Exploring the Design for Wearability of Wearable Devices: A Scoping Review
Abstract
:1. Introduction
1.1. Wearable Devices
1.2. Design Perspective
1.3. Research Questions
- What are the key factors influencing the wearability of wearable devices?
- What methodologies and measures are used to assess the wearability of wearable devices?
- What are the reported user experiences and satisfaction levels regarding the wearability of different types of wearable devices?
1.4. Design Considerations
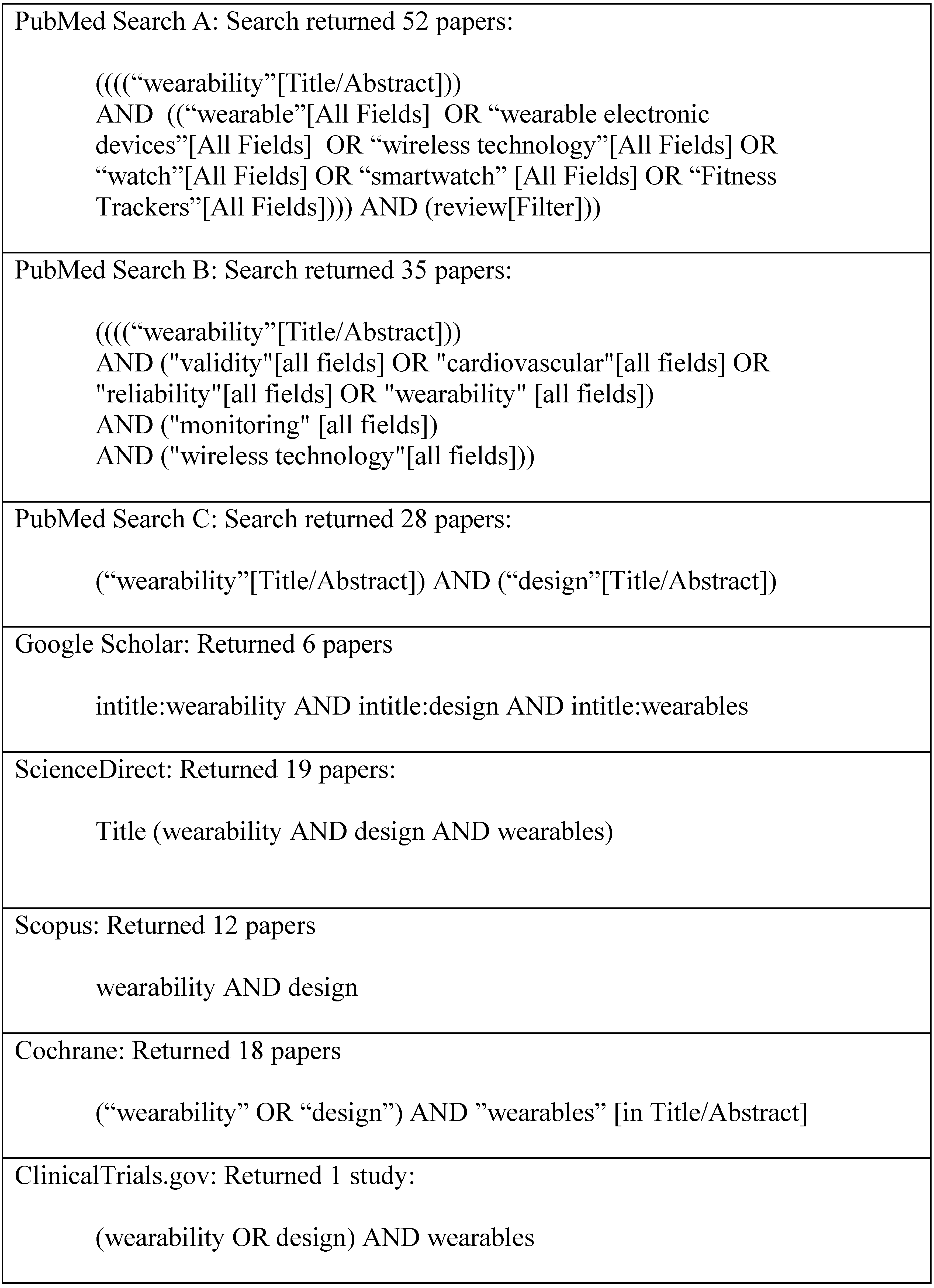
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria and Screening
3. Results
4. Discussion
Limitations
- Despite providing insight into the limited data available to support design for wearability, the sample size for the scoping review was small and the search terms may not have been adequate to tease out design data. The field of digital medicine continues to evolve rapidly, and investigators may use terms in their studies that we did not use in our search.
- Our search was limited to the peer-reviewed literature. It seems reasonable that we are unaware of many usability studies undertaken by technology manufacturers—the clinical trials we reviewed that were sponsored by the industry appeared to be more for the goal of collecting marketing data, not providing design insight.
5. Conclusions
- Lack of Standardized Assessment Methods: The absence of an accepted and standardized method for assessing wearability has resulted in inconsistent evaluations across studies. Researchers often rely on subjective criteria, leading to variability in how wearability is measured and reported.
- Qualitative Nature of Assessments: Most existing assessments of wearability remain qualitative, lacking objective metrics for rigorous analysis. While self-report scales provide valuable insights, they fall short of quantifying wearability in a consistent and comparable manner.
- Limited Utility for Design: Despite the wealth of existing studies, their qualitative nature and lack of quantifiable data hinder their practical utility in designing wearable devices. Insights gleaned from these studies do not directly inform design decisions or address the specific needs of users.
Future Directions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Siegel, C. Wearable and Medical Device Litigation Is on the Rise. Available online: https://www.witlegal.com/insights/blog/wearable-and-medical-device-litigation-is-on-the-rise/ (accessed on 20 March 2024).
- Spatz, E.S.; Ginsburg, G.S.; Rumsfeld, J.S.; Turakhia, M.P. Wearable Digital Health Technologies for Monitoring in Cardiovascular Medicine. N. Engl. J. Med. 2024, 390, 346–356. [Google Scholar] [CrossRef] [PubMed]
- Friend, S.H.; Ginsburg, G.S.; Picard, R.W. Wearable Digital Health Technology. N. Engl. J. Med. 2023, 389, 2100–2101. [Google Scholar] [CrossRef] [PubMed]
- Ginsburg, G.S.; Picard, R.W.; Friend, S.H. Key Issues as Wearable Digital Health Technologies Enter Clinical Care. N. Engl. J. Med. 2024, 390, 1118–1127. [Google Scholar] [CrossRef] [PubMed]
- Varma, N.; Han, J.K.; Passman, R.; Rosman, L.A.; Ghanbari, H.; Noseworthy, P.; Avari Silva, J.N.; Deshmukh, A.; Sanders, P.; Hindricks, G.; et al. Promises and Perils of Consumer Mobile Technologies in Cardiovascular Care: JACC Scientific Statement. J. Am. Coll. Cardiol. 2024, 83, 611–631. [Google Scholar] [CrossRef]
- Velasco, E. How Wearable Sensors Will Transform the Practice of Medicine. Available online: https://magazine.caltech.edu/post/how-wearable-sensors-will-transform-the-practice-of-medicine (accessed on 30 June 2024).
- Xian, X. Frontiers of Wearable Biosensors for Human Health Monitoring. Biosensors 2023, 13, 964. [Google Scholar] [CrossRef]
- Smith, A.A.; Li, R.; Tse, Z.T.H. Reshaping Healthcare with Wearable Biosensors. Sci. Rep. 2023, 13, 4998. [Google Scholar] [CrossRef]
- Lopez, X.; Afrin, K.; Nepal, B. Examining the Design, Manufacturing and Analytics of Smart Wearables. Med. Devices Sens. 2020, 3, e10087. [Google Scholar] [CrossRef]
- Kulkarni, M.B.; Rajagopal, S.; Prieto-Simón, B.; Pogue, B.W. Recent Advances in Smart Wearable Sensors for Continuous Human Health Monitoring. Talanta 2024, 272, 125817. [Google Scholar] [CrossRef]
- Seshadri, D.R.; Li, R.T.; Voos, J.E.; Rowbottom, J.R.; Alfes, C.M.; Zorman, C.A.; Drummond, C.K. Wearable Sensors for Monitoring the Physiological and Biochemical Profile of the Athlete. npj Digit. Med. 2019, 2, 72. [Google Scholar] [CrossRef]
- Seshadri, D.R.; Li, R.T.; Voos, J.E.; Rowbottom, J.R.; Alfes, C.M.; Zorman, C.A.; Drummond, C.K. Wearable Sensors for Monitoring the Internal and External Workload of the Athlete. npj Digit. Med. 2019, 2, 71. [Google Scholar] [CrossRef]
- Vandrico. Wearable Technology Database. Available online: https://vandrico.com/wearables.html (accessed on 15 January 2021).
- Tong, R.K.Y. (Ed.) Wearable Technology in Medicine and Health Care, 1st ed.; Academic Press: London, UK; San Diego, CA, USA, 2018; ISBN 978-0-12-811810-8. [Google Scholar]
- LeMoyne, R.; Mastroianni, T. (Eds.) Wearable and Wireless Systems for Gait Analysis and Reflex Quantification. In Wearable and Wireless Systems for Healthcare I: Gait and Reflex Response Quantification; Springer Nature: Singapore, 2024; pp. 1–19. ISBN 978-981-9724-39-0. [Google Scholar]
- Ferguson, C.; Hickman, L.D.; Turkmani, S.; Breen, P.; Gargiulo, G.; Inglis, S.C. “Wearables Only Work on Patients That Wear Them”: Barriers and Facilitators to the Adoption of Wearable Cardiac Monitoring Technologies. Cardiovasc. Digit. Health J. 2021, 2, 137–147. [Google Scholar] [CrossRef] [PubMed]
- Slater, K. Human Comfort. Available online: https://www.abebooks.com/9780398051280/Human-Comfort-Slater-Keith-0398051283/plp (accessed on 21 February 2024).
- Coravos, A.; Doerr, M.; Goldsack, J.; Manta, C.; Shervey, M.; Woods, B.; Wood, W.A. Modernizing and Designing Evaluation Frameworks for Connected Sensor Technologies in Medicine. Npj Digit. Med. 2020, 3, 37. [Google Scholar] [CrossRef] [PubMed]
- Olaye, I.M.; Belovsky, M.P.; Bataille, L.; Cheng, R.; Ciger, A.; Fortuna, K.L.; Izmailova, E.S.; McCall, D.; Miller, C.J.; Muehlhausen, W.; et al. Recommendations for Defining and Reporting Adherence Measured by Biometric Monitoring Technologies: Systematic Review. J. Med. Internet Res. 2022, 24, e33537. [Google Scholar] [CrossRef] [PubMed]
- Tandon, A.; de Ferranti, S.D. Wearable Biosensors in Pediatric Cardiovascular Disease. Circulation 2019, 140, 350–352. [Google Scholar] [CrossRef]
- Lin, W.-Y.; Ke, H.-L.; Chou, W.-C.; Chang, P.-C.; Tsai, T.-H.; Lee, M.-Y. Realization and Technology Acceptance Test of a Wearable Cardiac Health Monitoring and Early Warning System with Multi-Channel MCGs and ECG. Sensors 2018, 18, 3538. [Google Scholar] [CrossRef]
- Knight, J.F.; Baber, C.; Schwirtz, A.; Bristow, H. The Comfort Assessment of Wearable Computers. In Proceedings of the Sixth International Symposium on Wearable Computers, Seattle, WA, USA, 10 October 2002. [Google Scholar] [CrossRef]
- Francés-Morcillo, L.; Morer-Camo, P.; Rodríguez-Ferradas, M.I.; Cazón-Martín, A. Wearable Design Requirements Identification and Evaluation. Sensors 2020, 20, 2599. [Google Scholar] [CrossRef]
- Ferraro, V.; Ugur, S. Designing Wearable Technologies through a User Centered Approach. In Proceedings of the 2011 Conference on Designing Pleasurable Products and Interfaces, Milano, Italy, 22–25 June 2011; Association for Computing Machinery: New York, NY, USA, 2011; pp. 1–8. [Google Scholar]
- Nuske, H.J.; Goodwin, M.S.; Kushleyeva, Y.; Forsyth, D.; Pennington, J.W.; Masino, A.J.; Finkel, E.; Bhattacharya, A.; Tan, J.; Tai, H.; et al. Evaluating Commercially Available Wireless Cardiovascular Monitors for Measuring and Transmitting Real-Time Physiological Responses in Children with Autism. Autism Res. 2022, 15, 117–130. [Google Scholar] [CrossRef]
- Sana, F.; Isselbacher, E.M.; Singh, J.P.; Heist, E.K.; Pathik, B.; Armoundas, A.A. Wearable Devices for Ambulatory Cardiac Monitoring. J. Am. Coll. Cardiol. 2020, 75, 1582–1592. [Google Scholar] [CrossRef]
- Hochstadt, A.; Chorin, E.; Viskin, S.; Schwartz, A.L.; Lubman, N.; Rosso, R. Continuous Heart Rate Monitoring for Automatic Detection of Atrial Fibrillation with Novel Bio-Sensing Technology. J. Electrocardiol. 2019, 52, 23–27. [Google Scholar] [CrossRef]
- Yock, P. Needs-Based Innovation: The Biodesign Process. BMJ Innov. 2015, 1, 3. [Google Scholar] [CrossRef]
- Fries, R.C. Handbook of Medical Device Design, 1st ed.; CRC Press: New York, NY, USA, 2000; ISBN 978-0-8247-0399-8. [Google Scholar]
- King, P.H.; Fries, R.C.; Johnson, A.T. Design of Biomedical Devices and Systems, 3rd ed.; CRC Press: Boca Raton, FL, USA, 2014; ISBN 978-1-4665-6913-3. [Google Scholar]
- Yock, P.; Zenios, S.; Makower, J.; Brinton, T.J.; Kumar, U.N.; Watkins, F.T.J.; Denend, L.; Krummel, T.; Kurihara, C.Q. BioDesign: The Process of Innovating New Medical Technologies; Cambridge University Press: Cambridge, UK, 2015. [Google Scholar]
- Stuart, S.; de Kok, M.; O’Searcoid, B.; Morrisroe, H.; Serban, I.B.; Jagers, F.; Dulos, R.; Houben, S.; van de Peppel, L.; van den Brand, J. Critical Design Considerations for Longer-Term Wear and Comfort of On-Body Medical Devices. Bioengineering 2024, 11, 1058. [Google Scholar] [CrossRef] [PubMed]
- Luo, X.; Tan, H.; Wen, W. Recent Advances in Wearable Healthcare Devices: From Material to Application. Bioengineering 2024, 11, 358. [Google Scholar] [CrossRef] [PubMed]
- Mouyal, N. New Standards for Wearable Technologies. Available online: https://etech.iec.ch/issue/2021-04/new-standards-for-wearable-technologies (accessed on 19 March 2024).
- Underwriters Laboratory. Keeping Wearable Technology Safe at Any Speed. Available online: https://www.ul.com/insights/keeping-wearable-technology-safe-any-speed (accessed on 21 March 2024).
- de Vries, M.J. Translating Customer Requirements into Technical Specifications. In Philosophy of Technology and Engineering Sciences; Meijers, A., Ed.; Handbook of the Philosophy of Science; North-Holland: Amsterdam, The Netherlands, 2009; pp. 489–512. [Google Scholar]
- Göhler, S.; Husung, S.; Howard, T. The Translation between Functional Requirements and Design Parameters for Robust Design. Procedia CIRP 2016, 43, 106–111. [Google Scholar] [CrossRef]
- Mak, S.; Thomas, A. Steps for Conducting a Scoping Review. J. Grad. Med. Educ. 2022, 14, 565–567. [Google Scholar] [CrossRef]
- Cochrane. Cochrane Database of Systematic Reviews. Available online: https://www.cochranelibrary.com/cdsr/about-cdsr (accessed on 30 June 2024).
- Canali, S.; Schiaffonati, V.; Aliverti, A. Challenges and Recommendations for Wearable Devices in Digital Health: Data Quality, Interoperability, Health Equity, Fairness. PLoS Digit. Health 2022, 1, e0000104. [Google Scholar] [CrossRef]
- Cho, S.; Chang, T.; Yu, T.; Lee, C.H. Smart Electronic Textiles for Wearable Sensing and Display. Biosensors 2022, 12, 222. [Google Scholar] [CrossRef]
- Gemperle, F.; Kasabach, C.; Stivoric, J.; Bauer, M.; Martin, R. Design for Wearability. In Proceedings of the Digest of Papers. Second International Symposium on Wearable Computers (Cat. No.98EX215), Pittsburgh, PA, USA, 19–20 October 1998; pp. 116–122. [Google Scholar]
- Haghi, M.; Danyali, S.; Ayasseh, S.; Wang, J.; Aazami, R.; Deserno, T.M. Wearable Devices in Health Monitoring from the Environmental towards Multiple Domains: A Survey. Sensors 2021, 21, 2130. [Google Scholar] [CrossRef]
- Jamshidi, M.; Park, C.B.; Azhari, F. The Design and Fabrication of a Wearable Lattice-Patterned 3D Sensing Skin. Sens. Actuators A Phys. 2024, 369, 115143. [Google Scholar] [CrossRef]
- Kim, J.; Campbell, A.S.; de Ávila, B.E.-F.; Wang, J. Wearable Biosensors for Healthcare Monitoring. Nat. Biotechnol. 2019, 37, 389–406. [Google Scholar] [CrossRef]
- Lee, R.; James, C.; Edwards, S.; Skinner, G.; Young, J.L.; Snodgrass, S.J. Evidence for the Effectiveness of Feedback from Wearable Inertial Sensors during Work-Related Activities: A Scoping Review. Sensors 2021, 21, 6377. [Google Scholar] [CrossRef]
- Lind, C.M.; Abtahi, F.; Forsman, M. Wearable Motion Capture Devices for the Prevention of Work-Related Musculoskeletal Disorders in Ergonomics—An Overview of Current Applications, Challenges, and Future Opportunities. Sensors 2023, 23, 4259. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.; Liu, L.; Gou, G.; Fang, Z.; Sun, J.; Chen, J.; Cheng, J.; Han, M.; Ma, T.; Liu, C.; et al. Recent Advancements in Physiological, Biochemical, and Multimodal Sensors Based on Flexible Substrates: Strategies, Technologies, and Integrations. ACS Appl. Mater. Interfaces 2023, 15, 21721–21745. [Google Scholar] [CrossRef] [PubMed]
- Shah, M.A.; Pirzada, B.M.; Price, G.; Shibiru, A.L.; Qurashi, A. Applications of Nanotechnology in Smart Textile Industry: A Critical Review. J. Adv. Res. 2022, 38, 55–75. [Google Scholar] [CrossRef] [PubMed]
- Tandon, A.; Cobb, B.R.; Centra, J.; Izmailova, E.; Manyakov, N.V.; McClenahan, S.; Patel, S.; Sezgin, E.; Vairavan, S.; Vrijens, B.; et al. A Systematic Scoping Review of Studies Describing Human Factors, Human-Centered Design, and Usability of Sensor-Based Digital Health Technologies. J Med internet Res 2024. [Google Scholar] [CrossRef]
- Uchitel, J.; Vidal-Rosas, E.E.; Cooper, R.J.; Zhao, H. Wearable, Integrated EEG-fNIRS Technologies: A Review. Sensors 2021, 21, 6106. [Google Scholar] [CrossRef]
- Zhao, H.; Su, R.; Teng, L.; Tian, Q.; Han, F.; Li, H.; Cao, Z.; Xie, R.; Li, G.; Liu, X.; et al. Recent Advances in Flexible and Wearable Sensors for Monitoring Chemical Molecules. Nanoscale 2022, 14, 1653–1669. [Google Scholar] [CrossRef]
- Zhao, L.; Liang, C.; Huang, Y.; Zhou, G.; Xiao, Y.; Ji, N.; Zhang, Y.-T.; Zhao, N. Emerging Sensing and Modeling Technologies for Wearable and Cuffless Blood Pressure Monitoring. npj Digit. Med. 2023, 6, 93. [Google Scholar] [CrossRef]
- Cohen, S.; Waks, Z.; Elm, J.J.; Gordon, M.F.; Grachev, I.D.; Navon-Perry, L.; Fine, S.; Grossman, I.; Papapetropoulos, S.; Savola, J.-M. Characterizing Patient Compliance over Six Months in Remote Digital Trials of Parkinson’s and Huntington Disease. BMC Med. Inform. Decis. Mak. 2018, 18, 138. [Google Scholar] [CrossRef]
- Nasirzadeh, F.; Karmakar, C.; Habib, A.; Benny Neelangal, K.; Mir, M.; Lee, S.; Arnel, T. Continuous Monitoring of Body Temperature for Objective Detection of Health and Safety Risks in Construction Sites: An Analysis of the Accuracy and Comfort of off-the-Shelf Wearable Sensors. Heliyon 2024, 10, e26947. [Google Scholar] [CrossRef]
- Su, M.; Hua, J.; Sun, X.; Liu, Z.; Shi, Y.; Pan, L. Wireless Wearable Devices and Recent Applications in Health Monitoring and Clinical Diagnosis. Biomed. Mater. Devices 2024, 2, 669–694. [Google Scholar] [CrossRef]
- Teng, S.; Kim, J.-Y.; Jeon, S.; Gil, H.-W.; Lyu, J.; Chung, E.H.; Kim, K.S.; Nam, Y. Analyzing Optimal Wearable Motion Sensor Placement for Accurate Classification of Fall Directions. Sensors 2024, 24, 6432. [Google Scholar] [CrossRef] [PubMed]
- Schaefer, S.E.; Van Loan, M.; German, J.B. A Feasibility Study of Wearable Activity Monitors for Pre-Adolescent School-Age Children. Prev. Chronic Dis. 2014, 11, E85. [Google Scholar] [CrossRef] [PubMed]
- Bouwstra, S.; Chen, W.; Feijs, L.M.G.; Bambang Oetomo, S. Smart Jacket Design for Neonatal Monitoring with Wearable Sensors. In Proceedings of the Sixth International Workshop on Wearable and Implantable Body Sensor Networks, Berkeley, CA, USA, 3–5 June 2009; pp. 162–167. [Google Scholar]
- Evans, E.W.; Abrantes, A.M.; Chen, E.; Jelalian, E. Using Novel Technology within a School-Based Setting to Increase Physical Activity: A Pilot Study in School-Age Children from a Low-Income, Urban Community. BioMed Res. Int. 2017, 2017, 4271483. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Tabares, F.J.; Gaviria-Gomez, N.; Castellanos-Dominguez, G. Very Long-Term ECG Monitoring Patch with Improved Functionality and Wearability. In Proceedings of the 2014 36th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Chicago, IL, USA, 26–30 August 2014; Volume 2014, pp. 5964–5967. [Google Scholar] [CrossRef]
- Chandrasekaran, R.; Katthula, V.; Moustakas, E. Patterns of Use and Key Predictors for the Use of Wearable Health Care Devices by US Adults: Insights from a National Survey. J. Med. Internet Res. 2020, 22, e22443. [Google Scholar] [CrossRef] [PubMed]


| User Need | Design Considerations | |
|---|---|---|
| A. | Comfort | Evaluate the comfort of the device when worn for extended periods. This includes assessing the materials used, fit, weight, and overall ergonomic design. |
| B. | Fit and Adjustability | Ensure that the device can fit various body types and sizes. This includes the design of adjustable straps, bands, or other mechanisms to secure the device properly. |
| C. | Battery Life | Assess the duration the device can operate before needing a recharge. Longer battery life is preferable to reduce the frequency of recharging, which can affect wearability and user compliance. |
| D. | Durability and Robustness | The device should withstand daily wear and tear, including exposure to different environmental conditions like moisture, dust, and physical impact. |
| E. | Ease of Use | Evaluate how easy it is for users to operate the device. This includes the simplicity of putting it on and taking it off, as well as the user interface for any necessary interactions. |
| F. | Data Accuracy and Reliability | Assess the precision and consistency of the data collected by the device. Reliable sensors and accurate data collection are crucial for clinical trial validity. |
| G. | Mobility and Range of Motion | Determine how the device affects natural movement and range of motion. Assess whether it restricts movement during various activities. |
| H. | Integration with Clothing and Accessories | Determine how well the device integrates with different types of clothing and accessories. Assess whether it can be worn discreetly or if it interferes with other wearable items. |
| I. | Aesthetic Appeal | Consider the visual design of the device. It should be appealing or at least unobtrusive to encourage regular wear. |
| J. | Skin Compatibility | Ensure that the materials used do not cause skin irritation or allergies. This includes testing for hypoallergenic properties and the breathability of materials in contact with the skin. |
| K. | Connectivity and Data Transfer | Evaluate how the device connects to other systems or devices for data transfer (including the reliability and security of connections). |
| L. | Regulatory Compliance | Ensure that the device meets all the necessary regulatory standards and guidelines for medical devices. This includes certifications and compliance with the relevant health and safety standards. |
| Assessment of User Need | Score |
|---|---|
| Reference does not mention or only briefly mentions, without detail. | 1–2 |
| Reference mentions with some detail. | 3–4 |
| Reference discusses with moderate detail and some context. | 5–6 |
| Reference provides detailed discussion w/ relevant data/examples. | 7–8 |
| Reference extensively provides comprehensive data, examples, and critical analysis. | 9–10 |
| Author | Year | Type | Title | |
|---|---|---|---|---|
| 1. | Canali et al. [40] | 2022 | R | Challenges and recommendations for wearable devices in digital health: Data quality, interoperability, health equity, fairness |
| 2. | Cho et al. [41] | 2022 | R | Smart electronic textiles for wearable sensing and display |
| 3. | Ferguson et al. [16] | 2021 | R | Wearables only work on patients that wear them: Barriers and facilitators to the adoption of wearable cardiac monitoring technologies |
| 4. | Ferraro and Yavuz [24] | 2011 | D | Designing wearable technologies through a user centered approach |
| 5. | Frances-Morcillo et al. [23] | 2020 | D | Wearable design requirements identification and evaluation. |
| 6. | Friend et al. [3] | 2023 | R | Wearable digital health technology. |
| 7. | Ginsburg et al. [4] | 2024 | D | Key Issues as Wearable Digital Health Technologies Enter Clinical Care |
| 8. | Gemperle et al. [42] | 1998 | D | Design for wearability |
| 9. | Haghi et al. [43] | 2021 | R | Wearable Devices in Health Monitoring from the Environmental towards Multiple Domains: A Survey |
| 10. | Jamshidi et al. [44] | 2024 | E | The design and fabrication of a wearable lattice-patterned 3D sensing skin |
| 11. | Kim et al. [45] | 2019 | R | Wearable biosensors for healthcare monitoring |
| 12. | Lee et al. [46] | 2021 | R | Evidence for the Effectiveness of Feedback from Wearable Inertial Sensors during Work-Related Activities: A Scoping Review |
| 13. | Lind et al. [47] | 2023 | D | Wearable Motion Capture Devices for the Prevention of Work-Related Musculoskeletal Disorders in Ergonomics |
| 14. | Liu et al. [48] | 2023 | R | Recent Advancements in Physiological, Biochemical, and Multimodal Sensors Based on Flexible Substances: Strategies, Technologies, and Integrations. |
| 15. | Shah et al. [49] | 2022 | R | Applications of nanotechnology in smart textile industry: A critical review. |
| 16. | Tandon et al. [50] | 2024 | R | A systematic scoping review of studies describing human factors, human-centered design, and usability of sensor-based digital health technologies |
| 17. | Uchitel et al. [51] | 2021 | R | Wearable, integrated EEG-fNIRS technologies: A review |
| 18. | Zhao et al. [52] | 2022 | R | Recent advances in flexible and wearable sensors for monitoring chemical molecules |
| 19. | Zhao et al. [53] | 2023 | D | Emerging sensing and modeling technologies for wearable and cuffless blood pressure monitoring |
| User Need Design Criteria | Average | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Reference | A | B | C | D | E | F | G | H | I | J | K | L | Score | |
| 1. | Canali et al. [40] | 2 | 2 | 1 | 3 | 2 | 4 | 2 | 1 | 2 | 2 | 2 | 1 | 2.0 |
| 2. | Cho et al. [41] | 2 | 2 | 1 | 1 | 5 | 7 | 3 | 1 | 1 | 1 | 3 | 1 | 2.3 |
| 3. | Ferguson et al. [16] | 4 | 4 | 4 | 4 | 8 | 5 | 1 | 3 | 7 | 1 | 3 | 1 | 3.8 |
| 4. | Ferraro and Yavuz [24] | 6 | 6 | 2 | 2 | 6 | 3 | 6 | 5 | 4 | 3 | 2 | 2 | 3.9 |
| 5. | Frances-Morcillo et al. [23] | 7 | 7 | 5 | 8 | 8 | 5 | 5 | 5 | 5 | 3 | 3 | 1 | 5.2 |
| 6. | Friend et al. [3] | 3 | 5 | 5 | 6 | 5 | 7 | 2 | 2 | 2 | 6 | 8 | 7 | 4.8 |
| 7. | Ginsburg et al. [4] | 1 | 1 | 5 | 3 | 7 | 9 | 5 | 3 | 3 | 6 | 9 | 9 | 5.1 |
| 8. | Gemperle et al. [42] | 3 | 8 | 1 | 7 | 1 | 1 | 9 | 2 | 2 | 6 | 1 | 1 | 3.5 |
| 9. | Haghi et al. [43] | 2 | 2 | 8 | 6 | 4 | 9 | 2 | 2 | 2 | 4 | 9 | 4 | 4.5 |
| 10. | Jamshidi et al. [44] | 1 | 1 | 1 | 4 | 4 | 6 | 1 | 1 | 5 | 10 | 5 | 1 | 3.3 |
| 11. | Kim et al. [45] | 2 | 2 | 5 | 4 | 4 | 7 | 4 | 4 | 4 | 10 | 10 | 1 | 4.8 |
| 12. | Lee et al. [46] | 3 | 5 | 5 | 6 | 5 | 6 | 10 | 7 | 2 | 4 | 7 | 1 | 5.1 |
| 13. | Lind et al. [47] | 1 | 3 | 1 | 3 | 1 | 6 | 9 | 9 | 2 | 2 | 3 | 2 | 3.5 |
| 14. | Liu et al. [48] | 2 | 2 | 6 | 6 | 1 | 3 | 1 | 1 | 2 | 6 | 5 | 1 | 3.0 |
| 15. | Shah et al. [49] | 1 | 1 | 4 | 4 | 4 | 4 | 1 | 9 | 6 | 4 | 5 | 1 | 3.7 |
| 16. | Tandon et al. [50] | 5 | 5 | 1 | 1 | 5 | 6 | 5 | 1 | 2 | 2 | 2 | 2 | 3.1 |
| 17. | Uchitel et al. [51] | 2 | 2 | 3 | 5 | 1 | 5 | 1 | 1 | 1 | 6 | 5 | 1 | 2.8 |
| 18. | Zhao et al. [52] | 1 | 2 | 2 | 2 | 1 | 7 | 1 | 1 | 2 | 5 | 5 | 1 | 2.5 |
| 19. | Zhao et al. [53] | 2 | 2 | 2 | 3 | 2 | 4 | 1 | 1 | 1 | 3 | 3 | 1 | 2.1 |
| Assessment | Average Score | Impact |
|---|---|---|
| Minimal value as a data source for design | Under 3 | Low |
| Provides indirect linkage to studies or reviews with data | 3–5 | Medium |
| Recites data that has potential support for device design | Over 5 | High |
| Paper | Author | Scale | Summary Description |
|---|---|---|---|
| 1 | Canali et al. [40] | L | The paper maps out the principles for which wearable devices can be measured and the ethical problems they present. The paper recognized the gap in equity and medical literacy when it comes to wearable devices. Though the paper recognizes and comments on ethical topics/issues, it does not touch on the design and engineering process of them. |
| 2 | Cho et al. [41] | L | The paper focuses on the aspects of the design and use of e-textiles. Though the paper mentions many issues related to the use of textiles for wearable technology, specific links to device design are absent. |
| 3 | Ferguson et al. [16] | M | This paper focuses not only on the developmental and design aspects of wearable technology, but it also addresses the ethical and social barriers that are presented that may hinder the use of them. Cardiac devices are used as an example and design for specific end-users is discussed, such as the elderly. |
| 4 | Ferraro and Yavuz [24] | M | The paper is directed towards designers who are responsible for upcoming wearable technology to consider the human aspects in the design. The paper has a portion focused on the wearability of products and suggests a user-adjustable approach to this issue. The paper also mentions how devices affect human life and what the body “senses” from these new technologies. The paper informs on psychological aspects of rejection reactions that might occur by patients of older age. |
| 5 | Frances-Morcillo et al. [23] | H | The paper is directed towards identifying the design features of the wearability of wearables. The paper includes surveys from experts who are developing wearable technology and presents the results of questionnaires. |
| 6 | Friend et al. [3] | M | The paper focuses on clinical insight that could result from the clinical trials of wearable devices. Although the paper identifies challenges in the field of wearables, no specific data are provided. |
| 7 | Ginsburg et al. [4] | H | The paper successfully mentions the challenges encountered while pursuing the application of wearable technologies to healthcare. It is ranked high due to the inclusion of regulatory issues and the need for design standards. |
| 8 | Gemperle et al. [42] | M | The paper is directed toward identifying specific design considerations that prevail when wearables are used in high-activity scenarios. The paper does not include design data but addresses device detachment during motion. |
| 9 | Haghi et al. [43] | M | The paper highlights the psychological aspect of utilizing wearability and the patient’s responses towards implanting or using or wearing wearables. Although the design specifications are not discussed, the specifications to be considered when applying wearable sensors to clinical settings are presented. |
| 10 | Jamshidi et al. [44] | M | With a focus on the interaction between wearable devices and body location, the paper provides ideas to consider when studying the interaction itself. The paper focuses on the joints and appropriate location of wearables. |
| 11 | Kim et al. [45] | M | The paper provides a comprehensive study of the different types of wearable sensor technology and the nature of the data that can be collected. This is an ideal manuscript to identify wearability relative to sensor data. |
| 12 | Lee et al. [46] | H | The paper highlights the influences of wearability on the biosensor field. Although the paper does not discuss the “design aspects” of wearability directly, it does discuss the guidelines of wearability. They introduce a “Technological and Design Checklist” of wearable inertial sensors and also underline the importance of personalized designs to enhance the wearability experience for patients |
| 13 | Lind et al. [47] | M | The paper highlights human movements in the context of typical work-related musculoskeletal activities. The paper recites issues in current use-case applications, challenges, and detailed future opportunities. The paper is focused on muscular data collection. |
| 14 | Liu et al. [48] | M | The paper is directed towards materials that can enhance the wearability experience of the patient. The paper then focuses highly on the improvements that should be made to utilize the fiber-contained devices to become practical in the field. |
| 15 | Shah et al. [49] | M | The paper focuses on the different smart textiles that can be utilized to enhance the wearability of sensor clothes. Additionally, it categorized different textiles for different usage of clothing sensors such as electrically conductive textiles and energy-storing textiles. |
| 16 | Tandon et al. [50]. | M | The paper offers a comprehensive review of digital health technologies relative to approaches to evaluating sensor wearability, with a special focus on human factors, human-centered design, and usability. Suggestions are included on how to improve the digital health technologies field, but no data are provided. |
| 17 | Uchitel et al. [51] | L | The paper emphasizes the integration of EEG and fNIRS for portable, affordable, and appropriate long-term monitoring. The paper highlights the evaluation of the types of EEG electrodes and amplifiers though only peripherally mentions device design aspects of the technologies. |
| 18 | Zhao et al. [52] | L | The paper emphasizes flexible wearable devices for real-time health monitoring based on small, soft, and low-cost materials. The paper focuses on the wearability of chemical sensors for various biomarkers, commenting on the advantages and disadvantages. |
| 19 | Zhao et al. [53] | L | The paper emphasizes the challenges of monitoring blood pressure and focuses on topics such as flexible sensing, signal collecting and processing, noise reduction, and estimation models for blood pressure extraction. The accuracy of continuous data collection is discussed. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seo, Y.W.; La Marca, V.; Tandon, A.; Chiao, J.-C.; Drummond, C.K. Exploring the Design for Wearability of Wearable Devices: A Scoping Review. Computers 2024, 13, 326. https://doi.org/10.3390/computers13120326
Seo YW, La Marca V, Tandon A, Chiao J-C, Drummond CK. Exploring the Design for Wearability of Wearable Devices: A Scoping Review. Computers. 2024; 13(12):326. https://doi.org/10.3390/computers13120326
Chicago/Turabian StyleSeo, Yeo Weon, Valentina La Marca, Animesh Tandon, Jung-Chih Chiao, and Colin K. Drummond. 2024. "Exploring the Design for Wearability of Wearable Devices: A Scoping Review" Computers 13, no. 12: 326. https://doi.org/10.3390/computers13120326
APA StyleSeo, Y. W., La Marca, V., Tandon, A., Chiao, J.-C., & Drummond, C. K. (2024). Exploring the Design for Wearability of Wearable Devices: A Scoping Review. Computers, 13(12), 326. https://doi.org/10.3390/computers13120326








