Comparison of Titanium and PEEK Medical Plastic Implant Materials for Their Bacterial Biofilm Formation Properties
Abstract
:1. Introduction
2. Materials and Methods
2.1. PEEK and Titanium Implant Preparation
2.2. Saliva Contamination
2.3. Bacterial Suspension Preparation and Biofilm Formation
2.4. Enumeration of Adhered Bacteria
2.5. Statistical Analysis
2.6. Preparation of Samples for Scanning Electron Microscopy (SEM)
3. Results
Bacterial Adhesion and Biofilm Formation
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gellrich, N.C.; Eckstein, F.M.; Lentge, F.; Zeller, A.N.; Korn, P. Complex Reconstructions in the Facial and Cranial Regions. Unfallchirurg 2021, 124, 807–816. [Google Scholar] [CrossRef] [PubMed]
- Lovald, S.; Kurtz, S.M. Applications of Polyetheretherketone in Trauma, Arthroscopy, and Cranial Defect Repair. In PEEK Biomaterials Handbook; William Andrew Publishing: Oxford, UK, 2012; pp. 243–260. [Google Scholar] [CrossRef]
- Ma, R.; Tang, T. Current Strategies to Improve the Bioactivity of PEEK. Int. J. Mol. Sci. 2014, 15, 5426. [Google Scholar] [CrossRef] [PubMed]
- Skirbutis, G.; Dzingutė, A.; Masiliūnaitė, V.; Šulcaitė, G.; Žilinskas, J. A Review of PEEK Polymer’s Properties and Its Use in Prosthodontics. Balt. Dent. Maxillofac. J. 2017, 19, 19–23. [Google Scholar]
- Ma, H.; Suonan, A.; Zhou, J.; Yuan, Q.; Liu, L.; Zhao, X.; Lou, X.; Yang, C.; Li, D.; Zhang, Y. Gang PEEK (Polyether-Ether-Ketone) and Its Composite Materials in Orthopedic Implantation. Arab. J. Chem. 2021, 14, 102977. [Google Scholar] [CrossRef]
- Stratton-Powell, A.A.; Pasko, K.M.; Brockett, C.L.; Tipper, J.L. The Biologic Response to Polyetheretherketone (PEEK) Wear Particles in Total Joint Replacement: A Systematic Review. Clin. Orthop. Relat. Res. 2016, 474, 2394–2404. [Google Scholar] [CrossRef] [PubMed]
- Papathanasiou, I.; Kamposiora, P.; Papavasiliou, G.; Ferrari, M. The Use of PEEK in Digital Prosthodontics: A Narrative Review. BMC Oral Health 2020, 20, 217. [Google Scholar] [CrossRef]
- Kurtz, S.M.; Devine, J.N. PEEK Biomaterials in Trauma, Orthopedic, and Spinal Implants. Biomaterials 2007, 28, 4845. [Google Scholar] [CrossRef]
- Goharian, A.; Abdullah, M.R.; Kadir, M.R.A. Bioinert Polymers (Polyetheretherketone). In Trauma Plating Systems: Biomechanical, Material, Biological, and Clinical Aspects; Elsevier: Oxford, UK, 2017; pp. 159–179. [Google Scholar] [CrossRef]
- Gerbino, G.; Zavattero, E.; Zenga, F.; Bianchi, F.A.; Garzino-Demo, P.; Berrone, S. Primary and Secondary Reconstruction of Complex Craniofacial Defects Using Polyetheretherketone Custom-Made Implants. J. Cranio-Maxillofac. Surg. 2015, 43, 1356–1363. [Google Scholar] [CrossRef]
- Alonso-Rodriguez, E.; Cebrián, J.L.; Nieto, M.J.; del Castillo, J.L.; Hernández-Godoy, J.; Burgueño, M. Polyetheretherketone Custom-Made Implants for Craniofacial Defects: Report of 14 Cases and Review of the Literature. J. Cranio-Maxillofac. Surg. 2015, 43, 1232–1238. [Google Scholar] [CrossRef]
- Jiang, C.P.; Cheng, Y.C.; Lin, H.W.; Chang, Y.L.; Pasang, T.; Lee, S.Y. Optimization of FDM 3D printing parameters for high strength PEEK using the Taguchi method and experimental validation. Rapid Prototyp. J. 2022, 28, 1260–1271. [Google Scholar] [CrossRef]
- Alageel, O. Three-dimensional printing technologies for dental prosthesis: A review. Rapid Prototyp. J. 2022. ahead-of-print. [Google Scholar] [CrossRef]
- Sarfraz, S.; Mäntynen, P.-H.; Laurila, M.; Suojanen, J.; Saarnio, J.; Rossi, S.; Horelli, J.; Kaakinen, M.; Leikola, J.; Reunanen, J. Effect of Surface Tooling Techniques of Medical Titanium Implants on Bacterial Biofilm Formation In Vitro. Materials 2022, 15, 3228. [Google Scholar] [CrossRef]
- Krätzig, T.; Mende, K.C.; Mohme, M.; von Kroge, S.; Stangenberg, M.; Dreimann, M.; Westphal, M.; Weisselberg, S.; Eicker, S.O. Bacterial Adhesion Characteristics on Implant Materials for Intervertebral Cages: Titanium or PEEK for Spinal Infections? Eur. Spine J. 2021, 30, 1774–1782. [Google Scholar] [CrossRef]
- Gu, X.; Sun, X.; Sun, Y.; Wang, J.; Liu, Y.; Yu, K.; Wang, Y.; Zhou, Y. Bioinspired Modifications of PEEK Implants for Bone Tissue Engineering. Front. Bioeng. Biotechnol. 2021, 8, 1508. [Google Scholar] [CrossRef]
- Lethaus, B.; Safi, Y.; ter Laak-Poort, M.; Kloss-Brandstätter, A.; Banki, F.; Robbenmenke, C.; Steinseifer, U.; Kessler, P. Cranioplasty with Customized Titanium and PEEK Implants in a Mechanical Stress Model. J. Neurotrauma 2012, 29, 1077–1083. [Google Scholar] [CrossRef]
- Owens, C.D.; Stoessel, K. Surgical Site Infections: Epidemiology, Microbiology and Prevention. J. Hosp. Infect. 2008, 70, 3–10. [Google Scholar] [CrossRef]
- Lenguerrand, E.; Whitehouse, M.R.; Beswick, A.D.; Jones, S.A.; Porter, M.L.; Blom, A.W. Revision for Prosthetic Joint Infection Following Hip Arthroplasty: Evidence from the National Joint Registry. Bone Jt. Res. 2017, 6, 391. [Google Scholar] [CrossRef]
- Webster, T.J.; Patel, A.A.; Rahaman, M.N.; Sonny Bal, B. Anti-Infective and Osteointegration Properties of Silicon Nitride, Poly(Ether Ether Ketone), and Titanium Implants. Acta Biomater. 2012, 8, 4447–4454. [Google Scholar] [CrossRef]
- Bock, R.M.; Jones, E.N.; Ray, D.A.; Sonny Bal, B.; Pezzotti, G.; McEntire, B.J. Bacteriostatic Behavior of Surface Modulated Silicon Nitride in Comparison to Polyetheretherketone and Titanium. J. Biomed. Mater. Res. A 2017, 105, 1521–1534. [Google Scholar] [CrossRef] [PubMed]
- Järvinen, S.; Suojanen, J.; Kormi, E.; Wilkman, T.; Kiukkonen, A.; Leikola, J.; Stoor, P. The Use of Patient Specific Polyetheretherketone Implants for Reconstruction of Maxillofacial Deformities. J. Craniomaxillofac. Surg. 2019, 47, 1072–1076. [Google Scholar] [CrossRef] [PubMed]
- Rochford, E.T.J.; Sabaté Brescó, M.; Poulsson, A.H.C.; Kluge, K.; Zeiter, S.; Ziegler, M.; O’Mahony, L.; Richards, R.G.; Moriarty, T.F. Infection Burden and Immunological Responses Are Equivalent for Polymeric and Metallic Implant Materials in Vitro and in a Murine Model of Fracture-Related Infection. J. Biomed. Mater. Res. B Appl. Biomater. 2019, 107, 1095–1106. [Google Scholar] [CrossRef] [PubMed]
- Suojanen, J.; Järvinen, S.; Hodzic, Z.; Reunanen, J.; Leikola, J.; Stoor, P. No Differences in Infections between Patient-Specific Implants and Conventional Mini-Plates in Mandibular Bilateral Sagittal Split Osteotomy-Up to 3-Year Follow-Up. J. Craniomaxillofac. Surg. 2019, 47, 1181–1184. [Google Scholar] [CrossRef]
- Suojanen, J.; Järvinen, S.; Kotaniemi, K.V.; Reunanen, J.; Palotie, T.; Stoor, P.; Leikola, J. Comparison between Patient Specific Implants and Conventional Mini-Plates in Le Fort I Osteotomy with Regard to Infections: No Differences in up to 3-Year Follow-Up. J. Craniomaxillofac. Surg. 2018, 46, 1814–1817. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Tian, W.; Chen, J.; Yu, J.; Zhang, J.; Chen, J. The Application of Polyetheretherketone (PEEK) Implants in Cranioplasty. Brain Res. Bull. 2019, 153, 143–149. [Google Scholar] [CrossRef]
- Rosenthal, G.; Ng, I.; Moscovici, S.; Lee, K.K.; Lay, T.; Martin, C.; Manley, G.T. Polyetheretherketone Implants for the Repair of Large Cranial Defects: A 3-Center Experience. Neurosurgery 2014, 75, 523–528. [Google Scholar] [CrossRef]
- Punchak, M.; Chung, L.K.; Lagman, C.; Bui, T.T.; Lazareff, J.; Rezzadeh, K.; Jarrahy, R.; Yang, I. Outcomes Following Polyetheretherketone (PEEK) Cranioplasty: Systematic Review and Meta-Analysis. J. Clin. Neurosci. 2017, 41, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Kwarcinski, J.; Boughton, P.; Ruys, A.; Doolan, A.; van Gelder, J. Cranioplasty and Craniofacial Reconstruction: A Review of Implant Material, Manufacturing Method and Infection Risk. Appl. Sci. 2017, 7, 276. [Google Scholar] [CrossRef]
- Koper, D.; ter Laak-Poort, M.; Lethaus, B.; Yamauchi, K.; Moroni, L.; Habibovic, P.; Kessler, P. Cranioplasty with Patient-Specific Implants in Repeatedly Reconstructed Cases. J. Craniomaxillofac. Surg. 2019, 47, 709–714. [Google Scholar] [CrossRef] [PubMed]
- Barkarmo, S.; Longhorn, D.; Leer, K.; Johansson, C.B.; Stenport, V.; Franco-Tabares, S.; Kuehne, S.A.; Sammons, R. Biofilm Formation on Polyetheretherketone and Titanium Surfaces. Clin. Exp. Dent. Res. 2019, 5, 427–437. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kunrath, M.F.; Dahlin, C. The Impact of Early Saliva Interaction on Dental Implants and Biomaterials for Oral Regeneration: An Overview. Int. J. Mol. Sci. 2022, 23, 2024. [Google Scholar] [CrossRef] [PubMed]
- Rudney, J.D.; Hickey, K.L.; Ji, Z. Cumulative Correlations of Lysozyme, Lactof Errin, Peroxidase, S-IgA, Amylase, and Total Protein Concentrations with Adherence of Oral Viridans Streptococci to Microplates Coated with Human Saliva. J. Dent. Res. 1999, 78, 759–768. [Google Scholar] [CrossRef]






| PEEK | Titanium | |
|---|---|---|
| Price for Single Piece Product | ~2000–2500 € | ~2000–2500 € |
| Material cost (% of total costs) | 30% | 20% |
| Virtual surgical planning core service including engineering and tooling service (% of total costs) | 70% | 80% |
| Relative material costs | 4 | 1 |
| Mechanical Characteristics | ||
| Compressive strength | + 1 | + |
| Bending stress | − 2 | + |
| Puzzle-type design (multiple pieces) | + | − |
| Undermining structures possible | − | + |
| Radio-opacity | minor | significant |
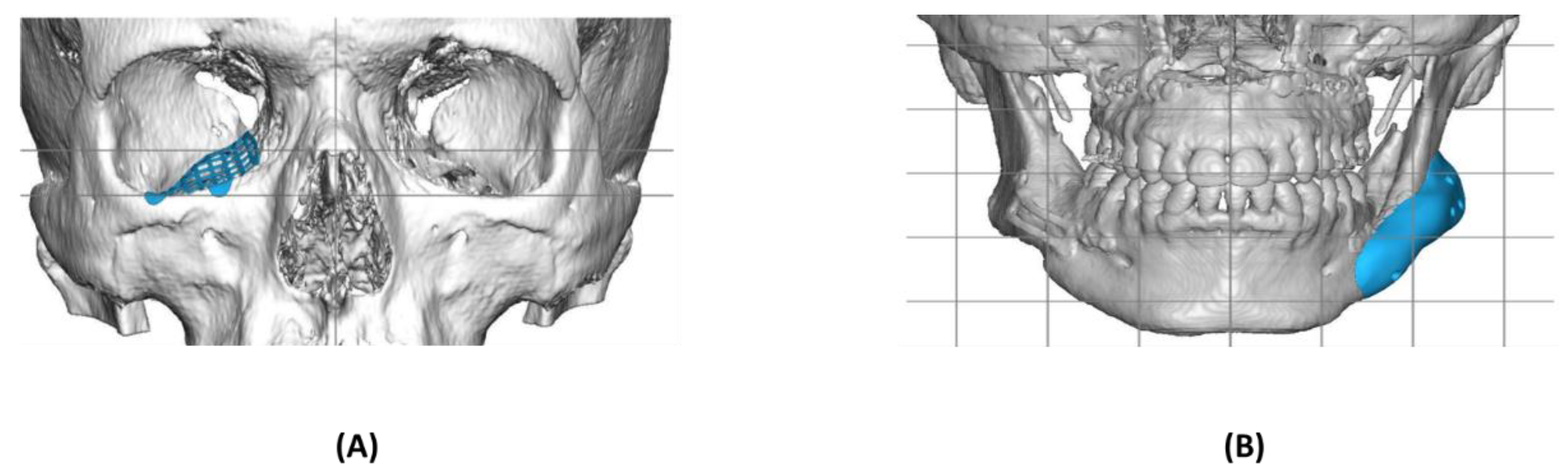
| Clinical Applications | Puzzle-type structures (e.g., orbita) | Large defects |
| Contour facial implants | Contour implants | |
| Cranial defects | Trauma | |
| Osteosynthesis |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sarfraz, S.; Mäntynen, P.-H.; Laurila, M.; Rossi, S.; Leikola, J.; Kaakinen, M.; Suojanen, J.; Reunanen, J. Comparison of Titanium and PEEK Medical Plastic Implant Materials for Their Bacterial Biofilm Formation Properties. Polymers 2022, 14, 3862. https://doi.org/10.3390/polym14183862
Sarfraz S, Mäntynen P-H, Laurila M, Rossi S, Leikola J, Kaakinen M, Suojanen J, Reunanen J. Comparison of Titanium and PEEK Medical Plastic Implant Materials for Their Bacterial Biofilm Formation Properties. Polymers. 2022; 14(18):3862. https://doi.org/10.3390/polym14183862
Chicago/Turabian StyleSarfraz, Sonia, Pilvi-Helinä Mäntynen, Marisa Laurila, Sami Rossi, Junnu Leikola, Mika Kaakinen, Juho Suojanen, and Justus Reunanen. 2022. "Comparison of Titanium and PEEK Medical Plastic Implant Materials for Their Bacterial Biofilm Formation Properties" Polymers 14, no. 18: 3862. https://doi.org/10.3390/polym14183862
APA StyleSarfraz, S., Mäntynen, P.-H., Laurila, M., Rossi, S., Leikola, J., Kaakinen, M., Suojanen, J., & Reunanen, J. (2022). Comparison of Titanium and PEEK Medical Plastic Implant Materials for Their Bacterial Biofilm Formation Properties. Polymers, 14(18), 3862. https://doi.org/10.3390/polym14183862





