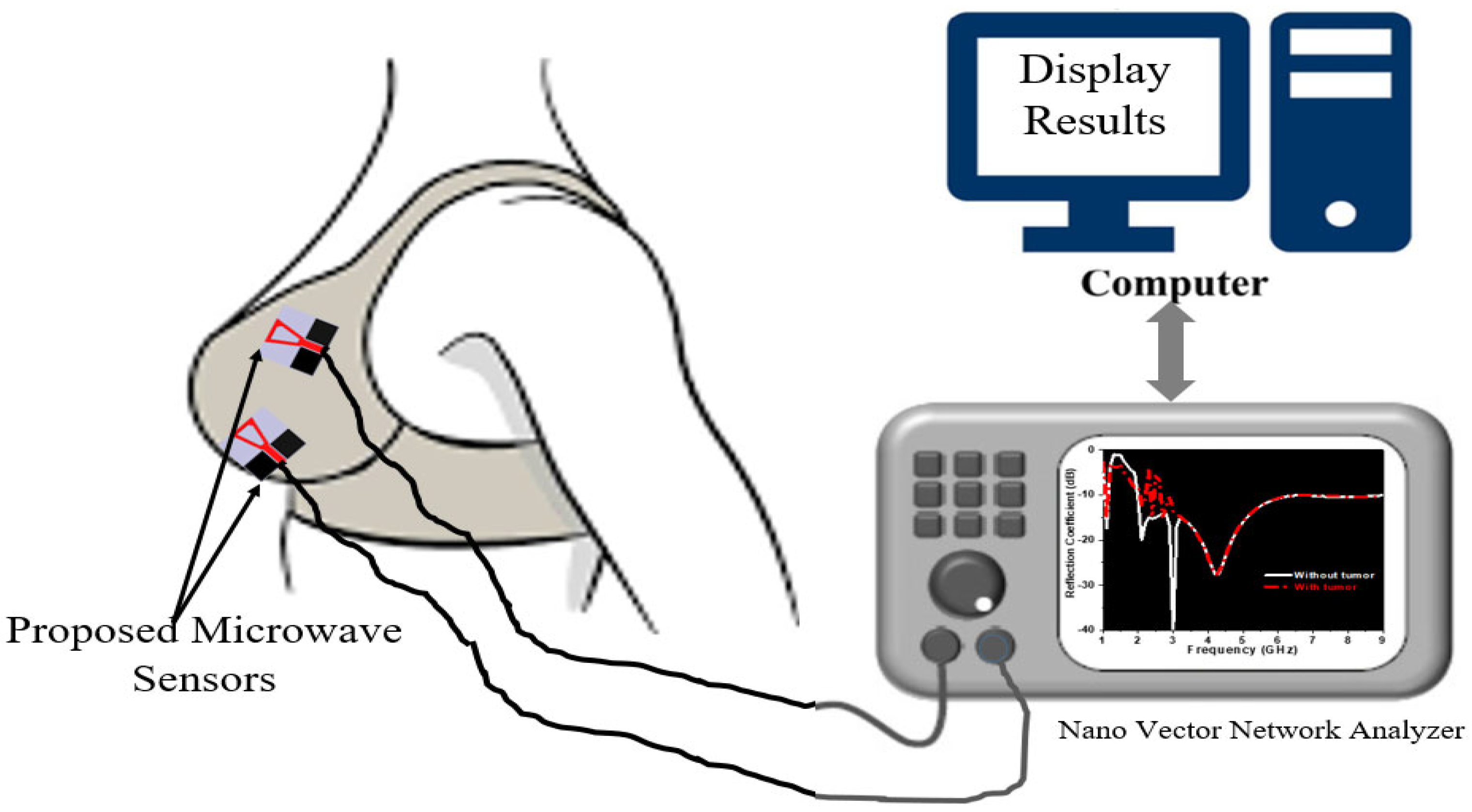
Circularly Polarized Textile Sensors for Microwave-Based Smart Bra Monitoring System
Abstract
:1. Introduction
2. Design and Characterization of Textile-Based Sensor
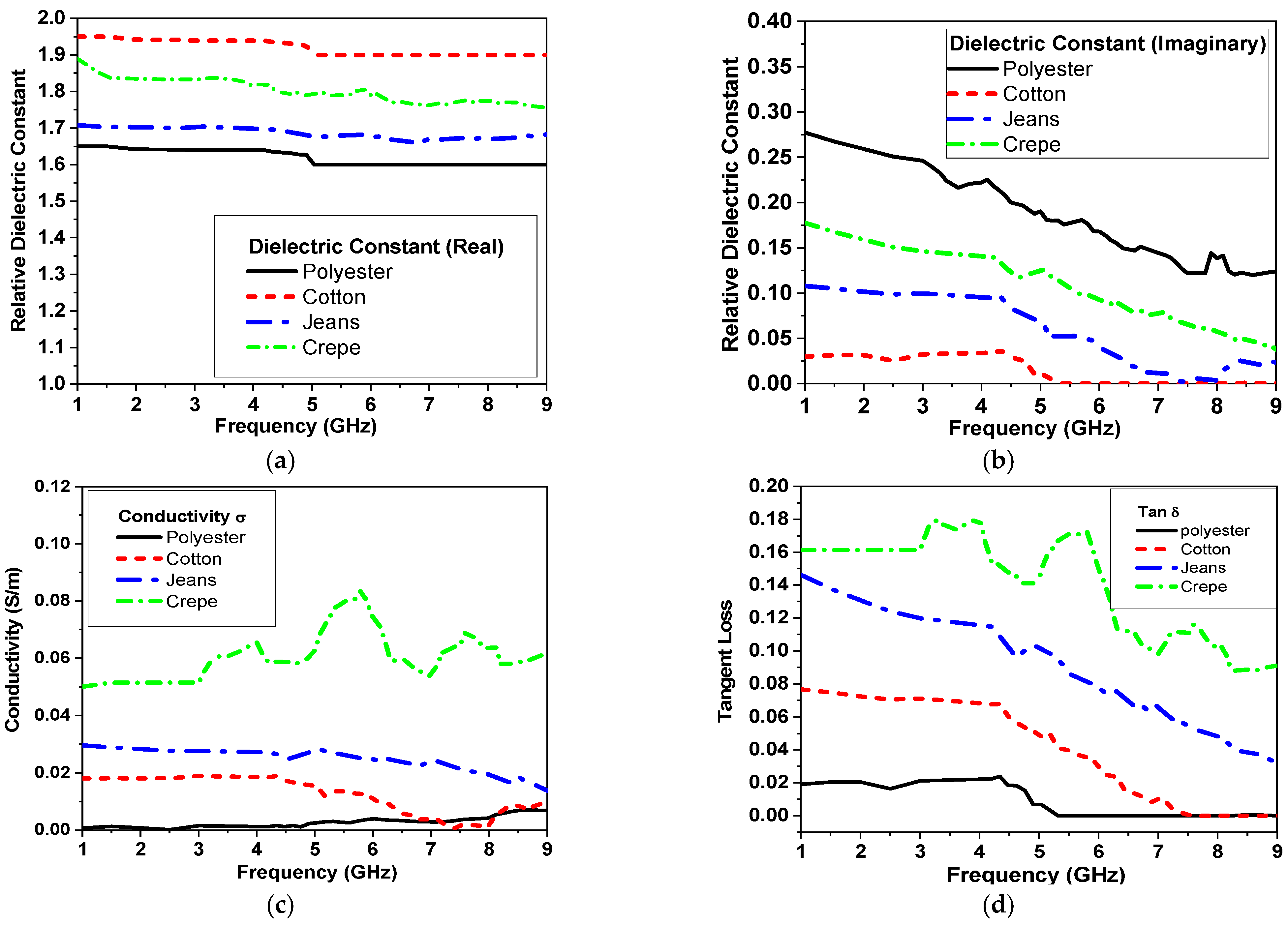
2.1. Characterization of Textile Substrates
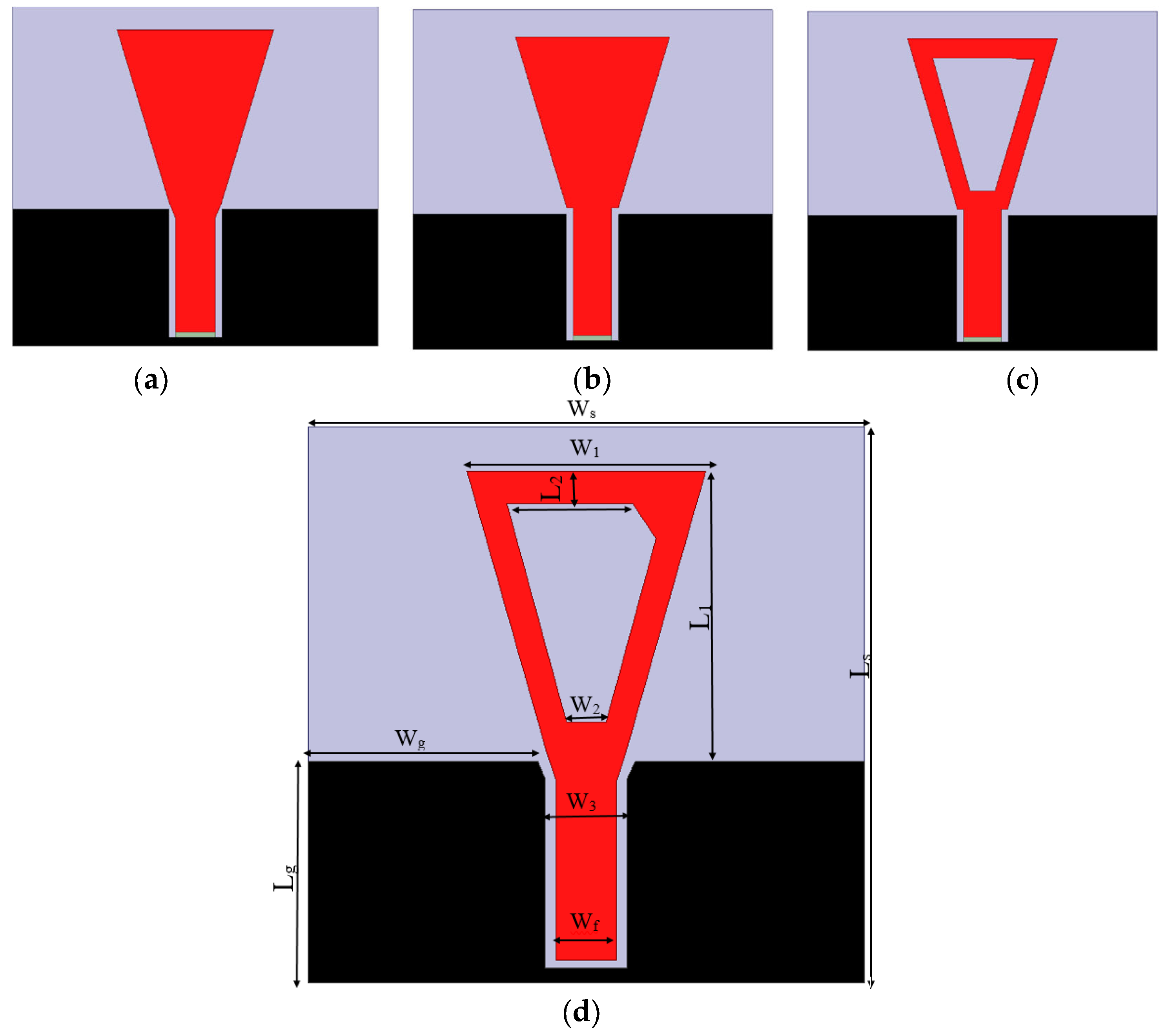
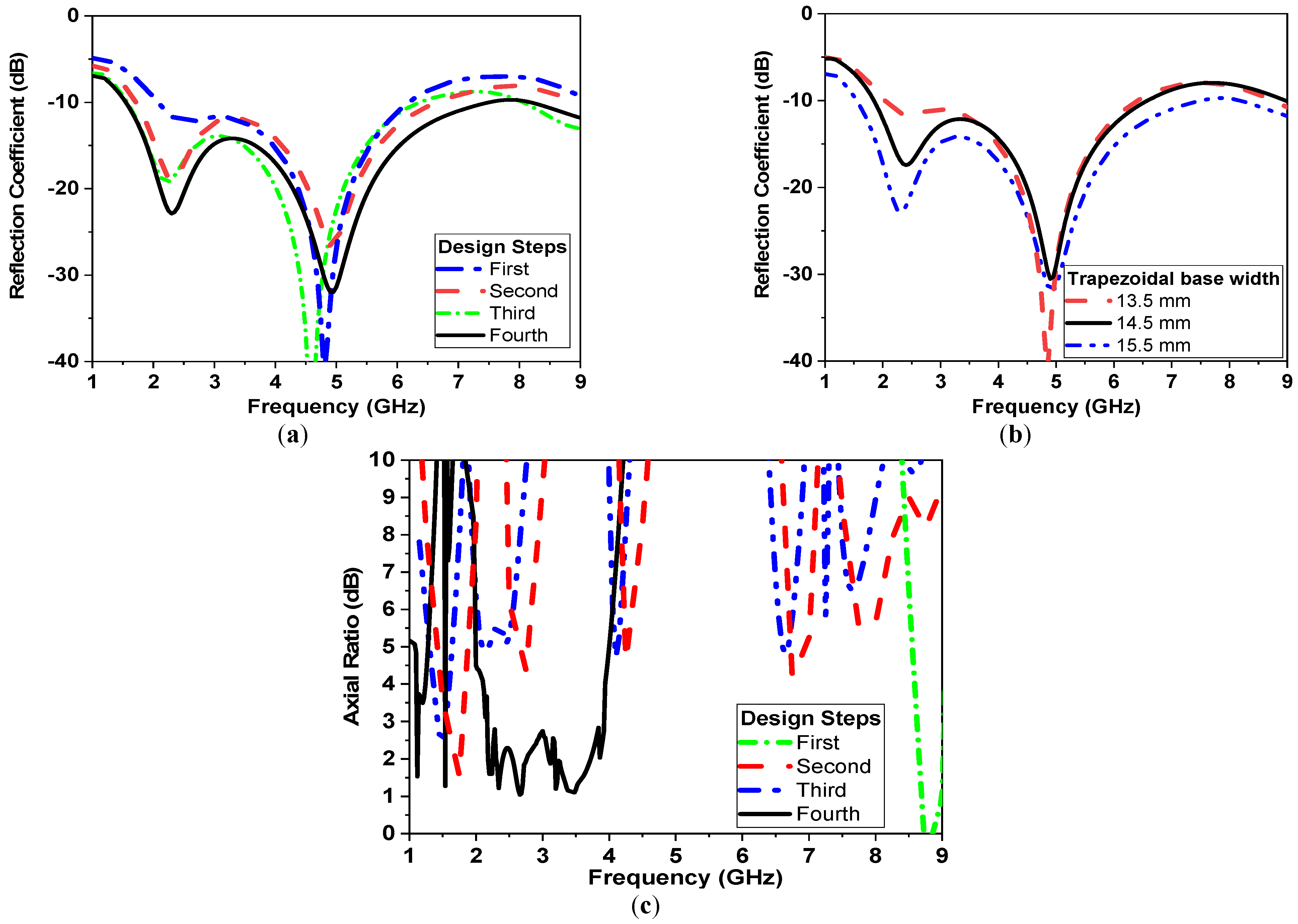
2.2. Textile-Based Circularly Polarized Antenna Design Approach
2.3. Characteristics of Breast Phantoms
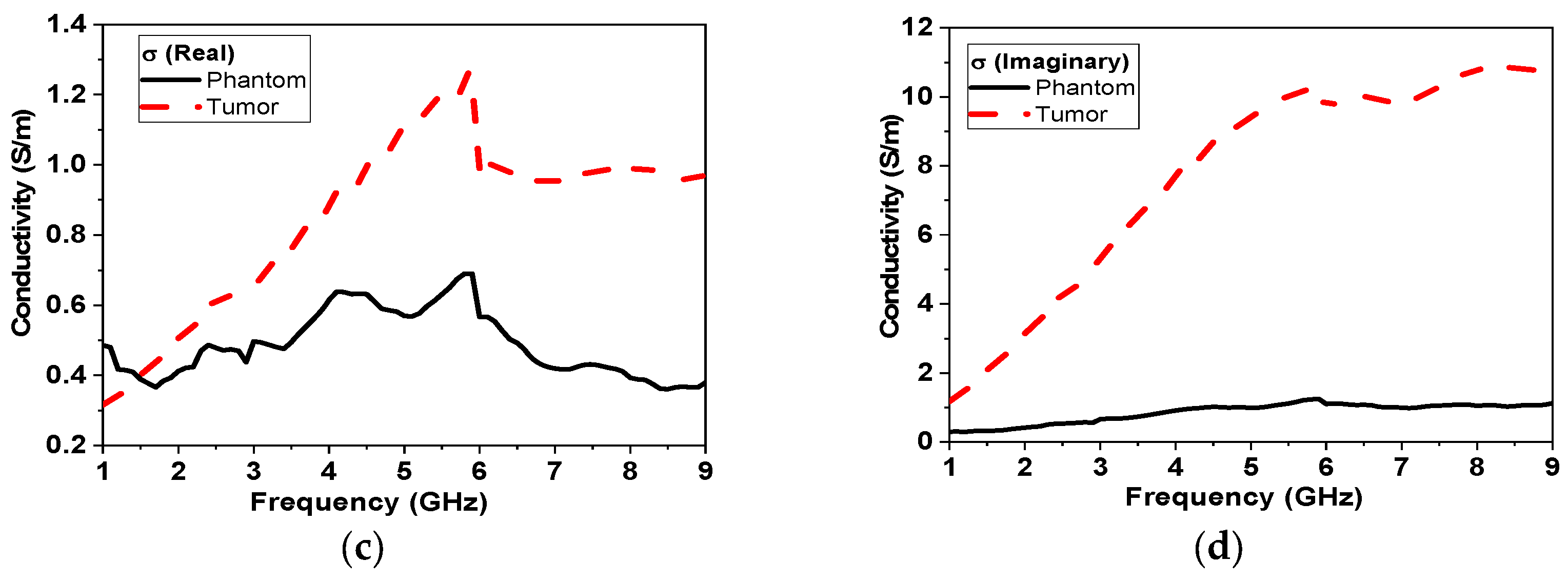
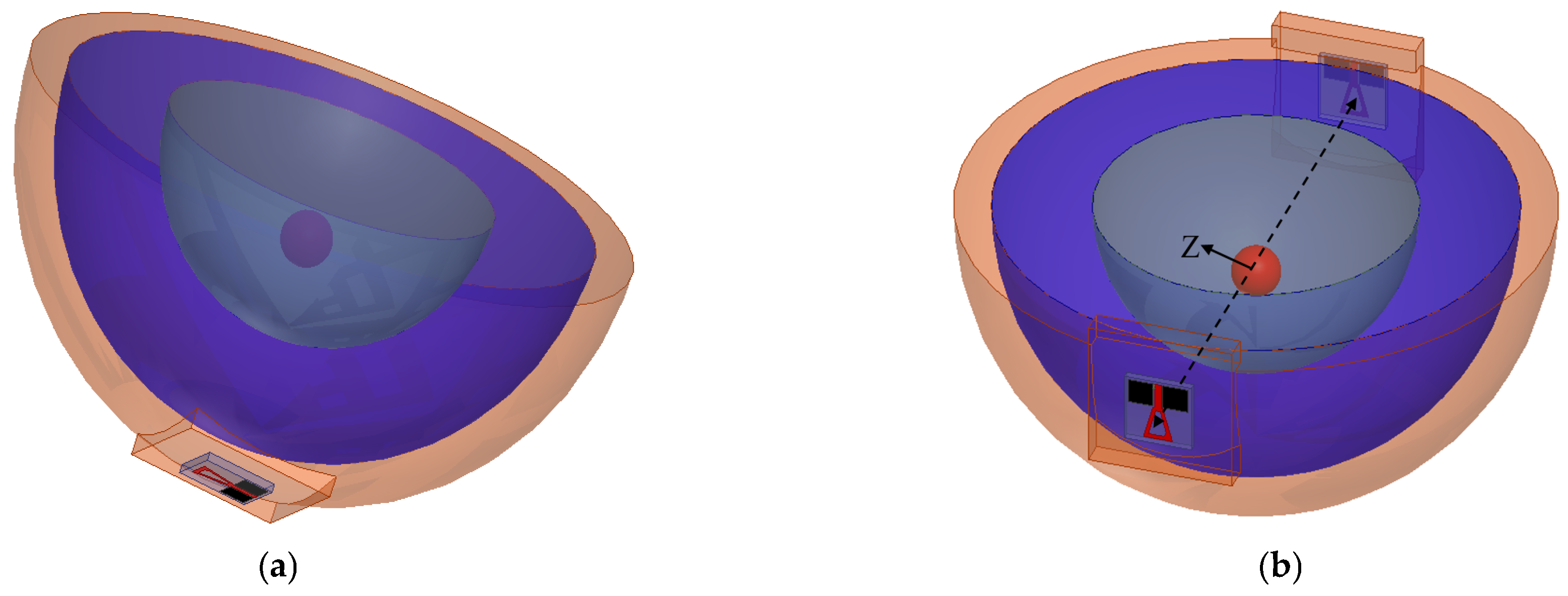
2.3.1. Numerical Models
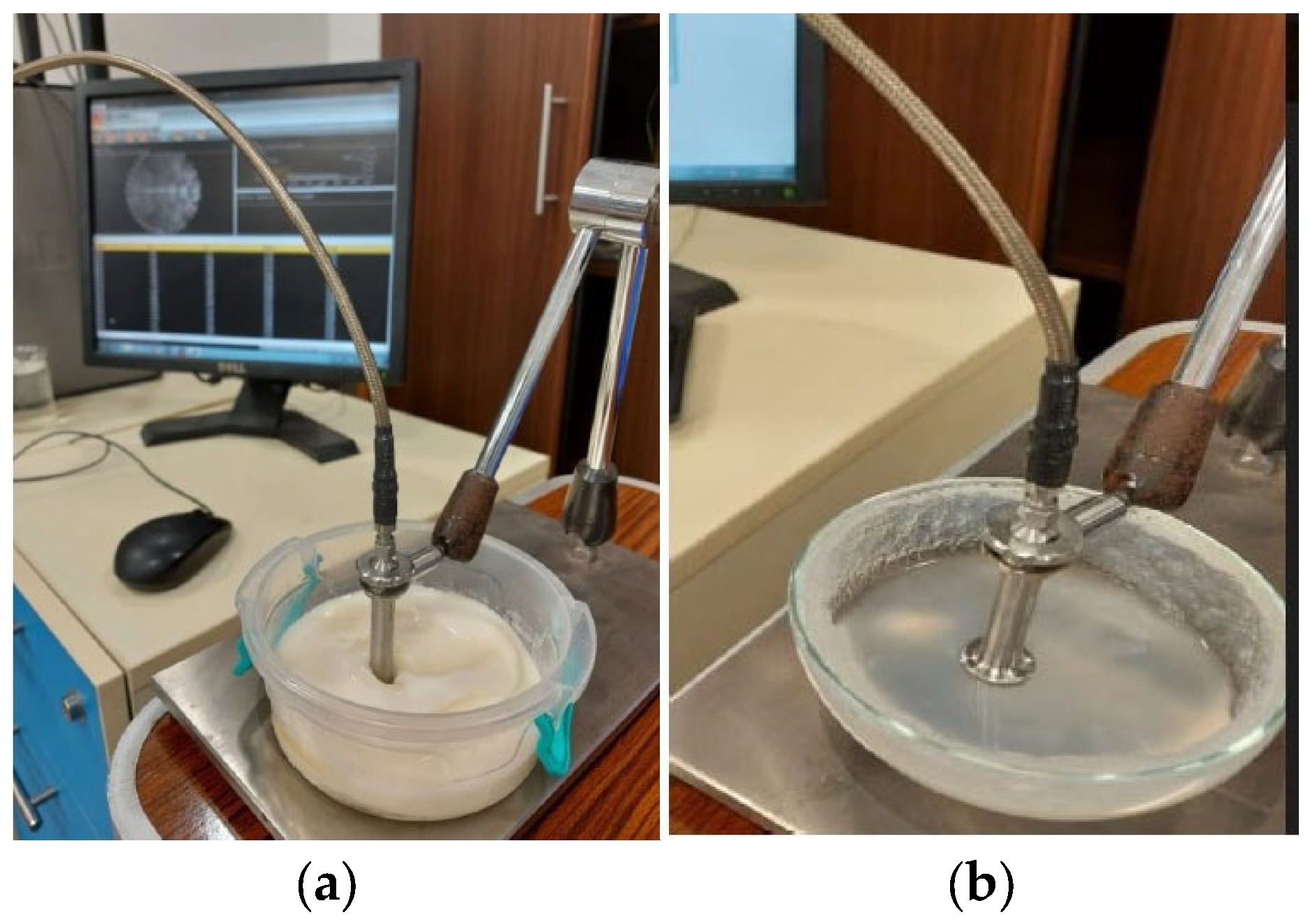
2.3.2. Fabricated Models
3. Simulation Results
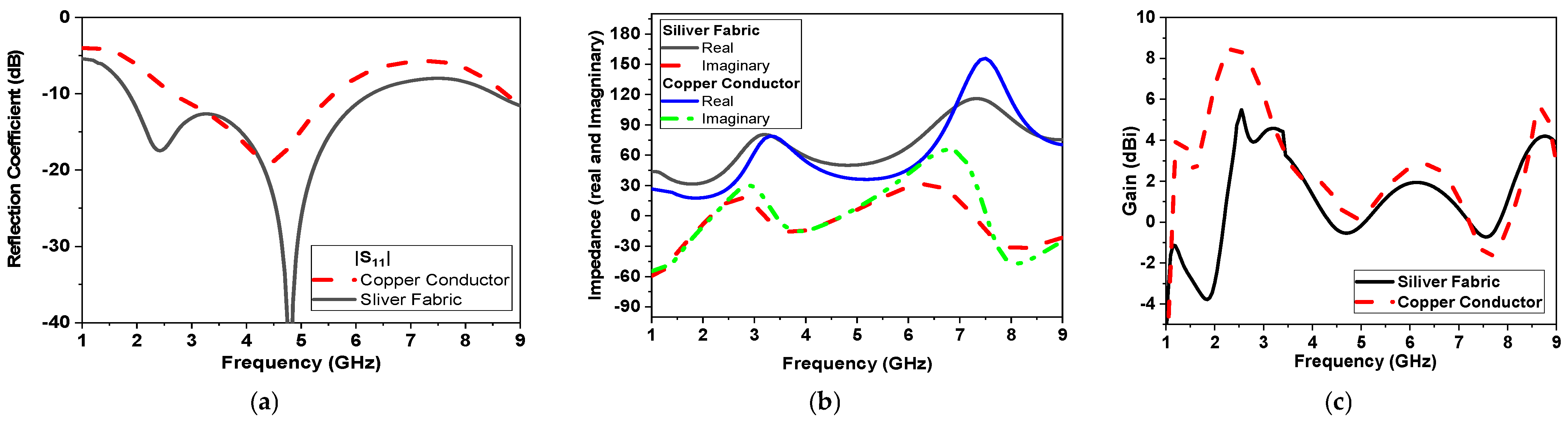
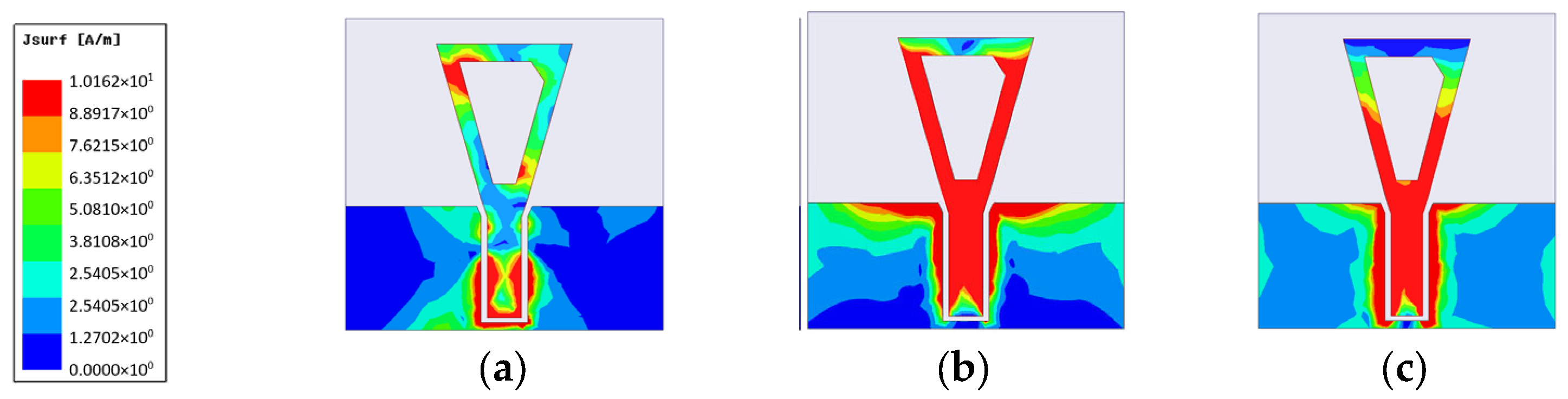
3.1. Effect of Changing Conductor Material
3.2. Placment on Breast Phantoms
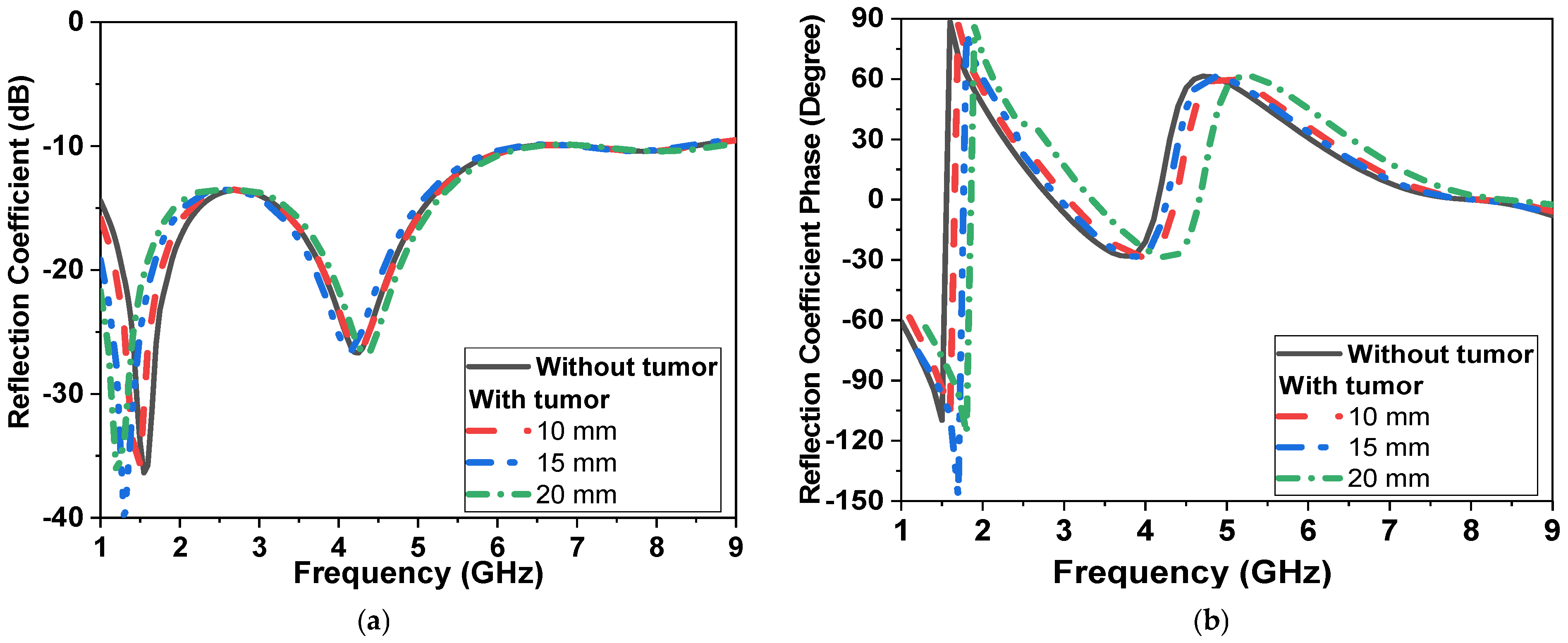
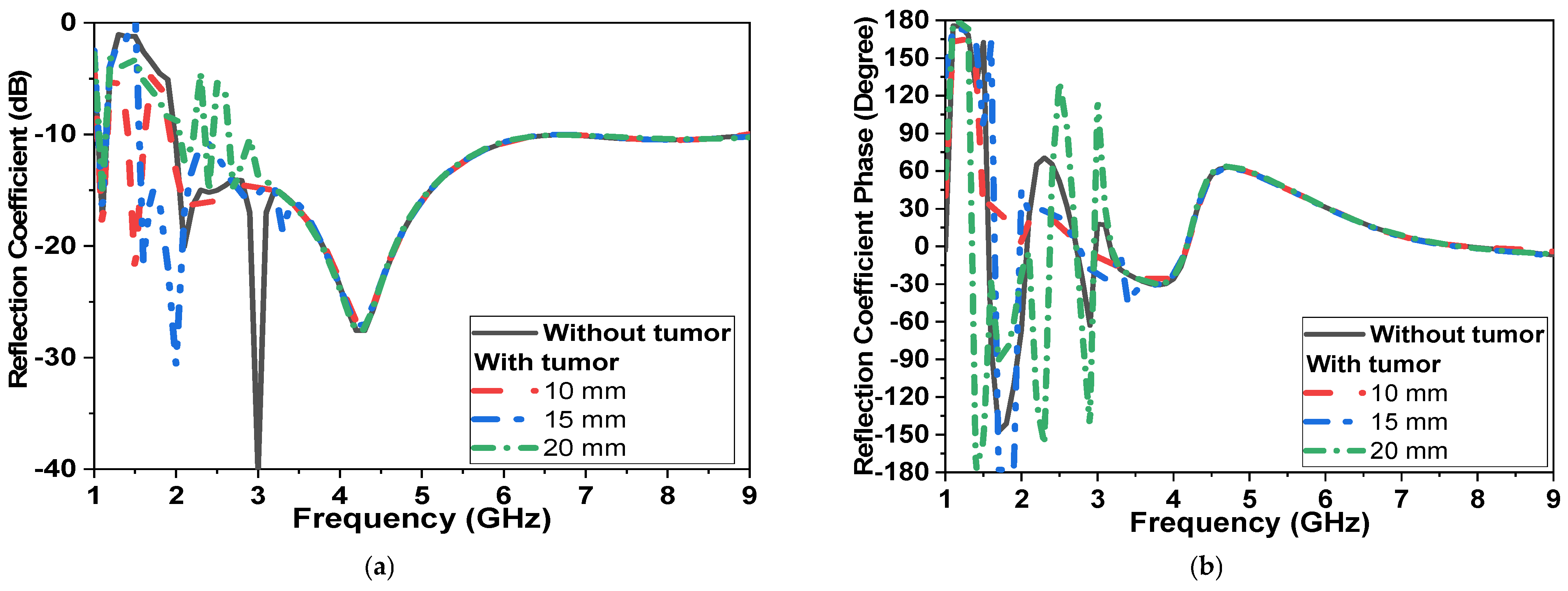
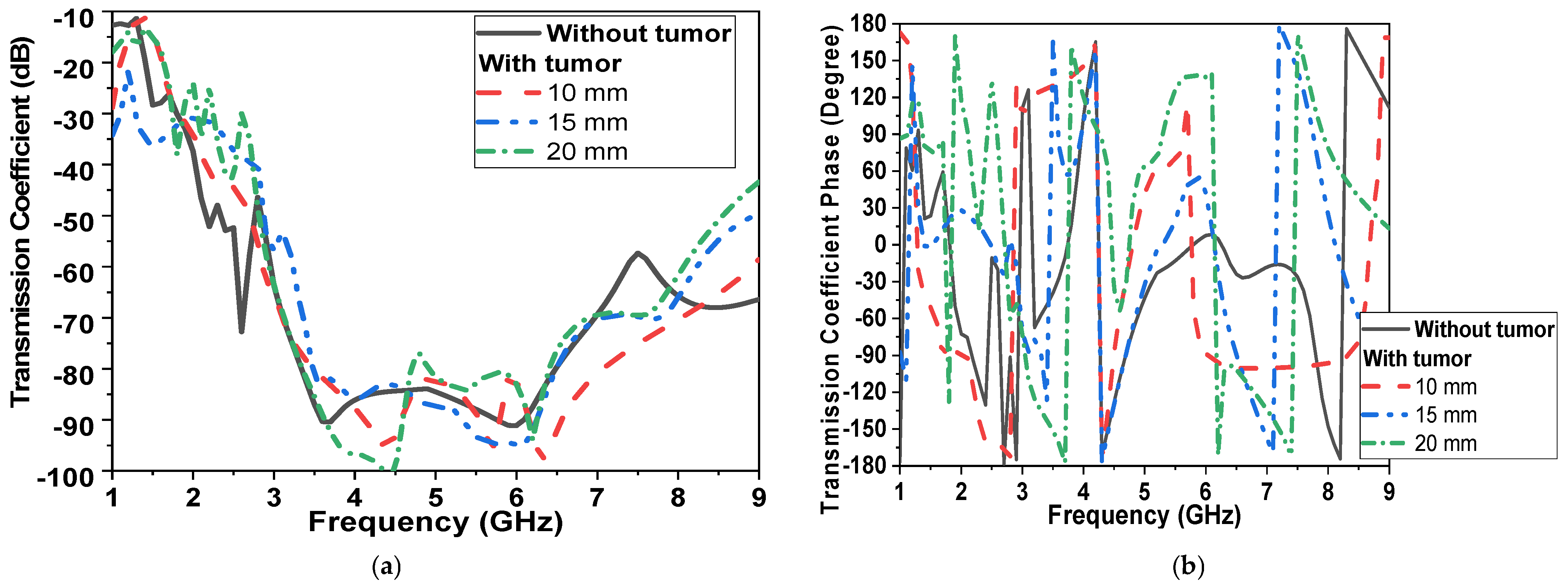
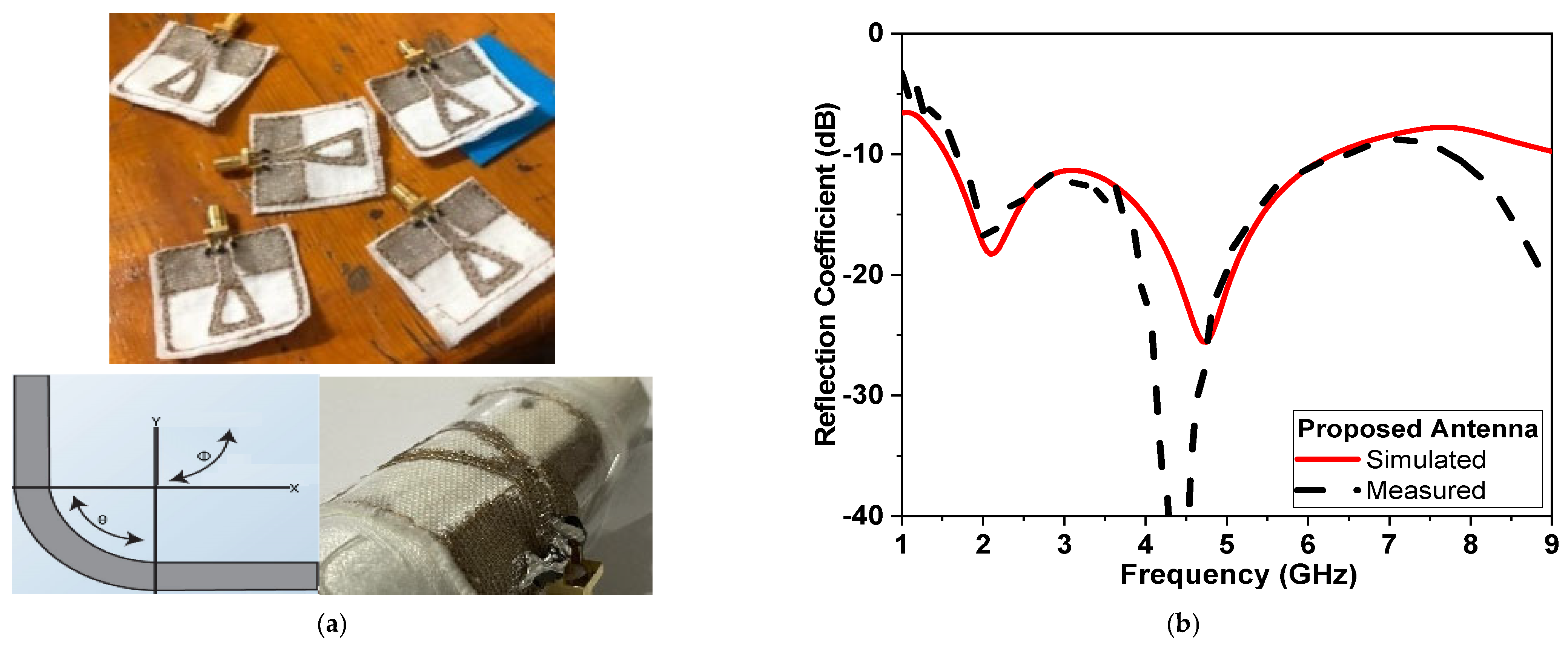
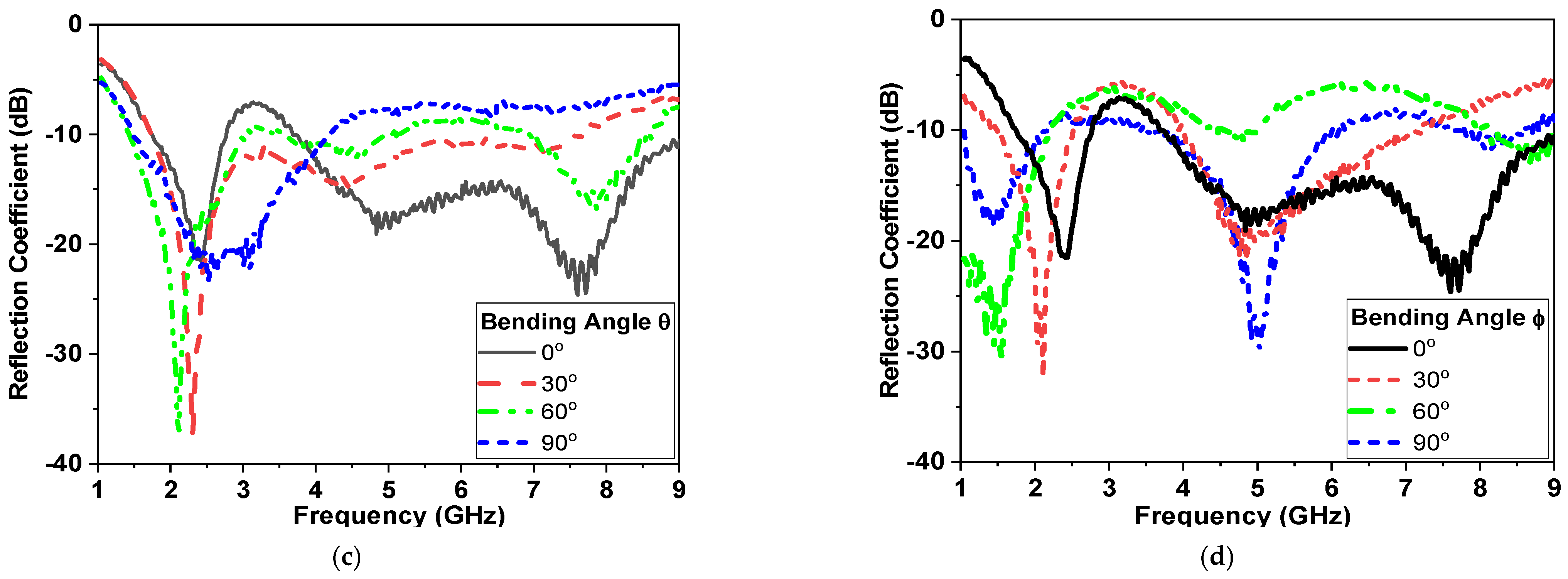
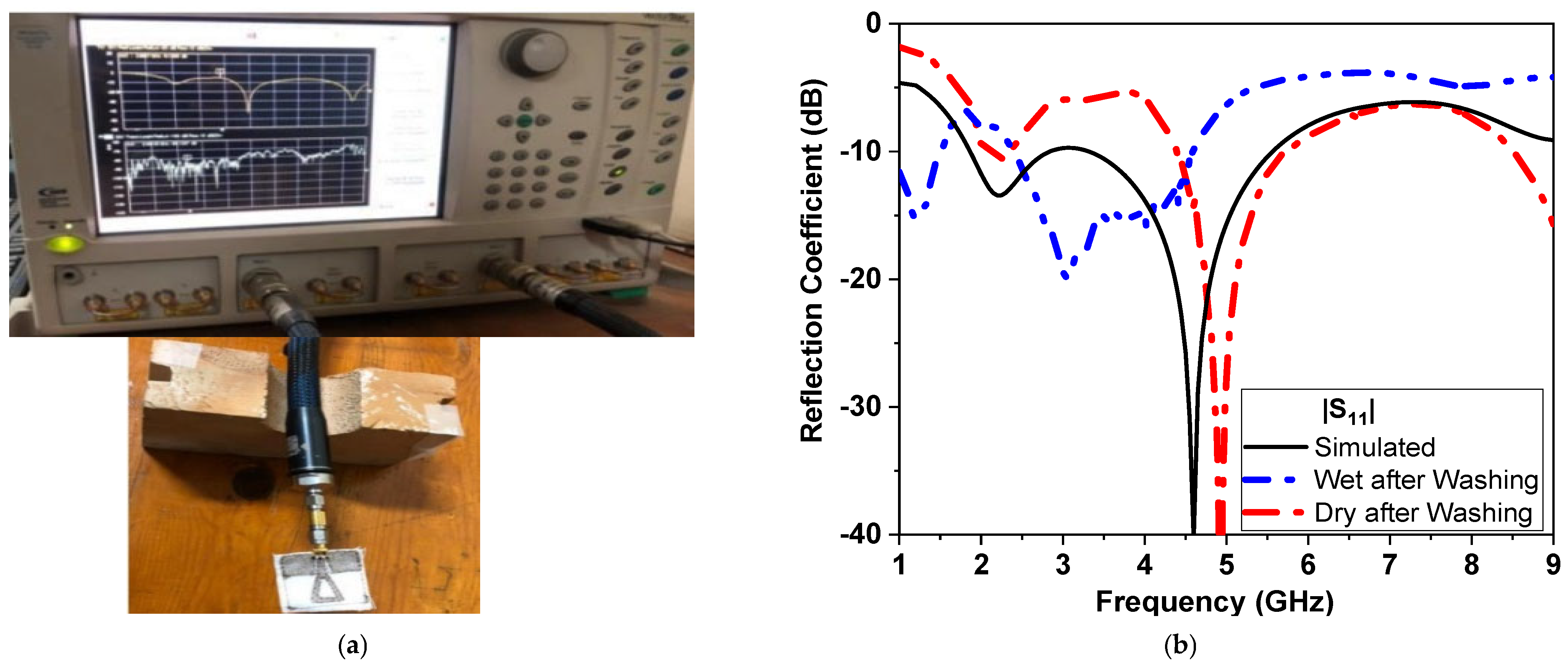
4. Experimental Results
4.1. Sensor Measurements
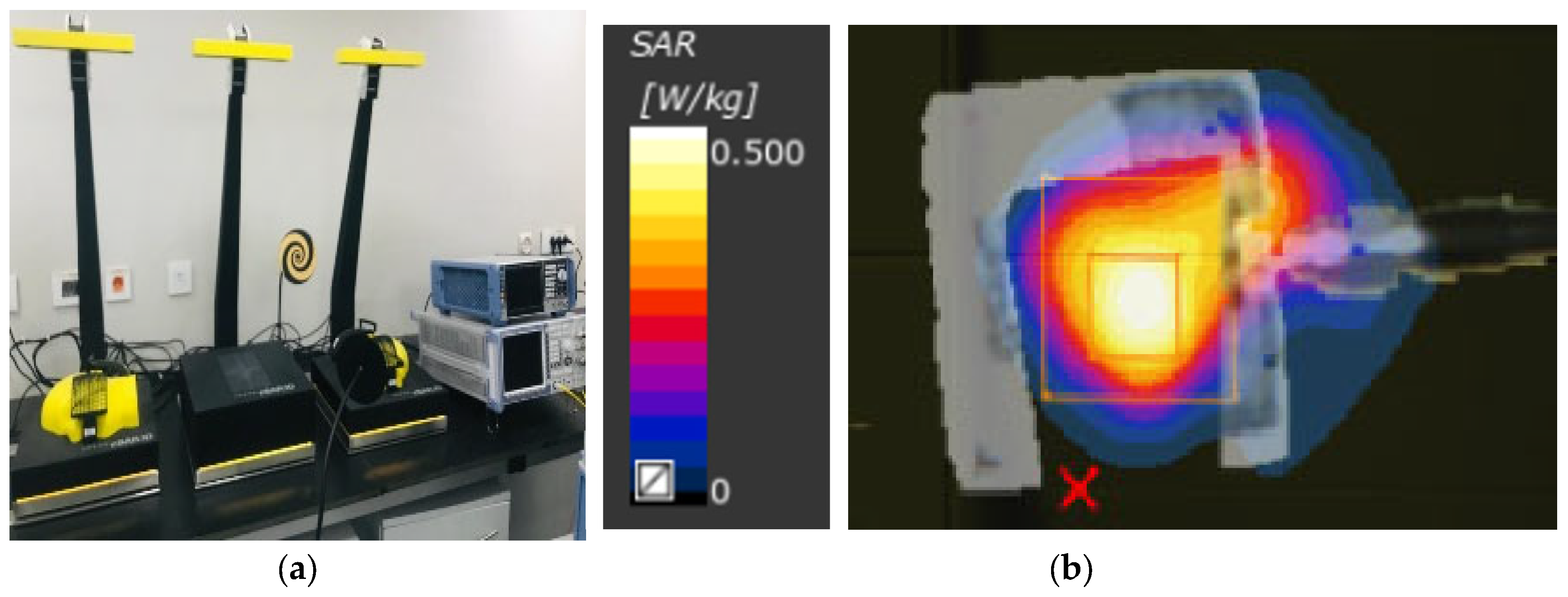
4.2. SAR Measurements
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Al-Gburi, A.J.A.; Zakaria, Z.; Alsariera, H.; Akbar, M.F.; Ibrahim, I.M.; Ahmad, K.S.; Ahmad, S.; Al-Bawri, S.S. Broadband Circular Polarised Printed Antennas for Indoor Wireless Communication Systems: A Comprehensive Review. Micromachines 2022, 13, 1048. [Google Scholar] [CrossRef]
- Fan, Y.; Liu, X.; Li, J.; Chang, T. A Miniaturized Circularly-Polarized Antenna for In-Body Wireless Communications. Micromachines 2019, 10, 70. [Google Scholar] [CrossRef] [Green Version]
- Mahmood, S.N.; Ishak, A.J.; Jalal, A.; Saeidi, T.; Shafie, S.; Soh, A.C.; Imran, M.A.; Abbasi, Q.H. A Bra Monitoring System Using a Miniaturized Wearable Ultra-Wideband MIMO Antenna for Breast Cancer Imaging. Electronics 2021, 10, 2563. [Google Scholar] [CrossRef]
- Porter, E.; Bahrami, H.; Santorelli, A.; Gosselin, B.; Rusch, L.A.; Popovic, M. A Wearable Microwave Antenna Array for Time-Domain Breast Tumor Screening. IEEE Trans. Med. Imaging 2016, 35, 1501–1509. [Google Scholar] [CrossRef] [Green Version]
- Kumar, S.; Nandan, D.; Srivastava, K.; Kumar, S.; Singh, H.; Marey, M.; Mostafa, H.; Kanaujia, B.K. Wideband Circularly Polarized Textile MIMO Antenna for Wearable Applications. IEEE Access 2021, 9, 108601–108613. [Google Scholar] [CrossRef]
- Lui, K.W.; Murphy, O.H.; Toumazou, C. A Wearable Wideband Circularly Polarized Textile Antenna for Effective Power Transmission on a Wirelessly-Powered Sensor Platform. IEEE Trans. Antennas Propag. 2013, 61, 3873–3876. [Google Scholar] [CrossRef]
- Yang, H.C.; Liu, X.Y.; Fan, Y.; Tentzeris, M.M. Flexible circularly polarized antenna with axial ratio bandwidth enhancement for off-body communications. IET Microw. Antennas Propag. 2021, 15, 754–767. [Google Scholar] [CrossRef]
- Elsheikh, D.; Eldamak, A.R. Microwave Textile Sensors for Breast Cancer Detection. In Proceedings of the 2021 38th National Radio Science Conference (NRSC), Mansoura, Egypt, 27–29 July 2021; Volume 1, pp. 288–294. [Google Scholar] [CrossRef]
- Kwon, S.; Lee, S. Recent Advances in Microwave Imaging for Breast Cancer Detection. Int. J. Biomed. Imaging 2016, 2016, 5054912. [Google Scholar] [CrossRef] [Green Version]
- O’Loughlin, D.; O’Halloran, M.J.; Moloney, B.M.; Glavin, M.; Jones, E.; Elahi, M.A. Microwave Breast Imaging: Clinical Advances and Remaining Challenges. IEEE Trans. Biomed. Eng. 2018, 65, 2580–2590. [Google Scholar] [CrossRef]
- Aldhaeebi, M.A.; Almoneef, T.S.; Ali, A.; Ren, Z.; Ramahi, O.M. Near Field Breast Tumor Detection Using Ultra-Narrow Band Probe with Machine Learning Techniques. Sci. Rep. 2018, 8, 12607. [Google Scholar] [CrossRef] [Green Version]
- Chaudhary, S.S.; Mishra, R.K.; Swarup, A.; Thomas, J.M. Dielectric properties of normal & malignant human breast tissues at radiowave & microwave frequencies. Indian J. Biochem. Biophys. 1984, 21, 76–79. [Google Scholar]
- Srinivasan, D.; Gopalakrishnan, M. Breast Cancer Detection Using Adaptable Textile Antenna Design. J. Med. Syst. 2019, 43, 177. [Google Scholar] [CrossRef]
- Rahayu, Y.; Waruwu, I. Early detection of breast cancer using ultra wide band slot antenna. Sinergi 2019, 23, 115. [Google Scholar] [CrossRef]
- Seager, R.; Zhang, S.; Chauraya, A.; Whittow, W.; Vardaxoglou, Y.; Acti, T.; Dias, T. Effect of the fabrication parameters on the performance of embroidered antennas. IET Microw. Antennas Propag. 2013, 7, 1174–1181. [Google Scholar] [CrossRef] [Green Version]
- Tsolis, A.; Whittow, W.G.; Alexandridis, A.A.; Vardaxoglou, J.C. Embroidery and Related Manufacturing Techniques for Wearable Antennas: Challenges and Opportunities. Electronics 2014, 3, 314–338. [Google Scholar] [CrossRef] [Green Version]
- Salonen, P.; Rahmat-Samii, Y.; Hurme, H.; Kivikoski, M. Effect of conductive material on wearable antenna performance: A case study of WLAN antennas. IEEE Antennas Propag. Soc. Symp. 2004, 1, 455–458. [Google Scholar] [CrossRef]
- Locher, I.; Klemm, M.; Kirstein, T.; Troster, G. Design and Characterization of Purely Textile Patch Antennas. IEEE Trans. Adv. Packag. 2006, 29, 777–788. [Google Scholar] [CrossRef] [Green Version]
- Chauraya, A.; Zhang, S.; Whittow, W.; Acti, T.; Seager, R.; Dias, T.; Vardaxoglou, Y.C. Addressing the challenges of fabricating microwave antennas using conductive threads. In Proceedings of the 2012 6th European Conference on Antennas and Propagation (EUCAP), Prague, Czech Republic, 26–30 March 2012; pp. 1365–1367. [Google Scholar] [CrossRef] [Green Version]
- Locher, I.; Tröster, G. Screen-printed Textile Transmission Lines. Text. Res. J. 2007, 77, 837–842. [Google Scholar] [CrossRef]
- Bahramiabarghouei, H.; Porter, E.; Santorelli, A.; Gosselin, B.; Popovic, M.; Rusch, L.A. Flexible 16 Antenna Array for Microwave Breast Cancer Detection. IEEE Trans. Biomed. Eng. 2015, 62, 2516–2525. [Google Scholar] [CrossRef]
- Sheeba, I.R.; Jayanthy, T. Design and Analysis of a Flexible Softwear Antenna for Tumor Detection in Skin and Breast Model. Wirel. Pers. Commun. 2019, 107, 887–905. [Google Scholar] [CrossRef]
- Alsharif, F.; Kurnaz, C. Wearable Microstrip Patch Ultra Wide Band Antenna for Breast Cancer Detection. In Proceedings of the 2018 41st International Conference on Telecommunications and Signal Processing (TSP), Athens, Greece, 4–6 July 2018; pp. 1–5. [Google Scholar]
- Schneider, S.W.; Kemp, J.; Georget, E.; Abdeddaim, R.; Sabouroux, P. A new method to design a multi-band flexible textile antenna [AMTA corner]. IEEE Antennas Propag. Mag. 2014, 56, 240–248. [Google Scholar] [CrossRef]
- Joachimowicz, N.; Conessa, C.; Henriksson, T.; Duchene, B. Breast Phantoms for Microwave Imaging. IEEE Antennas Wirel. Propag. Lett. 2014, 13, 1333–1336. [Google Scholar] [CrossRef]
- Lazebnik, M.; Madsen, E.L.; Frank, G.R.; Hagness, S.C. Tissue-mimicking phantom materials for narrowband and ultrawideband microwave applications. Phys. Med. Biol. 2005, 50, 4245–4258. [Google Scholar] [CrossRef]
- Henriksson, T.; Joachimowicz, N.; Conessa, C.; Bolomey, J.-C. Quantitative Microwave Imaging for Breast Cancer Detection Using a Planar 2.45 GHz System. IEEE Trans. Instrum. Meas. 2010, 59, 2691–2699. [Google Scholar] [CrossRef]
- Mashal, A.; Gao, F.; Hagness, S.C. Heterogeneous anthropomorphic phantoms with realistic dielectric properties for microwave breast imaging experiments. Microw. Opt. Technol. Lett. 2011, 53, 1896–1902. [Google Scholar] [CrossRef] [Green Version]
- Croteau, J.; Sill, J.; Williams, T.; Fear, E. Phantoms for testing radar-based microwave breast imaging. In Proceedings of the 2009 13th International Symposium on Antenna Technology and Applied Electromagnetics and the Canadian Radio Science Meeting, Banff, AB, Canada, 15–18 February 2009. [Google Scholar]
- Elsheakh, D.N.; Mohamed, R.A.; Fahmy, O.M.; Ezzat, K.; Eldamak, A.R. Complete Breast Cancer Detection and Monitoring System by Using Microwave Textile Based Antenna Sensors. Biosensors 2023, 13, 87. [Google Scholar] [CrossRef]
- Jiang, Z.H.; Cui, Z.; Yue, T.; Zhu, Y.; Werner, D.H. Compact, Highly Efficient, and Fully Flexible Circularly Polarized Antenna Enabled by Silver Nanowires for Wireless Body-Area Networks. IEEE Trans. Biomed. Circuits Syst. 2017, 11, 920–932. [Google Scholar] [CrossRef]
- Jiang, Z.H.; Gregory, M.D.; Werner, D.H. Design and Experimental Investigation of a Compact Circularly Polarized Integrated Filtering Antenna for Wearable Biotelemetric Devices. IEEE Trans. Biomed. Circuits Syst. 2016, 10, 328–338. [Google Scholar] [CrossRef]
- Ismail, M.F.; Rahim, M.K.A.; Saadon, E.I.S.; Mohd, M.S. Compact circularly polarized textile antenna. In Proceedings of the 2014 IEEE Symposium on Wireless Technology and Applications (ISWTA), Kota Kinabalu, Malaysia, 28 September–1 October 2014; pp. 134–136. [Google Scholar]
- Joachimowicz, N.; Duchêne, B.; Conessa, C.; Meyer, O. Easy-to-produce adjustable realistic breast phantoms for microwave imaging. In Proceedings of the 2016 10th European Conference on Antennas and Propagation (EuCAP), Davos, Switzerland, 10–15 April 2016. [Google Scholar]
- Burfeindt, M.J.; Colgan, T.J.; Mays, R.O.; Shea, J.D.; Behdad, N.; Van Veen, B.D.; Hagness, S.C. MRI-Derived 3-D-Printed Breast Phantom for Microwave Breast Imaging Validation. IEEE Antennas Wirel. Propag. Lett. 2012, 11, 1610–1613. [Google Scholar] [CrossRef] [Green Version]
- Herrera, D.R.; Reimer, T.; Nepote, M.S.; Pistorius, S. Manufacture and testing of anthropomorphic 3D-printed breast phantoms using a microwave radar algorithm optimized for propagation speed. In Proceedings of the 2017 11th European Conference on Antennas and Propagation (EUCAP), Paris, France, 19–24 March 2017. [Google Scholar]
- Islam, T.; Samsuzzaman, M.; Kibria, S.; Islam, M.T. Experimental Breast Phantoms for Estimation of Breast Tumor Using Microwave Imaging Systems. IEEE Access 2018, 6, 78587–78597. [Google Scholar] [CrossRef]
- Romeo, S.; Di Donato, L.; Bucci, O.M.; Catapano, I.; Crocco, L.; Scarfì, M.R.; Massa, R. Dielectric characterization study of liquid-based materials for mimicking breast tissues. Microw. Opt. Technol. Lett. 2011, 53, 1276–1280. [Google Scholar] [CrossRef]
- Rydholm, T.; Fhager, A.; Persson, M.; Geimer, S.; Meaney, P. Effects of the Plastic of the Realistic GeePS-L2S-Breast Phantom. Diagnostics 2018, 8, 61. [Google Scholar] [CrossRef] [Green Version]
- Loss, C.; Goncalves, R.; Lopes, C.; Salvado, R.; Pinho, P. Textile antenna for RF energy harvesting fully embedded in clothing. In Proceedings of the 2016 10th European Conference on Antennas and Propagation (EuCAP), Davos, Switzerland, 10–15 April 2016; pp. 1–4. [Google Scholar] [CrossRef]
- Mahmood, S.N.; Ishak, A.J.; Saeidi, T.; Soh, A.C.; Jalal, A.; Imran, M.A.; Abbasi, Q.H. Full Ground Ultra-Wideband Wearable Textile Antenna for Breast Cancer and Wireless Body Area Network Applications. Micromachines 2021, 12, 322. [Google Scholar] [CrossRef]
- Sharma, N.; Bhatia, S.S. Design of printed UWB antenna with CPW and microstrip-line-fed for DCS/PCS/bluetooth/WLAN wireless applications. Int. J. RF Microw. Comput. Eng. 2020, 31, e22488. [Google Scholar] [CrossRef]
- El Atrash, M.; Abdalla, M.A.; Elhennawy, H.M. A fully-textile wideband AMC-backed antenna for wristband WiMAX and medical applications. Int. J. Microw. Wirel. Technol. 2020, 13, 624–633. [Google Scholar] [CrossRef]
- Bahrami, H.; Porter, E.; Santorelli, A.; Gosselin, B.; Popovic, M.; Rusch, L.A. Flexible sixteen monopole antenna array for microwave breast cancer detection. In Proceedings of the 2014 36th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Chicago, IL, USA, 26–30 August 2014; pp. 3775–3778. [Google Scholar]
- Saha, P.; Mitra, D.; Parui, S.K. A circularly polarised implantable monopole antenna for biomedical applications. Prog. Electromagn. Res. C 2018, 85, 167–175. [Google Scholar] [CrossRef] [Green Version]
- Lin, X.; Chen, Y.; Gong, Z.; Seet, B.-C.; Huang, L.; Lu, Y. Ultrawideband Textile Antenna for Wearable Microwave Medical Imaging Applications. IEEE Trans. Antennas Propag. 2020, 68, 4238–4249. [Google Scholar] [CrossRef]
- Islam, S.; Azam, S.K.; Hossain, A.Z.; Ibrahimy, M.I.; Motakabber, S. A low-profile flexible planar monopole antenna for biomedical applications. Eng. Sci. Technol. Int. J. 2022, 35, 101112. [Google Scholar] [CrossRef]







| Wg | Lg | Wf | W3 | W2 | W1 | L2 | L1 | Ws | Ls |
|---|---|---|---|---|---|---|---|---|---|
| 14.5 | 13.5 | 4 | 5 | 2.5 | 14.5 | 2 | 17.5 | 33.5 | 33.5 |
| SAR Level for CPMS | Power Level | |
|---|---|---|
| 10 g | 1 g | (dBm) |
| 0.07 | 0.201 | 5 |
| 0.086 | 0.293 | 10 |
| 0.211 | 0.594 | 15 |
| 0.333 | 0.944 | 20 |
| BW of AR (GHz) & % | CP/LP | SAR (W/Kg) in 10 g | Fabrications | Dimensions (W × L × h) mm3 | Gain (dBi) | BW (GHz) | Ref. |
|---|---|---|---|---|---|---|---|
| 2.39–2.57 (7%) | CP | 81.5 at (1 W) | Rogers 3010 | 9.2 × 9.2 × 1.27 | NM | 2.39–2.57 | [2] |
| - | LP(MIMO) | 1.93 | Denim and felt | 24 × 24 × 1.4 | 5.72 | 4.8–30 | [3] |
| 5.2–7.1 | CP | 367.86 mW at (2 W) | Felt | 32:5 × 42 × 1 | 5.7 | 3.6–13 | [5] |
| −31% | |||||||
| 2.3–2.864 (22%) | CP | NM | Felt | 76 × 76× 1.5 | 4.9 | 1.086 | [6] |
| 5.730–5.955 | CP | 0.294 | Flexible Panasonic R-F770 | 35 × 35 × 2.24 | 7.2 | 5.67–6.05 | [7] |
| −4% | |||||||
| - | LP | NM | Cordura | 80 × 30 × 0.5 | 2.01 | 0.9, 1.8 | [40] |
| - | LP | 0.09 | Denim | 60 × 50 × 0.7 | 10.5 | 7–28 | [41] |
| - | LP | NM | FR4 | 27 × 27 × 1.6 | 8.65 | 1.23–20 | [42] |
| - | LP | 3.28 × 10−6 | Felt | 36 × 18 × 3 | 7.81 | 3.1–6.5 | [43] |
| - | Dual Polarized | NM | Kapton Polymidie | 20 × 20 × 0.05 | NM | 2–4 | [44] |
| 2.38–2.51(5%) | CP | 242 | RT Duroid | 10 × 10 × 0.3 | −7.79 | 2.3–2.64 | [45] |
| - | LP | 0.0014 at (1 mW) | Polyster fabric | 70 × 50 × 0.5 | 2.9 | 1.198–4 | [46] |
| - | LP | 1 (0.5 W) | Flexible Kapton Polyimide | 13 × 13 × 0.125 | 4.4 | 8.6–14 | [47] |
| 1.8–4 (73%) | CP | 0.489 (50 mW) | Cotton | 33.5 × 33.5 × 2 | 6 | 1.8–8 | This work |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Elsheakh, D.N.; Elgendy, Y.K.; Elsayed, M.E.; Eldamak, A.R. Circularly Polarized Textile Sensors for Microwave-Based Smart Bra Monitoring System. Micromachines 2023, 14, 586. https://doi.org/10.3390/mi14030586
Elsheakh DN, Elgendy YK, Elsayed ME, Eldamak AR. Circularly Polarized Textile Sensors for Microwave-Based Smart Bra Monitoring System. Micromachines. 2023; 14(3):586. https://doi.org/10.3390/mi14030586
Chicago/Turabian StyleElsheakh, Dalia N., Yasmine K. Elgendy, Mennatullah E. Elsayed, and Angie R. Eldamak. 2023. "Circularly Polarized Textile Sensors for Microwave-Based Smart Bra Monitoring System" Micromachines 14, no. 3: 586. https://doi.org/10.3390/mi14030586






