Shrinkage Stress and Temperature Variation in Resin Composites Cured via Different Photoactivation Methods: Insights for Standardisation of the Photopolymerisation
Abstract
:1. Introduction
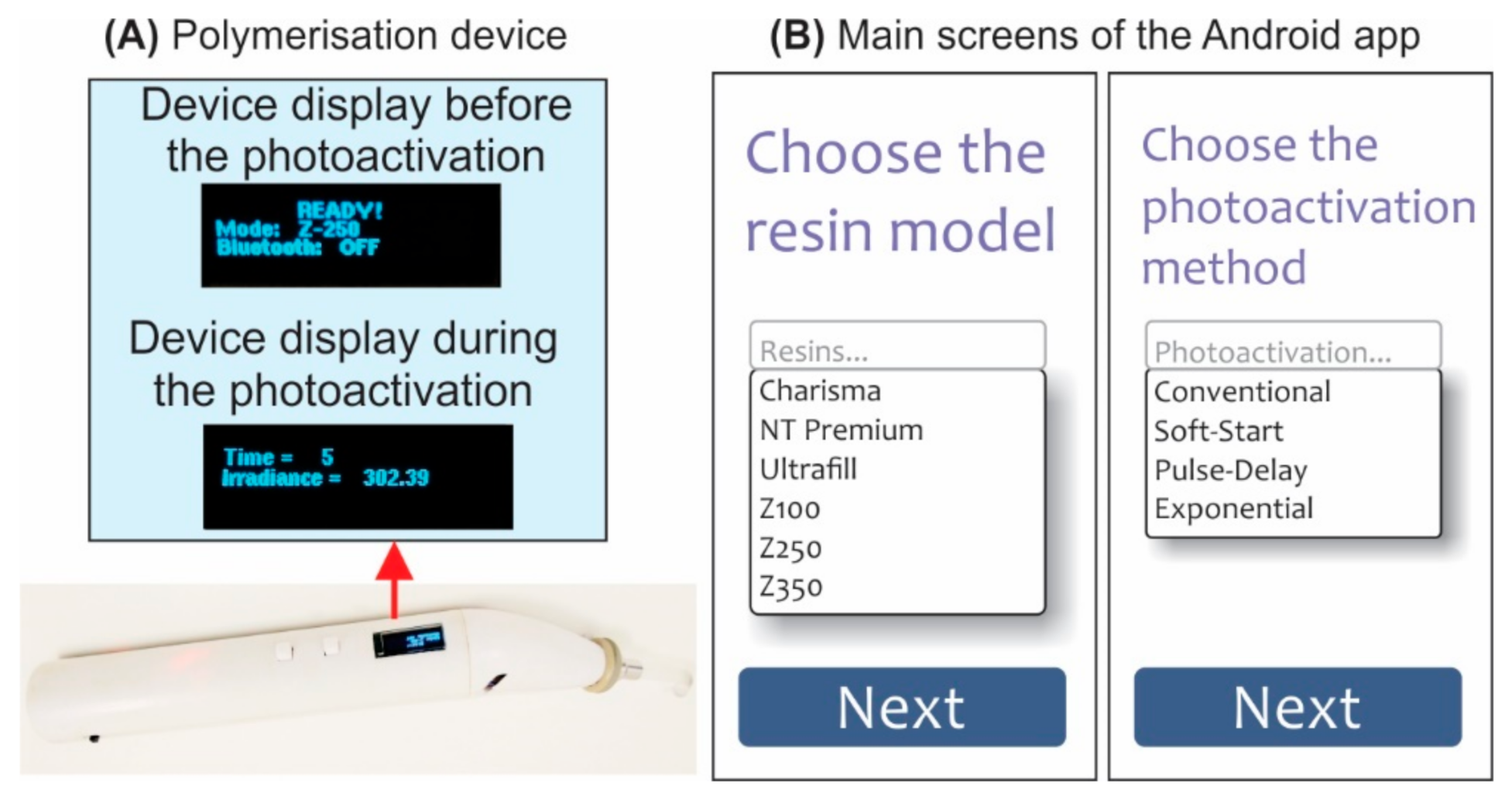
2. Materials and Methods
2.1. Resin Composites and Photoactivation Techniques
2.2. Monitoring of the Polymerisation Shrinkage Stress
2.3. Monitoring of the Resin/Tooth Temperature Variation
2.4. Depth of Cure Evaluation
2.5. Statistical Analyses
3. Results
3.1. Shrinkage Stress
3.2. Temperature Variation
3.3. Depth of Cure
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Jum’ah, A.A.; Creanor, S.; Wilson, N.H.F.; Burke, F.J.T.; Brunton, P.A. Dental Practice in the UK in 2015/2016. Part 3: Aspects of Indirect Restorations and Fixed Prosthodontics. Br. Dent. J. 2019, 226, 192–196. [Google Scholar] [CrossRef] [PubMed]
- Nejatian, T.; Sultan, Z.; Zafar, M.; Najeeb, S.; Shahab, S.; Mazafari, M.; Hopkinson, L.; Sefat, F. Dental Biocomposites. In Biomaterials for Oral and Dental Tissue Engineering; Woodhead Publishing: Sawston, UK, 2017; pp. 65–84. ISBN 978-0-08-100967-3. [Google Scholar]
- AlShaafi, M.M. Factors Affecting Polymerization of Resin-Based Composites: A Literature Review. Saudi Dent J. 2017, 29, 48–58. [Google Scholar] [CrossRef]
- Meereis, C.T.W.; Münchow, E.A.; de Oliveira da Rosa, W.L.; da Silva, A.F.; Piva, E. Polymerization Shrinkage Stress of Resin-Based Dental Materials: A Systematic Review and Meta-Analyses of Composition Strategies. J. Mech. Behav. Biomed. Mater. 2018, 82, 268–281. [Google Scholar] [CrossRef]
- Münchow, E.A.; Meereis, C.T.W.; de Oliveira da Rosa, W.L.; da Silva, A.F.; Piva, E. Polymerization Shrinkage Stress of Resin-Based Dental Materials: A Systematic Review and Meta-Analyses of Technique Protocol and Photo-Activation Strategies. J. Mech. Behav. Biomed. Mater. 2018, 82, 77–86. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.A.; Zafar, M.S.; Ghubayri, A.A.A.; AlMufareh, N.A.; Binobaid, A.; Eskandrani, R.M.; Al-Kheraif, A.A. Polymerisation of Restorative Dental Composites: Influence on Physical, Mechanical and Chemical Properties at Various Setting Depths. Mater. Technol. 2020, 1–7. [Google Scholar] [CrossRef]
- Rueggeberg, F.A.; Giannini, M.; Arrais, C.A.G.; Price, R.B.T.; Rueggeberg, F.A.; Giannini, M.; Arrais, C.A.G.; Price, R.B.T. Light Curing in Dentistry and Clinical Implications: A Literature Review. Braz. Oral Res. 2017, 31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Silva, V.A.D.; Silva, S.A.D.; Pecho, O.E.; Bacchi, A. Influence of Composite Type and Light Irradiance on Color Stability after Immersion in Different Beverages. J. Esthet. Restor. Dent. 2018, 30, 390–396. [Google Scholar] [CrossRef]
- Selig, D.; Haenel, T.; Hausnerová, B.; Moeginger, B.; Labrie, D.; Sullivan, B.; Price, R.B.T. Examining Exposure Reciprocity in a Resin Based Composite Using High Irradiance Levels and Real-Time Degree of Conversion Values. Dent. Mater. 2015, 31, 583–593. [Google Scholar] [CrossRef]
- Guimarães, G.F.; Marcelino, E.; Cesarino, I.; Vicente, F.B.; Grandini, C.R.; Simões, R.P.; Guimarães, G.F.; Marcelino, E.; Cesarino, I.; Vicente, F.B.; et al. Minimization of Polymerization Shrinkage Effects on Composite Resins by the Control of Irradiance during the Photoactivation Process. J. Appl. Oral Sci. 2018, 26. [Google Scholar] [CrossRef]
- van Dijken, J.W.V.; Pallesen, U. Durability of a Low Shrinkage TEGDMA/HEMA-Free Resin Composite System in Class II Restorations. A 6-Year Follow Up. Dent. Mater. 2017, 33, 944–953. [Google Scholar] [CrossRef]
- Celik, C.; Cehreli, S.B.; Arhun, N. Resin Composite Repair: Quantitative Microleakage Evaluation of Resin-Resin and Resin-Tooth Interfaces with Different Surface Treatments. Eur. J. Dent. 2015, 9, 92–99. [Google Scholar] [CrossRef]
- Rastelli, A.N.S.; Jacomassi, D.P.; Bagnato, V.S. Effect of Power Densities and Irradiation Times on the Degree of Conversion and Temperature Increase of a Microhybrid Dental Composite Resin. Laser Phys. 2008, 18, 1074–1079. [Google Scholar] [CrossRef]
- Vinagre, A.; Ramos, J.C.; Rebelo, C.; Basto, J.F.; Messias, A.; Alberto, N.; Nogueira, R. Pulp Temperature Rise Induced by Light-Emitting Diode Light-Curing Units Using an Ex Vivo Model. Materials 2019, 12, 411. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gonçalves, F.; Calheiros, F.C.; Witzel, M.F.; Kawano, Y.; Braga, R.R. Effect of Photoactivation Protocol and Radiant Exposure on Monomer Conversion and Flexural Strength of a Resin Composite after Water and Ethanol Storage. J. Biomed. Mater. Res. Part B Appl. Biomater. 2007, 82, 89–92. [Google Scholar] [CrossRef]
- Watts, D.C.; Kaiser, C.; O’Neill, C.; Price, R.B. Reporting of Light Irradiation Conditions in 300 Laboratory Studies of Resin-Composites. Dent. Mater. 2019, 35, 414–421. [Google Scholar] [CrossRef]
- Cardoso, K.A.O.R.d.F.; Zarpellon, D.C.; Madruga, C.F.L.; Rodrigues, J.A.; Arrais, C.A.G.; Zarpellon, D.C.; Madruga, C.F.L.; Rodrigues, J.A.; Arrais, C.A.G. Effects of Radiant Exposure Values Using Second and Third Generation Light Curing Units on the Degree of Conversion of a Lucirin-Based Resin Composite. J. Appl. Oral Sci. 2017, 25, 140–146. [Google Scholar] [CrossRef] [Green Version]
- Thorat, S.; Patra, N.; Ruffilli, R.; Diaspro, A.; Salerno, M. Preparation and Characterization of a BisGMA-Resin Dental Restorative Composites with Glass, Silica and Titania Fillers. Dent. Mater. J. 2012, 31, 635–644. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Derchi, G.; Vano, M.; Ceseracciu, L.; Diaspro, A.; Salerno, M. Stiffness Effect of Using Polywave or Monowave LED Units for Photo-Curing Different Bulk Fill Composites. Dent. Mater. J. 2018. [Google Scholar] [CrossRef] [Green Version]
- Alrahlah, A.; Silikas, N.; Watts, D.C. Post-Cure Depth of Cure of Bulk Fill Dental Resin-Composites. Dent. Mater. 2014, 30, 149–154. [Google Scholar] [CrossRef]
- Monte Alto, R.V.; Guimarães, J.G.A.; Poskus, L.T.; da Silva, E.M. Depth of Cure of Dental Composites Submitted to Different Light-Curing Modes. J. Appl. Oral Sci. 2006, 14, 71–76. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al-Ahdal, K.; Ilie, N.; Silikas, N.; Watts, D.C. Polymerization Kinetics and Impact of Post Polymerization on the Degree of Conversion of Bulk-Fill Resin-Composite at Clinically Relevant Depth. Dent. Mater. 2015, 31, 1207–1213. [Google Scholar] [CrossRef]
- Schneider, A.C.; Mendonça, M.J.; Rodrigues, R.B.; Busato, P.D.M.R.; Camilotti, V. Influência de Três Modos de Fotopolimerização Sobre a Microdureza de Três Resinas Compostas. Polímeros 2016, 26, 37–42. [Google Scholar] [CrossRef] [Green Version]
- Kim, R.J.-Y.; Lee, I.-B.; Yoo, J.-Y.; Park, S.-J.; Kim, S.-Y.; Yi, Y.-A.; Hwang, J.-Y.; Seo, D.-G. Real-Time Analysis of Temperature Changes in Composite Increments and Pulp Chamber during Photopolymerization. BioMed Res. Int. 2015, 2015, 923808. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ernst, C.-P.; Brand, N.; Frommator, U.; Rippin, G.; Willershausen, B. Reduction of Polymerization Shrinkage Stress and Marginal Microleakage Using Soft-Start Polymerization. J. Esthet. Restor. Dent. 2003, 15, 93–103. [Google Scholar] [CrossRef] [PubMed]
- Soares, C.; Bicalho, A.; Verissimo, C.; Soares, P.; Tantbirojn, D.; Versluis, A. Delayed Photo-Activation Effects on Mechanical Properties of Dual Cured Resin Cements and Finite Element Analysis of Shrinkage Stresses in Teeth Restored With Ceramic Inlays. Oper. Dent. 2016, 41, 491–500. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tauböck, T.T.; Feilzer, A.J.; Buchalla, W.; Kleverlaan, C.J.; Krejci, I.; Attin, T. Effect of Modulated Photo-Activation on Polymerization Shrinkage Behavior of Dental Restorative Resin Composites. Eur. J. Oral Sci. 2014, 122, 293–302. [Google Scholar] [CrossRef]
- Fujita, K.; Ikemi, T.; Nishiyama, N. Effects of Particle Size of Silica Filler on Polymerization Conversion in a Light-Curing Resin Composite. Dent. Mater. 2011, 27, 1079–1085. [Google Scholar] [CrossRef]
- Maghaireh, G.; Taha, N.; Alzraikat, H. The Silorane-Based Resin Composites: A Review. Oper. Dent. 2017, 42, E24–E34. [Google Scholar] [CrossRef] [PubMed]
- Ferracane, J.L. Resin Composite—State of the Art. Dent. Mater. 2011, 27, 29–38. [Google Scholar] [CrossRef] [PubMed]
- Yildirim Bicer, A.Z.; Karakis, D.; Dogan, A.; Mert, F. A Comparison of Wear Rate of Direct and Indirect Resin Composites: A Two-Body Wear Abrasion Test. J. Compos. Mater. 2015, 49, 2599–2607. [Google Scholar] [CrossRef]
- Habib, E.; Wang, R.; Wang, Y.; Zhu, M.; Zhu, X.X. Inorganic Fillers for Dental Resin Composites: Present and Future. ACS Biomater. Sci. Eng. 2016, 2, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Flury, S.; Peutzfeldt, A.; Lussi, A. Influence of Increment Thickness on Microhardness and Dentin Bond Strength of Bulk Fill Resin Composites. Dent. Mater. 2014, 30, 1104–1112. [Google Scholar] [CrossRef]
- Son, S.-A.; Roh, H.-M.; Hur, B.; Kwon, Y.-H.; Park, J.-K. The Effect of Resin Thickness on Polymerization Characteristics of Silorane-Based Composite Resin. Restor. Dent. Endod. 2014, 39, 310–318. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de Camargo, E.J.; Moreschi, E.; Baseggio, W.; Cury, J.A.; Pascotto, R.C. Composite depth of cure using four polymerization techniques. J. Appl. Oral Sci. 2009, 17, 446–450. [Google Scholar] [CrossRef] [PubMed]
- Chesterman, J.; Jowett, A.; Gallacher, A.; Nixon, P. Bulk-Fill Resin-Based Composite Restorative Materials: A Review. Br. Dent. J. 2017, 222, 337–344. [Google Scholar] [CrossRef]
- Beltrami, R.; Chiesa, M.; Scribante, A.; Allegretti, J.; Poggio, C. Comparison of Shear Bond Strength of Universal Adhesives on Etched and Nonetched Enamel. J. Appl. Biomater. Funct. Mater. 2016, 14, e78–e83. [Google Scholar] [CrossRef] [Green Version]
- Sunbul, H.A.; Silikas, N.; Watts, D.C. Polymerization Shrinkage Kinetics and Shrinkage-Stress in Dental Resin-Composites. Dent. Mater. 2016, 32, 998–1006. [Google Scholar] [CrossRef] [Green Version]
- Lau, A.; Li, J.; Heo, Y.C.; Fok, A. A Study of Polymerization Shrinkage Kinetics Using Digital Image Correlation. Dent. Mater. 2015, 31, 391–398. [Google Scholar] [CrossRef]
- Wang, R.; Zhang, M.; Liu, F.; Bao, S.; Wu, T.; Jiang, X.; Zhang, Q.; Zhu, M. Investigation on the Physical-Mechanical Properties of Dental Resin Composites Reinforced with Novel Bimodal Silica Nanostructures. Mater. Sci. Eng. C Mater. Biol. Appl. 2015, 50, 266–273. [Google Scholar] [CrossRef]
- Boroujeni, P.M.; Mousavinasab, S.M.; Hasanli, E. Effect of Configuration Factor on Gap Formation in Hybrid Composite Resin, Low-Shrinkage Composite Resin and Resin-Modified Glass Ionomer. J. Investig. Clin. Dent. 2015, 6, 156–160. [Google Scholar] [CrossRef]
- Gamarra, V.S.S.; Borges, G.A.; Júnior, L.H.B.; Spohr, A.M. Marginal Adaptation and Microleakage of a Bulk-Fill Composite Resin Photopolymerized with Different Techniques. Odontology 2018, 106, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Kumar, N.; Fareed, M.A.; Zafar, M.S.; Ghani, F.; Khurshid, Z. Influence of Various Specimen Storage Strategies on Dental Resin-Based Composite Properties. Mater. Technol. 2021, 36, 54–62. [Google Scholar] [CrossRef]
- Deepa, C.S.; Krishnan, V.K. Effect of Resin Matrix Ratio, Storage Medium, and Time upon the Physical Properties of a Radiopaque Dental Composite. J. Biomater. Appl. 2000, 14, 296–315. [Google Scholar] [CrossRef]
- Zhang, Y.; Xu, J. Effect of Immersion in Various Media on the Sorption, Solubility, Elution of Unreacted Monomers, and Flexural Properties of Two Model Dental Composite Compositions. J. Mater. Sci. Mater. Med. 2008, 19, 2477–2483. [Google Scholar] [CrossRef]
- Kumar, N.; Zafar, M.S.; Dahri, W.M.; Khan, M.A.; Khurshid, Z.; Najeeb, S. Effects of Deformation Rate Variation on Biaxial Flexural Properties of Dental Resin Composites. J. Taibah Univ. Med Sci. 2018, 13, 319–326. [Google Scholar] [CrossRef] [PubMed]
- Moldovan, M.; Balazsi, R.; Soanca, A.; Roman, A.; Sarosi, C.; Prodan, D.; Vlassa, M.; Cojocaru, I.; Saceleanu, V.; Cristescu, I. Evaluation of the Degree of Conversion, Residual Monomers and Mechanical Properties of Some Light-Cured Dental Resin Composites. Materials 2019, 12, 2109. [Google Scholar] [CrossRef] [Green Version]
- Park, J.-K.; Lee, G.-H.; Kim, J.-H.; Park, M.-G.; Ko, C.-C.; Kim, H.-I.; Kwon, Y.H. Polymerization Shrinkage, Flexural and Compression Properties of Low-Shrinkage Dental Resin Composites. Dent. Mater. J. 2014, 33, 104–110. [Google Scholar] [CrossRef] [PubMed] [Green Version]




| Resin | Manufacturer | Classification | Organic Matrix 1 | Inorganic Charge |
|---|---|---|---|---|
| Filtek Z-250 XT | (3M ESPE, St. Paul, MN, USA) | Nanohybrid | Bis-GMA TEG-DMA Bis-EMA PEG-DMA UDMA | Surface-modified Zirconia/silica (0.01–3.0 µm) Non-agglomerated/non-aggregated SiO2 (0.02 µm) Filler loading (68% volume) |
| Charisma Classic | (Heraeus Kulzer, Hanau, Germany) | Microhybrid | Bis-GMA | Microglass® Barium aluminium fluoride glass Particle size (0.005–10 µm) Filler loading (61% volume) |
| Ultrafill | (Biodinâmica Ltd.a, PR, Brazil) | Microhybrid | TEG-DMA UDMA | Inorganic charge (0.04–2.2 µm) Filler loading (79% volume) |
| Resin | ETOTAL (J) | Conventional | Soft-Start | Pulse-Delay | Exponential |
|---|---|---|---|---|---|
| Z-250 | 10 | Step 1: i: 1000 mW/cm2 Time: 10 s | Step 1: i: 500 mW/cm2 Time: 5 s Step 2: i: 1000 mW/cm2 Time: 7.5 s | Step 1: i: 500 mW/cm2 Time: 5 s Step 2: i: 0 mW/cm2 Time: 200 s Step 3: i: 1000 mW/cm2 Time: 7.5 s | Step 1: i: defined by Equation (2) Time: 30 s |
| Charisma | 20 | Step 1: i: 1000 mW/cm2 Time: 10 s | Step 1: i: 500 mW/cm2 Time: 10 s Step 2: i: 1000 mW/cm2 Time: 15 s | Step 1: i: 500 mW/cm2 Time: 10 s Step 2: i: 0 mW/cm2 Time: 200 s Step 3: i: 1000 mW/cm2 Time: 15 s | Step 1: i: defined by Equation (2) Time: 39 s |
| Ultrafill | 16 | Step 1: i: 1000 mW/cm2 Time: 16 s | Step 1: i: 500 mW/cm2 Time: 10 s Step 2: i: 1000 mW/cm2 Time: 11 s | Step 1: i: 500 mW/cm2 Time: 10 s Step 2: i: 0 mW/cm2 Time: 200 s Step 3: i: 1000 mW/cm2 Time: 11 s | Step 1: i: defined by Equation (2) Time: 37 s |
| Resin | Conventional (Mean ± SD) MPa | Soft-Start (Mean ± SD) MPa | Pulse-Delay (Mean ± SD) MPa | Exponential (Mean ± SD) MPa |
|---|---|---|---|---|
| Z250 | 1.24 ± 0.05 A,a | 0.99 ± 0.08 B,a | 0.74 ± 0.06 C,a | 0.73 ± 0.02 C,a |
| Charisma | 1.64 ± 0.08 A,b | 1.29 ± 0.05 B,b | 0.96 ± 0.07 C,b | 0.96 ± 0.10 C,b |
| Ultrafill | 1.91 ± 0.03 A,b | 1.41 ± 0.11 B,b | 0.90 ± 0.13 C,b | 0.88 ± 0.07 C,b |
| Resin | Conventional (Mean ± SD) °C | Soft-Start (Mean ± SD) °C | Pulse-Delay (Mean ± SD) °C | Exponential (Mean ± SD) °C |
|---|---|---|---|---|
| Z250 | 2.39 ± 0.11 A,a | 2.72 ± 0.11 B,a | 2.80 ± 0.21 B,a | 0.75 ± 0.09 C,a |
| Charisma | 1.84 ± 0.10 A,b | 1.01 ± 0.05 B,b | 2.23 ± 0.09 C,b | 0.59 ± 0.08 D,b |
| Ultrafill | 3.14 ± 0.18 A,a | 2.61 ± 0.19 B,a | 2.49 ± 0.09 B,a | 0.98 ± 0.15 C,a |
| Resin | Depth | Conventional (Mean ± SD) HV | Soft-Start (Mean ± SD) HV | Pulse-Delay (Mean ± SD) HV | Exponential (Mean ± SD) HV |
|---|---|---|---|---|---|
| Z250 | 0 mm | 82.5 ± 1.9 A,a | 81.4 ± 2.7 A,a | 82.9 ± 1.4 A,a | 81.8 ± 0.8 A,a |
| Charisma | 0 mm | 83.0 ± 1.8 A,a | 79.4 ± 1.9 A,a | 80.4 ± 2.4 A,a | 83.4 ± 0.9 A,a |
| Ultrafill | 0 mm | 72.8 ± 1.3 A,b | 74.0 ± 1.8 A,b | 73.1 ± 1.3 A,b | 72.3 ± 0.7 A,b |
| Z250 | 2 mm | 81.0 ± 3.6 A,a | 76.0 ± 6.1 A,a | 79.3 ± 6.7 A,a | 80.2 ± 2.8 A,a |
| Charisma | 2 mm | 79.8 ± 2.8 A,a | 78.6 ± 3.2 A,a | 78.6 ± 4.2 A,a | 80.4 ± 4.1 A,a |
| Ultrafill | 2 mm | 71.2 ± 6.7 A,b | 69.6 ± 3.4 A,b | 68.9 ± 4.8 A,b | 68.1 ± 4.3 A,b |
| Z250 | 4 mm | 48.7 ± 5.3 B,a,* | 47.6 ± 6.4 B,a,* | 39.1 ± 7.9 B,a,* | 52.0 ± 5.4 B,a,* |
| Charisma | 4 mm | 47.7 ± 5.6 B,a,* | 41.8 ± 4.5 B,a,* | 42.1 ± 5.1 B,a,* | 49.7 ± 5.7 B,a,* |
| Ultrafill | 4 mm | 30.0 ± 4.8 B,b,* | 34.1 ± 4.9 B,b,* | 30.5 ± 2.5 B,b,* | 33.1 ± 2.8 B,b,* |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
dos Santos Sousa, G.; Guimarães, G.F.; Marcelino, E.; Rodokas, J.E.P.; de Oliveira Júnior, A.J.; Cesarino, I.; Leão, A.L.; dos Santos Riccardi, C.; Arjmand, M.; Simões, R.P. Shrinkage Stress and Temperature Variation in Resin Composites Cured via Different Photoactivation Methods: Insights for Standardisation of the Photopolymerisation. Polymers 2021, 13, 2065. https://doi.org/10.3390/polym13132065
dos Santos Sousa G, Guimarães GF, Marcelino E, Rodokas JEP, de Oliveira Júnior AJ, Cesarino I, Leão AL, dos Santos Riccardi C, Arjmand M, Simões RP. Shrinkage Stress and Temperature Variation in Resin Composites Cured via Different Photoactivation Methods: Insights for Standardisation of the Photopolymerisation. Polymers. 2021; 13(13):2065. https://doi.org/10.3390/polym13132065
Chicago/Turabian Styledos Santos Sousa, Guilherme, Gabriel Felipe Guimarães, Edilmar Marcelino, José Eduardo Petit Rodokas, Arilson José de Oliveira Júnior, Ivana Cesarino, Alcides Lopes Leão, Carla dos Santos Riccardi, Mohammad Arjmand, and Rafael Plana Simões. 2021. "Shrinkage Stress and Temperature Variation in Resin Composites Cured via Different Photoactivation Methods: Insights for Standardisation of the Photopolymerisation" Polymers 13, no. 13: 2065. https://doi.org/10.3390/polym13132065
APA Styledos Santos Sousa, G., Guimarães, G. F., Marcelino, E., Rodokas, J. E. P., de Oliveira Júnior, A. J., Cesarino, I., Leão, A. L., dos Santos Riccardi, C., Arjmand, M., & Simões, R. P. (2021). Shrinkage Stress and Temperature Variation in Resin Composites Cured via Different Photoactivation Methods: Insights for Standardisation of the Photopolymerisation. Polymers, 13(13), 2065. https://doi.org/10.3390/polym13132065









