The Use of Acrylate Polymers in Dentistry
Abstract
1. Introduction
2. Use of Acrylate Polymers in Dentistry
3. Types of Acrylate Polymers in Dentistry
4. Composition of Dental Acrylate Polymers
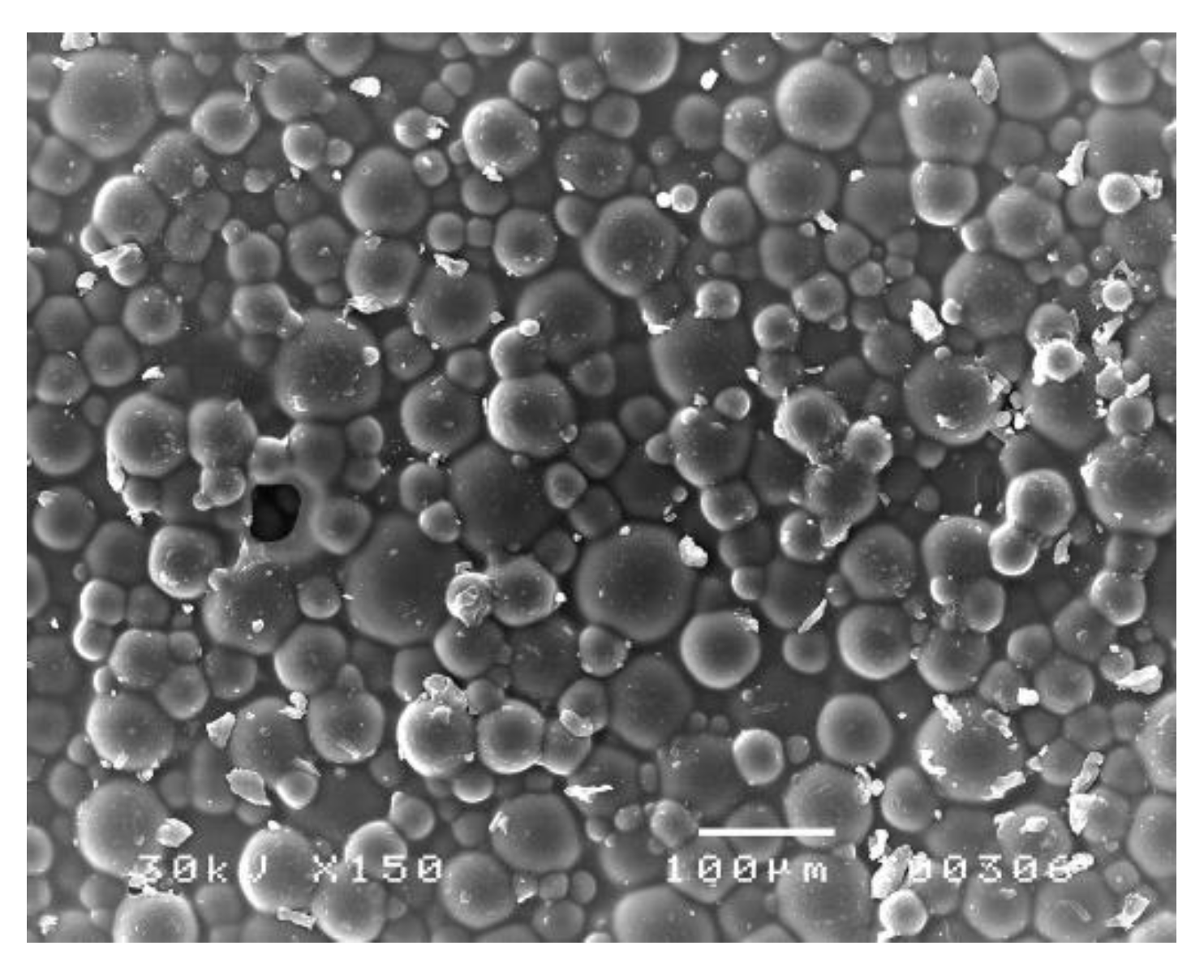
5. Physico-Mechanical Properties of Dental Acrylate Polymers
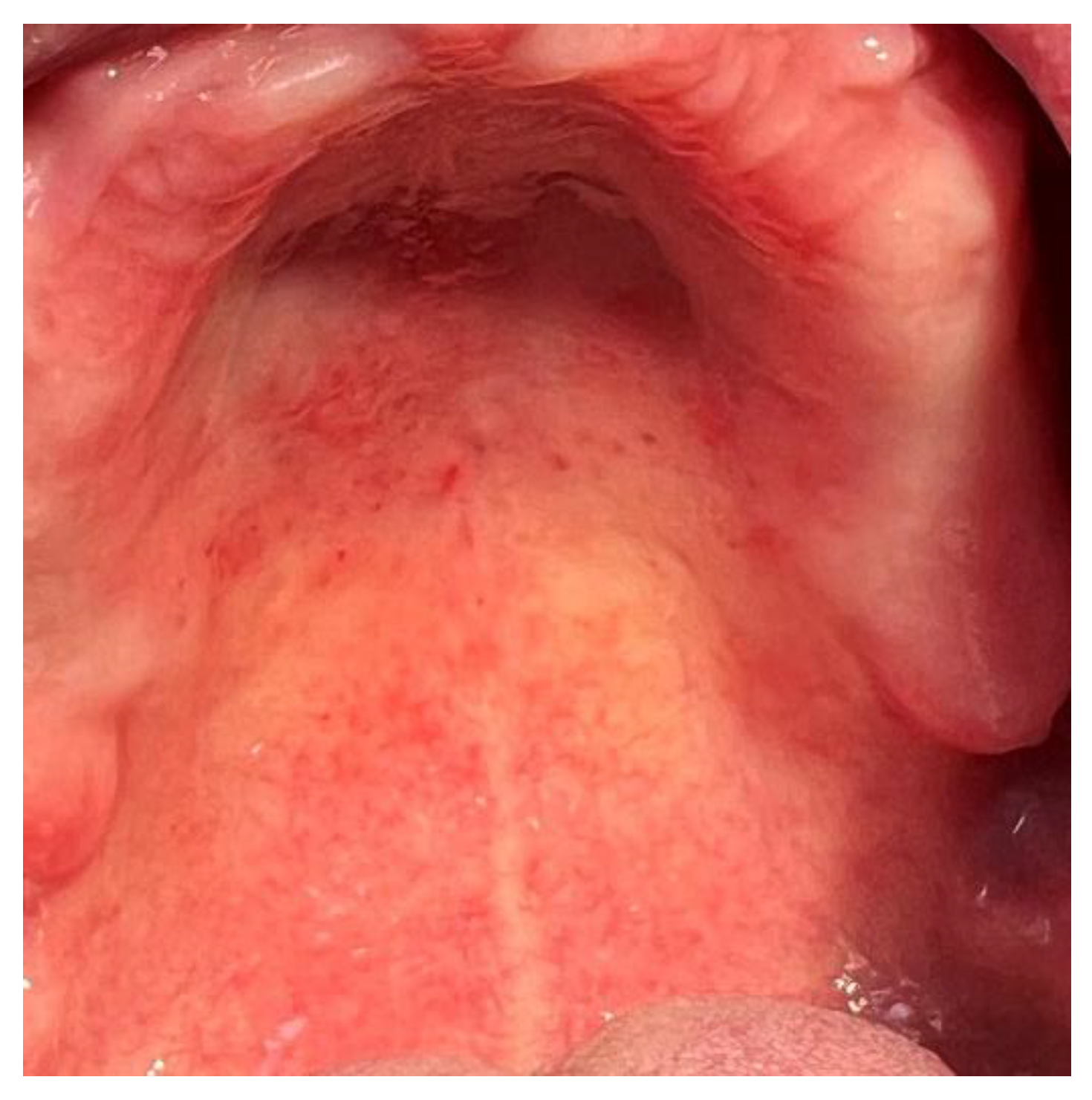
6. Biofilm on the Surface of Dental Acrylate Polymers
7. Release of Potentially Toxic Substances
8. Release of Residual Monomer
9. Other Potentially Toxic Substances
10. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Raszewski, Z.; Nowakowska-Toporowska, A.; Nowakowska, D.; Więckiewicz, W. Update on Acrylic Resins Used in Dentistry. Mini-Rev. Med. Chem. 2021, 21, 2130–2137. [Google Scholar] [CrossRef] [PubMed]
- Strang, R.; Whitters, C.; Brown, D.; Clarke, R.L.; Curtis, R.; Hatton, P.; Ireland, A.; Lloyd, C.; McCabe, J.; Nicholson, J.; et al. Dental materials: 1996 literature review. Part 2. J. Dent. 1998, 26, 273–291. [Google Scholar] [CrossRef]
- Gad, M.M.; Fouda, S.M.; Al-Harbi, F.A.; Näpänkangas, R.; Raustia, A. PMMA denture base material enhancement: A review of fiber, filler, and nanofiller addition. Int. J. Nanomed. 2017, 12, 3801–3812. [Google Scholar] [CrossRef] [PubMed]
- Zafar, M.S. Prosthodontic Applications of Polymethyl Methacrylate (PMMA): An Update. Polymers 2020, 12, 2299. [Google Scholar] [CrossRef] [PubMed]
- Kostic, M.; Pejcic, A.; Igic, M.; Gligorijević, N. Adverse reactions to denture resin materials. Eur. Rev. Med. Pharmacol. Sci. 2017, 21, 5298–5305. [Google Scholar]
- Mousavi, S.M.; Low, F.W.; Hashemi, S.A.; Lai, C.W.; Ghasemi, Y.; Soroshnia, S.; Savardashtaki, A.; Babapoor, A.; Rumjit, N.P.; Goh, S.M.; et al. Development of graphene based nanocomposites towards medical and biological applications. Artif. Cells Nanomed. Biotechnol. 2020, 48, 1189–1205. [Google Scholar] [CrossRef] [PubMed]
- Mousavi, S.; Zarei, M.; Hashemi, S.; Ramakrishna, S.; Chiang, W.-H.; Lai, C.; Gholami, A.; Omidifar, N.; Shokripour, M. Asymmetric Membranes: A Potential Scaffold for Wound Healing Applications. Symmetry 2020, 12, 1100. [Google Scholar] [CrossRef]
- Mousavi, S.-M.; Nejad, Z.M.; Hashemi, S.A.; Salari, M.; Gholami, A.; Ramakrishna, S.; Chiang, W.-H.; Lai, C.W. Bioactive Agent-Loaded Electrospun Nanofiber Membranes for Accelerating Healing Process: A Review. Membranes 2021, 11, 702. [Google Scholar] [CrossRef]
- Kostić, M.; Nikolić, L. Contemporary dental materials. Adv. Technol. 2019, 8, 78–85. [Google Scholar] [CrossRef]
- Petrovic, D.; Krunic, N.; Kostic, M. Risk factors and preventive measures for occupational diseases in dental technicians. Vojn. Pregl. 2013, 70, 959–963. [Google Scholar] [CrossRef]
- Frazer, R.Q.; Byron, R.T.; Osborne, P.B.; West, K.P. PMMA: An Essential Material in Medicine and Dentistry. J. Long-Term Eff. Med. Implant. 2005, 15, 629–639. [Google Scholar] [CrossRef] [PubMed]
- Ali, U.; Karim, K.J.B.A.; Buang, N.A. A Review of the Properties and Applications of Poly (Methyl Methacrylate) (PMMA). Polym. Rev. 2015, 55, 678–705. [Google Scholar] [CrossRef]
- ISO 1567; Dentistry: Denture Base Polymers. International Standards Organization: Geneva, Switzerland, 1999.
- Bartoloni, J.A.; Murchison, D.F.; Wofford, D.T.; Sarkar, N.K. Degree of conversion in denture base materials for varied polymerization techniques. J. Oral Rehabilit. 2000, 27, 488–493. [Google Scholar] [CrossRef] [PubMed]
- Memon, M.S.; Yunus, N.; A Razak, A. Some mechanical properties of a highly cross-linked, microwave-polymerized, injection-molded denture base polymer. Int. J. Prosthodont. 2001, 14, 214–218. [Google Scholar] [PubMed]
- Munksgaard, E.C. Plasticizers in denture soft-lining materials: Leaching and biodegradation. Eur. J. Oral Sci. 2005, 113, 166–169. [Google Scholar] [CrossRef]
- Hong, G.; Wang, W.Q.; Sun, L.; Han, J.M.; Sasaki, K. The Dynamic Viscoelasticity of Dental Soft Polymer Material Containing Citrate Ester-Based Plasticizers. Materials 2020, 13, 5078. [Google Scholar] [CrossRef] [PubMed]
- Arima, T.; Murata, H.; Hamada, T. Properties of highly cross-linked autopolymerizing reline acrylic resins. J. Prosthet. Dent. 1995, 73, 55–59. [Google Scholar] [CrossRef]
- Pisani, M.X.; Segundo, A.L.; Leite, V.M.; de Souza, R.F.; da Silva, M.A.; da Silva, C.H. Electromyography of masticatory muscles after denture relining with soft and hard denture liners. J. Oral Sci. 2013, 55, 217–224. [Google Scholar] [CrossRef][Green Version]
- Pfeifer, C.S.; Shelton, Z.R.; Braga, R.R.; Windmoller, D.; Machado, J.C.; Stansbury, J.W. Characterization of dimethacrylate polymeric networks: A study of the crosslinked structure formed by monomers used in dental composites. Eur. Polym. J. 2011, 47, 162–170. [Google Scholar] [CrossRef]
- Kawaguchi, T.; Lassila, L.V.; Tokue, A.; Takahashi, Y.; Vallittu, P.K. Influence of molecular weight of polymethyl(methacrylate) beads on the properties and structure of cross-linked denture base polymer. J. Mech. Behav. Biomed. Mater. 2011, 4, 1846–1851. [Google Scholar] [CrossRef]
- Uzun, G.; Hersek, N. Comparison of the Fracture Resistance of Six Denture Base Acrylic Resins. J. Biomater. Appl. 2002, 17, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Doǧan, A.; Bek, B.; Çevik, N.; Usanmaz, A. The effect of preparation conditions of acrylic denture base materials on the level of residual monomer, mechanical properties and water absorption. J. Dent. 1995, 23, 313–318. [Google Scholar] [CrossRef]
- Leão, R.D.S.; de Moraes, S.L.D.; Gomes, J.M.D.L.; Lemos, C.A.A.; Casado, B.G.D.S.; Vasconcelos, B.C.D.E.; Pellizzer, E.P. Influence of addition of zirconia on PMMA: A systematic review. Mater. Sci. Eng. C 2019, 106, 110292. [Google Scholar] [CrossRef]
- Jagger, D.C.; Harrison, A.; Jandt, K.D. The reinforcement of dentures. J. Oral Rehabilit. 1999, 26, 185–194. [Google Scholar] [CrossRef] [PubMed]
- Azzarri, M.J.; Cortizo, M.S.; Alessandrini, J.L. Effect of curing conditions on the properties of an acrylic denture base resin microwave-polymerized. J. Dent. 2003, 31, 463–468. [Google Scholar] [CrossRef]
- Shlosberg, S.R.; Goodacre, C.J.; A Munoz, C.; Moore, B.K.; Schnell, R.J. Microwave energy polymerization of poly(methyl methacrylate) denture base resin. Int. J. Prosthodont. 1989, 2, 453–458. [Google Scholar]
- Venkat, R.; Gopichander, N.; Vasantakumar, M. Comprehensive Analysis of Repair/Reinforcement Materials for Polymethyl Methacrylate Denture Bases: Mechanical and Dimensional Stability Characteristics. J. Indian Prosthodont. Soc. 2013, 13, 439–449. [Google Scholar] [CrossRef]
- Drago, C.; Borgert, A.J. Comparison of nonscheduled, postinsertion adjustment visits for complete dentures fabricated with conventional and CAD-CAM protocols: A clinical study. J. Prosthet. Dent. 2019, 122, 459–466. [Google Scholar] [CrossRef]
- Alves, P.V.M.; Filho, R.M.A.L.; Telles, E.; Bolognese, A. Surface Roughness of Acrylic Resins after Different Curing and Polishing Techniques. Angle Orthod. 2007, 77, 528–531. [Google Scholar] [CrossRef]
- Blagojevic, V.; Murphy, V.M. Microwave polymerization of denture base materials. A comparative study. J. Oral Rehabilit. 1999, 26, 804–808. [Google Scholar] [CrossRef]
- Jorge, J.H.; Giampaolo, E.T.; Machado, A.L.; Vergani, C.E. Cytotoxicity of denture base acrylic resins: A literature review. J. Prosthet. Dent. 2003, 90, 190–193. [Google Scholar] [CrossRef]
- Kostic, M.; Krunic, N.; Nikolić, L.; Nikolić, V.; Najman, S.; Kocic, J. Residual monomer content determination in some acrylic denture base materials and possibilities of its reduction. Vojn. Pregl. 2009, 66, 223–227. [Google Scholar] [CrossRef] [PubMed]
- Kostić, M.; Krunić, N.; Nikolić, L.; Nikolić, V.; Najman, S.; Kostić, I.; Rajković, J.; Manić, M.; Petković, D. Influence of residual monomer reduction on acrylic denture base resins quality. Hem. Ind. 2011, 65, 171–177. [Google Scholar] [CrossRef][Green Version]
- Lung, S.Y.; Darvell, B.W. Minimization of inevitable residual monomer in denture base acrylic. Dent. Mater 2005, 21, 1119–1128. [Google Scholar] [CrossRef] [PubMed]
- Kostić, M.; Nikolic, L.; Nikolic, V.; Petković, D.; Igić, M.; Krunić, N.; Manić, M.; Gligorijević, N.; Radenković, G. Effects of water boiling, microwave, and water bath post-polymerization on mechanical properties of acrylic denture resins. Hem. Ind. 2018, 72, 129–137. [Google Scholar] [CrossRef]
- Lung, C.; Darvell, B. Methyl methacrylate monomer–polymer equilibrium in solid polymer. Dent. Mater. 2007, 23, 88–94. [Google Scholar] [CrossRef]
- Bubalo, V.; Jerolimov, V.; Baučić, I.; Andreis, M.; Veskli, Z. Akrilatni polimeri u dentalnoj protetici: Procesi razgradnje. Polimeri 2012, 31, 47–53. [Google Scholar]
- Kostić, M.; Petrović, M.; Krunić, N.; Igić, M.; Janošević, P. Comparative analysis of water sorption by different acrylic materials. Acta Med. Median. 2014, 53, 5–9. [Google Scholar] [CrossRef]
- Lovas El Hadary, A.; Drummond, J.L. Comparative study of water sorption, solubility, and tensile bond strength of two soft lining materials. J. Prost. Dent. 2000, 83, 356–361. [Google Scholar] [CrossRef]
- Zissis, A.J.; Polyzois, G.L.; A Yannikakis, S.; Harrison, A. Roughness of denture materials: A comparative study. Int. J. Prosthodont. 2001, 13, 136–140. [Google Scholar]
- Kostić, M.; Krunić, N.; Najman, S.; Nikolić, L.; Nikolić, V.; Rajković, J.; Petrović, M.; Igić, M.; Ignjatović, A. Artificial saliva effect on release of toxic substances from acrylic resins. Vojn. Pregl. 2015, 72, 899–905. [Google Scholar] [CrossRef] [PubMed]
- Bollenl, C.M.; Lambrechts, P.; Quirynen, M. Comparison of surface roughness of oral hard materials to the threshold surface roughness for bacterial plaque retention: A review of the literature. Dent. Mater. 1997, 13, 258–269. [Google Scholar] [CrossRef]
- Kostić, M.; Krunić, N.; Najman, S.; Rajković, J.; Igić, M.; Petrović, M.; Janošević, P. Ispitivanje adherentnosti stomatoloških akrilatnih polimera in vivo. Acta Stomatol. Naissi 2014, 30, 1383–1392. [Google Scholar] [CrossRef]
- Li, Z.; Sun, J.; Lan, J.; Qi, Q. Effect of a denture base acrylic resin containing silver nanoparticles on Candida albicans adhesion and biofilm formation. Gerodontology 2016, 33, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Radford, D.; Challacombe, S.; Walter, J. Denture Plaque and Adherence of Candida Albicans To Denture-Base Materials in Vivo and in Vitro. Crit. Rev. Oral Biol. Med. 1999, 10, 99–116. [Google Scholar] [CrossRef]
- Park, S.E.; Blissett, R.; Susarla, S.M.; Weber, H.-P. Candida albicans Adherence to Surface-Modified Denture Resin Surfaces. J. Prosthodont. 2008, 17, 365–369. [Google Scholar] [CrossRef]
- Samaranayake, Y.H.; Wu, P.C.; Samaranayake, L.P.; So, M. Relationship between the cell surface hydrophobicity and adherence of Candida krusei and Candida albicans to epithelial and denture acrylic surfaces. APMIS 1995, 103, 707–713. [Google Scholar] [CrossRef]
- Minagi, S.; Miyake, Y.; Inagaki, K.; Tsuru, H.; Suginaka, H. Hydrophobic interaction in Candida albicans and Candida tropicalis adherence to various denture base resin materials. Infect. Immun. 1985, 47, 11–14. [Google Scholar] [CrossRef]
- Pereira-Cenci, T.; Cury, A.D.B.; Crielaard, W.; Cate, J.M.T. Development of Candida-associated denture stomatitis: New insights. J. Appl. Oral Sci. 2008, 16, 86–94. [Google Scholar] [CrossRef]
- Zamperini, C.A.; Machado, A.L.; Vergani, C.E.; Pavarina, A.C.; Giampaolo, E.T.; da Cruz, N.C. Adherence in vitro of Candida albicans to plasma treated acrylic resin. Effect of plasma parameters, surface roughness and salivary pellicle. Arch. Oral Biol. 2010, 55, 763–770. [Google Scholar] [CrossRef]
- Köhler, B.; Andréen, I.; Jonsson, B. The earlier the colonization by mutans streptococci, the higher the caries prevalence at 4 years of age. Oral Microbiol. Immunol. 1988, 3, 14–17. [Google Scholar] [CrossRef] [PubMed]
- Gaines, S.; James, T.; Folan, M.; Baird, A.; O’Farrelly, C. A novel spectrofluorometric microassay for Streptococcus mutans adherence to hydroxylapatite. J. Microbiol. Methods 2003, 54, 315–323. [Google Scholar] [CrossRef]
- Gendreau, L.; Loewy, Z.G. Epidemiology and Etiology of Denture Stomatitis. J. Prosthodont. 2011, 20, 251–260. [Google Scholar] [CrossRef] [PubMed]
- Elguezabal, N.; Maza, J.L.; Dorronsoro, S.; Ponton, J. Whole saliva has a dual role on the adherence of Candida albicans to polymethylmethacrylate. Open Dent. J. 2008, 2, 1–4. [Google Scholar]
- Patel, R. Biofilms and Antimicrobial Resistance. Clin. Orthop. Relat. Res. 2005, 437, 41–47. [Google Scholar] [CrossRef]
- Sabzghabaee, A.M.; Shirdare, Z.; Ebadian, B.; Aslani, A.; Ghannadi, A. Clinical evaluation of the essential oil of Pelargonium graveolens for the treatment of denture stomatitis. Dent. Res. J. 2011, 8, S105–S108. [Google Scholar]
- Bueno, M.; Urban, V.; Barbério, G.; Silva, W.; Porto, V.; Pinto, L.; Neppelenbroek, K. Effect of antimicrobial agents incorporated into resilient denture relines on the Candida albicans biofilm. Oral Dis. 2013, 21, 57–65. [Google Scholar] [CrossRef]
- Bueno, M.G.; de Sousa, E.J.B.; Hotta, J.; Porto, V.C.; Urban, V.M.; Neppelenbroek, K.H. Surface Properties of Temporary Soft Liners Modified by Minimum Inhibitory Concentrations of Antifungals. Braz. Dent. J. 2017, 28, 158–164. [Google Scholar] [CrossRef]
- Gligorijević, N.; Mihajlov-Krstev, T.; Kostić, M.; Nikolić, L.; Stanković, N.; Nikolić, V.; Dinić, A.; Igić, M.; Bernstein, N. Antimicrobial Properties of Silver-Modified Denture Base Resins. Nanomaterials 2022, 12, 2453. [Google Scholar] [CrossRef]
- Khurana, C.; Vala, A.K.; Andhariya, N.; Pandey, O.P.; Chudasama, B. Antibacterial activity of silver: The role of hydrodynamic particle size at nanoscale. J. Biomed. Mater. Res. Part A 2013, 102, 3361–3368. [Google Scholar] [CrossRef]
- de Castro, D.T.; Valente, M.L.; da Silva, C.H.; Watanabe, E.; Siqueira, R.L.; Schiavon, M.A.; Alves, O.L.; dos Reis, A.C. Evaluation of antibiofilm and mechanical properties of new nanocomposites based on acrylic resins and silvervanadate nanoparticles. Arch. Oral Biol. 2016, 67, 46–53. [Google Scholar] [CrossRef] [PubMed]
- Gad, M.M.; Al-Thobity, A.M.; Shahin, S.Y.; Alsaqer, B.T.; A Ali, A. Inhibitory effect of zirconium oxide nanoparticles on Candida albicans adhesion to repaired polymethyl methacrylate denture bases and interim removable prostheses: A new approach for denture stomatitis prevention. Int. J. Nanomed. 2017, 12, 5409–5419. [Google Scholar] [CrossRef]
- Obata, T.; Ueda, T.; Sakurai, K. Inhibition of denture plaque by TiO2 coating on denture base resins in the mouth. J. Prosthet. Dent. 2017, 118, 759–764. [Google Scholar] [CrossRef] [PubMed]
- Göcke, R.; Gerath, F.; Von Schwanewede, H. Quantitative determination of salivary components in the pellicle on PMMA denture base material. Clin. Oral Investig. 2002, 6, 227–235. [Google Scholar] [CrossRef]
- Puri, G.; Berzins, D.W.; Dhuru, V.B.; Raj, P.A.; Rambhia, S.K.; Dhir, G.; Dentino, A.R. Effect of phosphate group addition on the properties of denture base resins. J. Prosthet. Dent. 2008, 100, 302–308. [Google Scholar] [CrossRef]
- Park, S.E.; Periathamby, A.R.; Loya, J.C. Effect of surface-charged poly(methyl methacrylate) on adchesio of Candida albicans. J. Prosthodont. 2003, 12, 249–254. [Google Scholar] [CrossRef]
- Petrović, M.; Kostić, M.; Kostić, M.; Krunić, N.; Igić, M.; Pešić, Z.; Otašević, S. Therapeutic alternatives of natural compounds in treatment of Candida–associated denture stomatitis. Acta Med. Median. 2014, 53, 73–79. [Google Scholar]
- Takahashi, Y.; Imazato, S.; Russell, R.; Noiri, Y.; Ebisu, S. Influence of resin monomers on growth of oral streptococci. J. Dent. Res. 2004, 83, 302–306. [Google Scholar] [CrossRef]
- Dahl, J.E.; Frangou-Polyzois, M.J.; Polyzois, G.L. In vitro biocompatibility of denture relining materials. Gerodontology 2006, 23, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Kostić, M.; Najman, S.; Kocić, J.; Krunić, N.; Ajduković, Z.; Petrović, D.; Anđelković, M. Efekat ekstrakata akrilata za bazu pločaste zubne proteze na rast HeLa ćelija in vitro. Hem. Ind. 2008, 62, 217–222. [Google Scholar]
- Huang, F.M.; Tai, K.W.; Hu, C.C.; Chang, Y.C. Citotoxic effects of denture base materials on a permanent human oral epithelial cell line and on primary human oral fibroblasts in vitro. Int. J. Prosthodont. 2001, 14, 439–443. [Google Scholar]
- Cimpan, M.R.; Matre, R.; Cressey, L.I.; Tysnes, B.; Lie, S.A.; Gjertsen, B.T.; Skaug, N. The effect of heat- and auto-polymerized denture base polymers on clonogenicity, apoptosis, and necrosis in fibroblasts: Denture base polymers induce apoptosis and necrosis. Acta Odontol. Scand. 2000, 58, 217–228. [Google Scholar] [PubMed]
- Liu, J.; Wan, L.; Lu, X.; Li, S.; Zhang, J.; Cheng, J. Visualizing living fibroblast on co-cultured denture base resin by green fluorescent protein marker introduced into the cell. J. Biomed. Eng. Shengwu Yixue Gongchengxue Zazhi 2004, 21, 355–358. [Google Scholar]
- Tsuchiya, H.; Hoshino, Y.; Tajima, K.; Takagi, N. Leaching and citotoxicity of formaldehyde and methyl methacrylate from acrylic resins denture base materials. J. Prosthet. Dent. 1994, 71, 618–624. [Google Scholar] [CrossRef]
- Krunic, N.; Nikolić, L.; Kostic, M.; Najman, S.; Nikolić, V.; Najdanovic, J. In vitro examination of oral tissue conditioners potential toxicity. Chem. Ind. 2011, 65, 697–706. [Google Scholar] [CrossRef]
- Austin, A.T.; Basker, R.M. The level of residual monomer in acrylic denture base materials with particular reference to a modified method of analysis. Br. Dent. J. 1980, 149, 281–286. [Google Scholar] [CrossRef]
- Vergani, C.; Seo, R.S.; Pavarina, A.C.; Reis, J.M.D.S.N. Flexural strength of autopolymerizing denture reline resins with microwave postpolymerization treatment. J. Prosthet. Dent. 2005, 93, 577–583. [Google Scholar] [CrossRef]
- Graham, B.; Jones, D.; Sutow, E. An in vivo and in vitro Study of the Loss of Plasticizer from Soft Polymer-gel Materials. J. Dent. Res. 1991, 70, 870–873. [Google Scholar] [CrossRef] [PubMed]
- Gawkrodger, D.J. Investigation of reactions to denatl materials. Br. J. Derm. 2005, 153, 479–485. [Google Scholar] [CrossRef]
- Yoshii, E. Cytotoxic effects of acrylates and methacrylates: Relationships of monomer structures and cytotoxicity. J. Biomed. Mater. Res. 1997, 37, 517–524. [Google Scholar] [CrossRef]
- Lefebvre, C.; Schuster, G.; Rueggeberg, F.; Tamare-Selvy, K.; Knoernschild, K. Responses of oral epithelial cells to dental resin components. J. Biomater. Sci. Polym. Ed. 1996, 7, 965–976. [Google Scholar] [CrossRef] [PubMed]
- Miettinen, V.M.; Vallittu, P.K.; Docent, D.T. Water sorption and solubility of glass fiber-reinforced denture polymethyl methacrylate resin. J. Prosthet. Dent. 1997, 77, 531–534. [Google Scholar] [CrossRef]
- Urban, V.; Machado, A.L.; Oliveira, R.; Vergani, C.; Pavarina, A.C.; Cass, Q.B. Residual monomer of reline acrylic resins: Effect of water-bath and microwave post-polymerization treatments. Dent. Mater. 2007, 23, 363–368. [Google Scholar] [CrossRef] [PubMed]
- Harrison, A.; Huggett, R. Effect of the curing cycle on residual monomer levels of acrylic resin denture base polymers. J. Dent. 1992, 20, 370–374. [Google Scholar] [CrossRef]
- Takamata, T.; Setcos, J.C. Resin denture bases: Review of accuracy and methods of polymerization. Int. J. Prosthodont. 1989, 2, 555–562. [Google Scholar] [PubMed]
- Jorge, J.H.; Giampaolo, E.T.; Vergani, C.E.; Machado, A.L.; Pavarina, A.C.; Carlos, I.Z. Biocompatibility of denture base acrylic resins evaluated in culture of L929 cells. Effect of polymerisation cycle and post-polymerisation treatments. Gerodontology 2007, 24, 52–57. [Google Scholar] [CrossRef]
- Jorge, J.H.; Quishida, C.C.C.; Vergani, C.E.; Machado, A.L.; Pavarina, A.C.; Giampaolo, E.T. Clinical evaluation of failures in removable partial dentures. J. Oral Sci. 2012, 54, 337–342. [Google Scholar] [CrossRef]
- Alshahrani, F.A.; Al Toraibily, F.; Alzaid, M.; Mahrous, A.A.; Al Ghamdi, M.A.; Gad, M.M. An Updated Review of Salivary pH Effects on Polymethyl Methacrylate (PMMA)-Based Removable Dental Prostheses. Polymers 2022, 14, 3387. [Google Scholar] [CrossRef]
- Wei, X.; Pan, Y.; Wang, M.; Wang, Y.; Lin, H.; Jiang, L.; Lin, D.; Cheng, H. Comparative analysis of leaching residual monomer and biological effects of four types of conventional and CAD/CAM dental polymers: An in vitro study. Clin. Oral Investig. 2022, 26, 2887–2898. [Google Scholar] [CrossRef]
- Takaichi, A.; Fueki, K.; Murakami, N.; Ueno, T.; Inamochi, Y.; Wada, J.; Arai, Y.; Wakabayashi, N. A systematic review of digital removable partial dentures. Part II: CAD/CAM framework, artificial teeth, and denture base. J. Prosthodont. Res. 2022, 66, 53–67. [Google Scholar] [CrossRef]
- Kostić, M.; Stanojević, J.; Tačić, A.; Gligorijević, N.; Nikolić, L.; Nikolić, V.; Igić, M.; Vasić, M.B. Determination of residual monomer content in dental acrylic polymers and effect after tissues implantation. Biotechnol. Biotechnol. Equip. 2020, 34, 254–263. [Google Scholar] [CrossRef]
- Deb, S. Polymers in dentistry. Proc. Inst. Mech. Eng. H 1998, 212, 453–464. [Google Scholar] [CrossRef] [PubMed]
- Stafford, G.; Brooks, S. The loss of residual monomer from acrylic orthodontic resins. Dent. Mater. 1985, 1, 135–138. [Google Scholar] [CrossRef]
- Krunić, N.; Kostić, M.; Anđelković, M. Acrylic resins- still irreplaceable materials in prosthetic dentistry. Acta Stomatol. Naissi 2007, 23, 747–752. [Google Scholar]
- Davis, C.C.; Squier, C.A.; Lilly, G.E. Irritant Contact Stomatitis: A Review of the Condition. J. Periodontol. 1998, 69, 620–631. [Google Scholar] [CrossRef]
- LeSueur, B.W.; Yiannias, J.A. Contact stomatitis. Derm. Clin. 2003, 21, 105–114. [Google Scholar] [CrossRef]
- Lygre, G.B.; Gjerdet, N.R.; Grønningsaeter, A.G.; Björkman, L. Reporting on adverse reactions to dental materials-intraoral observations at a clinical follow-up. Community Dent. Oral Epidemiol. 2003, 31, 200–206. [Google Scholar] [CrossRef]
- Giunta, J.L.; Grauer, I.; Zablotsky, N. Allergic contact stomatitis caused by acrylic resin. J. Prosthet. Dent. 1979, 42, 188–190. [Google Scholar] [CrossRef]
- Ergun, G.; Mutlu-Sagesen, L.; Karaoglu, T.; Dogan, A. Cytotoxicity of provisional crown and bridge restoration materials: An in vitro study. J. Oral Sci. 2001, 43, 123–128. [Google Scholar] [CrossRef][Green Version]
- Devlin, H.; Watts, D.C. Acrylic ’allergy’? Br. Dent. J. 1984, 20, 272–275. [Google Scholar] [CrossRef]
- Freitas, J.B.; Gomez, R.S.; De Abreu, M.H.N.G.; E Ferreira, E.F. Relationship between the use of full dentures and mucosal alterations among elderly Brazilians. J. Oral Rehabilit. 2008, 35, 370–374. [Google Scholar] [CrossRef] [PubMed]
- Budtz-Jorgensen, E. Oral mucosal lesions associated with the wearing of removable dentures. J. Oral Pathol. Med. 1981, 10, 65–80. [Google Scholar] [CrossRef] [PubMed]
- Marks, J.G., Jr.; Besito, D.V.; DeLeo, V.A.; Fower, J.F.; Franswaz, A.F.; Maibach, H.I.; Mathias, C.G.; Pratt, M.D.; Rietschel, R.L.; Sherertz, E.F.; et al. North American contact dermatitis group patch-test results, 1998 to 2000. Am. J. Contact. Dermat. 2003, 14, 59–62. [Google Scholar] [CrossRef]
- Sipahi, C.; Ozen, J.; Ural, A.U.; Dalkiz, M.; Beydemir, B. The effect of two fibre impregnation methods on the cytotoxicity of a glass and carbon fibre-reinforced acrylic resin denture base material on oral epithelial cells and fibroblasts. J. Oral Rehabilit. 2006, 33, 666–673. [Google Scholar] [CrossRef]
- Hamann, C.P.; DePaola, L.G.; Rodgers, P.A. Occupation-related allergies in dentistry. J. Am. Dent. Assoc. 2005, 136, 500–510. [Google Scholar] [CrossRef] [PubMed]
- Barclay, S.C.; Forsyth, A.; Felix, D.H.; Watson, I.B. Case report-hypersensitivity to denture materials. Br. Dent. J. 1999, 187, 350–352. [Google Scholar] [CrossRef]
- Koutis, D.; Freeman, S. Allergic contact stomatitis caused by acrylic monomer in a denture. Australas. J. Dermatol. 2001, 42, 203–206. [Google Scholar] [CrossRef]
- Koch, P. Occupational contact dermatitis. Recognition and management. Am. J. Clin. Dermatol. 2001, 2, 353–365. [Google Scholar] [CrossRef]
- Alhendi, A.; Khounganian, R.; Almudhi, A.; Ahamad, S.R. Leaching of Different Clear Aligner Systems: An In Vitro Study. Dent. J. 2022, 10, 27. [Google Scholar] [CrossRef]
- Fuji, K. Fatigue properties of acrylic denture base resins. Dent. Mater. J. 1989, 8, 243–259. [Google Scholar] [CrossRef][Green Version]
- Goiato, M.C.; Freitas, E.; dos Santos, D.; de Medeiros, R.; Sonego, M. Acrylic Resin Cytotoxicity for Denture Base--Literature Review. Adv. Clin. Exp. Med. 2015, 24, 679–686. [Google Scholar] [CrossRef] [PubMed]
- Jacobsen, N.; Hensten-Pettersen, A. Occupational health problems and adverse patient reactions in orthodontics. Eur. J. Orthod. 1989, 11, 254–264. [Google Scholar] [CrossRef] [PubMed]
- Vamnes, J.S.; Lygre, G.B.; Gronningsaeter, A.G.; Gjerdet, N.R. Four years of clinical experience with an adverse reaction unit for dental biomaterials. Community Dent. Oral Epidemiol. 2004, 32, 150–157. [Google Scholar] [CrossRef] [PubMed]
- Watacha, J.C. Principles of biocompatibility for dental practitioners. J. Prosthet. Dent. 2001, 86, 203–209. [Google Scholar] [CrossRef]
- Kieć-Świerczyńska, M. Occupational allergic contact dermatitis due to acrylates in Lodz. Contact Dermat. 1996, 34, 419–422. [Google Scholar] [CrossRef]
- Sadoh, D.R.; Sharief, M.K.; Howard, R.S. Occupational exposure to methyl methacrylate monomer induces generalized neuropathy in a dental technician. Br. Dent. J. 1999, 186, 380–381. [Google Scholar] [CrossRef]
- Rubel, D.M.; Watchorn, R.B. Allergic contact dermatitis in dentistry. Australas. J. Dermatol. 2000, 41, 63–71. [Google Scholar] [CrossRef]
- Leggat, P.; Kedjarune, U. Toxicity of methyl methacrylate in dentistry. Int. Dent. J. 2003, 53, 126–131. [Google Scholar] [CrossRef]
- Wallenhammar, L.-M.; Örtengren, U.; Andreasson, H.; Barregård, L.; Björkner, B.; Karlsson, S.; Wrangsjö, K.; Meding, B. Contact allergy and hand eczema in Swedish dentists. Contact Dermat. 2000, 43, 192–199. [Google Scholar] [CrossRef]
- Minić, I.; Pejčić, A.; Kostić, M.; Krunić, N.; Mirković, D.; Igić, M. Prevalence of Oral Lesions in Elderly. W Indian. Med. J. 2016, 65, 375–378. [Google Scholar]
- Uslu, M.; Eltas, A.; Marakoğlu, I.; Dündar, S.; Şahin, K.; Özercan, I.H. Effects of diode laser application on inflammation and mpo in periodontal tissues in a rat model. J. Appl. Oral Sci. 2018, 26, e20170266. [Google Scholar] [CrossRef] [PubMed]
- Kostić, M.; Igić, M.; Jevtovic-Stoimenov, T.; Pejcić, A.; Pesić Stanković, J. Determination of Salivary Myeloperoxidase, Immunoglobulin E and Tumor Necrosis Factor Alpha after Complete Denture Insertion. Med. Princ. Pract. 2019, 28, 347–351. [Google Scholar] [CrossRef] [PubMed]

| Liquid (Monomer) | Powder (Polymer) |
|---|---|
| MMA | PMMA, PEMA, PBuMA |
| Polymerization inhibitor (0.006% hydroquinone or methoxy phenol) | Polymerization initiator (0.2 to 1.5% dibenzoyl peroxide) |
| Polymerization crosslinker (EGDMA, TMPT, 1.4-BDMA, 1.6-HDMA) | Plasticizers (dibutyl-, diethyl- and dicyclohexyl phthalate) |
| Polymerization accelerator (N,N dimethyl-p-toluidine, tertiary amines, sulfuric acid) * | Colours, pigments, and fibres of organic origin that imitate oral tissues and blood vessels |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kostić, M.; Igić, M.; Gligorijević, N.; Nikolić, V.; Stošić, N.; Nikolić, L. The Use of Acrylate Polymers in Dentistry. Polymers 2022, 14, 4511. https://doi.org/10.3390/polym14214511
Kostić M, Igić M, Gligorijević N, Nikolić V, Stošić N, Nikolić L. The Use of Acrylate Polymers in Dentistry. Polymers. 2022; 14(21):4511. https://doi.org/10.3390/polym14214511
Chicago/Turabian StyleKostić, Milena, Marko Igić, Nikola Gligorijević, Vesna Nikolić, Nenad Stošić, and Ljubiša Nikolić. 2022. "The Use of Acrylate Polymers in Dentistry" Polymers 14, no. 21: 4511. https://doi.org/10.3390/polym14214511
APA StyleKostić, M., Igić, M., Gligorijević, N., Nikolić, V., Stošić, N., & Nikolić, L. (2022). The Use of Acrylate Polymers in Dentistry. Polymers, 14(21), 4511. https://doi.org/10.3390/polym14214511







