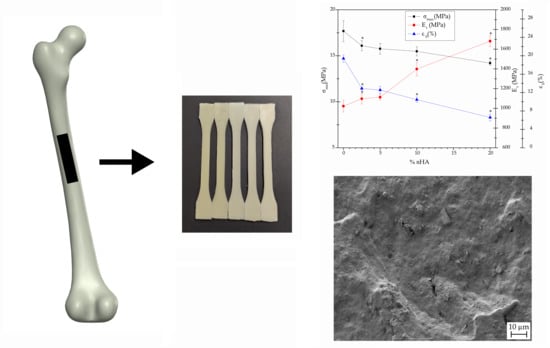
3.1. Mechanical Characterization of the P(3HB-co-3HHx)/nHA Parts
The data collected for the mechanical properties from the tensile, flexural, hardness, and impact Charpy tests of the neat P(3HB-
co-3HHx) and P(3HB-
co-3HHx)/nHA composite parts produced with the different compositions is summarized in
Table 3.
Figure 1 and
Figure 2 display the effect of nHA incorporation on the tensile and flexural properties, respectively, whereas
Table 4 shows the correlation coefficient (
rs) and
p for each mechanical property according to the Spearman’s test.
The tensile properties of the injection-molded P(3HB-
co-3HHx) parts were relatively similar to those reported by Giubilini et al. [
40], although the here-prepared materials were slightly less mechanically resistant and more ductile. These differences could be related to the 3HHx monomer content in the copolyester as well as to differences in processing. One can observe in both
Table 3 and
Figure 1 that the values of σ
max and ε
b decreased, while those of E
t increased with increasing nHA concentration in the nanocomposite parts. The Spearman’s test confirmed the existence of a trend between the tensile properties of the nanocomposites and the nHA content, showing a negative
rs trend (inversely proportional correlation) for σ
max and ε
b and a positive trend (directly proportional correlation) for E
t, while in all cases
p < 0.05. In particular, the addition of 20 wt % of nHA produced a slight decrease of σ
max from 17.7 to 14.4 MPa, but an increase of nearly 64% in E
t (from approximately 1 to 1.7 GPa) accompanied with a significant loss of ductility (ε
b was reduced from 19.4 to 6.5%). The reduction in stress was probably caused by the poor interface adhesion between biopolymer and nanofiller. Higher interfacial adhesion can probably be promoted through the pretreatment of nHA with silanes [
41], but it could negatively affect the biocompatibility of the parts. The increase in E
t was anticipated, since nHA forms highly rigid structures. Furthermore, as it will be discussed during the thermal characterization, the addition of nHA could promote higher degrees of crystallinity and, hence, higher stiffness. Although similar results have been reported earlier [
42,
43], the here-prepared parts showed higher ductility due to the use of a more flexible PHA. The decrease observed in stiffness with increasing nHA content can be attributed to insufficient wetting and impregnation of the nanoparticles by the polymer matrix, mainly due to particle agglomeration during manufacture or processing of the materials [
44]. However, melt-mixing methodologies using co-rotating twin-screw extruders, as adopted here, can generally yield well-dispersed nanocomposites [
45]. Ductility loss was expected since the presence of nHA can prompt polymer crystallinity, hindering chain mobility due to adsorption of biopolymer chains on the surface of the nanoparticles [
46,
47].
In
Figure 2, it can be seen that the addition of nHA to P(3HB-
co-3HHx) increased both σ
f and E
f, particularly the latter. The former increased up to a content of 5 wt % of nHA and then became insensitive to higher nanoparticle contents, since the values showed no significant differences. Indeed, the Spearman’s test showed a positive correlation (
rs > 0) for both E
f and σ
f, however, for the latter, the statistical hypothesis should be rejected as p was higher than 0.05. Contrarily, the addition of 20 wt % of nHA caused an increase of approximately 60% of E
f, as similarly observed above for E
t. The resultant increase in mechanical strength can be related to the intrinsic high values of compressive strength and modulus of nHA, which are in the ranges of 500–1000 MPa and 80–110 GPa, respectively [
48,
49].
In comparison with the mechanical values of other degradable and non-degradable materials, the P(3HB-
co-3HHx)/nHA parts produced in this study showed intermediate values to most biodegradable polymers and metal alloys. For instance, the E
t values of poly(ε-caprolactone) (PCL) and PLA materials range between 400–600 MPa [
50] and 2−3 GPa [
51,
52], respectively, while other biodegradable copolyesters such as poly(butylene adipate-
co-terephthalate) (PBAT) show significantly lower values [
53]. However, PLA is a brittle polymer, which can limit its application in bone fixation devices, or any other biomedical device that would be subjected to local flexural stress or impacts. The values attained are relatively similar to those of poly(lactic-
co-glycolic acid) (PLGA), that is, 1.4−2.8 GPa [
54]. Indeed, PLGA is widely used in biomedical and pharmaceutical applications, but it shows longer degradation times, which can extend up to 12 months [
55]. Regarding metal alloys, the E
t values of the most widely used stainless steels for implant fixing devices and screws, that is, SUS316L stainless steel and cobalt-chrome (Co-Cr) alloys, are around 180 GPa and 210 GPa, respectively [
56]. Lower values have been reported for titanium (Ti) and its light alloys, such as Ti-6Al-4V ELI, which are also widely used for making implant devices, having a value of around 110 GPa [
57]. As shown above, in comparison to metal alloys, the elasticity of the P(3HB-
co-3HHx)/nHA composites prepared in this study is nearer to that of the natural bone, which is in the 8–25 GPa range [
5]. Thus, from a mechanical point of view, their use in bone scaffolds and resorbable plates or screws looks promising.
As expected, hardness increased with the presence of nHA that, due to its ceramic nature, is highly rigid. The increase was significant at nHA contents higher than 2.5 wt % and this effect was statistically corroborated by Spearman’s test, showing a positive trend with an
rs value of ~0.98. In addition, molecular mobility could be reduced due to the presence of the nanoparticles [
58]. In particular, the incorporation of 20 wt % of nHA yielded an increase of 8% in hardness. A similar increase in Shore D hardness was reported by Ferri et al. [
39] for PLA after the incorporation of nHA. In particular, it increased from 73.9, for neat PLA, up to 78.4, for the PLA composite containing 30 wt % of nHA. As also anticipated, the impact strength of the nanocomposites diminished significantly with increasing nHA content with significant differences between the samples, which was confirmed by the negative correlation obtained by the Spearman’s test (
rs ≃ −0.84). For instance, the nanocomposite parts containing 20 wt % of nHA revealed an impact strength approximately three times lower than that of the neat P(3HB-
co-3HHx) part, that is, it reduced from 5.1 to 1.7 kJ/m
2. Lower values of impact strength were reported for V-notched injection-molded pieces of PLA, that is, 2.1 kJ/m
2 [
51]. In addition, significantly higher values have been described for Ti-6Al-4V, with a Rockwell hardness C (HRC) of 38 and approximately 112 kJ/m
2 impact strength [
59]. In the case of natural bone, toughness varies widely with age and type. For instance, the impact strength of the femora ranges from 4 to 70 kJ/m
2 [
60]. Therefore, the various mechanicals tests revealed a clear tendency towards a decrease in ductility and an increase in stiffness of the injection-molded parts with increasing nHA content, which are closer to those of the natural bone.
In summary, the here-developed P(3HB-co-3HHx)/nHA parts showed an improvement of the stiffness determined in terms of Et and Ef, in which a positive trend was observed in both cases (rs > 0). The ductile properties, that is, εb and impact strength, showed negative trends (rs < 0), which was ascribed to a chain mobility reduction that also contributed to a hardness increase of the nanocomposite, showing a positive trend in the Spearman’s test.
3.2. Thermal Characterization of the P(3HB-co-3HHx)/nHA Parts
Figure 3 displays the DSC curves for the neat P(3HB-
co-3HHx) part and the P(3HB-
co-3HHx)/nHA composite parts with different nanoparticle contents.
Table 5 presents the thermal properties obtained from the second heating scan, after erasing the thermal history of the sample. At approximately 0 °C, one could observe a step change in the base lines, which corresponded to the glass transition temperature (T
g) of P(3HB-
co-3HHx). This second-order thermal transition was located at −0.3 °C for the neat biopolymer and it was significantly unaffected by the presence of nHA. The exothermic peaks located between 40 and 70 °C corresponded to the cold crystallization temperature (T
cc) of P(3HB-
co-3HHx). In the case of the neat biopolymer part, this peak was located at 49.8 °C. It could be observed that the values of T
cc increased with increasing nHA content until 10 wt %, and then slightly decreased at the highest content tested, that is, 20 wt %. These results suggested that low nHA contents impaired the movement of P(3HB-
co-3HHx) chains and, hence, hindered the crystallization process. A similar thermal behavior during the analysis of the second heating curves was recently observed by Senatov et al. [
61], who associated the presence of nHA to a decrease in the molecular chain mobility of the biopolymer that impeded the crystallization process. Finally, the crystalline P(3HB-
co-3HHx) domains melted in the thermal range from 100 to 150 °C in two peaks. Furthermore, the occurrence of a broad melting region suggested the presence of heterogeneous crystallites with different degrees of perfection, commonly produced in PHAs with relatively high comonomer contents [
62]. The thermogram of neat P(3HB-
co-3HHx) revealed two melting temperatures (T
m1 and T
m2) at approximately 113 and 140 °C. Similar thermal properties were reported by Zhou et al. [
63] for P(3HB-
co-3HHx) with 11 mol % content of 3HHx, who also observed a double-melting peak phenomenon in the DSC heating curves of this copolyester. The presence of two melting peaks have been previously ascribed to the melting–recrystallization–melting process of P(3HB-
co-3HHx) [
64]. During this process, imperfect crystals melt at lower temperatures and the amorphous regions order into packed spherulites with thicker lamellar thicknesses that, thereafter, melt at higher temperatures. Alternatively, the melting peaks attained at low temperatures, that is, 110–115 °C, could also relate to the crystalline phase of the 3HHx-rich fractions. Lastly, one could observe that the melting profile of P(3HB-
co-3HHx) was nearly unaffected by the nHA presence, indicating that the nanoparticles did not significantly influence the crystallization process.
In addition to the characteristic values of T
g, T
cc, and T
m, the enthalpies corresponding to the cold crystallization (ΔH
cc) and melting (ΔH
m) enthalpies were collected from the DSC curves. The latter parameter was used to determine the maximum degree of crystallinity, that is,
XC_max, which gives more information about the effect of the additives on the biopolymer, since it does not consider the crystals formed during cold crystallization. It can be seen that P(3HB-
co-3HHx) showed a maximum degree of crystallinity of 21.4%. One can also observe that crystallinity varied significantly with nHA content. In particular, as nHA was gradually incorporated in higher percentages, the crystallinity increased steadily up to a maximum of nearly 29% at 5 wt % of nHA and then it slightly decreased to values close to 25% for nHA contents of 10 and 20 wt %. This result, in combination with the slightly higher T
cc and T
m values, suggests that the nanoparticles hindered the formation of crystals at low temperatures, but the crystals formed were slightly more perfect and more mass crystallized. This is in agreement with previous studies that concluded that the introduction of nHA into biopolyesters has an effect on the ordering of their molecular chains by acting as a nucleating agent [
61,
65].
Figure 4 presents the thermogravimetric data for all the materials, while
Table 6 gathers the main thermal stability parameters obtained from the TGA curves. Thermal degradation of P(3HB-
co-3HHx) was observed to occur through a one-step process, which is in agreement with the values reported by Li et al. [
20], who showed that the thermal stability of the microbial copolyester was as high as 225 °C with almost no mass loss. The temperature at 5% mass loss (T
5%) showed no significant differences with nHA contents of up to 5 wt %, but a significant decrease was observed for higher loadings. The temperature at which the maximum mass loss rate occurred (T
deg) increased from 296.7 °C, for the neat P(3HB-
co-3HHx) part, to 300.9 °C, for the part of P(3HB-
co-3HHx) filled with 2.5 %wt of nHA. This increase in thermal stability has been previously ascribed to the formation of strong hydrogen interactions and Van der Walls forces between the inorganic nanoparticles and the biopolymer chains during the melt-mixing process [
66]. The values of T
deg remained nearly constant, showing no significant differences for nHA contents from 2.5 to 10 wt %, but it significantly decreased to 295.6 °C in the part filled with 20 wt % of nHA. The onset of degradation was also reduced for the most filled sample, showing a T
5% value of 254.8 °C, which represents a reduction of approximately 18 °C in comparison to the unfilled P(3HB-
co-3HHx) sample and its nanocomposites at low contents. These results further indicate that the nanoparticles formed aggregates at high contents, which created volumetric gradients of concentration [
66]. In this regard, Bikiaris et al. [
65] suggested that when high amounts of nanosized filler aggregates are formed, the structure shifts from nanocomposite to microcomposite and, thus, the shielding effect of the nanosized particles is lessened. In addition, Chen et al. [
67] reported that high loadings of nHA in PHBV lower the onset degradation temperature since they can catalyze thermal decomposition. In any case, low nHA loadings (<10 wt %) slightly improved the thermal stability of P(3HB-
co-3HHx) parts and their thermal stability is considered to be high enough for bone tissue engineering and biomedical applications, which can require thermal sterilization methods such as dry heat sterilization (160 °C for 2 h) and steam sterilization (121 °C for 20–60 min) [
68]. However, the relatively low T
m of P(3HB-
co-3HHx) would limit the use of these techniques for sterilization and the resultant implantable biomedical devices should be sterilized at low temperatures using ethylene oxide (EO) gas, gamma radiation or ozone. Finally, it can be observed that the residual mass at 700 °C increased gradually with the nHA content due to the high thermal stability of the mineral nanoparticles.
3.3. Thermomechanical Characterization of the P(3HB-co-3HHx)/nHA Parts
DMTA was carried out on the injection-molded composite parts in order to understand the role played by nHA on the viscoelastic behavior of P(3HB-
co-3HHx)/nHA.
Figure 5 illustrates the DMTA curves of the neat P(3HB-
co-3HHx) part and the P(3HB-
co-3HHx)/nHA composite parts with different nanoparticle contents.
Figure 5a gathers the evolution of the storage moduli (E’) in the temperature sweep from −40 to 80 °C at a frequency of 1 Hz. The T
g values and the corresponding values of E’ at −40, 37, and 70 °C are presented in
Table 7, since the first and last temperatures are representative of the stored elastic energy of the amorphous phase of P(3HB-
co-3HHx) in its glassy and rubber states, respectively, whereas the middle one corresponds to the actual temperature of the human body. It can be observed that all the P(3HB-
co-3HHx)-based parts presented a similar thermomechanical profile. In particular, the samples showed high E’ values, that is, high stiffness, at temperatures below 0 °C and then E’ sharply decreased. This thermomechanical change was produced because the temperature exceeded the alpha (α)-relaxation of the biopolymer, which is related to its T
g. One can also observe that the rate of decrease of E’ reduced somewhat when the temperature reached approximately 40 °C due to the occurrence of cold crystallization. The values of E’ at −40, 37, and 70 °C of the neat P(3HB-
co-3HHx) part were 1909.9, 519.2, and 210.5 MPa, respectively. The E’ value attained at 37 °C was in accordance with the mechanical data presented in
Section 3.1, which indicated that only the P(3HB-
co-3HHx) parts filled with the highest nHA contents, that is, 15 and 20 wt %, showed significantly higher values. However, the results also indicated that the parts crystallized during the ageing process since the thermomechanical changes during and after cold crystallization were relatively low. As expected, the E’ values progressively increased with increasing the nHA content, given the high stiffness of the nanoparticles. It is worth noting that the reinforcing effect was more noticeable at higher temperatures since the amorphous phase of P(3HB-
co-3HHx) was in the rubber state. Indeed, at higher temperatures, the thermomechanical response of all the P(3HB-
co-3HHx) composite parts was significantly different, dependent upon the nHA content. For instance, at −40 °C the E’ value increased from 1935.2 MPa for the nanocomposite part containing 2.5 wt % of nHA, to 2100.4 MPa for the part filled with 20 wt % of nHA, whereas these values increased from 212.3 MPa to 333.1 MPa at 70 °C.
The loss tangent or dynamic damping factor (
tan δ) curves are shown in
Figure 5b. Since the position of the
tan δ peak gives an indication of the biopolymer’s T
g, these values were also included in
Table 7. In the case of the neat P(3HB-
co-3HHx) part, the
tan δ peak was located at 10.7 °C, which is similar to that reported by Valentini et al. [
69]. It is worth mentioning that, in all cases, the
tan δ peaks were approximately 10 °C higher than the T
g values. Since
tan δ represents the ratio of the viscous to the elastic response of a viscoelastic material, this indicates that part of the applied load was dissipated by energy dissipation mechanisms such as segmental motions, which are related to T
g, but part of the energy was also stored and released upon removal of the load at higher temperatures. One can observe that the incorporation of nHA shifted slightly the position of the
tan δ peaks and also reduced their intensity for the highest nHA loadings, that is, 10 and 20 wt %. Decreasing
tan δ peaks intensity indicated that the nanocomposite parts showed a more elastic response and, hence, presented more potential to store the applied load rather than dissipating it [
70]. This reduction is directly related to the higher E’ values attained due to nanoparticle reinforcement and it confirmed that nHA imposed restrictions on the molecular motion of the P(3HB-
co-3HHx) chains, resulting in a material with more elastic behavior [
71]. It also correlated well with the DSC results shown above, indicating that P(3HB-
co-3HHx) developed more crystallinity in the nanocomposite parts due to the nucleating effect of nHA and, thus, the less amorphous phase underwent glass transition.
The effect of temperature on the dimensional stability of the P(3HB-
co-3HHx)/nHA parts was also determined by TMA. The coefficient of linear thermal expansion (CLTE), both below and above T
g, was obtained from the change in dimensions versus temperature and it is also included in
Table 7 along with the T
g values. In all cases, lower CLTE values were attained in the parts below T
g, due to the lower mobility of the P(3HB-
co-3HHx) chains of the amorphous regions in the glassy state. As anticipated, both below and above T
g, the CLTE values decreased significantly with increasing nHA content due to the increasing replacement of the soft biopolymer matrix by a ceramic material with a considerably lower CLTE value, that is, 13.6 μm/m·°C [
72]. As a result, the CLTE value below T
g was reduced from 64.3 μm/m·°C for the neat P(3HB-
co-3HHx) part, to 56.7 μm/m·°C for the nanocomposite part filled with 20 wt % of nHA. Similarly, above T
g, it decreased from 177.2 to 159.1 μm/m·°C, respectively. This thermomechanical response was slightly better than that of the PLA/nHA composites, in which the CLTE values below T
g decreased from 73 to 71 μm/m·°C after the incorporation of 20 wt % of nHA into PLA μm/m·°C [
73]. These results point out that the nanocomposite parts prepared herein show excellent dimensional stability against temperature exposition. However, it is also worth mentioning that, as expected, the CLTE of Ti-based materials was significantly lower, having a mean value of 8.7 μm/m·°C [
72].
3.4. Morphological Characterization of the P(3HB-co-3HHx)/nHA Parts
Figure 6 shows the samples before and after the various processing steps. Combining melt compounding and injection molding represents a cost-competitive melt-processing methodology to produce a large number of parts using nanocomposites. According to this route, the P(3HB-
co-3HHx) pellets and the nHA powder were pre-mixed and fed together to the co-rotating twin-screw extruder. In this way, pellets of nanocomposites containing different contents of dispersed nHA particles were obtained. They were subsequently injection molded into dumbbell bars. All parts were defect-free and had a bright surface, the nHA content influencing their color; neat P(3HB-
co-3HHx) parts were yellow pale, typical of microbial PHA, while the presence of nanoparticles induced a whiter color.
Figure 7 shows the FESEM image, taken at 10,000×, of the nHA powder. The nanoparticles show a flake-like morphology based on plates with sizes 60–120 nm and mean cross-sections of approximately 30 nm. This particular morphology of nHA has been reported to occur at pH values below 9, due to the solution environment changes by the OH
− ions during synthesis using polyethylene glycol (PEG) as a template [
74].
Micrographs obtained by FESEM of the fracture surfaces of the injection-molded parts of P(3HB-
co-3HHx) and the various P(3HB-
co-3HHx)/nHA composites after the Charpy impact tests are gathered in
Figure 8. The fracture surface of the neat P(3HB-
co-3HHx) part, shown in
Figure 8a, indicated that the material presented a relatively high toughness, since it yielded a rough surface with the presence of multiple microcracks and some holes. Some microparticles could be seen in the inset FESEM micrograph taken at higher magnification, which could be related to the presence of nucleating agents and/or fillers added by the manufacturer, such as boron nitride (BN). In this regard, Türkez, et al. [
75] have recently demonstrated that BN nanoparticles show slight cytotoxicity potential. In particular, contents below 100 mg/L did not lead to lethal response on human primary alveolar epithelial cells (HPAEpiC), suggesting their safe and effective use in both pharmacological and medical applications.
Figure 8b–e gather the fracture surfaces of the P(3HB-
co-3HHx)/nHA composite parts. The morphological characteristics of the fracture surfaces for the nanocomposites filled with low nHA contents, that is, 2.5 and 5 wt %, remained very similar to that of neat P(3HB-
co-3HHx)/nHA. In all cases, the nanoparticles were relatively well dispersed and distributed within the biopolymer matrix. However, at higher contents, the nanoparticles tended to form some microaggreagates and the resultant fracture surfaces were smoother, indicating that the nanocomposites were more brittle.
Due to the low nHA particle size and the presence of BN and/or additives in the P(3HB-
co-3HHx) matrix, selective separation was carried out on the fracture surfaces of the nanocomposite parts, in order to better evaluate the dispersion of the nanoparticles.
Figure 9 presents the FESEM images of the fracture surfaces subjected to treatment with 6 M HCl for 12 h. The voids and holes formed in the surfaces were related to removed/dissolved nHA and the overall void size and distribution gave an indication of the original particle dispersion. The micrographs revealed that some microholes were produced after the selective attack on the P(3HB-
co-3HHx) parts filled with 10 and 20 wt % of nHA, which should correspond to nHA aggregates, whereas the nanocomposites containing low nanoparticle loadings showed nano-sized holes well distributed along the biopolymer matrix, which suggested an efficient dispersion. Agglomeration was particularly noticeable for the nanocomposite part containing 20 wt % of nHA, thus indicating that the presence of aggregates could induce particle debonding during fracture, as a result of the dissimilar mechanical strength and rigidity of the ceramic nanoparticles and biopolymer matrix. Therefore, the present results correlate well with the mechanical and thermal properties described above, in which nHA loadings of up to 10 wt % increased the mechanical and thermal performance of the P(3HB-
co-3HHx) parts, whereas the highest nHA content impaired the overall properties due to nanoparticle aggregation.