Pre-Sleep Alpha-Lactalbumin Supplementation Does Not Improve the Habitual Sleep and Performance of Sportspeople with Sleep Difficulties
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
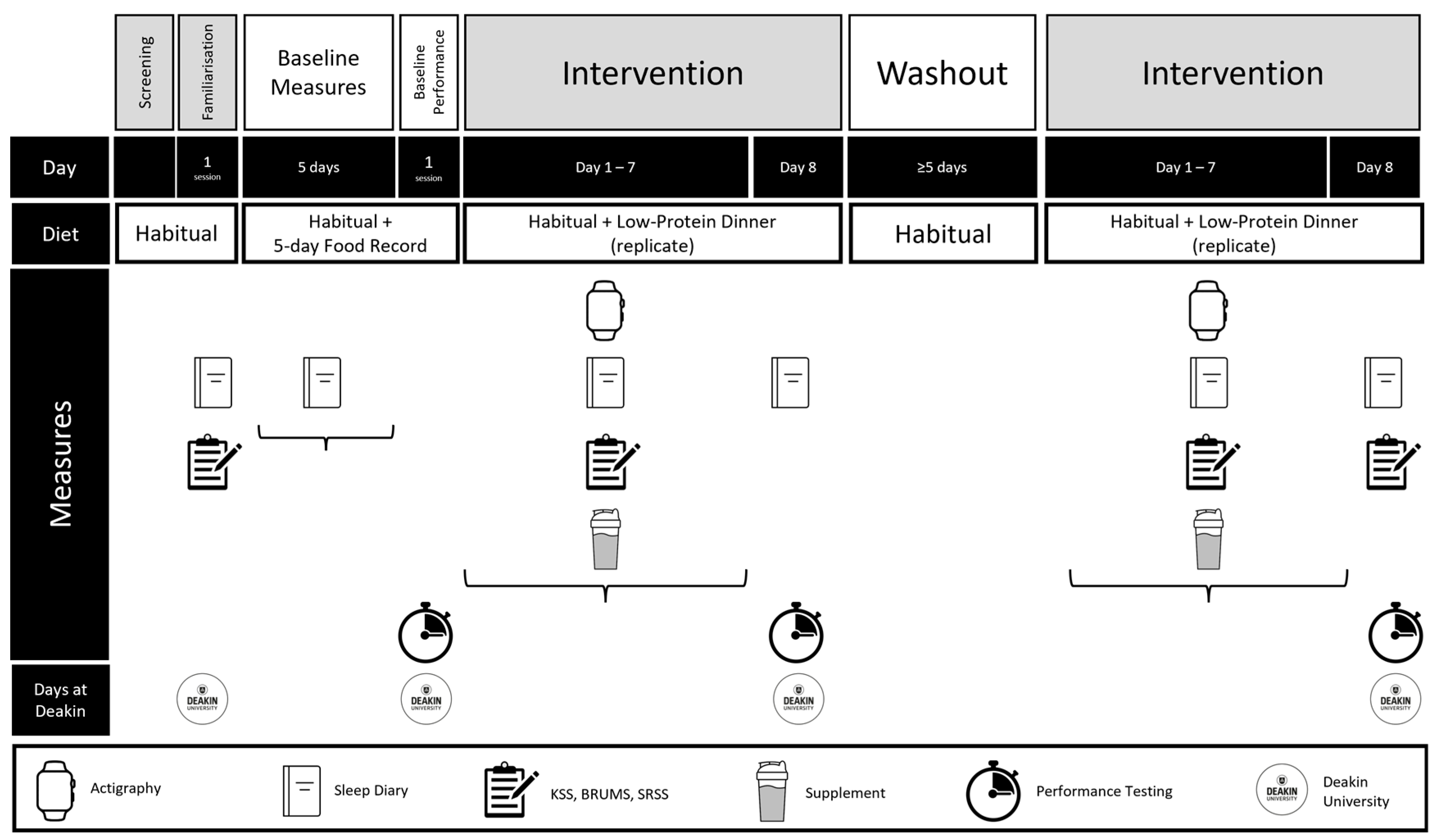
2.2. Study Design
2.3. Experimental Trials
2.4. Dietary Supplement
2.5. Dietary Standardisation
2.6. Sleep Assessment
- Bedtime (HH:MM): The self-reported clock time at which a participant attempts sleep.
- Waketime (HH:MM): The self-reported clock time at which a participant awakes for the final time and stops attempting sleep.
- Total sleep time (TST; min): The amount of sleep obtained between initial sleep onset and final awakening.
- Sleep efficiency (SE; %): The percentage of time in bed between bedtime and final wake time that was spent asleep.
- Sleep onset latency (SOL; min): The period between bedtime and initial sleep onset.
- Wake after sleep onset (WASO; min): The time spent awake after initial sleep onset and before final awakening.
- Awakenings (n): The number of wake periods detected after initial sleep onset.
2.7. Subjective Measures
2.8. Karolinska Sleepiness Scale
2.9. Brunel Mood Scale
2.10. Short Recovery Stress Scale for Sport
2.11. Consensus Sleep Diary
2.12. Training Diary
2.13. Physical Performance
2.14. The 30 s Continuous Jump Test (CJ30)
2.15. Yo-Yo Intermittent Recovery Test Level 1 (YYIR1)
2.16. Reaction Time
2.17. Statistical Analysis
3. Results
3.1. Sleep
3.1.1. Objective Sleep
3.1.2. Subjective Sleep
3.2. Questionnaires
3.2.1. Sleepiness and Mood
3.2.2. Recovery and Stress
3.3. Performance Measures
3.3.1. The 30 s Continuous Jump Test (CJ30)
3.3.2. Yo-Yo Intermittent Recovery Test Level 1
3.3.3. Dynavision Lightboard
4. Discussion
5. Conclusions
Practical Applications
- Overall, 40 g α-lactalbumin two hours before bedtime does not impair sleep efficiency or duration over one week.
- Negative emotional states may be reduced following ALAC consumption in the evening.
- Pre-sleep subjective mental and physical performance capability may be reduced post-ALAC consumption.
- Future sleep studies within trained populations with sleep difficulties should opt for more comprehensive sleep tools (e.g., portable electroencephalography) and objectively confirm baseline sleep difficulties.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ALAC | Alpha-lactalbumin |
| ASSQ | Athlete Sleep Screening Questionnaire |
| BRUMS | Brunel Mood Scale |
| CJ30 | 30 s countermovement jump test |
| KSS | Karolinska Sleepiness Scale |
| LNAA | Large neutral amino acid |
| NREM | Non-rapid eye movement |
| PSQI | Pittsburgh Sleep Quality Index |
| SRSS | Short Recovery Stress Scale in Sport |
| TRP | Tryptophan |
| YYIR1 | Yo-Yo Intermittent Recovery Test Level 1 |
References
- Fullagar, H.H.K.; Skorski, S.; Duffield, R.; Hammes, D.; Coutts, A.J.; Meyer, T. Sleep and athletic performance: The effects of sleep loss on exercise performance, and physiological and cognitive responses to exercise. Sports Med. 2015, 45, 161–186. [Google Scholar]
- Walsh, N.P.; Halson, S.L.; Sargent, C.; Roach, G.D.; Nédélec, M.; Gupta, L.; Leeder, J.; Fullagar, H.H.; Coutts, A.J.; Edwards, B.J. Sleep and the athlete: Narrative review and 2021 expert consensus recommendations. Br. J. Sports Med. 2021, 55, 356–368. [Google Scholar]
- Ohayon, M.; Wickwire, E.M.; Hirshkowitz, M.; Albert, S.M.; Avidan, A.; Daly, F.J.; Dauvilliers, Y.; Ferri, R.; Fung, C.; Gozal, D. National Sleep Foundation’s sleep quality recommendations: First report. Sleep Health 2017, 3, 6–19. [Google Scholar] [PubMed]
- Roberts, S.S.H.; Teo, W.-P.; Aisbett, B.; Warmington, S.A. Extended sleep maintains endurance performance better than normal or restricted sleep. Med. Sci. Sports Exerc. 2019, 51, 2516–2523. [Google Scholar]
- Barnard, J.; Roberts, S.; Lastella, M.; Aisbett, B.; Condo, D. The impact of dietary factors on the sleep of athletically trained populations: A systematic review. Nutrients 2022, 14, 3271. [Google Scholar] [CrossRef] [PubMed]
- Richard, D.M.; Dawes, M.A.; Mathias, C.W.; Acheson, A.; Hill-Kapturczak, N.; Dougherty, D.M. L-tryptophan: Basic metabolic functions, behavioral research and therapeutic indications. Int. J. Tryptophan Res. 2009, 2, IJTR-S2129. [Google Scholar]
- Markus, C.R. Dietary amino acids and brain serotonin function; implications for stress-related affective changes. Neuromol. Med. 2008, 10, 247–258. [Google Scholar]
- Gratwicke, M.; Miles, K.; Clark, B.; Pumpa, K. The effect of α-lactalbumin consumption on sleep quality and quantity in female rugby union athletes: A field-based study. Biol. Sport 2022, 40, 449–455. [Google Scholar]
- Miles, K.H.; Clark, B.; Fowler, P.M.; Gratwicke, M.J.; Martin, K.; Welvaert, M.; Miller, J.; Pumpa, K.L. ɑ-lactalbumin improves sleep and recovery post simulated evening competition in female athletes. Med. Sci. Sports Exerc. 2021, 53, 2618–2627. [Google Scholar]
- Barnard, J.; Roberts, S.; Lastella, M.; Callahan, D.L.; Aisbett, B.; Condo, D. Evening alpha-lactalbumin supplementation alters sleep architecture and reduces morning reaction time in an athletically trained population with sleep difficulties. Int. J. Sport Nutr. Exerc. Metab. 2025, 1, 1–10. [Google Scholar] [CrossRef]
- Barnard, J.; Roberts, S.; Kelly, M.; Lastella, M.; Aisbett, B.; Condo, D. Alpha-lactalbumin and sleep: A systematic review. J. Sleep Res. 2024, 33, e14141. [Google Scholar] [PubMed]
- MacInnis, M.J.; Dziedzic, C.E.; Wood, E.; Oikawa, S.Y.; Phillips, S.M. Presleep α-lactalbumin consumption does not improve sleep quality or time-trial performance in cyclists. Int. J. Sport Nutr. Exerc. Metab. 2020, 30, 197–202. [Google Scholar] [CrossRef]
- Oikawa, S.Y.; Macinnis, M.J.; Tripp, T.R.; McGlory, C.; Baker, S.K.; Phillips, S.M. Lactalbumin, not collagen, augments muscle protein synthesis with aerobic exercise. Med. Sci. Sports Exerc. 2020, 52, 1394–1403. [Google Scholar] [CrossRef] [PubMed]
- Spinweber, C.L. L-tryptophan administered to chronic sleep-onset insomniacs: Late-appearing reduction of sleep latency. Psychopharmacology 1986, 90, 151–155. [Google Scholar] [PubMed]
- Silber, B.Y.; Schmitt, J.A.J. Effects of tryptophan loading on human cognition, mood, and sleep. Neurosci. Biobehav. Rev. 2010, 34, 387–407. [Google Scholar]
- Williams, M. Dietary supplements and sports performance: Amino acids. J. Int. Soc. Sports Nutr. 2005, 2, 63. [Google Scholar]
- Halson, S.L.; Shaw, G.; Versey, N.; Miller, D.J.; Sargent, C.; Roach, G.D.; Nyman, L.; Carter, J.M.; Baar, K. Optimisation and validation of a nutritional intervention to enhance sleep quality and quantity. Nutrients 2020, 12, 2579. [Google Scholar] [CrossRef]
- McKay, A.K.A.; Stellingwerff, T.; Smith, E.S.; Martin, D.T.; Mujika, I.; Goosey-Tolfrey, V.L.; Sheppard, J.; Burke, L.M. Defining training and performance caliber: A participant classification framework. Int. J. Sports Physiol. 2021, 17, 317–331. [Google Scholar]
- De Pauw, K.; Roelands, B.; Cheung, S.S.; De Geus, B.; Rietjens, G.; Meeusen, R. Guidelines to classify subject groups in sport-science research. Int. J. Sports Physiol. 2013, 8, 111–122. [Google Scholar]
- Åkerstedt, T.; Gillberg, M. Subjective and objective sleepiness in the active individual. Int. J. Neurosci. 1990, 52, 29–37. [Google Scholar]
- aan het Rot, M.; Moskowitz, D.S.; Pinard, G.; Young, S.N. Social behaviour and mood in everyday life: The effects of tryptophan in quarrelsome individuals. J. Psychiatry Neurosci. 2006, 31, 253–262. [Google Scholar] [PubMed]
- Thomas, C.; Kingshott, R.N.; Allott, K.M.; Tang, J.C.Y.; Dunn, R.; Fraser, W.D.; Thorley, J.; Virgilio, N.; Prawitt, J.; Hogervorst, E. Collagen peptide supplementation before bedtime reduces sleep fragmentation and improves cognitive function in physically active males with sleep complaints. Eur. J. Nutr. 2024, 63, 323–335. [Google Scholar] [PubMed]
- Wurtman, R.J.; Wurtman, J.J.; Regan, M.M.; McDermott, J.M.; Tsay, R.H.; Breu, J.J. Effects of normal meals rich in carbohydrates or proteins on plasma tryptophan and tyrosine ratios. Am. J. Clin. Nutr. 2003, 77, 128–132. [Google Scholar]
- Fuller, K.L.; Juliff, L.; Gore, C.J.; Peiffer, J.J.; Halson, S.L. Software thresholds alter the bias of actigraphy for monitoring sleep in team-sport athletes. J. Sci. Med. Sport 2017, 20, 756–760. [Google Scholar]
- Sargent, C.; Lastella, M.; Halson, S.L.; Roach, G.D. The validity of activity monitors for measuring sleep in elite athletes. J. Sci. Med. Sport 2016, 19, 848–853. [Google Scholar] [PubMed]
- Kaida, K.; Takahashi, M.; Åkerstedt, T.; Nakata, A.; Otsuka, Y.; Haratani, T.; Fukasawa, K. Validation of the Karolinska sleepiness scale against performance and EEG variables. Clin. Neurophysiol. 2006, 117, 1574–1581. [Google Scholar]
- Terry, P.C.; Lane, A.M.; Lane, H.J.; Keohane, L. Development and validation of a mood measure for adolescents. J. Sports Sci. 1999, 17, 861–872. [Google Scholar]
- Kölling, S.; Schaffran, P.; Bibbey, A.; Drew, M.; Raysmith, B.; Nässi, A.; Kellmann, M. Validation of the Acute Recovery and Stress Scale (ARSS) and the Short Recovery and Stress Scale (SRSS) in three English-speaking regions. J. Sports Sci. 2020, 38, 130–139. [Google Scholar]
- Carney, C.E.; Buysse, D.J.; Ancoli-Israel, S.; Edinger, J.D.; Krystal, A.D.; Lichstein, K.L.; Morin, C.M. The consensus sleep diary: Standardizing prospective sleep self-monitoring. Sleep 2012, 35, 287–302. [Google Scholar]
- Waterhouse, J.; Drust, B.; Weinert, D.; Edwards, B.; Gregson, W.; Atkinson, G.; Kao, S.; Aizawa, S.; Reilly, T. The circadian rhythm of core temperature: Origin and some implications for exercise performance. Chronobiol. Int. 2005, 22, 207–225. [Google Scholar]
- Dal Pupo, J.; Gheller, R.G.; Dias, J.A.; Rodacki, A.L.F.; Moro, A.R.P.; Santos, S.G. Reliability and validity of the 30-s continuous jump test for anaerobic fitness evaluation. J. Sci. Med. Sport 2014, 17, 650–655. [Google Scholar] [PubMed]
- Krustrup, P.; Mohr, M.; Amstrup, T.; Rysgaard, T.; Johansen, J.; Steensberg, A.; Pedersen, P.K.; Bangsbo, J. The yo-yo intermittent recovery test: Physiological response, reliability, and validity. Med. Sci. Sports Exerc. 2003, 35, 697–705. [Google Scholar] [PubMed]
- Ong, N.C.H. The use of Dynavision in sport and exercise research: A review. Int. J. Sports Exerc. Psychol. 2020, 18, 561–580. [Google Scholar]
- Vesia, M.; Esposito, J.; Prime, S.L.; Klavora, P. Correlations of selected psychomotor and visuomotor tests with initial Dynavision performance. Percept. Mot. Ski. 2008, 107, 14–20. [Google Scholar]
- Sadeh, A. The role and validity of actigraphy in sleep medicine: An update. Sleep Med. Rev. 2011, 15, 259–267. [Google Scholar]
- Grillon, C.; Quispe-Escudero, D.; Mathur, A.; Ernst, M. Mental fatigue impairs emotion regulation. Emotion 2015, 15, 383. [Google Scholar]
- Baker, F.C.; Lee, K.A. Menstrual cycle effects on sleep. Sleep Med. Clin. 2022, 17, 283–294. [Google Scholar]
- Carmichael, M.A.; Thomson, R.L.; Moran, L.J.; Wycherley, T.P. The Impact of menstrual cycle phase on athletes’ performance: A narrative review. Int. J. Environ. Res. Public Health 2021, 18, 1667. [Google Scholar] [CrossRef]
| Variable | Mean ± SD |
|---|---|
| Age (years) | 25.9 ± 5.3 |
| Body mass (kg) | 80.0 ± 10.6 |
| Height (m) | 1.8 ± 0.1 |
| ASSQ (sleep difficulty score) | 8.6 ± 2.2 |
| PSQI (global score) | 10.0 ± 3.0 |
| Subjective sleep latency (min) | 30.3 ± 16.4 |
| Large Neutral Amino Acids (LNAAs) | α-Lactalbumin (40 g) | Control— Collagen (40 g) |
|---|---|---|
| Isoleucine (g) | 2.4 | 0.5 |
| Leucine (g) | 4.3 | 1.0 |
| Phenylalanine (g) | 1.6 | 0.6 |
| Tyrosine (g) | 1.8 | 0.2 |
| Valine (g) | 1.7 | 0.9 |
| Tryptophan (g) | 1.9 | 0.0 |
| Sleep Metric | CON | ALAC | p Value | Treatment Coefficient | 95% CI | |
|---|---|---|---|---|---|---|
| Actigraphy-derived metrics | ||||||
| TST (h) | 7.26 ± 1.06 | 7.12 ± 1.04 | 0.084 | −0.139 | −0.297 | 0.019 |
| SOL (min) | 16.53 ± 15.51 | 16.70 ± 13.34 | 0.932 | 0.128 | −2.834 | 3.089 |
| WASO (min) | 34.69 ± 21.14 | 37.58 ± 23.20 | 0.075 | 3.191 | −0.328 | 6.711 |
| SE (%) | 88.77 ± 5.20 | 87.96 ± 5.32 | 0.077 | −0.838 | −1.767 | 0.091 |
| Awakenings (#) | 10.25 ± 5.28 | 11.01 ± 5.79 | 0.031 * | 0.846 | 0.078 | 1.613 |
| Subjective sleep metrics | ||||||
| Bedtime (HH:MM) | 22:45 ± 01:09 | 22:54 ± 01:25 | 0.237 | 0.005 (00:07) | −0.003 (−00:04) | 0.013 (00:18) |
| Waketime (HH:MM) | 07:02 ± 01:32 | 07:08 ± 01:39 | 0.541 | 0.002 (00:03) | −0.005 (−00:08) | 0.010 (00:15) |
| sSOL (min) | 18.98 ± 18.43 | 21.31 ± 22.81 | 0.153 | 2.519 | −0.944 | 5.983 |
| sWASO (min) | 9.56 ± 20.72 | 12.91 ± 26.51 | 0.165 | 3.530 | −1.459 | 8.519 |
| Awakenings (#) | 1.52 ± 1.38 | 1.81 ± 1.69 | 0.041 * | 0.266 | 0.011 | 0.521 |
| Sleep Quality (1–5) | 3.34 ± 0.83 | 3.36 ± 0.85 | 0.785 | 0.023 | −0.143 | 0.189 |
| Recovery/Stress State | CON | A-LAC | p Value | Treatment Coefficient | 95% CI | |
|---|---|---|---|---|---|---|
| Evening | ||||||
| Muscular Stress | 2.48 ± 1.40 | 2.35 ± 1.50 | 0.375 | −0.119 | −0.381 | 0.144 |
| Lack of Activation | 2.21 ± 1.38 | 2.15 ± 1.33 | 0.661 | −0.050 | −0.276 | 0.176 |
| Negative Emotional State | 1.41 ± 1.33 | 1.04 ± 1.08 | 0.001 * | −0.331 | −0.527 | −0.136 |
| Overall Stress | 2.20 ± 1.37 | 2.26 ± 1.36 | 0.572 | 0.068 | −0.170 | 0.306 |
| Physical Performance | 3.16 ± 1.27 | 2.84 ± 1.26 | 0.004 * | −0.327 | −0.549 | −0.106 |
| Mental Performance | 3.18 ± 1.47 | 2.77 ± 1.16 | <0.001 * | −0.422 | −0.637 | −0.207 |
| Emotional Balance | 3.68 ± 1.40 | 3.46 ± 1.25 | 0.026 * | −0.252 | −0.474 | −0.031 |
| Overall Recovery | 3.16 ± 1.27 | 2.99 ± 1.27 | 0.118 | −0.186 | −0.419 | 0.047 |
| CJ30 Outcome | Baseline | CON | ALAC | p Value | Treatment Coefficient | 95% CI | |
|---|---|---|---|---|---|---|---|
| Total jumps (n) | 19.74 ± 4.73 | 21.39 ± 5.06 # | 21.83 ± 4.73 | 0.458 | 0.435 | −0.759 | 1.629 |
| Maximum jump height (cm) | 33.36 ± 6.25 | 32.16 ± 5.73 # | 32.26 ± 5.59 | 0.836 | 0.010 | −0.889 | 1.089 |
| Average jump height (cm) | 28.72 ± 5.55 | 28.58 ± 5.53 | 27.68 ± 5.14 # | 0.037 * | −0.907 | −1.753 | −0.061 |
| Total jump load (cm) | 550.96 ± 116.22 | 595.80 ± 128.91 # | 590.15 ± 122.31 # | 0.733 | −5.659 | −39.605 | 28.286 |
| Fatigue Index (%) | 16.62 ± 10.88 | 15.90 ± 8.30 | 20.36 ± 10.85 | 0.059 | 4.461 | −0.179 | 9.101 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barnard, J.; Roberts, S.; Lastella, M.; Aisbett, B.; Condo, D. Pre-Sleep Alpha-Lactalbumin Supplementation Does Not Improve the Habitual Sleep and Performance of Sportspeople with Sleep Difficulties. Nutrients 2025, 17, 1196. https://doi.org/10.3390/nu17071196
Barnard J, Roberts S, Lastella M, Aisbett B, Condo D. Pre-Sleep Alpha-Lactalbumin Supplementation Does Not Improve the Habitual Sleep and Performance of Sportspeople with Sleep Difficulties. Nutrients. 2025; 17(7):1196. https://doi.org/10.3390/nu17071196
Chicago/Turabian StyleBarnard, Jackson, Spencer Roberts, Michele Lastella, Brad Aisbett, and Dominique Condo. 2025. "Pre-Sleep Alpha-Lactalbumin Supplementation Does Not Improve the Habitual Sleep and Performance of Sportspeople with Sleep Difficulties" Nutrients 17, no. 7: 1196. https://doi.org/10.3390/nu17071196
APA StyleBarnard, J., Roberts, S., Lastella, M., Aisbett, B., & Condo, D. (2025). Pre-Sleep Alpha-Lactalbumin Supplementation Does Not Improve the Habitual Sleep and Performance of Sportspeople with Sleep Difficulties. Nutrients, 17(7), 1196. https://doi.org/10.3390/nu17071196









