Myths and Facts Regarding Low-Carbohydrate Diets
Abstract
1. Introduction
2. Materials and Methods
3. Concerns About Low-Carbohydrate Diets
3.1. Side-Effects
3.2. The Human Need for Carbohydrates
3.3. Heart Disease
3.4. Type 2 Diabetes
3.5. Other Disease Conditions
3.6. Other Dietary Approaches
3.7. Sustainability, Cost, and Nutritional Adequacy
3.8. Other Concerns
4. Discussion
5. Conclusions
- The low-carbohydrate (or ketogenic) diet is supported by a large body of clinical trial research demonstrating its safety and efficacy.
- Commonly held concerns, such as the idea that low-carbohydrate diets increase mortality or increases the risk of heart disease, are not supported by the evidence.
- There are no harmful side effects of low-carbohydrate diets.
- The “keto flu” that some patients experience at the start of the diet can be treated and avoided.
- Low-carbohydrate diets can be sustainable and nutritionally complete.
Author Contributions
Funding
Conflicts of Interest
References
- O’Hearn, M.; Lauren, B.N.; Wong, J.B.; Kim, D.D.; Mozaffarian, D. Trends and Disparities in Cardiometabolic Health Among U.S. Adults, 1999–2018. J. Am. Coll. Cardiol. 2022, 80, 138–151. [Google Scholar] [CrossRef] [PubMed]
- Goldenberg, J.Z.; Day, A.; Brinkworth, G.D.; Sato, J.; Yamada, S.; Jönsson, T.; Beardsley, J.; Johnson, J.A.; Thabane, L.; Johnston, B.C. Efficacy and Safety of Low and Very Low Carbohydrate Diets for Type 2 Diabetes Remission: Systematic Review and Meta-analysis of Published and Unpublished Randomized Trial Data. BMJ 2021, 372, m4743. [Google Scholar] [CrossRef] [PubMed]
- Kazeminasab, F.; Miraghajani, M.; Khalafi, M.; Sakhaei, M.H.; Rosenkranz, S.K.; Santos, H.O. Effects of Low-carbohydrate Diets, With and Without Caloric Restriction, on Inflammatory Markers in Adults: A Systematic Review and Meta-analysis of Randomized Clinical Trials. Eur. J. Clin. Nutr. 2024, 78, 569–584. [Google Scholar] [CrossRef] [PubMed]
- Volek, J.S.; Phinney, S.D.; Krauss, R.M.; Johnson, R.J.; Saslow, L.R.; Gower, B.; Yancy, W.S., Jr.; King, J.C.; Hecht, F.M.; Teicholz, N.; et al. Alternative Dietary Patterns for Americans: Low-Carbohydrate Diets. Nutrients 2021, 13, 3299. [Google Scholar] [CrossRef]
- Davies, M.J.; D’Alessio, D.A.; Fradkin, J.; Kernan, W.N.; Mathieu, C.; Mingrone, G.; Rossing, P.; Tsapas, A.; Wexler, D.J.; Buse, J.B. Management of Hyperglycemia in Type 2 Diabetes, 2018. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2018, 41, 2669–2701. [Google Scholar] [CrossRef]
- Diabetes Canada Position Statement on Low-Carbohydrate Diets for Adults With Diabetes: A Rapid Review. Can. J. Diabetes 2020, 44, 295–299. [CrossRef]
- Stranks, S.N.; Lawlor-Smith, N. Managing Type 2 Diabetes with Therapeutic Carbohydrate Reduction (TCR) [Internet]; Australian Diabetes Society: Sydney, Australia, 2022. Available online: https://www.diabetessociety.com.au/wp-content/uploads/2023/11/Managing-Type-2-Diabetes-with-Therapeutic-Carbohydrate-reduction-TCR-November-2023_Final.pdf (accessed on 9 March 2025).
- Evert, A.B.; Dennison, M.; Gardner, C.D.; Garvey, W.T.; Lau, K.H.K.; MacLeod, J.; Mitri, J.; Pereira, R.F.; Rawlings, K.; Robinson, S.; et al. Nutrition Therapy for Adults with Diabetes or Prediabetes: A Consensus Report. Diabetes Care 2019, 42, 731–754. [Google Scholar] [CrossRef]
- Alexander, L.; Christensen, S.M.; Richardson, L.; Ingersoll, A.B.; Burridge, K.; Golden, A.; Karjoo, S.; Cortez, D.; Shelver, M.; Bays, H.E. Nutrition and physical activity: An Obesity Medicine Association (OMA) Clinical Practice Statement 2022. Obes. Pillars 2022, 1, 100005. [Google Scholar] [CrossRef]
- Joseph, J.J.; Deedwania, P.; Acharya, T.; Aguilar, D.; Bhatt, D.L.; Chyun, D.A.; Di Palo, K.E.; Golden, S.H.; Sperling, L.S.; American Heart Association Diabetes Committee of the Council on Lifestyle and Cardiometabolic Health; et al. Comprehensive Management of Cardiovascular Risk Factors for Adults With Type 2 Diabetes: A Scientific Statement From the American Heart Association. Circulation 2022, 145, e722–e759. [Google Scholar] [CrossRef]
- Ludwig, D.S.; Aronne, L.J.; Astrup, A.; de Cabo, R.; Cantley, L.C.; Friedman, M.I.; Heymsfield, S.B.; Johnson, J.D.; King, J.C.; Krauss, R.M.; et al. The carbohydrate-insulin model: A physiological perspective on the obesity pandemic. Am. J. Clin. Nutr. 2021, 114, 1873–1885. [Google Scholar] [CrossRef]
- Gardner, C.D.; Vadiveloo, M.K.; Petersen, K.S.; Anderson, C.A.M.; Springfield, S.; Van Horn, L.; Khera, A.; Lamendola, C.; Mayo, S.M.; Joseph, J.J.; et al. Popular Dietary Patterns: Alignment with American Heart Association 2021 Dietary Guidance: A Scientific Statement from the American Heart Association. Circulation 2023, 147, 1715–1730. [Google Scholar] [CrossRef] [PubMed]
- Volek, J.S.; Phinney, S.D. The Art and Science of Low Carbohydrate Living; Beyond Obesity Publishing: Miami, FL, USA, 2011; p. 41. [Google Scholar]
- Harvey, C.J.D.C.; Schofield, G.M.; Williden, M. The use of nutritional supplements to induce ketosis and reduce symptoms associated with keto-induction: A narrative review. PeerJ 2018, 6, e4488. [Google Scholar] [CrossRef] [PubMed]
- Feinman, R.D.; Pogozelski, W.K.; Astrup, A.; Bernstein, R.K.; Fine, E.J.; Westman, E.C.; Accurso, A.; Frassetto, L.; Gower, B.A.; McFarlane, S.I.; et al. Dietary carbohydrate restriction as the first approach in diabetes management: Critical review and evidence base. Nutrition 2015, 31, 1–13, Erratum in Nutrition 2019, 62, 213. [Google Scholar] [CrossRef]
- Dehghan, M.; Mente, A.; Zhang, X.; Swaminathan, S.; Li, W.; Mohan, V.; Iqbal, R.; Kumar, R.; Wentzel-Viljoen, E.; Rosengren, A.; et al. Associations of fats and carbohydrate intake with cardiovascular disease and mortality in 18 countries from five continents (PURE): A prospective cohort study. Lancet 2017, 390, 2050–2062. [Google Scholar] [CrossRef]
- Volek, J.S.; Yancy, W.S., Jr.; Gower, B.A.; Phinney, S.D.; Slavin, J.; Koutnik, A.P.; Hurn, M.; Spinner, J.; Cucuzzella, M.; Hecht, F.M. Expert consensus on nutrition and lower-carbohydrate diets: An evidence- and equity-based approach to dietary guidance. Front. Nutr. 2024, 11, 1376098. [Google Scholar] [CrossRef]
- Ehrmann, D.; Kulzer, B.; Roos, T.; Haak, T.; Al-Khatib, M.; Hermanns, N. Risk factors and prevention strategies for diabetic ketoacidosis in people with established type 1 diabetes. Lancet Diabetes Endocrinol. 2020, 8, 436–446. [Google Scholar] [CrossRef]
- Thiruvenkatarajan, V.; Meyer, E.J.; Nanjappa, N.; Van Wijk, R.M.; Jesudason, D. Perioperative diabetic ketoacidosis associated with sodium-glucose co-transporter-2 inhibitors: A systematic review. Br. J. Anaesth. 2019, 123, 27–36. [Google Scholar] [CrossRef]
- Devlin, T. Textbook of Biochemistry with Clinical Correlations, 7th ed.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2010; pp. 699–700. [Google Scholar]
- Ludwig, D.S.; Hu, F.B.; Tappy, L.; Brand-Miller, J. Dietary carbohydrates: Role of quality and quantity in chronic disease. BMJ 2018, 361, k2340. [Google Scholar] [CrossRef]
- Chourpiliadis, C.; Mohiuddin, S.S. Biochemistry, Gluconeogenesis. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK544346/ (accessed on 28 September 2024).
- Food and Nutrition Board; Institute of Medicine; National Academies of Sciences. Dietary Reference Intakes for Energy, Carbohydrates, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids; National Academy Press: Washington, DC, USA, 2005. [Google Scholar]
- Forsythe, C.E.; Phinney, S.D.; Feinman, R.D.; Volk, B.M.; Freidenreich, D.; Quann, E.; Ballard, K.; Puglisi, M.J.; Maresh, C.M.; Kraemer, W.J.; et al. Limited effect of dietary saturated fat on plasma saturated fat in the context of a low carbohydrate diet. Lipids 2010, 45, 947–962. [Google Scholar] [CrossRef]
- Astrup, A.; Magkos, F.; Bier, D.M.; Brenna, J.T.; de Oliveira Otto, M.C.; Hill, J.O.; King, J.C.; Mente, A.; Ordovas, J.M.; Volek, J.S.; et al. Saturated Fats and Health: A Reassessment and Proposal for Food-Based Recommendations: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2020, 76, 844–857. [Google Scholar] [CrossRef]
- Astrup, A.; Teicholz, N.; Magkos, F.; Bier, D.M.; Brenna, J.T.; King, J.C.; Mente, A.; Ordovas, J.M.; Volek, J.S.; Yusuf, S.; et al. Dietary Saturated Fats and Health: Are the U.S. Guidelines Evidence-Based? Nutrients 2021, 13, 3305. [Google Scholar] [CrossRef] [PubMed]
- Virta Health. How to Eat Low Carb as a Vegan or Vegetarian [Internet]. Virta Health. February 2018. Available online: https://www.virtahealth.com/blog/vegan-vegetarian-low-carb-keto (accessed on 24 September 2024).
- Soto-Mota, A.; Flores-Jurado, Y.; Norwitz, N.G.; Feldman, D.; Pereira, M.A.; Danaei, G.; Ludwig, D.S. Increased low-density lipoprotein cholesterol on a low-carbohydrate diet in adults with normal but not high body weight: A meta-analysis. Am. J. Clin. Nutr. 2024, 119, 740–747. [Google Scholar] [CrossRef] [PubMed]
- Budoff, M.; Manubolu, V.S.; Kininger, A.; Norwitz, N.G.; Feldman, D.; Wood, T.R.; Fialkow, J.; Cury, R.; Feldman, T.; Nasir, K. Carbohydrate Restriction-Induced Elevations in LDL-Cholesterol and Atherosclerosis: The KETO Trial. JACC Adv. 2024, 3, 101–109. [Google Scholar] [CrossRef] [PubMed]
- Bhanpuri, N.H.; Hallberg, S.J.; Williams, P.T.; McKenzie, A.L.; Ballard, K.D.; Campbell, W.W.; McCarter, J.P.; Phinney, S.D.; Volek, J.S. Cardiovascular disease risk factor responses to a type 2 diabetes care model including nutritional ketosis induced by sustained carbohydrate restriction at 1 year: An open label, non-randomized, controlled study. Cardiovasc. Diabetol. 2018, 17, 56. [Google Scholar] [CrossRef]
- Norwitz, N.G.; Soto-Mota, A.; Kalayjian, T. A Company Is Only as Healthy as Its Workers: A 6-Month Metabolic Health Management Pilot Program Improves Employee Health and Contributes to Cost Savings. Metabolites 2022, 12, 848. [Google Scholar] [CrossRef]
- Zeraatkar, D.; Han, M.A.; Guyatt, G.H.; Vernooij, R.W.M.; El Dib, R.; Cheung, K.; Milio, K.; Zworth, M.; Bartoszko, J.J.; Valli, C.; et al. Red and Processed Meat Consumption and Risk for All-Cause Mortality and Cardiometabolic Outcomes: A Systematic Review and Meta-analysis of Cohort Studies. Ann. Intern. Med. 2019, 171, 703–710. [Google Scholar] [CrossRef]
- Han, M.A.; Zeraatkar, D.; Guyatt, G.H.; Vernooij, R.W.M.; El Dib, R.; Zhang, Y.; Algarni, A.; Leung, G.; Storman, D.; Valli, C.; et al. Reduction of Red and Processed Meat Intake and Cancer Mortality and Incidence: A Systematic Review and Meta-analysis of Cohort Studies. Ann. Intern. Med. 2019, 171, 711–720. [Google Scholar] [CrossRef]
- Vernooij, R.W.M.; Zeraatkar, D.; Han, M.A.; El Dib, R.; Zworth, M.; Milio, K.; Sit, D.; Lee, Y.; Gomaa, H.; Valli, C.; et al. Patterns of Red and Processed Meat Consumption and Risk for Cardiometabolic and Cancer Outcomes: A Systematic Review and Meta-analysis of Cohort Studies. Ann. Intern. Med. 2019, 171, 732–741. [Google Scholar] [CrossRef]
- Zeraatkar, D.; Johnston, B.C.; Bartoszko, J.; Cheung, K.; Bala, M.M.; Valli, C.; Rabassa, M.; Sit, D.; Milio, K.; Sadeghirad, B.; et al. Effect of Lower Versus Higher Red Meat Intake on Cardiometabolic and Cancer Outcomes: A Systematic Review of Randomized Trials. Ann. Intern. Med. 2019, 171, 721–731. [Google Scholar] [CrossRef]
- Riddle, M.C.; Cefalu, W.T.; Evans, P.H.; Gerstein, H.C.; Nauck, M.A.; Oh, W.K.; Rothberg, A.E.; le Roux, C.W.; Rubino, F.; Schauer, P.; et al. Consensus Report: Definition and Interpretation of Remission in Type 2 Diabetes. Diabetes Care 2021, 44, 2438–2444. [Google Scholar] [CrossRef]
- McKenzie, A.L.; Hallberg, S.J.; Creighton, B.C.; Volk, B.M.; Link, T.M.; Abner, M.K.; Glon, R.M.; McCarter, J.P.; Volek, J.S.; Phinney, S.D. A Novel Intervention Including Individualized Nutritional Recommendations Reduces Hemoglobin A1c Level, Medication Use, and Weight in Type 2 Diabetes. JMIR Diabetes 2017, 2, e5. [Google Scholar] [CrossRef]
- Athinarayanan, S.J.; Adams, R.N.; Hallberg, S.J.; McKenzie, A.L.; Bhanpuri, N.H.; Campbell, W.W.; Volek, J.S.; Phinney, S.D.; McCarter, J.P. Long-Term Effects of a Novel Continuous Remote Care Intervention Including Nutritional Ketosis for the Management of Type 2 Diabetes: A 2-Year Non-randomized Clinical Trial. Front. Endocrinol. 2019, 10, 348. [Google Scholar] [CrossRef] [PubMed]
- Unwin, D.; Delon, C.; Unwin, J.; Tobin, S.; Taylor, R. What predicts drug-free type 2 diabetes remission? Insights from an 8-year general practice service evaluation of a lower carbohydrate diet with weight loss. BMJ Nutr. Prev. Health 2023, 6, 46–55. [Google Scholar] [CrossRef] [PubMed]
- Oh, R.C.; Murphy, K.C.; Jenks, C.M.; Lopez, K.B.; Patel, M.A.; Scotland, E.E.; Khanna, M. Low-Carbohydrate and Ketogenic Dietary Patterns for Type 2 Diabetes Management. Fed. Pract. 2024, 41, 6–15. [Google Scholar] [CrossRef]
- Kelly, T.; Unwin, D.; Finucane, F. Low-Carbohydrate Diets in the Management of Obesity and Type 2 Diabetes: A Review from Clinicians Using the Approach in Practice. Int. J. Environ. Res. Public Health 2020, 17, 2557. [Google Scholar] [CrossRef]
- Society of Metabolic Health Practitioners. Clinical Guidelines for Therapeutic Carbohydrate Restriction [Internet]. February 2022. Available online: https://thesmhp.org/wp-content/uploads/2023/02/Clinical-Guidelines-General-Intervention-v1.3.9-updated-web-link-1.pdf (accessed on 24 September 2024).
- Apovian, C.M.; Okemah, J.; O’Neil, P.M. Body Weight Considerations in the Management of Type 2 Diabetes. Adv. Ther. 2019, 36, 44–58. [Google Scholar] [CrossRef]
- Aldhaleei, W.A.; Abegaz, T.M.; Bhagavathula, A.S. Glucagon-like Peptide-1 Receptor Agonists Associated Gastrointestinal Adverse Events: A Cross-Sectional Analysis of the National Institutes of Health All of Us Cohort. Pharmaceuticals 2024, 17, 199. [Google Scholar] [CrossRef]
- Liss, D.T.; Cherupally, M.; O’Brien, M.J.; Kang, R.H.; Aikman, C.; Wallia, A.; Cooper, A.J.; Koep, E.; Parker, E.D.; Ackermann, R.T. Treatment modification after initiating second-line medication for type 2 diabetes. Am. J. Manag. Care 2023, 29, 661–668. [Google Scholar]
- Austin, G.L.; Thiny, M.T.; Westman, E.C.; Yancy, W.S., Jr.; Shaheen, N.J. A very low-carbohydrate diet improves gastroesophageal reflux and its symptoms. Dig. Dis. Sci. 2006, 51, 1307–1312. [Google Scholar] [CrossRef]
- Yancy, W.S., Jr.; Provenzale, D.; Westman, E.C. Improvement of gastroesophageal reflux disease after initiation of a low-carbohydrate diet: Five brief case reports. Altern. Ther. Health Med. 2001, 7, 120, 116–119. [Google Scholar]
- Pointer, S.D.; Rickstrew, J.; Slaughter, J.C.; Vaezi, M.F.; Silver, H.J. Dietary carbohydrate intake, insulin resistance and gastro-oesophageal reflux disease: A pilot study in European- and African-American obese women. Aliment. Pharmacol. Ther. 2016, 44, 976–988. [Google Scholar] [CrossRef] [PubMed]
- Ho, K.S.; Tan, C.Y.; Mohd Daud, M.A.; Seow-Choen, F. Stopping or reducing dietary fiber intake reduces constipation and its associated symptoms. World J. Gastroenterol. 2012, 18, 4593–4596. [Google Scholar] [CrossRef] [PubMed]
- Nybacka, S.; Törnblom, H.; Josefsson, A.; Hreinsson, J.P.; Böhn, L.; Frändemark, Å.; Weznaver, C.; Störsrud, S.; Simrén, M. A low FODMAP diet plus traditional dietary advice versus a low-carbohydrate diet versus pharmacological treatment in irritable bowel syndrome (CARIBS): A single-centre, single-blind, randomised controlled trial. Lancet Gastroenterol. Hepatol. 2024, 9, 507–520. [Google Scholar] [CrossRef] [PubMed]
- Devries, M.C.; Sithamparapillai, A.; Brimble, K.S.; Banfield, L.; Morton, R.W.; Phillips, S.M. Changes in Kidney Function Do Not Differ between Healthy Adults Consuming Higher- Compared with Lower- or Normal-Protein Diets: A Systematic Review and Meta-Analysis. J. Nutr. 2018, 148, 1760–1775. [Google Scholar] [CrossRef]
- Athinarayanan, S.J.; Roberts, C.G.P.; Vangala, C.; Shetty, G.K.; McKenzie, A.L.; Weimbs, T.; Volek, J.S. The case for a ketogenic diet in the management of kidney disease. BMJ Open Diabetes Res. Care 2024, 12, e004101. [Google Scholar] [CrossRef]
- Iacovides, S.; Maloney, S.K.; Bhana, S.; Angamia, Z.; Meiring, R.M. Could the Ketogenic Diet Induce a Shift in Thyroid Function and Support a Metabolic Advantage in Healthy Participants? A Pilot Randomized-controlled-crossover trial. PLoS ONE 2022, 17, e0269440. [Google Scholar] [CrossRef]
- Festi, D.; Colecchia, A.; Orsini, M.; Sangermano, A.; Sottili, S.; Simoni, P.; Mazzella, G.; Villanova, N.; Bazzoli, F.; Lapenna, D.; et al. Gallbladder motility and gallstone formation in obese patients following very low calorie diets. Use it (fat) to lose it (well). Int. J. Obes. Relat. Metab. Disord. 1998, 22, 592–600. [Google Scholar] [CrossRef]
- Stokes, C.S.; Gluud, L.L.; Casper, M.; Lammert, F. Ursodeoxycholic acid and diets higher in fat prevent gallbladder stones during weight loss: A meta-analysis of randomized controlled trials. Clin. Gastroenterol. Hepatol. 2014, 12, 1090–1100. [Google Scholar] [CrossRef]
- Marzio, L.; Capone, F.; Neri, M.; Mezzetti, A.; De Angelis, C.; Cuccurullo, F. Gallbladder kinetics in obese patients. Effect of a regular meal and low-calorie meal. Dig. Dis. Sci. 1988, 33, 4–9. [Google Scholar] [CrossRef]
- Newman, J.C.; Covarrubias, A.J.; Zhao, M.; Yu, X.; Gut, P.; Ng, C.P.; Huang, Y.; Haldar, S.; Verdin, E. Ketogenic Diet Reduces Midlife Mortality and Improves Memory in Aging Mice. Cell Metab. 2017, 26, 547–557.e8. [Google Scholar] [CrossRef]
- Roberts, M.N.; Wallace, M.A.; Tomilov, A.A.; Zhou, Z.; Marcotte, G.R.; Tran, D.; Perez, G.; Gutierrez-Casado, E.; Koike, S.; Knotts, T.A.; et al. A Ketogenic Diet Extends Longevity and Healthspan in Adult Mice. Cell Metab. 2017, 26, 539–546. [Google Scholar] [CrossRef] [PubMed]
- Ornish, D.; Scherwitz, L.W.; Billings, J.H.; Brown, S.E.; Gould, K.L.; Merritt, T.A.; Sparler, S.; Armstrong, W.T.; Ports, T.A.; Kirkeeide, R.L.; et al. Intensive lifestyle changes for reversal of coronary heart disease. JAMA 1998, 280, 2001–2007. [Google Scholar] [CrossRef] [PubMed]
- Niu, Y.; Cao, H.; Zhou, H.; Cao, J.; Wang, Z. Effects of a vegetarian diet combined with exercise on lipid profiles and blood pressure: A systematic review and meta-analysis. Crit. Rev. Food Sci. Nutr. 2024, 64, 2289–2303. [Google Scholar] [CrossRef] [PubMed]
- Termannsen, A.D.; Clemmensen, K.K.B.; Thomsen, J.M.; Nørgaard, O.; Díaz, L.J.; Torekov, S.S.; Quist, J.S.; Faerch, K. Effects of vegan diets on cardiometabolic health: A systematic review and meta-analysis of randomized controlled trials. Obes. Rev. 2022, 23, e13462. [Google Scholar] [CrossRef]
- Picasso, M.C.; Lo-Tayraco, J.A.; Ramos-Villanueva, J.M.; Pasupuleti, V.; Hernandez, A.V. Effect of vegetarian diets on the presentation of metabolic syndrome or its components: A systematic review and meta-analysis. Clin. Nutr. 2019, 38, 1117–1132. [Google Scholar] [CrossRef]
- Orlich, M.J.; Singh, P.N.; Sabaté, J.; Jaceldo-Siegl, K.; Fan, J.; Knutsen, S.; Beeson, W.L.; Fraser, G.E. Vegetarian dietary patterns and mortality in Adventist Health Study 2. JAMA Intern. Med. 2013, 173, 1230–1238. [Google Scholar] [CrossRef]
- Stamler, J.; Epstein, F.H. Coronary heart disease: Risk factors as guides to preventive action. Prev. Med. 1972, 1, 27–48. [Google Scholar] [CrossRef]
- Howard, B.V.; Manson, J.E.; Stefanick, M.L.; Beresford, S.A.; Frank, G.; Jones, B.; Rodabough, R.J.; Snetselaar, L.; Thomson, C.; Tinker, L.; et al. Low-fat dietary pattern and weight change over 7 years: The Women’s Health Initiative Dietary Modification Trial. JAMA 2006, 295, 39–49. [Google Scholar] [CrossRef]
- Knopp, R.H.; Walden, C.E.; Retzlaff, B.M.; McCann, B.S.; Dowdy, A.A.; Albers, J.J.; Gey, G.O.; Cooper, M.N. Long-term cholesterol-lowering effects of 4 fat-restricted diets in hypercholesterolemic and combined hyperlipidemic men. The Dietary Alternatives Study. JAMA 1997, 278, 1509–1515. [Google Scholar] [CrossRef]
- Bueno, N.B.; de Melo, I.S.; de Oliveira, S.L.; da Rocha Ataide, T. Very-low-carbohydrate ketogenic diet v. low-fat diet for long-term weight loss: A meta-analysis of randomised controlled trials. Br. J. Nutr. 2013, 110, 1178–1187. [Google Scholar] [CrossRef]
- Lei, L.; Huang, J.; Zhang, L.; Hong, Y.; Hui, S.; Yang, J. Effects of low-carbohydrate diets versus low-fat diets on metabolic risk factors in overweight and obese adults: A meta-analysis of randomized controlled trials. Front. Nutr. 2022, 9, 935234. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; He, T.; Hu, Y.; Gao, C. Low-Carbohydrate Diet is More Helpful for Weight Loss Than Low-Fat Diet in Adolescents with Overweight and Obesity: A Systematic Review and Meta-Analysis. Diabetes Metab. Syndr. Obes. 2024, 17, 2997–3007. [Google Scholar] [CrossRef] [PubMed]
- Achterberg, C.; Astrup, A.; Bier, D.M.; King, J.C.; Krauss, R.M.; Teicholz, N.; Volek, J.S. An analysis of the recent US dietary guidelines process in light of its federal mandate and a National Academies report. PNAS Nexus 2022, 1, pgac107. [Google Scholar] [CrossRef]
- Cucuzzella, M.; Tondt, J.; Dockter, N.E.; Saslow, L.; Wood, T.R. A low-carbohydrate survey: Evidence for Sustainable Metabolic Syndrome Reversal. J. Insul. Resist. 2017, 2, 1–25. [Google Scholar] [CrossRef]
- Ministry of Health. Eating and Activity Guidelines for New Zealand Adults; Updated 2020; Ministry of Health: Wellington, New Zealand, 2015.
- Zinn, C.; North, S.; Donovan, K.; Muir, C.; Henderson, G. Low-carbohydrate, healthy-fat eating: A cost comparison with national dietary guidelines. Nutr. Diet. 2020, 77, 283–291. [Google Scholar] [CrossRef]
- Teicholz, N. For Richer, For Poorer: Low-Carb Diets Work for All Incomes [Internet]. Medscape. July 2024. Available online: https://www.medscape.com/viewarticle/richer-poorer-low-carb-diets-work-all-incomes-2024a1000cw5?form=fpf (accessed on 25 September 2024).
- Cucuzzella, M.; Sullivan, K. Low-Carb for Any Budget: A Low-Carb Shopping and Recipe Starter [Internet]. February 2020. Updated April 2023. Available online: https://www.guidelinecentral.com/guideline/41586/patient-education/560599/#section-anchor-2652973 (accessed on 15 September 2024).
- Zinn, C.; Rush, A.; Johnson, R. Assessing the nutrient intake of a low-carbohydrate, high-fat (LCHF) diet: A hypothetical case study design. BMJ Open 2018, 8, e018846. [Google Scholar] [CrossRef]
- Banner, L.; Rice Bradley, B.H.; Clinthorne, J. Nutrient analysis of three low-carbohydrate diets differing in carbohydrate content. Front. Nutr. 2024, 11, 1449109. [Google Scholar] [CrossRef]
- Zinn, C.; Lenferna De La Motte, K.A.; Rush, A.; Johnson, R. Assessing the Nutrient Status of Low Carbohydrate, High-Fat (LCHF) Meal Plans in Children: A Hypothetical Case Study Design. Nutrients 2022, 14, 1598. [Google Scholar] [CrossRef]
- Harish, P.; Subramoniam, A.; Aleo, J.J. Glucose Inhibits Cellular Ascorbic Acid Uptake by Fibroblasts in Vitro. Cell Biol. Int. Rep. 1985, 9, 531–538. [Google Scholar]
- U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2020–2025, 9th ed.; U.S. Department of Agriculture and U.S. Department of Health and Human Services: Washington, DC, USA, 2020.
- Prairie, A.M.; King, A.E.; Cotrufo, M.F. Restoring particulate and mineral-associated organic carbon through regenerative agriculture. Proc. Natl. Acad. Sci. USA 2023, 120, e2217481120. [Google Scholar] [CrossRef]
- US Environmental Protection Agency. Greenhouse Gas Emissions. Sources of Greenhouse Gas Emissions. Total U.S. Greenhouse Gas Emissions by Economic Sector in 2022. [Internet]. July 2024. Available online: https://www.epa.gov/ghgemissions/sources-greenhouse-gas-emissions (accessed on 24 September 2024).
- McSwiney, F.T.; Wardrop, B.; Hyde, P.N.; Lafountain, R.A.; Volek, J.S.; Doyle, L. Keto-adaptation enhances exercise performance and body composition responses to training in endurance athletes. Metabolism 2018, 81, 25–34. [Google Scholar] [CrossRef] [PubMed]
- Kephart, W.C.; Pledge, C.D.; Roberson, P.A.; Mumford, P.W.; Romero, M.A.; Mobley, C.B.; Martin, J.S.; Young, K.C.; Lowery, R.P.; Wilson, J.M.; et al. The Three-Month Effects of a Ketogenic Diet on Body Composition, Blood Parameters, and Performance Metrics in CrossFit Trainees: A Pilot Study. Sports 2018, 6, 1. [Google Scholar] [CrossRef] [PubMed]
- Paoli, A.; Grimaldi, K.; D’Agostino, D.; Cenci, L.; Moro, T.; Bianco, A.; Palma, A. Ketogenic diet does not affect strength performance in elite artistic gymnasts. J. Int. Soc. Sports Nutr. 2012, 9, 34. [Google Scholar] [CrossRef] [PubMed]
- Miele, E.M.; Vitti, S.; Christoph, L.; O’Neill, E.C.; Matthews, T.D.; Wood, R.J. The Effects Of a Six-week Ketogenic Diet on the Performance of Short-duration, High-intensity Exercise: A Pilot Study. Med. Sci. Sports Exerc. 2018, 50, 792. [Google Scholar] [CrossRef]
- Cipryan, L.; Plews, D.J.; Ferretti, A.; Maffetone, P.B.; Laursen, P.B. Effects of a 4-Week Very Low-Carbohydrate Diet on High-Intensity Interval Training Responses. J. Sports Sci. Med. 2018, 17, 259–268. [Google Scholar]
- Volek, J.S.; LaFountain, R.A.; Dituro, P. Extended Ketogenic Diet and Physical Training Intervention in Military Personnel. Mil. Med. 2019, 184, 199–200. [Google Scholar] [CrossRef]
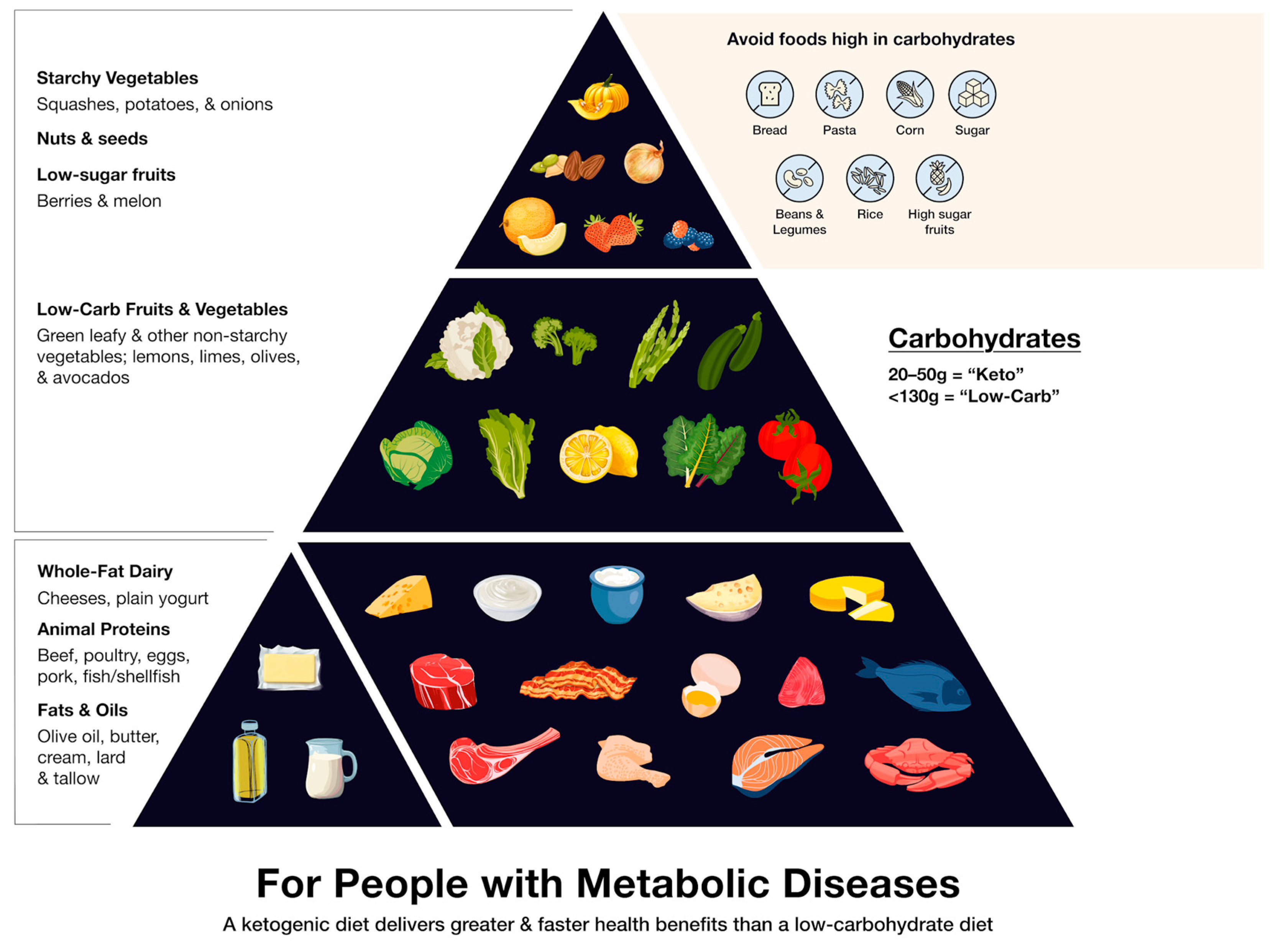
| Diet | Carbohydrates as % of Daily Calories | Grams of Carbohydrates Daily |
|---|---|---|
| Low-carbohydrate | 25% | 130 or less |
| Ketogenic (“keto”) | 10% | 20–50 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Teicholz, N.; Croft, S.M.; Cuaranta, I.; Cucuzzella, M.; Glandt, M.; Griauzde, D.H.; Jerome-Zapadka, K.; Kalayjian, T.; Murphy, K.; Nelson, M.; et al. Myths and Facts Regarding Low-Carbohydrate Diets. Nutrients 2025, 17, 1047. https://doi.org/10.3390/nu17061047
Teicholz N, Croft SM, Cuaranta I, Cucuzzella M, Glandt M, Griauzde DH, Jerome-Zapadka K, Kalayjian T, Murphy K, Nelson M, et al. Myths and Facts Regarding Low-Carbohydrate Diets. Nutrients. 2025; 17(6):1047. https://doi.org/10.3390/nu17061047
Chicago/Turabian StyleTeicholz, Nina, Steven M. Croft, Ignacio Cuaranta, Mark Cucuzzella, Mariela Glandt, Dina H. Griauzde, Karen Jerome-Zapadka, Tro Kalayjian, Kendrick Murphy, Mark Nelson, and et al. 2025. "Myths and Facts Regarding Low-Carbohydrate Diets" Nutrients 17, no. 6: 1047. https://doi.org/10.3390/nu17061047
APA StyleTeicholz, N., Croft, S. M., Cuaranta, I., Cucuzzella, M., Glandt, M., Griauzde, D. H., Jerome-Zapadka, K., Kalayjian, T., Murphy, K., Nelson, M., Shanahan, C., Nishida, J. L., Oh, R. C., Parrella, N., Saner, E. M., Sethi, S., Volek, J. S., Williden, M., & Wolver, S. (2025). Myths and Facts Regarding Low-Carbohydrate Diets. Nutrients, 17(6), 1047. https://doi.org/10.3390/nu17061047








