Caffeine Consumption and Sleep Quality in Australian Adults
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Measures
2.4. Statistical Analysis
3. Results
3.1. Study Participants
3.2. Types of Foods/Beverages That Contribute to Caffeine Intake by Gender
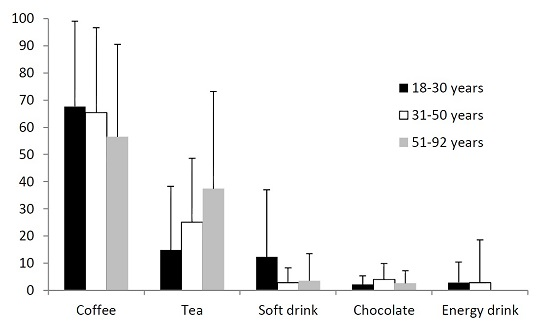
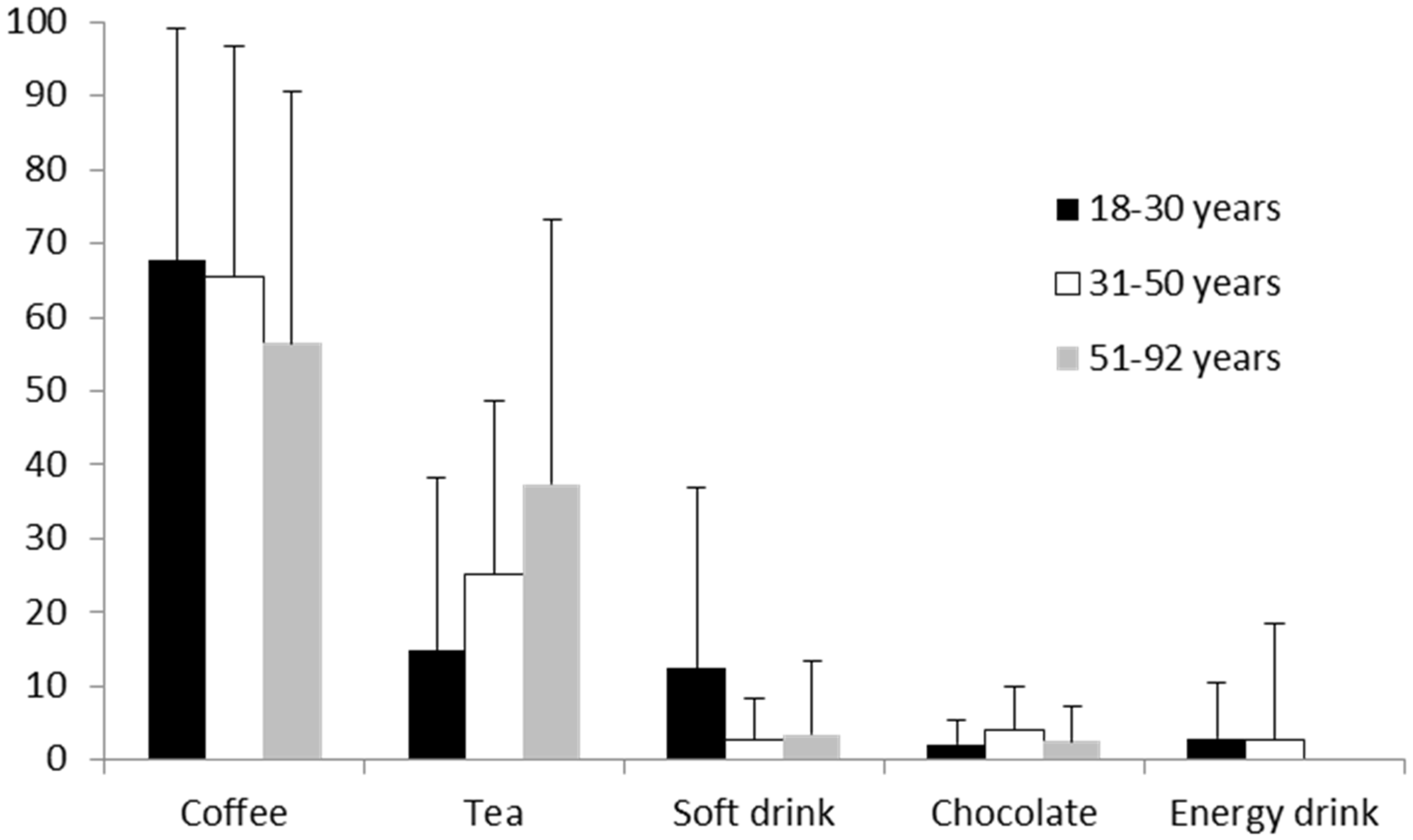
3.3. Types of Foods/Beverages That Contribute to Caffeine Intake by Age
3.4. Impact of Caffeine on Sleep Quality
3.5. Caffeine Intake between Self-Reported Good and Poor Sleepers
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| TST | Total Sleep Time |
| TIB | Time in Bed |
| FFQ | Food Frequency Questionnaire |
| PSQI | Pittsburgh Sleep Quality Index |
| SOL | Sleep Onset Latency |
| C-FFQ | Caffeine food frequency questionnaire |
| SE | Sleep Efficiency |
References
- Dorrian, J.; Paterson, J.; Dawson, D.; Pincombe, J.; Grech, C.; Rogers, A.E. Sleep, stress and compensatory behaviors in Australian nurses and midwives. Rev. Saude Publica 2011, 45, 922–930. [Google Scholar] [CrossRef] [PubMed]
- Porkka-Heiskanen, T.; Strecker, R.E.; Thakkar, M.; Bjørkum, A.A.; Greene, R.W.; McCarley, R.W. Adenosine: A mediator of the sleep-inducing effects of prolonged wakefulness. Science 1997, 276, 1265–1268. [Google Scholar] [CrossRef] [PubMed]
- Strecker, R.E.; Morairty, S.; Thakkar, M.M.; Porkka-Heiskanen, T.; Basheer, R.; Dauphin, L.J.; Rainnie, D.G.; Portas, C.M.; Greene, R.W.; McCarley, R.W. Adenosinergic modulation of basal forebrain and preoptic/anterior hypothalamic neuronal activity in the control of behavioral state. Behav. Brain Res. 2000, 115, 183–204. [Google Scholar] [CrossRef]
- Brice, C.; Smith, A. The effects of caffeine on simulated driving, subjective alertness and sustained attention. Hum. Psychopharmacol. Clin. Exp. 2001, 16, 523–531. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics Australian Health Survey: Nutrition First Results—Foods and Nutrients, 2011–12. Available online: http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/4364.0.55.007~2011-12~Main%20Features~Non-alcoholic%20beverages~701 (accessed on 15 December 2015).
- Hirshkowitz, M.; Whiton, K.; Albert, S.M.; Alessi, C.; Bruni, O.; DonCarlos, L.; Hazen, N.; Herman, J.; Hillard, P.J.A.; Katz, E.S. National sleep foundation’s updated sleep duration recommendations: Final report. Sleep Health 2015, 1, 233–243. [Google Scholar] [CrossRef]
- Cappuccio, F.P.; D’Elia, L.; Strazzullo, P.; Miller, M.A. Quantity and quality of sleep and incidence of type 2 diabetes a systematic review and meta-analysis. Diabetes Care 2010, 33, 414–420. [Google Scholar] [CrossRef] [PubMed]
- Cappuccio, F.P.; Taggart, F.M.; Kandala, N.; Currie, A.; Peile, E.; Stranges, S.; Miller, M.A. Meta-analysis of short sleep duration and obesity in children and adults. Sleep 2008, 31, 619–626. [Google Scholar] [PubMed]
- Jennings, J.; Muldoon, M.; Hall, M. Self-reported sleep quality is associated with the metabolic syndrome. Sleep 2007, 30, 219–223. [Google Scholar] [PubMed]
- Xie, L.; Kang, H.; Xu, Q.; Chen, M.J.; Liao, Y.; Thiyagarajan, M.; O’Donnell, J.; Christensen, D.J.; Nicholson, C.; Iliff, J.J. Sleep drives metabolite clearance from the adult brain. Science 2013, 342, 373–377. [Google Scholar] [CrossRef] [PubMed]
- Shilo, L.; Sabbah, H.; Hadari, R.; Kovatz, S.; Weinberg, U.; Dolev, S.; Dagan, Y.; Shenkman, L. The effects of coffee consumption on sleep and melatonin secretion. Sleep Med. 2002, 3, 271–273. [Google Scholar] [CrossRef]
- Drapeau, C.; Hamel-Hebert, I.; Robillard, R.; Selmaoui, B.; Filipini, D.; Carrier, J. Challenging sleep in aging: The effects of 200 mg of caffeine during the evening in young and middle-aged moderate caffeine consumers. J. Sleep Res. 2006, 15, 133–141. [Google Scholar] [CrossRef] [PubMed]
- Carrier, J.; Fernandez-Bolanos, M.; Robillard, R.; Dumont, M.; Paquet, J.; Selmaoui, B.; Filipini, D. Effects of caffeine are more marked on daytime recovery sleep than on nocturnal sleep. Neuropsychopharmacology 2007, 32, 964–972. [Google Scholar] [CrossRef] [PubMed]
- Hindmarch, I.; Rigney, U.; Stanley, N.; Quinlan, P.; Rycroft, J.; Lane, J. A naturalistic investigation of the effects of day-long consumption of tea, coffee and water on alertness, sleep onset and sleep quality. Psychopharmacology 2000, 149, 203–216. [Google Scholar] [CrossRef] [PubMed]
- Grant, D.M.; Tang, B.K.; Kalow, W. Variability in caffeine metabolism. Clin. Pharmacol. Ther. 1983, 33, 591–602. [Google Scholar] [CrossRef] [PubMed]
- Regestein, Q.; Natarajan, V.; Pavlova, M.; Kawasaki, S.; Gleason, R.; Koff, E. Sleep debt and depression in female college students. Psychiatry Res. 2010, 176, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Ortuno, M.; Moore, N.; Taillard, J.; Valtat, C.; Leger, D.; Bioulac, B.; Philip, P. Sleep duration and caffeine consumption in a French middle-aged working population. Sleep Med. 2005, 6, 247–251. [Google Scholar] [CrossRef] [PubMed]
- Lund, H.G.; Reider, B.D.; Whiting, A.B.; Prichard, J. Sleep patterns and predictors of disturbed sleep in a large population of college students. J. Adolesc. Health 2010, 46, 124–132. [Google Scholar] [CrossRef] [PubMed]
- Zunhammer, M.; Eichhammer, P.; Busch, V. Sleep quality during exam stress: The role of alcohol, caffeine and nicotine. PLoS ONE 2014, 9, e109490. [Google Scholar] [CrossRef] [PubMed]
- Whittier, A.; Sanchez, S.; Castaneda, B.; Sanchez, E.; Gelaye, B.; Yanez, D.; Williams, M.A. Eveningness chronotype, daytime sleepiness, caffeine consumption, and use of other stimulants among Peruvian university students. J. Caffeine Res. 2014, 4, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Kant, A.K.; Graubard, B.I. Association of self-reported sleep duration with eating behaviors of American adults: NHANES 2005–2010. Am. J. Clin. Nutr. 2014, 100, 938–947. [Google Scholar] [CrossRef] [PubMed]
- Reid, A.; Baker, F.C. Perceived sleep quality and sleepiness in South African university students. S. Afr. J. Psychol. 2008, 38, 287–303. [Google Scholar] [CrossRef]
- Brick, C.A.; Seely, D.L.; Palermo, T.M. Association between sleep hygiene and sleep quality in medical students. Behav. Sleep Med. 2010, 8, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Watson, E.; Kohler, M.; Banks, S.; Coates, A. Development of an Australian caffeine food frequency questionnaire. Nutrients 2016. under review. [Google Scholar]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Cole, J.C.; Motivala, S.J.; Buysse, D.J.; Oxman, M.N.; Levin, M.J.; Irwin, M.R. Validation of a 3-factor scoring model for the Pittsburgh sleep quality index in older adults. Sleep 2006, 29, 112–116. [Google Scholar] [PubMed]
- Backhaus, J.; Junghanns, K.; Broocks, A.; Riemann, D.; Hohagen, F. Test–retest reliability and validity of the Pittsburgh sleep quality index in primary insomnia. J. Psychosom. Res. 2002, 53, 737–740. [Google Scholar] [CrossRef]
- Armitage, R.; Trivedi, M.; Hoffmann, R.; Rush, A.J. Relationship between objective and subjective sleep measures in depressed patients and healthy controls. Depression Anxiety 1997, 5, 97–102. [Google Scholar] [CrossRef]
- Zinkhan, M.; Berger, K.; Hense, S.; Nagel, M.; Obst, A.; Koch, B.; Penzel, T.; Fietze, I.; Ahrens, W.; Young, P. Agreement of different methods for assessing sleep characteristics: A comparison of two actigraphs, wrist and hip placement, and self-report with polysomnography. Sleep Med. 2014, 15, 1107–1114. [Google Scholar] [CrossRef] [PubMed]


| Mean (SD) | Median (IQR) | Range | |
|---|---|---|---|
| Total caffeine (mg) | 165.1 (105.3) | 133.4 (120.1) | 41.6–726.6 |
| Coffee (mg) | 109.9 (99.4) | 87.2 (82.3) | 0.0–646.6 |
| Tea (mg) | 38.0 (56.2) | 13.6 (50.9) | 0.0–271.4 |
| Chocolate (mg) | 3.5 (4.6) | 1.7 (4.3) | 0.0–20.6 |
| Soft Drink (mg) | 9.0 (24.0) | 0.0 (8.6) | 0.0–182.4 |
| Energy drink (mg) | 4.9 (20.4) | 0.0 (0.0) | 0.0–135.0 |
| PSQI global score | 5.3 (2.5) | 5.0 (4.0) | 0.0–21.0 |
| SOL (min) | 18.8 (11.8) | 20.0 (20.0) | 1.0–60.0 |
| SE (%) | 88.3 (9.3) | 89.1 (13.7) | 55.6–100.0 |
| TIB (h) | 8.0 (1.0) | 8.0 (1.0) | 6.0–13.3 |
| Good Sleep Quality n = 35 | Poor Sleep Quality n = 45 | p Values | |||
|---|---|---|---|---|---|
| Mean (SD) | Median (IQR) | Mean (SD) | Median (IQR) | ||
| Total caffeine (mg) | 130.0 (62.6) | 123.2 (58.2) | 192.1 (122.5) | 140.4 (160.6) | 0.008 I |
| Coffee (mg) | 81.7 (68.5) | 66.5 (83.1) | 132.2 (115.0) | 99.2 (83.3) | 0.019 M |
| Tea (mg) | 35.4 (48.4) | 13.6 (54.3) | 39.5 (61.5) | 13.6 (55.0) | 0.874 M |
| Chocolate (mg) | 3.6 (4.0) | 1.7 (4.5) | 3.5 (4.9) | 1.7 (4.5) | 0.658 M |
| Soft Drink (mg) | 6.5 (13.2) | 0.0 (5.2) | 10.9 (29.2) | 0.0 (10.4) | 0.368 M |
| Energy drink (mg) | 2.9 (15.4) | 0.0 (0.0) | 6.0 (23.0) | 0.0 (0.0) | 0.395 M |
| SOL (min) | 11.4 (7.6) | 10.0 (13.0) | 24.3 (11.0) | 30.0 (15.0) | 0.000 C |
| SE (%) | 95.0 (4.6) | 94.1 (8.6) | 82.9 (8.8) | 82.4 (11.1) | 0.239 M |
| TIB (h) | 7.9 (0.7) | 8.0 (1.3) | 8.2 (1.2) | 8.0 (1.1) | 0.000 C |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Watson, E.J.; Coates, A.M.; Kohler, M.; Banks, S. Caffeine Consumption and Sleep Quality in Australian Adults. Nutrients 2016, 8, 479. https://doi.org/10.3390/nu8080479
Watson EJ, Coates AM, Kohler M, Banks S. Caffeine Consumption and Sleep Quality in Australian Adults. Nutrients. 2016; 8(8):479. https://doi.org/10.3390/nu8080479
Chicago/Turabian StyleWatson, Emily J., Alison M. Coates, Mark Kohler, and Siobhan Banks. 2016. "Caffeine Consumption and Sleep Quality in Australian Adults" Nutrients 8, no. 8: 479. https://doi.org/10.3390/nu8080479
APA StyleWatson, E. J., Coates, A. M., Kohler, M., & Banks, S. (2016). Caffeine Consumption and Sleep Quality in Australian Adults. Nutrients, 8(8), 479. https://doi.org/10.3390/nu8080479