Microfluidic Applications in Prostate Cancer Research
Abstract
1. Introduction
2. Human Prostate Modeling
2.1. In Vivo Animal Models of the Human Prostate
2.2. In Vitro Models of the Human Prostate
3. Prostate Cancer Development
3.1. Prostate Carcinogenesis
3.1.1. Adenocarcinoma of the Prostate (Carcinoma In Situ)
3.1.2. Monoculture Models
3.1.3. Co-Culture Models
3.2. Prostate Cancer Metastasis
3.2.1. Invasion
3.2.2. Intravasation
3.2.3. Circulation
3.2.4. Extravasation
Bone Tropism
3.2.5. Dormancy and Colonization
| Reference | Cells/Samples Used | Culture Type | Field of Investigation | Device Properties | Findings |
|---|---|---|---|---|---|
| Dolega [48] | Non-malignant RWPE-1, PC3, MCF-10A | 3D | Prostate cancer physiology | Glass capillaries mounted with needles were used to form circular channels through PDMS. Devices were coated with a thin membrane of Matrigel or layered polyelectrolyte. | Cells adhered to and proliferate in channels of diameter ≥150 μm. Continuous flow through channels did not induce cellular detachment. |
| Jiang [49] | Immortalized PrEC, BHPrS1 | 3D | Prostate cancer physiology | Two stacked, z-shaped PDMS channels separated by a polyester membrane with a 0.8 μm pore size. Each channel consisted of 500 μm height, 1 mm width, and 40 mm length, with a 20 mm overlapping segment of the microchannels. | Established an in vitro model of the human prostate. Demonstrated R1881-mediated epithelium differentiation. |
| Picollet-D’hahan [59] | PC3, PNT-2 | 2D | Prostate cancer physiology | Polyelectrolyte films on multi-well plates were fabricated with anionic PSS (poly(sodium 4-styrenesulphonate))-terminated and cationic PAH (poly(allylamine hydrochloride))-terminated coatings in 2 nm-thick layers. | PAH-terminated surfaces had better initial attachment of PC3 but prevented clustering, reduced focal adhesion points, and decreased proliferation rate compared to PSS. No polyelectrolyte surfaces affected biological responses of PNT-2. |
| Liberio [60] | LNCaP | 2D | Prostate cancer physiology | 96-well plates were coated with one of the following substances: 1.3 μL laminin; 1 μL human placenta type IV collagen; 0.4 μL fibronectin; 50 μL poly-L-ornithine; or 0.32 μL poly-L-lysine. | Fibronectin, poly-L-lysine, and poly-L-ornithine improved LNCaP adherence and reduced cell mobility. Laminin and collagen type IV promoted cell aggregation. No coatings affected the expression of androgen receptor-regulated genes. |
| Cheung [62] | PC3N, MDA-MB-231-N | 3D | Prostate cancer physiology | Straight channel (100 μm height, 32 mm length, 1 mm width) PDMS microchannel surfaces were immobilized with antibodies for cell capture. | Detachment of cells depended on flow rate and acceleration. A proposed exponential-like empirical model could predict the flow rate required for cell detachment as a function of flow acceleration. |
| Liu [63] | PC3 | 3D | Prostate cancer physiology | PDMS and glass device with 32 μm-thick PDMS diaphragm between upper and lower layers. The upper PDMS channel consisted of 4 rectangular chambers connected to external gas sources for generating shear forces. | The microfluidic chip could culture cancer cells for at least one month and output cancer cells externally using only hydrodynamic forces. |
| Liu [64] | LNCaP, DU145, PC3 | 2D | Prostate cancer physiology | Single-channel PDMS device (300 μm length, 25 μm height, 25 μm width) under a flow rate of 0.2 μL/s. Microfluidic methods were verified using atomic force microscopy. | Androgen-insensitive prostate cancer cell lines (PC3 and DU145) had a higher elastic modulus than androgen-sensitive (LNCaP) cell lines. |
| Dolega [65] | RWPE1, WPE1-NB26 | 3D | Prostate cancer physiology | 3D cell cultures were grown in Matrigel and thawed into 4-well or 8-well Labtek plates. | Lensfree imaging allowed for the observation of epithelial tissue morphogenesis via the distinction between acini and spheroids in cancerous and normal models. Cell–cell and cell–environment interactions during differentiation could be studied by modulating stimuli within the ECM. |
| Tricoli [66] | Patient-derived normal and malignant prostate CRCs | 3D | Prostate cancer physiology | 2 polycarbonate cell culture inserts were placed in a 6-well plate and coated with 0.1% gelatin in 3 alternating applications. | Both normal and tumor-derived prostate epithelial cells underwent rapid basal-to-luminal differentiation (2 weeks) in 3D culture. |
| Fang [73] | C4-2 transfected with pcDNA3.1 or PKD1-GFP, WPMY-1 | 3D | Prostate cancer physiology | Alginate hydrogel in a microfluidic device with PLO perm selective basement membrane. Device specifications not mentioned. | Co-culture of epithelial and stromal cells allowed for the measurement of the shed component of E-cadherin. The amount of E-cadherin present in conditioned media was influenced by epithelial–stromal interaction. |
| Businaro [74] | B16 melanoma cells, immune cells isolated from spleen of wild-type (WT) and IRF-8 KO mice. | 3D | Prostate cancer physiology | PDMS device with two culture chambers (1 mm width, 8 mm length, 100 μm height) and center channels (4 mm length, 1 mm width) connected via four sets of microchannels (12 μm width, 500 μm length, 10 μm height). | WT spleen cells more readily migrated toward B16 cells compared to IRF-8 KO immune cells. |
| Jeong [75] | HT-29 human colorectal carcinoma cells, CCD-18Co human normal fibroblasts | 3D | Prostate cancer physiology | PDMS devices were loaded with hydrogel mixture and bonded to either a glass coverslip or a PDMS membrane. Channels were coated with poly-dopamine. | HT-29 grew into 3D tumor spheroids (TS) when co-cultured with fibroblasts. Fibroblasts demonstrated increased αSMA expression and migratory activity. |
| Ivich [77] | Immortalized PrECs, BHPrS1 | 3D | Prostate cancer physiology | Two stacked, z-shaped PDMS channels separated by a polyester membrane with a 0.8 μm pore size. Each channel consisted of 500 μm height, 1 mm width, and 40 mm length with a 20 mm overlapping segment of the microchannels. | Normal epithelium differentiation was induced and regulated by normal stroma. Normal stroma assumed a cancer-associated fibroblast phenotype when co-cultivated with cancerous epithelium. |
| Jiang [78] | Immortalized PrECs, BHPrS1, EMP, C4-2, 22Rv1 | 3D | Prostate cancer physiology; Invasion | Two stacked, z-shaped PDMS channels separated by a polyester membrane with either a 0.8 μm or 8 μm pore size. Each channel consists of 500 μm height, 1 mm width, and 34 mm length with a 20 mm overlapping segment of the microchannels. Tumor invasion studies were performed using devices with a serpentine channel overlaying a straight channel. | Tumor cells downregulated androgen receptor (AR) expression and induced CAF biomarkers in stromal fibroblasts. Both tumor cells and stromal CAFs migrated through the 8 μm pore size membrane and into their neighboring channel. |
| Graham [87] | ARCaPM androgen-independent mesenchymal prostate carcinoma | 3D | Invasion | Invasion assays performed using Boyden chambers with 8 μm pore size polycarbonate membrane inserts coated with Matrigel. | ZEB1 downregulation in ARCaPM cells resulted in a significant (8-fold) reduction of invasion through Matrigel compared to control siRNA-treated cells. |
| Siddiqui [88] | PNT2-C2, PC3, DU145 | 3D | Invasion | Chemotaxis assays performed using 8 μm Boyden chambers in 24-well plates with Matrigel coating. | Overexpression of CK2 blocked the repression of migration and invasion by PRH. PRH knockdown in prostate cells resulted in increased invasion and decreased E-cadherin expression. |
| Wei [90] | 1E8-H, 2B4-L human prostate epithelial cell lines | 3D | Invasion | 24-well Transwell chambers with 8 μm pore size polycarbonate filters. No mention of coating. | Vimentin transfection drastically increased invasion ability of 2B4-L cells and decreased invasion ability of 1E8-H cells. |
| Wang [91] | LNCaP, CWR22Rv1 | 3D | Invasion | 12-well chambers with 12 μm pore size filters and Matrigel coating. LNCaP-SOX9 cell invasion was monitored for 24 h. Noninvaded cells were scraped off, while invaded cells were collected and quantified with fluorescence dye. | A greater number of LNCaP-SOX9 cells migrated through Matrigel-coated filters compared to uninduced and parental cells, indicating that SOX9 expression enhances tumor invasion. |
| Wang [92] | LNCaP, PC3, DU145, RPWE-1 | 3D | Invasion | 24-well Transwell plate with 8 μm pore size polycarbonate filters. Upper chambers were coated with 50 μL Matrigel. | Knockdown of HOXA1 reduced the growth, invasion, and migration ability of DU145 and PC3. |
| Bonaccorsi [94] | PC3, DU145 | 3D | Invasion | Invasion assays performed using Boyden chambers overlayed with Matrigel-coated membranes. | The addition of an inhibitor of EGFR gefitinib decreased invasion of androgen-insensitive cell lines by inhibiting EGFR autotransphosphorylation and PI3K activation. |
| Hara [95] | MDA PCa 2b, androgen-independent MDA PCa 2b subline, 293T, LNCaP | 3D | Invasion | Invasion assays performed using Matrigel invasion chambers with 8 μm pore size membranes. | Invasive (MDA-I) cells demonstrated increased AR expression compared with MDA PCa2b parental cells as well as maintaining AR dependence. |
| Li [96] | PshTertAR (immortalized, AR-positive), PshTert (immortalized, AK-negative), PC3 | 3D | Invasion | BD Biocoat Matrigel invasion chambers were used with stromal cells added to lower chamber and PC3 placed on the insert. | Stromal cells lacking AR increased the invasion ability of PC3 in vitro. |
| Palm [97] | PC3, PC3-luc | 3D | Invasion | Norepinephrine and propranolol were mixed with PC3-luc in buffered type I collagen solution and filled into self-constructed chambers. | Treatment of cells with norepinephrine led to significant increase in migratory activity. |
| Ayala [98] | DU145, mouse ganglia/nerves, dorsal root ganglia/nerves (DRG) | 3D | Invasion | Perineural invasion coculture model consists of DU145 and DRG embedded in Matrigel. DU145 cultured as monolayer adherent cells in microchamber system. | 3 (NFκB, PIM-2, DAD-1) out of 15 genes overexpressed in DU145/DRG cocultures were known components of anti-apoptosis signaling pathways. |
| Sima [100] | PC3 | 3D | Invasion | The device consisted of 4 microreservoirs for cell culture and chemoattractant inputs connected by embedded glass channels. A panpipe-shaped polymeric scaffold in the device observation area consisted of 6 channels ranging from 6 to 21 μm in length. | PC3 migrated through channel lengths of 11 μm, 14 μm, and 21 μm in under 2 h by splitting into vesicular fragments and reassembling into single bodies. |
| Molter [101] | PC3, DU145, 22Rv1, LNCaP | 2D | Invasion | PDMS substrates of varying stiffness were prepared by mixing different concentrations of Sylgard 184 PDMS cross-linking agent with the PDMS mixture. Stiffnesses of 1 kPa (resembling soft lymph node and brain tissue), 3 kPa (resembling normal prostate tissue), 12 kPa (resembling stiffened prostate tumor microenvironment), and 50 kPa (resembling non-mineralized bone environment) were used. | Substrate stiffness influenced the migratory behavior, contractility, and modulation of cell stiffness of prostate cancer cells. Aggressive cells (DU145 and PC3) exerted higher contractile stress compared to tumorigenic and lowly metastatic cells (22Rv1 and LNCaP). |
| Lopez-Cavestany [102] | DU145, PC3 | 2D | Invasion | Substrates of varying stiffness were used to investigate the role of stiffness in progression of the EMT phenotype. Two PA gels were used at stiffnesses of 5 kPa and 60 kPa, and a final glass substrate with a stiffness of 72 GPa was used as a positive control. | Increased matrix stiffness increased calcium steady-state concentration, increased vimentin expression, and decreased E-cadherin expression. |
| Ao [103] | NAFs, CAFs, SCC61 | 3D | Invasion | PDMS with vacuum chambers on either side of a suspended middle chamber (5 mm length, 1 mm width, 100 μm height) with a suspended PDMS membrane (10 μm thick) | Stretched normal tissue-associated fibroblasts altered the structure of secreted fibronectin and enhance cancer cell migration. |
| Jouybar [104] | MCF-7, MDA-MB-231, MCF-10A | 3D | Invasion | PDMS devices were fabricated using soft lithography methods to achieve a channel height of 100μm, and the PDMS slabs were bonded to glass slides. A temperature control platform was created using a Low Force Stereolithography 3D printer and bonded to glass slides. Cells were encapsulated in Matrigel and placed in a droplet maker chip to create hydrogel droplets. Cells containing beads were sandwiched between two collagen I layers. | Highly invasive (MDA-MB-231) cells invaded the surrounding matrix in a single-cell manner, whereas poorly invasive (MCF-7) cells did so collectively. |
| Khodavirdi [109] | LNCaP (androgen-sensitive adenocarcinoma), PC3 (human prostate carcinoma) | 3D | Intravasation | Matrigel invasion assays performed with 8 μm pore size membrane inserts. | Osteopontin overexpression enhanced the invasive ability significantly for LNCaP and somewhat for PC3. Anti-osteopontin antibodies in invasion assays significantly suppressed the response to osteopontin overexpression. |
| Conn [110] | PC-lo/diss, PC-hi/diss, HMVECs (human microvascular endothelial cells), CEFs (chick embryonic fibroblasts | 3D | Intravasation | 96-well clusters were coated with 5 μg/mL type I collagen, 10 μg/mL fibronectin, or 10 μg/mL Matrigel for adhesion assays. For invasion assays, cells were plated on 24-well clusters with 8 μm size pores with 2 μg/mL Matrigel. | Western blot and qPCR showed substantial reduction of epithelial marker E-cadherin in PC-hi/diss and demonstrated increased ability to invade through Matrigel compared to PC-lo/diss. |
| Zervantonakis [115] | HT1080 human fibrosarcoma, MDA231 breast carcinoma, primary MVEC, macrovascular endothelial cells. RAW264.7 | 3D | Intravasation | 3D ECM hydrogel sandwiched between two microfluidic channels (500 μm wide, 20 mm length, and 120 μm height). | Permeability measurements indicated that signaling with macrophages, via secretion of tumor necrosis factor-α, degraded the endothelial barrier and increased intravasation rates. |
| Li [116] | MDA-MB-231, PC3, MDA-MB-435S, Raw 264.7 mouse macrophages. | 3D | Intravasation | Collagen gel sandwiched between two microchannels (500 μm width) in PDMS devices. | The presence of macrophages enhanced the speed and persistence of PC3 cell migration in an MMP-dependent fashion. |
| Shin [119] | Metastatic LOVO, non-metastatic SW480 | 3D | Intravasation-Extravasation | Device consists of two parts; intravasation chamber for 3D culture using Matrigel, and extravasation chamber for detection of metastasized cells. | Invasion of LOVOs was higher compared to SW480. Treatment of cells with MMP inhibitors decreased invasion. |
| Cui [120] | Primary human vascular endothelial cells, MDA-MB-231, MCF-10A. | 3D | Intravasation-Extravasation | Porous membrane (20 μm thickness, 4 mm by 4 mm area) sandwiched between two flow layers fabricated using soft lithography for PDMS. Underneath the layer is an accessible microchamber for cell collection. | Migratory MDA-MB-231 cells exhibited a higher body aspect ratio and faster planar migration compared to non-migratory cells. |
| Sima [123] | PC3 | 3D | Intravasation-Extravasation | L-shaped glass biochip fabricated by femtosecond laser-assisted etching. Two microreservoir inlets and one microreservoir for collecting migrated cells (1000 μm diameter, 280 μm height). Two embedded connecting channels (1500 μm length, 60 μm height). One channel consisted of two rows of glass elliptical pillars (150 μm diameter) 200 μm apart. Collagen coating. | PC3 cells migrated through narrow submicrometer channels with speeds up to 1.5 μm/min. The cells retained viability during and after migration, and the probability of proliferation was unchanged. |
| Stott [139] | Serum specimens from healthy and metastatic prostate cancer patients | 3D | CTCs | CTC-Chip with a surface area of 970 mm2 and 78,000 microposts coated with antibodies to EpCAM. Image processing algorithms used with scoring criteria to analyze CTCs in a 3D matrix. | CTCs in blood circulation had a short half-life for patients with preoperative CTCs. |
| Kirby [140] | Peripheral blood samples from healthy and metastatic castrate-resistant prostate cancer patients | 3D | CTCs | Oxygen plasma deep reactive ion etcher used to etch to a depth of 100 μm. PDMS sheets (3 mm thick) were clamped to the top of the device to create closed channels populated with post arrays. | Median of 54 CTCs/mL captured in CRPC patients versus 3 in healthy donors. Chip design allowed for monitoring of drug-target engagement. |
| Au [143] | Breast or melanoma patient liquid biopsies | 3D | CTCs | Devices mimicked hydrodynamic properties of capillary networks (ΔP = 5–58 mm Hg) by tapering 16 parallel microchannels (50 μm diameter) into 5 μm, 7 μm, or 10 μm constrictions. | Clusters transited through capillaries in a single-file manner. |
| Vigmostad [144] | PC3, PrEC LH | 3D | CTCs | Micropipette puller, microforge, micromanipulator, and thin-walled glass capillaries (5–8 μm internal diameter) used to partially aspirate a suspended cell and record measurements at various suction pressures. | PrEC LH cells were 140% stiffer than PC3 without exposure to FSS and experienced no significant change after FSS exposure. The Young’s modulus after exposure to high and low FSS increased for PC3. |
| Marcolino [148] | PNT2-C2, PC3, HuVEC | 3D | Extravasation | In vitro extravasation assays performed using transwell chambers with Matrigel coating. | Endogenous PRH knockdown led to significant decrease in extravasation. |
| Manuelli [155] | Human prostate cancer cells (1532-CP2TX, 1535-CP1TX, 1542-CP3TX), AsPC-1 human pancreatic tumor cells, PC3. | 3D | Extravasation | Coverslips were coated with Cy3-conjugated gelatine. | All cancer cell lines except for PC3 demonstrated the ability to synthesize invadopodia. |
| Lautscham [158] | A125 lung carcinoma, MDA-MB-231, HT-1080, primary breast cancer cells (IFDUC1) | 3D | Extravasation | PDMS devices with a stiffness of 1.77 mPa and linear channel segments (20 μm length, 3.7 μm height, decreasing width from 11.2 to 1.7 μm) were used to measure the migratory ability of cells. Self-assembled collagen networks (550 Pa) with 3 μm pore size were used to investigate migratory behavior in a soft environment. | The nucleus was the limiting biophysical factor for 3D invasion. Cell stiffness was weakly correlated with invasiveness. |
| Gakhar [163] | PC3, C4-2, LNCaP, MDA PCa 2b, KGI | 3D | CTCs, Extravasation | Microrenathane tubes (50 cm length, 300 μm diameter) were incubated with 10 μg/mL human recombinant IgG E-selectin and mounted on a microscope. Known concentrations of cells were perfused over the surface to measure interactions with E-selectin. | CTCs from prostate cancer patients tethered and interacted with E-selectin and E-selectin expressing HUVECs. |
| Chen [166] | GFP or RFP-expressing HUVEC, NHLF (normal human lung fibroblasts), MDA-MB-231, A-375 MA2, 4T1, SUM 159 | 3D | Extravasation | Three ECM hydrogel regions (1.3 mm width, 110 μm height, 0.8 cm length) separated by media channels and held in place via small trapezoidal microposts. | β1-depleted cells could not sustain protrusions into the matrix compared to control cells, suggesting β1 is a requirement for invasion through the endothelial basement membrane. |
| Verbruggen [169] | MLO-Y4 osteocyte-like mouse cell line, MDA-MB-231, MCF-7, PC3, LNCaP | 3D | Extravasation | PDMS device containing two parallel microchannels separated by PDMS membrane (2% porosity) for cancer cell and osteocyte co-culture. Channels were coated with collagen I. Mechanical stimulation was generated using increased flow rate (1000 μL/h compared to 30 μL/h) in osteocyte channel. | Mechanical stimulation of osteocytes led to increased invasion of breast and prostate cancer cells and may prohibit the suppression of metastasis. |
| Shulby [173] | PC3 N, PC3 ML (bone metastatic human prostate carcinoma), LNCaP, hFOB (human osteoblasts), human MDA PCa 2b, DU145 | 3D | Bone tropism | Flow chamber cell adhesion assay performed using 24 × 50 mm glass coverslips coated with collagen and fibronectin. Cell migration assay performed by plating cells on FluoroBlock insert (8 μm pore size) in a 24-well plate. | Bone-derived prostate cancer cells adhered to bone marrow endothelial cells under flow. |
| Dimitroff [175] | Human HPC KG1a, murine monocytic WEHI-3, Human prostate tumor MDA PCa 2b, PC3, PC3M, PC3M Pro-4, PC3M LN-4, PC-R1, PC-E1, LNCaP, LNCaP Pro-5, LNCaP LN-3 | 3D | Bone tropism | Cell rolling assessed at 0.6 dynes/cm2 at 100× magnification using parallel-plate flow analysis. E-selectin/immunoglobulin-reactive 150 kDa membrane proteins analyzed using MALDI-TOF mass spectrometry. | PSGL-1 expression may be associated with bone metastasis. Bone metastasis of prostate cancer may mirror the process of HPC homing to bone. |
| Sottnik [177] | MLO-Y4 (murine osteocytes), DU145, LNCaP, PC3, BPH-1, H441, A549, MDA-MB-231, MCF7 | 3D | Bone tropism | Cells were seeded into Thermo Fisher Scientific Opticell cassettes. Hydrostatic pressure was adjusted using an IV bag containing cell culture media. | Applying pressure to osteocytes induced prostate cancer growth and invasion via the upregulation of CCL5 and MMP. |
| Hsiao [178] | PC3, HUVEC, MC3T3-E1 | 3D | Bone tropism | PDMS device with two stacked channels separated by semi-permeable 5 μm pore size polycarbonate membrane. Upper channel (200 μm height, 50 μm width) had 28 side channels (200 × 200 × 200 μm) and was used for cell capture. Lower channel (100 μm height, 2 mm width). Membrane surfaces treated with 1% w/v Pluronic F108. | Proliferation rate of PC3 was greatly decreased without a reduction in viability. |
| Bischel [179] | LNCaP, C4-2B, MC3T3, MC3T3-E1 | 3D | Bone tropism | ECM hydrogel in a microfluidic channel. | Bone metastatic LNCaPs (C4-2Bs) demonstrated increased invasive ability compared to LNCaP in co-culture with osteoblasts. |
| Ahn [180] | SW620 (colorectal cancer cells), MKN74 (gastric cancer cells), HUVEC | 3D | Colorectal and gastric cancer metastasis to the bone | PDMS single-channel devices (800 μm width) were bonded to glass coverslips with ports for hydrogel injection and medium reservoirs. | High concentrations of hydroxyapatite drastically reduced migration of SW620 and MKN72. |
| Mei [181] | MLO-Y4, RAW264.7, MDA-MB-231, HUVEC | 3D | Breast cancer metastasis to the bone | Double channel PDMS microfluidic device with fibronectin coating. Lumen channel was coated with Matrigel and collagen mixture. Custom microfluidic pump designed to operate in oscillating fashion. | Mechanical stimulation of osteocytes reduced breast cancer extravasation via reduction of extravasation distance and percentage of extravasated side-channels. |
| Jasuja [182] | hMSCs (PT-2501), PC3 | 3D | Bone tropism | Biocompatible crosslinked PMMA device with a rectangular culture chamber (50 mm × 30 mm × 32 mm) each supporting a scaffold sample were exposed to two flow rates (0.2 mL/min and 0.05 mL/min). A gas permeable membrane on top of the chamber permitted gas exchange with the culture chamber. | CXCR4 upregulation in bone led to a high migration rate of PC3. |
| Osawa [183] | HS5 (human bone stromal cells), PC3-GFP, C4-2B | 3D | Bone tropism | 6-well dish was used to create a recirculating system with primary tumor and metastatic sites. PE tubing coated with collagen I was used to connect the primary and metastatic sites to each other as well as to a peristaltic pump. | Macrofluidic model demonstrated cell migration from primary sites to metastatic sites. |
| Wheeler [195] | MDA-MB-231, MCF7, hepatocytes, NPC (neural progenitor cells) | 3D | Dormancy and colonization | Scaffolds of commercially available LiverChip device (CN Bio Innovations Limited) were coated with 1% rat tail collagen type I and seeded with hepatocytes and NPCs. | Breast cancer cells integrated into hepatic niche and entered quiescence and therefore did not interfere with hepatocyte function. |
| Hassell [198] | H1975 human NSCLC adenocarcinoma cells, primary lung alveolar cells | 3D | Dormancy and colonization | Bilayer PDMS microfluidic device (top channel: 1 mm width, 1 mm height; bottom channel: 1 mm width, 200 μm height) with a porous ECM-coated membrane (0.4 μm or 9 μm pore size). Cyclic suction was applied to two parallel side chambers to mimic physiological breathing motion. | Lung cancer cell growth and invasion were sensitive to cues associated with breathing motions. |
| Ma [199] | Human foreskin fibroblast cells, K-562, Jurkat cells | 3D | Dormancy and colonization | PDMS microfluidic device with a unique droplet collection chamber design and filters to prevent debris. The channel height was comparable to that of a cell diameter. | Droplet microfluidic technology allowed for the characterization of metabolic differences between proliferating and quiescent cells. |
| Liu [201] | REF/E23 derived from rat embryonic fibroblasts REF52 | 3D | Dormancy and colonization | PDMS microfluidic devices bonded with glass slides. Channels were coated with 2% fibronectin. | Increasing flow rate as well as increased extracellular factor replacement drove cells to shallower quiescence. |
4. Prostate Cancer Detection
4.1. Prostate Cancer Biomarkers
4.1.1. Prostate-Specific Antigen (PSA)
4.1.2. Circulating Tumor Cells (CTCs)
4.1.3. Extracellular Vesicles (EVs)
4.1.4. Urine
5. Prostate Cancer Therapy
5.1. Drug Discovery and Screening
5.2. Prostate Cancer Resistance to Treatment and Management
- Summary of selected microfluidic systems used in prostate cancer research (Table 1. continued).
| Reference | Cells/Samples Used | Culture Type | Field of Investigation | Device Properties | Findings |
| Annese [208] | Plasma samples from healthy men and men with prostate cancer | 3D | Detection of prostate cancer (PSA) | Disposable chip cartridge (120 PGA chip package, CMOS chip, microfluidic capillary network, and reagents), reader (STM32F334R8T6 microcontroller on an ST Nucleo F334R8 board, 8.5 × 7.5 × 4.0 cm, 150 g weight), and GUI (custom software) | System could detect prostate cancer with a sensitivity of 94% and specificity of 70%. |
| Petricoin [215] | Serum samples from: asymptomatic men aged ≥50 years; normal healthy men; men undergoing radical prostatectomy, (pre- and postoperative); | 2D | Detection of prostate cancer (PSA, serum proteomics) | Thawed sera were applied to a C16 hydrophobic interaction protein chip. SELDI-TOF serum profiling and bioinformatics algorithm used to analyze samples and distinguish between cancerous and benign prostate conditions over a range of PSA levels. | Serum proteomics could distinguish prostate cancer with 95% sensitivity, even when PSA levels were in an indeterminate range (4–10 ng/mL). Test had a high clinical relevance as a complement to physical exams, imaging, and serum PSA levels. |
| Fernández-Sánchez [216] | f-PSA and t-PSA stock solutions | 2D | Detection of prostate cancer (PSA) | Integrated single-use immunosensor with nitrocellulose membrane coated with f-PSA and t-PSA antibodies. Storage blister with urea solution allowed for washing away unbound species. Impedance spectra were used to detect the specific affinity event. | PSA concentrations were detected down to 3 ng/mL and allowed for visual detection via colloidal gold antibody tracers. |
| Triroj [217] | PSA in complex with GOx enzyme | 2D | Detection of prostate cancer (PSA) | Biochemical sensing platform with a working electrode (5 × 5 array of <100 nm pores) milled using an ion beam and I2 gas, PDMS microchannels (30 μm height), and microelectrode platform. Nanoelectrodes were functionalized to detect PSA-GOx complex via cyclic voltammetry. | PSA concentration could be detected as low as 10 pg/mL. |
| Chiriacò [218] | Prepared solutions with varying PSA ratios | 2D | Detection of prostate cancer (PSA) | PDMS biochip with a microfluidic module (7 mm × 4 mm × 100μm height) and two transducer arrays of gold interdigitated microelectrode sensing platforms. Electrodes were functionalized to calibrate for f-PSA and PSA in complex with ACT. | PSA ratios could be calculated to identify cases of prostate cancer or BPH with distinction. |
| Zhau [222] | LNCaP, normal human prostatic fibroblasts | 3D | Detection of prostate cancer (PSA) | Slow-Turning Lateral Vessel (STLV) seeded with Cytodex-3 microcarriers at a density of 5 mg/mL. Vessels were rotated at 25–30 rpm. | DHT induced differentiation-promoting behavior of LNCaP in microgravity-simulated conditions. LNCaP expressed high levels of PSA mRNA and protein under coculture with fibroblasts. |
| Kuske [244] | Samples from 86 prostate cancer patients (median age 67) prior to radical prostatectomy | 2D | Detection of prostate cancer (CTCs) | Combined analysis from three CTC assays (CellSearch, CellCollector, and EPISPOT). | CTC detection by EPISPOT prior to radical prostatectomy significantly correlated with PSA serum values. |
| Gila [247] | PC3, MCF-7, blood samples from patients with localized and metastatic prostate cancer | 3D | Detection of prostate cancer (CTCs) | Herringbone–microfluidic channel-less probe with EpCAM, PSMA, and PSA captured antibody stripes. Blood is injected from the central aperture and aspirated from crescent-shaped peripheral apertures. | CTCs were captured from blood samples as they traversed several antibody capture lines. |
| Cho [248] | Peripheral blood samples from patients with localized prostate cancer, mCRPC, or mHSPC | 3D | Detection of prostate cancer (CTCs) | Microseparater with disposable substrate, two inlets and outlets, vacuum trench, and reusable substrate with ferromagnetic wires. | Successful microfluidic isolation of CTCs indicated increased CTC count with progressing stages of prostate cancer. |
| Wang [254] | Exosomes extracted from LNCaP and PrEC (enriched with anti-CD63 magnetic nanoparticles), serum samples from 10 prostate cancer patients and 8 healthy cases | 2D | Detection of prostate cancer (extracellular vesicles) | PDMS devices (SU8-2075 negative photoresist) bonded to glass slides. Raman spectra were collected on a confocal micro-Raman system. | Exosomes from clinical samples could be analyzed within 1 h at a limit of 1.6 × 102 particles/mL with 20 μm samples. |
| Rzhevskiy [261] | DU145, midstream urine samples from 14 healthy patients and 14 patients with localized prostate cancer | 3D | Detection of prostate cancer (urine) | PDMS spiral microchannel device bonded to PDMS. Anti-Glypican-1 used as the primary antibody for identification of collected tumor cells. | Device could capture DU145 cells with >85% efficiency and was functional in 79% of cases for capturing cells from urine samples of patients with localized prostate cancer. |
| Borkowetz [263] | PNT2 human normal prostate epithelium, LNCaP clone FGC and 11Rv1 | 3D | Detection of prostate cancer (urine) | Three microchannels as a positive control (biocompatible with PPOx), negative control, and test (limit non-specific binding between surface-bound PSMA antibodies) channels. | Biosensing platform was able to identify and capture cells with a sensitivity and specificity of 72.4% and 71.4%, respectively. |
| Chan [265] | PNT2, LNCaP clone FGC, 22rv1, prostate cancer patient urine samples | 3D | Detection of prostate cancer (urine) | PMMA microfluidic channels coated with polyoxazoline. | Photodynamic diagnostic with immunocapture could detect prostate cancer biomarkers without prior DRE with a sensitivity of 72.4% and specificity of 71.4% |
| Lang [272] | MDA-MB-468, PC3 | 3D | Prostate cancer therapy | Mixed cells with buffered collagen solution, neurotransmitters, and pharmacological substances. Cell–collagen mixture was filled into self-constructed migration chambers. Selected 30 cells in each sample and recorded migration every 15 min for 12 h. | Strong increase in migratory activity of PC3 cells as a result of norepinephrine treatment. β1-specific blocker atenolol partially reduced migration; β2-specific blocker ICI 118,771 entirely inhibited norepinephrine induction. |
| An [273] | PC3 | 3D | Prostate cancer therapy | PDMS device consisting of two layers. The first is a fluidic layer with a diffusive mixer and microchambers (100μL volume) for cell culture. The second is a pneumatic layer with 10 channels to control microvalves in the fluidic layer. | The optimal concentration of curcumin for sensitizing PC3 cells at lower-dose TRAIL treatment was determined. |
6. Summary
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Key Statistics for Prostate Cancer | Prostate Cancer Facts. Available online: https://www.cancer.org/cancer/types/prostate-cancer/about/key-statistics.html (accessed on 23 May 2023).
- Goddard, E.T.; Bozic, I.; Riddell, S.R.; Ghajar, C.M. Dormant Tumour Cells, Their Niches and the Influence of Immunity. Nat. Cell Biol. 2018, 20, 1240–1249. [Google Scholar] [CrossRef] [PubMed]
- Koukourakis, I.M.; Platoni, K.; Kouloulias, V.; Arelaki, S.; Zygogianni, A. Prostate Cancer Stem Cells: Biology and Treatment Implications. Int. J. Mol. Sci. 2023, 24, 14890. [Google Scholar] [CrossRef]
- Lambert, A.W.; Pattabiraman, D.R.; Weinberg, R.A. Emerging Biological Principles of Metastasis. Cell 2017, 168, 670–691. [Google Scholar] [CrossRef] [PubMed]
- Páez, D.; Labonte, M.J.; Bohanes, P.; Zhang, W.; Benhanim, L.; Ning, Y.; Wakatsuki, T.; Loupakis, F.; Lenz, H.-J. Cancer Dormancy: A Model of Early Dissemination and Late Cancer Recurrence. Clin. Cancer Res. 2012, 18, 645–653. [Google Scholar] [CrossRef] [PubMed]
- Massagué, J.; Obenauf, A.C. Metastatic Colonization by Circulating Tumour Cells. Nature 2016, 529, 298–306. [Google Scholar] [CrossRef]
- Hoarau-Véchot, J.; Rafii, A.; Touboul, C.; Pasquier, J. Halfway between 2D and Animal Models: Are 3D Cultures the Ideal Tool to Study Cancer-Microenvironment Interactions? Int. J. Mol. Sci. 2018, 19, 181. [Google Scholar] [CrossRef]
- Thomas, R.S.; Black, M.B.; Li, L.; Healy, E.; Chu, T.-M.; Bao, W.; Andersen, M.E.; Wolfinger, R.D. A Comprehensive Statistical Analysis of Predicting In Vivo Hazard Using High-Throughput In Vitro Screening. Toxicol. Sci. 2012, 128, 398–417. [Google Scholar] [CrossRef]
- Selimović, Š.; Dokmeci, M.R.; Khademhosseini, A. Organs-on-a-Chip for Drug Discovery. Curr. Opin. Pharmacol. 2013, 13, 829–833. [Google Scholar] [CrossRef]
- Frantz, C.; Stewart, K.M.; Weaver, V.M. The Extracellular Matrix at a Glance. J. Cell Sci. 2010, 123, 4195–4200. [Google Scholar] [CrossRef]
- Swartz, M.A.; Fleury, M.E. Interstitial Flow and Its Effects in Soft Tissues. Annu. Rev. Biomed. Eng. 2007, 9, 229–256. [Google Scholar] [CrossRef]
- Mak, I.W.; Evaniew, N.; Ghert, M. Lost in Translation: Animal Models and Clinical Trials in Cancer Treatment. Am. J. Transl. Res. 2014, 6, 114–118. [Google Scholar] [PubMed]
- Niculescu, A.-G.; Chircov, C.; Bîrcă, A.C.; Grumezescu, A.M. Fabrication and Applications of Microfluidic Devices: A Review. Int. J. Mol. Sci. 2021, 22, 2011. [Google Scholar] [CrossRef] [PubMed]
- Pattanayak, P.; Singh, S.K.; Gulati, M.; Vishwas, S.; Kapoor, B.; Chellappan, D.K.; Anand, K.; Gupta, G.; Jha, N.K.; Gupta, P.K.; et al. Microfluidic Chips: Recent Advances, Critical Strategies in Design, Applications and Future Perspectives. Microfluid. Nanofluid. 2021, 25, 99. [Google Scholar] [CrossRef]
- Berlanda, S.F.; Breitfeld, M.; Dietsche, C.L.; Dittrich, P.S. Recent Advances in Microfluidic Technology for Bioanalysis and Diagnostics. Anal. Chem. 2021, 93, 311–331. [Google Scholar] [CrossRef]
- Regmi, S.; Poudel, C.; Adhikari, R.; Luo, K.Q. Applications of Microfluidics and Organ-on-a-Chip in Cancer Research. Biosensors 2022, 12, 459. [Google Scholar] [CrossRef]
- Preetam, S.; Nahak, B.K.; Patra, S.; Toncu, D.C.; Park, S.; Syväjärvi, M.; Orive, G.; Tiwari, A. Emergence of Microfluidics for next Generation Biomedical Devices. Biosens. Bioelectron. X 2022, 10, 100106. [Google Scholar] [CrossRef]
- Kumari, S.; Saha, U.; Bose, M.; Murugan, D.; Pachauri, V.; Sai, V.V.R.; Madaboosi, N. Microfluidic Platforms for Single Cell Analysis: Applications in Cellular Manipulation and Optical Biosensing. Chemosensors 2023, 11, 107. [Google Scholar] [CrossRef]
- Roman, G.T.; Kennedy, R.T. Fully Integrated Microfluidic Separations Systems for Biochemical Analysis. J. Chromatogr. A 2007, 1168, 170–188. [Google Scholar] [CrossRef]
- Franzen, N.; Van Harten, W.H.; Retèl, V.P.; Loskill, P.; Van Den Eijnden-van Raaij, J.; IJzerman, M. Impact of Organ-on-a-Chip Technology on Pharmaceutical R&D Costs. Drug Discov. Today 2019, 24, 1720–1724. [Google Scholar] [CrossRef]
- Ayuso, J.M.; Virumbrales-Muñoz, M.; Lang, J.M.; Beebe, D.J. A Role for Microfluidic Systems in Precision Medicine. Nat. Commun. 2022, 13, 3086. [Google Scholar] [CrossRef]
- Akgönüllü, S.; Bakhshpour, M.; Pişkin, A.K.; Denizli, A. Microfluidic Systems for Cancer Diagnosis and Applications. Micromachines 2021, 12, 1349. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; Chen, H.; Xu, D.; Liu, R.; Zhao, Y. Developing Organs-on-chips for Biomedical Applications. Smart Med. 2024, 3, e20240009. [Google Scholar] [CrossRef] [PubMed]
- Huh, D.; Kim, H.J.; Fraser, J.P.; Shea, D.E.; Khan, M.; Bahinski, A.; Hamilton, G.A.; Ingber, D.E. Microfabrication of Human Organs-on-Chips. Nat. Protoc. 2013, 8, 2135–2157. [Google Scholar] [CrossRef]
- Novak, R.; Ingram, M.; Marquez, S.; Das, D.; Delahanty, A.; Herland, A.; Maoz, B.M.; Jeanty, S.S.F.; Somayaji, M.R.; Burt, M.; et al. Robotic Fluidic Coupling and Interrogation of Multiple Vascularized Organ Chips. Nat. Biomed. Eng. 2020, 4, 407–420. [Google Scholar] [CrossRef]
- Han, S.J.; Park, H.-K.; Kim, K.S. Applications of Microfluidic Devices for Urology. Int. Neurourol. J. 2017, 21 (Suppl. S1), S4–S9. [Google Scholar] [CrossRef]
- Bernstein, D.E.; Piedad, J.; Hemsworth, L.; West, A.; Johnston, I.D.; Dimov, N.; Inal, J.M.; Vasdev, N. Prostate Cancer and Microfluids. Urol. Oncol. Semin. Orig. Investig. 2021, 39, 455–470. [Google Scholar] [CrossRef]
- Sassi, A.; You, L. Microfluidics-Based Technologies for the Assessment of Castration-Resistant Prostate Cancer. Cells 2024, 13, 575. [Google Scholar] [CrossRef] [PubMed]
- Toivanen, R.; Shen, M.M. Prostate Organogenesis: Tissue Induction, Hormonal Regulation and Cell Type Specification. Development 2017, 144, 1382–1398. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer Statistics, 2016. CA A Cancer J. Clin. 2016, 66, 7–30. [Google Scholar] [CrossRef]
- Attard, G.; Parker, C.; Eeles, R.A.; Schröder, F.; Tomlins, S.A.; Tannock, I.; Drake, C.G.; De Bono, J.S. Prostate Cancer. Lancet 2016, 387, 70–82. [Google Scholar] [CrossRef]
- Cunha, G.R.; Vezina, C.M.; Isaacson, D.; Ricke, W.A.; Timms, B.G.; Cao, M.; Franco, O.; Baskin, L.S. Development of the Human Prostate. Differentiation 2018, 103, 24–45. [Google Scholar] [CrossRef] [PubMed]
- Aaron, L.; Franco, O.E.; Hayward, S.W. Review of Prostate Anatomy and Embryology and the Etiology of Benign Prostatic Hyperplasia. Urol. Clin. N. Am. 2016, 43, 279–288. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.Z.; Wong, Y.C. Sex Hormone-Induced Prostatic Carcinogenesis in the Noble Rat: The Role of Insulin-like Growth Factor-1 (IGF-1) and Vascular Endothelial Growth Factor (VEGF) in the Development of Prostate Cancer. Prostate 1998, 35, 165–177. [Google Scholar] [CrossRef]
- Van Leenders, G.J.L.H.; Schalken, J.A. Epithelial Cell Differentiation in the Human Prostate Epithelium: Implications for the Pathogenesis and Therapy of Prostate Cancer. Crit. Rev. Oncol./Hematol. 2003, 46, 3–10. [Google Scholar] [CrossRef]
- Uzgare, A.R.; Xu, Y.; Isaacs, J.T. In Vitro Culturing and Characteristics of Transit Amplifying Epithelial Cells from Human Prostate Tissue. J. Cell. Biochem. 2004, 91, 196–205. [Google Scholar] [CrossRef] [PubMed]
- Whitacre, D.C.; Chauhan, S.; Davis, T.; Gordon, D.; Cress, A.E.; Miesfeld, R.L. Androgen Induction of in Vitro Prostate Cell Differentiation. Cell Growth Differ. 2002, 13, 1–11. [Google Scholar]
- Heer, R.; Robson, C.N.; Shenton, B.K.; Leung, H.Y. The Role of Androgen in Determining Differentiation and Regulation of Androgen Receptor Expression in the Human Prostatic Epithelium Transient Amplifying Population. J. Cell. Physiol. 2007, 212, 572–578. [Google Scholar] [CrossRef]
- Lamb, D.J.; Weigel, N.L.; Marcell, M. Androgen Receptors and Their Biology. In Vitamins & Hormones; Elsevier: Amsterdam, The Netherlands, 2001; Volume 62, pp. 199–230. ISBN 978-0-12-709862-3. [Google Scholar]
- Lamb, L.E.; Knudsen, B.S.; Miranti, C.K. E-Cadherin-Mediated Survival of Androgen-Receptor-Expressing Secretory Prostate Epithelial Cells Derived from a Stratified in Vitro Differentiation Model. J. Cell Sci. 2010, 123, 266–276. [Google Scholar] [CrossRef]
- Nelson, C.M.; Bissell, M.J. Of Extracellular Matrix, Scaffolds, and Signaling: Tissue Architecture Regulates Development, Homeostasis, and Cancer. Annu. Rev. Cell Dev. Biol. 2006, 22, 287–309. [Google Scholar] [CrossRef]
- Huber, D.; Oskooei, A.; Casadevall i Solvas, X.; deMello, A.; Kaigala, G.V. Hydrodynamics in Cell Studies. Chem. Rev. 2018, 118, 2042–2079. [Google Scholar] [CrossRef]
- Tarbell, J.M.; Weinbaum, S.; Kamm, R.D. Cellular Fluid Mechanics and Mechanotransduction. Ann. Biomed. Eng. 2005, 33, 1719–1723. [Google Scholar] [CrossRef] [PubMed]
- Lutolf, M.P.; Hubbell, J.A. Synthetic Biomaterials as Instructive Extracellular Microenvironments for Morphogenesis in Tissue Engineering. Nat. Biotechnol. 2005, 23, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Huh, D.; Hamilton, G.A.; Ingber, D.E. From 3D Cell Culture to Organs-on-Chips. Trends Cell Biol. 2011, 21, 745–754. [Google Scholar] [CrossRef] [PubMed]
- Sosa-Hernández, J.E.; Villalba-Rodríguez, A.M.; Romero-Castillo, K.D.; Aguilar-Aguila-Isaías, M.A.; García-Reyes, I.E.; Hernández-Antonio, A.; Ahmed, I.; Sharma, A.; Parra-Saldívar, R.; Iqbal, H.M.N. Organs-on-a-Chip Module: A Review from the Development and Applications Perspective. Micromachines 2018, 9, 536. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Chen, J.; Bai, H.; Wang, H.; Hao, S.; Ding, Y.; Peng, B.; Zhang, J.; Li, L.; Huang, W. An Overview of Organs-on-Chips Based on Deep Learning. Research 2022, 2022, 9869518. [Google Scholar] [CrossRef]
- Dolega, M.E.; Wagh, J.; Gerbaud, S.; Kermarrec, F.; Alcaraz, J.-P.; Martin, D.K.; Gidrol, X.; Picollet-D’hahan, N. Facile Bench-Top Fabrication of Enclosed Circular Microchannels Provides 3D Confined Structure for Growth of Prostate Epithelial Cells. PLoS ONE 2014, 9, e99416. [Google Scholar] [CrossRef]
- Jiang, L.; Ivich, F.; Tahsin, S.; Tran, M.; Frank, S.B.; Miranti, C.K.; Zohar, Y. Human Stroma and Epithelium Co-Culture in a Microfluidic Model of a Human Prostate Gland. Biomicrofluidics 2019, 13, 064116. [Google Scholar] [CrossRef]
- Dondossola, E.; Paindelli, C. In Vitro Three-Dimensional Modeling for Prostate Cancer. In Biomaterials for 3D Tumor Modeling; Elsevier: Amsterdam, The Netherlands, 2020; pp. 251–286. ISBN 978-0-12-818128-7. [Google Scholar]
- Centenera, M.M.; Hickey, T.E.; Jindal, S.; Ryan, N.K.; Ravindranathan, P.; Mohammed, H.; Robinson, J.L.; Schiewer, M.J.; Ma, S.; Kapur, P.; et al. A Patient-derived Explant ( PDE ) Model of Hormone-dependent Cancer. Mol. Oncol. 2018, 12, 1608–1622. [Google Scholar] [CrossRef]
- Young, E.W.K. Cells, Tissues, and Organs on Chips: Challenges and Opportunities for the Cancer Tumor Microenvironment. Integr. Biol. 2013, 5, 1096. [Google Scholar] [CrossRef]
- Liu, X.; Fang, J.; Huang, S.; Wu, X.; Xie, X.; Wang, J.; Liu, F.; Zhang, M.; Peng, Z.; Hu, N. Tumor-on-a-Chip: From Bioinspired Design to Biomedical Application. Microsyst. Nanoeng. 2021, 7, 50. [Google Scholar] [CrossRef]
- Knudsen, B.S.; Vasioukhin, V. Mechanisms of Prostate Cancer Initiation and Progression. In Advances in Cancer Research; Elsevier: Amsterdam, The Netherlands, 2010; Volume 109, pp. 1–50. ISBN 978-0-12-380890-5. [Google Scholar]
- Strand, D.W.; Goldstein, A.S. The Many Ways to Make a Luminal Cell and a Prostate Cancer Cell. Endocr.-Relat. Cancer 2015, 22, T187–T197. [Google Scholar] [CrossRef] [PubMed]
- Roberts, J.A.; Zhou, M.; Park, Y.W.; Ro, J.Y. Intraductal Carcinoma of Prostate: A Comprehensive and Concise Review. Korean J. Pathol. 2013, 47, 307. [Google Scholar] [CrossRef] [PubMed]
- Baig, F.A.; Hamid, A.; Mirza, T.; Syed, S. Ductal and Acinar Adenocarcinoma of Prostate: Morphological and Immunohistochemical Characterization. Oman Med. J. 2015, 30, 162–166. [Google Scholar] [CrossRef]
- Ranasinha, N.; Omer, A.; Philippou, Y.; Harriss, E.; Davies, L.; Chow, K.; Chetta, P.M.; Erickson, A.; Rajakumar, T.; Mills, I.G.; et al. Ductal Adenocarcinoma of the Prostate: A Systematic Review and Meta-analysis of Incidence, Presentation, Prognosis, and Management. BJUI Compass 2021, 2, 13–23. [Google Scholar] [CrossRef]
- Picollet-D’hahan, N.; Gerbaud, S.; Kermarrec, F.; Alcaraz, J.-P.; Obeid, P.; Bhajun, R.; Guyon, L.; Sulpice, E.; Cinquin, P.; Dolega, M.E.; et al. The Modulation of Attachment, Growth and Morphology of Cancerous Prostate Cells by Polyelectrolyte Nanofilms. Biomaterials 2013, 34, 10099–10108. [Google Scholar] [CrossRef]
- Liberio, M.S.; Sadowski, M.C.; Soekmadji, C.; Davis, R.A.; Nelson, C.C. Differential Effects of Tissue Culture Coating Substrates on Prostate Cancer Cell Adherence, Morphology and Behavior. PLoS ONE 2014, 9, e112122. [Google Scholar] [CrossRef]
- Zhang, B.; Kim, M.-C.; Thorsen, T.; Wang, Z. A Self-Contained Microfluidic Cell Culture System. Biomed. Microdevices 2009, 11, 1233–1237. [Google Scholar] [CrossRef] [PubMed]
- Cheung, L.S.L.; Zheng, X.; Stopa, A.; Baygents, J.C.; Guzman, R.; Schroeder, J.A.; Heimark, R.L.; Zohar, Y. Detachment of Captured Cancer Cells under Flow Acceleration in a Bio-Functionalized Microchannel. Lab. Chip 2009, 9, 1721–1731. [Google Scholar] [CrossRef]
- Liu, L.; Loutherback, K.; Liao, D.; Yeater, D.; Lambert, G.; Estévez-Torres, A.; Sturm, J.C.; Getzenberg, R.H.; Austin, R.H. A Microfluidic Device for Continuous Cancer Cell Culture and Passage with Hydrodynamic Forces. Lab. Chip 2010, 10, 1807. [Google Scholar] [CrossRef]
- Liu, N.; Du, P.; Xiao, X.; Liu, Y.; Peng, Y.; Yang, C.; Yue, T. Microfluidic-Based Mechanical Phenotyping of Androgen-Sensitive and Non-Sensitive Prostate Cancer Cells Lines. Micromachines 2019, 10, 602. [Google Scholar] [CrossRef]
- Dolega, M.E.; Allier, C.; Vinjimore Kesavan, S.; Gerbaud, S.; Kermarrec, F.; Marcoux, P.; Dinten, J.-M.; Gidrol, X.; Picollet-D’Hahan, N. Label-Free Analysis of Prostate Acini-like 3D Structures by Lensfree Imaging. Biosens. Bioelectron. 2013, 49, 176–183. [Google Scholar] [CrossRef] [PubMed]
- Tricoli, L.; Berry, D.L.; Albanese, C. A Rapid Filter Insert-Based 3D Culture System for Primary Prostate Cell Differentiation. J. Vis. Exp. 2017, 120, 55279. [Google Scholar] [CrossRef]
- Wong, Y.C.; Tam, N.N.C. Dedifferentiation of Stromal Smooth Muscle as a Factor in Prostate Carcinogenesis. Differentiation 2002, 70, 633–645. [Google Scholar] [CrossRef] [PubMed]
- Krušlin, B.; Ulamec, M.; Tomas, D. Prostate Cancer Stroma: An Important Factor in Cancer Growth and Progression. Bosn. J. Basic. Med. Sci. 2015, 15, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Shiga, K.; Hara, M.; Nagasaki, T.; Sato, T.; Takahashi, H.; Takeyama, H. Cancer-Associated Fibroblasts: Their Characteristics and Their Roles in Tumor Growth. Cancers 2015, 7, 2443–2458. [Google Scholar] [CrossRef]
- Melzer, C.; Yang, Y.; Hass, R. Interaction of MSC with Tumor Cells. Cell Commun. Signal 2016, 14, 20. [Google Scholar] [CrossRef]
- Barcellos-de-Souza, P.; Comito, G.; Pons-Segura, C.; Taddei, M.L.; Gori, V.; Becherucci, V.; Bambi, F.; Margheri, F.; Laurenzana, A.; Del Rosso, M.; et al. Mesenchymal Stem Cells Are Recruited and Activated into Carcinoma-Associated Fibroblasts by Prostate Cancer Microenvironment-Derived TGF-Β1. Stem Cells 2016, 34, 2536–2547. [Google Scholar] [CrossRef]
- Tyekucheva, S.; Bowden, M.; Bango, C.; Giunchi, F.; Huang, Y.; Zhou, C.; Bondi, A.; Lis, R.; Van Hemelrijck, M.; Andrén, O.; et al. Stromal and Epithelial Transcriptional Map of Initiation Progression and Metastatic Potential of Human Prostate Cancer. Nat. Commun. 2017, 8, 420. [Google Scholar] [CrossRef]
- Fang, X.; Sittadjody, S.; Gyabaah, K.; Opara, E.C.; Balaji, K.C. Novel 3D Co-Culture Model for Epithelial-Stromal Cells Interaction in Prostate Cancer. PLoS ONE 2013, 8, e75187. [Google Scholar] [CrossRef]
- Businaro, L.; De Ninno, A.; Schiavoni, G.; Lucarini, V.; Ciasca, G.; Gerardino, A.; Belardelli, F.; Gabriele, L.; Mattei, F. Cross Talk between Cancer and Immune Cells: Exploring Complex Dynamics in a Microfluidic Environment. Lab. Chip 2013, 13, 229–239. [Google Scholar] [CrossRef]
- Jeong, S.-Y.; Lee, J.-H.; Shin, Y.; Chung, S.; Kuh, H.-J. Co-Culture of Tumor Spheroids and Fibroblasts in a Collagen Matrix-Incorporated Microfluidic Chip Mimics Reciprocal Activation in Solid Tumor Microenvironment. PLoS ONE 2016, 11, e0159013. [Google Scholar] [CrossRef] [PubMed]
- Fan, Q.; Liu, R.; Jiao, Y.; Tian, C.; Farrell, J.D.; Diao, W.; Wang, X.; Zhang, F.; Yuan, W.; Han, H.; et al. A Novel 3-D Bio-Microfluidic System Mimicking in Vivo Heterogeneous Tumour Microstructures Reveals Complex Tumour–Stroma Interactions. Lab. Chip 2017, 17, 2852–2860. [Google Scholar] [CrossRef] [PubMed]
- Ivich, F.; Tran, M.; Tahsin, S.; Frank, S.B.; Kraft, A.; Miranti, C.K.; Zohar, Y.; Jiang, L. Application of a Microfluidic-Based Model of a Human Prostate Gland for Cancer Research. In Proceedings of the 2018 IEEE 12th International Conference on Nano/Molecular Medicine and Engineering (NANOMED), Waikiki Beach, HI, USA, 2–5 December 2018; pp. 109–112. [Google Scholar]
- Jiang, L.; Khawaja, H.; Tahsin, S.; Clarkson, T.A.; Miranti, C.K.; Zohar, Y. Microfluidic-Based Human Prostate-Cancer-on-Chip. Front. Bioeng. Biotechnol. 2024, 12, 1302223. [Google Scholar] [CrossRef] [PubMed]
- Hanahan, D.; Weinberg, R.A. Hallmarks of Cancer: The Next Generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef]
- Bacac, M.; Stamenkovic, I. Metastatic Cancer Cell. Annu. Rev. Pathol. Mech. Dis. 2008, 3, 221–247. [Google Scholar] [CrossRef]
- Bubendorf, L.; Schöpfer, A.; Wagner, U.; Sauter, G.; Moch, H.; Willi, N.; Gasser, T.C.; Mihatsch, M.J. Metastatic Patterns of Prostate Cancer: An Autopsy Study of 1,589 Patients. Human. Pathol. 2000, 31, 578–583. [Google Scholar] [CrossRef]
- Raman, D.; Baugher, P.J.; Thu, Y.M.; Richmond, A. Role of Chemokines in Tumor Growth. Cancer Lett. 2007, 256, 137–165. [Google Scholar] [CrossRef]
- Datta, K.; Muders, M.; Zhang, H.; Tindall, D.J. Mechanism of Lymph Node Metastasis in Prostate Cancer. Future Oncol. 2010, 6, 823–836. [Google Scholar] [CrossRef]
- Zhang, X.; Karim, M.; Hasan, M.M.; Hooper, J.; Wahab, R.; Roy, S.; Al-Hilal, T.A. Cancer-on-a-Chip: Models for Studying Metastasis. Cancers 2022, 14, 648. [Google Scholar] [CrossRef]
- Bostwick, D.G.; Brawer, M.K. Prostatic Intra-Epithelial Neoplasia and Early Invasion in Prostate Cancer. Cancer 1987, 59, 788–794. [Google Scholar] [CrossRef]
- Thiery, J.P. Epithelial–Mesenchymal Transitions in Tumour Progression. Nat. Rev. Cancer 2002, 2, 442–454. [Google Scholar] [CrossRef] [PubMed]
- Graham, T.R.; Zhau, H.E.; Odero-Marah, V.A.; Osunkoya, A.O.; Kimbro, K.S.; Tighiouart, M.; Liu, T.; Simons, J.W.; O’Regan, R.M. Insulin-like Growth Factor-I–Dependent Up-Regulation of ZEB1 Drives Epithelial-to-Mesenchymal Transition in Human Prostate Cancer Cells. Cancer Res. 2008, 68, 2479–2488. [Google Scholar] [CrossRef] [PubMed]
- Siddiqui, Y.H.; Kershaw, R.M.; Humphreys, E.H.; Assis Junior, E.M.; Chaudhri, S.; Jayaraman, P.-S.; Gaston, K. CK2 Abrogates the Inhibitory Effects of PRH/HHEX on Prostate Cancer Cell Migration and Invasion and Acts through PRH to Control Cell Proliferation. Oncogenesis 2017, 6, e293. [Google Scholar] [CrossRef] [PubMed]
- Perner, S.; Mosquera, J.-M.; Demichelis, F.; Hofer, M.D.; Paris, P.L.; Simko, J.; Collins, C.; Bismar, T.A.; Chinnaiyan, A.M.; De Marzo, A.M.; et al. TMPRSS2-ERG Fusion Prostate Cancer: An Early Molecular Event Associated With Invasion. Am. J. Surg. Pathol. 2007, 31, 882. [Google Scholar] [CrossRef]
- Wei, J.; Xu, G.; Wu, M.; Zhang, Y.; Li, Q.; Liu, P.; Zhu, T.; Song, A.; Zhao, L.; Han, Z.; et al. Overexpression of Vimentin Contributes to Prostate Cancer Invasion and Metastasis via Src Regulation. Anticancer. Res. 2008, 28, 327–334. [Google Scholar]
- Wang, H.; Leav, I.; Ibaragi, S.; Wegner, M.; Hu, G.; Lu, M.L.; Balk, S.P.; Yuan, X. SOX9 Is Expressed in Human Fetal Prostate Epithelium and Enhances Prostate Cancer Invasion. Cancer Res. 2008, 68, 1625–1630. [Google Scholar] [CrossRef]
- Wang, H.; Liu, G.; Shen, D.; Ye, H.; Huang, J.; Jiao, L.; Sun, Y. HOXA1 Enhances the Cell Proliferation, Invasion and Metastasis of Prostate Cancer Cells. Oncol. Rep. 2015, 34, 1203–1210. [Google Scholar] [CrossRef] [PubMed]
- Bonaccorsi, L.; Muratori, M.; Carloni, V.; Zecchi, S.; Formigli, L.; Forti, G.; Baldi, E. Androgen Receptor and Prostate Cancer Invasion. Int. J. Androl. 2003, 26, 21–25. [Google Scholar] [CrossRef]
- Bonaccorsi, L.; Marchiani, S.; Muratori, M.; Carloni, V.; Forti, G.; Baldi, E. Signaling Mechanisms That Mediate Invasion in Prostate Cancer Cells. Ann. N. Y. Acad. Sci. 2004, 1028, 283–288. [Google Scholar] [CrossRef]
- Hara, T.; Miyazaki, H.; Lee, A.; Tran, C.P.; Reiter, R.E. Androgen Receptor and Invasion in Prostate Cancer. Cancer Res. 2008, 68, 1128–1135. [Google Scholar] [CrossRef]
- Li, Y.; Li, C.X.; Ye, H.; Chen, F.; Melamed, J.; Peng, Y.; Liu, J.; Wang, Z.; Tsou, H.C.; Wei, J.; et al. Decrease in Stromal Androgen Receptor Associates with Androgen-Independent Disease and Promotes Prostate Cancer Cell Proliferation and Invasion. J. Cell. Mol. Med. 2008, 12, 2790–2798. [Google Scholar] [CrossRef] [PubMed]
- Palm, D.; Lang, K.; Niggemann, B.; Drell IV, T.L.; Masur, K.; Zaenker, K.S.; Entschladen, F. The Norepinephrine-Driven Metastasis Development of PC-3 Human Prostate Cancer Cells in BALB/c Nude Mice Is Inhibited by β-Blockers. Int. J. Cancer 2006, 118, 2744–2749. [Google Scholar] [CrossRef] [PubMed]
- Ayala, G.E.; Dai, H.; Ittmann, M.; Li, R.; Powell, M.; Frolov, A.; Wheeler, T.M.; Thompson, T.C.; Rowley, D. Growth and Survival Mechanisms Associated with Perineural Invasion in Prostate Cancer. Cancer Res. 2004, 64, 6082–6090. [Google Scholar] [CrossRef] [PubMed]
- Cai, C.; Hsieh, C.-L.; Omwancha, J.; Zheng, Z.; Chen, S.-Y.; Baert, J.-L.; Shemshedini, L. ETV1 Is a Novel Androgen Receptor-Regulated Gene That Mediates Prostate Cancer Cell Invasion. Mol. Endocrinol. 2007, 21, 1835–1846. [Google Scholar] [CrossRef] [PubMed]
- Sima, F.; Kawano, H.; Miyawaki, A.; Kelemen, L.; Ormos, P.; Wu, D.; Xu, J.; Midorikawa, K.; Sugioka, K. 3D Biomimetic Chips for Cancer Cell Migration in Nanometer-Sized Spaces Using “Ship-in-a-Bottle” Femtosecond Laser Processing. ACS Appl. Bio Mater. 2018, 1, 1667–1676. [Google Scholar] [CrossRef]
- Molter, C.W.; Muszynski, E.F.; Tao, Y.; Trivedi, T.; Clouvel, A.; Ehrlicher, A.J. Prostate Cancer Cells of Increasing Metastatic Potential Exhibit Diverse Contractile Forces, Cell Stiffness, and Motility in a Microenvironment Stiffness-Dependent Manner. Front. Cell Dev. Biol. 2022, 10, 932510. [Google Scholar] [CrossRef]
- Lopez-Cavestany, M.; Hahn, S.B.; Hope, J.M.; Reckhorn, N.T.; Greenlee, J.D.; Schwager, S.C.; VanderBurgh, J.A.; Reinhart-King, C.A.; King, M.R. Matrix Stiffness Induces Epithelial-to-Mesenchymal Transition via Piezo1-Regulated Calcium Flux in Prostate Cancer Cells. iScience 2023, 26, 106275. [Google Scholar] [CrossRef]
- Ao, M.; Brewer, B.M.; Yang, L.; Franco Coronel, O.E.; Hayward, S.W.; Webb, D.J.; Li, D. Stretching Fibroblasts Remodels Fibronectin and Alters Cancer Cell Migration. Sci. Rep. 2015, 5, 8334. [Google Scholar] [CrossRef]
- Jouybar, M.; Sleeboom, J.J.F.; Vaezzadeh, E.; Sahlgren, C.M.; Den Toonder, J.M.J. An in Vitro Model of Cancer Invasion with Heterogeneous ECM Created with Droplet Microfluidics. Front. Bioeng. Biotechnol. 2023, 11, 1267021. [Google Scholar] [CrossRef]
- Harryman, W.L.; Marr, K.D.; Hernandez-Cortes, D.; Nagle, R.B.; Garcia, J.G.N.; Cress, A.E. Cohesive Cancer Invasion of the Biophysical Barrier of Smooth Muscle. Cancer Metastasis Rev. 2021, 40, 205–219. [Google Scholar] [CrossRef]
- Sznurkowska, M.K.; Aceto, N. The Gate to Metastasis: Key Players in Cancer Cell Intravasation. FEBS J. 2022, 289, 4336–4354. [Google Scholar] [CrossRef] [PubMed]
- Conn, E.M.; Madsen, M.A.; Cravatt, B.F.; Ruf, W.; Deryugina, E.I.; Quigley, J.P. Cell Surface Proteomics Identifies Molecules Functionally Linked to Tumor Cell Intravasation. J. Biol. Chem. 2008, 283, 26518–26527. [Google Scholar] [CrossRef] [PubMed]
- Chiang, S.P.H.; Cabrera, R.M.; Segall, J.E. Tumor Cell Intravasation. Am. J. Physiol.-Cell Physiol. 2016, 311, C1–C14. [Google Scholar] [CrossRef] [PubMed]
- Khodavirdi, A.C.; Song, Z.; Yang, S.; Zhong, C.; Wang, S.; Wu, H.; Pritchard, C.; Nelson, P.S.; Roy-Burman, P. Increased Expression of Osteopontin Contributes to the Progression of Prostate Cancer. Cancer Res. 2006, 66, 883–888. [Google Scholar] [CrossRef] [PubMed]
- Conn, E.M.; Botkjaer, K.A.; Kupriyanova, T.A.; Andreasen, P.A.; Deryugina, E.I.; Quigley, J.P. Comparative Analysis of Metastasis Variants Derived from Human Prostate Carcinoma Cells. Am. J. Pathol. 2009, 175, 1638–1652. [Google Scholar] [CrossRef]
- Bekes, E.M.; Deryugina, E.I.; Kupriyanova, T.A.; Zajac, E.; Botkjaer, K.A.; Andreasen, P.A.; Quigley, J.P. Activation of Pro-uPA Is Critical for Initial Escape from the Primary Tumor and Hematogenous Dissemination of Human Carcinoma Cells. Neoplasia 2011, 13, 806–821. [Google Scholar] [CrossRef]
- Gligorijevic, B.; Bergman, A.; Condeelis, J. Multiparametric Classification Links Tumor Microenvironments with Tumor Cell Phenotype. PLoS Biol. 2014, 12, e1001995. [Google Scholar] [CrossRef]
- Masi, I.; Caprara, V.; Bagnato, A.; Rosanò, L. Tumor Cellular and Microenvironmental Cues Controlling Invadopodia Formation. Front. Cell Dev. Biol. 2020, 8, 584181. [Google Scholar] [CrossRef]
- Eddy, R.J.; Weidmann, M.D.; Sharma, V.P.; Condeelis, J.S. Tumor Cell Invadopodia: Invasive Protrusions That Orchestrate Metastasis. Trends Cell Biol. 2017, 27, 595–607. [Google Scholar] [CrossRef]
- Zervantonakis, I.K.; Hughes-Alford, S.K.; Charest, J.L.; Condeelis, J.S.; Gertler, F.B.; Kamm, R.D. Three-Dimensional Microfluidic Model for Tumor Cell Intravasation and Endothelial Barrier Function. Proc. Natl. Acad. Sci. USA 2012, 109, 13515–13520. [Google Scholar] [CrossRef]
- Li, R.; Hebert, J.D.; Lee, T.A.; Xing, H.; Boussommier-Calleja, A.; Hynes, R.O.; Lauffenburger, D.A.; Kamm, R.D. Macrophage-Secreted TNFα and TGFβ1 Influence Migration Speed and Persistence of Cancer Cells in 3D Tissue Culture via Independent Pathways. Cancer Res. 2017, 77, 279–290. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Park, W.; Ryu, H.; Jeon, N.L. A Microfluidic Platform for Quantitative Analysis of Cancer Angiogenesis and Intravasation. Biomicrofluidics 2014, 8, 054102. [Google Scholar] [CrossRef] [PubMed]
- Buchanan, C.F.; Voigt, E.E.; Szot, C.S.; Freeman, J.W.; Vlachos, P.P.; Rylander, M.N. Three-Dimensional Microfluidic Collagen Hydrogels for Investigating Flow-Mediated Tumor-Endothelial Signaling and Vascular Organization. Tissue Eng. Part. C Methods 2014, 20, 64–75. [Google Scholar] [CrossRef] [PubMed]
- Shin, M.K.; Kim, S.K.; Jung, H. Integration of Intra- and Extravasation in One Cell-Based Microfluidic Chip for the Study of Cancer Metastasis. Lab. Chip 2011, 11, 3880. [Google Scholar] [CrossRef] [PubMed]
- Cui, X.; Guo, W.; Sun, Y.; Sun, B.; Hu, S.; Sun, D.; Lam, R.H.W. A Microfluidic Device for Isolation and Characterization of Transendothelial Migrating Cancer Cells. Biomicrofluidics 2017, 11, 014105. [Google Scholar] [CrossRef]
- Nagaraju, S.; Truong, D.; Mouneimne, G.; Nikkhah, M. Microfluidic Tumor–Vascular Model to Study Breast Cancer Cell Invasion and Intravasation. Adv. Healthc. Mater. 2018, 7, 1701257. [Google Scholar] [CrossRef]
- Jing, B.; Luo, Y.; Lin, B.; Li, J.; Wang, Z.A.; Du, Y. Establishment and Application of a Dynamic Tumor-Vessel Microsystem for Studying Different Stages of Tumor Metastasis and Evaluating Anti-Tumor Drugs. RSC Adv. 2019, 9, 17137–17147. [Google Scholar] [CrossRef]
- Sima, F.; Kawano, H.; Hirano, M.; Miyawaki, A.; Obata, K.; Serien, D.; Sugioka, K. Mimicking Intravasation–Extravasation with a 3D Glass Nanofluidic Model for the Chemotaxis-Free Migration of Cancer Cells in Confined Spaces. Adv. Mater. Technol. 2020, 5, 2000484. [Google Scholar] [CrossRef]
- Micalizzi, D.S.; Maheswaran, S.; Haber, D.A. A Conduit to Metastasis: Circulating Tumor Cell Biology. Genes. Dev. 2017, 31, 1827–1840. [Google Scholar] [CrossRef]
- Juric, D.; Castel, P.; Griffith, M.; Griffith, O.L.; Won, H.H.; Ellis, H.; Ebbesen, S.H.; Ainscough, B.J.; Ramu, A.; Iyer, G.; et al. Convergent Loss of PTEN Leads to Clinical Resistance to a PI(3)Kα Inhibitor. Nature 2015, 518, 240–244. [Google Scholar] [CrossRef]
- Wong, S.Y.; Hynes, R.O. Lymphatic or Hematogenous Dissemination: How Does a Metastatic Tumor Cell Decide? Cell Cycle 2006, 5, 812–817. [Google Scholar] [CrossRef] [PubMed]
- Guo, B.; Oliver, T.G. Partners in Crime: Neutrophil–CTC Collusion in Metastasis. Trends Immunol. 2019, 40, 556–559. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.S.; Di Tomaso, E.; McDonald, D.M.; Jones, R.; Jain, R.K.; Munn, L.L. Mosaic Blood Vessels in Tumors: Frequency of Cancer Cells in Contact with Flowing Blood. Proc. Natl. Acad. Sci. USA 2000, 97, 14608–14613. [Google Scholar] [CrossRef] [PubMed]
- Tibbe, A.G.J.; Miller, M.C.; Terstappen, L.W.M.M. Statistical Considerations for Enumeration of Circulating Tumor Cells. Cytometry Pt. A 2007, 71A, 154–162. [Google Scholar] [CrossRef] [PubMed]
- Park, Y. Expected Clinical Applications of Circulating Tumor Cells in Breast Cancer. World J. Clin. Oncol. 2011, 2, 303. [Google Scholar] [CrossRef]
- Balic, M.; Lin, H.; Williams, A.; Datar, R.H.; Cote, R.J. Progress in Circulating Tumor Cell Capture and Analysis: Implications for Cancer Management. Expert Rev. Mol. Diagn. 2012, 12, 303–312. [Google Scholar] [CrossRef]
- Andergassen, U.; Kölbl, A.C.; Mahner, S.; Jeschke, U. Real-Time RT-PCR Systems for CTC Detection from Blood Samples of Breast Cancer and Gynaecological Tumour Patients (Review). Oncol. Rep. 2016, 35, 1905–1915. [Google Scholar] [CrossRef]
- Strilic, B.; Offermanns, S. Intravascular Survival and Extravasation of Tumor Cells. Cancer Cell 2017, 32, 282–293. [Google Scholar] [CrossRef]
- Yadavalli, S.; Jayaram, S.; Manda, S.S.; Madugundu, A.K.; Nayakanti, D.S.; Tan, T.Z.; Bhat, R.; Rangarajan, A.; Chatterjee, A.; Gowda, H.; et al. Data-Driven Discovery of Extravasation Pathway in Circulating Tumor Cells. Sci. Rep. 2017, 7, 43710. [Google Scholar] [CrossRef]
- Leone, K.; Poggiana, C.; Zamarchi, R. The Interplay between Circulating Tumor Cells and the Immune System: From Immune Escape to Cancer Immunotherapy. Diagnostics 2018, 8, 59. [Google Scholar] [CrossRef]
- Umer, M.; Vaidyanathan, R.; Nguyen, N.-T.; Shiddiky, M.J.A. Circulating Tumor Microemboli: Progress in Molecular Understanding and Enrichment Technologies. Biotechnol. Adv. 2018, 36, 1367–1389. [Google Scholar] [CrossRef] [PubMed]
- Rejniak, K.A. Circulating Tumor Cells: When a Solid Tumor Meets a Fluid Microenvironment. In Systems Biology of Tumor Microenvironment; Rejniak, K.A., Ed.; Advances in Experimental Medicine and Biology; Springer International Publishing: Cham, Switzerland, 2016; Volume 936, pp. 93–106. ISBN 978-3-319-42021-9. [Google Scholar]
- Krog, B.L.; Henry, M.D. Biomechanics of the Circulating Tumor Cell Microenvironment. In Biomechanics in Oncology; Dong, C., Zahir, N., Konstantopoulos, K., Eds.; Advances in Experimental Medicine and Biology; Springer International Publishing: Cham, Switzerland, 2018; Volume 1092, pp. 209–233. ISBN 978-3-319-95293-2. [Google Scholar]
- Stott, S.L.; Lee, R.J.; Nagrath, S.; Yu, M.; Miyamoto, D.T.; Ulkus, L.; Inserra, E.J.; Ulman, M.; Springer, S.; Nakamura, Z.; et al. Isolation and Characterization of Circulating Tumor Cells from Patients with Localized and Metastatic Prostate Cancer. Sci. Transl. Med. 2010, 2, 25ra23. [Google Scholar] [CrossRef]
- Kirby, B.J.; Jodari, M.; Loftus, M.S.; Gakhar, G.; Pratt, E.D.; Chanel-Vos, C.; Gleghorn, J.P.; Santana, S.M.; Liu, H.; Smith, J.P.; et al. Functional Characterization of Circulating Tumor Cells with a Prostate-Cancer-Specific Microfluidic Device. PLoS ONE 2012, 7, e35976. [Google Scholar] [CrossRef]
- Gogoi, P.; Sepehri, S.; Zhou, Y.; Gorin, M.A.; Paolillo, C.; Capoluongo, E.; Gleason, K.; Payne, A.; Boniface, B.; Cristofanilli, M.; et al. Development of an Automated and Sensitive Microfluidic Device for Capturing and Characterizing Circulating Tumor Cells (CTCs) from Clinical Blood Samples. PLoS ONE 2016, 11, e0147400. [Google Scholar] [CrossRef] [PubMed]
- Lim, C.T.; Zhou, E.H.; Quek, S.T. Mechanical Models for Living Cells—A Review. J. Biomech. 2006, 39, 195–216. [Google Scholar] [CrossRef]
- Au, S.H.; Storey, B.D.; Moore, J.C.; Tang, Q.; Chen, Y.-L.; Javaid, S.; Sarioglu, A.F.; Sullivan, R.; Madden, M.W.; O’Keefe, R.; et al. Clusters of Circulating Tumor Cells Traverse Capillary-Sized Vessels. Proc. Natl. Acad. Sci. USA 2016, 113, 4947–4952. [Google Scholar] [CrossRef] [PubMed]
- Vigmostad, S.; Krog, B.; Nauseef, J.; Henry, M.; Keshav, V. Alterations in Cancer Cell Mechanical Properties after Fluid Shear Stress Exposure: A Micropipette Aspiration Study. J. Child Health Care 2015, 7, 25–35. [Google Scholar] [CrossRef][Green Version]
- Peinado, H.; Zhang, H.; Matei, I.R.; Costa-Silva, B.; Hoshino, A.; Rodrigues, G.; Psaila, B.; Kaplan, R.N.; Bromberg, J.F.; Kang, Y.; et al. Pre-Metastatic Niches: Organ-Specific Homes for Metastases. Nat. Rev. Cancer 2017, 17, 302–317. [Google Scholar] [CrossRef]
- Sökeland, G.; Schumacher, U. The Functional Role of Integrins during Intra- and Extravasation within the Metastatic Cascade. Mol. Cancer 2019, 18, 12. [Google Scholar] [CrossRef]
- Ward, M.P.; Kane, L.E.; Norris, L.A.; Mohamed, B.M.; Kelly, T.; Bates, M.; Clarke, A.; Brady, N.; Martin, C.M.; Brooks, R.D.; et al. Platelets, Immune Cells and the Coagulation Cascade; Friend or Foe of the Circulating Tumour Cell? Mol. Cancer 2021, 20, 59. [Google Scholar] [CrossRef]
- Marcolino, E.; Siddiqui, Y.H.; van den Bosch, M.; Poole, A.W.; Jayaraman, P.-S.; Gaston, K. Blood Platelets Stimulate Cancer Extravasation through TGFβ-Mediated Downregulation of PRH/HHEX. Oncogenesis 2020, 9, 10. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, D.X.; Bos, P.D.; Massagué, J. Metastasis: From Dissemination to Organ-Specific Colonization. Nat. Rev. Cancer 2009, 9, 274–284. [Google Scholar] [CrossRef] [PubMed]
- Natoni, A.; Macauley, M.S.; O’Dwyer, M.E. Targeting Selectins and Their Ligands in Cancer. Front. Oncol. 2016, 6, 93. [Google Scholar] [CrossRef]
- Läubli, H.; Borsig, L. Selectins Promote Tumor Metastasis. Semin. Cancer Biol. 2010, 20, 169–177. [Google Scholar] [CrossRef]
- Strell, C.; Entschladen, F. Extravasation of Leukocytes in Comparison to Tumor Cells. Cell Commun. Signal 2008, 6, 10. [Google Scholar] [CrossRef] [PubMed]
- Miles, F.L.; Pruitt, F.L.; Van Golen, K.L.; Cooper, C.R. Stepping out of the Flow: Capillary Extravasation in Cancer Metastasis. Clin. Exp. Metastasis 2008, 25, 305–324. [Google Scholar] [CrossRef] [PubMed]
- Leong, H.S.; Robertson, A.E.; Stoletov, K.; Leith, S.J.; Chin, C.A.; Chien, A.E.; Hague, M.N.; Ablack, A.; Carmine-Simmen, K.; McPherson, V.A.; et al. Invadopodia Are Required for Cancer Cell Extravasation and Are a Therapeutic Target for Metastasis. Cell Rep. 2014, 8, 1558–1570. [Google Scholar] [CrossRef]
- Manuelli, V.; Cahill, F.; Wylie, H.; Gillett, C.; Correa, I.; Heck, S.; Rimmer, A.; Haire, A.; Van Hemelrijck, M.; Rudman, S.; et al. Invadopodia Play a Role in Prostate Cancer Progression. BMC Cancer 2022, 22, 386. [Google Scholar] [CrossRef]
- Ma, Y.-H.V.; Middleton, K.; You, L.; Sun, Y. A Review of Microfluidic Approaches for Investigating Cancer Extravasation during Metastasis. Microsyst. Nanoeng. 2018, 4, 17104. [Google Scholar] [CrossRef]
- Irimia, D.; Toner, M. Spontaneous Migration of Cancer Cells under Conditions of Mechanical Confinement. Integr. Biol. 2009, 1, 506. [Google Scholar] [CrossRef]
- Lautscham, L.A.; Kämmerer, C.; Lange, J.R.; Kolb, T.; Mark, C.; Schilling, A.; Strissel, P.L.; Strick, R.; Gluth, C.; Rowat, A.C.; et al. Migration in Confined 3D Environments Is Determined by a Combination of Adhesiveness, Nuclear Volume, Contractility, and Cell Stiffness. Biophys. J. 2015, 109, 900–913. [Google Scholar] [CrossRef] [PubMed]
- Wei, S.C.; Yang, J. Forcing through Tumor Metastasis: The Interplay between Tissue Rigidity and Epithelial–Mesenchymal Transition. Trends Cell Biol. 2016, 26, 111–120. [Google Scholar] [CrossRef] [PubMed]
- Ma, S.; Fu, A.; Chiew, G.G.Y.; Luo, K.Q. Hemodynamic Shear Stress Stimulates Migration and Extravasation of Tumor Cells by Elevating Cellular Oxidative Level. Cancer Lett. 2017, 388, 239–248. [Google Scholar] [CrossRef]
- Zhang, Q.; Liu, T.; Qin, J. A Microfluidic-Based Device for Study of Transendothelial Invasion of Tumor Aggregates in Realtime. Lab. Chip 2012, 12, 2837. [Google Scholar] [CrossRef]
- Hughes, A.D.; Mattison, J.; Western, L.T.; Powderly, J.D.; Greene, B.T.; King, M.R. Microtube Device for Selectin-Mediated Capture of Viable Circulating Tumor Cells from Blood. Clin. Chem. 2012, 58, 846–853. [Google Scholar] [CrossRef]
- Gakhar, G.; Navarro, V.N.; Jurish, M.; Lee, G.Y.; Tagawa, S.T.; Akhtar, N.H.; Seandel, M.; Geng, Y.; Liu, H.; Bander, N.H.; et al. Circulating Tumor Cells from Prostate Cancer Patients Interact with E-Selectin under Physiologic Blood Flow. PLoS ONE 2013, 8, e85143. [Google Scholar] [CrossRef]
- Riahi, R.; Yang, Y.L.; Kim, H.; Jiang, L.; Wong, P.K.; Zohar, Y. A Microfluidic Model for Organ-Specific Extravasation of Circulating Tumor Cells. Biomicrofluidics 2014, 8, 024103. [Google Scholar] [CrossRef] [PubMed]
- Roberts, S.A.; Waziri, A.E.; Agrawal, N. Development of a Single-Cell Migration and Extravasation Platform through Selective Surface Modification. Anal. Chem. 2016, 88, 2770–2776. [Google Scholar] [CrossRef]
- Chen, M.B.; Lamar, J.M.; Li, R.; Hynes, R.O.; Kamm, R.D. Elucidation of the Roles of Tumor Integrin Β1 in the Extravasation Stage of the Metastasis Cascade. Cancer Res. 2016, 76, 2513–2524. [Google Scholar] [CrossRef]
- Wu, Y.; Zhou, Y.; Paul, R.; Qin, X.; Islam, K.; Liu, Y. Adaptable Microfluidic Vessel-on-a-Chip Platform for Investigating Tumor Metastatic Transport in Bloodstream. Anal. Chem. 2022, 94, 12159–12166. [Google Scholar] [CrossRef]
- Wang, H.; Zhang, W.; Bado, I.; Zhang, X.H.-F. Bone Tropism in Cancer Metastases. Cold Spring Harb. Perspect. Med. 2020, 10, a036848. [Google Scholar] [CrossRef] [PubMed]
- Verbruggen, S.W.; Thompson, C.L.; Duffy, M.P.; Lunetto, S.; Nolan, J.; Pearce, O.M.T.; Jacobs, C.R.; Knight, M.M. Mechanical Stimulation Modulates Osteocyte Regulation of Cancer Cell Phenotype. Cancers 2021, 13, 2906. [Google Scholar] [CrossRef] [PubMed]
- Ganguly, S.S.; Hostetter, G.; Tang, L.; Frank, S.B.; Saboda, K.; Mehra, R.; Wang, L.; Li, X.; Keller, E.T.; Miranti, C.K. Notch3 Promotes Prostate Cancer-Induced Bone Lesion Development via MMP-3. Oncogene 2020, 39, 204–218. [Google Scholar] [CrossRef] [PubMed]
- Salamanna, F.; Contartese, D.; Maglio, M.; Fini, M. A Systematic Review on in Vitro 3D Bone Metastases Models: A New Horizon to Recapitulate the Native Clinical Scenario? Oncotarget 2016, 7, 44803–44820. [Google Scholar] [CrossRef] [PubMed]
- Laranga, R.; Duchi, S.; Ibrahim, T.; Guerrieri, A.N.; Donati, D.M.; Lucarelli, E. Trends in Bone Metastasis Modeling. Cancers 2020, 12, 2315. [Google Scholar] [CrossRef]
- Shulby, S.A.; Dolloff, N.G.; Stearns, M.E.; Meucci, O.; Fatatis, A. CX3CR1-Fractalkine Expression Regulates Cellular Mechanisms Involved in Adhesion, Migration, and Survival of Human Prostate Cancer Cells. Cancer Res. 2004, 64, 4693–4698. [Google Scholar] [CrossRef]
- Jamieson, W.L.; Shimizu, S.; D’Ambrosio, J.A.; Meucci, O.; Fatatis, A. CX3CR1 Is Expressed by Prostate Epithelial Cells and Androgens Regulate the Levels of CX3CL1/Fractalkine in the Bone Marrow: Potential Role in Prostate Cancer Bone Tropism. Cancer Res. 2008, 68, 1715–1722. [Google Scholar] [CrossRef]
- Dimitroff, C.J.; Descheny, L.; Trujillo, N.; Kim, R.; Nguyen, V.; Huang, W.; Pienta, K.J.; Kutok, J.L.; Rubin, M.A. Identification of Leukocyte E-Selectin Ligands, P-Selectin Glycoprotein Ligand-1 and E-Selectin Ligand-1, on Human Metastatic Prostate Tumor Cells. Cancer Res. 2005, 65, 5750–5760. [Google Scholar] [CrossRef]
- McCabe, N.P.; De, S.; Vasanji, A.; Brainard, J.; Byzova, T.V. Prostate Cancer Specific Integrin Avβ3 Modulates Bone Metastatic Growth and Tissue Remodeling. Oncogene 2007, 26, 6238–6243. [Google Scholar] [CrossRef]
- Sottnik, J.L.; Dai, J.; Zhang, H.; Campbell, B.; Keller, E.T. Tumor-Induced Pressure in the Bone Microenvironment Causes Osteocytes to Promote the Growth of Prostate Cancer Bone Metastases. Cancer Res. 2015, 75, 2151–2158. [Google Scholar] [CrossRef]
- Hsiao, A.Y.; Torisawa, Y.; Tung, Y.-C.; Sud, S.; Taichman, R.S.; Pienta, K.J.; Takayama, S. Microfluidic System for Formation of PC-3 Prostate Cancer Co-Culture Spheroids. Biomaterials 2009, 30, 3020–3027. [Google Scholar] [CrossRef] [PubMed]
- Bischel, L.L.; Casavant, B.P.; Beebe, D.J. Abstract 4304: A Microfluidic Invasion Assay to Investigate the Mechanisms Involved in Prostate Cancer Metastasis to Bone. Cancer Res. 2012, 72, 4304. [Google Scholar] [CrossRef]
- Ahn, J.; Lim, J.; Jusoh, N.; Lee, J.; Park, T.-E.; Kim, Y.; Kim, J.; Jeon, N.L. 3D Microfluidic Bone Tumor Microenvironment Comprised of Hydroxyapatite/Fibrin Composite. Front. Bioeng. Biotechnol. 2019, 7, 168. [Google Scholar] [CrossRef] [PubMed]
- Mei, X.; Middleton, K.; Shim, D.; Wan, Q.; Xu, L.; Ma, Y.-H.V.; Devadas, D.; Walji, N.; Wang, L.; Young, E.W.K.; et al. Microfluidic Platform for Studying Osteocyte Mechanoregulation of Breast Cancer Bone Metastasis. Integr. Biol. 2019, 11, 119–129. [Google Scholar] [CrossRef]
- Jasuja, H.; Jaswandkar, S.V.; Katti, D.R.; Katti, K.S. Interstitial Fluid Flow Contributes to Prostate Cancer Invasion and Migration to Bone; Study Conducted Using a Novel Horizontal Flow Bioreactor. Biofabrication 2023, 15, 025017. [Google Scholar] [CrossRef]
- Osawa, T.; Wang, W.; Dai, J.; Keller, E.T. Macrofluidic Recirculating Model of Skeletal Metastasis. Sci. Rep. 2019, 9, 14979. [Google Scholar] [CrossRef] [PubMed]
- Terzi, M.Y.; Izmirli, M.; Gogebakan, B. The Cell Fate: Senescence or Quiescence. Mol. Biol. Rep. 2016, 43, 1213–1220. [Google Scholar] [CrossRef]
- Kwon, J.S.; Everetts, N.J.; Wang, X.; Wang, W.; Della Croce, K.; Xing, J.; Yao, G. Controlling Depth of Cellular Quiescence by an Rb-E2F Network Switch. Cell Rep. 2017, 20, 3223–3235. [Google Scholar] [CrossRef]
- Jahanban-Esfahlan, R.; Seidi, K.; Manjili, M.H.; Jahanban-Esfahlan, A.; Javaheri, T.; Zare, P. Tumor Cell Dormancy: Threat or Opportunity in the Fight against Cancer. Cancers 2019, 11, 1207. [Google Scholar] [CrossRef]
- Chernosky, N.M.; Tamagno, I. The Role of the Innate Immune System in Cancer Dormancy and Relapse. Cancers 2021, 13, 5621. [Google Scholar] [CrossRef]
- Endo, H.; Inoue, M. Dormancy in Cancer. Cancer Sci. 2019, 110, 474–480. [Google Scholar] [CrossRef] [PubMed]
- Sampieri, K.; Fodde, R. Cancer Stem Cells and Metastasis. Semin. Cancer Biol. 2012, 22, 187–193. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Reed-Newman, T.; Anant, S.; Ramasamy, T.S. Regulatory Role of Quiescence in the Biological Function of Cancer Stem Cells. Stem Cell Rev. Rep. 2020, 16, 1185–1207. [Google Scholar] [CrossRef] [PubMed]
- Pradhan, S.; Sperduto, J.L.; Farino, C.J.; Slater, J.H. Engineered In Vitro Models of Tumor Dormancy and Reactivation. J. Biol. Eng. 2018, 12, 37. [Google Scholar] [CrossRef]
- Rao, S.S.; Kondapaneni, R.V.; Narkhede, A.A. Bioengineered Models to Study Tumor Dormancy. J. Biol. Eng. 2019, 13, 3. [Google Scholar] [CrossRef]
- Sistigu, A.; Musella, M.; Galassi, C.; Vitale, I.; De Maria, R. Tuning Cancer Fate: Tumor Microenvironment’s Role in Cancer Stem Cell Quiescence and Reawakening. Front. Immunol. 2020, 11, 2166. [Google Scholar] [CrossRef]
- Kang, D.-K.; Lu, J.; Zhang, W.; Chang, E.; Eckert, M.A.; Ali, M.M.; Zhao, W.; Li, X. (James) Microfluidic Devices for Stem Cell Analysis. In Microfluidic Devices for Biomedical Applications; Elsevier: Amsterdam, The Netherlands, 2021; pp. 437–487. ISBN 978-0-12-819971-8. [Google Scholar]
- Wheeler, S.E.; Clark, A.M.; Taylor, D.P.; Young, C.L.; Pillai, V.C.; Stolz, D.B.; Venkataramanan, R.; Lauffenburger, D.; Griffith, L.; Wells, A. Spontaneous Dormancy of Metastatic Breast Cancer Cells in an All Human Liver Microphysiologic System. Br. J. Cancer 2014, 111, 2342–2350. [Google Scholar] [CrossRef] [PubMed]
- Khazali, A.S.; Clark, A.M.; Wells, A. Inflammatory Cytokine IL-8/CXCL8 Promotes Tumour Escape from Hepatocyte-Induced Dormancy. Br. J. Cancer 2018, 118, 566–576. [Google Scholar] [CrossRef]
- Clark, A.M.; Kumar, M.P.; Wheeler, S.E.; Young, C.L.; Venkataramanan, R.; Stolz, D.B.; Griffith, L.G.; Lauffenburger, D.A.; Wells, A. A Model of Dormant-Emergent Metastatic Breast Cancer Progression Enabling Exploration of Biomarker Signatures. Mol. Cell. Proteom. 2018, 17, 619–630. [Google Scholar] [CrossRef]
- Hassell, B.A.; Goyal, G.; Lee, E.; Sontheimer-Phelps, A.; Levy, O.; Chen, C.S.; Ingber, D.E. Human Organ Chip Models Recapitulate Orthotopic Lung Cancer Growth, Therapeutic Responses, and Tumor Dormancy In Vitro. Cell Rep. 2017, 21, 508–516. [Google Scholar] [CrossRef]
- Ma, N.; Kamalakshakurup, G.; Aghaamoo, M.; Lee, A.P.; Digman, M.A. Label-Free Metabolic Classification of Single Cells in Droplets Using the Phasor Approach to Fluorescence Lifetime Imaging Microscopy. Cytom. Pt. A 2019, 95, 93–100. [Google Scholar] [CrossRef] [PubMed]
- Argüello-Miranda, O.; Marchand, A.J.; Kennedy, T.; Russo, M.A.X.; Noh, J. Cell Cycle–Independent Integration of Stress Signals by Xbp1 Promotes Non-G1/G0 Quiescence Entry. J. Cell Biol. 2022, 221, e202103171. [Google Scholar] [CrossRef] [PubMed]
- Liu, B.; Wang, X.; Jiang, L.; Xu, J.; Zohar, Y.; Yao, G. Extracellular Fluid Flow Induces Shallow Quiescence Through Physical and Biochemical Cues. Front. Cell Dev. Biol. 2022, 10, 792719. [Google Scholar] [CrossRef] [PubMed]
- Descotes, J.-L. Diagnosis of Prostate Cancer. Asian J. Urol. 2019, 6, 129–136. [Google Scholar] [CrossRef]
- Khan, T.; Altamimi, M.A.; Hussain, A.; Ramzan, M.; Ashique, S.; Alhuzani, M.R.; Alnemer, O.A.; Khuroo, T.; Alshammari, H.A. Understanding of PSA Biology, Factors Affecting PSA Detection, Challenges, Various Biomarkers, Methods, and Future Perspective of Prostate Cancer Detection and Diagnosis. Adv. Cancer Biol.-Metastasis 2022, 5, 100059. [Google Scholar] [CrossRef]
- Ignatiadis, M.; Sledge, G.W.; Jeffrey, S.S. Liquid Biopsy Enters the Clinic—Implementation Issues and Future Challenges. Nat. Rev. Clin. Oncol. 2021, 18, 297–312. [Google Scholar] [CrossRef]
- Descamps, L.; Le Roy, D.; Deman, A.-L. Microfluidic-Based Technologies for CTC Isolation: A Review of 10 Years of Intense Efforts towards Liquid Biopsy. Int. J. Mol. Sci. 2022, 23, 1981. [Google Scholar] [CrossRef]
- Hägglöf, C.; Hammarsten, P.; Strömvall, K.; Egevad, L.; Josefsson, A.; Stattin, P.; Granfors, T.; Bergh, A. TMPRSS2-ERG Expression Predicts Prostate Cancer Survival and Associates with Stromal Biomarkers. PLoS ONE 2014, 9, e86824. [Google Scholar] [CrossRef]
- Albala, D.; Mouraviev, V.; Rieger-Christ, K.M.; Sullivan, T.B.; Kella, N.; Knopf, K.B.; Rashid, H.H.; Manak, M.S.; Hogan, B.J.; Dixit, G.; et al. A Live Cell Microfluidics Device Utilizing Phenotypic Biomarkers for Prostate Cancer. J. Clin. Oncol. 2016, 34, 338. [Google Scholar] [CrossRef]
- Annese, V.F.; Patil, S.B.; Hu, C.; Giagkoulovits, C.; Al-Rawhani, M.A.; Grant, J.; Macleod, M.; Clayton, D.J.; Heaney, L.M.; Daly, R.; et al. A Monolithic Single-Chip Point-of-Care Platform for Metabolomic Prostate Cancer Detection. Microsyst. Nanoeng. 2021, 7, 21. [Google Scholar] [CrossRef]
- Sikaris, K. Abnormal Laboratory Results: Prostate Specific Antigen. Aust. Prescr. 2011, 34, 186–188. [Google Scholar] [CrossRef]
- Farha, M.W.; Salami, S.S. Biomarkers for Prostate Cancer Detection and Risk Stratification. Ther. Adv. Urol. 2022, 14, 175628722211039. [Google Scholar] [CrossRef] [PubMed]
- Balk, S.P.; Ko, Y.-J.; Bubley, G.J. Biology of Prostate-Specific Antigen. J. Clin. Oncol. 2003, 21, 383–391. [Google Scholar] [CrossRef] [PubMed]
- Djavan, B.; Zlotta, A.; Kratzik, C.; Remzi, M.; Seitz, C.; Schulman, C.C.; Marberger, M. PSA, PSA Density, PSA Density of Transition Zone, Free/Total PSA Ratio, and PSA Velocity for Early Detection of Prostate Cancer in Men with Serum PSA 2.5 to 4.0 Ng/mL. Urology 1999, 54, 517–522. [Google Scholar] [CrossRef]
- Thompson, I.M.; Ankerst, D.P. Prostate-Specific Antigen in the Early Detection of Prostate Cancer. Can. Med. Assoc. J. 2007, 176, 1853–1858. [Google Scholar] [CrossRef] [PubMed]
- Pezaro, C.; Woo, H.H.; Davis, I.D. Prostate Cancer: Measuring PSA. Intern. Med. J. 2014, 44, 433–440. [Google Scholar] [CrossRef]
- Petricoin, E.F., III; Ornstein, D.K.; Paweletz, C.P.; Ardekani, A.; Hackett, P.S.; Hitt, B.A.; Velassco, A.; Trucco, C.; Wiegand, L.; Wood, K.; et al. Serum Proteomic Patterns for Detection of Prostate Cancer. J. Natl. Cancer Inst. 2002, 94, 1576–1578. [Google Scholar] [CrossRef]
- Fernández-Sánchez, C.; McNeil, C.J.; Rawson, K.; Nilsson, O. Disposable Noncompetitive Immunosensor for Free and Total Prostate-Specific Antigen Based on Capacitance Measurement. Anal. Chem. 2004, 76, 5649–5656. [Google Scholar] [CrossRef]
- Triroj, N.; Jaroenapibal, P.; Shi, H.; Yeh, J.I.; Beresford, R. Microfluidic Chip-Based Nanoelectrode Array as Miniaturized Biochemical Sensing Platform for Prostate-Specific Antigen Detection. Biosens. Bioelectron. 2011, 26, 2927–2933. [Google Scholar] [CrossRef]
- Chiriacò, M.S.; Primiceri, E.; Montanaro, A.; De Feo, F.; Leone, L.; Rinaldi, R.; Maruccio, G. On-Chip Screening for Prostate Cancer: An EIS Microfluidic Platform for Contemporary Detection of Free and Total PSA. Analyst 2013, 138, 5404. [Google Scholar] [CrossRef]
- Lee, S.-M.; Hwang, K.S.; Yoon, H.-J.; Yoon, D.S.; Kim, S.K.; Lee, Y.-S.; Kim, T.S. Sensitivity Enhancement of a Dynamic Mode Microcantilever by Stress Inducer and Mass Inducer to Detect PSA at Low Picogram Levels. Lab. Chip 2009, 9, 2683. [Google Scholar] [CrossRef] [PubMed]
- Uludag, Y.; Tothill, I.E. Cancer Biomarker Detection in Serum Samples Using Surface Plasmon Resonance and Quartz Crystal Microbalance Sensors with Nanoparticle Signal Amplification. Anal. Chem. 2012, 84, 5898–5904. [Google Scholar] [CrossRef]
- Di Cera, E. Mechanisms of Ligand Binding. Biophys. Rev. 2020, 1, 011303. [Google Scholar] [CrossRef] [PubMed]
- Zhau, H.E.; Goodwin, T.J.; Chang, S.-M.; Baker, T.L.; Chung, L.W.K. Establishment of a Three-Dimensional Human Prostate Organoid Coculture under Microgravity-Simulated Conditions: Evaluation of Androgen-Induced Growth and Psa Expression. Vitr. Cell.Dev.Biol.-Anim. 1997, 33, 375–380. [Google Scholar] [CrossRef] [PubMed]
- Padmyastuti, A.; Sarmiento, M.G.; Dib, M.; Ehrhardt, J.; Schoon, J.; Somova, M.; Burchardt, M.; Roennau, C.; Pinto, P.C. Microfluidic-Based Prostate Cancer Model for Investigating the Secretion of Prostate-Specific Antigen and microRNAs in Vitro. Sci. Rep. 2023, 13, 11623. [Google Scholar] [CrossRef] [PubMed]
- Feng, Z.; Wu, J.; Lu, Y.; Chan, Y.-T.; Zhang, C.; Wang, D.; Luo, D.; Huang, Y.; Feng, Y.; Wang, N. Circulating Tumor Cells in the Early Detection of Human Cancers. Int. J. Biol. Sci. 2022, 18, 3251–3265. [Google Scholar] [CrossRef] [PubMed]
- Nagrath, S.; Sequist, L.V.; Maheswaran, S.; Bell, D.W.; Irimia, D.; Ulkus, L.; Smith, M.R.; Kwak, E.L.; Digumarthy, S.; Muzikansky, A.; et al. Isolation of Rare Circulating Tumour Cells in Cancer Patients by Microchip Technology. Nature 2007, 450, 1235–1239. [Google Scholar] [CrossRef]
- Habli, Z.; AlChamaa, W.; Saab, R.; Kadara, H.; Khraiche, M.L. Circulating Tumor Cell Detection Technologies and Clinical Utility: Challenges and Opportunities. Cancers 2020, 12, 1930. [Google Scholar] [CrossRef]
- Cho, H.-Y.; Choi, J.-H.; Lim, J.; Lee, S.-N.; Choi, J.-W. Microfluidic Chip-Based Cancer Diagnosis and Prediction of Relapse by Detecting Circulating Tumor Cells and Circulating Cancer Stem Cells. Cancers 2021, 13, 1385. [Google Scholar] [CrossRef]
- Li, C.; He, W.; Wang, N.; Xi, Z.; Deng, R.; Liu, X.; Kang, R.; Xie, L.; Liu, X. Application of Microfluidics in Detection of Circulating Tumor Cells. Front. Bioeng. Biotechnol. 2022, 10, 907232. [Google Scholar] [CrossRef]
- Galletti, G.; Portella, L.; Tagawa, S.T.; Kirby, B.J.; Giannakakou, P.; Nanus, D.M. Circulating Tumor Cells in Prostate Cancer Diagnosis and Monitoring: An Appraisal of Clinical Potential. Mol. Diagn. Ther. 2014, 18, 389–402. [Google Scholar] [CrossRef] [PubMed]
- Cieślikowski, W.A.; Antczak, A.; Nowicki, M.; Zabel, M.; Budna-Tukan, J. Clinical Relevance of Circulating Tumor Cells in Prostate Cancer Management. Biomedicines 2021, 9, 1179. [Google Scholar] [CrossRef]
- Bankó, P.; Lee, S.Y.; Nagygyörgy, V.; Zrínyi, M.; Chae, C.H.; Cho, D.H.; Telekes, A. Technologies for Circulating Tumor Cell Separation from Whole Blood. J. Hematol. Oncol. 2019, 12, 48. [Google Scholar] [CrossRef]
- Edd, J.F.; Mishra, A.; Smith, K.C.; Kapur, R.; Maheswaran, S.; Haber, D.A.; Toner, M. Isolation of Circulating Tumor Cells. iScience 2022, 25, 104696. [Google Scholar] [CrossRef] [PubMed]
- Au, S.H.; Edd, J.; Stoddard, A.E.; Wong, K.H.K.; Fachin, F.; Maheswaran, S.; Haber, D.A.; Stott, S.L.; Kapur, R.; Toner, M. Microfluidic Isolation of Circulating Tumor Cell Clusters by Size and Asymmetry. Sci. Rep. 2017, 7, 2433. [Google Scholar] [CrossRef] [PubMed]
- Miller, M.C.; Robinson, P.S.; Wagner, C.; O’Shannessy, D.J. The ParsortixTM Cell Separation System—A Versatile Liquid Biopsy Platform. Cytom. Pt. A 2018, 93, 1234–1239. [Google Scholar] [CrossRef]
- Luo, H.; Zhao, C.; Song, K.; Liu, D.; Ma, W.; Yu, X.; Su, H.; Zhang, Z.; Zohar, Y.; Lee, Y.-K. A Nonlinear Two-Degree-of-Freedom Mass–Damper–Spring Model to Predict the Isolation of Circulating Tumor Cells in Microfluidic-Elasto-Filtration Devices. Microfluid. Nanofluid. 2019, 23, 72. [Google Scholar] [CrossRef]
- Chen, J.; Liu, C.-Y.; Wang, X.; Sweet, E.; Liu, N.; Gong, X.; Lin, L. 3D Printed Microfluidic Devices for Circulating Tumor Cells (CTCs) Isolation. Biosens. Bioelectron. 2020, 150, 111900. [Google Scholar] [CrossRef]
- Wu, S.; Gu, L.; Qin, J.; Zhang, L.; Sun, F.; Liu, Z.; Wang, Y.; Shi, D. Rapid Label-Free Isolation of Circulating Tumor Cells from Patients’ Peripheral Blood Using Electrically Charged Fe3O4 Nanoparticles. ACS Appl. Mater. Interfaces 2020, 12, 4193–4203. [Google Scholar] [CrossRef]
- Zhou, J.; Tu, C.; Liang, Y.; Huang, B.; Fang, Y.; Liang, X.; Ye, X. The Label-Free Separation and Culture of Tumor Cells in a Microfluidic Biochip. Analyst 2020, 145, 1706–1715. [Google Scholar] [CrossRef]
- Cho, H.-Y.; Hossain, M.K.; Lee, J.-H.; Han, J.; Lee, H.J.; Kim, K.-J.; Kim, J.-H.; Lee, K.-B.; Choi, J.-W. Selective Isolation and Noninvasive Analysis of Circulating Cancer Stem Cells through Raman Imaging. Biosens. Bioelectron. 2018, 102, 372–382. [Google Scholar] [CrossRef] [PubMed]
- Varillas, J.I.; Zhang, J.; Chen, K.; Barnes, I.I.; Liu, C.; George, T.J.; Fan, Z.H. Microfluidic Isolation of Circulating Tumor Cells and Cancer Stem-Like Cells from Patients with Pancreatic Ductal Adenocarcinoma. Theranostics 2019, 9, 1417–1425. [Google Scholar] [CrossRef] [PubMed]
- Allard, W.J.; Matera, J.; Miller, M.C.; Repollet, M.; Connelly, M.C.; Rao, C.; Tibbe, A.G.J.; Uhr, J.W.; Terstappen, L.W.M.M. Tumor Cells Circulate in the Peripheral Blood of All Major Carcinomas but Not in Healthy Subjects or Patients with Nonmalignant Diseases. Clin. Cancer Res. 2004, 10, 6897–6904. [Google Scholar] [CrossRef]
- Alix-Panabières, C.; Vendrell, J.-P.; Pellé, O.; Rebillard, X.; Riethdorf, S.; Müller, V.; Fabbro, M.; Pantel, K. Detection and Characterization of Putative Metastatic Precursor Cells in Cancer Patients. Clin. Chem. 2007, 53, 537–539. [Google Scholar] [CrossRef]
- Theil, G.; Fischer, K.; Weber, E.; Medek, R.; Hoda, R.; Lücke, K.; Fornara, P. The Use of a New CellCollector to Isolate Circulating Tumor Cells from the Blood of Patients with Different Stages of Prostate Cancer and Clinical Outcomes-A Proof-of-Concept Study. PLoS ONE 2016, 11, e0158354. [Google Scholar] [CrossRef] [PubMed]
- Kuske, A.; Gorges, T.M.; Tennstedt, P.; Tiebel, A.-K.; Pompe, R.; Preißer, F.; Prues, S.; Mazel, M.; Markou, A.; Lianidou, E.; et al. Improved Detection of Circulating Tumor Cells in Non-Metastatic High-Risk Prostate Cancer Patients. Sci. Rep. 2016, 6, 39736. [Google Scholar] [CrossRef]
- Danila, D.C.; Samoila, A.; Patel, C.; Schreiber, N.; Herkal, A.; Anand, A.; Bastos, D.; Heller, G.; Fleisher, M.; Scher, H.I. Clinical Validity of Detecting Circulating Tumor Cells by AdnaTest Assay Compared With Direct Detection of Tumor mRNA in Stabilized Whole Blood, as a Biomarker Predicting Overall Survival for Metastatic Castration-Resistant Prostate Cancer Patients. Cancer J. 2016, 22, 315–320. [Google Scholar] [CrossRef]
- Park, M.-H.; Reátegui, E.; Li, W.; Tessier, S.N.; Wong, K.H.K.; Jensen, A.E.; Thapar, V.; Ting, D.; Toner, M.; Stott, S.L.; et al. Enhanced Isolation and Release of Circulating Tumor Cells Using Nanoparticle Binding and Ligand Exchange in a Microfluidic Chip. J. Am. Chem. Soc. 2017, 139, 2741–2749. [Google Scholar] [CrossRef]
- Glia, A.; Deliorman, M.; Sukumar, P.; Janahi, F.K.; Samara, B.; Brimmo, A.T.; Qasaimeh, M.A. Herringbone Microfluidic Probe for Multiplexed Affinity-Capture of Prostate Circulating Tumor Cells. Adv. Mater. Technol. 2021, 6, 2100053. [Google Scholar] [CrossRef]
- Cho, H.; Chung, J.I.; Kim, J.; Seo, W.I.; Lee, C.H.; Morgan, T.M.; Byun, S.; Chung, J.; Han, K. Multigene Model for Predicting Metastatic Prostate Cancer Using Circulating Tumor Cells by Microfluidic Magnetophoresis. Cancer Sci. 2021, 112, 859–870. [Google Scholar] [CrossRef]
- Su, W.; Li, H.; Chen, W.; Qin, J. Microfluidic Strategies for Label-Free Exosomes Isolation and Analysis. TrAC Trends Anal. Chem. 2019, 118, 686–698. [Google Scholar] [CrossRef]
- Cheng, H.; Yang, Q.; Wang, R.; Luo, R.; Zhu, S.; Li, M.; Li, W.; Chen, C.; Zou, Y.; Huang, Z.; et al. Emerging Advances of Detection Strategies for Tumor-Derived Exosomes. Int. J. Mol. Sci. 2022, 23, 868. [Google Scholar] [CrossRef]
- Raju, D.; Bathini, S.; Badilescu, S.; Ghosh, A.; Packirisamy, M. Microfluidic Platforms for the Isolation and Detection of Exosomes: A Brief Review. Micromachines 2022, 13, 730. [Google Scholar] [CrossRef]
- Adriani, R.R.; Gargari, S.L.M. Comparative Application of Microfluidic Systems in Circulating Tumor Cells and Extracellular Vesicles Isolation; a Review. Biomed. Microdevices 2023, 25, 4. [Google Scholar] [CrossRef]
- Liu, Y.; Li, M.; Liu, H.; Kang, C.; Wang, C. Cancer Diagnosis Using Label-Free SERS-Based Exosome Analysis. Theranostics 2024, 14, 1966–1981. [Google Scholar] [CrossRef]
- Wang, Y.; Li, Q.; Shi, H.; Tang, K.; Qiao, L.; Yu, G.; Ding, C.; Yu, S. Microfluidic Raman Biochip Detection of Exosomes: A Promising Tool for Prostate Cancer Diagnosis. Lab. Chip 2020, 20, 4632–4637. [Google Scholar] [CrossRef]
- Lin, C.-C.; Tseng, C.-C.; Chuang, T.-K.; Lee, D.-S.; Lee, G.-B. Urine Analysis in Microfluidic Devices. Analyst 2011, 136, 2669. [Google Scholar] [CrossRef]
- Liao, C.; Wu, Z.; Lin, C.; Chen, X.; Zou, Y.; Zhao, W.; Li, X.; Huang, G.; Xu, B.; Briganti, G.E.; et al. Nurturing the Marriages of Urinary Liquid Biopsies and Nano-diagnostics for Precision Urinalysis of Prostate Cancer. Smart Med. 2023, 2, e20220020. [Google Scholar] [CrossRef]
- Groskopf, J.; Aubin, S.M.; Deras, I.L.; Blase, A.; Bodrug, S.; Clark, C.; Brentano, S.; Mathis, J.; Pham, J.; Meyer, T.; et al. APTIMA PCA3 Molecular Urine Test: Development of a Method to Aid in the Diagnosis of Prostate Cancer. Clin. Chem. 2006, 52, 1089–1095. [Google Scholar] [CrossRef]
- Nilsson, J.; Skog, J.; Nordstrand, A.; Baranov, V.; Mincheva-Nilsson, L.; Breakefield, X.O.; Widmark, A. Prostate Cancer-Derived Urine Exosomes: A Novel Approach to Biomarkers for Prostate Cancer. Br. J. Cancer 2009, 100, 1603–1607. [Google Scholar] [CrossRef]
- Zitka, O.; Krizkova, S.; Krejcova, L.; Hynek, D.; Gumulec, J.; Masarik, M.; Sochor, J.; Adam, V.; Hubalek, J.; Trnkova, L.; et al. Microfluidic Tool Based on the Antibody-modified Paramagnetic Particles for Detection of 8-hydroxy-2′-deoxyguanosine in Urine of Prostate Cancer Patients. Electrophoresis 2011, 32, 3207–3220. [Google Scholar] [CrossRef]
- Jedinak, A.; Vuichoud, C.; El-Hayek, A.; Kaplan, K.; Savage, J.; Prophet, S.; Feldman, A.S.; Camphausen, K.A.; Loughlin, K.R.; Moses, M.A. Abstract 711: Mechanistic Implications of COL1A1 as a Prostate Cancer Biomarker. Cancer Res. 2017, 77, 711. [Google Scholar] [CrossRef]
- Rzhevskiy, A.S.; Razavi Bazaz, S.; Ding, L.; Kapitannikova, A.; Sayyadi, N.; Campbell, D.; Walsh, B.; Gillatt, D.; Ebrahimi Warkiani, M.; Zvyagin, A.V. Rapid and Label-Free Isolation of Tumour Cells from the Urine of Patients with Localised Prostate Cancer Using Inertial Microfluidics. Cancers 2019, 12, 81. [Google Scholar] [CrossRef]
- Woo, H.-K.; Park, J.; Ku, J.Y.; Lee, C.H.; Sunkara, V.; Ha, H.K.; Cho, Y.-K. Urine-Based Liquid Biopsy: Non-Invasive and Sensitive AR-V7 Detection in Urinary EVs from Patients with Prostate Cancer. Lab. Chip 2019, 19, 87–97. [Google Scholar] [CrossRef]
- Borkowetz, A.; Lohse-Fischer, A.; Scholze, J.; Lotzkat, U.; Thomas, C.; Wirth, M.P.; Fuessel, S.; Erdmann, K. Evaluation of MicroRNAs as Non-Invasive Diagnostic Markers in Urinary Cells from Patients with Suspected Prostate Cancer. Diagnostics 2020, 10, 578. [Google Scholar] [CrossRef]
- Shirazi, H.S.; Chan, K.M.; Rouget, J.; Ostrikov, K.; McNicholas, K.; Li, J.; Butler, L.; Gleadle, J.M.; Vasilev, K.; MacGregor, M. Plasma Enabled Devices for the Selective Capture and Photodynamic Identification of Prostate Cancer Cells. Biointerphases 2020, 15, 031002. [Google Scholar] [CrossRef]
- Chan, K.M.; Gleadle, J.M.; Gregory, P.A.; Phillips, C.A.; Shirazi, H.S.; Whiteley, A.; Li, J.; Vasilev, K.; MacGregor, M. Selective Microfluidic Capture and Detection of Prostate Cancer Cells from Urine without Digital Rectal Examination. Cancers 2021, 13, 5544. [Google Scholar] [CrossRef]
- Posdzich, P.; Darr, C.; Hilser, T.; Wahl, M.; Herrmann, K.; Hadaschik, B.; Grünwald, V. Metastatic Prostate Cancer—A Review of Current Treatment Options and Promising New Approaches. Cancers 2023, 15, 461. [Google Scholar] [CrossRef]
- Levesque, C.; Nelson, P.S. Cellular Constituents of the Prostate Stroma: Key Contributors to Prostate Cancer Progression and Therapy Resistance. Cold Spring Harb. Perspect. Med. 2018, 8, a030510. [Google Scholar] [CrossRef]
- Bargahi, N.; Ghasemali, S.; Jahandar-Lashaki, S.; Nazari, A. Recent Advances for Cancer Detection and Treatment by Microfluidic Technology, Review and Update. Biol. Proced. Online 2022, 24, 5. [Google Scholar] [CrossRef]
- Kimura, H.; Sakai, Y.; Fujii, T. Organ/Body-on-a-Chip Based on Microfluidic Technology for Drug Discovery. Drug Metab. Pharmacokinet. 2018, 33, 43–48. [Google Scholar] [CrossRef]
- Niemeyer, B.F.; Zhao, P.; Tuder, R.M.; Benam, K.H. Advanced Microengineered Lung Models for Translational Drug Discovery. SLAS Discov. 2018, 23, 777–789. [Google Scholar] [CrossRef]
- Tan, M.E.; Li, J.; Xu, H.E.; Melcher, K.; Yong, E. Androgen Receptor: Structure, Role in Prostate Cancer and Drug Discovery. Acta Pharmacol. Sin. 2015, 36, 3–23. [Google Scholar] [CrossRef]
- Lang, K.; Drell, T.L.; Lindecke, A.; Niggemann, B.; Kaltschmidt, C.; Zaenker, K.S.; Entschladen, F. Induction of a Metastatogenic Tumor Cell Type by Neurotransmitters and Its Pharmacological Inhibition by Established Drugs. Int. J. Cancer 2004, 112, 231–238. [Google Scholar] [CrossRef]
- An, D.; Kim, K.; Kim, J. Microfluidic System Based High Throughput Drug Screening System for Curcumin/TRAIL Combinational Chemotherapy in Human Prostate Cancer PC3 Cells. Biomol. Ther. 2014, 22, 355–362. [Google Scholar] [CrossRef]
- Ewart, L.; Apostolou, A.; Briggs, S.A.; Carman, C.V.; Chaff, J.T.; Heng, A.R.; Jadalannagari, S.; Janardhanan, J.; Jang, K.-J.; Joshipura, S.R.; et al. Performance Assessment and Economic Analysis of a Human Liver-Chip for Predictive Toxicology. Commun. Med. 2022, 2, 154. [Google Scholar] [CrossRef]
- Miyamoto, D.T.; Lee, R.J.; Stott, S.L.; Ting, D.T.; Wittner, B.S.; Ulman, M.; Smas, M.E.; Lord, J.B.; Brannigan, B.W.; Trautwein, J.; et al. Androgen Receptor Signaling in Circulating Tumor Cells as a Marker of Hormonally Responsive Prostate Cancer. Cancer Discov. 2012, 2, 995–1003. [Google Scholar] [CrossRef]
- Khanal, G.; Hiemstra, S.; Pappas, D. Probing Hypoxia-Induced Staurosporine Resistance in Prostate Cancer Cells with a Microfluidic Culture System. Analyst 2014, 139, 3274–3280. [Google Scholar] [CrossRef]
- Miyamoto, D.T.; Lee, R.J.; Kalinich, M.; LiCausi, J.A.; Zheng, Y.; Chen, T.; Milner, J.D.; Emmons, E.; Ho, U.; Broderick, K.; et al. An RNA-Based Digital Circulating Tumor Cell Signature Is Predictive of Drug Response and Early Dissemination in Prostate Cancer. Cancer Discov. 2018, 8, 288–303. [Google Scholar] [CrossRef]
- Ingber, D.E. Human Organs-on-Chips for Disease Modelling, Drug Development and Personalized Medicine. Nat. Rev. Genet. 2022, 23, 467–491. [Google Scholar] [CrossRef]
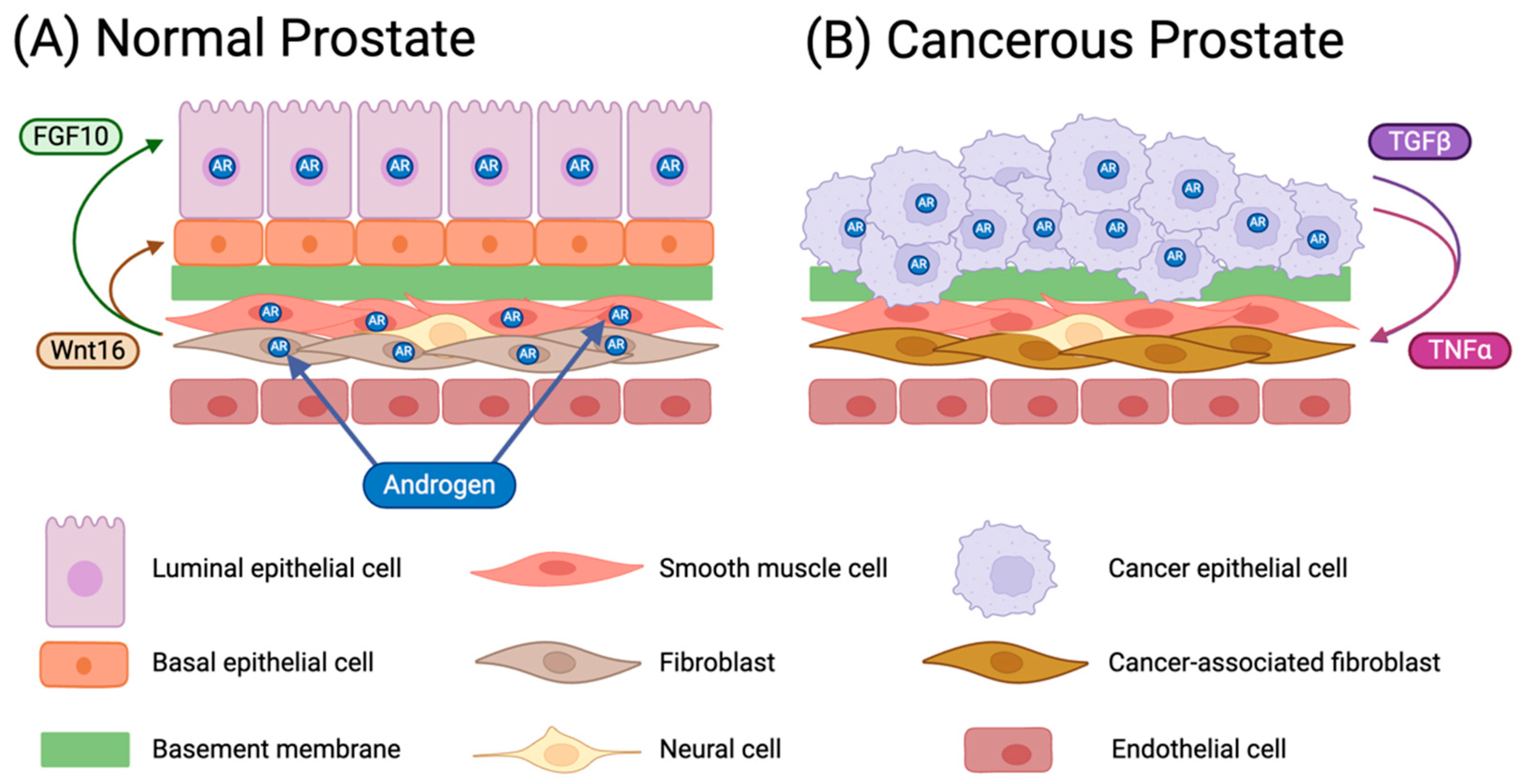
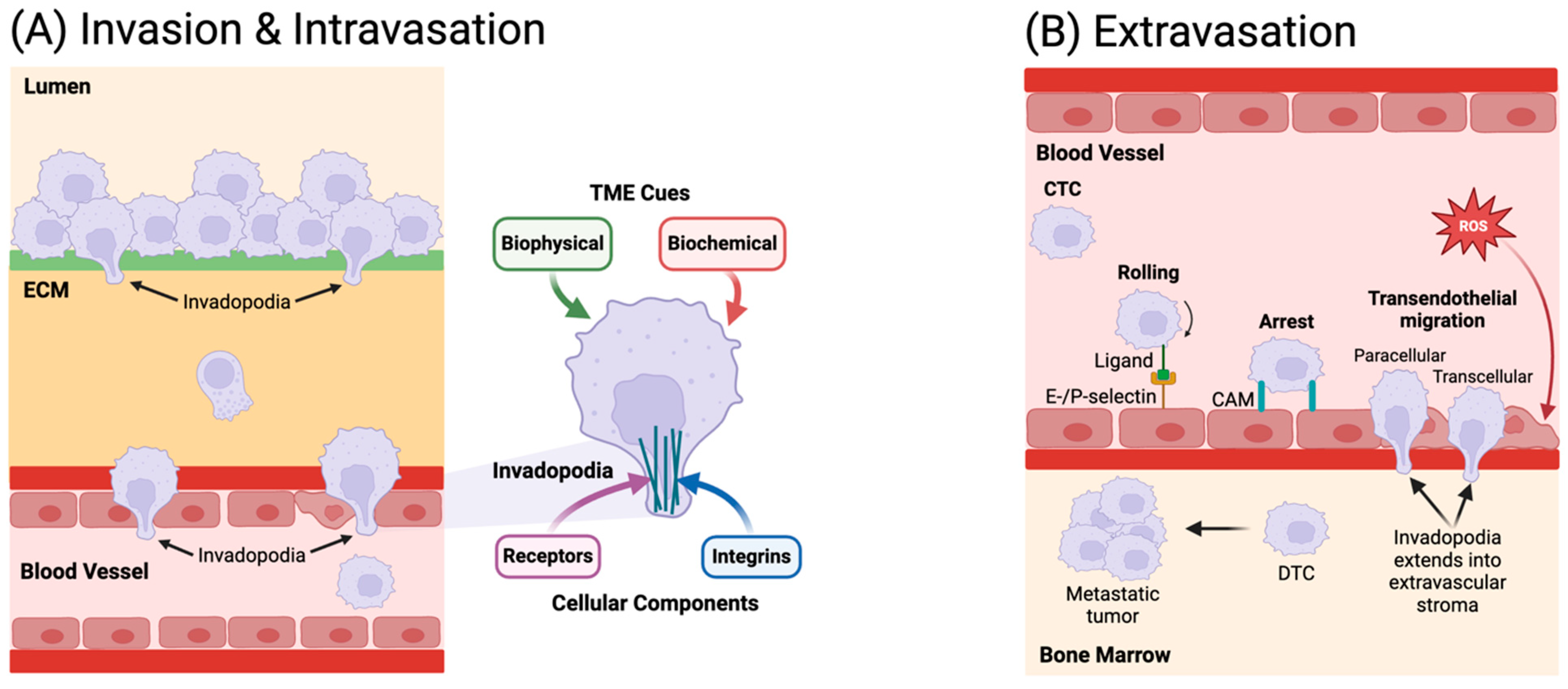

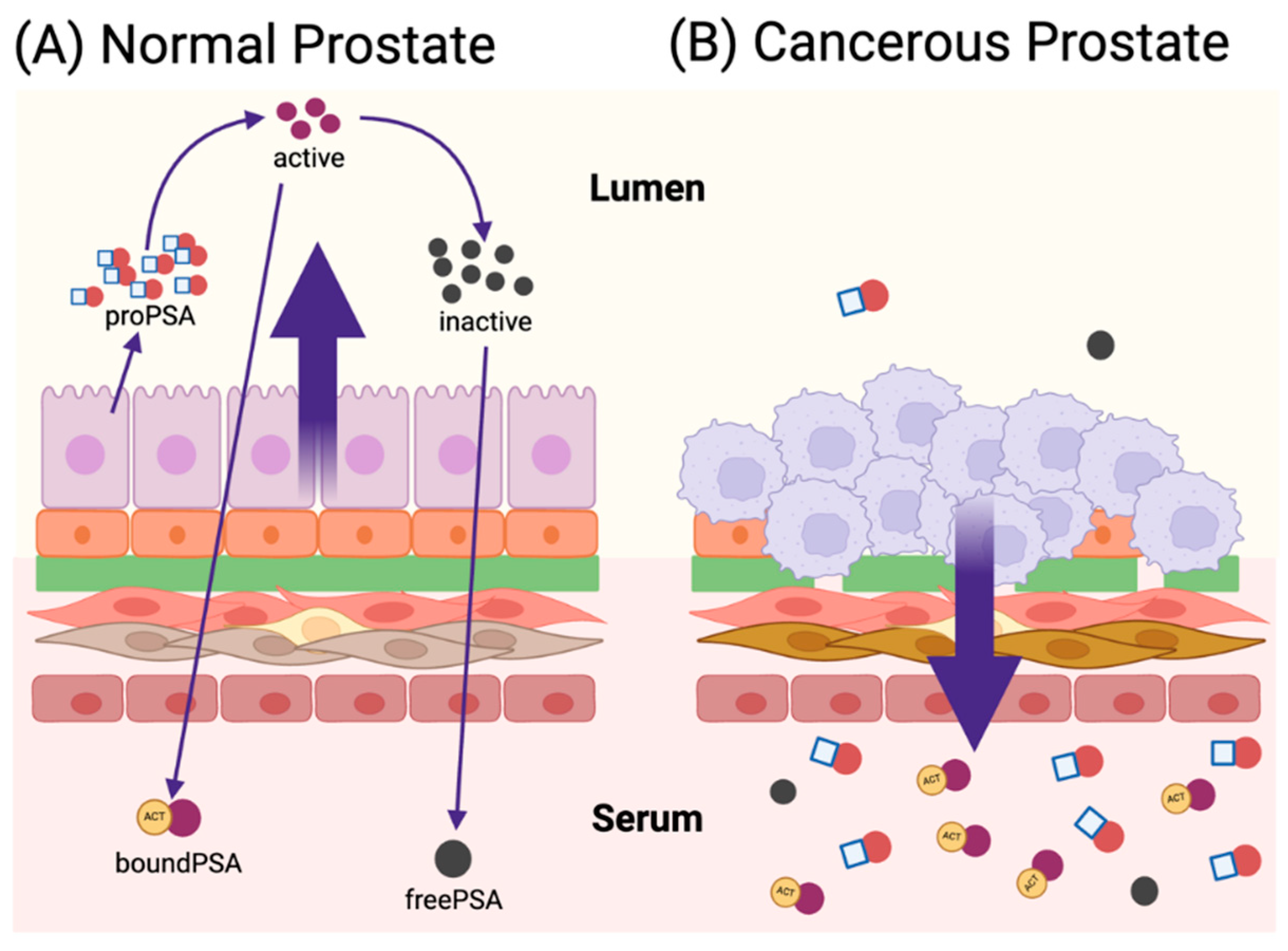
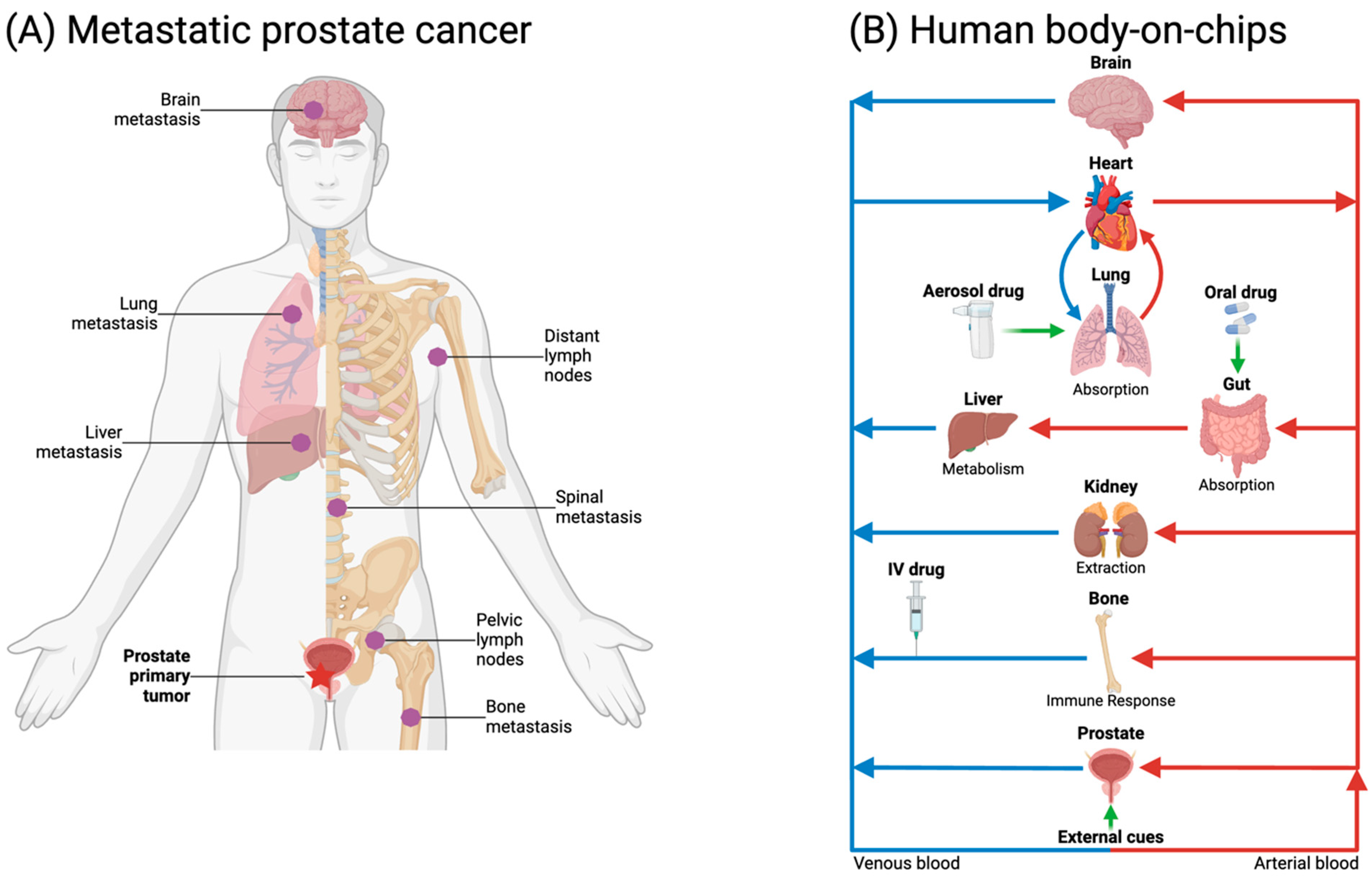
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szewczyk, K.; Jiang, L.; Khawaja, H.; Miranti, C.K.; Zohar, Y. Microfluidic Applications in Prostate Cancer Research. Micromachines 2024, 15, 1195. https://doi.org/10.3390/mi15101195
Szewczyk K, Jiang L, Khawaja H, Miranti CK, Zohar Y. Microfluidic Applications in Prostate Cancer Research. Micromachines. 2024; 15(10):1195. https://doi.org/10.3390/mi15101195
Chicago/Turabian StyleSzewczyk, Kailie, Linan Jiang, Hunain Khawaja, Cindy K. Miranti, and Yitshak Zohar. 2024. "Microfluidic Applications in Prostate Cancer Research" Micromachines 15, no. 10: 1195. https://doi.org/10.3390/mi15101195
APA StyleSzewczyk, K., Jiang, L., Khawaja, H., Miranti, C. K., & Zohar, Y. (2024). Microfluidic Applications in Prostate Cancer Research. Micromachines, 15(10), 1195. https://doi.org/10.3390/mi15101195






_Miranti.png)


