Ketogenic Diets for Body Weight Loss: A Comparison with Other Diets
Abstract
:1. Introduction
2. Methodology
3. Obesity and Overweight
3.1. Obesity and Overweight Statistics
3.2. Obesity and Overweight Classification
3.3. Obesity—A Disease or a Metabolic Disorder?
3.4. Causes of Obesity
3.5. Health Consequences of Overweight and Obesity
4. Ketogenic Diets as a Body Weight Loss Strategy
5. Areas Where the Ketogenic Diet May Be More Efficient for Weight Loss than Diets Richer in Carbohydrates
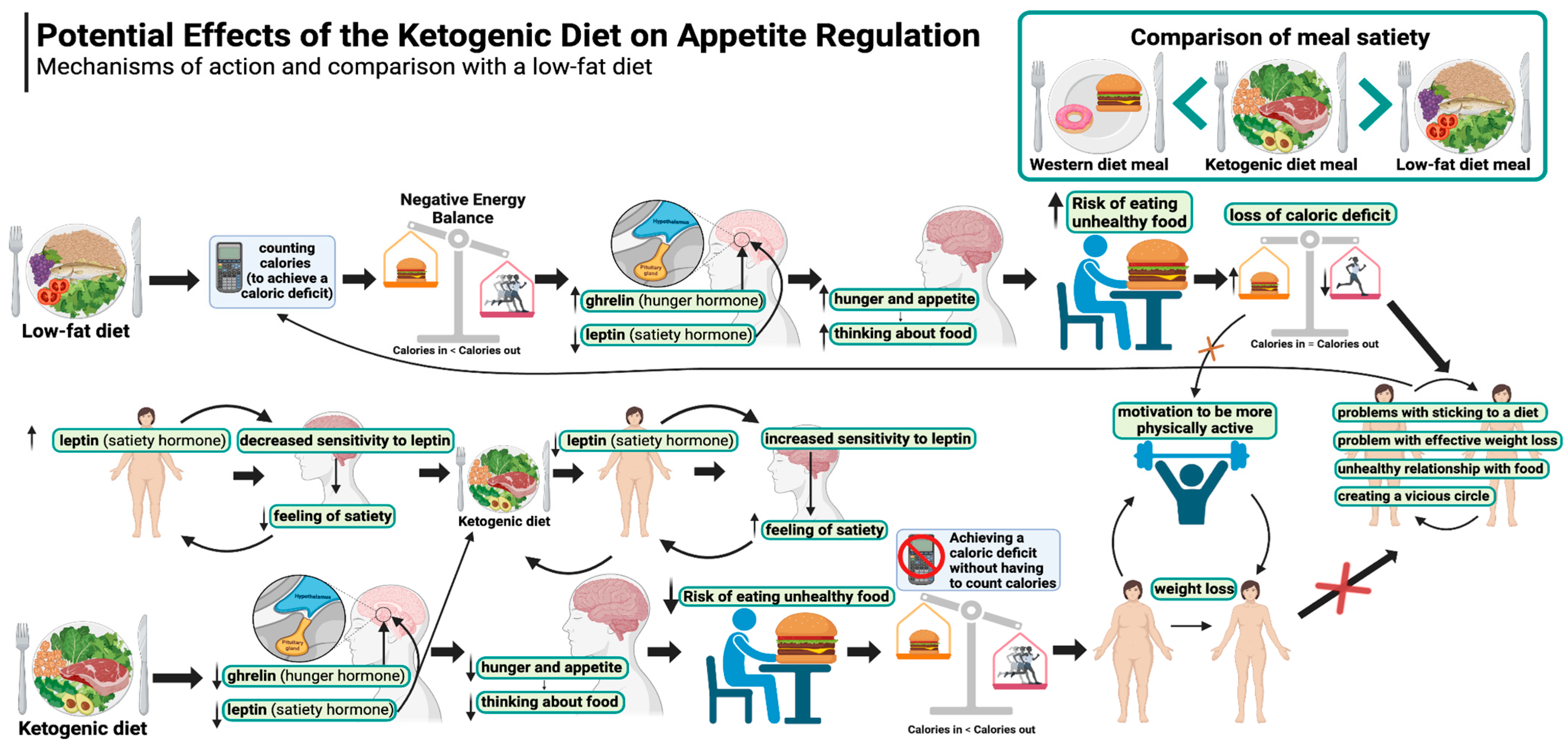
5.1. Appetite Regulation
5.1.1. Appetite and Hunger During Weight Loss in a Standard Approach
5.1.2. Appetite and Hunger During Weight Loss on a Ketogenic Diet
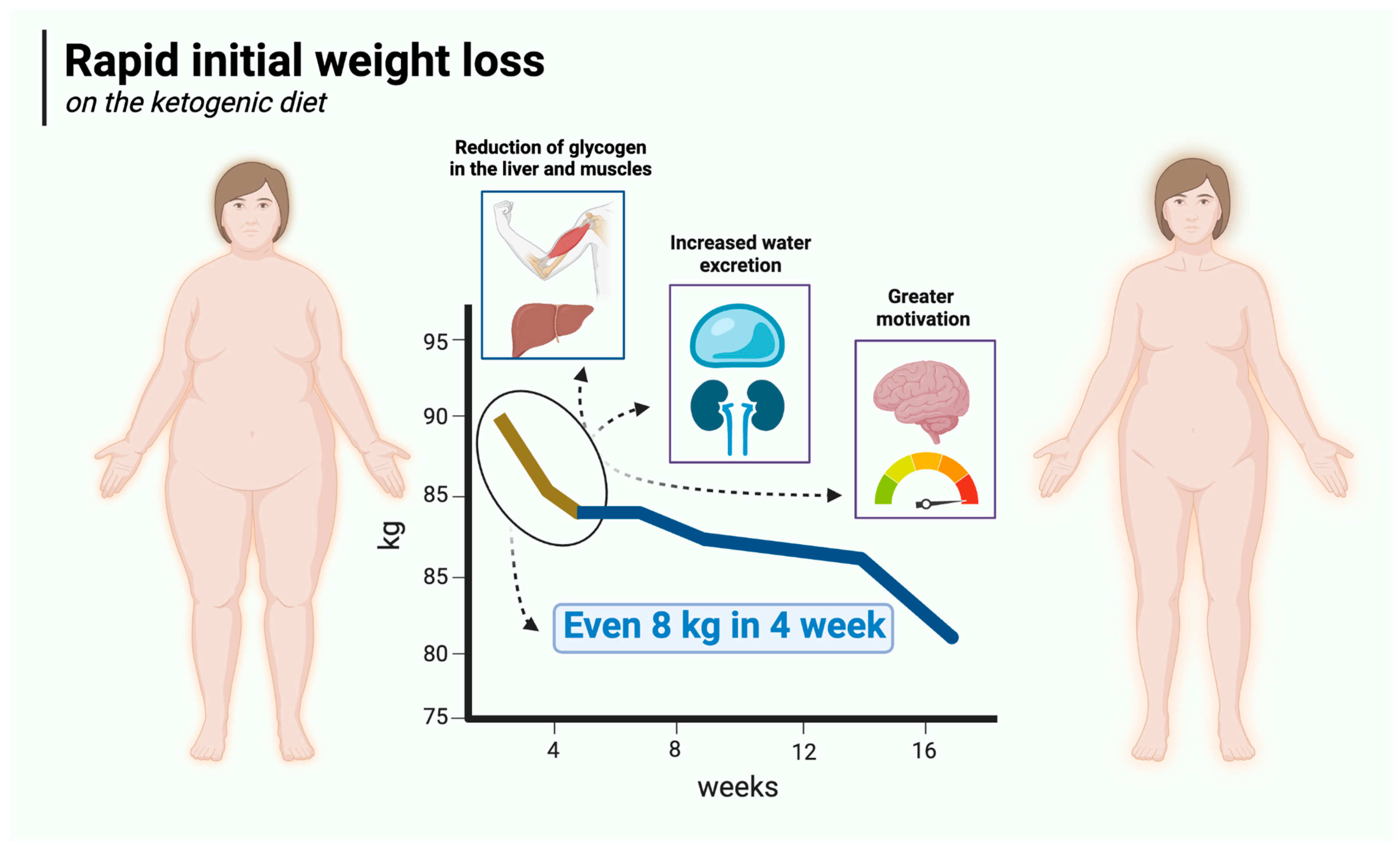
5.2. Rapid Initial Weight Loss
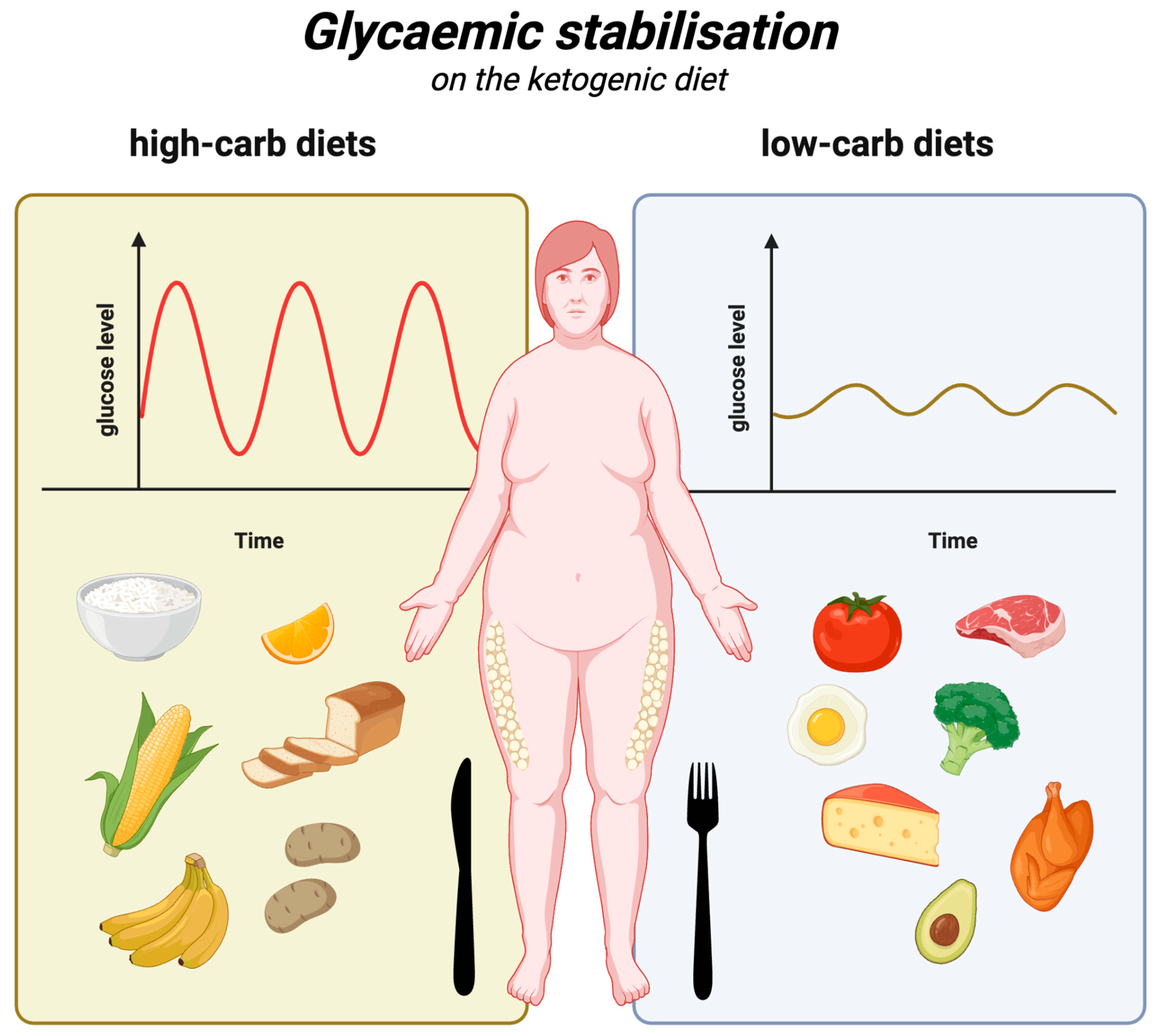
5.3. Glycaemic Stabilisation
5.4. Reducing Insulin Resistance
5.5. Reducing Inflammation
5.6. Reduced Need for Obesity Medication
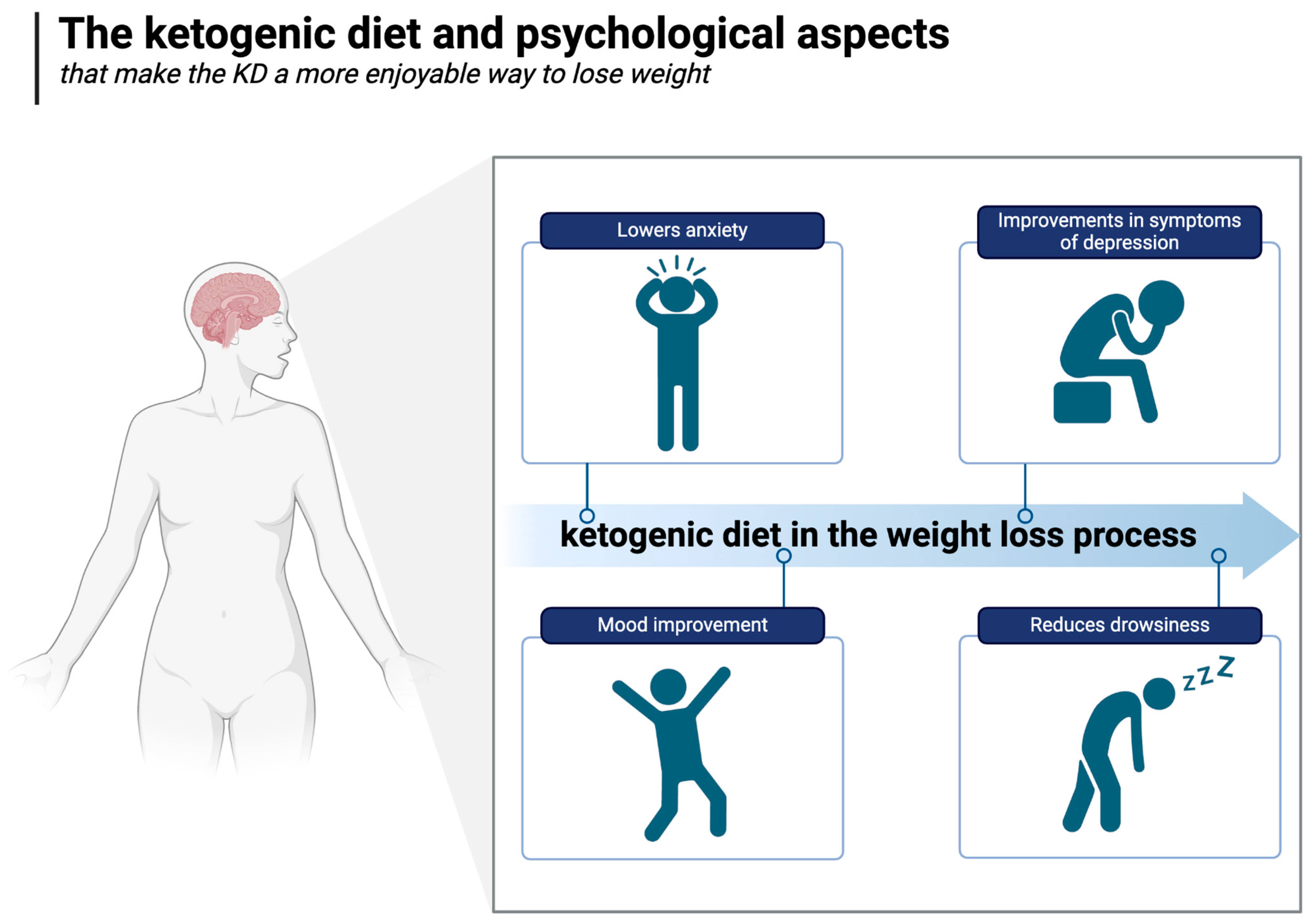
5.7. Psychological Advantages
5.8. The KD as a Potential Treatment for Substance Use Disorders and Food Addiction
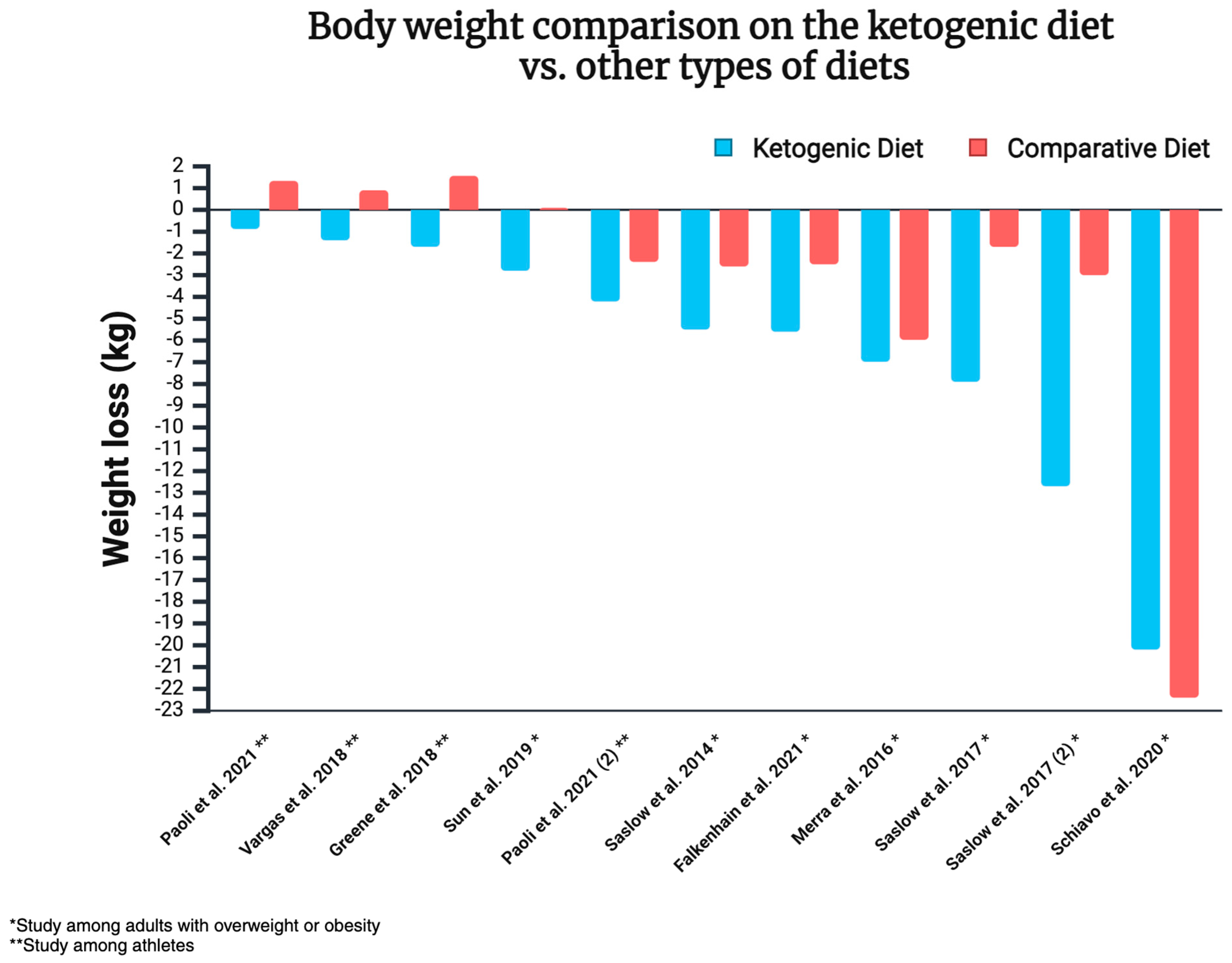
6. Ketogenic Diet and Weight Loss—Overview of Most Recent Studies
6.1. Ketogenic Diet and Weight Loss—Background and Results of Meta-Analyses
6.2. Ketogenic Diets and Weight Loss—Randomised Controlled Trials from the Last 10 Years
7. The Carnivore Diet as a Type of Ketogenic Diet
7.1. Current Research on the Carnivore Diet and Weight Loss
7.2. Potential Mechanisms Underlying Weight Reduction and Metabolic Efficiency
7.2.1. Lectins
7.2.2. Reduced Omega-6 Intake and Inflammation
7.2.3. Nutrient Density and Gut Health
7.3. Carnivore Diet and Weight Loss—Summary
8. Ketogenic Diet and Health
9. Contraindications and Side Effects of the Ketogenic Diet
10. Limitations
11. Summary
- A ketogenic diet offers an improved regulation of hunger and satiety. It is known that hunger and appetite increase on low-calorie diets, making the weight loss process much more difficult. Conversely, the ketogenic diet increases the feeling of satiety and mitigates the feeling of hunger, even despite a negative energy balance and weight loss, unlike in carbohydrate-based diets.
- Weight loss is greater during the initial phase of the ketogenic diet, as it reduces water retention and lowers glycogen levels in the body. In addition to the effect on total body weight, this may be important from the psychological perspective, as individuals who experience rapid weight loss will be more motivated to adhere to the diet.
- The spikes and diurnal fluctuations in glucose and insulin concentrations are smaller because KD meals do not raise glucose levels or insulin levels as much as carbohydrate-based meals (even in those with a low glycaemic index). In the absence of pronounced glucose fluctuations, bouts of hunger and overeating during the day are less likely, and overall daily glycaemia (as demonstrated by HbA1c levels) is improved. Lower glucose levels support lower insulin levels, the sensitisation of body cells to this hormone, and reduced insulin resistance, which often accompanies obesity and overweight and hinders weight loss.
- Ketogenic diets may help reduce inflammation associated with overweight and obesity to a greater extent than weight loss alone; thus, further research is needed in this area.
- The effect of the ketogenic diet (unlike carbohydrate-based diets) offers similar potential benefits to those of obesity medications but without the side effects. Thus, there is less need for these medications in subjects adhering to this diet. Obesity drugs reduce energy intake by increasing a sense of satiety, reducing appetite (by acting centrally or reducing glucose fluctuations), and/or inhibiting the digestion of fats. The ketogenic diet reduces the feeling of hunger (e.g., by affecting the hunger and satiety hormones), improves glycaemic control, and also lowers energy intake, even without intentional calorie restriction (which is more difficult to achieve with other dietary approaches).
- Weight loss on the KD can be more enjoyable (relative to low-fat diets), as it can simultaneously improve mood and cognitive function. The KD may even reduce symptoms of food addiction and binge eating. Many studies show that the beneficial (even therapeutic) psychological effects of ketogenic diets are superior to those of carbohydrate-based diets, exceeding those expected from weight loss alone (although there is a synergy between the two, as described in previous paragraphs).
- The best results are achieved by using a low-calorie ketogenic diet (and the calorie deficit itself can often be achieved intuitively).
12. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tiwari, A.; Balasundaram, P. Public Health Considerations Regarding Obesity. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar] [PubMed]
- Available online: https://www.who.int/activities/controlling-the-global-obesity-epidemic (accessed on 17 June 2024).
- Snetselaar, L.G.; de Jesus, J.M.; DeSilva, D.M.; Stoody, E.E. Dietary Guidelines for Americans, 2020-2025: Understanding the Scientific Process, Guidelines, and Key Recommendations. Nutr. Today 2021, 56, 287–295. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- United Nations Children’s Fund (UNICEF). Review of National Food-Based Dietary Guidelines and Associated Guidance for Infants, Children, Adolescents, and Pregnant and Lactating Women; UNICEF: New York, NY, USA, 2020. [Google Scholar]
- Available online: https://www.fao.org/nutrition/education/food-based-dietary-guidelines (accessed on 17 June 2024).
- Available online: https://nutritionsource.hsph.harvard.edu/healthy-weight/diet-reviews/ketogenic-diet/ (accessed on 18 June 2024).
- Wilson, J.; Lowery, R. The Ketogenic Bible; Victory Belt Publishing Inc.: Las Vegas, NV, USA, 2017; ISBN 13: 978-1-628601-04-6. [Google Scholar]
- Ashtary-Larky, D.; Bagheri, R.; Bavi, H.; Baker, J.S.; Moro, T.; Mancin, L.; Paoli, A. Ketogenic diets, physical activity and body composition: A review. Br. J. Nutr. 2022, 127, 1898–1920. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dyńka, D.; Kowalcze, K.; Paziewska, A. The Role of Ketogenic Diet in the Treatment of Neurological Diseases. Nutrients 2022, 14, 5003. [Google Scholar] [CrossRef] [PubMed]
- Puchalska, P.; Crawford, P.A. Multi-dimensional Roles of Ketone Bodies in Fuel Metabolism, Signaling, and Therapeutics. Cell Metab. 2017, 25, 262–284. [Google Scholar] [CrossRef]
- Paoli, A.; Bianco, A.; Moro, T.; Mota, J.F.; Coelho-Ravagnani, C.F. The Effects of Ketogenic Diet on Insulin Sensitivity and Weight Loss, Which Came First: The Chicken or the Egg? Nutrients 2023, 15, 3120. [Google Scholar] [CrossRef]
- Longo, R.; Peri, C.; Cricrì, D.; Coppi, L.; Caruso, D.; Mitro, N.; De Fabiani, E.; Crestani, M. Ketogenic Diet: A New Light Shining on Old but Gold Biochemistry. Nutrients 2019, 11, 2497. [Google Scholar] [CrossRef]
- Malinowska, D.; Żendzian-Piotrowska, M. Ketogenic diet: Areview of composition diversity, mechanism of action and clinical application. J. Nutr. Metab. Hindawi Publ. Corp. 2024, 2024, 6666171. [Google Scholar] [CrossRef]
- Williams, M.S.; Turos, E. The Chemistry of the Ketogenic Diet: Updates and Opportunities in Organic Synthesis. Int. J. Mol. Sci. 2021, 22, 5230. [Google Scholar] [CrossRef]
- Flier, J.S. Moderating “the great debate”: The carbohydrate-insulin vs. the energy balance models of obesity. Cell Metab. 2023, 35, 737–741. [Google Scholar] [CrossRef] [PubMed]
- Ludwig, D.S.; Aronne, L.J.; Astrup, A.; de Cabo, R.; Cantley, L.C.; Friedman, M.I.; Heymsfield, S.B.; Johnson, J.D.; King, J.C.; Krauss, R.M.; et al. The carbohydrate-insulin model: A physiological perspective on the obesity pandemic. Am. J. Clin. Nutr. 2021, 114, 1873–1885. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Available online: https://health.usnews.com/best-diet/best-diets-overall (accessed on 18 June 2024).
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in underweight and obesity from 1990 to 2022: A pooled analysis of 3663 population-representative studies with 222 million children, adolescents, and adults. Lancet 2024, 403, 1027–1050. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 2 January 2025).
- Available online: https://www.who.int/publications/i/item/WHO-NMH-NHD-17.3 (accessed on 2 January 2025).
- Astrup, A.; Bügel, S. Overfed but undernourished: Recognizing nutritional inadequacies/deficiencies in patients with overweight or obesity. Int. J. Obes. 2019, 43, 219–232. [Google Scholar] [CrossRef] [PubMed]
- Kobylińska, M.; Antosik, K.; Decyk, A.; Kurowska, K. Malnutrition in Obesity: Is It Possible? Obes. Facts 2022, 15, 19–25. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mahase, E. Global cost of overweight and obesity will hit $4.32tn a year by 2035, report warns. BMJ 2023, 380, 523. [Google Scholar] [CrossRef]
- Okunogbe, A.; Nugent, R.; Spencer, G.; Powis, J.; Ralston, J.; Wilding, J. Economic impacts of overweight and obesity: Current and future estimates for 161 countries. BMJ Glob. Health 2022, 7, e009773. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Weir, C.B.; Jan, A. BMI Classification Percentile and Cut off Points. [Updated 26 June 2023]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK541070/ (accessed on 2 January 2025).
- Purnell, J.Q. Definitions, Classification, and Epidemiology of Obesity. [Updated 4 May 2023]. In Endotext [Internet]; Feingold, K.R., Anawalt, B., Blackman, M.R., Boyce, A., Chrousos, G., Corpas, E., de Herder, W.W., Dhatariya, K., Dungan, K., Hofland, J., et al., Eds.; MDText.com, Inc.: South Dartmouth, MA, USA, 2000. Available online: https://www.ncbi.nlm.nih.gov/books/NBK279167/ (accessed on 2 January 2025).
- Wu, Y.; Li, D.; Vermund, S.H. Advantages and Limitations of the Body Mass Index (BMI) to Assess Adult Obesity. Int. J. Environ. Res. Public Health 2024, 21, 757. [Google Scholar] [CrossRef]
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Food and Nutrition Board; Roundtable on Obesity Solutions; Callahan, E.A. (Eds.) Translating Knowledge of Foundational Drivers of Obesity into Practice: Proceedings of a Workshop Series; National Academies Press (US): Washington, DC, USA, 31 July 2023; 10, The Science, Strengths, and Limitations of Body Mass Index. Available online: https://www.ncbi.nlm.nih.gov/books/NBK594362/ (accessed on 2 January 2025).
- Raheem, J.; Sliz, E.; Shin, J.; Holmes, M.V.; Pike, G.B.; Richer, L.; Gaudet, D.; Paus, T.; Pausova, Z. Visceral adiposity is associated with metabolic profiles predictive of type 2 diabetes and myocardial infarction. Commun. Med. 2022, 2, 81. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ross, R.; Neeland, I.J.; Yamashita, S.; Shai, I.; Seidell, J.; Magni, P.; Santos, R.D.; Arsenault, B.; Cuevas, A.; Hu, F.B.; et al. Waist circumference as a vital sign in clinical practice: A Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat. Rev. Endocrinol. 2020, 16, 177–189. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sweatt, K.; Garvey, W.T.; Martins, C. Strengths and Limitations of BMI in the Diagnosis of Obesity: What is the Path Forward? Curr. Obes. Rep. 2024, 13, 584–595. [Google Scholar] [CrossRef]
- Veghari, G.; Salehi, A.; Vaghari, M. The comparison of waist circumference, waist-to-hip ratio, and waist-to-height ratio among rural women adults in the North of Iran, between the years 2004 and 2013. ARYA Atheroscler. 2018, 14, 169–176. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Available online: https://www.cdc.gov/growthcharts/extended-bmi.htm (accessed on 26 June 2024).
- Available online: https://policysearch.ama-assn.org/policyfinder/detail/obesity?uri=%2FAMADoc%2FHOD.xml-0-3858.xml (accessed on 22 August 2024).
- Rosen, H. Is Obesity A Disease or A Behavior Abnormality? Did the AMA Get It Right? Mo. Med. 2014, 111, 104–108. [Google Scholar] [PubMed] [PubMed Central]
- Available online: https://ptlo.org.pl/dla_pacjenta/24-co_to_jest_otylosc (accessed on 22 August 2024).
- Burki, T. European Commission classifies obesity as a chronic disease. Lancet Diabetes Endocrinol. 2021, 9, 418. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.icd10data.com/ICD10CM/Codes/E00-E89/E65-E68/E66- (accessed on 22 August 2024).
- Luli, M.; Yeo, G.; Farrell, E.; Ogden, J.; Parretti, H.; Frew, E.; Bevan, S.; Brown, A.; Logue, J.; Menon, V.; et al. The implications of defining obesity as a disease: A report from the Association for the Study of Obesity 2021 annual conference. EClinicalMedicine 2023, 58, 101962. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Steele, M.; Finucane, F.M. Philosophically, is obesity really a disease? Obes. Rev. 2023, 24, e13590. [Google Scholar] [CrossRef] [PubMed]
- Padwal, R.S.; Pajewski, N.M.; Allison, D.B.; Sharma, A.M. Using theEdmonton obesity staging system to predict mortality in apopulation-representative cohort of people with overweight andobesity. Can. Med. Assoc. 2011, 183, E1059–E1066.3. [Google Scholar] [CrossRef]
- Amundson, D.E.; Djurkovic, S.; Matwiyoff, G.N. The obesity paradox. Crit. Care Clin. 2010, 26, 583–596. [Google Scholar] [CrossRef]
- Westbury, S.; Oyebode, O.; van Rens, T.; Barber, T.M. Obesity Stigma: Causes, Consequences, and Potential Solutions. Curr. Obes. Rep. 2023, 12, 10–23. [Google Scholar] [CrossRef]
- Levy, R.B.; Barata, M.F.; Leite, M.A.; Andrade, G.C. How and why ultra-processed foods harm human health. Proc. Nutr. Soc. 2024, 83, 1–8. [Google Scholar] [CrossRef] [PubMed]
- LaFata, E.M.; Allison, K.C.; Audrain-McGovern, J.; Forman, E.M. Ultra-Processed Food Addiction: A Research Update. Curr. Obes. Rep. 2024, 13, 214–223. [Google Scholar] [CrossRef]
- Swinburn, B.A.; Sacks, G.; Hall, K.D.; McPherson, K.; Finegood, D.T.; Moodie, M.L.; Gortmaker, S.L. The global obesity pandemic: Shaped by global drivers and local environments. Lancet 2011, 378, 804–814. [Google Scholar] [CrossRef]
- Noakes, T.D. So What Comes First: The Obesity or the Insulin Resistance? And Which Is More Important? Clin. Chem. 2018, 64, 7–9. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.who.int/news-room/questions-and-answers/item/obesity-health-consequences-of-being-overweight (accessed on 19 June 2024).
- Volpe, M.; Gallo, G. Obesity and cardiovascular disease: An executive document on pathophysiological and clinical links promoted by the Italian Society of Cardiovascular Prevention (SIPREC). Front. Cardiovasc. Med. 2023, 10, 1136340. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lopez-Jimenez, F.; Almahmeed, W.; Bays, H.; Cuevas, A.; Di Angelantonio, E.; le Roux, C.W.; Sattar, N.; Sun, M.C.; Wittert, G.; Pinto, F.J.; et al. Obesity and cardiovascular disease: Mechanistic insights and management strategies. A joint position paper by the World Heart Federation and World Obesity Federation. Eur. J. Prev. Cardiol. 2022, 29, 2218–2237. [Google Scholar] [CrossRef] [PubMed]
- Chandrasekaran, P.; Weiskirchen, R. The Role of Obesity in Type 2 Diabetes Mellitus—An Overview. Int. J. Mol. Sci. 2024, 25, 1882. [Google Scholar] [CrossRef]
- Brown, K.F.; Rumgay, H.; Dunlop, C.; Ryan, M.; Quartly, F.; Cox, A.; Deas, A.; Elliss-Brookes, L.; Gavin, A.; Hounsome, L.; et al. The fraction of cancer attributable to modifiable risk factors in England, Wales, Scotland, Northern Ireland, and the United Kingdom in 2015. Br. J. Cancer 2018, 118, 1130–1141. [Google Scholar] [CrossRef]
- Pati, S.; Irfan, W.; Jameel, A.; Ahmed, S.; Shahid, R.K. Obesity and Cancer: A Current Overview of Epidemiology, Pathogenesis, Outcomes, and Management. Cancers 2023, 15, 485. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Available online: https://www.cdc.gov/healthy-weight-growth/food-activity/overweight-obesity-impacts-health.html (accessed on 19 June 2024).
- Wójcik, K.; Łyszczarz, A.; Kolarzyk, E. Motywacja aktywnych fizycznie kobiet do podjęcia diety ketogenicznej oraz ocena ich sposobu żywieniai stanu odżywienia. Med. Og. Nauk. Zdr. 2021, 27, 466–472. [Google Scholar] [CrossRef]
- Butt, M.U.; Bawa, M.D.; Ahmed, H. Knowledge and perception about ketogenic diet among medical students. Biomedica 2020, 36, 126–131. [Google Scholar] [CrossRef]
- Alshaikh, N.A. Ketogenic diet: Knowledge, awareness, and perception among university students in Saudi Arabia. BioMedica 2022, 20, 64–69. [Google Scholar] [CrossRef]
- Fatima, W.; Alanazi, D.F.N.; Alanazi, N.B.; Zaidi, R.F.; Ansari, M.I. Knowledge and Perception Regarding Ketogenic Diet Among Students ofCollege of Nursing, Medicine and Applied Medical Sciences at NorthernBorder University, Arar, KSA. Curr. Nutr. Food Sci. 2023, 19, e270422204119. [Google Scholar] [CrossRef]
- Xing, N.N.; Ren, F.; Yang, H. Effects of ketogenic diet on weight loss parameters among obese or overweight patients with polycystic ovary syndrome: A systematic review and meta-analysis of randomized controlled trails. Food Nutr. Res. 2024, 68. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhou, C.; Wang, M.; Liang, J.; He, G.; Chen, N. Ketogenic Diet Benefits to Weight Loss, Glycemic Control, and Lipid Profiles in Overweight Patients with Type 2 Diabetes Mellitus: A Meta-Analysis of Randomized Controlled Trails. Int. J. Environ. Res. Public Health 2022, 19, 10429. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Muscogiuri, G.; El Ghoch, M.; Colao, A.; Hassapidou, M.; Yumuk, V.; Busetto, L. Obesity Management Task Force (OMTF) of the European Association for the Study of Obesity (EASO). European Guidelines for Obesity Management in Adults with a Very Low-Calorie Ketogenic Diet: A Systematic Review and Meta-Analysis. Obes. Facts 2021, 14, 222–245. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Finkler, E.; Heymsfield, S.B.; St-Onge, M.P. Rate of weight loss can be predicted by patient characteristics and intervention strategies. J. Acad. Nutr. Diet. 2012, 112, 75–80. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- ElSayed, N.A.; Aleppo, G.; Aroda, V.R.; Bannuru, R.R.; Brown, F.M.; Bruemmer, D.; Collins, B.S.; Hilliard, M.E.; Isaacs, D.; Johnson, E.L.; et al. 8. Obesity and Weight Management for the Prevention and Treatment of Type 2 Diabetes: Standards of Care in Diabetes—2023. Diabetes Care 2023, 46 (Supp. S1), S128–S139. [Google Scholar] [CrossRef]
- Available online: https://www.cdc.gov/healthy-weight-growth/physical-activity/index.html (accessed on 27 June 2024).
- DeBenedictis, J.N.; Nymo, S.; Ollestad, K.H.; Boyesen, G.A.; Rehfeld, J.F.; Holst, J.J.; Truby, H.; Kulseng, B.; Martins, C. Changes in the Homeostatic Appetite System After Weight Loss Reflect a Normalization Toward a Lower Body Weight. J. Clin. Endocrinol. Metab. 2020, 105, e2538–e2546. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nymo, S.; Coutinho, S.; Eknes, P.; Vestbostad, I.; Rehfeld, J.; Truby, H.; Kulseng, B.; Martins, C. Investigation of the long-term sustainability of changes in appetite after weight loss. Int. J. Obes. 2018, 42, 1489–1499. [Google Scholar] [CrossRef]
- Doucet, E.; Imbeault, P.; St-Pierre, S.; Alméras, N.; Mauriège, P.; Richard, D.; Tremblay, A. Appetite after weight loss by energy restriction and a low-fat diet-exercise follow-up. Int. J. Obes. Relat. Metab. Disord. 2000, 24, 906–914. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.healthline.com/nutrition/ways-reduce-hunger-appetite (accessed on 27 June 2024).
- Hopkins, M.; Blundell, J.E. Energy balance, body composition, sedentariness and appetite regulation: Pathways to obesity. Clin. Sci. 2016, 130, 1615–1628. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.virtahealth.com/blog/ketosis-appetite-hunger (accessed on 2 January 2025).
- Malhotra, A.; Noakes, T. Phinney SIt is time to bust the myth of physical inactivity and obesity: You cannot outrun a bad diet. Br. J. Sports Med. 2015, 49, 967–968. [Google Scholar] [CrossRef]
- Mansfeldt, J.M.; Magkos, F. Compensatory Responses to Exercise Training As Barriers to Weight Loss: Changes in Energy Intake and Non-exercise Physical Activity. Curr. Nutr. Rep. 2023, 12, 327–337. [Google Scholar] [CrossRef] [PubMed]
- Beaulieu, K.; Casanova, N.; Oustric, P.; Turicchi, J.; Gibbons, C.; Hopkins, M.; Varady, K.; Blundell, J.; Finlayson, G. Matched Weight Loss Through Intermittent or Continuous Energy Restriction Does Not Lead To Compensatory Increases in Appetite and Eating Behavior in a Randomized Controlled Trial in Women with Overweight and Obesity. J. Nutr. 2020, 150, 623–633. [Google Scholar] [CrossRef] [PubMed]
- Hadi, P. A review of global studies on emotional eating, hunger, and fast food addiction. Neuro Quantology 2023, 21, 2005–2013. [Google Scholar]
- Coutinho, S.R.; With, E.; Rehfeld, J.F.; Kulseng, B.; Truby, H.; Martins, C. The impact of rate of weight loss on body composition and compensatory mechanisms during weight reduction: A randomized control trial. Clin. Nutr. 2018, 37, 1154–1162. [Google Scholar] [CrossRef] [PubMed]
- Janssen, H.G.; Davies, I.G.; Richardson, L.D.; Stevenson, L. Determinants of takeaway and fast food consumption: A narrative review. Nutr. Res. Rev. 2018, 31, 16–34. [Google Scholar] [CrossRef] [PubMed]
- Butland, B.; Jebb, S.A.; Kopelman, P. Foresight Tackling Obesities: Future Choices Project; Foresight Programme of the Government Office for Science: London, UK, 2007. [Google Scholar]
- Fazzino, T.L.; Dorling, J.L.; Apolzan, J.W.; Martin, C.K. Meal composition during an ad libitum buffet meal and longitudinal predictions of weight and percent body fat change: The role of hyper-palatable, energy dense, and ultra-processed foods. Appetite 2021, 167, 105592. [Google Scholar] [CrossRef]
- Taneri, P.E.; Wehrli, F.; Roa-Díaz, Z.M.; Itodo, O.A.; Salvador, D.; Raeisi-Dehkordi, H.; Bally, L.; Minder, B.; Jong, J.C.K.-D.; Laine, J.E.; et al. Association between ultra-processed food intake and all-cause mortality: A systematic review and meta-analysis. Am. J. Epidemiol. 2022, 191, 1323–1335. [Google Scholar] [CrossRef]
- Hamano, S.; Sawada, M.; Aihara, M.; Sakurai, Y.; Sekine, R.; Usami, S.; Kubota, N.; Yamauchi, T. Ultra-processed foods cause weight gain and increased energy intake associated with reduced chewing frequency: A randomized, open-label, crossover study. Diabetes Obes. Metab. 2024, 26, 5431–5443. [Google Scholar] [CrossRef] [PubMed]
- Gibson, A.A.; Seimon, R.V.; Lee, C.M.; Ayre, J.; Franklin, J.; Markovic, T.P.; Caterson, I.D.; Sainsbury, A. Do ketogenic diets really suppress appetite? A systematic review and meta-analysis. Obes. Rev. 2015, 16, 64–76. [Google Scholar] [CrossRef] [PubMed]
- Roekenes, J.; Martins, C. Ketogenic diets and appetite regulation. Curr. Opin. Clin. Nutr. Metab. Care 2021, 24, 359–363. [Google Scholar] [CrossRef] [PubMed]
- Nymo, S.; Coutinho, S.R.; Jorgensen, J.; Rehfeld, J.F.; Truby, H.; Kulseng, B.; Martins, C. Timeline of changes in appetite during weight loss with a ketogenic diet. Int. J. Obes. 2017, 41, 1224–1231. [Google Scholar] [CrossRef] [PubMed]
- McKenzie, A.L.; Hallberg, S.J.; Creighton, B.C.; Volk, B.M.; Link, T.M.; Abner, M.K.; Glon, R.M.; McCarter, J.P.; Volek, J.S.; Phinney, S.D. A Novel Intervention Including Individualized Nutritional Recommendations Reduces Hemoglobin A1c Level, Medication Use, and Weight in Type 2 Diabetes. JMIR Diabetes 2017, 2, e5. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hallberg, S.J.; McKenzie, A.L.; Williams, P.T.; Bhanpuri, N.H.; Peters, A.L.; Campbell, W.W.; Hazbun, T.L.; Volk, B.M.; McCarter, J.P.; Phinney, S.D.; et al. Effectiveness and Safety of a Novel Care Model for the Management of Type 2 Diabetes at 1 Year: An Open-Label, Non-Randomized, Controlled Study. Diabetes Ther. 2018, 9, 583–612, Erratum in Diabetes Ther. 2018, 9, 613–621. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Martins, C.; Nymo, S.; Truby, H.; Rehfeld, J.F.; Hunter, G.R.; Gower, B.A. Association Between Ketosis and Changes in Appetite Markers with Weight Loss Following a Very Low-Energy Diet. Obesity 2020, 28, 2331–2338. [Google Scholar] [CrossRef] [PubMed]
- Graybeal, A.J.; Kreutzer, A.; Rack, P.; Moss, K.; Augsburger, G.; Willis, J.L.; Braun-Trocchio, R.; Shah, M. Perceptions of appetite do not match hormonal measures of appetite in trained competitive cyclists and triathletes following a ketogenic diet compared to a high-carbohydrate or habitual diet: A randomized crossover trial. Nutr. Res. 2021, 93, 111–123. [Google Scholar] [CrossRef] [PubMed]
- Castro, A.I.; Gomez-Arbelaez, D.; Crujeiras, A.B.; Granero, R.; Aguera, Z.; Jimenez-Murcia, S.; Sajoux, I.; Lopez-Jaramillo, P.; Fernandez-Aranda, F.; Casanueva, F.F. Effect of A Very Low-Calorie Ketogenic Diet on Food and Alcohol Cravings, Physical and Sexual Activity, Sleep Disturbances, and Quality of Life in Obese Patients. Nutrients 2018, 10, 1348. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lodi, A.; Zarantonello, L.; Bisiacchi, P.S.; Cenci, L.; Paoli, A. Ketonemia and Glycemia Affect Appetite Levels and Executive Functions in Overweight Females During Two Ketogenic Diets. Obesity 2020, 28, 1868–1877. [Google Scholar] [CrossRef] [PubMed]
- Sumithran, P.; Prendergast, L.A.; Delbridge, E.; Purcell, K.; Shulkes, A.; Kriketos, A.; Proietto, J. Ketosis and appetite-mediating nutrients and hormones after weight loss. Eur. J. Clin. Nutr. 2013, 67, 759–764. [Google Scholar] [CrossRef] [PubMed]
- Volek, J.S.; Phinney, S.D.; Forsythe, C.E.; Quann, E.E.; Wood, R.J.; Puglisi, M.J.; Kraemer, W.J.; Bibus, D.M.; Fernandez, M.L.; Feinman, R.D. Carbohydrate Restriction has a More Favorable Impact on the Metabolic Syndrome than a Low Fat Diet. Lipids 2009, 44, 297–309. [Google Scholar] [CrossRef]
- Dornbush, S.; Aeddula, N.R. Physiology, Leptin. [Updated 10 April 2023]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK537038/ (accessed on 2 January 2025).
- Gruzdeva, O.; Borodkina, D.; Uchasova, E.; Dyleva, Y.; Barbarash, O. Leptin resistance: Underlying mechanisms and diagnosis. Diabetes Metab. Syndr. Obes. 2019, 12, 191–198. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- de Git, K.C.G.; Adan, R.A.H. Leptin resistance in diet-induced obesity: The role of hypothalamic inflammation. Obes. Rev. 2015, 16, 207–224. [Google Scholar] [CrossRef] [PubMed]
- Khanna, D.; Khanna, S.; Khanna, P.; Kahar, P.; Patel, B.M. Obesity: A Chronic Low-Grade Inflammation and Its Markers. Cureus 2022, 14, e22711. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ji, J.; Fotros, D.; Sohouli, M.H.; Velu, P.; Fatahi, S.; Liu, Y. The effect of a ketogenic diet on inflammation-related markers: A systematic review and meta-analysis of randomized controlled trials. Nutr. Rev. 2024, 83, 40–58. [Google Scholar] [CrossRef] [PubMed]
- Lambadiari, V.; Katsimbri, P.; Kountouri, A.; Korakas, E.; Papathanasi, A.; Maratou, E.; Pavlidis, G.; Pliouta, L.; Ikonomidis, I.; Malisova, S.; et al. The Effect of a Ketogenic Diet versus Mediterranean Diet on Clinical and Biochemical Markers of Inflammation in Patients with Obesity and Psoriatic Arthritis: A Randomized Crossover Trial. Int. J. Mol. Sci. 2024, 25, 2475. [Google Scholar] [CrossRef]
- De Amicis, R.; Leone, A.; Lessa, C.; Foppiani, A.; Ravella, S.; Ravasenghi, S.; Trentani, C.; Ferraris, C.; Veggiotti, P.; De Giorgis, V.; et al. Long-Term Effects of a Classic Ketogenic Diet on Ghrelin and Leptin Concentration: A 12-Month Prospective Study in a Cohort of Italian Children and Adults with GLUT1-Deficiency Syndrome and Drug Resistant Epilepsy. Nutrients 2019, 11, 1716. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chyra, M.; Swietochowska, E.; Gorska-Flak, K.; Dudzinska, M.; Oswiecimska, J. The effect of the ketogenic diet on leptin, chemerin and resistin levels in children with epilepsy. Neuroendocrinol. Lett. 2021, 42, 489–499. [Google Scholar] [PubMed]
- Ackermans, M.A.; Jonker, N.C.; Bennik, E.C.; de Jong, P.J. Hunger increases negative and decreases positive emotions in women with a healthy weight. Appetite 2022, 168, 105746. [Google Scholar] [CrossRef]
- Reichenberger, J.; Schnepper, R.; Arend, A.K.; Blechert, J. Emotional eating in healthy individuals and patients with an eating disorder: Evidence from psychometric, experimental and naturalistic studies. Proc. Nutr. Soc. 2020, 79, 290–299. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ha, O.R.; Lim, S.L. The role of emotion in eating behavior and decisions. Front. Psychol. 2023, 14, 1265074. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pigsborg, K.; Kalea, A.Z.; De Dominicis, S.; Magkos, F. Behavioral and Psychological Factors Affecting Weight Loss Success. Curr. Obes. Rep. 2023, 12, 223–230. [Google Scholar] [CrossRef] [PubMed]
- Masood, W.; Annamaraju, P.; Khan Suheb, M.Z.; Uppaluri, K.R. Ketogenic Diet. [Updated 16 June 2023]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK499830/ (accessed on 2 January 2025).
- Oh, R.; Gilani, B.; Uppaluri, K.R. Low-Carbohydrate Diet. [Updated 17 August 2023]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK537084/ (accessed on 2 January 2025).
- Sumithran, P.; Proietto, J. Ketogenic dietsfor weight loss: A review of their principles, safety and efficacy. Obes. Res. Clin. Pract. 2008, 2, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Athinarayanan, S.J.; Roberts, C.G.P.; Vangala, C.; Shetty, G.K.; McKenzie, A.L.; Weimbs, T.; Volek, J.S. The case for a ketogenic diet in the management of kidney disease. BMJ Open Diabetes Res. Care 2024, 12, e004101. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dyńka, D.; Kowalcze, K.; Ambrozkiewicz, F.; Paziewska, A. Effect of the Ketogenic Diet on the Prophylaxis and Treatment of Diabetes Mellitus: A Review of the Meta-Analyses and Clinical Trials. Nutrients 2023, 15, 500. [Google Scholar] [CrossRef] [PubMed]
- Leonard, T. The physiology of ketosis and the ketogenic diet. S. Afr. J. Anaesth. Analg. 2020, 26, S94–S97. [Google Scholar] [CrossRef]
- Daghlas, S.A.; Mohiuddin, S.S. Biochemistry, Glycogen. [Updated 1 May 2023]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK539802/ (accessed on 2 January 2025).
- Roach, P.J.; Depaoli-Roach, A.A.; Hurley, T.D.; Tagliabracci, V.S. Glycogen and its metabolism: Some new developments and old themes. Biochem. J. 2012, 441, 763–787. [Google Scholar] [CrossRef]
- Jensen, J.; Rustad, P.I.; Kolnes, A.J.; Lai, Y.C. The role of skeletal muscle glycogen breakdown for regulation of insulin sensitivity by exercise. Front. Physiol. 2011, 2, 112. [Google Scholar] [CrossRef]
- Fernández-Elías, V.E.; Ortega, J.F.; Nelson, R.K.; Mora-Rodriguez, R. Relationship between muscle water and glycogen recovery after prolonged exercise in the heat in humans. Eur. J. Appl. Physiol. 2015, 115, 1919–1926. [Google Scholar] [CrossRef]
- McArdle, W.D.; Katch, F.I.; Katch, V.L. Special aids to exercise training and performance. In Exercise Physiology: Nutrition, Energy, and Human Performance; Lippincott Williams and Wilkins: Philadelphia, PA, USA, 2014; pp. 543–591. [Google Scholar]
- Olsson, B.Y.K.E.; Saltin, B. Variation in Total Body Water with Muscle Glycogen Changes in Man. Acta Physiol. Scand. 1970, 80, 11–18. [Google Scholar] [CrossRef]
- DeFronzo, R.A. The effect of insulin on renal sodium metabolism. A review with clinical implications. Diabetologia 1981, 21, 165–171. [Google Scholar] [CrossRef] [PubMed]
- Brands, M.W.; Manhiani, M.M. Sodium-retaining effect of insulin in diabetes. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2012, 303, R1101–R1109. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Unwin, D.J.; Tobin, S.D.; Murray, S.W.; Delon, C.; Brady, A.J. Substantial and Sustained Improvements in Blood Pressure, Weight and Lipid Profiles from a Carbohydrate Restricted Diet: An Observational Study of Insulin Resistant Patients in Primary Care. Int. J. Environ. Res. Public Health 2019, 16, 2680. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, F.W.; Majeed, M.S.; Kirresh, O. Non-Diabetic Hypoglycemia. [Updated 17 July 2023]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK573079/ (accessed on 2 January 2025).
- Schultes, B.; Oltmanns, K.M.; Kern, W.; Fehm, H.L.; Born, J.; Peters, A. Modulation of hunger by plasma glucose and metformin. J. Clin. Endocrinol. Metab. 2003, 88, 1133–1141. [Google Scholar] [CrossRef] [PubMed]
- Gielkens, H.A.; Verkijk, M.; Lam, W.F.; Lamers, C.B.; Masclee, A.A. Effects of hyperglycemia and hyperinsulinemia on satiety in humans. Metabolism 1998, 47, 321–324. [Google Scholar] [CrossRef] [PubMed]
- Schmid, S.M.; Jauch-Chara, K.; Hallschmid, M.; Oltmanns, K.M.; Born, J.; Schultes, B. Short-term nocturnal hypoglycaemia increases morning food intake in healthy humans. Diabet. Med. 2008, 25, 232–235. [Google Scholar] [CrossRef] [PubMed]
- Holesh, J.E.; Aslam, S.; Martin, A. Physiology, Carbohydrates. [Updated 12 May 2023]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK459280/ (accessed on 2 January 2025).
- Shin, Y.; Park, S.; Choue, R. Comparison of time course changes in blood glucose, insulin and lipids between high carbohydrate and high fat meals in healthy young women. Nutr. Res. Pract. 2009, 3, 128–133. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chabot, F.; Caron, A.; Laplante, M.; St-Pierre, D.H. Interrelationships between ghrelin, insulin and glucose homeostasis: Physiological relevance. World J. Diabetes 2014, 5, 328–341. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Insulin and hunger. JAMA 1932, 99, 1692. [CrossRef]
- Wyatt, P.; Berry, S.E.; Finlayson, G.; O’driscoll, R.; Hadjigeorgiou, G.; Drew, D.A.; Al Khatib, H.; Nguyen, L.H.; Linenberg, I.; Chan, A.T.; et al. Postprandial glycaemic dips predict appetite and energy intake in healthyindividuals. Nat. Metab. 2021, 3, 523–529. [Google Scholar] [CrossRef]
- Enyama, Y.; Takeshita, Y.; Tanaka, T.; Sako, S.; Kanamori, T.; Takamura, T. Distinct effects of carbohydrate ingestion timing on glucose fluctuation and energy metabolism in patients with type 2 diabetes: A randomized controlled study. Endocr. J. 2021, 68, 1225–1236. [Google Scholar] [CrossRef] [PubMed]
- Al-Sowayan, N.; Almeneay, B.; Al Othaim, T. Effect of Low and High Glycemic Index Meals on Hunger and Satiety. Adv. Biosci. Biotechnol. 2023, 14, 409–418. [Google Scholar] [CrossRef]
- Ludwig, D.S.; Majzoub, J.A.; Al-Zahrani, A.; Dallal, G.E.; Blanco, I.; Roberts, S.B. High glycemic index foods, overeating, and obesity. Pediatrics 1999, 103, E26. [Google Scholar] [CrossRef] [PubMed]
- Buga, A.; Kackley, M.L.; Crabtree, C.D.; Bedell, T.N.; Robinson, B.T.; Stoner, J.T.; Decker, D.D.; Hyde, P.N.; LaFountain, R.A.; Brownlow, M.L.; et al. Fasting and diurnal blood ketonemia and glycemia responses to a six-week, energy-controlled ketogenic diet, supplemented with racemic R/S-BHB salts. Clin. Nutr. ESPEN 2023, 54, 277–287. [Google Scholar] [CrossRef] [PubMed]
- Battezzati, A.; Foppiani, A.; Leone, A.; De Amicis, R.; Spadafranca, A.; Mari, A.; Bertoli, S. Acute Insulin Secretory Effects of a Classic Ketogenic Meal in Healthy Subjects: A Randomized Cross-Over Study. Nutrients 2023, 15, 1119. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Choi, Y.J.; Jeon, S.M.; Shin, S. Impact of a Ketogenic Diet on Metabolic Parameters in Patients with Obesity or Overweight and with or without Type 2 Diabetes: A Meta-Analysis of Randomized Controlled Trials. Nutrients 2020, 12, 2005. [Google Scholar] [CrossRef]
- Rafiullah, M.; Musambil, M.; David, S.K. Effect of a very low-carbohydrate ketogenic diet vs recommended diets in patients with type 2 diabetes: A meta-analysis. Nutr. Rev. 2022, 80, 488–502. [Google Scholar] [CrossRef] [PubMed]
- Parcha, V.; Heindl, B.; Kalra, R.; Li, P.; Gower, B.; Arora, G.; Arora, P. Insulin Resistance and Cardiometabolic Risk Profile Among Nondiabetic American Young Adults: Insights From NHANES. J. Clin. Endocrinol. Metab. 2022, 107, e25–e37. [Google Scholar] [CrossRef]
- Arneth, B. Mechanisms of Insulin Resistance in Patients with Obesity. Endocrines 2024, 5, 153–165. [Google Scholar] [CrossRef]
- Wondmkun, Y.T. Obesity, Insulin Resistance, and Type 2 Diabetes: Associations and Therapeutic Implications. Diabetes Metab. Syndr. Obes. 2020, 13, 3611–3616. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ludwig, D.S.; Apovian, C.M.; Aronne, L.J.; Astrup, A.; Cantley, L.C.; Ebbeling, C.B.; Heymsfield, S.B.; Johnson, J.D.; King, J.C.; Krauss, R.M.; et al. Competing paradigms of obesity pathogenesis: Energy balance versus carbohydrate-insulin models. Eur. J. Clin. Nutr. 2022, 76, 1209–1221. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ludwig, D.S. Carbohydrate-insulin model: Does the conventional view of obesity reverse cause and effect? Philos. Trans. R. Soc. Lond. B Biol. Sci. 2023, 378, 20220211. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Saslow, L.R.; Mason, A.E.; Kim, S.; Goldman, V.; Ploutz-Snyder, R.; Bayandorian, H.; Daubenmier, J.; Hecht, F.M.; Moskowitz, J.T. An Online Intervention Comparing a Very Low-Carbohydrate Ketogenic Diet and Lifestyle Recommendations Versus a Plate Method Diet in Overweight Individuals with Type 2 Diabetes: A Randomized Controlled Trial. J. Med. Internet Res. 2017, 19, e36. [Google Scholar] [CrossRef] [PubMed]
- Johnstone, A.M.; Horgan, G.W.; Murison, S.D.; Bremner, D.M.; Lobley, G.E. Effects of a high-protein ketogenic diet on hunger, appetite, and weight loss in obese men feeding ad libitum. Am. J. Clin. Nutr. 2008, 87, 44–55. [Google Scholar] [CrossRef] [PubMed]
- Saslow, L.R.; Kim, S.; Daubenmier, J.J.; Moskowitz, J.T.; Phinney, S.D.; Goldman, V.; Murphy, E.J.; Cox, R.M.; Moran, P.; Hecht, F.M. A randomized pilot trial of a moderate carbohydrate diet compared to a very low carbohydrate diet in overweight or obese individuals with type 2 diabetes mellitus or prediabetes. PLoS ONE 2014, 9, e91027. [Google Scholar] [CrossRef] [PubMed]
- Luukkonen, P.K.; Dufour, S.; Lyu, K.; Zhang, X.M.; Hakkarainen, A.; Lehtimäki, T.E.; Cline, G.W.; Petersen, K.F.; Shulman, G.I.; Yki-Järvinen, H. Effect of a ketogenic diet on hepatic steatosis and hepatic mitochondrial metabolism in nonalcoholic fatty liver disease. Proc. Natl. Acad. Sci. USA 2020, 117, 7347–7354. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yuan, X.; Wang, J.; Yang, S.; Gao, M.; Cao, L.; Li, X.; Hong, D.; Tian, S.; Sun, C. Effect of the ketogenic diet on glycemic control, insulin resistance, and lipid metabolism in patients with T2DM: A systematic review and meta-analysis. Nutr. Diabetes 2020, 10, 38. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hildebrandt, X.; Ibrahim, M.; Peltzer, N. Cell death and inflammation during obesity: “Know my methods, WAT(son)”. Cell Death Differ. 2023, 30, 279–292. [Google Scholar] [CrossRef]
- Artemniak-Wojtowicz, D.; Kucharska, A.M.; Pyrżak, B. Obesity and chronic inflammation crosslinking. Cent. Eur. J. Immunol. 2020, 45, 461–468. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wang, T.; He, C. Pro-inflammatory cytokines: The link between obesity and osteoarthritis. Cytokine Growth Factor Rev. 2018, 44, 38–50. [Google Scholar] [CrossRef] [PubMed]
- Dyńka, D.; Kowalcze, K.; Charuta, A.; Paziewska, A. The Ketogenic Diet and Cardiovascular Diseases. Nutrients 2023, 15, 3368. [Google Scholar] [CrossRef]
- Youm, Y.-H.; Nguyen, K.Y.; Grant, R.W.; Goldberg, E.L.; Bodogai, M.; Kim, D.; D’Agostino, D.; Planavsky, N.; Lupfer, C.; Kanneganti, T.-D.; et al. The ketone metabolite β-hydroxybutyrate blocks NLRP3 inflammasome–mediated inflammatory disease. Nat. Med. 2015, 21, 263–269. [Google Scholar] [CrossRef]
- Ma, X.; Nan, F.; Liang, H.; Shu, P.; Fan, X.; Song, X.; Hou, Y.; Zhang, D. Excessive intake of sugar: An accomplice of inflammation. Front. Immunol. 2022, 13, 988481. [Google Scholar] [CrossRef] [PubMed]
- Karimi, E.; Yarizadeh, H.; Setayesh, L.; Sajjadi, S.F.; Ghodoosi, N.; Khorraminezhad, L.; Mirzaei, K. High carbohydrate intakes may predict more inflammatory status than high fat intakes in pre-menopause women with overweight or obesity: A cross-sectional study. BMC Res. Notes 2021, 14, 279. [Google Scholar] [CrossRef] [PubMed]
- Yang, B.; Glenn, A.J.; Liu, Q.; Madsen, T.; Allison, M.A.; Shikany, J.M.; Manson, J.E.; Chan, K.H.K.; Wu, W.C.; Li, J.; et al. Added Sugar, Sugar-Sweetened Beverages, and Artificially Sweetened Beverages and Risk of Cardiovascular Disease: Findings from the Women’s Health Initiative and a Network Meta-Analysis of Prospective Studies. Nutrients 2022, 14, 4226. [Google Scholar] [CrossRef] [PubMed]
- Ramachandran, R.; Manan, A.; Kim, J.; Choi, S. NLRP3 inflammasome: A key player in the pathogenesis of life-style disorders. Exp. Mol. Med. 2024, 56, 1488–1500. [Google Scholar] [CrossRef]
- Alenezi, S.A.; Khan, R.; Snell, L.; Aboeldalyl, S.; Amer, S. The Role of NLRP3 Inflammasome in Obesity and PCOS-A Systematic Review and Meta-Analysis. Int. J. Mol. Sci. 2023, 24, 10976. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wani, K.; AlHarthi, H.; Alghamdi, A.; Sabico, S.; Al-Daghri, N.M. Role of NLRP3 Inflammasome Activation in Obesity-Mediated Metabolic Disorders. Int. J. Environ. Res. Public Health 2021, 18, 511. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhang, X.; Wang, Z.; Zheng, Y.; Yu, Q.; Zeng, M.; Bai, L.; Yang, L.; Guo, M.; Jiang, X.; Gan, J. Inhibitors of the NLRP3 inflammasome pathway as promising therapeutic candidates for inflammatory diseases (Review). Int. J. Mol. Med. 2023, 51, 35. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Neudorf, H.; Little, J.P. Impact of fasting & ketogenic interventions on the NLRP3 inflammasome: A narrative review. Biomed. J. 2024, 47, 100677. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rondanelli, M.; Perna, S.; Ilyas, Z.; Peroni, G.; Bazire, P.; Sajuox, I.; Maugeri, R.; Nichetti, M.; Gasparri, C. Effect of very low-calorie ketogenic diet in combination with omega-3 on inflammation, satiety hormones, body composition, and metabolic markers. A pilot study in class I obese subjects. Endocrine 2022, 75, 129–136. [Google Scholar] [CrossRef]
- Wood, R.J.; Volek, J.S.; Davis, S.R.; Dell’Ova, C.; Fernandez, M.L. Effects of a carbohydrate-restricted diet on emerging plasma markers for cardiovascular disease. Nutr. Metab. 2006, 3, 19. [Google Scholar] [CrossRef]
- Barrea, L.; Verde, L.; Di Lorenzo, C.; Savastano, S.; Colao, A.; Muscogiuri, G. Can the ketogenic diet improve our dreams? Effect of very low-calorie ketogenic diet (VLCKD) on sleep quality. J. Transl. Med. 2023, 21, 479. [Google Scholar] [CrossRef] [PubMed]
- Phillips, C.L.; Grayson, B.E. The immune remodel: Weight loss-mediated inflammatory changes to obesity. Exp. Biol. Med. 2020, 245, 109–121. [Google Scholar] [CrossRef] [PubMed]
- Sarin, H.V.; Lee, J.H.; Jauhiainen, M.; Joensuu, A.; Borodulin, K.; Männistö, S.; Jin, Z.; Terwilliger, J.D.; Isola, V.; Ahtiainen, J.P.; et al. Substantial fat mass loss reduces low-grade inflammation and induces positive alteration in cardiometabolic factors in normal-weight individuals. Sci. Rep. 2019, 9, 3450. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, V.E. Weight loss is a critical factor to reduce inflammation. Clin. Nutr. ESPEN 2018, 28, 21–35. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.M.; Myers, M.; Vieira-Potter, V.J. Adipose tissue inflammation and metabolic dysfunction: Role of exercise. Mo. Med. 2014, 111, 65–72. [Google Scholar] [PubMed] [PubMed Central]
- Chakhtoura, M.; Haber, R.; Ghezzawi, M.; Rhayem, C.; Tcheroyan, R.; Mantzoros, C.S. Pharmacotherapy of obesity: An update on the available medications and drugs under investigation. EClinicalMedicine 2023, 58, 101882. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bansal, A.B.; Patel, P.; Al Khalili, Y. Orlistat. [Updated 14 February 2024]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK542202/ (accessed on 2 January 2025).
- Konwar, M.; Bose, D.; Jaiswal, S.K.; Maurya, M.K.; Ravi, R. Efficacy and Safety of Liraglutide 3.0 mg in Patients with Overweight and Obese with or without Diabetes: A Systematic Review and Meta-Analysis. Int. J. Clin. Pract. 2022, 2022, 1201977. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nuffer, W.A.; Trujillo, J.M. Liraglutide: A New Option for the Treatment of Obesity. Pharmacotherapy 2015, 35, 926–934. [Google Scholar] [CrossRef] [PubMed]
- Tamayo-Trujillo, R.; Ruiz-Pozo, V.A.; Cadena-Ullauri, S.; Guevara-Ramírez, P.; Paz-Cruz, E.; Zambrano-Villacres, R.; Simancas-Racines, D.; Zambrano, A.K. Molecular mechanisms of semaglutide and liraglutide as a therapeutic option for obesity. Front. Nutr. 2024, 11, 1398059. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hu, E.-H.; Tsai, M.-L.; Lin, Y.; Chou, T.-S.; Chen, T.-H. A Review and Meta-Analysis of the Safety and Efficacy of Using Glucagon-like Peptide-1 Receptor Agonists. Medicina 2024, 60, 357. [Google Scholar] [CrossRef]
- Alarim, R.A.; Alasmre, F.A.; Alotaibi, H.A.; Alshehri, M.A.; Hussain, S.A. Effects of the Ketogenic Diet on Glycemic Control in Diabetic Patients: Meta-Analysis of Clinical Trials. Cureus 2020, 12, e10796. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Singh, J.; Kumar, R. Phentermine-topiramate: First combination drug for obesity. Int. J. Appl. Basic Med. Res. 2015, 5, 157–158. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Li, W.; Li, W.; Wang, D.; Wang, D.; Chen, H.; Chen, H.; Liu, Y.; Liu, Y.; Dong, S.; Dong, S.; et al. The relationship between psychological distress and weight maintenance in weight cycling: Mediating role of eating behavior. BMC Public Health 2024, 24, 894. [Google Scholar] [CrossRef] [PubMed]
- Heshmati, H.M.; Luzi, L.; Greenway, F.L.; Rebello, C.J. Editorial: Stress-induced weight changes. Front. Endocrinol. 2023, 14, 1209975. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Steptoe, A.; Frank, P. Obesity and psychological distress. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2023, 378, 20220225. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Eik-Nes, T.T.; Tokatlian, A.; Raman, J.; Spirou, D.; Kvaløy, K. Depression, anxiety, and psychosocial stressors across BMI classes: A Norwegian population study—The HUNT Study. Front. Endocrinol. 2022, 13, 886148. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jung, F.U.C.E.; Riedel-Heller, S.G.; Luck-Sikorski, C. The relationship between weight history and psychological health-Differences related to gender and weight loss patterns. PLoS ONE 2023, 18, e0281776. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- El Karkafi, R.; Gebara, T.; Salem, M.; Kamel, J.; El Khoury, G.; Zalal, M.; Fakhoury, M. Ketogenic Diet and Inflammation: Implications for Mood and Anxiety Disorders. Adv. Exp. Med. Biol. 2023, 1411, 537–554. [Google Scholar] [CrossRef] [PubMed]
- Henderson, L.R.; van den Berg, M.; Shaw, D.M. The effect of a 2 week ketogenic diet, versus a carbohydrate-based diet, on cognitive performance, mood and subjective sleepiness during 36 h of extended wakefulness in military personnel: An exploratory study. J. Sleep Res. 2023, 32, e13832. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.apa.org/monitor/2013/10/hunger (accessed on 11 July 2024).
- Kakoschke, N.; Zajac, I.T.; Tay, J.; Luscombe-Marsh, N.D.; Thompson, C.H.; Noakes, M.; Buckley, J.D.; Wittert, G.; Brinkworth, G.D. Effects of very low-carbohydrate vs. high-carbohydrate weight loss diets on psychological health in adults with obesity and type 2 diabetes: A 2-year randomized controlled trial. Eur. J. Nutr. 2021, 60, 4251–4262. [Google Scholar] [CrossRef] [PubMed]
- Brinkworth, G.D.; Luscombe-Marsh, N.D.; Thompson, C.H.; Noakes, M.; Buckley, J.D.; Wittert, G.; Wilson, C.J. Long-term effects of very low-carbohydrate and high-carbohydrate weight-loss diets on psychological health in obese adults with type 2 diabetes: Randomized controlled trial. J. Intern. Med. 2016, 280, 388–397. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://baszuckigroup.com/our-work/metabolic-mental-health/metabolic-psychiatry-initiative/ (accessed on 3 March 2025).
- Available online: https://nutrition-network.org/research/other-conditions-2/ (accessed on 11 July 2024).
- Norwitz, N.G.; Sethi, S.; Palmer, C.M. Ketogenic diet as a metabolic treatment for mental illness. Curr. Opin. Endocrinol. Diabetes Obes. 2020, 27, 269–274. [Google Scholar] [CrossRef] [PubMed]
- Sethi, S.; Wakeham, D.; Ketter, T.; Hooshmand, F.; Bjornstad, J.; Richards, B.; Westman, E.; Krauss, R.M.; Saslow, L. Ketogenic Diet Intervention on Metabolic and Psychiatric Health in Bipolar and Schizophrenia: A Pilot Trial. Psychiatry Res. 2024, 335, 115866. [Google Scholar] [CrossRef] [PubMed]
- Sethi, S.; Berk, M.; Andreazza, A.C.; Mujica-Parodi, L.R.; Campbell, I.; Campbell, H.; Longhitano, C.; Rasgon, N.; Volek, J.; Calkin, C.V.; et al. Metabolic Psychiatry: A Conceptual Framework Targeting Metabolic Dysfunction in Psychiatric Disease. PsyArXiv 2024. [Google Scholar] [CrossRef]
- Danan, A.; Westman, E.C.; Saslow, L.R.; Ede, G. The Ketogenic Diet for Refractory Mental Illness: A Retrospective Analysis of 31 Inpatients. Front. Psychiatry 2022, 13, 951376. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jacka, F.N.; O’Neil, A.; Opie, R.; Itsiopoulos, C.; Cotton, S.; Mohebbi, M.; Castle, D.; Dash, S.; Mihalopoulos, C.; Chatterton, M.L. A randomised controlled trial of dietary improvement for adults with major depression (the ‘SMILES’ trial). BMC Med. 2017, 15, 23. [Google Scholar] [CrossRef]
- Calabrese, L.; Frase, R.; Ghaloo, M. Complete remission of depression and anxiety using a ketogenic diet: Case series. Front. Nutr. 2024, 11, 1396685. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mahajan, V.R.; Elvig, S.K.; Vendruscolo, L.F.; Koob, G.F.; Darcey, V.L.; King, M.T.; Kranzler, H.R.; Volkow, N.D.; Wiers, C.E. Nutritional Ketosis as a Potential Treatment for Alcohol Use Disorder. Front. Psychiatry 2021, 12, 781668. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wiers, C.E.; Manza, P.; Wang, G.J.; Volkow, N.D. Ketogenic diet reduces a neurobiological craving signature in in patients with alcohol use disorder. Front. Nutr. 2024, 11, 1254341. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wiers, C.E.; Vendruscolo, L.F.; van der Veen, J.W.; Manza, P.; Shokri-Kojori, E.; Kroll, D.S.; Feldman, D.E.; McPherson, K.L.; Biesecker, C.L.; Zhang, R.; et al. Ketogenic diet reduces alcohol withdrawal symptoms in humans and alcohol intake in rodents. Sci. Adv. 2021, 7, eabf6780. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Li, X.; Young, A.J.; Pereira-Rufino, L.S.; Shi, Z.; Byanyima, J.; Vesslee, S.; Reddy, R.; Pond, T.; Elliott, M.; Reddy, R.; et al. Pharmacokinetic effects of a single-dose nutritional ketone ester supplement on brain ketone and glucose metabolism in alcohol use disorder—A pilot study. medRxiv 2023. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jia, D.; Xu, Y. Effects of an 8-week Baduanjin intervention combined with low-carbohydrates diet among overweight people who struggle with drug addiction. Front. Public Health 2022, 10, 989519. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kong, D.; Sun, J.X.; Yang, J.Q.; Li, Y.S.; Bi, K.; Zhang, Z.Y.; Wang, K.H.; Luo, H.Y.; Zhu, M.; Xu, Y. Ketogenic diet: A potential adjunctive treatment for substance use disorders. Front. Nutr. 2023, 10, 1191903. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sethi, S.; Sinha, A.; Gearhardt, A.N. Low carbohydrate ketogenic therapy as a metabolic treatment for binge eating and ultraprocessed food addiction. Curr. Opin. Endocrinol. Diabetes Obes. 2020, 27, 275–282. [Google Scholar] [CrossRef] [PubMed]
- Carmen, M.; Safer, D.L.; Saslow, L.R.; Kalayjian, T.; Mason, A.E.; Westman, E.C.; Sethi, S. Treating binge eating and food addiction symptoms with low-carbohydrate Ketogenic diets: A case series. J. Eat. Disord. 2020, 8, 2, Erratum in J. Eat. Disord. 2023, 11, 171. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rostanzo, E.; Marchetti, M.; Casini, I.; Aloisi, A.M. Very-Low-Calorie Ketogenic Diet: A Potential Treatment for Binge Eating and Food Addiction Symptoms in Women. A Pilot Study. Int. J. Environ. Res. Public Health 2021, 18, 12802. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Unwin, J.; Delon, C.; Giæver, H.; Kennedy, C.; Painschab, M.; Sandin, F.; Poulsen, C.S.; Wiss, D.A. Low carbohydrate and psychoeducational programs show promise for the treatment of ultra-processed food addiction. Front. Psychiatry 2022, 13, 1005523. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zaki, H.A.; Iftikhar, H.; Bashir, K.; Gad, H.; Samir Fahmy, A.; Elmoheen, A. A Comparative Study Evaluating the Effectiveness Between Ketogenic and Low-Carbohydrate Diets on Glycemic and Weight Control in Patients with Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis. Cureus 2022, 14, e25528. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Choy, K.Y.C.; Louie, J.C.Y. The effects of the ketogenic diet for the management of type 2 diabetes mellitus: A systematic review and meta-analysis of recent studies. Diabetes Metab. Syndr. 2023, 17, 102905. [Google Scholar] [CrossRef] [PubMed]
- Soltani, S.; Jayedi, A.; Abdollahi, S.; Vasmehjani, A.A.; Meshkini, F.; Shab-Bidar, S. Effect of carbohydrate restriction on body weight in overweight and obese adults: A systematic review and dose-response meta-analysis of 110 randomized controlled trials. Front. Nutr. 2023, 10, 1287987. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Castellana, M.; Conte, E.; Cignarelli, A.; Perrini, S.; Giustina, A.; Giovanella, L.; Giorgino, F.; Trimboli, P. Efficacy and safety of very low calorie ketogenic diet (VLCKD) in patients with overweight and obesity: A systematic review and meta-analysis. Rev. Endocr. Metab. Disord. 2020, 21, 5–16. [Google Scholar] [CrossRef] [PubMed]
- Bueno, N.B.; de Melo, I.S.; de Oliveira, S.L.; da Rocha Ataide, T. Very-low-carbohydrate ketogenic diet v. low-fat diet for long-term weight loss: A meta-analysis of randomised controlled trials. Br. J. Nutr. 2013, 110, 1178–1187. [Google Scholar] [CrossRef] [PubMed]
- Di Rosa, C.; Lattanzi, G.; Spiezia, C.; Imperia, E.; Piccirilli, S.; Beato, I.; Gaspa, G.; Micheli, V.; De Joannon, F.; Vallecorsa, N.; et al. Mediterranean Diet versus Very Low-Calorie Ketogenic Diet: Effects of Reaching 5% Body Weight Loss on Body Composition in Subjects with Overweight and with Obesity-A Cohort Study. Int. J. Environ. Res. Public Health 2022, 19, 13040. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cunha, G.M.; Guzman, G.; Correa De Mello, L.L.; Trein, B.; Spina, L.; Bussade, I.; Marques Prata, J.; Sajoux, I.; Countinho, W. Efficacy of a 2-Month Very Low-Calorie Ketogenic Diet (VLCKD) Compared to a Standard Low-Calorie Diet in Reducing Visceral and Liver Fat Accumulation in Patients with Obesity. Front. Endocrinol. 2020, 11, 607. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Burén, J.; Svensson, M.; Liv, P.; Sjödin, A. Effects of a Ketogenic Diet on Body Composition in Healthy, Young, Normal-Weight Women: A Randomized Controlled Feeding Trial. Nutrients 2024, 16, 2030. [Google Scholar] [CrossRef]
- Paoli, A.; Cenci, L.; Pompei, P.; Sahin, N.; Bianco, A.; Neri, M.; Caprio, M.; Moro, T. Effects of Two Months of Very Low Carbohydrate Ketogenic Diet on Body Composition, Muscle Strength, Muscle Area, and Blood Parameters in Competitive Natural Body Builders. Nutrients 2021, 13, 374. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Antonio Paoli, A.; Mancin, L.; Caprio, M.; Monti, E.; Narici, M.V.; Cenci, L.; Piccini, F.; Pincella, M.; Grigoletto, D.; Marcolin, G. Effects of 30 days of ketogenic diet on body composition, muscle strength, muscle area, metabolism, and performance in semi-professional soccer players. J. Int. Soc. Sports Nutr. 2021, 18, 62. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Falkenhain, K.; Locke, S.R.; Lowe, D.A.; Reitsma, N.J.; Lee, T.; Singer, J.; Weiss, E.J.; Little, J.P. Keyto app and device versus WW app on weight loss and metabolic risk in adults with overweight or obesity: A randomized trial. Obesity 2021, 29, 1606–1614. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Schiavo, L.; De Stefano, G.; Persico, F.; Gargiulo, S.; Di Spirito, F.; Griguolo, G.; Petrucciani, N.; Fontas, E.; Iannelli, A.; Pilone, V. A Randomized, Controlled Trial Comparing the Impact of a Low-Calorie Ketogenic vs a Standard Low-Calorie Diet on Fat-Free Mass in Patients Receiving an Elipse™ Intragastric Balloon Treatment. Obes. Surg. 2021, 31, 1514–1523. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sun, S.; Kong, Z.; Shi, Q.; Hu, M.; Zhang, H.; Zhang, D.; Nie, J. Non-Energy-Restricted Low-Carbohydrate Diet Combined with Exercise Intervention Improved Cardiometabolic Health in Overweight Chinese Females. Nutrients 2019, 11, 3051. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Greene, D.A.; Varley, B.J.; Hartwig, T.B.; Chapman, P.; Rigney, M. A Low-Carbohydrate Ketogenic Diet Reduces Body Mass Without Compromising Performance in Powerlifting and Olympic Weightlifting Athletes. J. Strength Cond. Res. 2018, 32, 3373–3382. [Google Scholar] [CrossRef] [PubMed]
- Vargas, S.; Romance, R.; Petro, J.L.; Bonilla, D.A.; Galancho, I.; Espinar, S.; Kreider, R.B.; Benítez-Porres, J. Efficacy of ketogenic diet on body composition during resistance training in trained men: A randomized controlled trial. J. Int. Soc. Sports Nutr. 2018, 15, 31. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Saslow, L.R.; Daubenmier, J.J.; Moskowitz, J.T.; Kim, S.; Murphy, E.J.; Phinney, S.D.; Ploutz-Snyder, R.; Goldman, V.; Cox, R.M.; Mason, A.E.; et al. Twelve-month outcomes of a randomized trial of a moderate-carbohydrate versus very low-carbohydrate diet in overweight adults with type 2 diabetes mellitus or prediabetes. Nutr. Diabetes 2017, 7, 304. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Merra, G.; Miranda, R.; Barrucco, S.; Gualtieri, P.; Mazza, M.; Moriconi, E.; Marchetti, M.; Chang, T.F.; De Lorenzo, A.; Di Renzo, L. Very-low-calorie ketogenic diet with aminoacid supplement versus very low restricted-calorie diet for preserving muscle mass during weight loss: A pilot double-blind study. Eur. Rev. Med. Pharmacol. Sci. 2016, 20, 2613–2621. [Google Scholar] [PubMed]
- Siekierko, N.; Lewandowski, M.; Żołnierek, M.; Kotusiewicz, W.; Gacoń, E.; Zembala, J.; Kucharski, J.; Zapała, B.; Ząber, A.; Świętochowski, J. Influence of ketogenic diet on athletes’ performance and other aspects of body function–review of literature. J. Educ. Health Sport 2023, 28, 138–154. [Google Scholar] [CrossRef]
- Harvey, K.L.; Holcomb, L.E.; Kolwicz, S.C., Jr. Ketogenic Diets and Exercise Performance. Nutrients 2019, 11, 2296. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Leaf, A.; Rothschild, J.A.; Sharpe, T.M.; Sims, S.T.; Macias, C.J.; Futch, G.G.; Roberts, M.D.; Stout, J.R.; Ormsbee, M.J.; Aragon, A.A.; et al. International society of sports nutrition position stand: Ketogenic diets. J. Int. Soc. Sports Nutr. 2024, 21, 2368167. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Noakes, T.D. Ketogenic Diets Are Beneficial for Athletic Performance. Med. Sci. Sports Exerc. 2024, 56, 753–755. [Google Scholar] [CrossRef]
- O’Hearn, A. Can a carnivore diet provide all essential nutrients? Curr. Opin. Endocrinol. Diabetes Obes. 2020, 27, 312–316. [Google Scholar] [CrossRef]
- Martin, P.; Johansson, M.; Ek, A. A Zero Carbohydrate, Carnivore Diet can Normalize Hydrogen Positive Small Intestinal Bacterial Overgrowth Lactulose Breath Tests: A Case Report; Research Square: Durham, NC, USA, 2021. [Google Scholar] [CrossRef]
- Lennerz, B.S.; Mey, J.T.; Henn, O.H.; Ludwig, D.S. Behavioral Characteristics and Self-Reported Health Status among 2029 Adults Consuming a “Carnivore Diet”. Curr. Dev. Nutr. 2021, 5, nzab133. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Norwitz, N.G.; Soto-Mota, A. Case report: Carnivore-ketogenic diet for the treatment of inflammatory bowel disease: A case series of 10 patients. Front. Nutr. 2024, 11, 1467475. [Google Scholar] [CrossRef] [PubMed]
- McClellan, W.S.; Du Bois, E.F. Clinical calorimetry: XLV. Prolonged meat diets with a study of kidney function and ketosis. J. Biol. Chem. 1930, 87, 651–668. [Google Scholar] [CrossRef]
- Shechter, Y. Bound lectins that mimic insulin produce persistent insulin-like activities. Endocrinology 1983, 113, 1921–1926. [Google Scholar] [CrossRef] [PubMed]
- Dalla Pellegrina, C.; Perbellini, O.; Scupoli, M.T.; Tomelleri, C.; Zanetti, C.; Zoccatelli, G.; Fusi, M.; Peruffo, A.; Rizzi, C.; Chignola, R. Effects of wheat germ agglutinin on human gastrointestinal epithelium: Insights from an experimental model of immune/epithelial cell interaction. Toxicol. Appl. Pharmacol. 2009, 237, 146–153. [Google Scholar] [CrossRef]
- Urugo, M.M.; Tringo, T.T. Naturally Occurring Plant Food Toxicants and the Role of Food Processing Methods in Their Detoxification. Int. J. Food Sci. 2023, 2023, 9947841. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Blasbalg, T.L.; Hibbeln, J.R.; Ramsden, C.E.; Majchrzak, S.F.; Rawlings, R.R. Changes in consumption of omega-3 and omega-6 fatty acids in the United States during the 20th century. Am. J. Clin. Nutr. 2011, 93, 950–962. [Google Scholar] [CrossRef]
- Mercola, J.; D’Adamo, C.R. Linoleic Acid: A Narrative Review of the Effects of Increased Intake in the Standard American Diet and Associations with Chronic Disease. Nutrients 2023, 15, 3129. [Google Scholar] [CrossRef]
- Alvheim, A.R.; Malde, M.K.; Osei-Hyiaman, D.; Lin, Y.H.; Pawlosky, R.J.; Madsen, L.; Kristiansen, K.; Frøyland, L.; Hibbeln, J.R. Dietary linoleic acid elevates endogenous 2-AG and anandamide and induces obesity. Obesity Silver Spring Md. 2012, 20, 1984–1994. [Google Scholar] [CrossRef]
- Deol, P.; Evans, J.R.; Dhahbi, J.; Chellappa, K.; Han, D.S.; Spindler, S.; Sladek, F.M. Soybean Oil Is More Obesogenic and Diabetogenic than Coconut Oil and Fructose in Mouse: Potential Role for the Liver. PLoS ONE 2015, 10, e0132672. [Google Scholar] [CrossRef]
- Deol, P.; Fahrmann, J.; Yang, J.; Evans, J.R.; Rizo, A.; Grapov, D.; Salemi, M.; Wanichthanarak, K.; Fiehn, O.; Phinney, B.; et al. Omega-6 and omega-3 oxylipins are implicated in soybean oil-induced obesity in mice. Sci. Rep. 2017, 7, 12488. [Google Scholar] [CrossRef]
- Russo, G.L. Dietary n-6 and n-3 polyunsaturated fatty acids: From biochemistry to clinical implications in cardiovascular prevention. Biochem. Pharmacol. 2009, 77, 937–946. [Google Scholar] [CrossRef] [PubMed]
- Sanders, T.A.B. Omega-6 Fatty Acids and Cardiovascular Disease. Circulation 2019, 139, 2437–2439. [Google Scholar] [CrossRef] [PubMed]
- Mazidi, M.; Shekoohi, N.; Katsiki, N.; Banach, M. Omega-6 fatty acids and the risk of cardiovascular disease: Insights from a systematic review and meta-analysis of randomized controlled trials and a Mendelian randomization study. Arch. Med. Sci. 2021, 18, 466–479. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Budoff, M.; Manubolu, V.S.; Kinninger, A.; Norwitz, N.G.; Feldman, D.; Wood, T.R.; Fialkow, J.; Cury, R.; Feldman, T.; Nasir, K. Carbohydrate Restriction-Induced Elevations in LDL-Cholesterol and Atherosclerosis: The KETO Trial. JACC Adv. 2024, 3, 101109. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Beal, T.; Ortenzi, F. Priority Micronutrient Density in Foods. Front. Nutr. 2022, 9, 806566. [Google Scholar] [CrossRef]
- Goedeke, S.; Murphy, T.; Rush, A.; Zinn, C. Assessing the Nutrient Composition of a Carnivore Diet: A Case Study Model. Nutrients 2025, 17, 140. [Google Scholar] [CrossRef]
- McMacken, M.; Shah, S. A plant-based diet for the prevention and treatment of type 2 diabetes. J. Geriatr. Cardiol. JGC 2017, 14, 342. [Google Scholar]
- Łuszczki, E.; Boakye, F.; Zielińska, M.; Dereń, K.; Bartosiewicz, A.; Oleksy, Ł.; Stolarczyk, A. Vegan diet: Nutritional components, implementation, and effects on adults’ health. Front. Nutr. 2023, 10, 1294497. [Google Scholar] [CrossRef]
- Ho, K.S.; Tan, C.Y.M.; Mohd Daud, M.A.; Seow-Choen, F. Stopping or reducing dietary fiber intake reduces constipation and its associated symptoms. World J. Gastroenterol. WJG 2012, 18, 4593–4596. [Google Scholar] [CrossRef]
- Jing, T.; Zhang, S.; Bai, M.; Chen, Z.; Gao, S.; Li, S.; Zhang, J. Effect of Dietary Approaches on Glycemic Control in Patients with Type 2 Diabetes: A Systematic Review with Network Meta-Analysis of Randomized Trials. Nutrients 2023, 15, 3156. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hanners, A.; Melnyk, B.M.; Volek, J.; Kelley, M.M. Ketogenic diet, African American women, and cardiovascular health: A systematic review. Worldviews Evid. Based Nurs. 2022, 19, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Luo, W.; Zhang, J.; Xu, D.; Zhou, Y.; Qu, Z.; Yang, Q.; Lv, Q. Low carbohydrate ketogenic diets reduce cardiovascular risk factor levels in obese or overweight patients with T2DM: A meta-analysis of randomized controlled trials. Front. Nutr. 2022, 9, 1092031. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wang, Z.; Chen, T.; Wu, S.; Dong, X.; Zhang, M.; Ma, G. Impact of the ketogenic diet as a dietary approach on cardiovascular disease risk factors: A meta-analysis of randomized clinical trials. Am. J. Clin. Nutr. 2024, 120, 294–309. [Google Scholar] [CrossRef] [PubMed]
- Joo, M.; Moon, S.; Lee, Y.S.; Kim, M.G. Effects of very low-carbohydrate ketogenic diets on lipid profiles in normal-weight (body mass index < 25 kg/m2) adults: A meta-analysis. Nutr. Rev. 2023, 81, 1393–1401. [Google Scholar] [CrossRef] [PubMed]
- Dyńka, D.; Rodzeń, Ł.; Rodzeń, M.; Łojko, D.; Kraszewski, S.; Ibrahim, A.; Hussey, M.; Deptuła, A.; Grzywacz, Ż.; Ternianov, A.; et al. Beneficial Effects of the Ketogenic Diet on Nonalcoholic Fatty Liver Disease (NAFLD/MAFLD). J. Clin. Med. 2024, 13, 4857. [Google Scholar] [CrossRef]
- Li, M.; Zhang, L.; Li, X.; Zhao, Y. Impact of short-term ketogenic diet on sex hormones and glucose-lipid metabolism in overweight or obese patients with polycystic ovary syndrome. J. Obstet. Gynaecol. Res. 2025, 51, e16178. [Google Scholar] [CrossRef] [PubMed]
- Di Renzo, L.; Gualtieri, P.; Zomparelli, S.; De Santis, G.L.; Seraceno, S.; Zuena, C.; Frank, G.; Cianci, R.; Centofanti, D.; De Lorenzo, A. Modified Mediterranean-Ketogenic Diet and Carboxytherapy as Personalized Therapeutic Strategies in Lipedema: A Pilot Study. Nutrients 2023, 15, 3654. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fomin, D.A.; Handfield, K. The ketogenic diet and dermatology: A primer on current literature. Cutis 2020, 105, 40–43. [Google Scholar] [PubMed]
- Verde, L.; Frias-Toral, E.; Cacciapuoti, S.; Simancas-Racines, D.; Megna, M.; Caiazzo, G.; Potestio, L.; Maisto, M.; Tenore, G.C.; Colao, A.; et al. Very low-calorie ketogenic diet (VLCKD): A therapeutic nutritional tool for acne? J. Transl. Med. 2024, 22, 322. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mustafa, M.S.; Shafique, M.A.; Aheed, B.; Ashraf, F.; Ali, S.M.S.; Iqbal, M.F.; Haseeb, A. The impact of ketogenic diet on drug-resistant epilepsy in children: A comprehensive review and meta-analysis. Ir. J. Med. Sci. 2024, 193, 1495–1503. [Google Scholar] [CrossRef] [PubMed]
- Díez-Arroyo, C.; García-García, M.; Soto-Méndez, M.J.; Molina-Montes, E.; Gil-Campos, M.; Gil, Á.; Gutiérrez-Jimeno, M.; Hernández-Ruiz, Á. Effect of the ketogenic diet as a treatment for refractory epilepsy in children and adolescents: A systematic review of reviews. Nutr. Rev. 2024, 82, 487–502. [Google Scholar] [CrossRef] [PubMed]
- Kirkpatrick, C.F.; Bolick, J.P.; Kris-Etherton, P.M.; Sikand, G.; Aspry, K.E.; Soffer, D.E.; Willard, K.E.; Maki, K.C. Review of current evidence and clinical recommendations on the effects of low-carbohydrate and very-low-carbohydrate (including ketogenic) diets for the management of body weight and other cardiometabolic risk factors: A scientific statement from the National Lipid Association Nutrition and Lifestyle Task Force. J. Clin. Lipidol. 2019, 13, 689–711.e1. [Google Scholar] [CrossRef] [PubMed]
- Menzies, J.; Sundararaj, A.; Cardamone, M.; McHarg, A.; Leach, S.; Krishnan, U. Ketogenic Diets in Children with Intractable Epilepsy and its Effects on Gastrointestinal Function, Gut Microbiome, Inflammation, and Quality of Life. J. Pediatr. Gastroenterol. Nutr. 2023, 77, 679–685. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Huang, L.; Li, H.; Chen, G.; Yang, L.; Wang, D.; Han, H.; Zheng, G.; Wang, X.; Liang, J.; et al. Effects of ketogenic diet on the classification and functional composition of intestinal flora in children with mitochondrial epilepsy. Front. Neurol. 2023, 14, 1237255. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dahlin, M.; Singleton, S.S.; David, J.A.; Basuchoudhary, A.; Wickström, R.; Mazumder, R.; Prast-Nielsen, S. Higher levels of Bifidobacteria and tumor necrosis factor in children with drug-resistant epilepsy are associated with anti-seizure response to the ketogenic diet. EBioMedicine 2022, 80, 104061. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kenig, S.; Petelin, A.; Poklar Vatovec, T.; Mohorko, N.; Jenko-Pražnikar, Z. Assessment of micronutrients in a 12-wk ketogenic diet in obese adults. Nutrition 2019, 67–68, 110522. [Google Scholar] [CrossRef] [PubMed]
- Ting, R.; Dugre, N.; Allan, G.M.; Lindblad, A.J. Ketogenic diet for weight loss. Can. Fam. Physician 2018, 64, 906. [Google Scholar]
- Available online: https://sci-fit.net/adhere-ketogenic-diet/#Are_Keto_Dieters_More_Likely_to_Drop_Out (accessed on 8 February 2025).
- Iacovides, S.; Maloney, S.K.; Bhana, S.; Angamia, Z.; Meiring, R.M. Could the ketogenic diet induce a shift in thyroid function and support a metabolic advantage in healthy participants? A pilot randomized-controlled-crossover trial. PLoS ONE 2022, 17, e0269440, Erratum in PLoS ONE 2023, 18, e0295112. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Goldberg, E.L.; Asher, J.L.; Molony, R.D.; Shaw, A.C.; Zeiss, C.J.; Wang, C.; Morozova-Roche, L.A.; Herzog, R.I.; Iwasaki, A.; Dixit, V.D. β-Hydroxybutyrate Deactivates Neutrophil NLRP3 Inflammasome to Relieve Gout Flares. Cell Rep. 2017, 18, 2077–2087. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Muhammad, K.R. Evaluation of uric acid levels and other biochemical parameters among Gout patients with Ketogenic diet in Erbil province. Cell. Mol. Biol. 2024, 70, 37–42. [Google Scholar] [CrossRef] [PubMed]
- Roster, K.; Xie, L.; Nguyen, T.; Lipner, S.R. Impact of Ketogenic and Low-Glycemic Diets on Inflammatory Skin Conditions. Cutis 2024, 113, 75–80. [Google Scholar] [CrossRef] [PubMed]
- Goswami, J.N.; Sharma, S. Current Perspectives On The Role Of The Ketogenic Diet In Epilepsy Management. Neuropsychiatr. Dis. Treat. 2019, 15, 3273–3285. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cervenka, M.C.; Wood, S.; Bagary, M.; Balabanov, A.; Bercovici, E.; Brown, M.G.; Devinsky, O.; Di Lorenzo, C.; Doherty, C.P.; Felton, E.; et al. International Recommendations for the Management of Adults Treated with Ketogenic Diet Therapies. Neurol. Clin. Pract. 2021, 11, 385–397. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Watanabe, M.; Tuccinardi, D.; Ernesti, I.; Basciani, S.; Mariani, S.; Genco, A.; Manfrini, S.; Lubrano, C.; Gnessi, L. Scientific evidence underlying contraindications to the ketogenic diet: An update. Obes. Rev. 2020, 21, e13053. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shalabi, H.; Alotaibi, A.; Alqahtani, A.; Alattas, H.; Alghamdi, Z. Ketogenic Diets: Side Effects, Attitude, and Quality of Life. Cureus 2021, 13, e20390. [Google Scholar] [CrossRef]
- Bostock, E.C.S.; Kirkby, K.C.; Taylor, B.V.; Hawrelak, J.A. Consumer Reports of “Keto Flu” Associated with the Ketogenic Diet. Front. Nutr. 2020, 7, 20. [Google Scholar] [CrossRef]
- Fedorovich, S.V.; Voronina, P.P.; Waseem, T.V. Ketogenic diet versus ketoacidosis: What determines the influence of ketone bodies on neurons? Neural Regen. Res. 2018, 13, 2060–2063. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lizzo, J.M.; Goyal, A.; Gupta, V. Adult Diabetic Ketoacidosis. [Updated 10 July 2023]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK560723/ (accessed on 8 February 2025).
- Mullins, G.; Hallam, C.L.; Broom, I. Ketosis, ketoacidosis and very-low-calorie diets: Putting the record straight. Nutr. Bull. 2011, 36, 397–402. [Google Scholar] [CrossRef]
- Charoensri, S.; Sothornwit, J.; Trirattanapikul, A.; Pongchaiyakul, C. Ketogenic Diet-Induced Diabetic Ketoacidosis in a Young Adult with Unrecognized Type 1 Diabetes. Case Rep. Endocrinol. 2021, 2021, 6620832. [Google Scholar] [CrossRef]
- Palmer, B.F.; Clegg, D.J. Euglycemic Ketoacidosis as a Complication of SGLT2 Inhibitor Therapy. Clin. J. Am. Soc. Nephrol. 2021, 16, 1284–1291. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Al Alawi, A.M.; Al Flaiti, A.; Falhammar, H. Lactation Ketoacidosis: A Systematic Review of Case Reports. Medicina 2020, 56, 299. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dyńka, D.; Rodzeń, Ł.; Rodzeń, M.; Pacholak-Klimas, A.; Ede, G.; Sethi, S.; Łojko, D.; Bartoń, K.; Berry, K.; Deptuła, A.; et al. Ketogenic Diets for Body Weight Loss: A Comparison with Other Diets. Nutrients 2025, 17, 965. https://doi.org/10.3390/nu17060965
Dyńka D, Rodzeń Ł, Rodzeń M, Pacholak-Klimas A, Ede G, Sethi S, Łojko D, Bartoń K, Berry K, Deptuła A, et al. Ketogenic Diets for Body Weight Loss: A Comparison with Other Diets. Nutrients. 2025; 17(6):965. https://doi.org/10.3390/nu17060965
Chicago/Turabian StyleDyńka, Damian, Łukasz Rodzeń, Mateusz Rodzeń, Anna Pacholak-Klimas, Georgia Ede, Shebani Sethi, Dorota Łojko, Karolina Bartoń, Ken Berry, Adam Deptuła, and et al. 2025. "Ketogenic Diets for Body Weight Loss: A Comparison with Other Diets" Nutrients 17, no. 6: 965. https://doi.org/10.3390/nu17060965
APA StyleDyńka, D., Rodzeń, Ł., Rodzeń, M., Pacholak-Klimas, A., Ede, G., Sethi, S., Łojko, D., Bartoń, K., Berry, K., Deptuła, A., Grzywacz, Ż., Martin, P., Unwin, J., & Unwin, D. (2025). Ketogenic Diets for Body Weight Loss: A Comparison with Other Diets. Nutrients, 17(6), 965. https://doi.org/10.3390/nu17060965











