The Use of Poly(N-vinyl pyrrolidone) in the Delivery of Drugs: A Review
Abstract
:1. Introduction
2. Different Morphologies as Drug Delivery Systems
2.1. Microparticles and Nanoparticles
2.2. Fibers
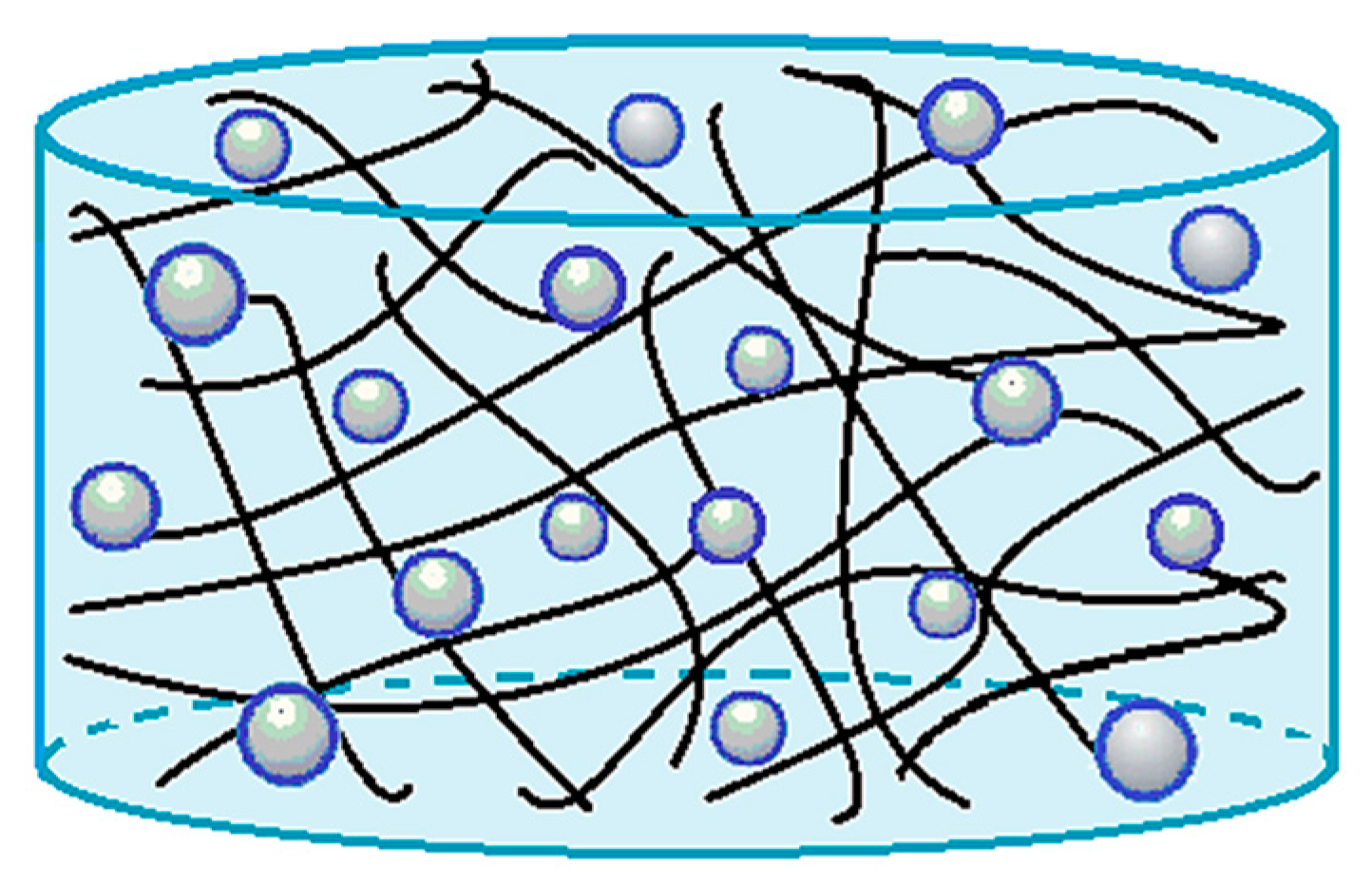
2.3. Hydrogels
2.4. Tablets
2.5. Films
3. Conclusions and Perspectives
Author Contributions
Funding
Conflicts of Interest
References
- Folttmann, H.; Quadir, A. Polyvinylpyrrolidone (PVP)—One of the most widely used excipients in pharmaceuticals: An overview. Drug Deliv. Technol. 2008, 8, 22–27. [Google Scholar]
- Bothiraja, C.; Shinde, M.B.; Rajalakshmi, S.; Pawar, A.P. Evaluation of molecular pharmaceutical and in—Vivo properties of spray—Dried isolated andrographolide—PVP. J. Pharm. Pharmacol. 2009, 61, 1465–1472. [Google Scholar] [CrossRef]
- Martins, R.M.; Pereira, S.V.; Siqueira, S.; Salomão, W.F.; Freitas, L.A.P. Curcuminoid content and antioxidant activity in spray dried microparticles containing turmeric extract. Food Res. Int. 2013, 50, 657–663. [Google Scholar] [CrossRef] [Green Version]
- Rasekh, M.; Karavasili, C.; Soong, Y.L.; Bouropoulos, N.; Morris, M.; Armitage, D.; Li, X.; Fatouros, D.G.; Ahmad, Z. Electrospun PVP–indomethacin constituents for transdermal dressings and drug delivery devices. Int. J. Pharm. 2014, 473, 95–104. [Google Scholar] [CrossRef] [PubMed]
- Fogaça, R.; Catalani, L.H. PVP hydrogel membranes produced by electrospinning for protein release devices. Soft Mater. 2013, 11, 61–68. [Google Scholar] [CrossRef]
- Del Consuelo, I.D.; Falson, F.; Guy, R.H.; Jacques, Y. Ex vivo evaluation of bioadhesive films for buccal delivery of fentanyl. J. Control. Release 2007, 122, 135–140. [Google Scholar] [CrossRef]
- Robinson, B.; Sullivan, F.; Borzelleca, J.; Schwartz, S. PVP: A Critical Review of the Kinetics and Toxicology of Polyvinylpyrrolidone (Povidone); Lewis Publisher: Chelsea, MI, USA, 1990. [Google Scholar]
- Zheng, X.; Zhang, T.; Song, X.; Zhang, L.; Zhang, C.; Jin, S.; Xing, J.; Liang, X.-J. Structural impact of graft and block copolymers based on poly (N-vinylpyrrolidone) and poly (2-dimethylaminoethyl methacrylate) in gene delivery. J. Mater. Chem. B 2015, 3, 4027–4035. [Google Scholar] [CrossRef]
- Zhang, L.; Liang, Y.; Meng, L.; Wang, C. Characterization of complexation of PVP copolymer with DNA. Polym. Adv. Technol. 2009, 20, 410–415. [Google Scholar] [CrossRef]
- Song, Y.; Zhang, T.; Song, X.; Zhang, L.; Zhang, C.; Xing, J.; Liang, X.-J. Polycations with excellent gene transfection ability based on PVP-g-PDMAEMA with random coil and micelle structures as non-viral gene vectors. J. Mater. Chem. B 2015, 3, 911–918. [Google Scholar] [CrossRef]
- Saxena, A.; Mozumdar, S.; Johri, A.K. Ultra-low sized cross-linked polyvinylpyrrolidone nanoparticles as non-viral vectors for in vivo gene delivery. Biomaterials 2006, 27, 5596–5602. [Google Scholar] [CrossRef]
- Sheu, S.-J.; Chou, L.-C.; Bee, Y.-S.; Chen, J.-F.; Lin, H.-C.; Lin, P.-R.; Lam, H.-C.; Tai, M.-H. Suppression of choroidal neovascularization by intramuscular polymer-based gene delivery of vasostatin. Exp. Eye Res. 2005, 81, 673–679. [Google Scholar] [CrossRef] [PubMed]
- Hu, M.; Li, C.; Li, X.; Zhou, M.; Sun, J.; Sheng, F.; Shi, S.; Lu, L. Zinc oxide/silver bimetallic nanoencapsulated in PVP/PCL nanofibres for improved antibacterial activity. Artif. Cells Nanomed. Biotechnol. 2018, 46, 1248–1257. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hecold, M.; Buczkowska, R.; Mucha, A.; Grzesiak, J.; Rac-Rumijowska, O.; Teterycz, H.; Marycz, K. The effect of PEI and PVP-stabilized gold nanoparticles on equine platelets activation: Potential application in equine regenerative medicine. J. Nanomater. 2017, 2017, 8706921. [Google Scholar]
- Goetten de Lima, G.; de Lima, D.W.; de Oliveira, M.J.; Lugão, A.B.; Alcántara, M.S.; Devine, D.M.; de Sá, M.J. Synthesis and in vivo behaviour of PVP/CMC/Agar hydrogel membranes impregnated with silver nanoparticles for wound healing applications. ACS Appl. Bio Mater. 2018, 1, 1842–1852. [Google Scholar] [CrossRef]
- Ramalingam, V.; Varunkumar, K.; Ravikumar, V.; Rajaram, R. Target delivery of doxorubicin tethered with PVP stabilized gold nanoparticles for effective treatment of lung cancer. Sci. Rep. 2018, 8, 1–12. [Google Scholar] [CrossRef]
- Rose, P.A.; Praseetha, P.; Bhagat, M.; Alexander, P.; Abdeen, S.; Chavali, M. Drug embedded PVP coated magnetic nanoparticles for targeted killing of breast cancer cells. Technol. Cancer Res. Treat. 2013, 12, 463–472. [Google Scholar] [CrossRef]
- Gupta, P.; Bansal, A.K. Spray drying for generation of a ternary amorphous system of celecoxib, PVP, and meglumine. Pharm. Dev. Technol. 2005, 10, 273–281. [Google Scholar] [CrossRef]
- Dowding, P.J.; Atkin, R.; Vincent, B.; Bouillot, P. Oil core/polymer shell microcapsules by internal phase separation from emulsion droplets. II: Controlling the release profile of active molecules. Langmuir 2005, 21, 5278–5284. [Google Scholar] [CrossRef]
- Wu, K.; Li, J.; Wang, W.; Winstead, D.A. Formation and characterization of solid dispersions of piroxicam and polyvinylpyrrolidone using spray drying and precipitation with compressed antisolvent. J. Pharm. Sci. 2009, 98, 2422–2431. [Google Scholar] [CrossRef] [PubMed]
- Prosapio, V.; De Marco, I.; Reverchon, E. PVP/corticosteroid microspheres produced by supercritical antisolvent coprecipitation. Chem. Eng. J. 2016, 292, 264–275. [Google Scholar] [CrossRef]
- Yu, D.; Shen, X.; Zhang, X.; Branford-White, C.; Zhu, L. Preparation and characterization of fast-dissolving electrospun drug-loaded nanofiber membrane. Acta Polym. Sinica 2009, 11, 88–92. [Google Scholar]
- Dai, X.-Y.; Nie, W.; Wang, Y.-C.; Shen, Y.; Li, Y.; Gan, S.-J. Electrospun emodin polyvinylpyrrolidone blended nanofibrous membrane: A novel medicated biomaterial for drug delivery and accelerated wound healing. J. Mater. Sci. Mater. 2012, 23, 2709–2716. [Google Scholar] [CrossRef]
- Sriyanti, I.; Edikresnha, D.; Munir, M.M.; Rachmawati, H.; Khairurrijal, K. Electrospun Polyvinylpyrrolidone (PVP) Nanofiber Mats Loaded by Garcinia Mangostana L. Extracts. Mater. Sci. Forum 2017, 880, 11–14. [Google Scholar] [CrossRef]
- Yu, D.G.; Zhang, X.F.; Shen, X.X.; Brandford—White, C.; Zhu, L.M. Ultrafine ibuprofen-loaded polyvinylpyrrolidone fiber mats using electrospinning. Polym. Int. 2009, 58, 1010–1013. [Google Scholar] [CrossRef]
- Mishra, R.K.; Datt, M.; Banthia, A.K. Synthesis and characterization of pectin/PVP hydrogel membranes for drug delivery system. Aaps Pharmscitech 2008, 9, 395–403. [Google Scholar] [CrossRef] [Green Version]
- Rapado Raneque, M.; Rodríguez Rodríguez, A.; Peniche Covas, C. Hydrogel wound dressing preparation at laboratory scale by using electron beam and gamma radiation. Nucleus 2013, 53, 24–31. [Google Scholar]
- Ajji, Z.; Maarouf, M.; Khattab, A.; Ghazal, H. Synthesis of pH-responsive hydrogel based on PVP grafted with crotonic acid for controlled drug delivery. Radiat. Phys. Chem. 2020, 170, 108612. [Google Scholar] [CrossRef]
- Risbud, M.V.; Hardikar, A.A.; Bhat, S.V.; Bhonde, R.R. pH-sensitive freeze-dried chitosan–polyvinyl pyrrolidone hydrogels as controlled release system for antibiotic delivery. J. Control. Release 2000, 68, 23–30. [Google Scholar] [CrossRef]
- Wlodarski, K.; Tajber, L.; Sawicki, W. Physicochemical properties of direct compression tablets with spray dried and ball milled solid dispersions of tadalafil in PVP-VA. Eur. J. Pharm. Biopharm. 2016, 109, 14–23. [Google Scholar] [CrossRef] [PubMed]
- Janugade, B.; Patil, S.; Patil, S.; Lade, P. Effect of PVP concentration on lag time of press-coated Montelukast sodium tablet. J. Pharm. Res. 2009, 2, 502–506. [Google Scholar]
- Karavas, E.; Georgarakis, E.; Bikiaris, D. Application of PVP/HPMC miscible blends with enhanced mucoadhesive properties for adjusting drug release in predictable pulsatile chronotherapeutics. Eur. J. Pharm. Biopharm. 2006, 64, 115–126. [Google Scholar] [CrossRef] [PubMed]
- Perioli, L.; Ambrogi, V.; Angelici, F.; Ricci, M.; Giovagnoli, S.; Capuccella, M.; Rossi, C. Development of mucoadhesive patches for buccal administration of ibuprofen. J. Control. Release 2004, 99, 73–82. [Google Scholar] [CrossRef] [PubMed]
- Mohabe, V.; Akhand, R.; Pathak, A.K. Preparation and evaluation of captopril transdermal patches. Bull. Pharm. Res 2011, 1, 47–52. [Google Scholar]
- Sadashivaiah, R.; Dinesh, B.; Patil, U.A.; Raghu, K. Design and in vitro evaluation of haloperidol lactate transdermal patches containing ethyl cellulose-povidone as film formers. Asian J. Pharm. 2014, 2, 43–49. [Google Scholar]
- Gupta, R.; Mukherjee, B. Development and in vitro evaluation of diltiazem hydrochloride transdermal patches based on povidone–ethylcellulose matrices. Drug Dev. Ind. Pharm. 2003, 29, 1–7. [Google Scholar] [CrossRef]
- Savjani, K.T.; Gajjar, A.K.; Savjani, J.K. Drug solubility: Importance and enhancement techniques. ISRN Pharm 2012, 2012, 195727. [Google Scholar] [CrossRef] [Green Version]
- Paradkar, A.; Ambike, A.A.; Jadhav, B.K.; Mahadik, K. Characterization of curcumin–PVP solid dispersion obtained by spray drying. Int. J. Pharm. 2004, 271, 281–286. [Google Scholar] [CrossRef]
- Thybo, P.; Pedersen, B.L.; Hovgaard, L.; Holm, R.; Müllertz, A. Characterization and physical stability of spray dried solid dispersions of probucol and PVP-K30. Pharm. Dev. Technol. 2008, 13, 375–386. [Google Scholar] [CrossRef]
- Gun, W.J.; Routh, A.F. Formation and characterization of pH-responsive liquid core microcapsules. Langmuir 2013, 29, 12541–12548. [Google Scholar] [CrossRef]
- Chhouk, K.; Kanda, H.; Kawasaki, S.-I.; Goto, M. Micronization of curcumin with biodegradable polymer by supercritical anti-solvent using micro swirl mixer. Front. Chem. Sci. Eng. 2018, 12, 184–193. [Google Scholar] [CrossRef]
- Prosapio, V.; Reverchon, E.; De Marco, I. Incorporation of liposoluble vitamins within PVP microparticles using supercritical antisolvent precipitation. J. CO2 Util. 2017, 19, 230–237. [Google Scholar] [CrossRef]
- Ha, E.-S.; Kim, J.-S.; Baek, I.-H.; Hwang, S.-J.; Kim, M.-S. Enhancement of dissolution and bioavailability of ezetimibe by amorphous solid dispersion nanoparticles fabricated using supercritical antisolvent process. J. Pharm. Invest. 2015, 45, 641–649. [Google Scholar] [CrossRef]
- Majerik, V.; Charbit, G.; Badens, E.; Horváth, G.; Szokonya, L.; Bosc, N.; Teillaud, E. Bioavailability enhancement of an active substance by supercritical antisolvent precipitation. J. Supercrit. Fluids 2007, 40, 101–110. [Google Scholar] [CrossRef]
- Park, J.; Cho, W.; Cha, K.-H.; Ahn, J.; Han, K.; Hwang, S.-J. Solubilization of the poorly water soluble drug, telmisartan, using supercritical anti-solvent (SAS) process. Int. J. Pharm. 2013, 441, 50–55. [Google Scholar] [CrossRef] [PubMed]
- Adami, R.; Di Capua, A.; Reverchon, E. Supercritical Assisted Atomization for the production of curcumin-biopolymer microspheres. Powder Technol. 2017, 305, 455–461. [Google Scholar] [CrossRef]
- Di Capua, A.; Adami, R.; Reverchon, E. Production of luteolin/biopolymer microspheres by supercritical assisted atomization. Ind. Eng. Chem. Res. 2017, 56, 4334–4340. [Google Scholar] [CrossRef]
- Di Capua, A.; Bejarano, A.; Adami, R.; Reverchon, E. Preparation and characterization of Chilean propolis coprecipitates using Supercritical Assisted Atomization. Chem. Eng. Res. Des. 2018, 136, 776–785. [Google Scholar] [CrossRef]
- Di Capua, A.; Adami, R.; Cosenza, E.; Jalaber, V.; Crampon, C.; Badens, E.; Reverchon, E. β-Carotene/PVP microspheres produced by Supercritical Assisted Atomization. Powder Technol. 2019, 346, 228–236. [Google Scholar] [CrossRef]
- Uzun, İ.N.; Sipahigil, O.; Dinçer, S. Coprecipitation of Cefuroxime Axetil–PVP composite microparticles by batch supercritical antisolvent process. J. Supercrit. Fluids 2011, 55, 1059–1069. [Google Scholar] [CrossRef]
- Prosapio, V.; Reverchon, E.; De Marco, I. Formation of PVP/nimesulide microspheres by supercritical antisolvent coprecipitation. J. Supercrit. Fluids 2016, 118, 19–26. [Google Scholar] [CrossRef]
- Prosapio, V.; De Marco, I.; Scognamiglio, M.; Reverchon, E. Folic acid–PVP nanostructured composite microparticles by supercritical antisolvent precipitation. Chem. Eng. J. 2015, 277, 286–294. [Google Scholar] [CrossRef]
- Prosapio, V.; Reverchon, E.; De Marco, I. Coprecipitation of polyvinylpyrrolidone/β-carotene by supercritical antisolvent processing. Ind. Eng. Chem. Res. 2015, 54, 11568–11575. [Google Scholar] [CrossRef]
- Matos, R.L.; Lu, T.; Prosapio, V.; McConville, C.; Leeke, G.; Ingram, A. Coprecipitation of curcumin/PVP with enhanced dissolution properties by the supercritical antisolvent process. J. CO2 Util. 2019, 30, 48–62. [Google Scholar] [CrossRef]
- Franco, P.; Reverchon, E.; De Marco, I. PVP/ketoprofen coprecipitation using supercritical antisolvent process. Powder Technol. 2018, 340, 1–7. [Google Scholar] [CrossRef]
- Ozkan, G.; Franco, P.; Capanoglu, E.; De Marco, I. PVP/flavonoid coprecipitation by supercritical antisolvent process. Chem. Eng. Process. 2019, 146, 107689. [Google Scholar] [CrossRef]
- Nkansah, P.; Antipas, A.; Lu, Y.; Varma, M.; Rotter, C.; Rago, B.; El-Kattan, A.; Taylor, G.; Rubio, M.; Litchfield, J. Development and evaluation of novel solid nanodispersion system for oral delivery of poorly water-soluble drugs. J. Control. Release 2013, 169, 150–161. [Google Scholar] [CrossRef]
- Qin, X.; Guo, Z.; Liu, Z.; Zhang, W.; Wan, M.; Yang, B. Folic acid-conjugated graphene oxide for cancer targeted chemo-photothermal therapy. J. Photochem. Photobiol. B 2013, 120, 156–162. [Google Scholar] [CrossRef]
- Xu, H.; Hou, Z.; Zhang, H.; Kong, H.; Li, X.; Wang, H.; Xie, W. An efficient Trojan delivery of tetrandrine by poly (N-vinylpyrrolidone)-block-poly (ε-caprolactone)(PVP-b-PCL) nanoparticles shows enhanced apoptotic induction of lung cancer cells and inhibition of its migration and invasion. Int. J. Nanomed. 2014, 9, 231. [Google Scholar]
- Paudel, A.; Loyson, Y.; Van den Mooter, G. An investigation into the effect of spray drying temperature and atomizing conditions on miscibility, physical stability, and performance of naproxen–PVP K 25 solid dispersions. J. Pharm. Sci. 2013, 102, 1249–1267. [Google Scholar] [CrossRef]
- Paudel, A.; Van den Mooter, G. Influence of solvent composition on the miscibility and physical stability of naproxen/PVP K 25 solid dispersions prepared by cosolvent spray-drying. Pharm. Res. 2012, 29, 251–270. [Google Scholar] [CrossRef]
- Sairam, M.; Ramesh Babu, V.; Krishna Rao, K.; Aminabhavi, T. Poly (methylmethacrylate)-poly (vinyl pyrrolidone) microspheres as drug delivery systems: Indomethacin/cefadroxil loading and in vitro release study. J. Appl. Pol. Sci. 2007, 104, 1860–1865. [Google Scholar] [CrossRef]
- Cavallari, C.; Luppi, B.; Di Pietra, A.M.; Rodriguez, L.; Fini, A. Enhanced release of indomethacin from PVP/stearic acid microcapsules prepared coupling co-freeze-drying and ultrasound assisted spray-congealing process. Pharm. Res. 2007, 24, 521–529. [Google Scholar] [CrossRef] [PubMed]
- Mennini, N.; Furlanetto, S.; Cirri, M.; Mura, P. Quality by design approach for developing chitosan-Ca-alginate microspheres for colon delivery of celecoxib-hydroxypropyl-β-cyclodextrin-PVP complex. Eur. J. Pharm. Biopharm. 2012, 80, 67–75. [Google Scholar] [CrossRef]
- El-Maradny, H.; Mortada, S.; Kamel, O.; Hikal, A. Characterization of ternary complexes of meloxicam-HPβCD and PVP or L-arginine prepared by the spray-drying technique. Acta Pharm. 2008, 58, 455–466. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Balata, G.; Mahdi, M.; Bakera, R.A. Improvement of solubility and dissolution properties of ketoconazole by solid dispersions and inclusion complexes. Asian J. Pharm. Sci. 2010, 5, 1–12. [Google Scholar]
- Valero, M.; Tejedor, J.; Rodríguez, L.J. Encapsulation of nabumetone by means of-drug:(β-cyclodextrin) 2: Polyvinylpyrrolidone ternary complex formation. J. Lumin. 2007, 126, 297–302. [Google Scholar] [CrossRef]
- Tong, W.; Song, X.; Gao, C. Layer-by-layer assembly of microcapsules and their biomedical applications. Chem. Soc. Rev. 2012, 41, 6103–6124. [Google Scholar] [CrossRef]
- Antipina, M.N.; Kiryukhin, M.V.; Skirtach, A.G.; Sukhorukov, G.B. Micropackaging via layer-by-layer assembly: Microcapsules and microchamber arrays. Int. Mater. Rev. 2014, 59, 224–244. [Google Scholar] [CrossRef]
- Zhang, Y.; Guan, Y.; Yang, S.; Xu, J.; Han, C.C. Fabrication of hollow capsules based on hydrogen bonding. Adv. Mater. 2003, 15, 832–835. [Google Scholar] [CrossRef]
- Kumar, K.A.; Ray, S.B.; Nagaraja, V.; Raichur, A.M. Encapsulation and release of rifampicin using poly (vinyl pyrrolidone)-poly (methacrylic acid) polyelectrolyte capsules. Mat. Sci. Eng. C 2009, 29, 2508–2513. [Google Scholar] [CrossRef]
- Dam, H.H.; Caruso, F. Formation and degradation of layer-by-layer-assembled polyelectrolyte polyrotaxane capsules. Langmuir 2013, 29, 7203–7208. [Google Scholar] [CrossRef]
- Parekh, G.; Pattekari, P.; Joshi, C.; Shutava, T.; DeCoster, M.; Levchenko, T.; Torchilin, V.; Lvov, Y. Layer-by-layer nanoencapsulation of camptothecin with improved activity. Int. J. Pharm. 2014, 465, 218–227. [Google Scholar] [CrossRef] [Green Version]
- Matos, R.L.; Lu, T.; Leeke, G.; Prosapio, V.; McConville, C.; Ingram, A. Single-step coprecipitation and coating to prepare curcumin formulations by supercritical fluid technology. J. Supercrit. Fluids 2020, 159, 104758. [Google Scholar] [CrossRef]
- Park, H.J.; Yoon, T.J.; Kwon, D.E.; Yu, K.; Lee, Y.-W. Coprecipitation of hydrochlorothiazide/PVP for the dissolution rate improvement by precipitation with compressed fluid antisolvent process. J. Supercrit. Fluids 2017, 126, 37–46. [Google Scholar] [CrossRef]
- Zahran, F.; Cabañas, A.; Cheda, J.A.R.; Renuncio, J.A.R.; Pando, C. Dissolution rate enhancement of the anti-inflammatory drug diflunisal by coprecipitation with a biocompatible polymer using carbon dioxide as a supercritical fluid antisolvent. J. Supercrit. Fluids 2014, 88, 56–65. [Google Scholar] [CrossRef]
- Franco, P.; Reverchon, E.; De Marco, I. Zein/diclofenac sodium coprecipitation at micrometric and nanometric range by supercritical antisolvent processing. J. CO2 Util. 2018, 27, 366–373. [Google Scholar] [CrossRef]
- Prosapio, V.; De Marco, I.; Reverchon, E. Supercritical antisolvent coprecipitation mechanisms. J. Supercrit. Fluids 2018, 138, 247–258. [Google Scholar] [CrossRef]
- Xu, W.; Ling, P.; Zhang, T. Polymeric micelles, a promising drug delivery system to enhance bioavailability of poorly water-soluble drugs. J. Drug Deliv. 2013, 2013, 340315. [Google Scholar] [CrossRef]
- Lukyanov, A.N.; Torchilin, V.P. Micelles from lipid derivatives of water-soluble polymers as delivery systems for poorly soluble drugs. Adv. Drug Del. Rev. 2004, 56, 1273–1289. [Google Scholar] [CrossRef]
- Gaucher, G.; Dufresne, M.-H.; Sant, V.P.; Kang, N.; Maysinger, D.; Leroux, J.-C. Block copolymer micelles: Preparation, characterization and application in drug delivery. J. Control. Release 2005, 109, 169–188. [Google Scholar] [CrossRef]
- Benahmed, A.; Ranger, M.; Leroux, J.-C. Novel polymeric micelles based on the amphiphilic diblock copolymer poly (N-vinyl-2-pyrrolidone)-block-poly (D, L-lactide). Pharm. Res. 2001, 18, 323–328. [Google Scholar] [CrossRef] [PubMed]
- Kuskov, A.N.; Voskresenskaya, A.A.; Goryachaya, A.V.; Artyukhov, A.A.; Shtilman, M.I.; Tsatsakis, A.M. Preparation and characterization of amphiphilic poly-N-vinylpyrrolidone nanoparticles containing indomethacin. J. Mater. Sci. Mater. 2010, 21, 1521–1530. [Google Scholar] [CrossRef]
- Kuskov, A.; Villemson, A.; Shtilman, M.; Larionova, N.; Tsatsakis, A.; Tsikalas, I.; Rizos, A. Amphiphilic poly-N-vinylpyrrolidone nanocarriers with incorporated model proteins. J. Phys. 2007, 19, 205139. [Google Scholar] [CrossRef]
- Luss, A.L.; Kulikov, P.P.; Romme, S.B.; Andersen, C.L.; Pennisi, C.P.; Docea, A.O.; Kuskov, A.N.; Velonia, K.; Mezhuev, Y.O.; Shtilman, M.I. Nanosized carriers based on amphiphilic poly-N-vinyl-2-pyrrolidone for intranuclear drug delivery. Nanomedicine 2018, 13, 703–715. [Google Scholar] [CrossRef] [Green Version]
- Le Garrec, D.; Taillefer, J.; Van Lier, J.; Lenaerts, V.; Leroux, J.-C. Optimizing pH-responsive polymeric micelles for drug delivery in a cancer photodynamic therapy model. J. Drug Target. 2002, 10, 429–437. [Google Scholar] [CrossRef]
- Fournier, E.; Dufresne, M.-H.; Smith, D.C.; Ranger, M.; Leroux, J.-C. A novel one-step drug-loading procedure for water-soluble amphiphilic nanocarriers. Pharm. Res. 2004, 21, 962–968. [Google Scholar] [CrossRef]
- Luo, L.; Ranger, M.; Lessard, D.G.; Le Garrec, D.; Gori, S.; Leroux, J.-C.; Rimmer, S.; Smith, D. Novel amphiphilic diblock copolymer of low molecular weight poly (n-vinylpyrrolidone)-b lock-poly (d, l-lactide): Synthesis, characterization, and micellization. Macromolecules 2004, 37, 4008–4013. [Google Scholar] [CrossRef]
- Quan, J.; Yu, Y.; Branford-White, C.; Williams, G.R.; Yu, D.-G.; Nie, W.; Zhu, L.-M. Preparation of ultrafine fast-dissolving feruloyl-oleyl-glycerol-loaded polyvinylpyrrolidone fiber mats via electrospinning. Colloids Surf. B 2011, 88, 304–309. [Google Scholar] [CrossRef]
- Suwantong, O.; Pankongadisak, P.; Deachathai, S.; Supaphol, P. Electrospun poly (L-lactic acid) fiber mats containing crude Garcinia mangostana extracts for use as wound dressings. Polym. Bull. 2014, 71, 925–949. [Google Scholar] [CrossRef]
- Shen, X.; Yu, D.; Zhu, L.; Branford-White, C.; White, K.; Chatterton, N.P. Electrospun diclofenac sodium loaded Eudragit® L 100-55 nanofibers for colon-targeted drug delivery. Int. J. Pharm. 2011, 408, 200–207. [Google Scholar] [CrossRef]
- Yoshimoto, H.; Shin, Y.; Terai, H.; Vacanti, J. A biodegradable nanofiber scaffold by electrospinning and its potential for bone tissue engineering. Biomaterials 2003, 24, 2077–2082. [Google Scholar] [CrossRef]
- Theron, S.; Zussman, E.; Yarin, A. Experimental investigation of the governing parameters in the electrospinning of polymer solutions. Polymer 2004, 45, 2017–2030. [Google Scholar] [CrossRef]
- Chen, Y.Z.; Peng, P.; Guo, Z.X.; Yu, J.; Zhan, M.S. Effect of hyperbranched poly (ester amine) additive on electrospinning of low concentration poly (methyl methacrylate) solutions. J. Appl. Pol. Sci. 2010, 115, 3687–3696. [Google Scholar] [CrossRef]
- Wang, L.; Chang, M.-W.; Ahmad, Z.; Zheng, H.; Li, J.-S. Mass and controlled fabrication of aligned PVP fibers for matrix type antibiotic drug delivery systems. Chem. Eng. J. 2017, 307, 661–669. [Google Scholar] [CrossRef]
- Jiang, Y.-N.; Mo, H.-Y.; Yu, D.-G. Electrospun drug-loaded core–sheath PVP/zein nanofibers for biphasic drug release. Int. J. Pharm. 2012, 438, 232–239. [Google Scholar] [CrossRef]
- Saheb, D.N.; Jog, J.P. Natural fiber polymer composites: A review. Adv. Polyme. Technol. 1999, 18, 351–363. [Google Scholar] [CrossRef]
- Satturwar, P.M.; Fulzele, S.V.; Dorle, A.K. Evaluation of polymerized rosin for the formulation and development of transdermal drug delivery system: A technical note. AAPS PharmSciTech 2005, 6, E649–E654. [Google Scholar] [CrossRef] [Green Version]
- Román-Doval, R.; Tellez-Cruz, M.; Rojas-Chávez, H.; Cruz-Martínez, H.; Carrasco-Torres, G.; Vásquez-Garzón, V. Enhancing electrospun scaffolds of PVP with polypyrrole/iodine for tissue engineering of skin regeneration by coating via a plasma process. J. Mater. Sci. 2019, 54, 3342–3353. [Google Scholar] [CrossRef]
- He, P.; Zhong, Q.; Ge, Y.; Guo, Z.; Tian, J.; Zhou, Y.; Ding, S.; Li, H.; Zhou, C. Dual drug loaded coaxial electrospun PLGA/PVP fiber for guided tissue regeneration under control of infection. Mat. Sci. Eng. C 2018, 90, 549–556. [Google Scholar] [CrossRef]
- Suganya, S.; Senthil Ram, T.; Lakshmi, B.; Giridev, V. Herbal drug incorporated antibacterial nanofibrous mat fabricated by electrospinning: An excellent matrix for wound dressings. J. Appl. Pol. Sci. 2011, 121, 2893–2899. [Google Scholar] [CrossRef]
- Nie, W.; Yu, D.; Branford-White, C.; Shen, X.; Zhu, L. Electrospun zein–PVP fibre composite and its potential medical application. Mater. Res. Innov. 2012, 16, 14–18. [Google Scholar] [CrossRef]
- Lee, H.; Xu, G.; Kharaghani, D.; Nishino, M.; Song, K.H.; Lee, J.S.; Kim, I.S. Electrospun tri-layered zein/PVP-GO/zein nanofiber mats for providing biphasic drug release profiles. Int. J. Pharm. 2017, 531, 101–107. [Google Scholar] [CrossRef]
- Sun, B.; Duan, B.; Yuan, X. Preparation of core/shell PVP/PLA ultrafine fibers by coaxial electrospinning. J. Appl. Pol. Sci. 2006, 102, 39–45. [Google Scholar] [CrossRef]
- Xu, J.; Jiao, Y.; Shao, X.; Zhou, C. Controlled dual release of hydrophobic and hydrophilic drugs from electrospun poly (l-lactic acid) fiber mats loaded with chitosan microspheres. Mater. Lett. 2011, 65, 2800–2803. [Google Scholar] [CrossRef]
- Samprasit, W.; Akkaramongkolporn, P.; Ngawhirunpat, T.; Rojanarata, T.; Kaomongkolgit, R.; Opanasopit, P. Fast releasing oral electrospun PVP/CD nanofiber mats of taste-masked meloxicam. Int. J. Pharm. 2015, 487, 213–222. [Google Scholar] [CrossRef]
- Yao, C.; Li, X.; Song, T. Electrospinning and cross-linking of zein nanofiber mats. J. Appl. Pol. Sci. 2007, 103, 380–385. [Google Scholar] [CrossRef]
- Miyoshi, T.; Toyohara, K.; Minematsu, H. Preparation of ultrafine fibrous zein membranes via electrospinning. Polym. Int. 2005, 54, 1187–1190. [Google Scholar] [CrossRef]
- Jiang, Q.; Reddy, N.; Yang, Y. Cytocompatible cross-linking of electrospun zein fibers for the development of water-stable tissue engineering scaffolds. Acta Biomater. 2010, 6, 4042–4051. [Google Scholar] [CrossRef] [Green Version]
- Torres-Giner, S.; Ocio, M.J.; Lagaron, J.M. Novel antimicrobial ultrathin structures of zein/chitosan blends obtained by electrospinning. Carbohydr. Polym. 2009, 77, 261–266. [Google Scholar] [CrossRef]
- Yao, C.; Li, X.; Song, T. Fabrication of zein/hyaluronic acid fibrous membranes by electrospinning. J. Biomater. Sci. Polyme. Ed. 2007, 18, 731–742. [Google Scholar] [CrossRef]
- Kim, G.-M.; Le, K.H.T.; Giannitelli, S.M.; Lee, Y.J.; Rainer, A.; Trombetta, M. Electrospinning of PCL/PVP blends for tissue engineering scaffolds. J. Mater. Sci. 2013, 24, 1425–1442. [Google Scholar] [CrossRef]
- Shadamarshan, R.P.; Balaji, H.; Rao, H.S.; Balagangadharan, K.; Chandran, S.V.; Selvamurugan, N. Fabrication of PCL/PVP electrospun fibers loaded with trans-anethole for bone regeneration in vitro. Colloids Surf. B 2018, 171, 698–706. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Chen, M.; Diao, G. Electrospinning β-cyclodextrin/poly (vinyl alcohol) nanofibrous membrane for molecular capture. Carbohydr. Polym. 2011, 86, 1410–1416. [Google Scholar] [CrossRef]
- Uyar, T.; Havelund, R.; Nur, Y.; Hacaloglu, J.; Besenbacher, F.; Kingshott, P. Molecular filters based on cyclodextrin functionalized electrospun fibers. J. Membr. Sci. 2009, 332, 129–137. [Google Scholar] [CrossRef]
- Bai, J.; Yang, Q.; Li, M.; Zhang, C.; Yiaoxian, L. Synthesis of poly (N-vinylpyrrolidone)/β-cyclodextrin composite nanofibers using electrospinning techniques. J. Mater. Process. Technol. 2008, 208, 251–254. [Google Scholar] [CrossRef]
- Hoffman, A.S. Hydrogels for biomedical applications. Adv. Drug Del. Rev. 2012, 64, 18–23. [Google Scholar] [CrossRef]
- Ghasemiyeh, P.; Mohammadi-Samani, S. Hydrogels as Drug Delivery Systems; Pros and Cons. Trends Pharm. Sci. 2019, 5, 7–24. [Google Scholar]
- Rosiak, J.M.; Yoshii, F. Hydrogels and their medical applications. Nucl. Instrum. Methods Phys. Res. Sect. B 1999, 151, 56–64. [Google Scholar] [CrossRef]
- Peppas, N. Devices based on intelligent biopolymers for oral protein delivery. Int. J. Pharm. 2004, 277, 11–17. [Google Scholar] [CrossRef]
- Mozalewska, W.; Czechowska-Biskup, R.; Olejnik, A.K.; Wach, R.A.; Ulański, P.; Rosiak, J.M. Chitosan-containing hydrogel wound dressings prepared by radiation technique. Radiat. Phys. Chem. 2017, 134, 1–7. [Google Scholar] [CrossRef]
- Szafulera, K.; Wach, R.A.; Olejnik, A.K.; Rosiak, J.M.; Ulański, P. Radiation synthesis of biocompatible hydrogels of dextran methacrylate. Radiat. Phys. Chem. 2018, 142, 115–120. [Google Scholar] [CrossRef]
- Rosiak, J.; Rucinska-Rybus, A.; Pekala, W. Method of Manufacturing Hydrogel Dressings. 4,871,490, 3 October 1989. [Google Scholar]
- Lopérgolo, L.C.; Lugao, A.B.; Catalani, L.H. Direct UV photocrosslinking of poly (N-vinyl-2-pyrrolidone)(PVP) to produce hydrogels. Polymer 2003, 44, 6217–6222. [Google Scholar] [CrossRef] [Green Version]
- Barros, J.A.G.; Fechine, G.J.M.; Alcantara, M.R.; Catalani, L.H. Poly (N-vinyl-2-pyrrolidone) hydrogels produced by Fenton reaction. Polymer 2006, 47, 8414–8419. [Google Scholar] [CrossRef]
- Fechine, G.; Barros, J.; Catalani, L. Poly (N-vinyl-2-pyrrolidone) hydrogel production by ultraviolet radiation: New methodologies to accelerate crosslinking. Polymer 2004, 45, 4705–4709. [Google Scholar] [CrossRef]
- Bueno, V.B.; Cuccovia, I.M.; Chaimovich, H.; Catalani, L.H. PVP superabsorbent nanogels. Colloid Polym. Sci. 2009, 287, 705–713. [Google Scholar] [CrossRef]
- Siegel, R.A.; Falamarzian, M.; Firestone, B.A.; Moxley, B.C. pH-controlled release from hydrophobic/polyelectrolyte copolymer hydrogels. J. Control. Release 1988, 8, 179–182. [Google Scholar] [CrossRef]
- Patel, V.R.; Amiji, M.M. Preparation and characterization of freeze-dried chitosan-poly (ethylene oxide) hydrogels for site-specific antibiotic delivery in the stomach. Pharm. Res. 1996, 13, 588–593. [Google Scholar] [CrossRef]
- Husain, M.S.B.; Gupta, A.; Alashwal, B.Y.; Sharma, S. Synthesis of PVA/PVP based hydrogel for biomedical applications: A review. Energy Sources Part A 2018, 40, 2388–2393. [Google Scholar] [CrossRef]
- Shah, R.; Saha, N.; Saha, P. Influence of temperature, pH and simulated biological solutions on swelling and structural properties of biomineralized (CaCO 3) PVP–CMC hydrogel. Prog. Biomater. 2015, 4, 123–136. [Google Scholar] [CrossRef] [Green Version]
- Thomas, J.; Gomes, K.; Lowman, A.; Marcolongo, M. The effect of dehydration history on PVA/PVP hydrogels for nucleus pulposus replacement. J. Biomed. Mater. Res. Part B 2004, 69, 135–140. [Google Scholar] [CrossRef]
- Nokhodchi, A.; Raja, S.; Patel, P.; Asare-Addo, K. The role of oral controlled release matrix tablets in drug delivery systems. BioImpacts BI 2012, 2, 175. [Google Scholar] [PubMed] [Green Version]
- Khokhar, P.; Shukla, V. Formulation and evaluation of fast dissolving tablets of diclofenac sodium using pvp. Int. J. Pharma Res. Rev. 2014, 7, 12–19. [Google Scholar]
- Banchero, M.; Manna, L.; Ronchetti, S.; Campanelli, P.; Ferri, A. Supercritical solvent impregnation of piroxicam on PVP at various polymer molecular weights. J. Supercrit. Fluids 2009, 49, 271–278. [Google Scholar] [CrossRef]
- Yakubu, R.; Peh, K.K.; Tan, Y.T. Design of a 24-hour controlled porosity osmotic pump system containing PVP: Formulation variables. Drug Dev. Ind. Pharm. 2009, 35, 1430–1438. [Google Scholar] [CrossRef] [PubMed]
- Nakagawa, T.; Kondo, S.-I.; Sasai, Y.; Kuzuya, M. Preparation of floating drug delivery system by plasma technique. Chem. Pharm. Bull. 2006, 54, 514–518. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Okwuosa, T.C.; Stefaniak, D.; Arafat, B.; Isreb, A.; Wan, K.-W.; Alhnan, M.A. A lower temperature FDM 3D printing for the manufacture of patient-specific immediate release tablets. Pharm. Res. 2016, 33, 2704–2712. [Google Scholar] [CrossRef] [PubMed]
- Kempin, W.; Domsta, V.; Grathoff, G.; Brecht, I.; Semmling, B.; Tillmann, S.; Weitschies, W.; Seidlitz, A. Immediate release 3D-printed tablets produced via fused deposition modeling of a thermo-sensitive drug. Pharm. Res. 2018, 35, 124. [Google Scholar] [CrossRef]
- Skowyra, J.; Pietrzak, K.; Alhnan, M.A. Fabrication of extended-release patient-tailored prednisolone tablets via fused deposition modelling (FDM) 3D printing. Eur. J. Pharm. Sci. 2015, 68, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Goyanes, A.; Buanz, A.B.; Basit, A.W.; Gaisford, S. Fused-filament 3D printing (3DP) for fabrication of tablets. Int. J. Pharm. 2014, 476, 88–92. [Google Scholar] [CrossRef]
- Goyanes, A.; Buanz, A.B.; Hatton, G.B.; Gaisford, S.; Basit, A.W. 3D printing of modified-release aminosalicylate (4-ASA and 5-ASA) tablets. Eur. J. Pharm. Biopharm. 2015, 89, 157–162. [Google Scholar] [CrossRef]
- Goyanes, A.; Chang, H.; Sedough, D.; Hatton, G.B.; Wang, J.; Buanz, A.; Gaisford, S.; Basit, A.W. Fabrication of controlled-release budesonide tablets via desktop (FDM) 3D printing. Int. J. Pharm. 2015, 496, 414–420. [Google Scholar] [CrossRef] [PubMed]
- Siepmann, F.; Eckart, K.; Maschke, A.; Kolter, K.; Siepmann, J. Modeling drug release from PVAc/PVP matrix tablets. J. Control. Release 2010, 141, 216–222. [Google Scholar] [CrossRef] [PubMed]
- Karki, S.; Kim, H.; Na, S.-J.; Shin, D.; Jo, K.; Lee, J. Thin films as an emerging platform for drug delivery. Aasian J. Pharm. Sci. 2016, 11, 559–574. [Google Scholar] [CrossRef] [Green Version]
- Mandeep, K.; Rana, A.; Nimrata, S. Fast Dissolving Films: An Innovative Drug Delivery System. Int. J. Pharm. Res. Allied Sci. 2013, 2, 14–24. [Google Scholar]
- Abha, D.; Sheeja, K.; Bhagyashri, J. Design and evaluation of buccal film of diclofenac sodium. Int. J. Pharm. Bio. Sci. 2011, 1, 17–30. [Google Scholar]
- Rao, P.R.; Diwan, P.V. Formulation and in vitro evaluation of polymeric films of diltiazem hydrochloride and indomethacin for transdermal administration. Drug Dev. Ind. Pharm. 1998, 24, 327–336. [Google Scholar] [CrossRef]
- El-Nabarawi, M.A.; Shaker, D.S.; Attia, D.A.; Hamed, S.A. In vitro skin permeation and biological evaluation of lornoxicam monolithic transdermal patches. Int. J. Pharm. Pharm. Sci. 2013, 5, 242–248. [Google Scholar]
- Bhavya, B.; Shivakumar, H.; Bhat, V. In-Vitro drug release behavior of PVP/Guar Gum polymer blend transdermal film with Diclofenac Potassium. Asian J. Pharm. Clin. Res. 2012, 5, 149–152. [Google Scholar]




| Technique | Polymeric Carrier | Active Compound | Results | Reference |
|---|---|---|---|---|
| Spray drying | PVP | Andrographolide | MPs with m.s. in the range 2.8–3.6 µm | [2] |
| PVP/meglumine | Celecobix | slightly rough MPs with m.s. in the range 3–5 µm | [18] | |
| PVP | Curcuma Extract | rough spherical MPs | [3] | |
| PVP | Curcumin | collapsed MPs | [38] | |
| PVP | Naproxen | no SEM images reported | [60] | |
| PVP | Probucol | collapsed MPs with m.s. in the range 7.4–9.0 µm | [39] | |
| PVP/HP-β-CD | meloxicam | collapsed and slightly coalescent MPs (m.s. 2.52 µm) | [65] | |
| Freeze-drying + ultrasound assisted spray-congealing | PVP/stearic acid | Indomethacin | crystals for freeze-dried PVP/drug; rough MCs PVP/stearic acid/drug | [63] |
| Coacervation | PVP or PVP/polystyrene | 2-propylpyridine, 4-nitroanisole, acridine, Sudan 2 and Sudan 3 | no SEM images reported | [19] |
| PVP | 4-nitroanisole and methylene blue | pH responsive MCs | [40] | |
| Dispersion Polymerization | PVP/PMMA | Cefadroxil and indomethacin | spherical drug-loaded PMMA microspheres coated with PVP | [62] |
| Layer-by-layer method | PVP/MPR with and without a PAA/PAH bilayer | - | hollow MCs (m.s. of PVP/MPR MCs about 440 nm) | [70] |
| Layer-by-layer method | PVP/PMA | Rifampicin | eight-layered MCs (size about 4 µm) | [71] |
| SAA process | PVP | Curcumin | collapsed SMPs and MPs with m.s. in the range 0.54–0.76 | [46] |
| PVP | Luteolin | collapsed SMPs with m.s. in the range 0.22–0.33 μm | [47] | |
| PVP | Propolis | SMPs with m.s. in the range 0.23–0.50 µm | [48] | |
| PVP | β-carotene | MPs and SMPs with m.s. in the range 0.28–0.84 μm | [49] | |
| spray drying or SAS process | PVP | Piroxicam | SAS MPs (0.1–5.0 µm); spray dried MPs (0.3–8.0 µm) | [20] |
| SAS process | PVP | Cefuroxime axetil | both coalescent and well-separated MPs (m.s. in the range 1.88–3.97 µm) | [50] |
| PVP | Curcumin | NPs and SMPs with m.s. in the range 0.03–0.34 µm | [41] | |
| PVP | Dexamethasone, prednisolone and budesonide | Dexamethasone MPs (m.s. 1.82–2.51 µm), prednisolone MPs (m.s. 1.96–3.03 µm) and budesonide MPs (m.s. 3.06–3.58 µm) | [21] | |
| PVP | Nimesulide | aggregates or MPs (m.s. 1.67–4.04 µm) | [51] | |
| PVP | α-tocopherol and menadione | α-tocopherol MPs (m.s. 1.80–4.08 µm) and menadione MPs (m.s. 2.64–5.09 µm) | [42] | |
| PVP | Folic Acid | SMPs and MPs with m.s. in the range 0.30–3.80 µm | [52] | |
| PVP | β-carotene | NPs (0.25 µm) with high molecular weight PVP (PVP K30); MPs (0.81–2.43 µm) with low molecular weight PVP (PVP K17) | [53] | |
| PVP | Curcumin | aggregates, NPs or SMPs with m.s. in the range 0.05–0.33 µm | [54] | |
| PVP and MCC, starch or lactose | Curcumin | irregular particles/crystals of MCC (size: 175 µm), starch (size: 15 µm) or lactose (size <5 µm) coated with PVP/curcumin particles | [74] | |
| PVP | Ketoprofen | MPs with m.s. ranging from 2.41 to 3.81 μm | [55] | |
| PVP | Quercetin and rutin | Quercetin MPs in the range 0.47–9.52 μm and rutin MPs in the range 0.84–8.17 μm | [56] | |
| PVP | Ezetimibe | NPs with m.s. 0.21–0.23 µm | [43] | |
| PVP | Oxeglitazar | Crystals | [44] | |
| PVP | Hydrochlorothiazide | NPs in the range 0.05–0.21 µm | [75] | |
| PVP | Telmisartan | SMPs and MPs with m.s. 0.38–0.60 µm | [45] | |
| PVP | Diflunisal | coalescent NPs and coalescent MPs (size in the range 0.4–8.1 µm) | [76] | |
| Co-grinding | PVP/HP-β-CD into chitosan/CaCl2/alginate | Celecoxib | MPs | [64] |
| PVP | Ingliforib, Furosemide and Celecoxib | stable colloidal particles (m.s. < 370 nm) | [57] | |
| Wet chemical method | PVP | Epirubicin hydrochloride (and iron oxide) | PVP coated NPs with m.s. in the range 60–113 nm | [17] |
| Free-radical polymerization, solvent evaporation | Amphiphilic PVP | Proteins | Drug-loaded PMs (size: 50–80 nm) | [84] |
| Free-radical polymerization, solvent evaporation | Amphiphilic PVP | Indomethacin | Drug-loaded PMs (m.s. < 200 nm) | [83] |
| Ring-opening polymerization, freeze-drying | PVP-b-PDLLA diblock copolymers | Paclitaxel docetaxel | Drug-loaded PMs (size: 20–60 nm) | [87] |
| Ring-opening polymerization, freeze-drying | PVP-b-PDLLA diblock copolymers | Indomethacin | Drug-loaded PMs (size: 40–100 nm) | [82] |
| Emulsification or ultrasonic dispersion | Amphiphilic PVP | Curcumin | Drug-loaded PMs (size < 100 nm with dispersion; size: 200–300 nm with the emulsion) | [85] |
| Dynamic stirring, quenching | PVP | Doxorubicin (and gold) | NPs (m.s. about 14 nm) | [16] |
| Technique | Polymeric Carrier | Active Compound | Results | Reference |
|---|---|---|---|---|
| Electrospinning | PVP | Indomethacin | - complete drug release in about 50 min - easy deposition of FBs onto usual existing dressings | [4] |
| PVP | Emodin | - complete drug release after 120 min - accelerated wound healing in 15 days | [23] | |
| PVP | Garcinia Mangostana L. extracts | complete extracts dissolution in 100 min | [24] | |
| PVP | Ibuprofen | improvement in the disintegration properties | [25] | |
| PVP | Feruloyl-oleyl-glycerol | improvement in the disintegration properties | [89] | |
| PVP | Tetracycline hydrochloride | - well-aligned FBs (both as single layer and multilayer) - complete release of antibiotic in 50 min | [95] | |
| zein/PVP blend | Ketoprofen | complete drug dissolution from 2.5 to 6 h | [102] | |
| PVP/PLLA blend | Benzoin | sustained benzoin release | [105] | |
| PVP/PCL blend | Tecomella undulata extract | - prolonged release up to 24 h - good bactericidal activity | [101] | |
| PVP/PCL blend | Trans-anethole | - sustained drug release - promotion of osteoblast differentiation for bone regeneration | [113] | |
| PVP/PCL blend | - | - FBs loaded with ZnO/Ag nanoparticles - improved antimicrobial activity | [13] | |
| PVP/HP-β-CD or PVP/β-CD blends | Meloxicam | - improved fibers stability against moisture - improvement in the disintegration properties - complete drug release after 60 min - good masking taste | [106] | |
| PVP coated with PPy/I | - | - improved viability and adhesion of cells - fast wound healing | [99] | |
| Coaxial electrospinning | core: zein shell: PVP | Ketoprofen | biphasic drug release: an initial burst (42%) followed by a sustained drug release | [96] |
| core: PVP shell: PLGA | core: naringin shell: metronidazole | dual release system: a short-term release of metronidazole, a long-term release of naringin | [100] | |
| core: PVP shell: PLA | - | - core/shell FBs - no drug incorporated | [104] | |
| Sequential electrospinning | top/bottom layers: zein middle layer: PVP blended with GO | Ketoprofen | - trilayer FBs - biphasic drug release: an initial burst (60%) from PVP layer in 1 h, followed by a sustained release in 15 h | [103] |
| Technique | Polymeric Carrier | Active Compound | Results | Reference |
|---|---|---|---|---|
| Casting | PVP/pectin | Salicylic acid | slightly faster drug release at slightly basic pH | [26] |
| Crosslinking by electron beam and gamma radiation | PVP/PEG PVP/Laponite | - | - high water uptake, improved elasticity and mechanical properties by adding Laponite - no active principle was loaded | [27] |
| Grafting by gamma irradiation | PVP grafted with CA | Ketoprofen | targeted release: a low drug release at acid pH compared to neutral/slightly basic pH | [28] |
| Casting, followed by freeze-drying or air-drying | PVP/chitosan | Amoxicillin | the best drug release achieved in an acid environment | [29] |
| Electrospinning, followed by crosslinking with UV-C radiation and Fenton reaction | PVP | BSA or collagenase | - high porosity of HGs - improvement in the protein dissolution rate | [5] |
| Gamma irradiation | PVP/PEG/ agar/CMC | - | - HGs loaded with silver nanoparticles - high antimicrobial activity - accelerated wound healing | [15] |
| Solution casting, followed by liquid diffusion technique | Biomineralized (CaCO3) PVP/CMC | - | - HGs responded to different stimuli: pH and temperature and simulated biological solutions | [131] |
| Technique | Polymeric Carrier | Active Compound | Results | Reference |
|---|---|---|---|---|
| Spray-drying or ball-milling followed by compression | PVP-VAc | Tadalafil | improved drug dissolution with TBs based on both spray-dried and ball-milled dispersions | [30] |
| Direct compression | PVP with CC, HPMC, lactose and mannitol | Diclofenac sodium | - good disintegration properties - increase in drug dissolution - the best formulation contained PVP/CC 2/1 w/w | [134] |
| core: direct compression coating: wet granulation | core: MCC/CC coating: PVP/EC/HPC | Montelukast sodium | the lag time in the release profiles was affected by the PVP content | [31] |
| core: wet granulation followed by compression coating: dip or spray coating | core: PVP/dextrose/MCC coating: PVP/TEC/cellulose acetate | Ketoprofen | PVP K30 was suitable to reach a 24 h drug release | [136] |
| Both for core and coating: solvent evaporation followed by compression | core: PVP coating: PVP/HPMC | Felodipine | drug release profiles with a delay time | [32] |
| Double compression | coating PVP/ERL/NaHCO3 | 5-fluorouracil | PVP/ERL/NaHCO3 68/17/15 w/w/w was the best formulation in terms of floating, mechanical strength, and drug release | [137] |
| Direct compression | PVP/PVAc | Diprophylline | a drug release model was proposed to facilitate the development of TBs in terms of time and costs | [144] |
| Supercritical impregnation followed by compression | PVP | Piroxicam | the best release profiles with PVP K15/piroxicam TBs containing less than 13% of drug | [135] |
| 3D printing | PVP | Dipyridamole or theophylline | - good mechanical and disintegration properties - acceptable in-batch variability | [138] |
| 3D printing | PVP | Pantoprazole sodium | PVP TBs allowed a faster drug release compared to other polymers (PEG, poloxamer 407) | [139] |
| Technique | Polymeric Carrier | Active Compound | Results | Reference |
|---|---|---|---|---|
| Solution casting | PVP | Fentanyl | - good mucoadhesion property - improvement in drug dissolution | [6] |
| PVP/NaCMC PVP/HPMC | Ibuprofen | higher performance of PVP films compared to Eudragits films | [33] | |
| PVP/PVA | Diclofenac sodium | PVP increased the swelling, but it reduced the strength and the elasticity of films | [147] | |
| PVP/HPMC PVP/EC | Captopril | EC/PVP 3/1 w/v with 5% of DBP (plasticizer and permeation enhancer) was indicated as the best formulation in terms of drug release, but no release kinetics was shown | [34] | |
| PVP/EC | Haloperidol lactate | improvement in the drug release | [35] | |
| PVP/EC | Diltiazem hydrochloride | - PVP/EC 1/2 w/w was one of the best formulations for a sustained drug release | [36] | |
| PVP/EC | Diltiazem hydrochloride and indomethacin | - improvement in the drug dissolution and its skin permeation - the release rate was independent of the film thickness - EC/PVP 4/1 w/w was the best formulation for a controlled drug release | [148] | |
| PVP/EC PVP/ERS100 PVP/ERSPM | Lornoxicam | - improvement in the drug dissolution and its skin permeation - the best patch consisted of PVP/EC 1.6/1 w/w + 10% of oleic acid as a plasticizer | [149] | |
| PVP/rosin | Diltiazem hydrochloride | improvement in the drug dissolution and its skin permeation | [98] | |
| PVP/guar gum | Diclofenac potassium | improvement in the drug release rate | [150] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Franco, P.; De Marco, I. The Use of Poly(N-vinyl pyrrolidone) in the Delivery of Drugs: A Review. Polymers 2020, 12, 1114. https://doi.org/10.3390/polym12051114
Franco P, De Marco I. The Use of Poly(N-vinyl pyrrolidone) in the Delivery of Drugs: A Review. Polymers. 2020; 12(5):1114. https://doi.org/10.3390/polym12051114
Chicago/Turabian StyleFranco, Paola, and Iolanda De Marco. 2020. "The Use of Poly(N-vinyl pyrrolidone) in the Delivery of Drugs: A Review" Polymers 12, no. 5: 1114. https://doi.org/10.3390/polym12051114
APA StyleFranco, P., & De Marco, I. (2020). The Use of Poly(N-vinyl pyrrolidone) in the Delivery of Drugs: A Review. Polymers, 12(5), 1114. https://doi.org/10.3390/polym12051114







