A Survey of the Thermal Analysis of Implanted Antennas for Wireless Biomedical Devices
Abstract
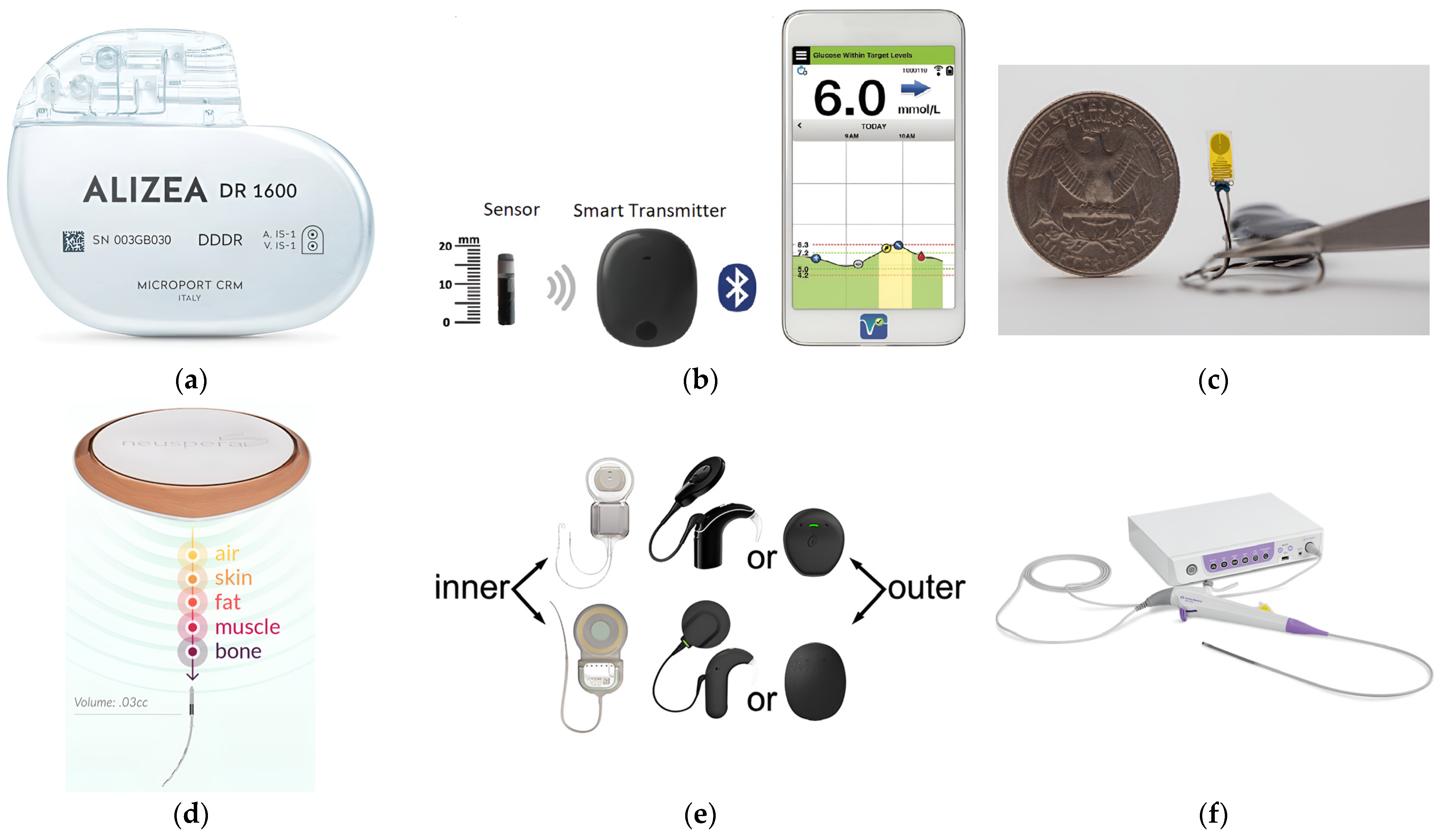
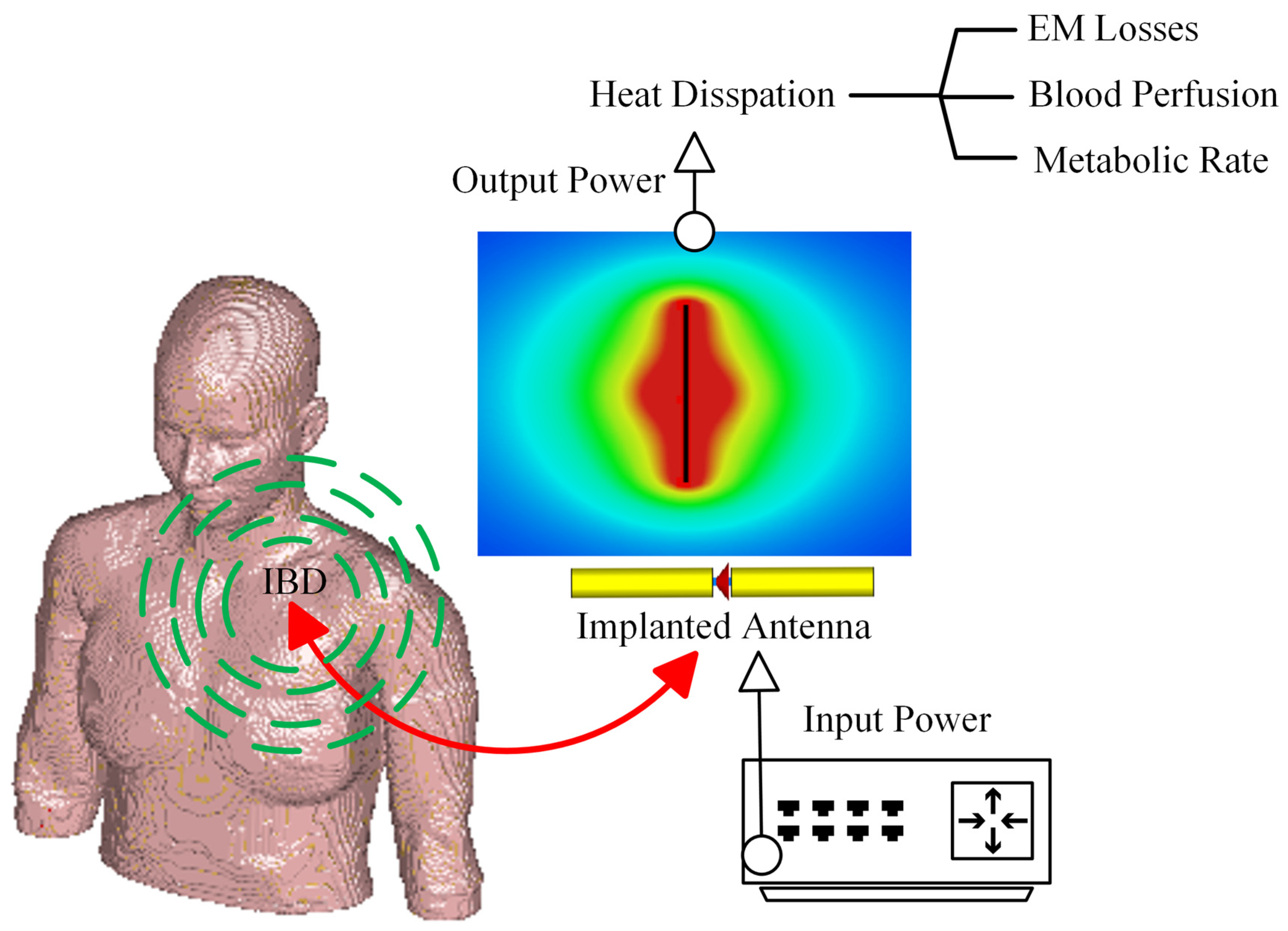
:1. Introduction
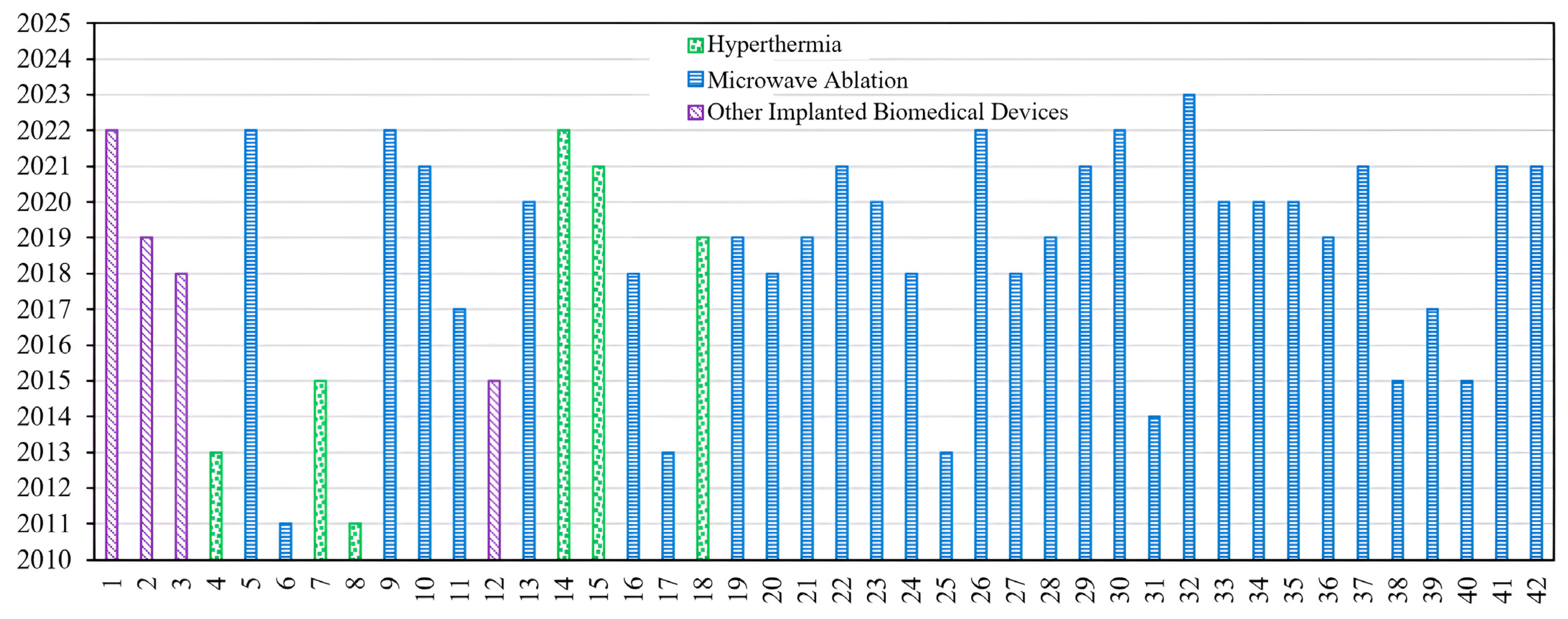
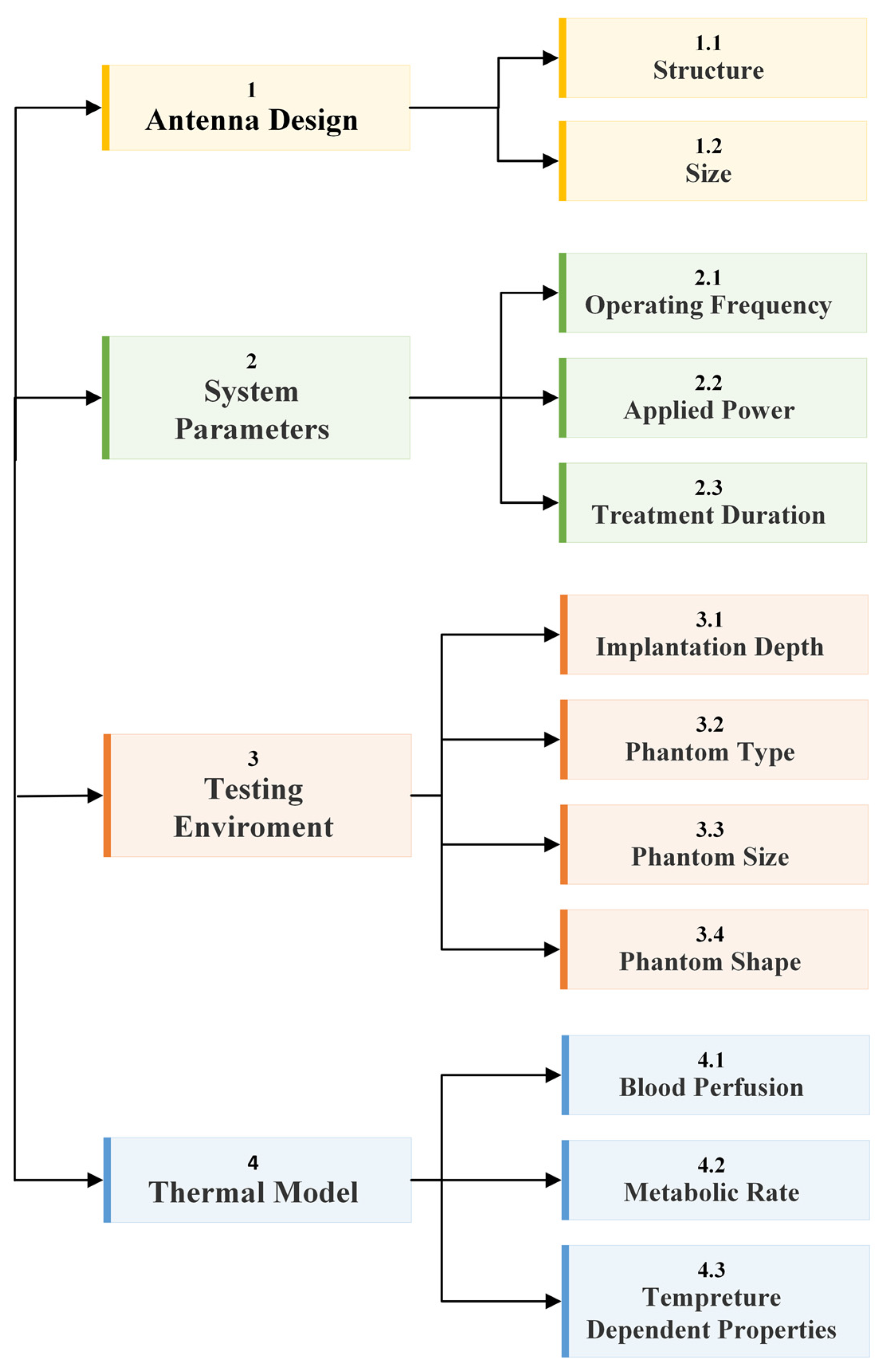
2. Methodology
3. Antenna Parameters
Antenna Size
4. System Parameters
| Frequency Standard | Frequency Range |
|---|---|
| Inductive Implant | <100 kHz |
| Medical Device Radiocommunication (MedRadio) | (401–406) MHz |
| Medical Micropower Networks (MMNs) | (413–457) MHz |
| Medical Body Area Networks (MBANs) | (2.36–2.40) GHz |
| Ultra-Wideband Band (UWB) | (3.1–10.6) GHz |
| Industrial, Scientific, and Medical (ISM) | (433.1–434.8) MHz (868–868.6) MHz (902.8–928) MHz (2.4–2.5) GHz (5.715–5.875) GHz |
| Wireless Medical Telemetry Service Frequency (WMTS) | (608–614) MHz (1.395–1.4) GHz (1.427–1.429) GHz |
| Wi-Fi, Bluetooth, and Zigbee 1 | (902–928) MHz (2.400–2.483) GHz (5.150–5.850) GHz (5.950–7.125) GHz |
| Frequency | Simulation Phantom | Measurement Phantom | |
|---|---|---|---|
| [15] | 2.45 GHz | Complex liver model | NA |
| [17] | NM | Layered model | NA |
| [19] | NM | NA 2 | Porcine muscle |
| [31] | (3.5–4.5) GHz | Voxel model | NA |
| [33] | NM | Breast | NA |
| [35] | 2.45 GHz | Homogeneous tissue | NA |
| [36] | 7.14 GHz | NM 1 | NA 2 |
| [37] | 0.1, 1, and 10 MHz | Tumor and healthy tissues | NA |
| [38] | 2.45 GHz | Torso segment | NA |
| [39] | 2.45 GHz | Liver | NA |
| [40] | (3–7) GHz | Breast | NA |
| [41] | 1.55 GHz and 700 MHz | Simplified leg | NA |
| [42] | 2.45 GHz | NM | Porcine liver |
| [43] | 2.45 GHz | Bone | Porcine bone |
| [44] | (1.9–26) GHz | Porcine muscle and liver | Porcine muscle |
| [45] | 2.45 GHz | Breast | Breast phantom |
| [46] | 434, 650, 915, and 1150 MHz | Head model | NA |
| [47] | 2.45 GHz | Liver | Bovine liver |
| [48] | 10 GHz and 6.4 GHz | Muscle and egg white | Porcine muscle |
| [49] | 915 MHz and 2.45 GHz | NA | Hepatic tumor |
| [50] | 2.45 GHz | Muscle | NA |
| [51] | 1.9, 6.0, 10, 14, and 18 GHz | Liver | Porcine liver |
| [52] | 2.45 GHz | NA | Porcine liver |
| [53] | 2.45 GHz | Lung | Porcine lung |
| [54] | 2.45 GHz | Liver | Porcine liver |
| [55] | 2.45 GHz and 6 GHz | Tumor | NA |
| [56] | 2.45 GHz | Liver | Porcine liver |
| [58] | NM | NA | Egg yolk and porcine lung |
| [59] | 2.45 GHz | Liver | Bovine liver |
| [60] | 2.45 GHz and 5.8 GHz | Layered tissue model | Bovine liver and adrenal |
| [61] | 1.9 GHz | Liver and egg white | Liver |
| [62] | 2.45 GHz | Liver, lung, kidney, and bone | NA |
| [63] | 10 GHz and 1.9 GHz | Liver | Bovine liver |
| [64] | 2.45 GHz | Liver | NA |
| [66] | 5 GHz | Homogeneous tissue | NA |
| [67] | 2.45 GHz and 915 MHz | Liver | Porcine muscle |
| [68] | 433 MHz | Liver | Porcine liver |
| [69] | 2.45 GHz | Liver | NA |
4.1. Operating Frequency
4.2. Applied Power
4.3. Operating Frequency, Applied Power, and Treatment Time
5. Testing Environment Parameters
5.1. Implantation Depth
5.2. Phantom Type
5.3. Phantom Size
5.4. Phantom Shape
6. Thermal Model Parameter
6.1. Blood Perfusion and Metabolic Rate
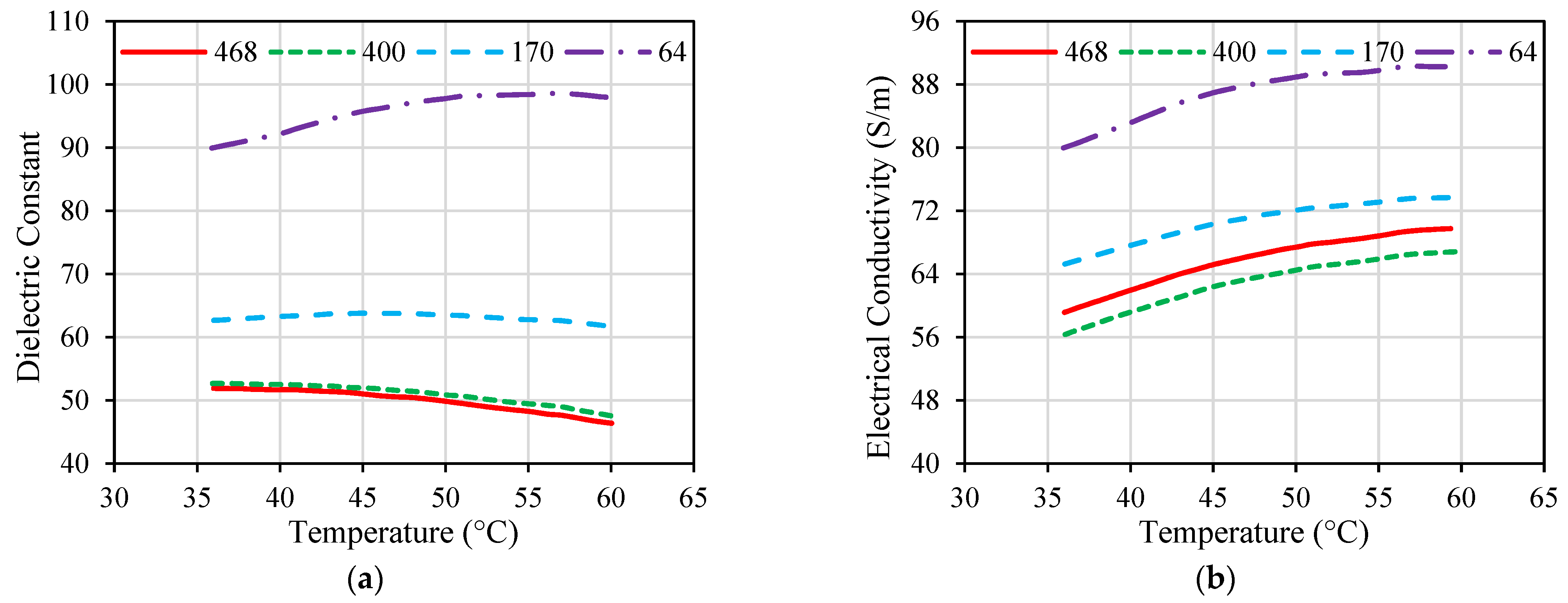
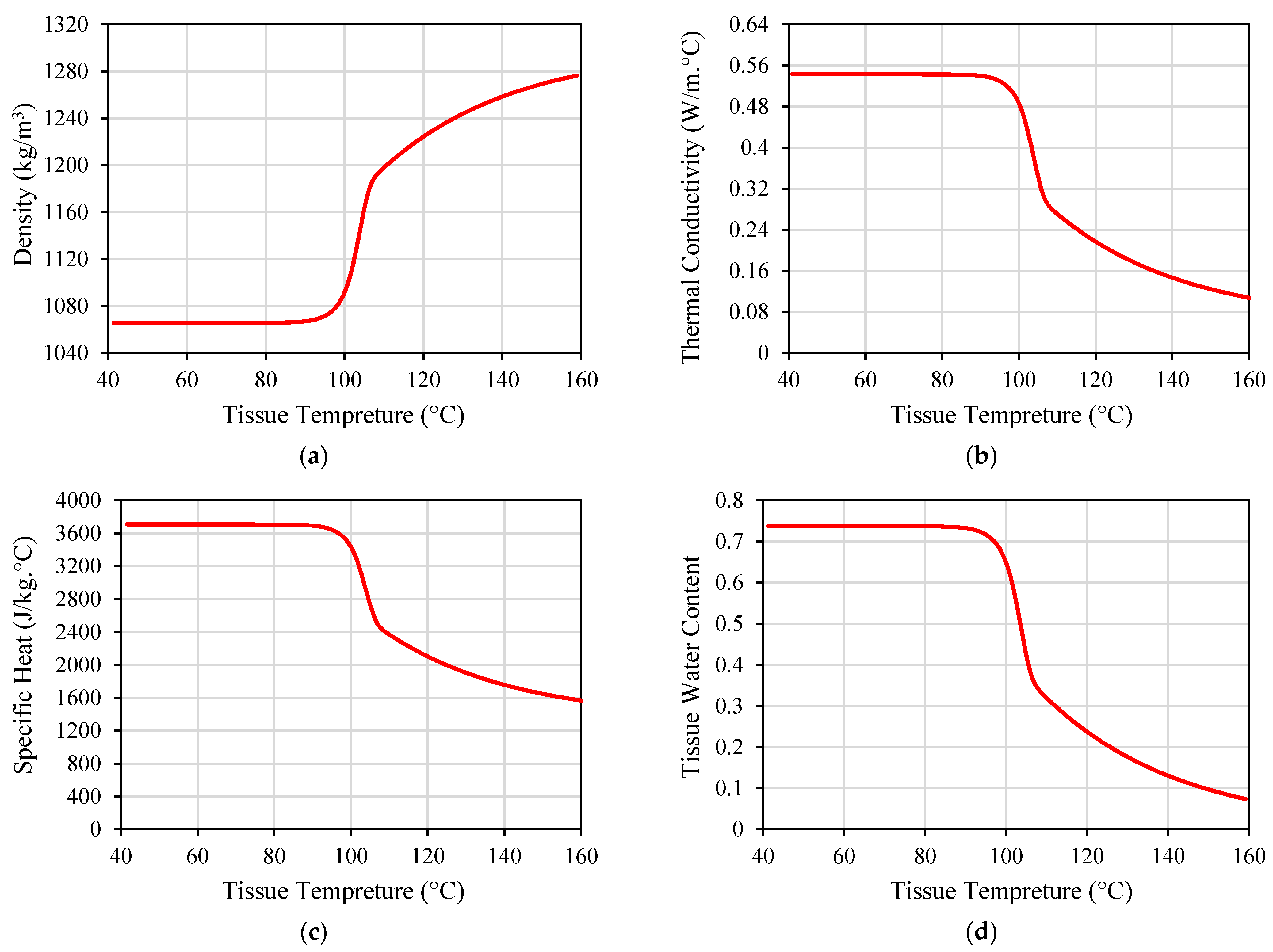
6.2. Temperature-Dependent Tissue Properties
7. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Li, P.; Lee, G.H.; Kim, S.Y.; Kwon, S.Y.; Kim, H.R.; Park, S. From Diagnosis to Treatment: Recent Advances in Patient-Friendly Biosensors and Implantable Devices. ACS Nano 2021, 15, 1960–2004. [Google Scholar] [CrossRef] [PubMed]
- Alemaryeen, A. Compact Wideband Antenna for Wireless Capsule Endoscopy System. Appl. Phys. A Mater. Sci. Process. 2021, 127, 271. [Google Scholar] [CrossRef]
- Joo, H.; Lee, Y.; Kim, J.; Yoo, J.S.; Yoo, S.; Kim, S.; Arya, A.K.; Kim, S.; Choi, S.H.; Lu, N.; et al. Soft Implantable Drug Delivery Device Integrated Wirelessly with Wearable Devices to Treat Fatal Seizures. Sci. Adv. 2021, 7, eabd4639. [Google Scholar] [CrossRef] [PubMed]
- Sharma, D.; Kanaujia, B.K.; Kaim, V.; Mittra, R.; Arya, R.K.; Matekovits, L. Design and Implementation of Compact Dual-Band Conformal Antenna for Leadless Cardiac Pacemaker System. Sci. Rep. 2022, 12, 3165. [Google Scholar] [CrossRef] [PubMed]
- Satish; Sen, K.; Anand, S. Demonstration of Microstrip Sensor for the Feasibility Study of Non-Invasive Blood-Glucose Sensing. Mapan—J. Metrol. Soc. India 2021, 36, 193–199. [Google Scholar] [CrossRef]
- Zhang, Y.; Liu, C.; Zhang, K.; Cao, H.; Liu, X. Design and In-Vivo Testing of a Low-Cost Miniaturized Capsule System for Body Temperature Monitoring. Int. J. RF Microw. Comput. Eng. 2019, 29, e21793. [Google Scholar] [CrossRef]
- Cehajic Kapetanovic, J.; Troelenberg, N.; Edwards, T.L.; Xue, K.; Ramsden, J.D.; Stett, A.; Zrenner, E.; MacLaren, R.E. Highest Reported Visual Acuity after Electronic Retinal Implantation. Acta Ophthalmol. 2020, 98, 736–740. [Google Scholar] [CrossRef] [PubMed]
- Hayat, S.; Shah, S.A.A.; Yoo, H. Miniaturized Dual-Band Circularly Polarized Implantable Antenna for Capsule Endoscopic System. IEEE Trans. Antennas Propag. 2021, 69, 1885–1895. [Google Scholar] [CrossRef]
- Healey, T.T.; March, B.T.; Baird, G.; Dupuy, D.E. Microwave Ablation for Lung Neoplasms: A Retrospective Analysis of Long-Term Results. J. Vasc. Interv. Radiol. 2017, 28, 206–211. [Google Scholar] [CrossRef]
- Izzo, F.; Granata, V.; Grassi, R.; Fusco, R.; Palaia, R.; Delrio, P.; Carrafiello, G.; Azoulay, D.; Petrillo, A.; Curley, S.A. Radiofrequency Ablation and Microwave Ablation in Liver Tumors: An Update. Oncologist 2019, 24, e990–e1005. [Google Scholar] [CrossRef]
- Zhou, W.; Zha, X.; Liu, X.; Ding, Q.; Chen, L.; Ni, Y.; Zhang, Y.; Xu, Y.; Chen, L.; Zhao, Y.; et al. US-Guided Percutaneous Microwave Coagulation of Small Breast Cancers: A Clinical Study. Radiology 2012, 263, 364–373. [Google Scholar] [CrossRef] [PubMed]
- Geyikoglu, M.D.; Cavusoglu, B. Non-Invasive Microwave Hyperthermia for Bone Cancer Treatment Using Realistic Bone Models and Flexible Antenna Arrays. Electromagn. Biol. Med. 2021, 40, 353–360. [Google Scholar] [CrossRef] [PubMed]
- Albarqi, H.A.; Demessie, A.A.; Sabei, F.Y.; Moses, A.S.; Hansen, M.N.; Dhagat, P.; Taratula, O.R.; Taratula, O. Systemically Delivered Magnetic Hyperthermia for Prostate Cancer Treatment. Pharmaceutics 2020, 12, 1020. [Google Scholar] [CrossRef] [PubMed]
- ATEŞ, Ö.F. Effectiveness and Reliability of Percutaneous Microwave Ablation Therapy in Early Stage Renal Cell Cancer: Intermediate Term Results. J. Surg. Med. 2020, 4, 1068–1072. [Google Scholar] [CrossRef]
- Shamekhi, L.; Sayehvand, H.O.; Karami, H. Tumour Shape-Dependent Microwave Hyperthermia Using a Novel Coaxial Micro-Cut Slot Antenna. J. Therm. Biol. 2020, 88, 102473. [Google Scholar] [CrossRef] [PubMed]
- Peng, T.; O’Neill, D.P.; Payne, S.J. A Two-Equation Coupled System for Determination of Liver Tissue Temperature during Thermal Ablation. Int. J. Heat Mass Transf. 2011, 54, 2100–2109. [Google Scholar] [CrossRef]
- Celik, N.; Turgut, E.; Bayazit, Y. Design Analysis of an Implant and Antenna System by Using Taguchi Method. Heat Mass Transf. 2018, 54, 403–413. [Google Scholar] [CrossRef]
- Kim, J.H.; Lee, J.K.; Kim, H.G.; Kim, K.B.; Kim, H.R. Possible Effects of Radiofrequency Electromagnetic Field Exposure on Central Nerve System. Biomol. Ther. 2019, 27, 265–275. [Google Scholar] [CrossRef]
- Martinsen, T.; Pettersen, F.J.; Kalvøy, H.; Tronstad, C.; Kvarstein, G.; Bakken, A.; Høgetveit, J.O.; Martinsen, Ø.G.; Grimnes, S.; Frich, L. Electrosurgery and Temperature Increase in Tissue with a Passive Metal Implant. Front. Surg. 2019, 6, 8. [Google Scholar] [CrossRef]
- Alizea Pacemaker System, USA. Available online: https://www.medicaldevice-network.com/projects/alizea-pacemaker-system-usa/ (accessed on 15 September 2023).
- Tardo, A.M.; Irace, C.; Del Baldo, F.; Foglia, A.; Fracassi, F. Clinical Use of a 180-Day Implantable Glucose Monitoring System in Dogs with Diabetes Mellitus: A Case Series. Animals 2022, 12, 860. [Google Scholar] [CrossRef]
- Implanted Tempreture Sensor. Available online: https://medicalxpress.com/news/2023-09-device-transplanted-early.html (accessed on 15 September 2023).
- Neurostimulation Therapy Implant. Available online: https://neuspera.com/technology/ (accessed on 15 September 2023).
- Hearing Aids. Available online: https://www.cochlearimplants.co.za/learn-about-cochlear-implants/ (accessed on 15 September 2023).
- Imaging Device. Available online: https://www.med-technews.com/medtech-insights/latest-medtech-insights/state-of-the-art-endoscopy-and-imaging-scivita-medical-s-g/ (accessed on 15 September 2023).
- IEEE. IEEE Standard for Safety Levels With Respect to Human Exposure to Radio Frequency Electromagnetic Fields, 3 KHz to 300 GHz; IEEE: New York, NY, USA, 2006; Volume 2005. [Google Scholar]
- Ahlbom, A.; Bergqvist, U.; Bernhardt, J.H.; Cesarini, J.P.; Court, L.A.; Grandolfo, M.; Hietanen, M.; McKinlay, A.F.; Repacholi, M.H.; Sliney, D.H.; et al. Guidelines for Limiting Exposure to Time-Varying Electric, Magnetic, and Electromagnetic Fields (up to 300 GHz). Health Phys. 1998, 74, 494–521. [Google Scholar]
- Das, S.; Mitra, D.; Chezhian, A.S.; Mandal, B.; Augustine, R. A Novel SAR Reduction Technique for Implantable Antenna Using Conformal Absorber Metasurface. Front. Med. Technol. 2022, 4, 924433. [Google Scholar] [CrossRef] [PubMed]
- Bhargava, D.; Rattanadecho, P.; Wessapan, T. The Effect of Metal Objects on the SAR and Temperature Increase in the Human Head Exposed to Dipole Antenna (Numerical Analysis). Case Stud. Therm. Eng. 2020, 22, 100789. [Google Scholar] [CrossRef]
- Karthik, V.; Rao, T.R. SAR Investigations on the Exposure Compliance of Wearable Wireless Devices Using Infrared Thermography. Bioelectromagnetics 2018, 39, 451–459. [Google Scholar] [CrossRef] [PubMed]
- Thotahewa, K.M.S.; Redoute, J.-M.; Yuce, M.R. Propagation, Power Absorption, and Temperature Analysis of UWB Wireless Capsule Endoscopy Devices Operating in the Human Body. IEEE Trans. Microw. Theory Tech. 2015, 63, 3823–3833. [Google Scholar] [CrossRef]
- Guido, K.; Kiourti, A. Wireless Wearables and Implants: A Dosimetry Review. Bioelectromagnetics 2020, 41, 3–20. [Google Scholar] [CrossRef] [PubMed]
- Kumar, J.; Repaka, R. Numerical Investigation on the Effect of Different Physiological Cancerous Breast Parameters on the Output of Microwave Ablation. ASME J. Med. Diagn. 2020, 3, 031001. [Google Scholar] [CrossRef]
- Lazzi, G. Thermal Effects of Bioimplants. IEEE Eng. Med. Biol. Mag. 2005, 24, 75–81. [Google Scholar] [CrossRef]
- Singh, S.; Repaka, R.; Al-Jumaily, A. Sensitivity Analysis of Critical Parameters Affecting the Efficacy of Microwave Ablation Using Taguchi Method. Int. J. RF Microw. Comput. Eng. 2019, 29, e21581. [Google Scholar] [CrossRef]
- Sloos, T.; Rustand, B.; Liu, X.; Keegan, C.; Sourki, R.; Milani, A.S. A Multi-Criteria Decision Analysis of Implanted Biomedical Device Antenna: Electro-Thermal Simulation, Design, and Data Analysis. Simulation 2022, 98, 863–873. [Google Scholar] [CrossRef]
- Jamil, M.; Yin-Kwee Ng, E. Ranking of Parameters in Bioheat Transfer Using Taguchi Analysis. Int. J. Therm. Sci. 2013, 63, 15–21. [Google Scholar] [CrossRef]
- Gorman, J.; Tan, W.; Abraham, J. Numerical Simulation of Microwave Ablation in the Human Liver. Processes 2022, 10, 361. [Google Scholar] [CrossRef]
- Keangin, P.; Rattanadecho, P.; Wessapan, T. An Analysis of Heat Transfer in Liver Tissue during Microwave Ablation Using Single and Double Slot Antenna. Int. Commun. Heat Mass Transf. 2011, 38, 757–766. [Google Scholar] [CrossRef]
- Nguyen, P.T.; Abbosh, A.; Crozier, S. Microwave Hyperthermia for Breast Cancer Treatment Using Electromagnetic and Thermal Focusing Tested on Realistic Breast Models and Antenna Arrays. IEEE Trans. Antennas Propag. 2015, 63, 4426–4434. [Google Scholar] [CrossRef]
- Işik, Ö.; Korkmaz, E.; Türetken, B. Antenna Arrangement Considerations for Microwave Hyperthermia Applications. In Proceedings of the 2011 30th URSI General Assembly and Scientific Symposium (URSIGASS), Istanbul, Turkey, 13–20 August 2011. [Google Scholar] [CrossRef]
- Wang, J.; Huang, S.; Gao, H.; Liu, J.; Zhang, Y.; Wu, S. Computer Simulations of Dual-Antenna Microwave Ablation and Comparison to Experimental Measurements. Appl. Sci. 2022, 13, 26. [Google Scholar] [CrossRef]
- Jessica Trujillo-Romero, C.; Leija-Salas, L.; Vera-Hernández, A.; Rico-Martínez, G.; Gutiérrez-Martínez, J. Double Slot Antenna for Microwave Thermal Ablation to Treat Bone Tumors: Modeling and Experimental Evaluation. Electronics 2021, 10, 761. [Google Scholar] [CrossRef]
- Sawicki, J.F.; Shea, J.D.; Behdad, N.; Hagness, S.C. The Impact of Frequency on the Performance of Microwave Ablation. Int. J. Hyperth. 2017, 33, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Ortega-Palacios, R.; Trujillo-Romero, C.J.; Cepeda-Rubio, M.F.J.; Leija, L.; Vera Hernández, A. Heat Transfer Study in Breast Tumor Phantom during Microwave Ablation: Modeling and Experimental Results for Three Different Antennas. Electronics 2020, 9, 535. [Google Scholar] [CrossRef]
- Redr, J.; Pokorny, T.; Drizdal, T.; Fiser, O.; Brunat, M.; Vrba, J.; Vrba, D. Microwave Hyperthermia of Brain Tumors: A 2D Assessment Parametric Numerical Study. Sensors 2022, 22, 6115. [Google Scholar] [CrossRef]
- Ibitoye, A.Z.; Bose Adedokun, M.; Nwoye, E.; Ogese, O.C.; Adedokun, M.B.; Habeebu, M.Y.; Nwoye, E.O.; Aweda, A.M. Evaluation of the Performance of Designed Coaxial Antennas for Hyperthermia Using Simulation and Experimental Methods. Pol. J. Med. Phys. Eng. 2021, 27, 109–117. [Google Scholar] [CrossRef]
- Mohtashami, Y.; Luyen, H.; Hagness, S.C.; Behdad, N. Non-Coaxial-Based Microwave Ablation Antennas for Creating Symmetric and Asymmetric Coagulation Zones. J. Appl. Phys. 2018, 123, 214903. [Google Scholar] [CrossRef]
- Simo, K.A.; Tsirline, V.B.; Sindram, D.; McMillan, M.T.; Thompson, K.J.; Swan, R.Z.; McKillop, I.H.; Martinie, J.B.; Iannitti, D.A. Microwave Ablation Using 915-MHz and 2.45-GHz Systems: What Are the Differences? HPB 2013, 15, 991–996. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Singh, S.P.; Singh, D. Compact Conformal Multilayer Slot Antenna for Hyperthermia. In Proceedings of the 2019 URSI Asia-Pacific Radio Science Conference, AP-RASC 2019, New Delhi, India, 9–15 March 2019. [Google Scholar]
- Sawicki, J.F.; Luyen, H.; Mohtashami, Y.; Shea, J.D.; Behdad, N.; Hagness, S.C. The Performance of Higher Frequency Microwave Ablation in the Presence of Perfusion. IEEE Trans. Biomed. Eng. 2019, 66, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Scapaticci, R.; Lopresto, V.; Pinto, R.; Cavagnaro, M.; Crocco, L. Monitoring Thermal Ablation via Microwave Tomography: An Ex Vivo Experimental Assessment. Diagnostics 2018, 8, 81. [Google Scholar] [CrossRef] [PubMed]
- Gao, X.; Tian, Z.; Cheng, Y.; Geng, B.; Chen, S.; Nan, Q. Experimental and Numerical Study of Microwave Ablation on Ex-Vivo Porcine Lung. Electromagn. Biol. Med. 2019, 38, 249–261. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Wu, S.; Wu, Z.; Gao, H.; Huang, S. Influences of Blood Flow Parameters on Temperature Distribution during Liver Tumor Microwave Ablation. Front. Biosci. Landmark 2021, 26, 504–516. [Google Scholar] [CrossRef]
- Tehrani, M.H.H.; Soltaniid, M.; Soltaniid, M.; Soltaniid, M.; Soltaniid, M.; Soltaniid, M.; Kashkooli, F.M.; Raahemifar, K.; Raahemifar, K.; Raahemifar, K. Use of Microwave Ablation for Thermal Treatment of Solid Tumors with Different Shapes and Sizes-A Computational Approach. PLoS ONE 2020, 15, e0233219. [Google Scholar] [CrossRef] [PubMed]
- Ibitoye, A.Z.; Orotoye, T.; Nwoye, E.O.; Aweda, M.A. Analysis of Efficiency of Different Antennas for Microwave Ablation Using Simulation and Experimental Methods. Egypt. J. Basic Appl. Sci. 2018, 5, 24–30. [Google Scholar] [CrossRef]
- Karampatzakis, A.; Kühn, S.; Tsanidis, G.; Neufeld, E.; Samaras, T.; Kuster, N. Antenna Design and Tissue Parameters Considerations for an Improved Modelling of Microwave Ablation in the Liver. Phys. Med. Biol. 2013, 58, 3191–3206. [Google Scholar] [CrossRef]
- Cai, H.; Tian, H.; Wei, Z.; Ye, X. Microwave Ablation of the Lung: Comparison of 19G with 14G and 16G Microwave Antennas in Ex Vivo Porcine Lung. J. Cancer Res. Ther. 2022, 18, 1876–1883. [Google Scholar] [CrossRef]
- Etoz, S.; Brace, C.L. Analysis of Microwave Ablation Antenna Optimization Techniques. Int. J. RF Microw. Comput. Eng. 2018, 28, e21224. [Google Scholar] [CrossRef]
- Fallahi, H.; Clausing, D.; Shahzad, A.; O’halloran, M.; Dennedy, M.C.; Prakash, P. Microwave Antennas for Thermal Ablation of Benign Adrenal Adenomas. Biomed. Phys. Eng. Express 2019, 5, 25044. [Google Scholar] [CrossRef]
- Mohtashami, Y.; Behdad, N.; Hagness, S.C. Ex Vivo Performance of a Flexible Microwave Ablation Antenna. IEEE Trans. Biomed. Eng. 2021, 68, 1680–1689. [Google Scholar] [CrossRef] [PubMed]
- Radmilović-Radjenović, M.; Radjenović, D.; Radjenović, B. Finite Element Analysis of the Effect of Microwave Ablation on the Liver, Lung, Kidney, and Bone Malignant Tissues. EPL 2022, 136, 28001. [Google Scholar] [CrossRef]
- Luyen, H.; Gao, F.; Hagness, S.C.; Behdad, N. Microwave Ablation at 10.0 GHz Achieves Comparable Ablation Zones to 1.9 GHz in Ex Vivo Bovine Liver. IEEE Trans. Biomed. Eng. 2014, 61, 1702–1710. [Google Scholar] [CrossRef] [PubMed]
- Kernot, D.; Yang, J.; Williams, N.; Thomas, T.; Ledger, P.; Arora, H.; van Loon, R. Transient Changes during Microwave Ablation Simulation: A Comparative Shape Analysis. Biomech. Model. Mechanobiol. 2023, 22, 271–280. [Google Scholar] [CrossRef] [PubMed]
- Selmi, M.; Bin Dukhyil, A.A.; Belmabrouk, H. Numerical Analysis of Human Cancer Therapy Using Microwave Ablation. Appl. Sci. 2020, 10, 211. [Google Scholar] [CrossRef]
- Singh, S.K.; Yadav, A.N. Design of a Novel Externally-Tapped Intertwining Helical Antenna for Microwave Ablation and Its Statistical Analysis on Tissue Model. Int. J. RF Microw. Comput. Eng. 2021, 31, e22905. [Google Scholar] [CrossRef]
- Curto, S.; Taj-Eldin, M.; Fairchild, D.; Prakash, P. Microwave Ablation at 915 MHz vs 2.45 GHz: A Theoretical and Experimental Investigation. Med. Phys. 2015, 42, 6152–6161. [Google Scholar] [CrossRef]
- Jiang, Y.; Zhao, J.; Li, W.; Yang, Y.; Liu, J.; Qian, Z. A Coaxial Slot Antenna with Frequency of 433 MHz for Microwave Ablation Therapies: Design, Simulation, and Experimental Research. Med. Biol. Eng. Comput. 2017, 55, 2027–2036. [Google Scholar] [CrossRef]
- Wang, T.; Zhao, G.; Qiu, B. Theoretical Evaluation of the Treatment Effectiveness of a Novel Coaxial Multi-Slot Antenna for Conformal Microwave Ablation of Tumors. Int. J. Heat Mass Transf. 2015, 90, 81–91. [Google Scholar] [CrossRef]
- Marin, M.; Hobiny, A.; Abbas, I. Finite Element Analysis of Nonlinear Bioheat Model in Skin Tissue Due to External Thermal Sources. Mathematics 2021, 9, 1459. [Google Scholar] [CrossRef]
- Andreozzi, A.; Brunese, L.; Iasiello, M.; Tucci, C.; Vanoli, G.P. Numerical Investigation of a Thermal Ablation Porous Media-Based Model for Tumoral Tissue with Variable Porosity. Computation 2021, 9, 50. [Google Scholar] [CrossRef]
- Converse, M.; Bond, E.J.; Van Veen, B.D.; Hagness, S.C. A Computational Study of Ultra-Wideband versus Narrowband Microwave Hyperthermia for Breast Cancer Treatment. IEEE Trans. Microw. Theory Tech. 2006, 54, 2169–2180. [Google Scholar] [CrossRef]
- Zastrow, E.; Hagness, S.C.; Van Veen, B.D.; Medow, J.E. Time-Multiplexed Beamforming for Noninvasive Microwave Hyperthermia Treatment. IEEE Trans. Biomed. Eng. 2011, 58, 1574–1584. [Google Scholar] [CrossRef]
- Brace, C. Thermal Tumor Ablation in Clinical Use. IEEE Pulse 2011, 2, 28–38. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.; Son, T. Helical Slot Antenna for the Microwave Ablation. Int. J. Antennas Propag. 2019, 2019, 2126879. [Google Scholar] [CrossRef]
- Pfannenstiel, A.; Keast, T.; Kramer, S.; Wibowo, H.; Prakash, P. Flexible Microwave Ablation Applicator for the Treatment of Pulmonary Malignancies. In Proceedings of the Energy-Based Treatment of Tissue and Assessment IX, San Francisco, CA, USA, 29–30 January 2017; Volume 10066. [Google Scholar]
- Alexander, E.S.; Healey, T.T.; Martin, D.W.; Dupuy, D.E. Use of Endobronchial Valves for the Treatment of Bronchopleural Fistulas after Thermal Ablation of Lung Neoplasms. J. Vasc. Interv. Radiol. 2012, 23, 1236–1240. [Google Scholar] [CrossRef]
- Bui, J.T.; Gaba, R.C.; Knuttinen, M.G.; Omene, B.O.; Shon, A.; Martinez, B.K.; Owens, C.A. Microwave Lung Ablation Complicated by Bronchocutaneous Fistula: Case Report and Literature Review. Semin. Intervent. Radiol. 2011, 28, 152–155. [Google Scholar] [CrossRef]
- Soliman, M.M.; Chowdhury, M.E.H.; Khandakar, A.; Islam, M.T.; Qiblawey, Y.; Musharavati, F.; Nezhad, E.Z. Review on Medical Implantable Antenna Technology and Imminent Research Challenges. Sensors 2021, 21, 3163. [Google Scholar] [CrossRef]
- Padma, S.; Martinie, J.B.; Iannitti, D.A. Liver Tumor Ablation: Percutaneous and Open Approaches. J. Surg. Oncol. 2009, 100, 619–634. [Google Scholar] [CrossRef] [PubMed]
- Martin, R.C.G.; Scoggins, C.R.; McMasters, K.M. Safety and Efficacy of Microwave Ablation of Hepatic Tumors: A Prospective Review of a 5-Year Experience. Ann. Surg. Oncol. 2010, 17, 171–178. [Google Scholar] [CrossRef]
- Alemaryeen, A.; Noghanian, S. Effect of Thermal Design Considerations of Implanted Antenna on Tissue Heating. In Proceedings of the 2023 International Applied Computational Electromagnetics Society Symposium (ACES), Monterey, CA, USA, 26–30 March 2023. [Google Scholar] [CrossRef]
- Abaqus-Mechanical and Civil Engineering Simulation. Available online: https://www.3ds.com/products-services/simulia/products/abaqus/ (accessed on 7 August 2023).
- Ansys|Engineering Simulation Software. Available online: https://www.ansys.com/ (accessed on 7 August 2023).
- The COMSOL® Software Product Suite. Available online: https://www.comsol.com/products (accessed on 7 August 2023).
- CST Studio Suite 3D EM Simulation and Analysis Software. Available online: https://www.3ds.com/products-services/simulia/products/cst-studio-suite/ (accessed on 7 August 2023).
- Zastrow, E.; Davis, S.K.; Lazebnik, M. Database of 3D Grid-Based Numerical Breast Phantoms for Use in Computational Electromagnetics Simulations; University of Wisconsin: Madison, WI, USA, 2007. [Google Scholar]
- Huang, H.W. Influence of Blood Vessel on the Thermal Lesion Formation during Radiofrequency Ablation for Liver Tumors. Med. Phys. 2013, 40, 073303. [Google Scholar] [CrossRef] [PubMed]
- Vaidya, N.; Baragona, M.; Lavezzo, V.; Maessen, R.; Veroy, K. Simulation Study of the Cooling Effect of Blood Vessels and Blood Coagulation in Hepatic Radio-Frequency Ablation. Int. J. Hyperth. 2021, 38, 95–104. [Google Scholar] [CrossRef] [PubMed]
- Waterman, F.M.; Tupchong, L.; Nerlinger, R.E.; Matthews, J. Blood Flow in Human Tumors during Local Hyperthermia. Int. J. Radiat. Oncol. Biol. Phys. 1991, 20, 1255–1262. [Google Scholar] [CrossRef] [PubMed]
- Silva, M.; Freitas, B.; Andrade, R.; Espregueira-Mendes, J.; Silva, F.; Carvalho, Ó.; Flores, P. Computational Modelling of the Bioheat Transfer Process in Human Skin Subjected to Direct Heating and/or Cooling Sources: A Systematic Review. Ann. Biomed. Eng. 2020, 48, 1616–1639. [Google Scholar] [CrossRef] [PubMed]
- Pennes, H.H. Analysis of Tissue and Arterial Blood Temperatures in the Resting Human Forearm. J. Appl. Physiol. 1998, 85, 5–34. [Google Scholar] [CrossRef] [PubMed]
- He, X.; Bhowmick, S.; Bischof, J.C. Thermal Therapy in Urologic Systems: A Comparison of Arrhenius and Thermal Isoeffective Dose Models in Predicting Hyperthermic Injury. J. Biomech. Eng. 2009, 131, 074507. [Google Scholar] [CrossRef]
- IT’IS Foundation. Tissue Properties Database; V4.0; IT’IS Foundation: Zurich, Switzerland, 2018. [Google Scholar]
- Duck, F.A. Physical Properties of Tissue. A Comprehensive Reference Book; Elsevier: Amsterdam, The Netherlands, 1990; Volume 18. [Google Scholar]
- Gordon, R.G.; Roemer, R.B.; Horvath, S.M. A Mathematical Model of the Human Temperature Regulatory System–Transient Cold Exposure Response. IEEE Trans. Biomed. Eng. 1976, BME-23, 434–444. [Google Scholar] [CrossRef]
- Fu, F.; Xin, S.X.; Chen, W. Temperature-and Frequency-Dependent Dielectric Properties of Biological Tissues within the Temperature and Frequency Ranges Typically Used for Magnetic Resonance Imaging-Guided Focused Ultrasound Surgery. Int. J. Hyperth. 2014, 30, 56–65. [Google Scholar] [CrossRef]
- Alemaryeen, A. On the Sensitivity of Implantable Antenna Performance to Variations in the Electrical Properties of Body Tissues. In Proceedings of the 2021 International Symposium on Networks, Computers and Communications, ISNCC 2021, Dubai, United Arab Emirates, 31 October–2 November 2021. [Google Scholar]
- Ji, Z.; Brace, C.L. Expanded Modeling of Temperature-Dependent Dielectric Properties for Microwave Thermal Ablation. Phys. Med. Biol. 2011, 56, 5249–5264. [Google Scholar] [CrossRef]
- Cavagnaro, M.; Pinto, R.; Lopresto, V. Numerical Models to Evaluate the Temperature Increase Induced by Ex Vivo Microwave Thermal Ablation. Phys. Med. Biol. 2015, 60, 3287–3311. [Google Scholar] [CrossRef]
- Rattanadecho, P.; Keangin, P. Numerical Study of Heat Transfer and Blood Flow in Two-Layered Porous Liver Tissue during Microwave Ablation Process Using Single and Double Slot Antenna. Int. J. Heat Mass Transf. 2013, 58, 457–470. [Google Scholar] [CrossRef]

| Ref. | Application | Antenna | System Parameters | Testing Environment | Thermal Model | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Structure | Size | Frequency | Power | Time | Implantation Depth | Phantom Type | Phantom Size | Phantom Shape | Blood Perfusion | Metabolic Rate | Temperature Dependent | ||
| 1_[36] | Other IBDs | X | X | ||||||||||
| 2_[19] | Other IBDs | X | X | X | |||||||||
| 3_[17] | Other IBDs | X | X | ||||||||||
| 4_[37] | Hyperthermia | X | X | X | X | X | |||||||
| 5_[38] | Microwave Ablation | X | X | ||||||||||
| 6_[39] | Microwave Ablation | X | X | ||||||||||
| 7_[40] | Hyperthermia | X | X | X | X | ||||||||
| 8_[41] | Hyperthermia | X | X | ||||||||||
| 9_[42] | Microwave Ablation | X | X | X | X | ||||||||
| 10_[43] | Microwave Ablation | X | X | ||||||||||
| 11_[44] | Microwave Ablation | X | X | X | X | X | X | ||||||
| 12_[31] | Other IBDs | X | X | ||||||||||
| 13_[45] | Microwave Ablation | X | X | ||||||||||
| 14_[46] | Hyperthermia | X | X | X | X | ||||||||
| 15_[47] | Hyperthermia | X | X | X | |||||||||
| 16_[48] | Microwave Ablation | X | X | X | |||||||||
| 17_[49] | Microwave Ablation | X | |||||||||||
| 18_[50] | Hyperthermia | X | X | ||||||||||
| 19_[51] | Microwave Ablation | X | X | ||||||||||
| 20_[52] | Microwave Ablation | X | |||||||||||
| 21_[53] | Microwave Ablation | X | X | ||||||||||
| 22_[54] | Microwave Ablation | X | X | X | |||||||||
| 23_[55] | Microwave Ablation | X | X | X | X | X | X | ||||||
| 24_[56] | Microwave Ablation | X | X | X | |||||||||
| 25_[57] | Microwave Ablation | X | X | X | X | X | |||||||
| 26_[58] | Microwave Ablation | X | X | X | |||||||||
| 27_[59] | Microwave Ablation | X | X | ||||||||||
| 28_[60] | Microwave Ablation | X | X | X | X | X | |||||||
| 29_[61] | Microwave Ablation | X | X | X | |||||||||
| 30_[62] | Microwave Ablation | X | X | ||||||||||
| 31_[63] | Microwave Ablation | X | X | X | |||||||||
| 32_[64] | Microwave Ablation | X | X | ||||||||||
| 33_[65] | Microwave Ablation | X | X | X | |||||||||
| 34_[15] | Microwave Ablation | X | X | ||||||||||
| 35_[33] | Microwave Ablation | X | X | X | |||||||||
| 36_[35] | Microwave Ablation | X | X | X | |||||||||
| 37_[66] | Microwave Ablation | X | X | ||||||||||
| 38_[67] | Microwave Ablation | X | X | X | X | ||||||||
| 39_[68] | Microwave Ablation | X | X | ||||||||||
| 40_[69] | Microwave Ablation | X | X | X | |||||||||
| 41_[70] | Hyperthermia | X | X | X | |||||||||
| 42_[71] | Microwave Ablation | X | |||||||||||
| Software | References | Co-analysis Procedure |
|---|---|---|
| Abaqus | [36] | Based on the linear coupling between thermal and electrical elements. Heat generation from the EM analysis influences a heat transfer analysis, determining the temperature distribution. Simultaneously, the temperature distribution impacts the electromagnetic fields via temperature-dependent material properties [83]. |
| ANSYS | [17,38] | Pennes’s equation is implemented utilizing commands of the functions of the parameters within the utility menu of the classical program. ANSYS-Thermal resolves the fundamental heat conduction equation 1 , and then the related blood perfusion term 2 is integrated into the software. Ultimately, the additional function will be employed to generate heat across all regions of the model [84]. |
| COMSOL | [39,42,43,45,46,47,53,54,55,59,60,61,62,66,67] | Mathematical models that involve coupled equations of EM wave propagation and bioheat equation are solved using 2D axisymmetric FEM [39]. The Helmholtz harmonic is employed to compute the EM energy deposition, while Pennes’s bioheat transfer equation is applied to address transient heat transfer within the tissue [85]. |
| CST MWS | [40,41,44,51,63] | The results from the EM simulations, specifically the spatial distribution of the volumetric rate of microwave energy deposition in the tissue and the ohmic losses in the metals serve as the input (i.e., the heat source) for the thermal solver [86]. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alemaryeen, A.; Noghanian, S. A Survey of the Thermal Analysis of Implanted Antennas for Wireless Biomedical Devices. Micromachines 2023, 14, 1894. https://doi.org/10.3390/mi14101894
Alemaryeen A, Noghanian S. A Survey of the Thermal Analysis of Implanted Antennas for Wireless Biomedical Devices. Micromachines. 2023; 14(10):1894. https://doi.org/10.3390/mi14101894
Chicago/Turabian StyleAlemaryeen, Ala, and Sima Noghanian. 2023. "A Survey of the Thermal Analysis of Implanted Antennas for Wireless Biomedical Devices" Micromachines 14, no. 10: 1894. https://doi.org/10.3390/mi14101894







