A Long Short-Term Memory Network Using Resting-State Electroencephalogram to Predict Outcomes Following Moderate Traumatic Brain Injury
Abstract
1. Introduction
2. Methodology
2.1. Participants
2.2. Patients’ Outcome Assessment
2.3. EEG Data Acquisition
2.4. EEG Dataset Preparation
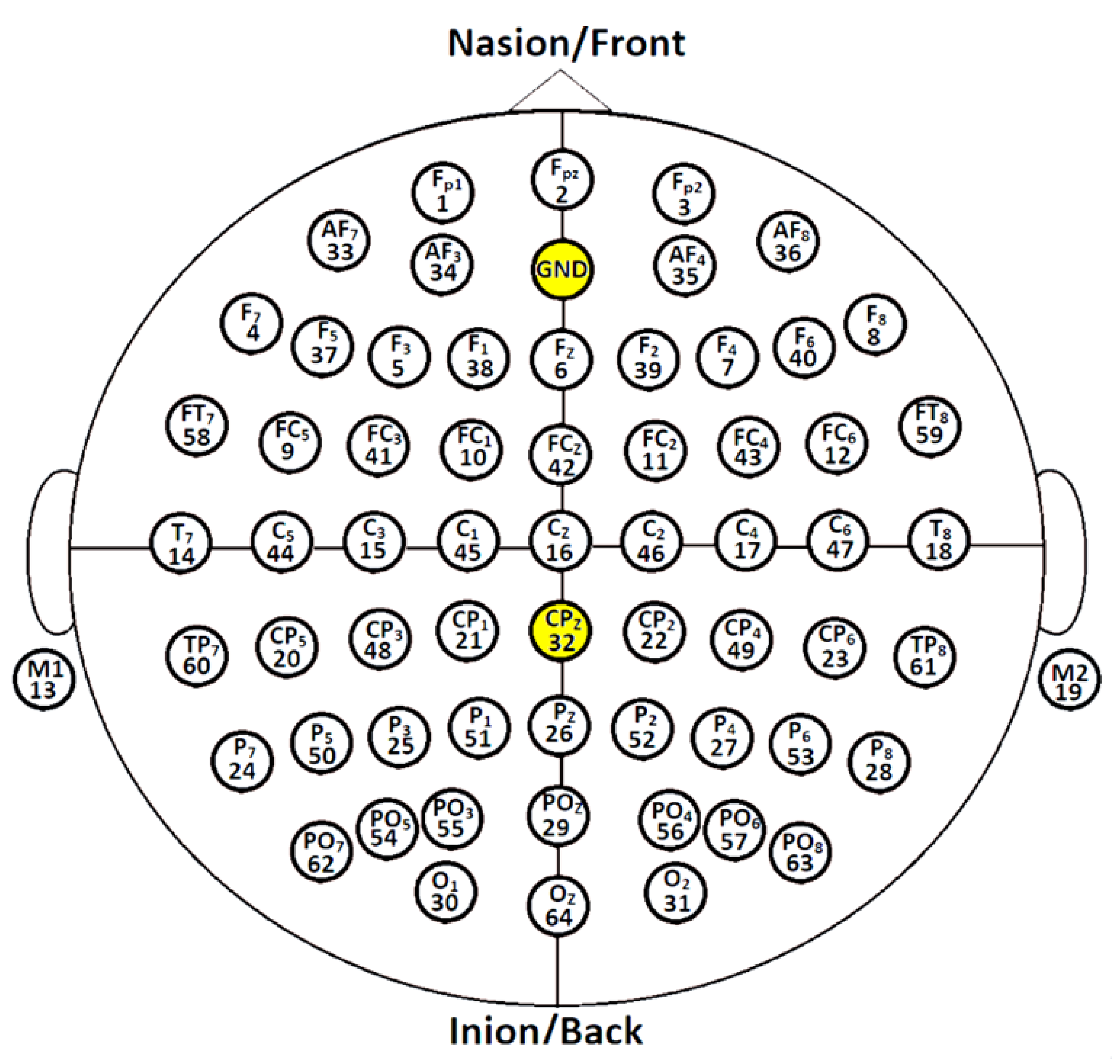
2.5. EEG Data Processing and Input EEG Signal Representation
2.6. Long Short-Term Memory
2.7. Data Augmentation Approach for Imbalanced Dataset
2.8. Training Procedure and Performance Evaluation for Imbalanced Dataset
3. Results and Discussion
| Architecture | Accuracy ± SD | [CI] |
|---|---|---|
| Support Vector Machine (SVM); | 81.98 ± 5.13 | [80.69, 83.27] |
| Chennu et al. [69] | ||
| Multivariate Auto Regression (MVAR); | 78.03 ± 21.07 | [73.29, 82.77] |
| Schorr et al. [70] | ||
| Logistic Regression (LR); | 49.97 ± 2.51 | [49.56, 50.37] |
| Lee et al. [71] | ||
| Proposed Raw-LSTM | 87.50 ± 0.05 | [87.12, 88.34] |
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Centers for Disease Control and Prevention. Available online: https://www.cdc.gov/traumaticbraininjury/get_the_facts.html (accessed on 5 July 2022).
- Rutland-Brown, W.; Langlois, J.A.; Thomas, K.E.; Xi, Y.L. Incidence of traumatic brain injury in the United States, 2003. J. Head Trauma Rehabil. 2006, 21, 544–548. [Google Scholar] [CrossRef] [PubMed]
- Feigin, V.; Theadom, A.; Barker-Collo, S.; Starkey, N.; McPherson, K.; Kahan, M.; Dowell, A.; Brown, P.; Parag, V.; Kydd, R.; et al. Incidence of traumatic brain injury in New Zealand: A population-based study. Lancet Neurol. 2013, 12, 53–64. (In English) [Google Scholar] [CrossRef] [PubMed]
- Dewan, M.; Rattani, A.; Gupta, S.; Baticulon, R.; Hung, Y.-C.; Punchak, M.; Agrawal, A.; Adeleye, A.; Shrime, M.; Rubiano, A.; et al. Estimating the global incidence of traumatic brain injury. J. Neurosurg. 2019, 130, 1080–1097. [Google Scholar] [CrossRef]
- Teasdale, G.; Jennett, B. Assessment of coma and impaired consciousness. A practical scale. Lancet 1974, 2, 81–84. (In English) [Google Scholar] [CrossRef]
- Teasdale, G.; Murray, G.; Parker, L.; Jennett, B. Adding up the Glasgow Coma Score. Acta Neurochir. Suppl. (Wien) 1979, 28, 13–16. [Google Scholar]
- Gomez, D.; Byrne, J.; Alali, A.; Xiong, W.; Hoeft, C.; Neal, M.; Subacius, H.; Nathens, A. Inclusion of highest glasgow coma scale motor component score in mortality risk adjustment for benchmarking of trauma center performance. J. Am. Coll. Surg. 2017, 225, 755–762. [Google Scholar] [CrossRef] [PubMed]
- Mena, J.H.; Sanchez, A.I.; Rubiano, A.M.; Peitzman, A.B.; Sperry, J.L.; Gutierrez, M.I.; Puyana, J.C. Effect of the modified Glasgow Coma Scale score criteria for mild traumatic brain injury on mortality prediction: Comparing classic and modified Glasgow Coma Scale score model scores of 13. J. Trauma 2011, 71, 1185–1193. (In English) [Google Scholar] [CrossRef]
- Watanitanon, A.; Lyons, V.H.; Lele, A.V.; Krishnamoorthy, V.; Chaikittisilpa, N.; Chandee, T.; Vavilala, M.S. Clinical Epidemiology of Adults With Moderate Traumatic Brain Injury. Crit. Care Med. 2018, 46, 781–787. (In English) [Google Scholar] [CrossRef]
- Cassidy, J.D.; Carroll, L.J.; Peloso, P.M.; Borg, J.; von Holst, H.; Holm, L.; Kraus, J.; Coronado, V.G.; WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. Incidence, risk factors and prevention of mild traumatic brain injury: Results of the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. J. Rehabil. Med. 2004, 36, 28–60. [Google Scholar] [CrossRef]
- Selassie, A.W.; Zaloshnja, E.; Langlois, J.A.; Miller, T.; Jones, P.; Steiner, C. Incidence of long-term disability following traumatic brain injury hospitalization, United States, 2003. J. Head Trauma Rehabil. 2008, 23, 123–131. [Google Scholar] [CrossRef]
- Steppacher, I.; Kaps, M.; Kissler, J. Against the odds: A case study of recovery from coma after devastating prognosis. Ann. Clin. Transl. Neurol. 2016, 3, 61–65. [Google Scholar] [CrossRef]
- Andriessen, T.M.J.C.; Horn, J.; Franschman, G.; van der Naalt, J.; Haitsma, I.; Jacobs, B.; Steyerberg, E.W.; Vos, P.E. Epidemiology, severity classification, and outcome of moderate and severe traumatic brain injury: A prospective multicenter study. J. Neurotrauma 2011, 28, 2019–2031. [Google Scholar] [CrossRef] [PubMed]
- Fearnside, M.; Mcdougall, P. Moderate Head Injury: A system of neurotrauma care. Aust. N. Z. J. Surg. 1998, 68, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Fabbri, A.; Servadei, F.; Marchesini, G.; Stein, S.C.; Vandelli, A. Early predictors of unfavourable outcome in subjects with moderate head injury in the emergency department. J. Neurol. Neurosurg. Psychiatry 2008, 79, 567. [Google Scholar] [CrossRef]
- Compagnone, C.; d’Avella, D.; Servadei, F.; Angileri, F.F.; Brambilla, G.; Conti, C.; Cristofori, L.; Delfini, R.; Denaro, L.; Ducati, A.; et al. Patients with moderate head injury: A prospective multicenter study of 315 patients. Neurosurgery 2009, 64, 690–697. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health and Human Services. Centers for Disease Control and Prevention. Moderate to Severe Traumatic Injury Is a Lifelong Condition. Available online: https://www.cdc.gov/traumaticbraininjury/pdf/moderate_to_severe_tbi_lifelong-a.pdf (accessed on 11 November 2022).
- Einarsen, C.E.; Naalt, J.V.; Jacobs, B.; Follestad, T.; Moen, K.G.; Vik, A.; Håberg, A.K.; Skandsen, T. Moderate traumatic brain injury: Clinical characteristics and a prognostic model of 12-month outcome. World Neurosurg. 2018, 114, e1199–e1210. [Google Scholar] [CrossRef] [PubMed]
- Department of Statistics Malaysia. Statistics on Causes of Death, Malaysia. 2021. Available online: https://www.dosm.gov.my/v1/index.php?r=column/cthemeByCat&cat=401&bul_id=R3VrRUhwSXZDN2k4SGN6akRhTStwQT09&menu_id=L0pheU43NWJwRWVSZklWdzQ4TlhUUT09 (accessed on 4 July 2022).
- Ministry of Health Malaysia Planning Division. Ministry of Health Malaysia, Kementerian Kesihatan Malaysia (KKM) Health Facts; Ministry of Health Malaysia Planning Division: Putrajaya, Malaysia, 2021.
- Schmitt, S.; Dichter, M.A. Electrophysiologic Recordings in Traumatic Brain Injury, 1st ed.; Elsevier B.V.: Amsterdam, The Netherlands, 2015; pp. 319–339. [Google Scholar]
- Walker, W.C.; Stromberg, K.A.; Marwitz, J.H.; Sima, A.P.; Agyemang, A.A.; Graham, K.M.; Harrison-Felix, C.; Hoffman, J.M.; Brown, A.W.; Kreutzer, J.S.; et al. Predicting long-term global outcome after traumatic brain injury: Development of a practical prognostic tool using the traumatic brain injury model systems national database. J. Neurotrauma 2018, 35, 1587–1595. [Google Scholar] [CrossRef]
- Maas, A.I.R.; Marmarou, A.; Murray, G.D.; Teasdale, S.G.M.; Steyerberg, E.W. Prognosis and clinical trial design in traumatic brain injury: The IMPACT study. J. Neurotrauma 2007, 24, 232–238. [Google Scholar] [CrossRef]
- Han, J.; King, N.K.K.; Neilson, S.J.; Gandhi, M.P.; Ng, I. External validation of the CRASH and IMPACT prognostic models in severe traumatic brain injury. J. Neurotrauma 2014, 31, 1146–1152. (In English) [Google Scholar] [CrossRef]
- MRC CRASH Trial Collaborators; Perel, P.; Arango, M.; Clayton, T.; Edwards, P.; Komolafe, E.; Poccock, S.; Roberts, I.; Shakur, H.; Steyerberg, E.; et al. Predicting outcome after traumatic brain injury: Practical prognostic models based on large cohort of international patients. BMJ 2008, 336, 425–429. [Google Scholar] [CrossRef]
- Lingsma, H.F.; Roozenbeek, B.; Steyerberg, E.W.; Murray, G.D.; Maas, A.I.R. Early prognosis in traumatic brain injury: From prophecies to predictions. Lancet Neurol. 2010, 9, 543–554. [Google Scholar] [CrossRef] [PubMed]
- Noor, N.S.E.M.; Ibrahim, H. Predicting outcomes in patients with traumatic brain injury using machine learning models. In Intelligent Manufacturing and Mechatronics, Melaka, Malaysia; Springer: Berlin/Heidelberg, Germany, 2019; pp. 12–20. [Google Scholar]
- Weir, J.; Steyerberg, E.W.; Butcher, I.; Lu, J.; Lingsma, H.F.; McHugh, G.S.; Roozenbeek, B.; Maas, A.I.R.; Murray, G.D. Does the extended glasgow outcome scale add value to the conventional glasgow outcome scale? J. Neurotrauma 2012, 29, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Haveman, M.E.; Putten, M.J.A.M.V.; Hom, H.W.; Eertman-Meyer, C.J.; Beishuizen, A.; Tjepkema-Cloostermans, M.C. Predicting outcome in patients with moderate to severe traumatic brain injury using electroencephalography. Crit. Care 2019, 23, 401. [Google Scholar] [CrossRef] [PubMed]
- van den Brink, R.L.; Nieuwenhuis, S.; van Boxtel, G.J.M.; Luijtelaar, G.v.; Eilander, H.J.; Wijnen, V.J.M. Task-free spectral EEG dynamics track and predict patient recovery from severe acquired brain injury. NeuroImage Clin. 2018, 17, 43–52. [Google Scholar] [CrossRef] [PubMed]
- Noor, N.S.E.M.; Ibrahim, H.; Lah, M.H.C.; Abdullah, J.M. Improving Outcome Prediction for Traumatic Brain Injury from Imbalanced Datasets Using RUSBoosted Trees on Electroencephalography Spectral Power. IEEE Access 2021, 9, 121608–121631. [Google Scholar] [CrossRef]
- Noor, N.S.E.M.; Ibrahim, H.; Lah, M.H.C.; Abdullah, J.M. Prediction of Recovery from Traumatic Brain Injury with EEG Power Spectrum in Combination of Independent Component Analysis and RUSBoost Model. Biomedinformatics 2022, 2, 106–123. [Google Scholar] [CrossRef]
- Noor, N.S.E.M.; Ibrahim, H. Machine learning algorithms and quantitative electroencephalography predictors for outcome prediction in traumatic brain injury: A systematic review. IEEE Access 2020, 8, 102075–102092. [Google Scholar] [CrossRef]
- He, Y.; Eguren, D.; Azorín, J.M.; Grossman, R.G.; Luu, T.P.; Contreras-Vidal, J.L. Brain–machine interfaces for controlling lower-limb powered robotic systems. J. Neural Eng. 2018, 15, 021004. [Google Scholar] [CrossRef]
- Chen, R.; Parhi, K.K. Seizure Prediction using Convolutional Neural Networks and Sequence Transformer Networks. In Proceedings of the 2021 43rd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Guadalajara, Mexico, 1–5 November 2021; pp. 6483–6486. [Google Scholar]
- Jana, R.; Mukherjee, I. Deep learning based efficient epileptic seizure prediction with EEG channel optimization. Biomed. Signal Process. Control 2021, 68, 102767. [Google Scholar] [CrossRef]
- Attia, T.P.; Viana, P.F.; Nasseri, M.; Richardson, M.P.; Brinkmann, B.H. Seizure forecasting from subcutaneous EEG using long short term memory neural networks: Algorithm development and optimization. In Proceedings of the 2021 IEEE International Conference on Bioinformatics and Biomedicine (BIBM), Houston, TX, USA, 9–12 December 2021; pp. 3599–3602. [Google Scholar]
- Sekkal, R.N.; Bereksi-Reguig, F.; Ruiz-Fernandez, D.; Dib, N.; Sekkal, S. Automatic sleep stage classification: From classical machine learning methods to deep learning. Biomed. Signal Process. Control 2022, 77, 103751. [Google Scholar] [CrossRef]
- Zhao, D.; Jiang, R.; Feng, M.; Yang, J.; Wang, Y.; Hou, X.; Wang, X. A deep learning algorithm based on 1D CNN-LSTM for automatic sleep staging. Technol. Health Care 2022, 30, 323–336. [Google Scholar] [CrossRef] [PubMed]
- Khalili, E.; Asl, B.M. Automatic sleep stage classification using temporal convolutional neural network and new data augmentation technique from raw single-channel EEG. Comput. Methods Programs Biomed. 2021, 204, 106063. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.; You, B.; Liu, Y.; Dai, Y. Patient-specific method of sleep electroencephalography using wavelet packet transform and Bi-LSTM for epileptic seizure prediction. Biomed. Signal Process. Control 2021, 70, 102963. [Google Scholar] [CrossRef]
- Gong, S.; Xing, K.; Cichocki, A.; Li, J. Deep learning in EEG: Advance of the last ten-year critical period. IEEE Trans. Cogn. Dev. Syst. 2021. [Google Scholar] [CrossRef]
- Hochreiter, S.; Schmidhuber, J. Long short-term memory. Neural Comput. 1997, 9, 1735–1780. [Google Scholar] [CrossRef]
- Levin, H.S.; Diaz-Arrastia, R.R. Diagnosis, prognosis, and clinical management of mild traumatic brain injury. Lancet Neurol. 2015, 14, 506–517. (In English) [Google Scholar] [CrossRef]
- McMillan, T.; Wilson, L.; Ponsford, J.; Levin, H.; Teasdale, G.; Bond, M. The glasgow outcome scale—40 years of application and refinement. Nat. Rev. Neurol. 2016, 12, 477. [Google Scholar] [CrossRef]
- Jennett, B.; Snoek, J.; Bond, M.R.; Brooks, N. Disability after severe head injury: Observations on the use of the glasgow outcome scale. J. Neurol. Neurosurg. Psychiatry 1981, 44, 285–293. [Google Scholar] [CrossRef]
- Jennett, B.; Bond, M. Assessment of outcome after severe brain damage: A practical scale. Lancet 1975, 305, 480–484. [Google Scholar] [CrossRef]
- Delorme, A.; Makeig, S. EEGLAB: An open source toolbox for analysis of single-trial EEG dynamics including independent component analysis. J. Neurosci. Methods 2004, 134, 9–21. [Google Scholar] [CrossRef]
- Alhussein, M.; Muhammad, G.; Hossain, M.S. EEG pathology detection based on deep learning. IEEE Access 2019, 7, 27781–27788. [Google Scholar] [CrossRef]
- Altıntop, Ç.G.; Latifoğlu, F.; Akın, A.K.; Çetin, B. A novel approach for detection of consciousness level in comatose patients from EEG signals with 1-D convolutional neural network. Biocybern. Biomed. Eng. 2022, 42, 16–26. [Google Scholar] [CrossRef]
- Chambon, S.; Galtier, M.N.; Arnal, P.J.; Wainrib, G.; Gramfort, A. A deep learning architecture for temporal sleep stage classification using multivariate and multimodal time series. IEEE Trans. Neural Syst. Rehabil. Eng. 2018, 26, 758–769. [Google Scholar] [CrossRef] [PubMed]
- Lai, C.Q.; Ibrahim, H.; Abdullah, M.Z.; Abdullah, J.M.; Suandi, S.A.; Azman, A. Arrangements of Resting State Electroencephalography as the Input to Convolutional Neural Network for Biometric Identification. Comput. Intell. Neurosci. 2019, 2019, 7895924. [Google Scholar] [CrossRef]
- Salehinejad, H.; Sankar, S.; Barfett, J.; Colak, E.; Valaee, S. Recent advances in recurrent neural networks. arXiv 2017, arXiv:1801.01078. [Google Scholar] [CrossRef]
- Srivastava, N.; Hinton, G.; Krizhevsky, A.; Sutskever, I.; Salakhutdinov, R. Dropout: A simple way to prevent neural networks from overfitting. J. Mach. Learn. Res. 2014, 15, 1929–1958. [Google Scholar]
- Salamon, J.; Bello, J.P. Deep convolutional neural networks and data augmentation for environmental sound classification. IEEE Signal Process. Lett. 2017, 24, 279–283. [Google Scholar] [CrossRef]
- Ahlawat, K.; Chug, A.; Singh, A.P. Benchmarking framework for class imbalance problem using novel sampling approach for big data. Int. J. Syst. Assur. Eng. Manag. 2019, 10, 824–835. [Google Scholar] [CrossRef]
- Longadge, R.; Dongre, S. Class imbalance problem in data mining review. arXiv 2013, arXiv:1305.1707. [Google Scholar] [CrossRef]
- Alhudhaif, A. A novel multi-class imbalanced EEG signals classification based on the adaptive synthetic sampling (ADASYN) approach. PeerJ Comput. Sci. 2021, 7, e523. [Google Scholar] [CrossRef]
- Chawla, N.V.; Lazarevic, A.; Hall, L.O.; Bowyer, K.W. SMOTEBoost: Improving prediction of the minority class in boosting. In Proceedings of the European Conference on Principles of Data Mining and Knowledge Discovery, Cavtat-Dubrovnik, Croatia, 22–26 September 2003; Springer: Berlin/Heidelberg, Germany, 2003; pp. 107–119. [Google Scholar]
- Krishnamoorthy, V.; Shoorangiz, R.; Weddell, S.J.; Beckert, L.; Jones, R.D. Deep Learning with Convolutional Neural Network for detecting microsleep states from EEG: A comparison between the oversampling technique and cost-based learning. In Proceedings of the 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Berlin, Germany, 23–27 July 2019; pp. 4152–4155. [Google Scholar]
- Buda, M.; Maki, A.; Mazurowski, M.A. A systematic study of the class imbalance problem in convolutional neural networks. Neural Netw. 2018, 106, 249–259. [Google Scholar] [CrossRef] [PubMed]
- Zoubir, A.M.; Boashash, B. The bootstrap and its application in signal processing. IEEE Signal Process. Mag. 1998, 15, 56–76. [Google Scholar] [CrossRef]
- Efron, B. The bootstrap and modern statistics. J. Am. Stat. Assoc. 2000, 95, 1293–1296. [Google Scholar] [CrossRef]
- Kaur, H.; Pannu, H.S.; Malhi, A.K. A systematic review on imbalanced data challenges in machine learning: Applications and solutions. ACM Comput. Surv. (CSUR) 2019, 52, 1–36. [Google Scholar] [CrossRef]
- Sun, Y.; Wong, A.K.C.; Kamel, M.S. Classification of imbalanced data: A review. Int. J. Pattern Recognit. Artif. Intell. 2009, 23, 687–719. [Google Scholar] [CrossRef]
- He, C.; Liu, J.; Zhu, Y.; Du, W. Data Augmentation for Deep Neural Networks Model in EEG Classification Task: A Review. Front. Hum. Neurosci. 2021, 15, 765525. (In English) [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Zhang, X.-R.; Zhang, B.; Lei, M.-Y.; Cui, W.-G.; Guo, Y.-Z. A channel-projection mixed-scale convolutional neural network for motor imagery EEG decoding. IEEE Trans. Neural Syst. Rehabil. Eng. 2019, 27, 1170–1180. [Google Scholar] [CrossRef]
- Lee, T.; Kim, M.; Kim, S.-P. Data augmentation effects using borderline-SMOTE on classification of a P300-based BCI. In Proceedings of the 2020 8th International Winter Conference on Brain-Computer Interface (BCI), Gangwon, Republic of Korea, 26–28 February 2020; pp. 1–4. [Google Scholar]
- Chennu, S.; Annen, J.; Wannez, S.; Thibaut, A.; Chatelle, C.; Cassol, H.; Martens, G.; Schnakers, C.; Gosseries, O.; Menon, D.; et al. Brain networks predict metabolism, diagnosis and prognosis at the bedside in disorders of consciousness. Brain 2017, 140, 2120–2132. [Google Scholar] [CrossRef]
- Schorr, B.; Schlee, W.; Arndt, M.; Bender, A. Coherence in resting-state EEG as a predictor for the recovery from unresponsive wakefulness syndrome. J. Neurol. 2016, 263, 937–953. [Google Scholar] [CrossRef]
- Lee, H.; Mizrahi, M.A.; Hartings, J.A.; Sharma, S.; Pahren, L.; Ngwenya, L.B.; Moseley, B.D.; Privitera, M.; Tortella, F.C.; Foreman, B. Continuous electroencephalography after moderate to severe traumatic brain injury. Crit. Care Med. 2019, 47, 574–582. (In English) [Google Scholar] [CrossRef]
- Chen, M.; Li, Z.; Yan, Z.; Ge, S.; Zhang, Y.; Yang, H.; Zhao, L.; Liu, L.; Zhang, X.; Cai, Y.; et al. Predicting neurological deterioration after moderate traumatic brain injury: Development and validation of a prediction model based on data collected on admission. J. Neurotrauma 2022, 39, 371–378. (In English) [Google Scholar] [CrossRef] [PubMed]
- Cnossen, M.C.; Polinder, S.; Andriessen, T.M.; van der Naalt, J.; Haitsma, I.; Horn, J.; Franschman, G.; Vos, P.E.; Steyerberg, E.W.; Lings, H. Causes and Consequences of Treatment Variation in Moderate and Severe Traumatic Brain Injury: A Multicenter Study. Crit. Care Med. 2017, 45, 660–669. (In English) [Google Scholar] [CrossRef] [PubMed]


| GOS Score | Functional Meaning | Outcome |
|---|---|---|
| 1 | Death | Poor |
| 2 | Persistent vegetative state; patient unresponsive and speechless for weeks or months | Poor |
| 3 | Severe disability; patients dependent on daily support | Poor |
| 4 | Moderate disability; patients independent in daily life | Poor |
| 5 | Good recovery; resumption of everyday life with minor neurological and physiological deficits | Good |
| Parameter | Setting |
|---|---|
| Learning rate | 0.001 |
| Minibatch size | 3 |
| regularization | 0.0005 |
| Optimizer | Adam |
| Training repetitions per epoch | 30 |
| Performance Metric | (%) | 95% CI | (%) |
|---|---|---|---|
| Accuracy ± SD | 87.50 ± 0.05 | [CI] | [87.12, 88.34] |
| Sensitivity ± SD | 91.65 ± 0.12 | [CI] | [90.13, 93.12] |
| Specificity ± SD | 87.50 ± 0.13 | [CI] | [82.13, 85.54] |
| G-mean ± SD | 87.50 ± 0.10 | [CI] | [85.76, 88.10] |
| F1 score ± SD | 87.50 ± 0.08 | [CI] | [87.02, 89.19] |
| Error ± SD | 12.50 ± 0.05 | [CI] | [11.66, 12.88] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohd Noor, N.S.E.; Ibrahim, H.; Lai, C.Q.; Abdullah, J.M. A Long Short-Term Memory Network Using Resting-State Electroencephalogram to Predict Outcomes Following Moderate Traumatic Brain Injury. Computers 2023, 12, 45. https://doi.org/10.3390/computers12020045
Mohd Noor NSE, Ibrahim H, Lai CQ, Abdullah JM. A Long Short-Term Memory Network Using Resting-State Electroencephalogram to Predict Outcomes Following Moderate Traumatic Brain Injury. Computers. 2023; 12(2):45. https://doi.org/10.3390/computers12020045
Chicago/Turabian StyleMohd Noor, Nor Safira Elaina, Haidi Ibrahim, Chi Qin Lai, and Jafri Malin Abdullah. 2023. "A Long Short-Term Memory Network Using Resting-State Electroencephalogram to Predict Outcomes Following Moderate Traumatic Brain Injury" Computers 12, no. 2: 45. https://doi.org/10.3390/computers12020045
APA StyleMohd Noor, N. S. E., Ibrahim, H., Lai, C. Q., & Abdullah, J. M. (2023). A Long Short-Term Memory Network Using Resting-State Electroencephalogram to Predict Outcomes Following Moderate Traumatic Brain Injury. Computers, 12(2), 45. https://doi.org/10.3390/computers12020045







