. Nutr. Metab. 2020, 2020, 5083140. [Google Scholar] [CrossRef] [PubMed]
- Arage, G.; Assefa, M.; Worku, T. Socio-demographic and economic factors are associated with nutritional status of adolescent school girls in Lay Guyint Woreda, Northwest Ethiopia. SAGE Open Med. 2019, 7, 2050312119844679. [Google Scholar] [CrossRef] [PubMed]
- Zemene, M.A.; Engidaw, M.T.; Gebremariam, A.D.; Asnakew, D.T.; Tiruneh, S.A. Nutritional status and associated factors among high school adolescents in Debre Tabor Town, South Gondar Zone, Northcentral Ethiopia. BMC Nutr. 2019, 5, 43. [Google Scholar] [CrossRef] [PubMed]
- Mengesha, D.K.; Prasad, R.P.; Asres, D.T. Prevalence and Associated factors of thinness among adolescent students in Finote Selam Town, Northwest Ethiopia. Sci. World J. 2020, 2020, 9170301. [Google Scholar] [CrossRef]
- Feyzabadi, V.Y.; Mohammadi, N.K.; Omidvar, N.; Karimi-Shahanjarini, A.; Nedjat, S.; Rashidian, A. Factors associated with unhealthy snacks consumption among adolescents in Iran’s schools. Int. J. Health Policy Manag. 2017, 6, 519–528. [Google Scholar] [CrossRef] [PubMed]
- Ashebir Kebede, W.; Yimer Ayele, B. Magnitude of stunting and associated factors among adolescent students in Legehida District, Northeast Ethiopia. J. Nutr. Metab. 2021, 2021, 2467883. [Google Scholar] [CrossRef] [PubMed]
- Pandurangi, R.; Mummadi, M.K.; Challa, S.; Reddy, N.S.; Kaliaperumal, V.; Khadar Babu, C.; Telikicherla, U.R.; Pullakandham, R.; Geddam, J.B.; Hemalatha, R. Burden and predictors of malnutrition among Indian adolescents (10–19 years): Insights from Comprehensive National Nutrition Survey Data. Front. Public Health 2022, 10, 877073. [Google Scholar] [CrossRef] [PubMed]
- Phuljhele, S.; Dewangan, S. Anu Assessment of the nutritional status of adolescent girls aged between 15 to 18 years studying in government high school in Raipur, Chhattisgarh, India. Pediatr. Rev. Int. J. Pediatr. Res. 2021, 8, 100–108. [Google Scholar] [CrossRef]
- Palriwala, R. Economics and patriliny: Consumption and authority within the household. Soc. Sci. 1993, 1, 47–73. [Google Scholar] [CrossRef]
- Kuhnlein, H.V.; Erasmus, B.; Spigelski, D. Indigenous Peoples’ Food Systems: The Many Dimensions of Culture, Diversity and Environment for Nutrition and Health; Food and Agriculture Organization of the United Nations (FAO): Rome, Italy, 2009. [Google Scholar]
- Toledo, Á.; Burlingame, B. Biodiversity and nutrition: A common path toward global food security and sustainable development. J. Food Compos. Anal. 2006, 19, 477–483. [Google Scholar] [CrossRef]
- Mannar, V.; Micha, R.; Allemandi, L.; Afshin, A.; Baker, P.; Battersby, J.; Bhutta, Z.; Corvalan, C.; Di Cesare, M.; Chen, K.; et al. 2020 Global Nutrition Report: Action on Equity to End Malnutrition; Development Initiatives Poverty Research: Bristol, UK, 2020; p. 89023. [Google Scholar]
- Bhatia, K.; Independent Expert Group, IEG. Global Nutrition Report: From Promise to Impact: Ending Malnutrition by 2030; Global Nutrition Report Stakeholder Group: Washington, DC, USA, 2016. [Google Scholar]
- Galab, S.; Ravi, C.; Revathi, E.; Sreedevi, N.; Aparna, P. Human Development Report 2017 Telangana State; Centre for Economic: Telangana, India, 2017. [Google Scholar]
- WHO. Measuring Change in Nutritional Status; World Health Organization: Geneva, Switzerland, 1982. [Google Scholar]
- WHO. Physical Status: The Use and Interpretation of Anthropometry; Report of a WHO Expert Committee; World Health Organization: Geneva, Switzerland, 1995. [Google Scholar]
- Querol, S.E.; Gill, P.; Iqbal, R.; Kletter, M.; Ozdemir, N.; Al-Khudairy, L. Adolescent undernutrition in South Asia: A scoping review. Nutr. Res. Rev. 2022, 35, 39–49. [Google Scholar] [CrossRef] [PubMed]
- Chandrashekarappa, S.M.; Ramakrishnaiah, N.M.M.; Manjunath, R. Nutritional status in adolescent girls: Attempt to determine its prevalence and its association with sociodemographic variables. Fam. Med. Community Health 2018, 6, 184–190. [Google Scholar] [CrossRef]
- Lemma Getacher, B.W.A.; Belachew, T. Lived Experience and Perceptions of Adolescents on Prevention, Causes and Consequences of Double Burden of Malnutrition in Debre Berhan City, Ethiopia: A Qualitative Study. Int. J. Gen. Med. 2023, 16, 337–356. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Bevan, M.T. A method of phenomenological interviewing. Qual. Health Res. 2014, 24, 136–144. [Google Scholar] [CrossRef]
- Laxmaiah, A.; Mallikharjuna Rao, K.; Hari Kumar, R.; Arlappa, N.; Venkaiah, K.; Brahmam, G. Diet and nutritional status of tribal population in ITDA project areas of Khammam district, Andhra Pradesh. J. Hum. Ecol. 2007, 21, 79–86. [Google Scholar] [CrossRef]
- Caulfield, L.E.; Elliot, V. Nutrition of Adolescent Girls and Women of Reproductive Age in Low- and Middle-Income Countries: Current Context and Scientific Basis for Moving Forward; Strengthening Partnerships, Results, and Innovations in Nutrition Globally (SPRING) Project: Arlington, VA, USA, 2015. [Google Scholar]
- Medhi, G.; Hazarika, N.; Mahanta, J. Nutritional status of adolescents among tea garden workers. Indian J. Pediatr. 2007, 74, 343–347. [Google Scholar] [CrossRef] [PubMed]
- Malhotra, A.; Passi, S.J. Diet quality and nutritional status of rural adolescent girl beneficiaries of ICDS in North India. Asia Pac. J. Clin. Nutr. 2007, 16, 8–16. [Google Scholar]
- Subramanian, S.; Smith, G.D. Patterns, distribution, and determinants of under-and overnutrition: A population-based study of women in India. Am. J. Clin. Nutr. 2006, 84, 633–640. [Google Scholar] [CrossRef]
- Ndukwu, C.; Egbuonu, I.; Ulasi, T.; Ebenebe, J. Determinants of undernutrition among primary school children residing in slum areas of a Nigerian city. Niger. J. Clin. Pract. 2013, 16, 178–183. [Google Scholar] [CrossRef] [PubMed]
- Sarkar, D.; Haldar, S.K. Socioeconomic Determinants of Child Malnutrition in India: Evidence from NFHS-III. SSRN 2014, 2420293. [Google Scholar] [CrossRef]
- Vyas, S.; Kandpal, S.; Semwal, J. A study on undernutrition and its socioeconomic correlates among toddlers in a rural area of Uttarakhand, India. Int. J. Community Med. Public Health 2017, 3, 1043–1048. [Google Scholar] [CrossRef]
- Madjdian, D.S.; Azupogo, F.; Osendarp, S.J.; Bras, H.; Brouwer, I.D. Socio-cultural and economic determinants and consequences of adolescent undernutrition and micronutrient deficiencies in LLMICs: A systematic narrative review. Ann. N. Y. Acad. Sci. 2018, 1416, 117–139. [Google Scholar] [CrossRef]
- Kumar, V.; Basu, D.; Reddy, B.M. Genetic heterogeneity in northeastern India: Reflection of tribe–caste continuum in the genetic structure. Am. J. Hum. Biol. Off. J. Hum. Biol. Assoc. 2004, 16, 334–345. [Google Scholar] [CrossRef]
- Padmaja, R.; Kavitha, K.; Pramanik, S.; Aravazhi, S. Prevalence of Malnutrition in Adolescent Girls: A Cross-Sectional Study in the Tribal Regions of Telangana. 2019, Volume 2, pp. 1–13. Available online: http://oar.icrisat.org/11380/1/ICRISAT-Malnutrition%20in%20Adolescent%20Girls-Fullpaper-AERA-2019.pdf (accessed on 12 December 2023).




| Particulars | Values |
|---|---|
| Household Type (%) | |
| Male and female adult | 65.47 |
| Female adult only | 9.93 |
| Male adult only | 24.60 |
| Gender of Household Head (%) | |
| Male | 86.47 |
| Female | 13.53 |
| Average age of household head (years) | 43.00 |
| Education Status of Household Head (%) | |
| Illiterate or just able to sign | 62.30 |
| Up to primary level | 13.53 |
| Secondary level or above | 24.17 |
| Household Income | |
| Average monthly per-capita income (in INR) | 1338 |
| Income (per-capita/month) ≤ INR 1000 (% of households) | 53.38 |
| Income (per-capita/month) between INR 1001–2000 (% of households) | 35.83 |
| Income (per-capita/month) > INR 2000 (% of households) | 10.79 |
| Family Size | |
| Average family size (Number of individuals) | 4.68 |
| Family size ≤ 4 (% of households) | 50.50 |
| Family size 5–6 (% of households) | 38.56 |
| Family size > 6 (% of households) | 10.94 |
| Sanitation—Toilet Availability (%) | |
| Yes | 18.85 |
| No | 81.15 |
| Indicator | Early Adolescent | Late Adolescent | Overall |
|---|---|---|---|
| Height (cm) | 141.89 (8.96) | 150.45 * (5.80) | 146.32 (8.62) |
| Weight (kg) | 33.05 (7.42) | 42.10 * (7.11) | 37.74 (8.55) |
| BMI (kg/m2) | 16.22 (2.43) | 18.54 * (2.72) | 17.42 (2.83) |
| Variable | Model 1 | Model 2 |
|---|---|---|
| (Exposure Variable: Stunted = 1 vs. Non-Stunted = 0) | (Exposure Variable: Underweight = 1 vs. Normal BMI = 0) | |
| Odds Ratio (OR) | Odds Ratio (OR) | |
| Adolescent dummy (Early adolescent = 0, Late adolescent = 1) | 1.676 *** (0.002) | 0.210 *** (0.000) |
| Household size | 1.008 (0.883) | 1.067 (0.305) |
| Head gender (Male = 1, Female = 0) | 1.231 (0.396) | 1.194 (0.522) |
| Age of household head (Years) | 0.985 (0.129) | 0.992 (0.501) |
| Education of head (Illiterate or just able to sign = 1, Up to primary = 2, Secondary and above = 3) | 0.782 *** (0.016) | 0.788 ** (0.036) |
| Monthly per-capita income (In INR “000”) | 1.000 (0.553) | 1.000 (0.149) |
| Access to toilet (Available = 1, Otherwise = 0) | 0.689 * (0.072) | 0.879 (0.570) |
| Education of adolescent (Illiterate or just able to sign = 1, Up to primary (Grade 1 to 5) = 2, Secondary level and above (Grade 6 and above) = 3 | 0.796 * (0.077) | 0.934 (0.632) |
| Constant | 5.021 *** (0.008) | 9.665 *** (0.001) |
| LR chi2 (8) | 24.52 | 92.55 |
| Prob > chi2 | 0.0019 | 0.0000 |
| Log likelihood | −457.055 | −382.598 |
| Pseudo R2 | 0.026 | 0.108 |
| Number of observations | 695 | 695 |
| Food Groups | Early Adolescent | Late Adolescent |
|---|---|---|
| Energy-rich | 10 | 20 |
| Micronutrient-rich | 45 | 20 |
| Protein-rich | 45 | 60 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ravula, P.; Kasala, K.; Pramanik, S.; Selvaraj, A. Stunting and Underweight among Adolescent Girls of Indigenous Communities in Telangana, India: A Cross-Sectional Study. Nutrients 2024, 16, 731. https://doi.org/10.3390/nu16050731
Ravula P, Kasala K, Pramanik S, Selvaraj A. Stunting and Underweight among Adolescent Girls of Indigenous Communities in Telangana, India: A Cross-Sectional Study. Nutrients. 2024; 16(5):731. https://doi.org/10.3390/nu16050731
Chicago/Turabian StyleRavula, Padmaja, Kavitha Kasala, Soumitra Pramanik, and Aravazhi Selvaraj. 2024. "Stunting and Underweight among Adolescent Girls of Indigenous Communities in Telangana, India: A Cross-Sectional Study" Nutrients 16, no. 5: 731. https://doi.org/10.3390/nu16050731







