Evaluation of Intermittent Restricted Eating Using the Interval Weight Loss Online Platform in an Everyday Setting
Abstract
1. Introduction
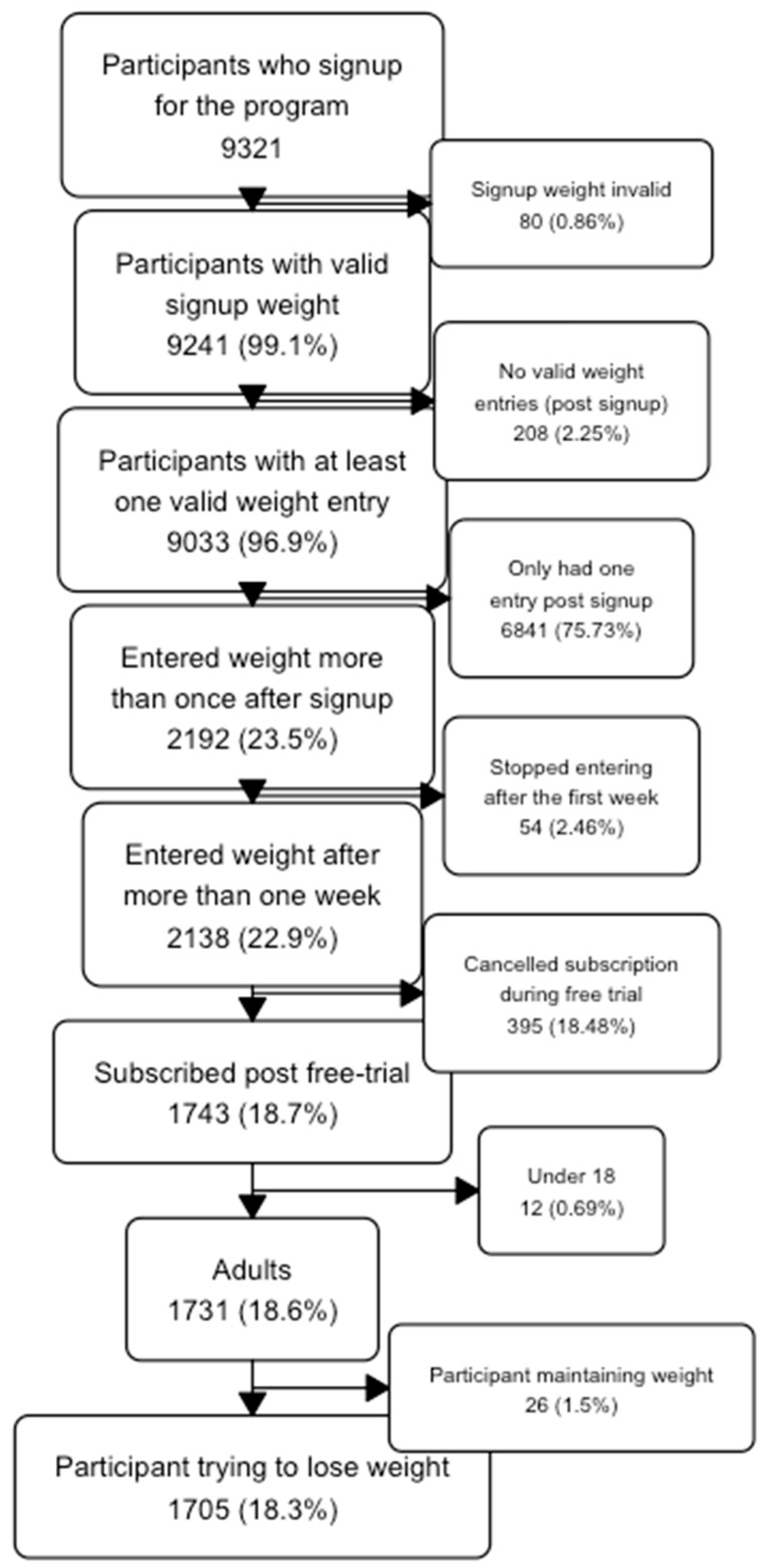
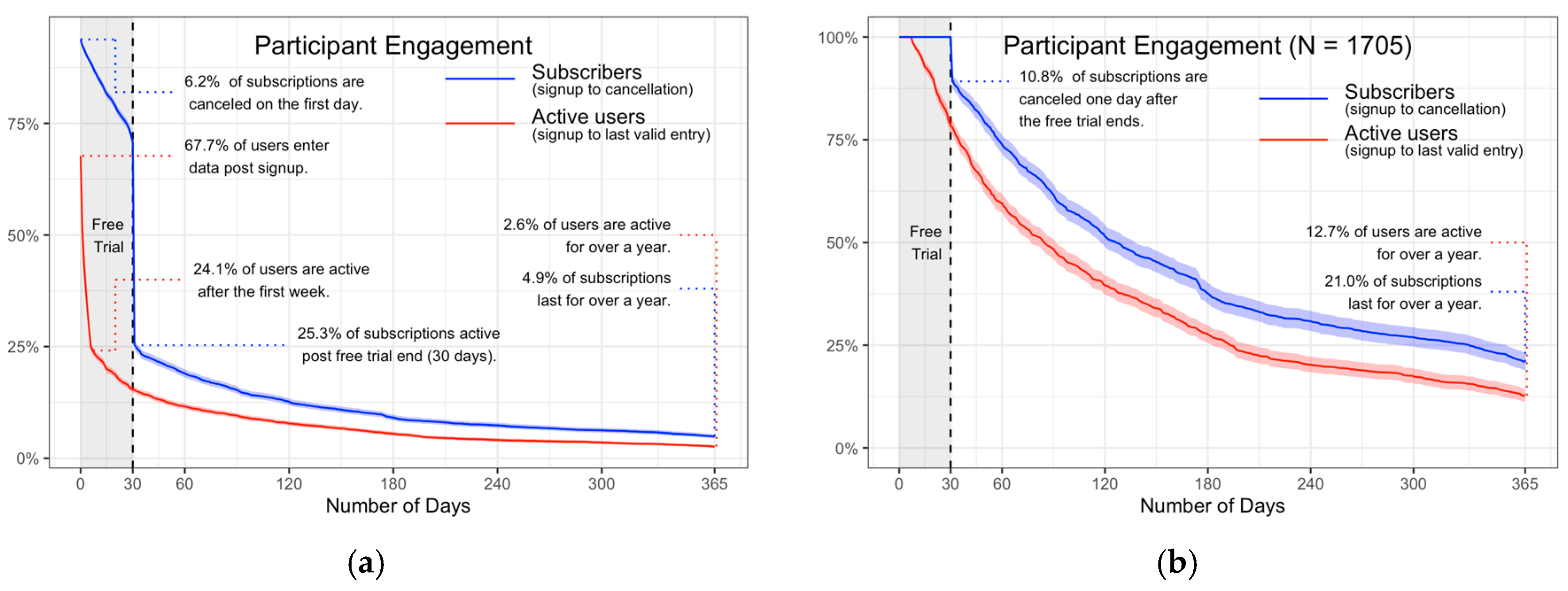
- Describe the participation patterns and dropout of subscribers to the IWL program;
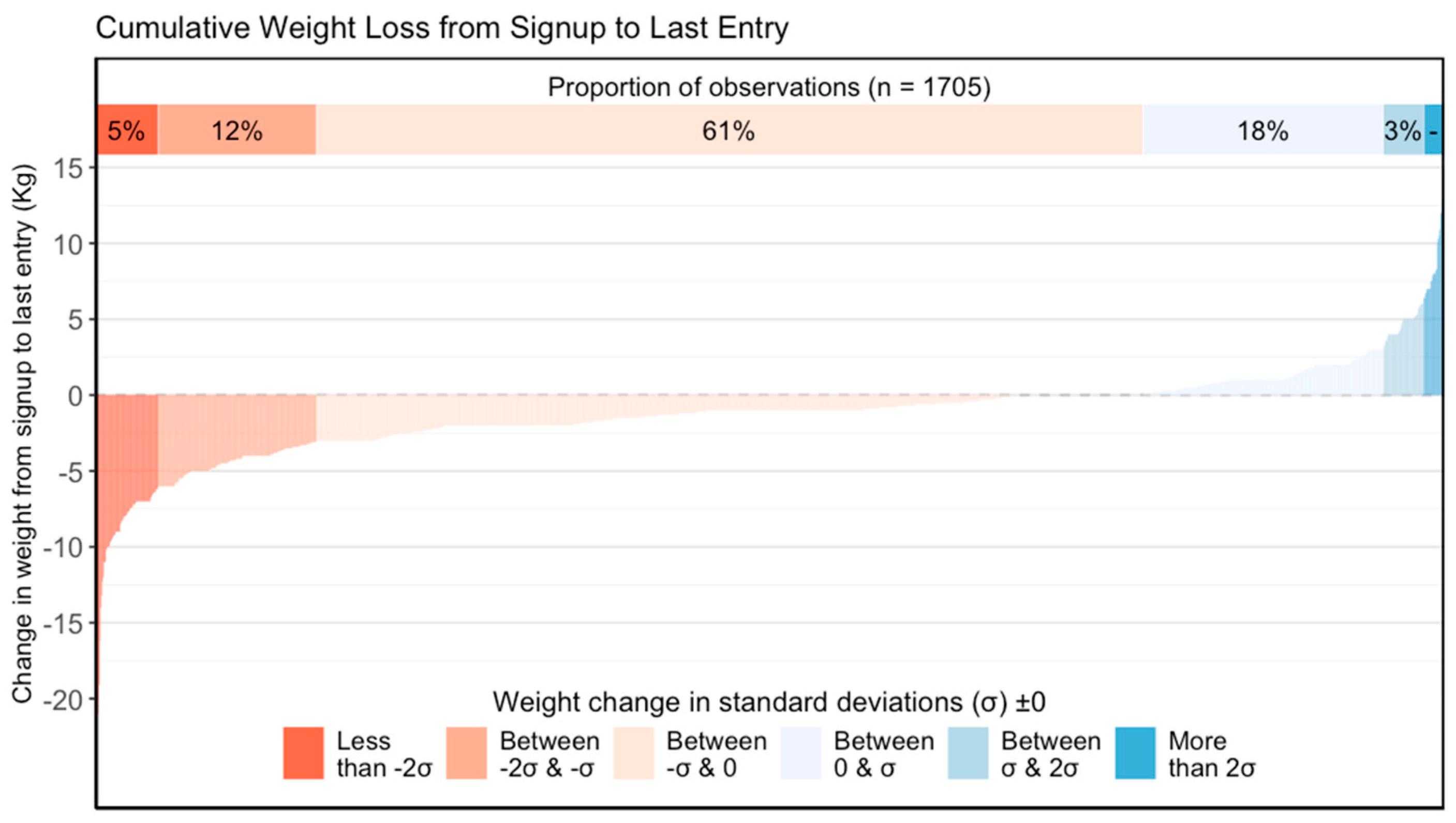
- Characterise the average long-term weight loss of subscribers;
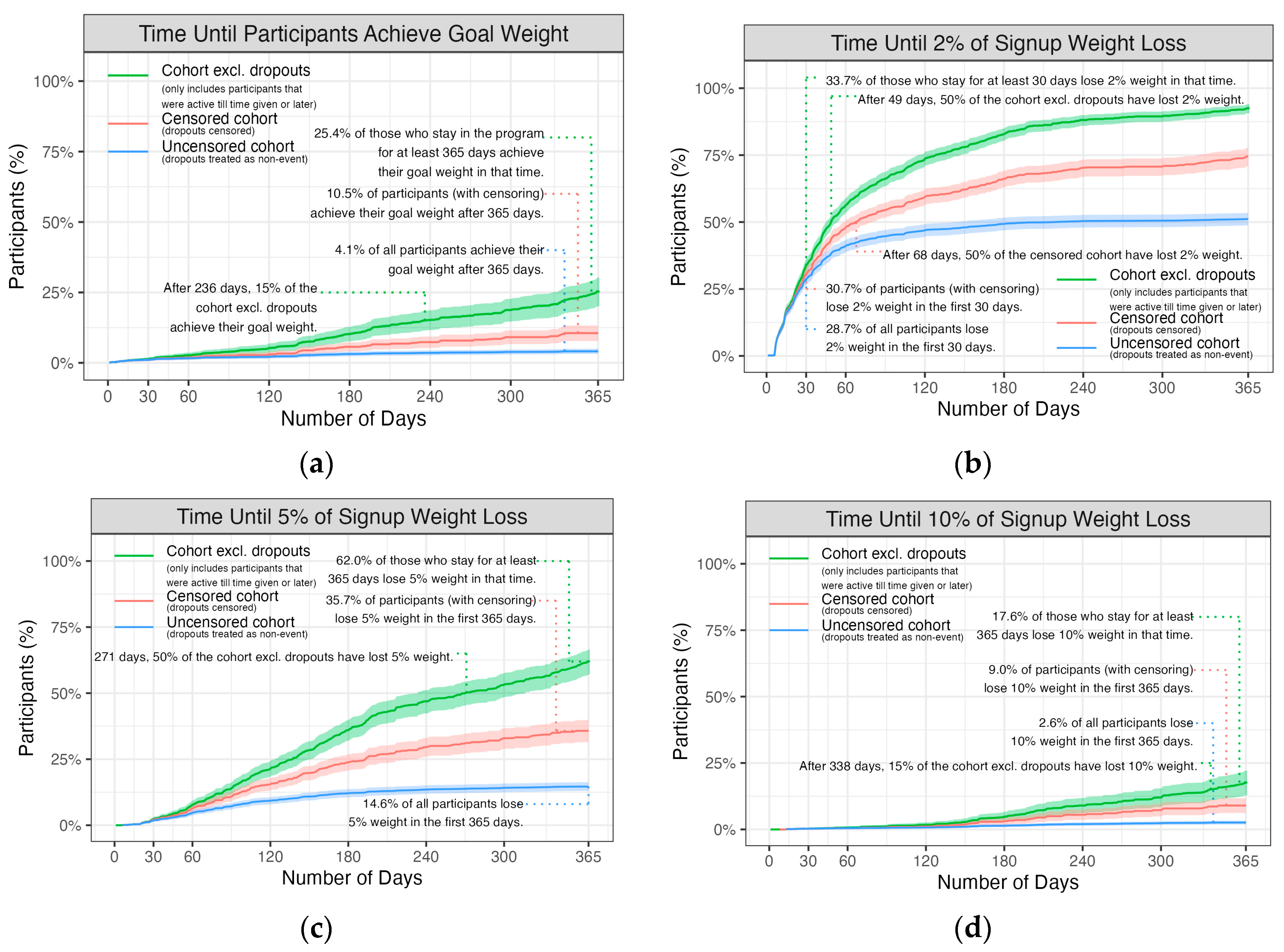
- Describe the success rates in terms of the proportion of subscribers who achieve their goal weight and the proportions losing 2%, 5%, and 10% of their starting weight;
- Identify the recorded attributes associated with greater weight loss;
- Describe the self-reported behavioural changes in response to the program.
2. Materials and Methods
2.1. The Interval Weight Loss Program
2.2. Data Collection
2.3. Statistical Methods
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in underweight and obesity from 1990 to 2022: A pooled analysis of 3663 population-representative studies with 222 million children, adolescents, and adults. Lancet 2024, 403, 1027–1050. [Google Scholar] [CrossRef] [PubMed]
- Beleigoli, A.M.; Andrade, A.Q.; Cancado, A.G.; Paulo, M.N.; Diniz, M.F.H.; Ribeiro, A.L. Web-Based Digital Health Interventions for Weight Loss and Lifestyle Habit Changes in Overweight and Obese Adults: Systematic Review and Meta-Analysis. J. Med. Internet Res. 2019, 21, e298. [Google Scholar] [CrossRef] [PubMed]
- Kupila, S.K.E.; Joki, A.; Suojanen, L.U.; Pietilainen, K.H. The Effectiveness of eHealth Interventions for Weight Loss and Weight Loss Maintenance in Adults with Overweight or Obesity: A Systematic Review of Systematic Reviews. Curr. Obes. Rep. 2023, 12, 371–394. [Google Scholar] [CrossRef]
- Islam, M.M.; Poly, T.N.; Walther, B.A.; Jack Li, Y.C. Use of Mobile Phone App Interventions to Promote Weight Loss: Meta-Analysis. JMIR Mhealth Uhealth 2020, 8, e17039. [Google Scholar] [CrossRef]
- Gonzales, K. Book Weight Loss Services in Australia—Market Research Report 2014–2029 ANZSIC 2006 9512; IBISWorld: Melbourne, Australia, 2024. [Google Scholar]
- Sumithran, P.; Prendergast, L.A.; Delbridge, E.; Purcell, K.; Shulkes, A.; Kriketos, A.; Proietto, J. Long-term persistence of hormonal adaptations to weight loss. N. Engl. J. Med. 2011, 365, 1597–1604. [Google Scholar] [CrossRef] [PubMed]
- Poon, E.T.; Tsang, J.H.; Sun, F.; Zheng, C.; Wong, S.H. Effects of intermittent dieting with break periods on body composition and metabolic adaptation: A systematic review and meta-analysis. Nutr. Rev. 2024, 83, 59–71. [Google Scholar] [CrossRef]
- Byrne, N.M.; Sainsbury, A.; King, N.A.; Hills, A.P.; Wood, R.E. Intermittent energy restriction improves weight loss efficiency in obese men: The MATADOR study. Int. J. Obes. 2018, 42, 129–138. [Google Scholar] [CrossRef]
- Batterham, M.; Tapsell, L.; Charlton, K.; O’Shea, J.; Thorne, R. Using data mining to predict success in a weight loss trial. J. Hum. Nutr. Diet. 2017, 30, 471–478. [Google Scholar] [CrossRef]
- Magkos, F.; Fraterrigo, G.; Yoshino, J.; Luecking, C.; Kirbach, K.; Kelly, S.C.; de las Fuentes, L.; He, S.; Okunade, A.L.; Patterson, B.W.; et al. Effects of Moderate and Subsequent Progressive Weight Loss on Metabolic Function and Adipose Tissue Biology in Humans with Obesity. Cell Metab. 2016, 23, 591–601. [Google Scholar] [CrossRef]
- Wing, R.R.; Phelan, S. Long-term weight loss maintenance. Am. J. Clin. Nutr. 2005, 82 (Suppl. S1), 222S–225S. [Google Scholar] [CrossRef]
- Hendrie, G.A.; Baird, D.L.; Brindal, E.; Williams, G.; Brand-Miller, J.; Muhlhausler, B. Weight Loss and Usage of an Online Commercial Weight Loss Program (the CSIRO Total Wellbeing Diet Online) Delivered in an Everyday Context: Five-Year Evaluation in a Community Cohort. J. Med. Internet Res. 2021, 23, e20981. [Google Scholar] [CrossRef]
- Ryan, D.H.; Yockey, S.R. Weight Loss and Improvement in Comorbidity: Differences at 5%, 10%, 15%, and Over. Curr. Obes. Rep. 2017, 6, 187–194. [Google Scholar] [CrossRef] [PubMed]
- Martin, A.; Fox, D.; Murphy, C.A.; Hofmann, H.; Koehler, K. Tissue losses and metabolic adaptations both contribute to the reduction in resting metabolic rate following weight loss. Int. J. Obes. 2022, 46, 1168–1175. [Google Scholar] [CrossRef] [PubMed]
- Sainsbury, A.; Wood, R.E.; Seimon, R.V.; Hills, A.P.; King, N.A.; Gibson, A.A.; Byrne, N.M. Rationale for novel intermittent dieting strategies to attenuate adaptive responses to energy restriction. Obes. Rev. 2018, 19 (Suppl. S1), 47–60. [Google Scholar] [CrossRef]
- De Cabo, R.; Mattson, M.P. Effects of Intermittent Fasting on Health, Aging, and Disease. N. Engl. J. Med. 2019, 381, 2541–2551. [Google Scholar] [CrossRef]
- Siles-Guerrero, V.; Romero-Márquez, J.M.; García-Pérez, R.N.; Novo-Rodríguez, C.; Guardia-Baena, J.M.; Hayón-Ponce, M.; Tenorio-Jiménez, C.; López-de-la-Torre-Casares, M.; Muñoz-Garach, A. Is Fasting Superior to Continuous Caloric Restriction for Weight Loss and Metabolic Outcomes in Obese Adults? A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Nutrients 2024, 16, 3533. [Google Scholar] [CrossRef]
- Sun, M.L.; Yao, W.; Wang, X.Y.; Gao, S.; Varady, K.A.; Forslund, S.K.; Zhang, M.; Shi, Z.Y.; Cao, F.; Zou, B.J.; et al. Intermittent fasting and health outcomes: An umbrella review of systematic reviews and meta-analyses of randomised controlled trials. EClinicalMedicine 2024, 70, 102519. [Google Scholar] [CrossRef]
- Pureza, I.; Macena, M.L.; da Silva Junior, A.E.; Praxedes, D.R.S.; Vasconcelos, L.G.L.; Bueno, N.B. Effect of early time-restricted feeding on the metabolic profile of adults with excess weight: A systematic review with meta-analysis. Clin. Nutr. 2021, 40, 1788–1799. [Google Scholar] [CrossRef]
- Gao, Y.; Tsintzas, K.; Macdonald, I.A.; Cordon, S.M.; Taylor, M.A. Effects of intermittent (5:2) or continuous energy restriction on basal and postprandial metabolism: A randomised study in normal-weight, young participants. Eur. J. Clin. Nutr. 2022, 76, 65–73. [Google Scholar] [CrossRef]
- Moro, T.; Tinsley, G.; Bianco, A.; Marcolin, G.; Pacelli, Q.F.; Battaglia, G.; Palma, A.; Gentil, P.; Neri, M.; Paoli, A. Effects of eight weeks of time-restricted feeding (16/8) on basal metabolism, maximal strength, body composition, inflammation, and cardiovascular risk factors in resistance-trained males. J. Transl. Med. 2016, 14, 290. [Google Scholar] [CrossRef]
- Klempel, M.C.; Bhutani, S.; Fitzgibbon, M.; Freels, S.; Varady, K.A. Dietary and physical activity adaptations to alternate day modified fasting: Implications for optimal weight loss. Nutr. J. 2010, 9, 35. [Google Scholar] [CrossRef]
- Heilbronn, L.K.; Smith, S.R.; Martin, C.K.; Anton, S.D.; Ravussin, E. Alternate-day fasting in nonobese subjects: Effects on body weight, body composition, and energy metabolism. Am. J. Clin. Nutr. 2005, 81, 69–73. [Google Scholar] [CrossRef]
- Harvey, J.; Howell, A.; Morris, J.; Harvie, M. Intermittent energy restriction for weight loss: Spontaneous reduction of energy intake on unrestricted days. Food Sci. Nutr. 2018, 6, 674–680. [Google Scholar] [CrossRef]
- McEvedy, S.M.; Sullivan-Mort, G.; McLean, S.A.; Pascoe, M.C.; Paxton, S.J. Ineffectiveness of commercial weight-loss programs for achieving modest but meaningful weight loss: Systematic review and meta-analysis. J. Health Psychol. 2017, 22, 1614–1627. [Google Scholar] [CrossRef]
- Batterham, M.; Tapsell, L.C.; Charlton, K.E. Baseline characteristics associated with different BMI trajectories in weight loss trials: A case for better targeting of interventions. Eur. J. Clin. Nutr. 2016, 70, 207–211. [Google Scholar] [CrossRef]
- Kompaniyets, L.; Freedman, D.S.; Belay, B.; Pierce, S.L.; Kraus, E.M.; Blanck, H.M.; Goodman, A.B. Probability of 5% or Greater Weight Loss or BMI Reduction to Healthy Weight Among Adults with Overweight or Obesity. JAMA Netw. Open 2023, 6, e2327358. [Google Scholar] [CrossRef]
- May, C.N.; Cox-Martin, M.; Ho, A.S.; McCallum, M.; Chan, C.; Blessing, K.; Behr, H.; Blanco, P.; Mitchell, E.S.; Michaelides, A. Weight loss maintenance after a digital commercial behavior change program (Noom Weight): Observational cross-sectional survey study. Obes. Sci. Pract. 2023, 9, 443–451. [Google Scholar] [CrossRef]
- Atallah, R.; Filion, K.B.; Wakil, S.M.; Genest, J.; Joseph, L.; Poirier, P.; Rinfret, S.; Schiffrin, E.L.; Eisenberg, M.J. Long-term effects of 4 popular diets on weight loss and cardiovascular risk factors: A systematic review of randomized controlled trials. Circ. Cardiovasc. Qual. Outcomes 2014, 7, 815–827. [Google Scholar] [CrossRef]
- Pagoto, S.; Xu, R.; Bullard, T.; Foster, G.D.; Bannor, R.; Arcangel, K.; DiVito, J.; Schroeder, M.; Cardel, M.I. An Evaluation of a Personalized Multicomponent Commercial Digital Weight Management Program: Single-Arm Behavioral Trial. J. Med. Internet Res. 2023, 25, e44955. [Google Scholar] [CrossRef]
- Batterham, M.; Tapsell, L.C.; Charlton, K.E. Predicting dropout in dietary weight loss trials using demographic and early weight change characteristics: Implications for trial design. Obes. Res. Clin. Pract. 2016, 10, 189–196. [Google Scholar] [CrossRef]
- Brown, J.D.; Buscemi, J.; Milsom, V.; Malcolm, R.; O’Neil, P.M. Effects on cardiovascular risk factors of weight losses limited to 5–10%. Transl. Behav. Med. 2015, 6, 339–346. [Google Scholar] [CrossRef]
- Dalle Grave, R.; Calugi, S.; Magri, F.; Cuzzolaro, M.; Dall’Aglio, E.; Lucchin, L.; Melchionda, N.; Marchesini, G.; Group, Q.S. Weight Loss Expectations in Obese Patients Seeking Treatment at Medical Centers. Obes. Res. 2004, 12, 2005–2012. [Google Scholar] [CrossRef]
- Fabricatore, A.N.; Wadden, T.A.; Rohay, J.M.; Pillitteri, J.L.; Shiffman, S.; Harkins, A.M.; Burton, S.L. Weight Loss Expectations and Goals in a Population Sample of Overweight and Obese US Adults. Obesity 2008, 16, 2445–2450. [Google Scholar] [CrossRef]
- Vosoughi, K.; Salman Roghani, R.; Camilleri, M. Effects of GLP-1 agonists on proportion of weight loss in obesity with or without diabetes: Systematic review and meta-analysis. Obes. Med. 2022, 35, 100456. [Google Scholar] [CrossRef]
- Gasoyan, H.; Pfoh, E.R.; Schulte, R.; Le, P.; Butsch, W.S.; Rothberg, M.B. One-Year Weight Reduction with Semaglutide or Liraglutide in Clinical Practice. JAMA Netw. Open 2024, 7, e2433326. [Google Scholar] [CrossRef]
- Pigsborg, K.; Kalea, A.Z.; De Dominicis, S.; Magkos, F. Behavioral and Psychological Factors Affecting Weight Loss Success. Curr. Obes. Rep. 2023, 12, 223–230. [Google Scholar] [CrossRef]
- Robertson, C.; Archibald, D.; Avenell, A.; Douglas, F.; Hoddinott, P.; van Teijlingen, E.; Boyers, D.; Stewart, F.; Boachie, C.; Fioratou, E.; et al. Systematic reviews of and integrated report on the quantitative, qualitative and economic evidence base for the management of obesity in men. Health Technol. Assess. 2014, 18. [Google Scholar] [CrossRef]
- Davy, S.R.; Benes, B.A.; Driskell, J.A. Sex differences in dieting trends, eating habits, and nutrition beliefs of a group of midwestern college students. J. Am. Diet. Assoc. 2006, 106, 1673–1677. [Google Scholar] [CrossRef]
- Benton, D.; Young, H.A. Reducing Calorie Intake May Not Help You Lose Body Weight. Perspect. Psychol. Sci. 2017, 12, 703–714. [Google Scholar] [CrossRef]
- Robinson, S.M.; Westbury, L.D.; Ward, K.; Syddall, H.; Cooper, R.; Cooper, C.; Sayer, A.A. Is lifestyle change around retirement associated with better physical performance in older age?: Insights from a longitudinal cohort. Eur. J. Ageing 2021, 18, 513–521. [Google Scholar] [CrossRef]
- Eglseer, D.; Traxler, M.; Embacher, S.; Reiter, L.; Schoufour, J.D.; Weijs, P.J.M.; Voortman, T.; Boirie, Y.; Cruz-Jentoft, A.; Bauer, S.; et al. Nutrition and Exercise Interventions to Improve Body Composition for Persons with Overweight or Obesity Near Retirement Age: A Systematic Review and Network Meta-Analysis of Randomized Controlled Trials. Adv. Nutr. 2023, 14, 516–538. [Google Scholar] [CrossRef] [PubMed]
- Brankovic, A.; Hendrie, G.A.; Baird, D.L.; Khanna, S. Predicting Disengagement to Better Support Outcomes in a Web-Based Weight Loss Program Using Machine Learning Models: Cross-Sectional Study. J. Med. Internet Res. 2023, 25, e43633. [Google Scholar] [CrossRef] [PubMed]
- Jakob, R.; Harperink, S.; Rudolf, A.M.; Fleisch, E.; Haug, S.; Mair, J.L.; Salamanca-Sanabria, A.; Kowatsch, T. Factors Influencing Adherence to mHealth Apps for Prevention or Management of Noncommunicable Diseases: Systematic Review. J. Med. Internet Res. 2022, 24, e35371. [Google Scholar] [CrossRef] [PubMed]
- Jakob, R.; Lepper, N.; Fleisch, E.; Kowatsch, T. Predicting early user churn in a public digital weight loss intervention. In Proceedings of the 2024 CHI Conference on Human Factors in Computing Systems, Honolulu, HI, USA, 11–16 May 2024. [Google Scholar]
- Ifejika, N.L.; Bhadane, M.; Cai, C.C.; Noser, E.A.; Grotta, J.C.; Savitz, S.I. Use of a Smartphone-Based Mobile App for Weight Management in Obese Minority Stroke Survivors: Pilot Randomized Controlled Trial with Open Blinded End Point. JMIR Mhealth Uhealth 2020, 8, e17816. [Google Scholar] [CrossRef]
- Bonn, S.E.; Trolle Lagerros, Y.; Balter, K. How valid are Web-based self-reports of weight? J. Med. Internet Res. 2013, 15, e52. [Google Scholar] [CrossRef]
| n Mean (CI) Median (IQR) | Subscription Length | Number of Days Active | Number of Weight Entries | Average Days Between Entries | Goal Weight (kg) | Weight (kg) on Signup | Weight (kg) on Final Entry | Change in Weight over Program | BMI on Signup | BMI on Final Entry | Change in BMI over Program |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | n = 1373 215 (203, 227) 127 (58, 333) | n = 1705 174 (163, 185) 85 (35, 193) | n = 1705 13 (12, 14) 7 (3, 16) | n = 1705 16 (15, 17) 9 (7, 14) | n = 1704 75.0 (74.3, 75.7) 72.9 (64.8, 82.0) | n = 1705 85.5 (84.7, 86.4) 83.0 (72.3, 95.2) | n = 1705 84.3 (83.5, 85.2) 82.0 (71.0, 94.0) | n = 1705 −1.2 (−1.4, −1.1) −1.0 (−2.2, 0.0) | n = 1578 30.9 (30.6, 31.2) 30.0 (26.7, 33.9) | n = 1578 30.4 (30.1, 30.7) 29.4 (26.4, 33.6) | n = 1578 −0.4 (−0.5, −0.4) −0.4 (−0.8, 0.0) |
| By Gender Female | n = 1192 218 (205, 231) 130 (59, 337) | n = 1463 178 (165, 190) 88 (35, 196) | n = 1463 13 (12, 14) 7 (3, 16) | n = 1463 17 (15, 18) 10 (7, 14) | n = 1462 72.5 (71.9, 73.1) 71.0 (63.9, 79.1) | n = 1463 83.1 (82.3, 84.0) 80.9 (71.1, 91.8) | n = 1463 82.0 (81.2, 82.9) 80.0 (70.0, 91.0) | n = 1463 −1.1 (−1.3, −1.0) −1.0 (−2.0, 0.0) | n = 1354 30.7 (30.4, 31.0) 29.8 (26.5, 33.6) | n = 1354 30.3 (30.0, 30.6) 29.2 (26.3, 33.5) | n = 1354 −0.4 (−0.5, −0.4) −0.4 (−0.8, 0.0) |
| Male | n = 181 198 (166, 230) 120 (56, 246) | n = 242 152 (124, 179) 74 (34, 182) | n = 242 13 (11, 16) 7 (3, 15) | n = 242 13 (11, 14) 9 (7, 14) | n = 242 90.1 (88.0, 92.2) 88.4 (79.2, 99.3) | n = 242 100.1 (97.6, 102.6) 98.8 (85.6, 113.7) | n = 242 98.2 (95.7, 100.8) 95.0 (84.0, 111.8) | n = 242 −1.8 (−2.3, −1.4) −1.8 (−3.0, 0.0) | n = 224 31.7 (30.9, 32.5) 31.3 (27.8, 35.1) | n = 224 31.1 (30.3, 31.9) 30.2 (27.0, 34.4) | n = 224 −0.6 (−0.8, −0.4) −0.5 (−1.1, 0.0) |
| By Age Group | |||||||||||
| Under 30 | n = 50 203 (124, 281) 94 (57, 181) | n = 56 182 (101, 264) 55 (29, 116) | n = 56 12 (6, 18) 5 (3, 10) | n = 56 20 (9, 31) 10 (7, 16) | n = 56 74.8 (71.0, 78.6) 74.0 (62.2, 83.9) | n = 56 82.8 (78.0, 87.6) 80.2 (70.0, 94.5) | n = 56 81.9 (77.2, 86.6) 82.0 (68.0, 93.0) | n = 56 −0.9 (−1.6, −0.2) −0.8 (−2.0, 0.4) | n = 53 29.1 (27.4, 30.7) 28.0 (25.2, 31.9) | n = 53 28.8 (27.2, 30.4) 28.1 (24.6, 31.6) | n = 53 −0.3 (−0.6, −0.0) −0.2 (−0.7, 0.3) |
| 30s | n = 209 209 (180, 237) 131 (62, 322) | n = 251 168 (139, 197) 81 (36, 181) | n = 251 12 (10, 14) 7 (4, 13) | n = 251 16 (14, 18) 10 (8, 16) | n = 251 77.8 (75.8, 79.9) 74.8 (66.5, 87.2) | n = 251 88.0 (85.5, 90.5) 84.0 (74.5, 98.6) | n = 251 87.2 (84.7, 89.7) 83.0 (73.0, 98.0) | n = 251 −0.8 (−1.2, −0.4) −0.8 (−2.0, 0.8) | n = 234 30.9 (30.1, 31.6) 29.8 (26.6, 34.1) | n = 234 30.6 (29.8, 31.3) 29.3 (26.2, 34.5) | n = 234 −0.3 (−0.4, −0.1) −0.3 (−0.7, 0.3) |
| 40s | n = 379 220 (200, 241) 152 (70, 348) | n = 452 171 (151, 191) 92 (35, 200) | n = 452 13 (11, 15) 7 (4, 15) | n = 452 17 (15, 20) 10 (7, 15) | n = 451 75.3 (74.0, 76.7) 73.0 (65.5, 82.0) | n = 452 86.0 (84.4, 87.7) 84.0 (73.0, 96.0) | n = 452 85.2 (83.5, 86.8) 82.0 (72.0, 95.0) | n = 452 −0.9 (−1.2, −0.6) −1.0 (−2.0, 0.0) | n = 425 31.0 (30.4, 31.5) 30.3 (26.6, 33.9) | n = 425 30.6 (30.1, 31.2) 29.8 (26.5, 33.7) | n = 425 −0.3 (−0.4, −0.2) −0.3 (−0.8, 0.0) |
| 50s | n = 421 220 (197, 243) 120 (54, 332) | n = 524 169 (149, 190) 77 (32, 194) | n = 524 13 (11, 14) 6 (3, 14) | n = 524 17 (15, 20) 10 (7, 14) | n = 524 74.4 (73.3, 75.6) 72.7 (64.5, 82.2) | n = 524 85.5 (83.9, 87.0) 82.1 (71.5, 96.0) | n = 524 84.2 (82.6, 85.7) 82.0 (70.8, 94.0) | n = 524 −1.3 (−1.6, −1.1) −1.0 (−2.1, 0.0) | n = 486 31.0 (30.5, 31.5) 30.1 (26.7, 34.1) | n = 486 30.5 (30.0, 31.1) 29.4 (26.3, 33.7) | n = 486 −0.5 (−0.6, −0.4) −0.4 (−0.8, 0.0) |
| 60s | n = 270 208 (180, 236) 108 (52, 313) | n = 359 186 (158, 213) 88 (40, 194) | n = 359 15 (13, 17) 8 (4, 20) | n = 359 13 (11, 15) 9 (7, 12) | n = 359 73.0 (71.6, 74.4) 70.5 (64.0, 80.0) | n = 359 83.4 (81.6, 85.1) 81.0 (72.2, 91.0) | n = 359 81.6 (79.8, 83.3) 80.0 (71.0, 89.5) | n = 359 −1.8 (−2.1, −1.5) −1.3 (−3.0, −0.3) | n = 323 30.7 (30.1, 31.3) 29.8 (26.9, 33.4) | n = 323 30.0 (29.5, 30.6) 29.0 (26.4, 33.1) | n = 323 −0.6 (−0.8, −0.5) −0.5 (−1.1, −0.1) |
| 70+ | n = 44 214 (139, 289) 119 (54, 313) | n = 63 182 (128, 236) 108 (42, 207) | n = 63 15 (11, 18) 10 (5, 20) | n = 63 13 (10, 16) 8 (7, 13) | n = 63 77.5 (73.9, 81.1) 76.2 (69.1, 80.2) | n = 63 87.4 (83.4, 91.4) 86.5 (79.2, 94.5) | n = 63 85.8 (81.8, 89.9) 86.0 (77.0, 92.5) | n = 63 −1.6 (−2.2, −1.0) −1.0 (−2.4, 0.0) | n = 57 31.8 (30.5, 33.0) 31.8 (28.5, 35.1) | n = 57 31.3 (30.0, 32.5) 30.5 (28.1, 34.5) | n = 57 −0.5 (−0.8, −0.3) −0.4 (−0.8, 0.0) |
| BMI Healthy Weight | n = 151 211 (177, 246) 116 (56, 294) | n = 185 179 (143, 215) 84 (32, 183) | n = 185 13 (10, 15) 6 (3, 15) | n = 185 19 (14, 24) 10 (7, 15) | n = 185 60.6 (59.7, 61.6) 60.0 (56.0, 64.0) | n = 185 65.4 (64.4, 66.4) 65.0 (60.0, 69.2) | n = 185 64.6 (63.6, 65.7) 64.0 (59.0, 69.0) | n = 185 −0.8 (−1.2, −0.4) −1.0 (−2.0, 0.0) | n = 185 23.5 (23.4, 23.7) 23.7 (23.0, 24.5) | n = 185 23.2 (23.0, 23.5) 23.3 (22.3, 24.2) | n = 185 −0.3 (−0.4, −0.2) −0.3 (−0.7, 0.0) |
| Overweight | n = 479 202 (182, 221) 120 (56, 288) | n = 602 172 (152, 191) 86 (34, 192) | n = 602 14 (12, 15) 7 (4, 17) | n = 602 15 (13, 17) 9 (7, 13) | n = 602 68.8 (68.1, 69.4) 67.8 (62.8, 73.2) | n = 602 76.3 (75.6, 77.0) 75.4 (70.0, 81.3) | n = 602 75.2 (74.5, 75.9) 74.0 (69.0, 81.0) | n = 602 −1.1 (−1.3, −0.9) −1.0 (−2.0, 0.0) | n = 602 27.5 (27.4, 27.6) 27.6 (26.2, 28.8) | n = 602 27.1 (27.0, 27.2) 27.1 (25.9, 28.4) | n = 602 −0.4 (−0.5, −0.3) −0.4 (−0.8, 0.0) |
| Obese Class I | n = 367 216 (193, 239) 133 (54, 351) | n = 469 164 (144, 184) 88 (34, 196) | n = 469 13 (11, 14) 7 (3, 15) | n = 469 15 (14, 17) 10 (7, 14) | n = 469 78.2 (77.3, 79.0) 76.6 (71.6, 83.1) | n = 469 89.9 (89.0, 90.8) 89.0 (83.0, 95.9) | n = 469 88.4 (87.5, 89.4) 88.0 (81.0, 95.0) | n = 469 −1.4 (−1.7, −1.1) −1.0 (−2.6, 0.0) | n = 469 32.2 (32.1, 32.3) 32.1 (31.1, 33.3) | n = 469 31.7 (31.5, 31.9) 31.6 (30.4, 33.1) | n = 469 −0.5 (−0.6, −0.4) −0.4 (−0.9, 0.0) |
| Obese Class II | n = 171 224 (191, 258) 130 (68, 338) | n = 215 169 (142, 197) 78 (40, 206) | n = 215 14 (11, 16) 7 (3, 15) | n = 215 16 (13, 18) 10 (7, 16) | n = 214 87.3 (85.7, 88.9) 85.4 (79.5, 92.0) | n = 215 103.2 (101.7, 104.7) 101.0 (95.5, 109.2) | n = 215 101.9 (100.4, 103.4) 101.0 (94.0, 109.0) | n = 215 −1.3 (−1.7, −0.9) −1.0 (−2.5, 0.0) | n = 215 36.8 (36.6, 37.0) 36.6 (35.6, 37.7) | n = 215 36.3 (36.1, 36.6) 36.3 (35.2, 37.5) | n = 215 −0.5 (−0.6, −0.3) −0.4 (−0.9, 0.0) |
| Obese Class III | n = 87 244 (186, 302) 124 (58, 356) | n = 107 182 (137, 228) 75 (30, 258) | n = 107 12 (9, 15) 6 (3, 14) | n = 107 19 (14, 25) 10 (7, 17) | n = 107 101.0 (97.8, 104.2) 97.5 (89.2, 110.5) | n = 107 123.1 (119.6, 126.6) 121.2 (110.0, 130.6) | n = 107 121.4 (117.7, 125.1) 118.0 (109.0, 129.0) | n = 107 −1.7 (−2.5, −0.9) −1.0 (−3.0, 0.0) | n = 107 44.7 (43.7, 45.6) 43.2 (40.9, 47.0) | n = 107 44.0 (43.1, 45.0) 42.3 (40.5, 46.4) | n = 107 −0.6 (−0.9, −0.3) −0.4 (−1.2, 0.0) |
| Year 2019 | n = 40 545 (426, 664) 520 (263, 648) | n = 52 538 (415, 662) 374 (250, 693) | n = 52 35 (26, 44) 24 (11, 50) | n = 52 24 (15, 33) 15 (11, 23) | n = 51 74.9 (70.9, 78.9) 73.0 (65.0, 82.8) | n = 52 86.0 (80.9, 91.0) 84.7 (72.2, 97.8) | n = 52 85.1 (80.1, 90.1) 85.0 (72.8, 95.2) | n = 52 −0.8 (−2.3, 0.6) 0.0 (−2.1, 1.2) | n = 49 31.0 (29.4, 32.6) 31.6 (26.5, 35.6) | n = 49 30.8 (29.1, 32.5) 31.2 (25.9, 34.4) | n = 49 −0.2 (−0.7, 0.3) 0.0 (−0.8, 0.5) |
| 2020 | n = 630 213 (194, 232) 130 (62, 235) | n = 673 181 (161, 202) 75 (36, 174) | n = 673 14 (12, 16) 7 (4, 15) | n = 673 17 (14, 19) 9 (7, 14) | n = 673 74.5 (73.4, 75.7) 72.3 (63.8, 82.0) | n = 673 85.1 (83.7, 86.5) 82.2 (71.2, 95.0) | n = 673 84.1 (82.7, 85.5) 82.0 (70.0, 94.0) | n = 673 −1.0 (−1.2, −0.8) −1.0 (−2.0, 0.0) | n = 578 30.9 (30.4, 31.4) 30.0 (26.8, 33.7) | n = 578 30.6 (30.1, 31.0) 29.5 (26.5, 33.6) | n = 578 −0.4 (−0.4, −0.3) −0.3 (−0.8, 0.0) |
| 2021 | n = 260 277 (251, 303) 234 (92, 366) | n = 294 205 (178, 232) 109 (42, 301) | n = 294 14 (12, 16) 8 (4, 17) | n = 294 18 (15, 21) 11 (8, 16) | n = 294 75.2 (73.6, 76.7) 72.5 (66.1, 81.0) | n = 294 85.7 (83.6, 87.7) 82.8 (73.2, 94.2) | n = 294 84.4 (82.3, 86.4) 81.0 (72.0, 93.0) | n = 294 −1.3 (−1.7, −0.9) −1.0 (−3.0, 0.0) | n = 266 30.5 (29.8, 31.2) 29.5 (26.3, 33.3) | n = 266 30.1 (29.4, 30.8) 29.0 (26.0, 33.3) | n = 266 −0.5 (−0.6, −0.3) −0.4 (−1.0, 0.0) |
| 2022 | n = 157 280 (253, 308) 308 (117, 380) | n = 190 203 (175, 231) 133 (48, 342) | n = 190 14 (12, 16) 7 (3, 17) | n = 190 20 (17, 24) 12 (9, 21) | n = 190 75.1 (73.1, 77.2) 73.2 (65.0, 81.8) | n = 190 86.0 (83.3, 88.6) 82.0 (72.2, 98.8) | n = 190 84.3 (81.6, 87.0) 81.0 (71.2, 94.8) | n = 190 −1.7 (−2.1, −1.3) −1.0 (−3.0, 0.0) | n = 190 31.0 (30.1, 31.8) 29.7 (26.4, 35.4) | n = 190 30.4 (29.5, 31.2) 28.8 (25.8, 34.1) | n = 190 −0.6 (−0.8, −0.5) −0.4 (−1.1, 0.0) |
| 2023 | n = 228 95 (84, 107) 65 (31, 120) | n = 412 109 (101, 118) 86 (29, 171) | n = 412 11 (10, 11) 8 (3, 15) | n = 412 12 (11, 14) 8 (7, 12) | n = 412 75.9 (74.5, 77.2) 73.4 (66.1, 83.6) | n = 412 86.2 (84.6, 87.9) 83.9 (74.0, 96.0) | n = 412 84.9 (83.2, 86.6) 82.0 (72.0, 95.0) | n = 412 −1.3 (−1.6, −1.1) −1.0 (−2.3, 0.0) | n = 411 31.0 (30.5, 31.5) 30.1 (27.2, 33.9) | n = 411 30.5 (30.0, 31.1) 29.4 (26.9, 33.5) | n = 411 −0.5 (−0.6, −0.4) −0.4 (−0.9, 0.0) |
| 2024 | n = 58 31 (31, 32) 31 (31, 31) | n = 84 29 (26, 32) 26 (16, 42) | n = 84 4 (4, 4) 4 (2, 5) | n = 84 7 (7, 8) 7 (6, 8) | n = 84 73.5 (71.0, 76.1) 72.8 (64.8, 81.0) | n = 84 83.8 (80.6, 86.9) 82.0 (72.0, 94.2) | n = 84 82.5 (79.3, 85.7) 81.0 (72.0, 93.0) | n = 84 −1.3 (−1.5, −1.0) −1.1 (−2.0, −0.6) | n = 84 30.5 (29.5, 31.5) 30.2 (26.7, 33.2) | n = 84 30.0 (29.0, 31.0) 29.9 (26.6, 32.4) | n = 84 −0.5 (−0.6, −0.4) −0.4 (−0.7, −0.2) |
| Time in Program First 100 days | n = 848 116 (108, 125) 71 (41, 121) | n = 940 44 (42, 45) 39 (23, 62) | n = 940 5 (5, 5) 4 (3, 7) | n = 940 10 (9, 10) 8 (6, 10) | n = 940 75.4 (74.4, 76.3) 73.0 (64.8, 83.4) | n = 940 85.6 (84.5, 86.8) 83.0 (72.0, 96.0) | n = 940 84.7 (83.5, 85.9) 82.0 (71.0, 95.0) | n = 940 −0.9 (−1.1, −0.8) −1.0 (−2.0, 0.0) | n = 866 30.8 (30.5, 31.2) 30.0 (26.7, 33.7) | n = 866 30.5 (30.1, 30.9) 29.7 (26.4, 33.6) | n = 866 −0.3 (−0.4, −0.3) −0.4 (−0.7, 0.0) |
| 100–200 days | n = 250 213 (199, 226) 176 (142, 241) | n = 364 149 (146, 152) 148 (120, 174) | n = 364 13 (13, 14) 13 (8, 18) | n = 364 16 (15, 18) 10 (8, 16) | n = 364 74.5 (73.0, 75.9) 72.5 (64.7, 81.0) | n = 364 84.8 (83.1, 86.6) 82.3 (73.0, 93.4) | n = 364 83.4 (81.6, 85.1) 80.0 (72.0, 93.0) | n = 364 −1.5 (−1.8, −1.2) −1.5 (−3.0, 0.0) | n = 341 30.6 (30.0, 31.1) 29.8 (26.6, 33.9) | n = 341 30.1 (29.5, 30.6) 29.0 (26.2, 33.5) | n = 341 −0.5 (−0.6, −0.4) −0.5 (−1.1, 0.0) |
| 200 days–1 year | n = 141 361 (336, 386) 355 (269, 374) | n = 184 284 (276, 291) 292 (234, 336) | n = 184 21 (20, 23) 22 (13, 28) | n = 184 22 (18, 26) 13 (10, 21) | n = 184 75.6 (73.8, 77.5) 74.3 (67.3, 81.0) | n = 184 86.8 (84.3, 89.4) 84.0 (74.3, 94.4) | n = 184 85.0 (82.4, 87.5) 81.5 (73.0, 94.0) | n = 184 −1.9 (−2.5, −1.3) −1.3 (−4.3, 0.1) | n = 176 31.2 (30.4, 32.1) 30.1 (27.3, 33.7) | n = 176 30.5 (29.7, 31.4) 29.1 (26.7, 33.4) | n = 176 −0.7 (−0.9, −0.5) −0.5 (−1.5, 0.0) |
| Over a year | n = 134 693 (649, 738) 648 (480, 805) | n = 217 687 (646, 727) 581 (463, 804) | n = 217 43 (38, 47) 40 (17, 57) | n = 217 39 (31, 46) 16 (10, 36) | n = 216 73.8 (71.9, 75.8) 71.0 (62.8, 81.4) | n = 217 85.1 (82.5, 87.8) 81.0 (70.5, 97.0) | n = 217 83.7 (81.1, 86.4) 80.0 (70.0, 93.0) | n = 217 −1.4 (−2.1, −0.7) −1.0 (−3.9, 1.0) | n = 195 31.2 (30.3, 32.2) 30.2 (26.2, 34.8) | n = 195 30.7 (29.8, 31.7) 29.2 (26.2, 34.2) | n = 195 −0.5 (−0.8, −0.3) −0.4 (−1.4, 0.4) |
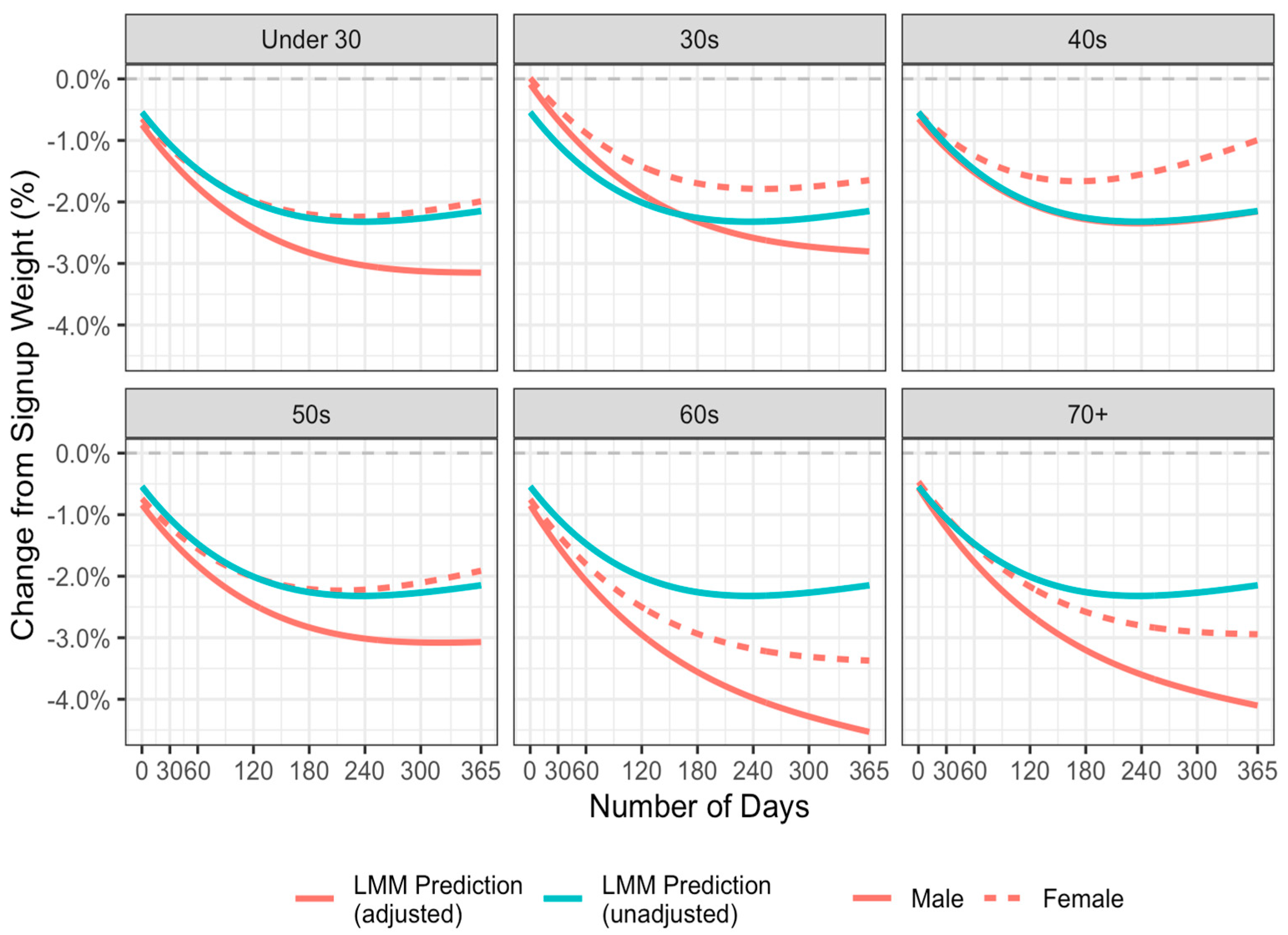
| Term | Estimate | Std. Error | df | t Value | p |
|---|---|---|---|---|---|
| Intercept | −1.604 | 0.320 | 2026 | −5.02 | <0.001 * |
| Time (in weeks) order = 1 | −10.139 | 11.718 | 22,304 | −0.87 | 0.387 |
| Time (in weeks) order = 2 | 47.049 | 2.604 | 22,369 | 18.07 | <0.001 * |
| Time (in weeks) order = 3 | −27.776 | 2.385 | 22,119 | −11.65 | <0.001 * |
| Time (in weeks) order = 4 | 49.248 | 2.330 | 22,005 | 21.14 | <0.001 * |
| Time (in weeks) order = 5 | −10.725 | 2.270 | 21,875 | −4.72 | <0.001 * |
| Male − Female | −0.099 | 0.174 | 1954 | −0.57 | 0.568 |
| 30s − Under 30 | 0.659 | 0.355 | 2034 | 1.85 | 0.064 |
| 40s − Under 30 | 0.097 | 0.340 | 2041 | 0.29 | 0.775 |
| 50s − Under 30 | −0.094 | 0.337 | 2047 | −0.28 | 0.781 |
| 60s − Under 30 | −0.104 | 0.344 | 2024 | −0.30 | 0.762 |
| 70+ − Under 30 | 0.181 | 0.445 | 1954 | 0.41 | 0.685 |
| Male × Time (in weeks) | −0.020 | 0.002 | 22,289 | −11.76 | <0.001 * |
| 30s × Time (in weeks) | −0.006 | 0.002 | 22,272 | −2.62 | 0.009 |
| 40s × Time (in weeks) | 0.017 | 0.002 | 22,282 | 7.65 | <0.001 * |
| 50s × Time (in weeks) | 0.003 | 0.002 | 22,381 | 1.49 | 0.136 |
| 60s × Time (in weeks) | −0.025 | 0.002 | 22,281 | −11.29 | <0.001 * |
| 70+ × Time (in weeks) | −0.022 | 0.004 | 22,408 | −6.09 | <0.001 * |
| Model | Predicted Weight Change (%, 95%CI) | |
| Unadjusted | −2.15 (−2.30, −2.00) | |
| Adjusted | ||
| Male | Under 30 | −3.15 (−3.85, −2.45) |
| Female | Under 30 | −1.99 (−2.63, −1.35) |
| Male | 30s | −2.80 (−3.25, −2.36) |
| Female | 30s | −1.65 (−1.99, −1.30) |
| Male | 40s | −2.15 (−2.57, −1.74) |
| Female | 40s | −0.99 (−1.25, −0.74) |
| Male | 50s | −3.07 (−3.47, −2.67) |
| Female | 50s | −1.91 (−2.15, −1.67) |
| Male | 60s | −4.53 (−4.95, −4.11) |
| Female | 60s | −3.37 (−3.65, −3.09) |
| Male | 70+ | −4.10 (−4.81, −3.39) |
| Female | 70+ | −2.94 (−3.59, −2.29) |
| Question | Response options | n(%) |
|---|---|---|
| What are the biggest changes you have made since starting on Interval Weight Loss? (multiple responses allowed) | Eating smaller dinner | 144 (70%) |
| Adopting a long-term weight loss strategy | 140 (68%) | |
| Eating bigger breakfast | 139 (68%) | |
| Eating more frequently | 122 (60%) | |
| Change in food choices | 111 (54%) | |
| Less comfort eating | 108 (53%) | |
| Eating more vegetables | 94 (46%) | |
| Eating less junk food | 93 (45%) | |
| Exercising more | 90 (44%) | |
| Getting more organized | 64 (31%) | |
| Reduced technology use | 54 (26%) | |
| Eating less takeaway | 54 (26%) | |
| Drinking less alcohol | 49 (24%) | |
| Sleeping more | 33 (16%) | |
| Cooking more | 33 (16%) | |
| Other | 12 (6%) | |
| What do you need to work on the most? (multiple responses allowed) | Exercising more | 107 (52%) |
| Eating smaller dinner | 91 (45%) | |
| Reducing technology use | 78 (38%) | |
| Changing my long-term weight loss strategy | 60 (29%) | |
| Sleeping more | 54 (26%) | |
| Less comfort eating | 50 (25%) | |
| Getting more organized | 44 (22%) | |
| Eating more frequently | 42 (21%) | |
| Eating more vegetables | 40 (20%) | |
| Drinking less alcohol | 36 (18%) | |
| Change in food choices | 32 (16%) | |
| Eating bigger breakfast | 28 (14%) | |
| Eating less junk food | 25 (12%) | |
| Cooking more | 17 (8%) | |
| Eating less takeaway | 9 (4%) | |
| Which change has been easiest to make? | Increasing consumption of nature’s treats | 56 (28%) |
| Change in meal size throughout the day | 54 (27%) | |
| Reducing processed food consumption | 47 (23%) | |
| Exercising | 15 (7%) | |
| Being more organized | 10 (5%) | |
| Change in evening time routine | 9 (4%) | |
| Other | 10 (5%) | |
| Which change has been hardest to make? | Change in meal size throughout the day | 67 (33%) |
| Change in evening time routine | 58 (28%) | |
| Exercising | 43 (21%) | |
| Reducing processed food consumption | 43 (21%) | |
| Being more organized | 9 (4%) | |
| Increasing consumption of nature’s treats | 8 (4%) | |
| Other | 10 (5%) | |
| How do you feel about your progress? (1 = I’m not progressing to 5 = I’m progressing very well) | 1 | 18 (9%) |
| 2 | 30 (15%) | |
| 3 | 90 (44%) | |
| 4 | 44 (21%) | |
| 5 | 23 (11%) |
| Mood | Response | Before IWL | During IWL | p Value |
|---|---|---|---|---|
| Balanced | ||||
| Yes | 14 (7%) | 58 (28%) | <0.001 | |
| No | 189 (93%) | 147 (72%) | ||
| Calm | ||||
| Yes | 10 (5%) | 42 (20%) | <0.001 | |
| No | 193 (95%) | 163 (80%) | ||
| Mostly Happy | ||||
| Yes | 89 (44%) | 137 (67%) | <0.001 | |
| No | 114 (56%) | 68 (33%) | ||
| Optimistic | ||||
| Yes | 29 (14%) | 90 (44%) | <0.001 | |
| No | 174 (86%) | 115 (56%) | ||
| Anxious | ||||
| Yes | 72 (35%) | 30 (15%) | <0.001 | |
| No | 131 (65%) | 175 (85%) | ||
| Busy | ||||
| Yes | 103 (51%) | 68 (33%) | <0.001 | |
| No | 100 (49% | 137 (67%) | ||
| Depressed | ||||
| Yes | 28 (14%) | 8 (4%) | <0.001 | |
| No | 175 (86%) | 197 (96%) | ||
| Mostly Unhappy | ||||
| Yes | 43 (17%) | 15 (7%) | <0.001 | |
| No | 169 (83%) | 190 (93%) | ||
| Stressed | ||||
| Yes | 107 (53%) | 37 (18%) | <0.001 | |
| No | 95 (47%) | 168 (82%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Batterham, M.; Wakefield, B. Evaluation of Intermittent Restricted Eating Using the Interval Weight Loss Online Platform in an Everyday Setting. Nutrients 2025, 17, 332. https://doi.org/10.3390/nu17020332
Batterham M, Wakefield B. Evaluation of Intermittent Restricted Eating Using the Interval Weight Loss Online Platform in an Everyday Setting. Nutrients. 2025; 17(2):332. https://doi.org/10.3390/nu17020332
Chicago/Turabian StyleBatterham, Marijka, and Bradley Wakefield. 2025. "Evaluation of Intermittent Restricted Eating Using the Interval Weight Loss Online Platform in an Everyday Setting" Nutrients 17, no. 2: 332. https://doi.org/10.3390/nu17020332
APA StyleBatterham, M., & Wakefield, B. (2025). Evaluation of Intermittent Restricted Eating Using the Interval Weight Loss Online Platform in an Everyday Setting. Nutrients, 17(2), 332. https://doi.org/10.3390/nu17020332





