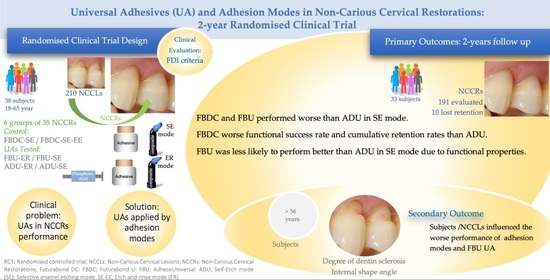
Universal Adhesives and Adhesion Modes in Non-Carious Cervical Restorations: 2-Year Randomised Clinical Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Trial Design
2.2. Sample Size
2.3. Participants
2.4. Randomisation and Blinding
2.5. Interventions
2.6. Follow-Up Examinations and Outcomes
2.7. Statistical Analysis
3. Results
3.1. Esthetic, Functional, and Biological Properties
3.2. Clinical Performance
3.3. Success Rates
3.4. Retention Rates
3.5. Participants’ and NCCLs’ Characteristics
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Takamizawa, T.; Barkmeier, W.W.; Tsujimoto, A.; Berry, T.P.; Watanabe, H.; Erickson, R.L.; Latta, M.A.; Miyazaki, M. Influence of different etching modes on bond strength and fatigue strength to dentin using universal adhesive systems. Dent. Mater. 2016, 32, e9–e21. [Google Scholar] [CrossRef] [PubMed]
- Perdigão, J.; Ceballos, L.; Giráldez, I.; Baracco, B.; Fuentes, M.V. Effect of a hydrophobic bonding resin on the 36-month performance of a universal adhesive—a randomized clinical trial. Clin. Oral Investig. 2020, 24, 765–776. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, A.A.; Leite, M.M.; Zago, J.K.M.; Nunes, C.A.B.C.M.; Barata, T.D.J.E.; De Freitas, G.C.; De Torres, É.M.; Lopes, L.G. Influence of different application protocols of universal adhesive system on the clinical behavior of Class I and II restorations of composite resin—A randomized and double-blind controlled clinical trial. BMC Oral Heal. 2019, 19, 252. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Shi, Y.; Li, T.; Pan, Y.; Cui, Y.; Xia, W. Adhesive interfacial characteristics and the related bonding performance of four self-etching adhesives with different functional monomers applied to dentin. J. Dent. 2017, 62, 72–80. [Google Scholar] [CrossRef]
- Bonding Performance of Universal Adhesives: An Updated Systematic Review and Meta-Analysis. J. Adhes. Dent. 2019, 21, 7–26.
- Nagarkar, S.; Theis-Mahon, N.; Perdigão, J. Universal dental adhesives: Current status, laboratory testing, and clinical performance. J. Biomed. Mater. Res. Part B Appl. Biomater. 2019, 107, 2121–2131. [Google Scholar] [CrossRef]
- Tsujimoto, A.; Barkmeier, W.W.; Takamizawa, T.; Watanabe, H.; Johnson, W.W.; Latta, M.A.; Miyazaki, M. Influence of duration of phosphoric acid pre-etching on bond durability of universal adhesives and surface free-energy characteristics of enamel. Eur. J. Oral Sci. 2016, 124, 377–386. [Google Scholar] [CrossRef]
- Suzuki, T.; Takamizawa, T.; Barkmeier, W.W.; Tsujimoto, A.; Endo, H.; Erickson, R.L.; Latta, M.A.; Miyazaki, M. Influence of Etching Mode on Enamel Bond Durability of Universal Adhesive Systems. Oper. Dent. 2016, 41, 520–530. [Google Scholar] [CrossRef] [Green Version]
- De Cardoso, G.C.; Nakanishi, L.; Isolan, C.P.; Jardim, P.D.S.; De Moraes, R.R. Bond Stability of Universal Adhesives Applied To Dentin Using Etch-And-Rinse or Self-Etch Strategies. Braz. Dent. J. 2019, 30, 467–475. [Google Scholar] [CrossRef]
- Papadogiannis, D.; Dimitriadi, M.; Zafiropoulou, M.; Gaintantzopoulou, M.-D.; Eliades, G. Universal Adhesives: Setting Characteristics and Reactivity with Dentin. Materials 2019, 12, 1720. [Google Scholar] [CrossRef] [Green Version]
- Peumans, M.; Politano, G.; Van Meerbeek, B. Treatment of noncarious cervical lesions: When, why, and how. Int. J. Esthet. Dent. 2020, 15, 16–42. [Google Scholar]
- Morsy, K.E.; Abdalla, A.I.; Shalaby, M.E. Clinical evaluation of three adhesive systems in class V carious lesions. Tanta Dent. J. 2018, 15, 132. [Google Scholar] [CrossRef]
- Mahn, E.; Rousson, V.; Heintze, S. Meta-Analysis of the Influence of Bonding Parameters on the Clinical Outcome of Tooth-colored Cervical Restorations. J. Adhes. Dent. 2015, 17, 391–403. [Google Scholar] [CrossRef]
- Ruschel, V.C.; Shibata, S.; Stolf, S.C.; Chung, Y.; Baratieri, L.N.; Heymann, H.O.; Walter, R. Eighteen-month Clinical Study of Universal Adhesives in Noncarious Cervical Lesions. Oper. Dent. 2018, 43, 241–249. [Google Scholar] [CrossRef]
- Kemaloğlu, H.; Atalayin, C.; Ergucu, Z.; Onal, B. Follow-up of flowable resin composites performed with a universal adhesive system in non-carious cervical lesions: A randomized, controlled 24-month clinical trial. Am. J. Dent. 2020, 33, 39–42. [Google Scholar]
- Burke, F.T.; Crisp, R.J.; Cowan, A.J.; Raybould, L.; Redfearn, P.; Sands, P.; Thompson, O.; Ravaghi, V. A Randomised Controlled Trial of a Universal Bonding Agent at Three Years: Self Etch vs Total Etch. Eur. J. Prosthodont. Restor. Dent. 2017, 25, 220–227. [Google Scholar]
- Atalay, C.; Ozgunaltay, G.; Yazici, A.R. Thirty-six-month clinical evaluation of different adhesive strategies of a universal adhesive. Clin. Oral Investig. 2020, 24, 1569–1578. [Google Scholar] [CrossRef]
- De Albuquerque, E.G.; Santana, F.W.K.; Calazans, F.S.; Poubel, L.A.; Marins, S.S.; Matos, T.D.P.; Hanzen, T.A.; Barceleiro, M.D.O.; Loguercio, A.D. A new universal simplified adhesive: 6-month randomized multi-center clinical trial. Rev. Bras. Odontol. 2017, 74, 251. [Google Scholar] [CrossRef] [Green Version]
- Perdigão, J.; Kose, C.; Mena-Serrano, A.P.; De Paula, E.A.; Tay, L.Y.; Reis, A.; Loguercio, A.D. A New Universal Simplified Adhesive: 18-Month Clinical Evaluation. Oper. Dent. 2014, 39, 113–127. [Google Scholar] [CrossRef] [Green Version]
- Oz, F.D.; Kutuk, Z.B.; Ozturk, C.; Soleimani, R.; Gurgan, S. An 18-month clinical evaluation of three different universal adhesives used with a universal flowable composite resin in the restoration of non-carious cervical lesions. Clin. Oral Investig. 2019, 23, 1443–1452. [Google Scholar] [CrossRef]
- Oz, F.D.; Ergin, E.; Canatan, S. Twenty-four-month clinical performance of different universal adhesives in etch-and-rinse, selective etching and self-etch application modes in NCCL—A randomized controlled clinical trial. J. Appl. Oral Sci. 2019, 27, 20180358. [Google Scholar] [CrossRef]
- Mena-Serrano, A.; Kose, C.; De Paula, E.A.; Tay, L.Y.; Reis, A.; Loguercio, A.D.; Perdigão, J. A New Universal Simplified Adhesive: 6-Month Clinical Evaluation. J. Esthet. Restor. Dent. 2012, 25, 55–69. [Google Scholar] [CrossRef]
- Manarte-Monteiro, P.; Domingues, J.; Teixeira, L.; Gavinha, S.; Manso, M.C. Multi-Mode adhesives performance and success/retention rates in NCCLs restorations: Randomised clinical trial one-year report. Biomater. Investig. Dent. 2019, 6, 43–53. [Google Scholar] [CrossRef] [Green Version]
- Lopes, L.; Calazans, F.; Hidalgo, R.; Buitrago, L.; Gutierrez, F.; Reis, A.; Loguercio, A.; Barceleiro, M. Six-month Follow-up of Cervical Composite Restorations Placed With a New Universal Adhesive System: A Randomized Clinical Trial. Oper. Dent. 2016, 41, 465–480. [Google Scholar] [CrossRef] [Green Version]
- Loguercio, A.D.; de Paula, E.A.; Hass, V.; Luque-Martinez, I.; Reis, A.; Perdigão, J. A new universal simplified adhesive: 36-Month randomized double-blind clinical trial. J. Dent. 2015, 43, 1083–1092. [Google Scholar] [CrossRef]
- Lawson, N.C.; Robles, A.; Fu, C.-C.; Lin, C.P.; Sawlani, K.; Burgess, J.O. Two-year clinical trial of a universal adhesive in total-etch and self-etch mode in non-carious cervical lesions. J. Dent. 2015, 43, 1229–1234. [Google Scholar] [CrossRef] [Green Version]
- Wv, V.D.J.; Ulla, P. Three-year Randomized Clinical Study of a One-step Universal Adhesive and a Two-step Self-etch Adhesive in Class II Composite Restorations. J. Adhes. Dent. 2017, 19, 287–294. [Google Scholar] [CrossRef]
- Hickel, R.; Roulet, J.-F.; Bayne, S.; Heintze, S.D.; Mjör, I.A.; Peters, M.; Rousson, V.; Randall, R.; Schmalz, G.; Tyas, M.; et al. Recommendations for conducting controlled clinical studies of dental restorative materials. Clin. Oral Investig. 2007, 11, 5–33. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Hopewell, S.; Schulz, K.F.; Montori, V.; Gøtzsche, P.C.; Devereaux, P.; Elbourne, D.; Egger, M.; Altman, D.G. CONSORT 2010 explanation and elaboration: Updated guidelines for reporting parallel group randomised trials. Int. J. Surg. 2012, 10, 28–55. [Google Scholar] [CrossRef] [Green Version]
- Greene, J.G.; Vermillion, J.R. The Simplified Oral Hygiene Index. J. Am. Dent. Assoc. 1964, 68, 7–13. [Google Scholar] [CrossRef]
- Pitts, N.B.; Ekstrand, K.; Foundation, T.I. International Caries Detection and Assessment System (ICDAS) and its International Caries Classification and Management System (ICCMS)—Methods for staging of the caries process and enabling dentists to manage caries. Commun. Dent. Oral Epidemiol. 2013, 41, e41–e52. [Google Scholar] [CrossRef] [PubMed]
- Ritter, A.V.; Heymann, H.O.; Swift, E.J.; Sturdevant, J.R.; Wilder, A.D. Clinical Evaluation of an All-in-one Adhesive in Non-Carious Cervical Lesions with Different Degrees of Dentin Sclerosis. Oper. Dent. 2008, 33, 370–378. [Google Scholar] [CrossRef] [PubMed]
- Loguercio, A.D.; Luque-Martinez, I.V.; Fuentes, S.; Reis, A.; Muñoz, M.A. Effect of dentin roughness on the adhesive performance in non-carious cervical lesions: A double-blind randomized clinical trial. J. Dent. 2017, 69, 60–69. [Google Scholar] [CrossRef] [PubMed]
- Ruschel, V.C.; Stolf, S.C.; Shibata, S.; Chung, Y.; Boushell, L.W.; Baratieri, L.N.; Walter, R. Three-year clinical evaluation of universal adhesives in non-carious cervical lesions. Am. J. Dent. 2019, 32, 223–228. [Google Scholar] [PubMed]
- Torres, C.R.G.; Zanatta, R.; Silva, T.J.; Huhtala, M.F.R.L.; Borges, A.B. Influence of previous acid etching on bond strength of universal adhesives to enamel and dentin. Gen. Dent. 2017, 65, e17–e21. [Google Scholar]
- Yoshihara, K.; Yoshida, Y.; Hayakawa, S.; Nagaoka, N.; Irie, M.; Ogawa, T.; Van Landuyt, K.L.; Osaka, A.; Suzuki, K.; Minagi, S.; et al. Nanolayering of phosphoric acid ester monomer on enamel and dentin. Acta Biomater. 2011, 7, 3187–3195. [Google Scholar] [CrossRef]
- Yoshihara, K.; Hayakawa, S.; Nagaoka, N.; Okihara, T.; Yoshida, Y.; Van Meerbeek, B. Etching Efficacy of Self-Etching Functional Monomers. J. Dent. Res. 2018, 97, 1010–1016. [Google Scholar] [CrossRef]
- Meerbeek, B.V.; Yoshihara, K.; Van Landuyt, K.; Yoshida, Y.; Peumans, M. From Buonocore’s Pioneering Acid-Etch Technique to Self-Adhering Restoratives. A Status Perspective of Rapidly Advancing Dental Adhesive Technology. J. Adhes. Den. 2020, 22, 7–34. [Google Scholar] [CrossRef]
- Yoshida, Y.; Yoshihara, K.; Nagaoka, N.; Hayakawa, S.; Torii, Y.; Ogawa, T.; Osaka, A.; Van Meerbeek, B. Self-assembled Nano-layering at the Adhesive Interface. J. Dent. Res. 2012, 91, 376–381. [Google Scholar] [CrossRef]
- Yoshihara, K.; Yoshida, Y.; Hayakawa, S.; Nagaoka, N.; Torii, Y.; Osaka, A.; Suzuki, K.; Minagi, S.; Van Meerbeek, B.; Van Landuyt, K. Self-etch Monomer-Calcium Salt Deposition on Dentin. J. Dent. Res. 2011, 90, 602–606. [Google Scholar] [CrossRef]
- Chen, C.; Niu, L.-N.; Xie, H.; Zhang, Z.-Y.; Zhou, L.-Q.; Jiao, K.; Chen, J.-H.; Pashley, D.; Tay, F. Bonding of universal adhesives to dentine—Old wine in new bottles? J. Dent. 2015, 43, 525–536. [Google Scholar] [CrossRef] [Green Version]
- Tian, F.; Zhou, L.; Zhang, Z.; Niu, L.; Zhang, L.; Chen, C.; Zhou, J.; Yang, H.; Wang, X.; Fu, B.; et al. Paucity of Nanolayering in Resin-Dentin Interfaces of MDP-based Adhesives. J. Dent. Res. 2016, 95, 380–387. [Google Scholar] [CrossRef]
- Yoshida, Y.; Yoshihara, K.; Hayakawa, S.; Nagaoka, N.; Okihara, T.; Matsumoto, T.; Minagi, S.; Osaka, A.; Van Landuyt, K.; Van Meerbeek, B. HEMA Inhibits Interfacial Nano-layering of the Functional Monomer MDP. J. Dent. Res. 2012, 91, 1060–1065. [Google Scholar] [CrossRef]
- Hosaka, K.; Nakajima, M.; Takahashi, M.; Itoh, S.; Ikeda, M.; Tagami, J.; Pashley, D.H. Relationship between mechanical properties of one-step self-etch adhesives and water sorption. Dent. Mater. 2010, 26, 360–367. [Google Scholar] [CrossRef]
- Sugimura, R.; Tsujimoto, A.; Hosoya, Y.; Fischer, N.; Barkmeier, W.W.; Takamizawa, T.; Latta, M.A.; Miyazaki, M. Surface moisture influence on etch-and-rinse universal adhesive bonding. Am. J. Dent. 2019, 32, 33–38. [Google Scholar]
- Peumans, M.; De Munck, J.; Mine, A.; Van Meerbeek, B. Clinical effectiveness of contemporary adhesives for the restoration of non-carious cervical lesions. A systematic review. Dent. Mater. 2014, 30, 1089–1103. [Google Scholar] [CrossRef]
- Yamauchi, K.; Tsujimoto, A.; Jurado, C.; Shimatani, Y.; Nagura, Y.; Takamizawa, T.; Barkmeier, W.W.; Latta, M.A.; Miyazaki, M. Etch-and-rinse vs self-etch mode for dentin bonding effectiveness of universal adhesives. J. Oral Sci. 2019, 61, 549–553. [Google Scholar] [CrossRef] [Green Version]
- Hickel, R.; Peschke, A.; Tyas, M.; Mjör, I.; Bayne, S.; Peters, M.; Hiller, K.-A.; Randall, R.; Vanherle, G.; Heintze, S.D. FDI World Dental Federation—Clinical Criteria for the Evaluation of Direct and Indirect Restorations. Update and Clinical Examples. J. Adhes. Dent. 2010, 12, 259–272. [Google Scholar] [CrossRef]
- Dutra, D.C.L.; Renata, G.; Carpena, L.G. One-year Clinical Evaluation of Resin Composite Restorations of Noncarious Cervical Lesions in Smokers. J. Adhes. Dent. 2015, 17, 405–411. [Google Scholar] [CrossRef]
- Stewardson, D.; Creanor, S.L.; Thornley, P.; Bigg, T.; Bromage, C.; Browne, A.; Cottam, D.; Dalby, D.; Gilmour, J.; Horton, J.; et al. The survival of Class V restorations in general dental practice: Part 3, five-year survival. Br. Dent. J. 2012, 212, E14. [Google Scholar] [CrossRef]
- Brackett, M.; Dib, A.; Franco, G.; Estrada, B.E.; Brackett, W. Two-Year Clinical Performance of Clearfil SE and Clearfil S3 in Restoration of Unabraded Non-carious Class V Lesions. Oper. Dent. 2010, 35, 273–278. [Google Scholar] [CrossRef] [PubMed]
- Say, E.C.; Özel, E.; Yurdagüven, H.; Soyman, M. Three-year clinical evaluation of a two-step self-etch adhesive with or without selective enamel etching in non-carious cervical sclerotic lesions. Clin. Oral Investig. 2014, 18, 1427–1433. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rosa, W.L.D.O.D.; Piva, E.; da Silva, A.F. Bond strength of universal adhesives: A systematic review and meta-analysis. J. Dent. 2015, 43, 765–776. [Google Scholar] [CrossRef] [PubMed]
- How “Universal” is Adhesion? Shear Bond Strength of Multi-mode Adhesives to Enamel and Dentin. J. Adhes. Dent. 2019, 21, 87–95.

| Material (Manufacturer) Lot # Number | Composition |
|---|---|
| Futurabond DC (FBDC) (Voco, Cuxhaven, Germany) Lot# 1532592 | Liquid 1. Acidic adhesive monomer 1; Bis-GMA (5–10%), HEMA (5–10%) ;Liquid 2. Ethanol (50–100%); Initiator (2.5–5%) Mixture. organic acids, BIS-GMA, HEMA, TMPTMA§, camphorquinone, amines (DABE), BHT, catalysts, fluorides, and ethanol pH = 1.5 |
| Futurabond® U (FBU) (Voco, Cuxhaven, Germany) Lot# 1543141 | Liquid 1. (2-HEMA) (25–50%); BIS-GMA (25–50%); HEDMA (10–25%); Acidic adhesive monomer (5–10%); UDMA (5–10%); catalysts (≤2.5%), silica nanoparticles; Liquid 2. Ethanol (50–100%); Initiator (2.5–5%); catalysts (≤2.5) pH = 2.3 |
| Vococid (Voco, Cuxhaven, Germany) Lot# 152135 | 35% orthophosphoric acid, water, synthetic amorphous silica, polyethylene glycol, aluminum oxide |
| Adhese Universal (ADU) (Ivoclar Vivadent AG,Liechtenstein) Lot# U35131 | Liquid: 2-HEMA (10 -< 25%); Bis-GMA (10 -< 25%); ethanol (10 -< 25%); 1,10-decandiol dimethacrylate (3 -< 10%); Methacrylated phosphoric acid ester (3 -< 10%); camphorquinone (1 -< 2.5%); 2-dimethylaminoethyl methacrylate (1 -<2.5%); 2-dimethylaminoethyl methacrylate (0.1 -< 2.5%). pH = 2.5–3.0 |
| Admira Fusion (Voco, Cuxhaven, Germany) Lot# (Shade A1, A2, A3, A3,5) 1508270, 150827, 1510508, 1509381 | Ormocer composite resin (organically modified ceramics, according to the respective manufacturer); camphorquinone, amine, BHT, classical silica particles (20–40 nm), Ba-Al-Si glass (1 μm), iron oxide, titanium dioxide |
| Research groups: Adhesive-adhesion mode | Application Procedures |
| FBDC-SE (Control group) | Mixture Liquid 1 into Liquid 2 (1:1 ratio). Apply and rub this homogeneous mixture to enamel and dentine for 20 s; Air-blow for 5 s; light cure (1000 mW/cm2) for 20 s. |
| FBDC-SE-EE (Control group) | Apply etchant selectively on enamel and leave for 30 s. Thoroughly rinse for 1 min and gently dry. Dentine surface must remain slightly wet. Mixture Liquid 1 into Liquid 2 (1:1 ratio). Apply and rub this homogeneous mixture to enamel and dentine for 20 s; Air-blow for 5 s; light cure (1000 mW/cm2) for 20 s. |
| FBU-ER | Apply etchant for 30 s on enamel and 15 s on dentine; Thoroughly rinse for 1 min and gently dry. Dentine surface remains with a silky matt appearance. Apply and rub adhesive for 20 s, and air-blow for 5 s; light-cured (1000 mW/cm2) for 20 s. |
| FBU-SE | Apply and rub adhesive for 20 s, and air-blow for 5 s; light-cured (1000 mW/cm2) for 20 s. |
| ADU-ER | Apply etchant for 30 s on enamel and 15 s on dentine; Thoroughly rinse for 1 min and gently dry. Dentine surface remains dry. Scrubbed adhesive for at least 20 s; Air-blow to disperse adhesive until a glossy, immobile film layer result; Light-cure (1000 mW/cm2) for 20 s. |
| ADU-SE | Scrubbed adhesive for at least 20 s; Air-blow to disperse adhesive until a glossy, immobile film layer result; Light-cure (1000 mW/cm2) for 20 s. |
| Participants/NCCLs’ Characteristicsat Baseline | ALL | FBDC SE | FBDC SE-EE | FBU ER | FBU SE | ADU ER | ADU SE | p ** | |
|---|---|---|---|---|---|---|---|---|---|
| Age | n | 38 | 35 | 35 | 35 | 35 | 35 | 35 | |
| Me (P25–P75) | 56 (41–59) | 56 (41–60) | 56 (43–59) | 55 (41–58) | 56 (43–59) | 56 (40–60) | 56 (41–60) | 0.999 | |
| min–max | 24–63 | 24–63 | 24–63 | 24–63 | 24–63 | 24–63 | 24–63 | ||
| Gender | Female | 17 (44.7%) | 15 (42.9%) | 16 (45.7%) | 16 (45.7%) | 16 (45.7%) | 14 (40%) | 14 (40%) | 0.990 |
| Male | 21 (55.3%) | 20 (57.1%) | 19 (54.3%) | 19 (54.3%) | 19 (54.3%) | 21 (60%) | 21 (60%) | ||
| Smoking habits | No | 32 (84.2%) | 30 (85.7%) | 30 (85.7%) | 30 (85.7%) | 30 (85.7%) | 29 (82.9%) | 30 (85.7%) | 0.999 |
| Yes | 6 (15.8%) | 5 (14.3%) | 5 (14.3%) | 5 (14.3%) | 5 (14.3%) | 6 (17.1%) | 5 (14.3%) | ||
| Oral hygiene [30] | Very Good | 25 (65.8%) | 23 (65.7%) | 25 (71.4%) | 25 (71.4%) | 24 (68.6%) | 23 (65.7%) | 22 (62.9%) | 0.966 |
| Good | 13 (34.2%) | 12 (34.3%) | 10 (28.6%) | 10 (28.6%) | 11 (31.4%) | 12 (34.3%) | 13 (37.1%) | ||
| Number of cigarettes for smokers | n | 6 | 5 | 5 | 5 | 5 | 6 | 5 | |
| Me (P25–P75) | 14 (5.3–20) | 15 (9.5–20) | 13 (4.5–17.5) | 13 (4.5–17.5) | 13 (4.5–17.5) | 14 (5.3–20) | 15 (4.5–20) | 0.943 | |
| min-max | 3–20 | 6–20 | 3–20 | 3–20 | 3–20 | 3–20 | 3–20 | ||
| Tooth type, n (%) | |||||||||
| Pre-molar tooth | 176 (83.8%) | 29 (82.9%) | 32 (91.4%) | 32 (91.4%) | 27 (77.1%) | 30 (85.7%) | 26 (74.3%) | 0.252 | |
| Molar tooth | 34 (16.2%) | 6 (17.1%) | 3 (8.6%) | 3 (8.6%) | 8 (22.9%) | 5 (14.3%) | 9 (25.7%) | ||
| Degree of dentin sclerosis [32] n (%) * | |||||||||
| Degree 1 | 146 (69.5%) | 29 (82.9%) | 24 (68.6%) | 26 (74.3%) | 20 (57.1%) | 23 (65.7%) | 24 (68.6%) | 0.353 | |
| Degree 2 | 35 (16.7%) | 4 (11.4%) | 7 (20%) | 5 (14.3%) | 7 (20%) | 5 (14.3%) | 7 (20%) | ||
| Degree 3, | 8 (3.8%) | 0 (0%) | 1 (2.9%) | 0 (0%) | 3 (8.6%) | 4 (11.4%) | 0 (0%) | ||
| Degree 4 | 21 (10%) | 2 (5.7%) | 3 (8.6%) | 4 (11.4%) | 5 (14.3%) | 3 (8.6%) | 4 (11.4%) | ||
| Cavity geometry (internal shape angle, °) [19] n(%) | |||||||||
| Acute (<45°) | 84 (40%) | 13 (37.1%) | 17 (48.6%) | 14 (40%) | 14 (40%) | 15 (42.9%) | 11 (31.4%) | 0.903 | |
| Acute-to-Right (45–90°) | 60 (28.6%) | 9 (25.7%) | 11 (31.4%) | 11 (31.4%) | 9 (25.7%) | 8 (22.9%) | 12 (34.3%) | ||
| Obtuse (>90°) | 66 (31.4%) | 13 (37.1%) | 7 (20%) | 10 (28.6%) | 12 (34.3%) | 12 (34.3%) | 12 (34.3%) | ||
| FDI Criteria/Score | Restorations (n) at Baseline and 2-Year Follow-Up | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| FBDC-SE | FBDC-SE-EE | FBU-ER | FBU-SE | ADU-ER | ADU-SE | ||||||||
| Base | 2y | Base | 2y | Base | 2y | Base | 2y | Base | 2y | Base | 2y | ||
| Staining margin | EX | 35 | 26 | 35 | 29 | 35 | 28 | 35 | 28 | 35 | 29 | 35 | 30 |
| GO | - | 2 | - | - | - | - | - | 1 | - | - | - | 1 | |
| SS | - | - | - | 1 | - | 1 | - | 1 | - | 1 | - | 2 | |
| UNS | - | - | - | - | - | - | - | - | - | 1 | - | - | |
| Fractures and Retention | EX | 35 | 28 | 35 | 29 | 35 | 29 | 35 | 27 * | 35 | 31 | 35 | 32 |
| GO | - | - | - | - | - | - | - | 2 * | - | - | - | 1 | |
| SS | - | - | - | - | - | - | - | - | - | - | - | - | |
| UNS | - | - | - | 1 | - | - | - | 1 * | - | - | - | - | |
| PO | - | 1 | - | 1 | - | 2 | - | 1 * | - | - | - | - | |
| Marginal Adaptation | EX | 31 | 20 * | 33 | 29 | 33 | 24 * | 28 | 24 * | 32 | 26 * | 33 | 27 * |
| GO | 4 | 5 * | 2 | - | 2 | 3 * | 7 | 3 * | 3 | 3 * | 2 | 2 * | |
| SS | - | 3 * | - | 1 | - | 2 * | - | 3 * | - | 2 * | - | 4 * | |
| UNS | - | - | - | - | - | - | - | - | - | - | - | ||
| Postoperative (Hiper-) sensitivity | EX | 35 | 28 | 35 | 28 | 35 | 29 | 35 | 28 | 34 | 30 | 34 | 32 |
| GO | - | - | - | 2 | - | - | - | 2 | 1 | 1 | 1 | 1 | |
| Recurrence of Caries | EX | 35 | 28 | 35 | 29 | 35 | 29 | 35 | 29 | 35 | 31 | 35 | 33 |
| GO | - | - | - | - | - | - | - | 1 | - | - | - | - | |
| SS | - | - | - | - | - | - | - | - | - | - | - | - | |
| UNS | - | - | - | 1 | - | - | - | - | - | - | - | - | |
| Primary Outcome NCCLrestorations’ Performance | SE Mode | SE-EE/ER Modes | Adhesives | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| FBDC vs. FBU | FBDC vs. ADU | FBU vs. ADU | FBDC vs. FBU | FBDC vs. ADU | FBU vs. ADU | FBDC vs. FBU | FBDC vs. ADU | FBU vs. ADU | ||
| Overall Clinical performance | 0.925 | 0.037 | 0.041 | 1.000 | 0.300 | 0.300 | 0.947 | 0.027 | 0.029 | |
| Esthetic success rate | 1.000 | 1.000 | 1.000 | 1.000 | 0.325 | 1.000 | 1.000 | 0.333 | 0.325 | |
| Functional success rate | 0.767 | 0.074 | 0.040 | 1.000 | 0.078 | 1.000 | 0.791 | 0.012 | 0.007 | |
| Biological success rate | 1.000 | 1.000 | 1.000 | 0.317 | 0.310 | 1.000 | 0.310 | 0.302 | 1.000 | |
| Retention rate | 0.953 | 0.074 | 0.079 | 0.650 | 0.154 | 0.078 | 0.791 | 0.022 | 0.012 | |
| Secondary Outcome Participants/NCCLs characteristics | SE mode | SE-EE/ER modes | FBDC | FBU | ADU | |||||
| Age | ≤56 vs. >56 y | 0.129 | 0.752 | 0.204 | 0.023 | 0.191 | ||||
| Gender | Fem. Vs. Masc. | 0.831 | 0.479 | 0.463 | 0.948 | 0.429 | ||||
| Smoking Habits | No vs. Yes | 0.965 | 0.283 | 0.859 | 0.303 | 0.670 | ||||
| Oral Hygiene [30] | Very Good vs. Good | 0.965 | 0.283 | 0.610 | 0.846 | 0.206 | ||||
| Tooth type | Pre-molar vs. Molar | 0.857 | 0.383 | 0.966 | 0.914 | 0.634 | ||||
| Dentin Sclerosis [32] | Degree * 1 vs. Degree 2 | 0.166 | 0.244 | 0.861 | 0.349 | 0.597 | ||||
| Degree 1 vs. Degree 3 | 0.021 | 0.571 | 0.736 | 0.051 | 0.792 | |||||
| Degree 1 vs. Degree 4 | 0.408 | 0.237 | 0.569 | 0.713 | 0.687 | |||||
| Degree 2 vs. Degree 3 | 0.276 | 1.000 | 0.763 | 0.305 | 1.000 | |||||
| Degree 2 vs. Degree 4 | 0.160 | 0.060 | 0.554 | 0.725 | 1.000 | |||||
| Degree 3 vs. Degree 4 | 0.019 | 0.352 | 0.655 | 0.219 | 1.000 | |||||
| Cavity geometry (internal shape angle) [19] | Acute vs. Acute-to-Right | 0.619 | 0.152 | 0.781 | 0.113 | 1.000 | ||||
| Acute vs. Obtuse | 0.272 | 0.284 | 0.155 | 0.476 | 0.317 | |||||
| Acute-to-Right vs. Obtuse | 0.137 | 0.033 | 0.143 | 0.037 | 0.363 | |||||
| Retention Rate | ||||||||||
| Age | ≤56 vs. >56 y | 0.135 | 0.479 | 0.406 | 0.071 | 1.000 | ||||
| Gender | Fem. vs. Masc. | 0.717 | 0.961 | 0.966 | 0.599 | 1.000 | ||||
| Smoking Habits | No vs. Yes | 0.331 | 0.372 | 0.392 | 0.345 | 1.000 | ||||
| Oral Hygiene | Very Good vs. Good | 0.485 | 0.702 | 0.196 | 0.933 | 1.000 | ||||
| Tooth type | Pre-molar vs. Molar | 0.748 | 0.468 | 0.662 | 0.282 | 1.000 | ||||
| Dentin Sclerosis | Degree 1 vs. Degree 2 | 0.299 | 0.305 | 0.954 | 0.902 | 1.000 | ||||
| Degree 1 vs. Degree 3 | 0.007 | 0.618 | 0.769 | 0.049 | 1.000 | |||||
| Degree 1 vs. Degree 4 | 0.484 | 0.658 | 0.511 | 0.705 | 1.000 | |||||
| Degree 2 vs. Degree 3 | 0.154 | 1.000 | 0.763 | 0.133 | 1.000 | |||||
| Degree 2 vs. Degree 4 | 0.260 | 0.192 | 0.500 | 0.219 | 1.000 | |||||
| Deg 3 vs. Deg 4 | 0.019 | 0.527 | 1.000 | 0.219 | 1.000 | |||||
| Cavity geometry (internal shape angle) | Acute vs. Acute-to-Right | 0.643 | 0.151 | 0.775 | 0.116 | 1.000 | ||||
| Acute vs. Obtuse | 0.681 | 0.932 | 0.659 | 0.759 | 1.000 | |||||
| Acute-to-Right vs. Obtuse | 0.394 | 0.139 | 0.508 | 0.075 | 1.000 | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Manarte-Monteiro, P.; Domingues, J.; Teixeira, L.; Gavinha, S.; Manso, M.C. Universal Adhesives and Adhesion Modes in Non-Carious Cervical Restorations: 2-Year Randomised Clinical Trial. Polymers 2022, 14, 33. https://doi.org/10.3390/polym14010033
Manarte-Monteiro P, Domingues J, Teixeira L, Gavinha S, Manso MC. Universal Adhesives and Adhesion Modes in Non-Carious Cervical Restorations: 2-Year Randomised Clinical Trial. Polymers. 2022; 14(1):33. https://doi.org/10.3390/polym14010033
Chicago/Turabian StyleManarte-Monteiro, Patricia, Joana Domingues, Liliana Teixeira, Sandra Gavinha, and Maria Conceição Manso. 2022. "Universal Adhesives and Adhesion Modes in Non-Carious Cervical Restorations: 2-Year Randomised Clinical Trial" Polymers 14, no. 1: 33. https://doi.org/10.3390/polym14010033