The Effectiveness of Artificial Intelligence in Assisting Mothers with Assessing Infant Stool Consistency in a Breastfeeding Cohort Study in China
Abstract
:1. Introduction
2. Materials and Methods
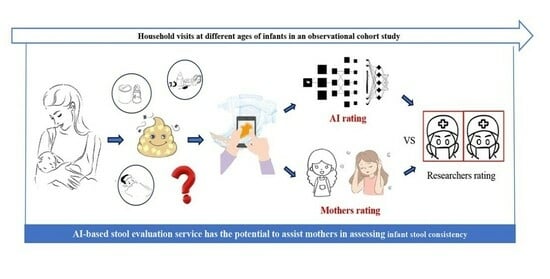
2.1. Schematic Overview of the Cohort Study
2.2. Study Participants
2.3. Site Investigation and Quality Control
2.4. Assessment of Infant Gastrointestinal Symptoms, Quality of Life, and Maternal Postpartum Depression
2.5. Photographic Documentation and Evaluation of Diaper Feces
2.6. Consistency Evaluation of Photographs of Baby Diaper Feces
2.7. Statistical Analysis
3. Results
3.1. Characteristics of the Study Population
3.2. Comparison of Mothers’ Self-Reported Scores and AI-Graded Scores
3.3. Analysis of Factors Influencing the Degree of Mothers’ Deviation
3.4. Multivariable Tobit Regression Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Quinlan, P.T.; Lockton, S.; Irwin, J.; Lucas, A.L. The relationship between stool hardness and stool composition in breast- and formula-fed infants. J. Pediatr. Gastroenterol. Nutr. 1995, 20, 81–90. [Google Scholar]
- Carnielli, V.P.; Verlato, G.; Pederzini, F.; Luijendijk, I.; Boerlage, A.; Pedrotti, D.; Sauer, P.J. Intestinal absorption of long-chain polyunsaturated fatty acids in preterm infants fed breast milk or formula. Am. J. Clin. Nutr. 1998, 67, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Toca, M.D.C.; Fernández, A.; Orsi, M.; Tabacco, O.; Vinderola, G. Lactose intolerance: Myths and facts. An update. Arch. Argent. Pediatr. 2022, 120, 59–66. [Google Scholar] [PubMed]
- Cederlund, A.; Kai-Larsen, Y.; Printz, G.; Yoshio, H.; Alvelius, G.; Lagercrantz, H.; Strömberg, R.; Jörnvall, H.; Gudmundsson, G.H.; Agerberth, B. Lactose in human breast milk an inducer of innate immunity with implications for a role in intestinal homeostasis. PLoS ONE 2013, 8, e53876. [Google Scholar] [CrossRef] [PubMed]
- Zivkovic, A.M.; German, J.B.; Lebrilla, C.B.; Mills, D.A. Human milk glycobiome and its impact on the infant gastrointestinal microbiota. Proc. Natl. Acad. Sci. USA 2011, 108 (Suppl. S1), 4653–4658. [Google Scholar] [CrossRef] [PubMed]
- Iacono, G.; Merolla, R.; D’amico, D.; Bonci, E.; Cavataio, F.; Di Prima, L.; Scalici, C.; Indinnimeo, L.; Averna, M.; Carroccio, A. Gastrointestinal symptoms in infancy: A population-based prospective study. Dig. Liver Dis. 2005, 37, 432–438. [Google Scholar] [CrossRef] [PubMed]
- Gustin, J.; Gibb, R.; Kenneally, D.; Kutay, B.; Siu, S.W.; Roe, D. Characterizing exclusively breastfed infant stool via a novel infant stool scale. JPEN J. Parenter. Enteral. Nutr. 2018, 42 (Suppl. S1), S5–S11. [Google Scholar] [CrossRef] [PubMed]
- Mahon, J.; Lifschitz, C.; Ludwig, T.; Thapar, N.; Glanville, J.; Miqdady, M.; Saps, M.; Quak, S.H.; Wijnkoop, I.L.; Edwards, M.; et al. The costs of functional gastrointestinal disorders and related signs and symptoms in infants: A systematic literature review and cost calculation for England. BMJ Open 2017, 7, e015594. [Google Scholar] [CrossRef]
- O’Donnell, L.J.; Virjee, J.; Heaton, K.W. Detection of pseudodiarrhoea by simple clinical assessment of intestinal transit rate. BMJ 1990, 300, 439–440. [Google Scholar] [CrossRef]
- Vandeputte, D.; Falony, G.; Vieira-Silva, S.; Tito, R.Y.; Joossens, M.; Raes, J. Stool consistency is strongly associated with gut microbiota richness and composition, enterotypes and bacterial growth rates. Gut 2016, 65, 57–62. [Google Scholar] [CrossRef]
- Huysentruyt, K.; Koppen, I.; Benninga, M.; Cattaert, T.; Cheng, J.; De Geyter, C.; Faure, C.; Gottrand, F.; Hegar, B.; Hojsak, I.; et al. The Brussels infant and toddler stool scale: A study on interobserver reliability. J. Pediatr. Gastroenterol. Nutr. 2019, 68, 207–213. [Google Scholar] [CrossRef]
- Heaton, K.W.; Radvan, J.; Cripps, H.; Mountford, R.A.; Braddon, F.E.; Hughes, A.O. Defecation frequency and timing, and stool form in the general population: A prospective study. Gut 1992, 33, 818–824. [Google Scholar] [CrossRef]
- Bekkali, N.; Hamers, S.L.; Reitsma, J.B.; Van Toledo, L.; Benninga, M.A. Infant stool form scale: Development and results. J. Pediatr. 2009, 154, 521–526.e521. [Google Scholar] [CrossRef]
- Ghanma, A.; Puttemans, K.; Deneyer, M.; Benninga, M.; Vandenplas, Y. Amsterdam infant stool scale is more useful for assessing children who have not been toilet trained than Bristol stool scale. Acta Paediatr. 2014, 103, 91–92. [Google Scholar] [CrossRef] [PubMed]
- Vandenplas, Y.; Szajewska, H.; Benninga, M.; Di Lorenzo, C.; Dupont, C.; Faure, C.; Miqdadi, M.; Osatakul, S.; Ribes-Konickx, C.; Saps, M.; et al. Development of the Brussels infant and toddler stool scale (‘BITSS’): Protocol of the study. BMJ Open 2017, 7, e014620. [Google Scholar] [CrossRef]
- Hofman, Y.M.C.; Vandenplas, Y.; Ludwig, T.; Chaib, A.O.; Kluyfhout, S.; Krikilion, J.; De Geyter, C.; Huysentruyt, K. Intra-rater variability of the Brussels infants and toddlers stool scale (BITSS) using photographed stools. J. Pediatr. Gastroenterol. Nutr. 2022, 75, 584–588. [Google Scholar] [CrossRef] [PubMed]
- Velasco-Benitez, C.A.; Llanos-Chea, A.; Saps, M. Utility of the brussels infant and toddler stool scale (BITSS) and bristol stool scale in non-toilet-trained children: A large comparative study. Neurogastroenterol. Motil. 2021, 33, e14015. [Google Scholar] [CrossRef] [PubMed]
- Aman, B.A.; Levy, E.I.; Hofman, B.; Vandenplas, Y.; Huysentruyt, K. Real time versus photographic assessment of stool consistency using the Brussels infant and toddler stool scale: Are they telling us the same? Pediatr. Gastroenterol. Hepatol. Nutr. 2021, 24, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Feng, B.; Huang, S.-D.; Luo, J.-F.; Zhang, H.-D. A validation study of a locally adapted Brussels infant and toddler stool scale of the Chinese version. Gastroenterol. Nurs 2022, 45, 85–90. [Google Scholar] [CrossRef] [PubMed]
- Webb, R.; Ayers, S. Cognitive biases in processing infant emotion by women with depression, anxiety and post-traumatic stress disorder in pregnancy or after birth: A systematic review. Cogn. Emot. 2015, 29, 1278–1294. [Google Scholar] [CrossRef]
- Esteva, A.; Kuprel, B.; Novoa, R.A.; Ko, J.; Swetter, S.M.; Blau, H.M.; Thrun, S. Dermatologist-level classification of skin cancer with deep neural networks. Nature 2017, 542, 115–118. [Google Scholar] [CrossRef]
- Hosny, A.; Parmar, C.; Quackenbush, J.; Schwartz, L.H.; Aerts, H. Artificial intelligence in radiology. Nat. Rev. Cancer 2018, 18, 500–510. [Google Scholar] [CrossRef]
- Chilamkurthy, S.; Ghosh, R.; Tanamala, S.; Biviji, M.; Campeau, N.G.; Venugopal, V.K.; Mahajan, V.; Rao, P.; Warier, P. Deep learning algorithms for detection of critical findings in head CT scans: A retrospective study. Lancet 2018, 392, 2388–2396. [Google Scholar] [CrossRef]
- Dar, S.U.H.; Öztürk, Ş.; Özbey, M.; Oguz, K.K.; Çukur, T. Parallel-stream fusion of scan-specific and scan-general priors for learning deep MRI reconstruction in low-data regimes. Comput. Biol. Med. 2023, 167, 107610. [Google Scholar] [CrossRef] [PubMed]
- Ludwig, T.; Oukid, I.; Wong, J.; Ting, S.; Huysentruyt, K.; Roy, P.; Foussat, A.C.; Vandenplas, Y. Machine learning supports automated digital image scoring of stool consistency in diapers. J. Pediatr. Gastroenterol. Nutr. 2021, 72, 255–261. [Google Scholar] [CrossRef] [PubMed]
- Xiao, F.; Wang, Y.; Ludwig, T.; Li, X.; Chen, S.; Sun, N.; Zheng, Y.; Huysentruyt, K.; Vandenplas, Y.; Zhang, T. Generation and application of a convolutional neural networks algorithm in evaluating stool consistency in diapers. Acta Paediatr. 2023, 112, 1333–1340. [Google Scholar] [CrossRef] [PubMed]
- Riley, A.W.; Trabulsi, J.; Yao, M.; Bevans, K.B.; DeRusso, P.A. Validation of a parent report questionnaire: The infant gastrointestinal symptom questionnaire. Clin. Pediatr. 2015, 54, 1167–1174. [Google Scholar] [CrossRef] [PubMed]
- Varni, J.W.; Limbers, C.A.; Neighbors, K.; Schulz, K.; Lieu, J.E.C.; Heffer, R.W.; Tuzinkiewicz, K.; Mangione-Smith, R.; Zimmerman, J.J.; Alonso, E.M. The PedsQL™ infant scales: Feasibility, internal consistency reliability, and validity in healthy and ill infants. Qual. Life Res. 2011, 20, 45–55. [Google Scholar] [CrossRef] [PubMed]
- Varni, J.W.; Burwinkle, T.M.; Seid, M. The PedsQL as a pediatric patient-reported outcome: Reliability and validity of the PedsQL measurement model in 25,000 children. Expert Rev. Pharmacoecon. Outcomes Res. 2005, 5, 705–719. [Google Scholar] [CrossRef]
- Cox, J.L.; Holden, J.M.; Sagovsky, R. Detection of postnatal depression. Development of the 10-item Edinburgh postnatal depression scale. Br. J. Psychiatry 1987, 150, 782–786. [Google Scholar] [CrossRef] [PubMed]
- Macedo, M.D.; Ellström Engh, M.; Siafarikas, F. Detailed classification of second-degree perineal tears in the delivery ward: An inter-rater agreement study. Acta Obstet. Gynecol. Scand. 2022, 101, 880–888. [Google Scholar] [CrossRef]
- Pimentel, M.; Mathur, R.; Wang, J.; Chang, C.; Hosseini, A.; Fiorentino, A.; Rashid, M.; Pichetshote, N.; Basseri, B.; Treyzon, L.; et al. A smartphone application using artificial intelligence is superior to subject self-reporting when assessing stool form. Am. J. Gastroenterol. 2022, 117, 1118–1124. [Google Scholar] [CrossRef]
- Wang, Z.; Liu, J.; Shuai, H.; Cai, Z.; Fu, X.; Liu, Y.; Xiao, X.; Zhang, W.; Krabbendam, E.; Liu, S.; et al. Mapping global prevalence of depression among postpartum women. Transl. Psychiatry 2021, 11, 543. [Google Scholar] [CrossRef]
- Nisar, A.; Yin, J.; Waqas, A.; Bai, X.; Wang, D.; Rahman, A.; Li, X. Prevalence of perinatal depression and its determinants in mainland China: A systematic review and meta-analysis. J. Affect. Disord. 2020, 277, 1022–1037. [Google Scholar] [CrossRef] [PubMed]
- Gotlib, I.H.; Krasnoperova, E.; Yue, D.N.; Joormann, J. Attentional biases for negative interpersonal stimuli in clinical depression. J. Abnorm. Psychol. 2004, 113, 121–135. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; Wang, S.; Li, X.Q. Association between mode of delivery and postpartum depression: A systematic review and network meta-analysis. Aust. N. Z. J. Psychiatry 2021, 55, 588–601. [Google Scholar] [CrossRef] [PubMed]
- Youn, H.; Lee, S.; Han, S.W.; Kim, L.Y.; Lee, T.-S.; Oh, M.-J.; Jeong, H.-G.; Cho, G.J. Obstetric risk factors for depression during the postpartum period in south Korea: A nationwide study. J. Psychosom. Res. 2017, 102, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Matsumura, K.; the Japan Environment and Children’s Study (JECS) Group; Hamazaki, K.; Tsuchida, A.; Kasamatsu, H.; Inadera, H. Education level and risk of postpartum depression: Results from the Japan environment and children’s study (JECS). BMC Psychiatry 2019, 19, 419. [Google Scholar] [CrossRef]
- Inandi, T.; Elci, O.C.; Ozturk, A.; Egri, M.; Polat, A.; Sahin, T.K. Risk factors for depression in postnatal first year, in eastern turkey. Int. J. Epidemiol. 2002, 31, 1201–1207. [Google Scholar] [CrossRef] [PubMed]
- Lewis, S.J.; Heaton, K.W. Stool form scale as a useful guide to intestinal transit time. Scand. J. Gastroenterol. 1997, 32, 920–924. [Google Scholar] [CrossRef] [PubMed]
- Morais, M.B. Signs and symptoms associated with digestive tract development. J. Pediatr. 2016, 92, S46–S56. [Google Scholar] [CrossRef]




| Characteristics | Classification | N (%) |
|---|---|---|
| Age of mother (years) | <30 | 51 (41.2) |
| 30–35 | 59 (45.0) | |
| >35 | 18 (13.8) | |
| Occupation | Employed | 117 (89.3) |
| Unemployed/Housewife | 14 (10.7) | |
| Education level | Junior college and below | 43 (32.8) |
| University and above | 88 (67.2) | |
| Per capita monthly income (yuan/month) | <6250 | 30 (22.9) |
| 6250–12,500 | 65 (49.6) | |
| >12,500 | 36 (27.5) | |
| Parity | Multiparity | 51 (38.9) |
| Primiparity | 80 (61.1) | |
| Pregnancy complication history | Yes | 78 (59.5) |
| No | 53 (40.5) | |
| Mode of delivery | Vaginal | 80 (61.1) |
| Cesarean | 51 (38.9) | |
| Feeding patterns | Breastfeeding | 72 (55.0) |
| Mixed feeding | 59 (45.0) | |
| Postpartum depression | Yes | 43 (32.8) |
| No | 88 (67.2) | |
| EPDS score * | 7 (4, 10) |
| Classification | Comparator Groups | ICC (95% CI) | Kendall’s W | Percentage Agreement (95% CI) |
|---|---|---|---|---|
| Seven types | AI vs. researchers | 0.754 (0.719, 0.784) | 0.836 * | 95.5 (94.1, 96.9) |
| Mothers vs. researchers | - | - | - | |
| Four categories | AI vs. researchers | 0.782 (0.752, 0.809) | 0.840 * | 95.8 (94.5, 97.1) |
| Mothers vs. researchers | 0.070 (−0.039, 0.169) | 0.523 | 66.9 (63.8, 70.0) |
| Characteristic | Classification | Degree of Mothers’ Deviation, M (P25, P75) | Z/H | p |
|---|---|---|---|---|
| Age of mother (years) | <30 (n = 37) | 0.00 (0.00, 0.44) | 4.305 | 0.116 |
| 30–35 (n = 44) | 0.20 (0.00, 0.90) | |||
| >35 (n = 17) | 0.29 (0.00, 0.83) | |||
| Occupation | Employed (n = 86) | 0.07 (0.00, 0.62) | −1.733 | 0.083 |
| Unemployed/Housewife (n = 12) | 0.54 (0.19, 0.88) | |||
| Education level | Junior college and below (n = 34) | 0.25 (0.05, 0.92) | −2.047 | 0.041 |
| University and above (n = 64) | 0.05 (0.00, 0.60) | |||
| Per capita monthly income (yuan/month) | <6250 (n = 21) | 0.07 (0.00, 0.80) | 1.629 | 0.443 |
| 6250–12,500 (n = 51) | 0.23 (0.00, 0.86) | |||
| >12,500 (n = 26) | 0.07 (0.00, 0.37) | |||
| Parity | Multiparity (n = 40) | 0.08 (0.00, 0.55) | −0.827 | 0.408 |
| Primiparity (n = 58) | 0.23 (0.00, 0.76) | |||
| Pregnancy complication history | Yes (n = 60) | 0.24 (0.00, 0.73) | −0.324 | 0.746 |
| No (n = 38) | 0.07 (0.00, 0.68) | |||
| Mode of delivery | Vaginal (n = 65) | 0.07 (0.00, 0.45) | −1.743 | 0.081 |
| Cesarean (n = 33) | 0.26 (0.00, 0.94) | |||
| Feeding patterns | Breast-feeding | 0.22 (0.00, 0.77) | −1.249 | 0.212 |
| Mixed-feeding | 0.03 (0.00, 0.53) | |||
| Postpartum depression | Yes (n = 30) | 0.33 (0.00, 0.94) | −1.719 | 0.086 |
| No (n = 68) | 0.07 (0.00, 0.48) | |||
| EPDS score * | 7.00 (4.00, 12.00) | 0.248 | 0.014 |
| Characteristic | β (95% CI) | SE | z | p |
|---|---|---|---|---|
| Constant | −0.196 (−0.962, 0.570) | 0.391 | 0.502 | 0.616 |
| EPDS score | 0.023 (0.001, 0.045) | 0.011 | 2.077 | 0.038 |
| Education level (ref. = Junior college and below) | ||||
| University and above | −0.149 (−0.403, 0.104) | 0.129 | −1.154 | 0.248 |
| Mode of delivery (ref. = Vaginal) | ||||
| Cesarean | 0.151 (−0.098, 0.399) | 0.127 | 1.190 | 0.234 |
| Occupation (ref. = Employed) | ||||
| Unemployed/Housewife | 0.205 (−0.153, 0.562) | 0.182 | 1.123 | 0.262 |
| Stratified Condition | EPDS Score | Mothers’ Deviation | β (95% CI) | SE | z | p |
|---|---|---|---|---|---|---|
| Junior college and below 1 | 9.00 (4.75, 12.25) | 0.25 (0.05, 0.92) | 0.025 (−0.002, 0.051) | 0.014 | 1.824 | 0.068 |
| University and above 1 | 6.50 (4.00, 9.00) | 0.05 (0.00, 0.60) | 0.028 (−0.007, 0.063) | 0.018 | 1.590 | 0.112 |
| Cesarean 2 | 8.00 (4.00, 12.00) | 0.26 (0.00, 0.94) | 0.040 (0.025, 0.075) | 0.018 | 2.262 | 0.024 |
| Vaginal 2 | 7.00 (4.00, 10.00) | 0.07 (0.00, 0.45) | 0.014 (−0.015, 0.044) | 0.015 | 0.955 | 0.339 |
| Employed 3 | 7.00 (4.00, 10.50) | 0.07 (0.00, 0.62) | 0.024 (0.000, 0.048) | 0.012 | 1.960 | 0.050 |
| Unemployed/Housewife 3 | 8.50 (2.50, 12.00) | 0.54 (0.19, 0.88) | 0.036 (−0.011, 0.082) | 0.024 | 1.508 | 0.132 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, J.; Dong, L.; Sun, Y.; Zhao, X.; Gan, J.; Wang, Z. The Effectiveness of Artificial Intelligence in Assisting Mothers with Assessing Infant Stool Consistency in a Breastfeeding Cohort Study in China. Nutrients 2024, 16, 855. https://doi.org/10.3390/nu16060855
Wu J, Dong L, Sun Y, Zhao X, Gan J, Wang Z. The Effectiveness of Artificial Intelligence in Assisting Mothers with Assessing Infant Stool Consistency in a Breastfeeding Cohort Study in China. Nutrients. 2024; 16(6):855. https://doi.org/10.3390/nu16060855
Chicago/Turabian StyleWu, Jieshu, Linjing Dong, Yating Sun, Xianfeng Zhao, Junai Gan, and Zhixu Wang. 2024. "The Effectiveness of Artificial Intelligence in Assisting Mothers with Assessing Infant Stool Consistency in a Breastfeeding Cohort Study in China" Nutrients 16, no. 6: 855. https://doi.org/10.3390/nu16060855
APA StyleWu, J., Dong, L., Sun, Y., Zhao, X., Gan, J., & Wang, Z. (2024). The Effectiveness of Artificial Intelligence in Assisting Mothers with Assessing Infant Stool Consistency in a Breastfeeding Cohort Study in China. Nutrients, 16(6), 855. https://doi.org/10.3390/nu16060855