A Review of Intelligent Sensor-Based Systems for Pressure Ulcer Prevention
Abstract
:1. Introduction
2. The Scope of This Review vs. Previous Reviews
3. Methodology and Review
- Identifying the purpose and intended goals of the review (Section 3.1);
- Search strategy (Section 3.2);
- Screening for inclusion (Section 3.3);
- Screening for exclusion (Section 3.4);
- Data extraction (Section 3.5);
- Writing the review.
3.1. Purpose of the Review
3.2. Searching the Literature
3.3. Screening for Inclusion
3.4. Screening for Exclusion
3.5. Data Extraction and Article Synthesis
4. Discussion and Findings
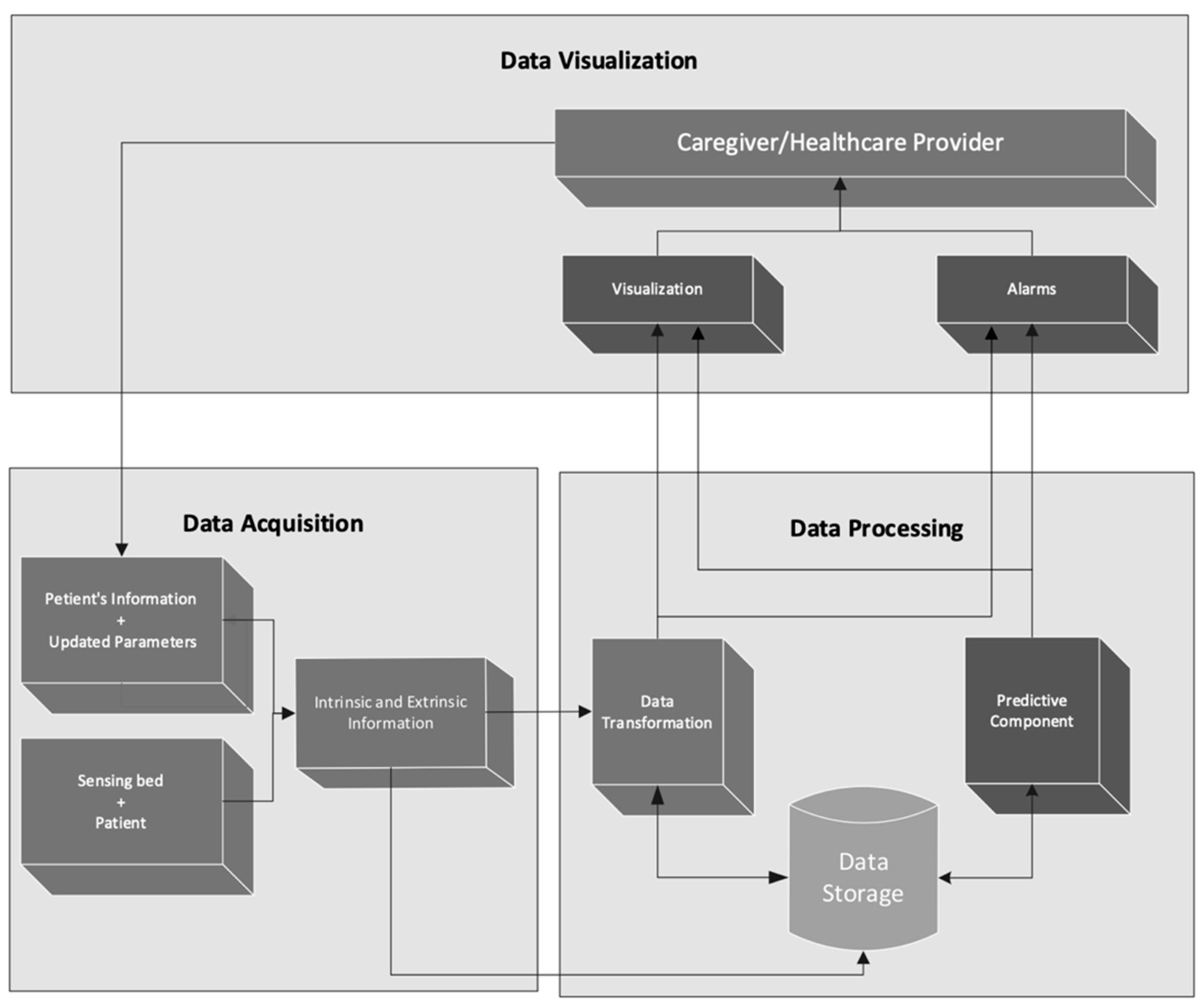
- Monitoring [12,14,17,22,24,29]—Information gathered from the sensors is stored in a server and can be accessed remotely by caregivers. This can include pressure maps for the platform or other relevant values (e.g., time since last change in position, physiological data, etc.). There are also some approaches where historical data regarding some of those values can be displayed, usually in graphical form. Mobile applications are often used by caregivers to access this information.
- Notifications [12,13,14,17,18,21,22,24,30,31]—The most common approach to ulcer prevention based on sensor information tends to be the raising of alarms in the caregivers’ mobile devices running a dedicated app. The most important alarm is raised when the patient is resting in the same position for longer than a specified amount of time. This reduces the risk of the patient resting for extended periods in the same position (the most common cause of pressure ulcers) and can save the caregiver’s time if the patient changes position spontaneously. Other alarms can be raised if the patient moves too much—when restlessness is a risk—or gets up from bed (maybe falling). Generally, the algorithms used for these alarms are very simple, relying in a few predefined rules to make the decision to raise an alarm or not.
- Personalization, e.g., [13,22,28]—Closely related with the previous points, several applications allow for the personalization of some items, both regarding visualization and alarms, dependent on the specific patient being monitored. Data to be visualized can be selected if it is relevant for that particular patient. Information regarding the patient’s medical history can be inputted into the application, to be displayed or used in some decision-making process. A specific example of this can be observed when patient dependent time limits are used for each lying position, e.g., to ensure less time is passed in a position that already has an ulcer.
- Actuation [14,17,28]—Some approaches use beds with actuators. These are not common and tend to be very expensive. As an example, temperature and humidity sensors can be used in conjunction with fans to control humidity and temperature. A few beds have pressure actuators that can control pressure in specific areas. Some of these actuators can be controlled remotely by the caregivers.
- Prediction [19,28]—The approaches we were most interested in were the ones that offered some kind of prediction of pressure ulcer occurrence based on diverse sources of information, both sensor-based and obtained in other ways, such as patient history or physiological data. Only two of the analyzed articles tackled this issue and, of these, only [28] provided a complete developed prediction approach, where instances constructed from both posture and non-posture data (only blood pressure is specifically mentioned) are labeled by health professionals and used to build a prediction model using a support vector machine algorithm. While the results of this approach are only validated in a simulated environment, and are not very conclusive, it still remains the only approach we have identified at this stage that tries to predict a probability of pressure ulcer occurrence based on multiple data streams and a complex ML algorithm.
5. A General Architecture for an Intelligent PU Prevention System
6. Conclusions and Future Work
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bluestein, D.; Javaheri, A. Pressure ulcers: Prevention, evaluation, and management. Am. Fam. Physicians 2008, 78, 1186–1194. [Google Scholar]
- Garcia, A.D.; Thomas, D.R. Assessment and management of chronic pressure ulcers in the elderly. Med. Clin. N. Am. 2006, 90, 925–944. [Google Scholar] [CrossRef]
- Haesler, E. (Ed.) National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance. In Prevention and Treatment of Pressure Ulcers: Quick Reference Guide; Cambridge Media: Osborne Park, Australia, 2014. [Google Scholar]
- National Institute for Health and Care Excellence: Pressure Ulcers. Quality Standard [QS89]. 2015. Available online: https://www.nice.org.uk/guidance/qs89 (accessed on 6 October 2021).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Marchione, F.G.; Araújo, L.M.Q.; Araújo, L. V: Approaches that use software to support the prevention of pressure ulcer: A systematic review. Int. J. Med. Inform. 2015, 84, 725–736. [Google Scholar] [CrossRef] [PubMed]
- Jiang, M.; Ma, Y.; Guo, S.; Jin, L.; Lv, L.; Han, L.; An, N. Using Machine Learning Technologies in Pressure Injury Management: Systematic Review. JMIR Med. Inf. 2021, 9, e25704. [Google Scholar] [CrossRef] [PubMed]
- Araujo, S.M.; Sousa, P.; Dutra, I. Clinical Decision Support Systems for Pressure Ulcer Management: Systematic Review. JMIR Med. Inf. 2020, 8, e21621. [Google Scholar] [CrossRef] [PubMed]
- Zahia, S.; Garcia Zapirain, M.B.; Sevillano, X.; González, A.; Kim, P.J.; Elmaghraby, A. Pressure injury image analysis with machine learning techniques: A systematic review on previous and possible future methods. Artif. Intell. Med. 2020, 102, 101742. [Google Scholar] [CrossRef] [PubMed]
- Koepp, J.; Baron, M.V.; Hernandes Martins, P.R.; Brandenburg, C.; Kira, A.T.F.; Trindade, V.D.; Ley Dominguez, L.M.; Carneiro, M.; Frozza, R.; Possuelo, L.G.; et al. The Quality of Mobile Apps Used for the Identification of Pressure Ulcers in Adults: Systematic Survey and Review of Apps in App Stores. JMIR mHealth uHealth 2020, 8, e14266. [Google Scholar] [CrossRef] [PubMed]
- Alinia, P.; Samadani, A.; Milosevic, M.; Ghasemzadeh, H.; Parvaneh, S. Pervasive Lying Posture Tracking. Sensors 2020, 20, 5953. [Google Scholar] [CrossRef] [PubMed]
- Pongthanisorn, G.; Viriyavit, W.; Prakayapan, T.; Deepaisam, S.; Somlertlamvanich, V. ECS: Elderly Care System for Fall and Bedsore Prevention using Non-Constraint Sensor. In Proceedings of the 2020 International Electronics Symposium (IES), Surabaya, Indonesia, 29–30 September 2020; pp. 340–344. [Google Scholar] [CrossRef]
- Bernal Monroy, E.; Polo Rodríguez, A.; Estevez, M.; Medina, J. Fuzzy Monitoring of In-bed Postural Changes for the Prevention of Pressure Ulcers using Inertial Sensors Attached to Clothing. J. Biomed. Inform. 2020, 107, 103476. [Google Scholar] [CrossRef] [PubMed]
- Abdelmoghith, A.; Shaaban, R.; Alsheghri, Z.; Ismail, L. IoT-Based Healthcare Monitoring System: Bedsores Prevention. In Proceedings of the 2020 Fourth World Conference on Smart Trends in Systems, Security and Sustainability (WorldS4), London, UK, 27–28 July 2020; pp. 64–69. [Google Scholar] [CrossRef]
- Polo Rodríguez, A.; Gil, D.; Nugent, C.; Medina, J. In-Bed Posture Classification from Pressure Mat Sensors for the Prevention of Pressure Ulcers Using Convolutional Neural Networks. In Bioinformatics and Biomedical Engineering; Springer: Cham, Switzerland, 2020. [Google Scholar] [CrossRef]
- Matar, G.; Lina, J.-M.; Kaddoum, G. Artificial Neural Network for in-Bed Posture Classification Using Bed-Sheet Pressure Sensors. IEEE J. Biomed. Health Inform. 2020, 24, 101–110. [Google Scholar] [CrossRef] [PubMed]
- Barroso, I.; Soares, S.; Rodrigues, V.; Silva, S.; Monteiro, M.; Rainho, C.; Duarte, D.; Valente, A. Assisted Care. In HCI International 2020—Late Breaking Papers: Universal Access and Inclusive Design; Springer: Cham, Switzerland, 2020. [Google Scholar] [CrossRef]
- Minteer, D.; Simon, P.; Taylor, D.; Jia, W.; Li, Y.; Sun, M.; Rubin, J. Pressure Ulcer Monitoring Platform—A Prospective, Human Subject Clinical Study to Validate Patient Repositioning Monitoring Device to Prevent Pressure Ulcers. Adv. Wound Care 2019, 9, 28–33. [Google Scholar] [CrossRef] [PubMed]
- Hong, Y.-S. Smart Care Beds for Elderly Patients with Impaired Mobility. Wirel. Commun. Mob. Comput. 2018, 2018, 1780904. [Google Scholar] [CrossRef] [Green Version]
- Pouyan, M.B.; Birjandtalab, J.; Heydarzadeh, M.; Nourani, M.; Ostadabbas, S. A pressure map dataset for posture and subject analytics. In Proceedings of the 2017 IEEE EMBS International Conference on Biomedical & Health Informatics (BHI), Orlando, FL, USA, 16–19 February 2017; pp. 65–68. [Google Scholar] [CrossRef]
- Qidwai, U.; Al-Sulaiti, S.; Ahmed, G.; Hegazy, A.; Ilyas, S.K. Intelligent integrated instrumentation platform for monitoring long-term bedridden patients. In Proceedings of the 2016 IEEE EMBS Conference on Biomedical Engineering and Sciences (IECBES), Kuala Lumpur, Malaysia, 4–8 December 2016; pp. 561–564. [Google Scholar] [CrossRef]
- Hsiao, R.-S.; Mi, Z.; Yang, B.-R.; Kau, L.-J.; Bitew, M.A.; Li, T.-Y. Body posture recognition and turning recording system for the care of bed bound patients. Technol. Health Care 2016, 24, S307–S312. [Google Scholar] [CrossRef] [PubMed]
- Hung, Y.-W.; Chiu, Y.; Jou, Y.-C.; Chen, W.-H.; Cheng, K.-S. Bed posture classification based on artificial neural network using fuzzy c-means and latent semantic analysis. J. Chin. Inst. Eng. 2015, 38, 415–425. [Google Scholar] [CrossRef]
- Daneshvarfard, F.; Moghimi, S.; Lotfi, R. Design and Evaluation of a Pressure and Temperature Monitoring System for Pressure Ulcer Prevention. Iran. J. Med. Phys. 2014, 11, 242–252. [Google Scholar] [CrossRef]
- Cruz-Santos, W.; Beltrán-Herrera, A.; Vázquez-Santacruz, E.; Gamboa-Zúñiga, M. Posture classification of lying down human bodies based on pressure sensors array. In Proceedings of the 2014 International Joint Conference on Neural Networks (IJCNN), Beijing, China, 6–11 July 2014; pp. 533–537. [Google Scholar] [CrossRef]
- Lee, H.J.; Hwang, S.H.; Lee, S.M.; Lim, Y.G.; Park, K.S. Estimation of Body Postures on Bed Using Unconstrained ECG Measurements. IEEE J. Biomed. Health Inform. 2013, 17, 985–993. [Google Scholar] [CrossRef] [PubMed]
- Bennett, S.L.; Goubran, R.; Rockwood, K.; Knoefel, F. Monitoring the relief of pressure points for pressure ulcer prevention: A subject dependent approach. In Proceedings of the 2013 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Gatineau, QC, Canada, 4–5 May 2013; pp. 135–138. [Google Scholar] [CrossRef]
- Yousefi, R.; Ostadabbas, S.; Faezipour, M.; Nourani, M.; Ng, V.; Tamil, L.; Bowling, A.; Behan, D.; Pompeo, M. A smart bed platform for monitoring & Ulcer prevention. In Proceedings of the 2011 4th International Conference on Biomedical Engineering and Informatics (BMEI), Shanghai, China, 15–17 October 2011; pp. 1362–1366. [Google Scholar] [CrossRef]
- Hsia, C.C.; Liou, K.J.; Aung, A.P.W.; Foo, V.; Huang, W.; Biswas, J. Analysis and comparison of sleeping posture classification methods using pressure sensitive bed system. In Proceedings of the 2009 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Minneapolis, MN, USA, 3–6 September 2009; pp. 6131–6134. [Google Scholar] [CrossRef]
- Lee, C.-N.; Yang, S.-C.; Li, C.-K.; Liu, M.-Z.; Kuo, P.-C. Alarm System For Bed Exit And Prolonged Bed Rest. In Proceedings of the 2018 International Conference on Machine Learning and Cybernetics (ICMLC), Chengdu, China, 15–18 July 2018; pp. 439–443. [Google Scholar] [CrossRef]
- Liu, J.; Chen, X.; Chen, S.; Liu, X.; Wang, Y.; Chen, L. TagSheet: Sleeping Posture Recognition with an Unobtrusive Passive Tag Matrix. In Proceedings of the IEEE INFOCOM 2019—IEEE Conference on Computer Communications, Paris, France, 29 April–2 May 2019; pp. 874–882. [Google Scholar] [CrossRef]
- Azeez, N.A.; Oyeniran, S.O.; der Vyver, C.; Misra, S.; Ahuja, R.; Damasevicius, R.; Maskeliunas, R. Diagnosing Oral Ulcers with Bayes Model. In Innovations in Bio-Inspired Computing and Applications; Abraham, A., Gandhi, N., Pant, M., Eds.; Springer International Publishing: Cham, Switzerland, 2019; pp. 485–494. [Google Scholar] [CrossRef]



| Review | Year | Focus | Studies | Timespan |
|---|---|---|---|---|
| [6] | 2015 | To identify the state-of-the-art approaches that use software to assist health professionals in PU prevention support. | 36 | 1989–2014 |
| [7] | 2021 | To analyze the use of ML technologies in PU management, identifying their strengths and weaknesses. | 32 | 2007–2020 |
| [8] | 2020 | To identify the outcomes from nurses when using support systems on clinical decision making for PU management. | 16 | 1995–2017 |
| [9] | 2020 | To describe imaging techniques used for the analysis and monitoring of pressure injuries, as an aid to their diagnosis, and proof of the efficiency of Deep Learning. | 82 | 1998–2018 |
| Review | Analysis/Results | Identified Opportunities and Future Research |
|---|---|---|
| [6] | Most of the approaches use sensors to monitor the patient’s exposure to pressure, temperature and humidity to generate reports regarding the intensity of each one of these risk factors, as well as the patient’s position in bed. Some approaches perform automated management of the risk factors using ventilation tubes and mattresses with porous cells to decrease the body’s temperature and movable cells to automatically redistribute the pressure over the body. | Perform Randomized Control Trials to verify which approaches are effective to reduce PU incidence and to verify which information provided by each of the approach is relevant to health professionals to support them in PU prevention. |
| [7] | Studies were classified and organized into three groups: 12 (38%) reported using ML technologies to develop predictive models to identify risk factors, 11 (34%) reported using them in posture detection and recognition, and 9 (28%) reported using them in image analysis for tissue classification and measurement of PU wound. | Apply these technologies on a large scale with clinical data to further verify and improve their effectiveness, as well as to improve methodological quality. The prevention of PU was studied under different approaches; however, they are related and should be studied together. For example: ML technologies on predictive model and posture recognition need feedback from PU wound image analysis to improve their performance. |
| [8] | All the analyzed studies describe knowledge-based systems that assessed the effects on clinical decision making, clinical effects secondary to clinical decision support system use, or factors that influenced the use, or intention to use, clinical decision support systems by health professionals and the success of their implementation in nursing practice. | Carry out studies that prioritize better adoption and interaction of nurses with clinical decision support systems, as well as studies with a representative sample of health care professionals. |
| [9] | This study focuses on previous contributions to wound image analysis, as well as an introduction to the usage of Deep Learning techniques as a more accurate approach for pressure injuries and chronic wound assessment. One of the findings is that one of the most limiting factors in the future evolution of pressure injury analysis via image processing is the scarcity of publicly available pressure injury image databases that allow a fair comparison between techniques | Concludes that 3D imaging techniques have proven successful for the retrieval of wound metrics that are essential for the efficient treatment of these wounds, and that the combination of these methods with Deep Learning techniques in a single system will eventually create a new optimal tool for accurate wound assessment and prognosis through imaging techniques. |
| Item | Description |
|---|---|
| sensors | Type of sensors (pressure, temperature, moisture, etc.) |
| features | Pre-processed features obtained from raw sensory data |
| algorithm | Algorithms used to process the data |
| alert | If and how the systems alert the caregivers |
| results | Main results achieved with the proposed approach |
| Sensors | Features | Algorithm | Recommendation | Results | |
|---|---|---|---|---|---|
| [11] | Single accelerometer | Amplitude, mean, minimum, and maximum values of the lateral and vertical axes | Ensemble trees, AdaLSTM to detect lying postures | NA | NA |
| [12] | Pressure and vibrational signals | Signal waves | Neural Network (NN) and Bayesian network for posture classification | Message notifications for going out of bed, period in same position and too frequent movement | Test household deployment with some problems |
| [13] | Three inertial sensors | Values for x, y, z data streams | SVM for posture classification, fuzzy knowledge-based system for protocol implementation | Priority of postural change for body zones | Preliminary tests with 7 users in controlled environment |
| [14] | Humidity, temperature sensors and force sensors | Sensor values, processing not described | A simple rule set to send notifications | Humidity and temperature values sent to a mobile application, so the caregiver can remotely adjust its levels. Notification of prolonged immobility. | Test performed with a mannequin, but results are not discussed |
| [15] | Pressure sensors | Gray image | A fuzzy approach to pre-process the signal, convolution NN for classification | NA | Good posture classification, but not tested with patient data |
| [16] | Pressure sensors | Histograms of oriented gradients and local binary patterns are computed from the original pressure image | Feed forward NN | NA | Competitive four posture classification when compared with state-of-the-art approaches |
| [17] | Humidity and temperature RFID sensors | Sensor values | Not described | Position change notifications | Tested in two homes with four patients, but with no significant results from the sensors |
| [18] | Accelerometer, gyroscope, magnetometer, light sensor and a thermometer for prototype 1, four pressure sensors for prototype 2 | Nine output channels for prototype 1, for pressure measures for prototype 2 | Not described | NA | Clinical trial with 10 patients, relatively high success in detecting repositioning |
| [19] | Pressure from Force Sensitive Application (FSA) pressure mapping mattresses. | Sensor values regarding both the average body size by age and the frequent location of bedsores | A sensing algorithm for fall risk assessment and pressure ulcer occurrence warning | Alerts using Google Firebase Cloud Messaging | Works well for several human models of various heights and weights |
| [20] | Pressure, using a commercial pressure mat | The input is a frame of the body pressure map. The pressure mat has 2048 sensor points. | Deep learning for subject identification in three common sleeping postures using statistical features extracted from the pressure distribution. Use of Restricted Boltzmann Machines to pretrain the model and find proper initial weights for training deep belief networks. | NA | Experiments showed promising results in subject identification and further validated the personal sleeping style of each participant |
| [21] | Force-sensitive sensor-strips placed under the patient on the bed on specific pressure zones, and a smart camera with embedded image processing | Values of the pressure sensors | Image processing algorithm developed to enhance the accuracy of determining whether the patient was moved | Displays/alerts for the medical staff | Initial results are very encouraging |
| [22] | Pressure sensors and patient’s body weight | Pressure sensing pad, containing force sensing resistor sensors, is used to detect patient’s body posture | Recognition algorithm based on fuzzy theory | The system notifies caregivers to change the patient’s body posture | The average posture recognition accuracy of this proposed module is 92% |
| [23] | Pressure sensor pad with 18 × 12 array of force sensing resistors | Pressure maps | Fuzzy c-means (FCM) algorithm used to transform the pressure contours and identify regions of interest (ROI) with high pressure for pressure ulcer prevention. An artificial neural network (ANN) model was applied for posture classification using the reduced feature vector. | NA | Posture classification |
| [24] | Temperature and pressure values from an array of sensors to prevent pressure ulcers (64 pressure and 64 temperature sensors) | Temperature map and pressure vs. time map | A MATLAB software developed to report real-time pressure and temperature maps, retrieve previous maps and risks, and generate alarms | Alarm is generated by the software if the pressure intensity of one sensor exceeded the adjusted threshold, and the pressure duration was longer than the time threshold | The proposed method for detecting posture was verified using a statistical analysis |
| [25] | Low-resolution pressure sensor array | Pressure maps from values acquired using a pressure sensor array | HOG and SIFT descriptors extracted from the pressure maps, that are considered as gray scale images | NA | The classification of posture pressure maps can be classified with a performance of 99.7% |
| [26] | Unconstrained ECG data measured from 12 CC electrodes on a bed were used for classification of four basic lying postures. | Average of ECG signals from contacted electrodes | Body posture estimation algorithm based on the QRS (Q wave, R wave, and S wave of ECG) complex of ECG measured capacitively from 12 channels on a bed. The features are extracted based on the morphology of the QRS complex and used in linear discriminant analysis, support vector machines with linear and radial basis function (RBF) kernels, and artificial neural networks (one and two layers). | NA | Body postures |
| [27] | Pressure sensitive mats. A 3 by 8 fiber optic pressure sensor array, embedded in polymer foam. | Mat software on a laptop receives data via Bluetooth and collects it in a file. A video is also recorded with patient movements. | Subject dependent algorithm that was able to detect when and where pressure points were relieved from underneath a supine subject, without any user inputs or assumptions | NA | The algorithm is able to detect when and where a pressure point was relieved |
| [28] | Used two types of sensor data: (1) posture-independent (e.g., physiological) data, such as blood pressure, and (2) posture-dependent values, such as pressure, temperature, or moisture on each point of body in contact with bed | Pressure images based on values acquired using pressure sensors | Support vector machines (SVM) are used to train a model for assessing a patient’s risk of developing pressure ulcers, by combining the features extracted in the modeling and profiling | The bed has a surface that creates a movable surface that can manipulate a patient without grasping her/him. Machine intelligence is used to analyze data, assess the risk and alert caregivers to intervene at an early stage to prevent pressure ulcers. | NA |
| [29] | Pressure sensors matrix | Values from pressure sensors | Algorithm to determine sleeping postures using Kurtosis and Skewness Estimation Approach, principal component analysis and support vector machines (SVM) for classification | NA | Results show that a 16-sensor configuration can detect the 3 sleeping postures with high accuracy for patients with low mobility. Its accuracy starts to drop when patients move and sleep on different angles. |
| [30] | Piezoresistive pressure sensors | Values of pressure sensors from a mattress of 10 sensors laid in bed to explore 8 states. | Alarm on/off based on pressure variation measured over time | Time-based alarm sent by a message to computer or mobile phone | No results are presented |
| [31] | Passive RFID tags. A 30 × 18 tag matrix on a thin plastic film. | Snapshot (a gray-scale image that consists of 30 × 18 pixels) of sleeping postures. | Sleep postures are identified in TagSheet by pre-processing each snapshot using Gaussian blur, Ostu-based binary conversion of the gray-level image and removal of scattered pixels. | NA | According to authors, experimental results show that TagSheet has a great performance |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silva, A.; Metrôlho, J.; Ribeiro, F.; Fidalgo, F.; Santos, O.; Dionisio, R. A Review of Intelligent Sensor-Based Systems for Pressure Ulcer Prevention. Computers 2022, 11, 6. https://doi.org/10.3390/computers11010006
Silva A, Metrôlho J, Ribeiro F, Fidalgo F, Santos O, Dionisio R. A Review of Intelligent Sensor-Based Systems for Pressure Ulcer Prevention. Computers. 2022; 11(1):6. https://doi.org/10.3390/computers11010006
Chicago/Turabian StyleSilva, Arlindo, José Metrôlho, Fernando Ribeiro, Filipe Fidalgo, Osvaldo Santos, and Rogério Dionisio. 2022. "A Review of Intelligent Sensor-Based Systems for Pressure Ulcer Prevention" Computers 11, no. 1: 6. https://doi.org/10.3390/computers11010006
APA StyleSilva, A., Metrôlho, J., Ribeiro, F., Fidalgo, F., Santos, O., & Dionisio, R. (2022). A Review of Intelligent Sensor-Based Systems for Pressure Ulcer Prevention. Computers, 11(1), 6. https://doi.org/10.3390/computers11010006









