Advanced Manufacturing in the Fabrication of a Lifelike Brain Glioblastoma Simulator for the Training of Neurosurgeons
Abstract
:1. Introduction
2. Fabrication of Proposed Medical Simulator
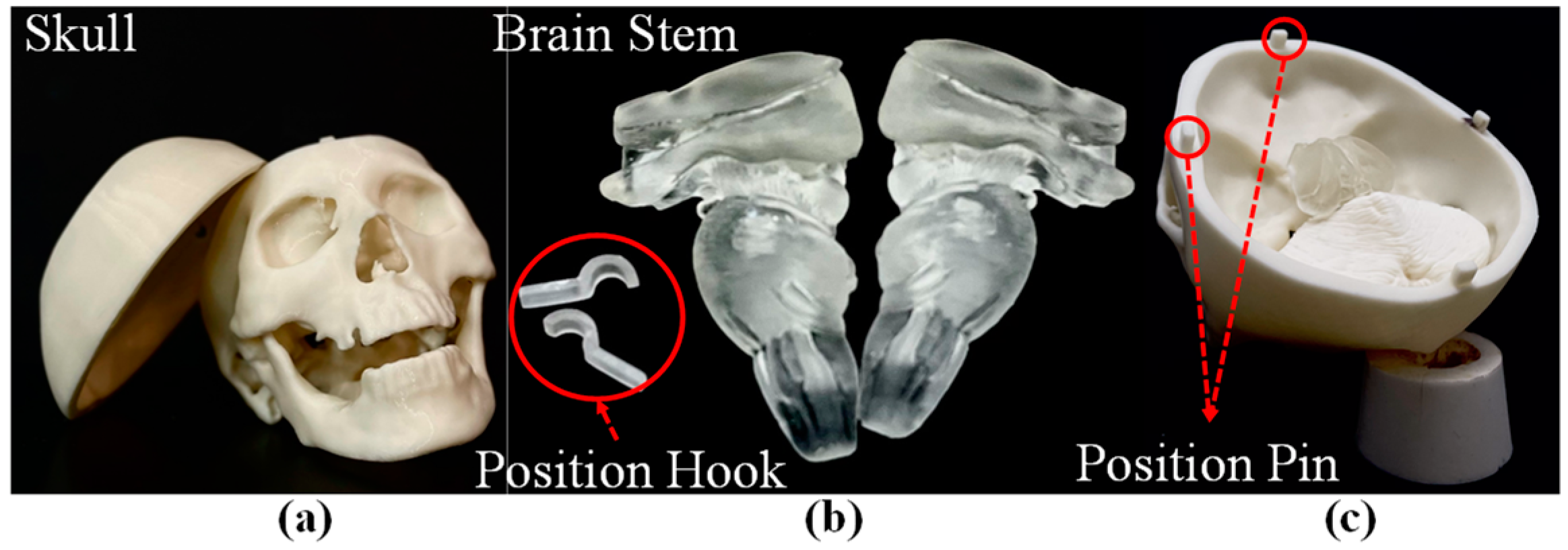
2.1. Manufacturing of Skull and Brain Stem
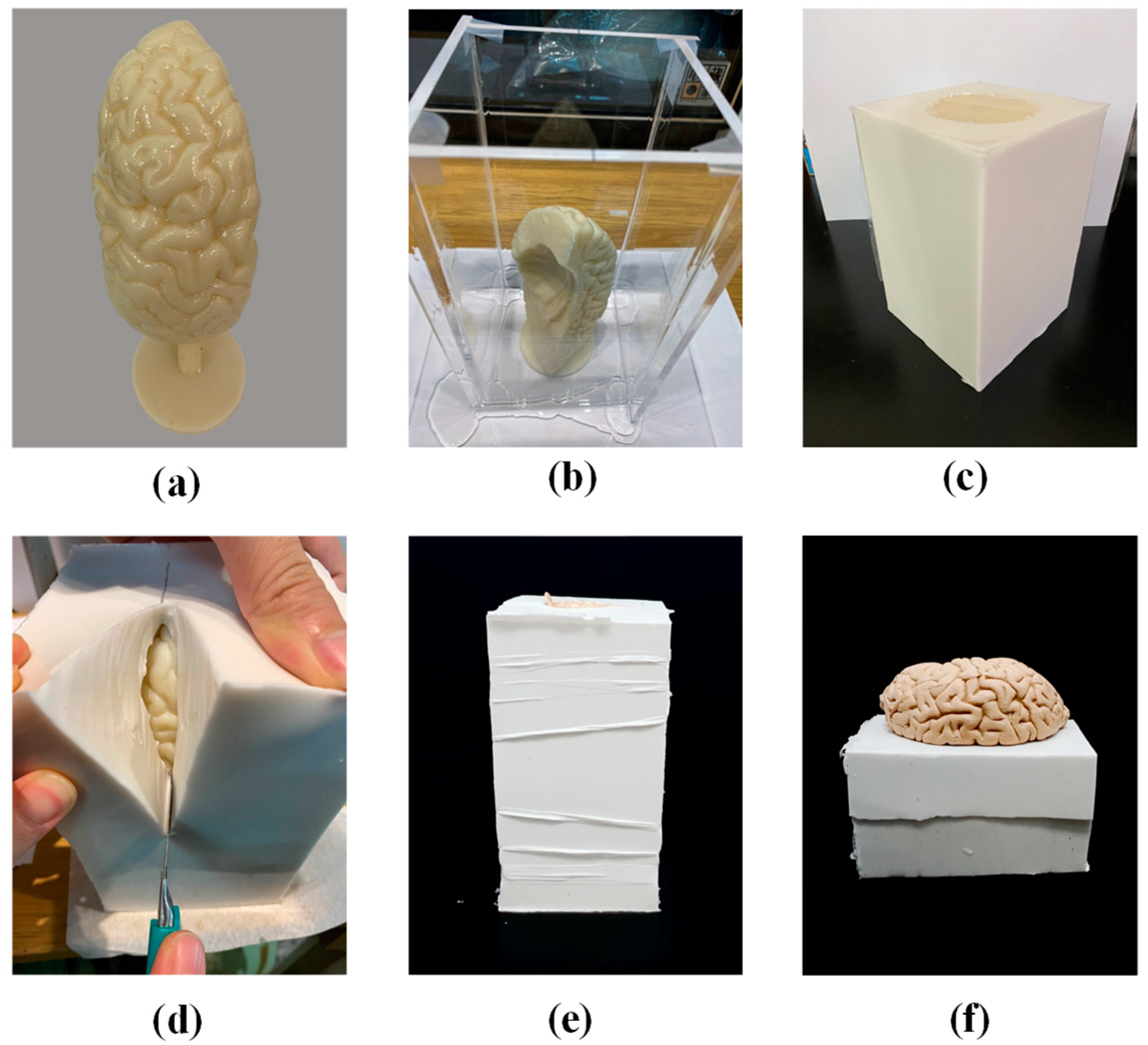
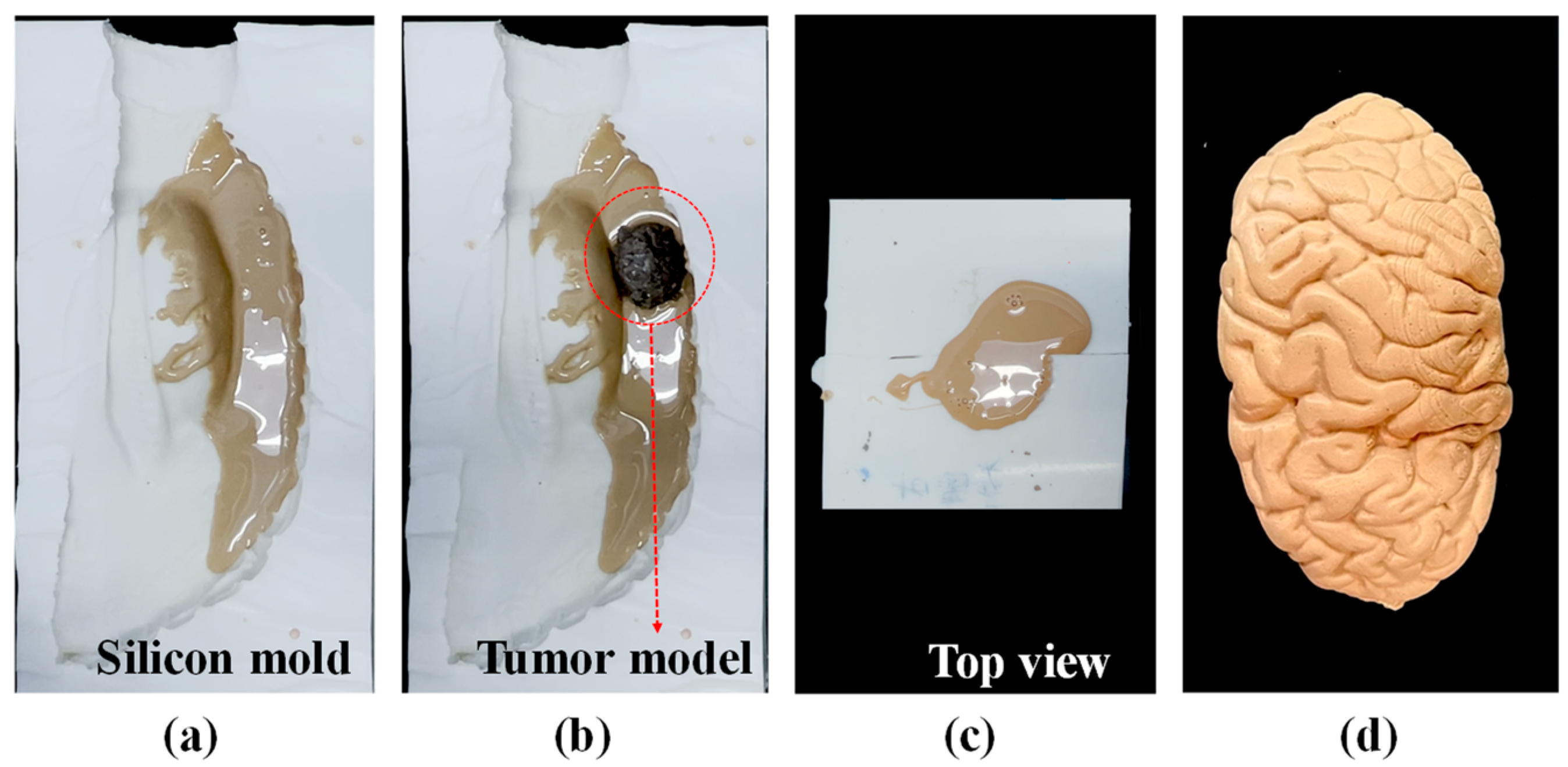
2.2. Fabrication of Brain Lobes and Cerebral Tumor
2.3. Fabrication of Brain with Cerebral Tumor
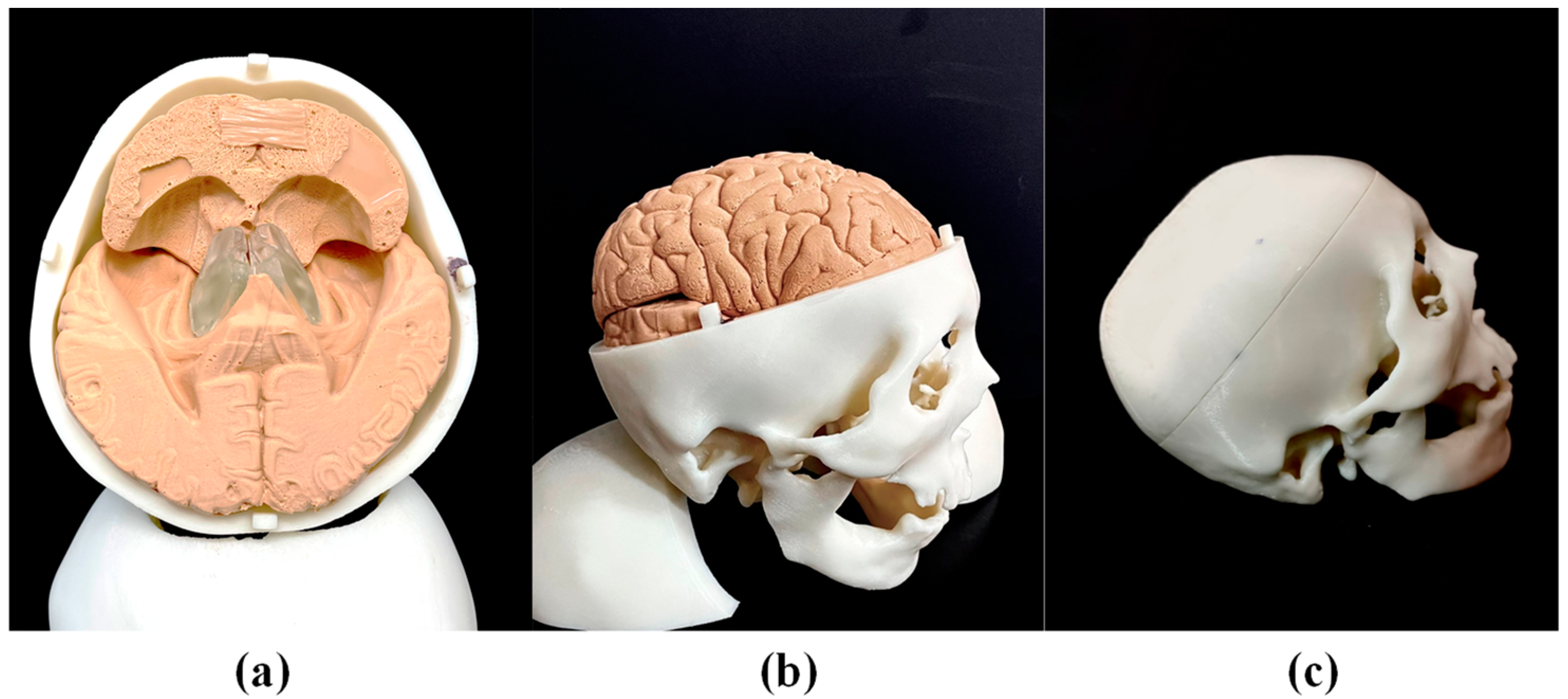
2.4. Assembly of Medical Simulator
3. Material Testing and Analysis
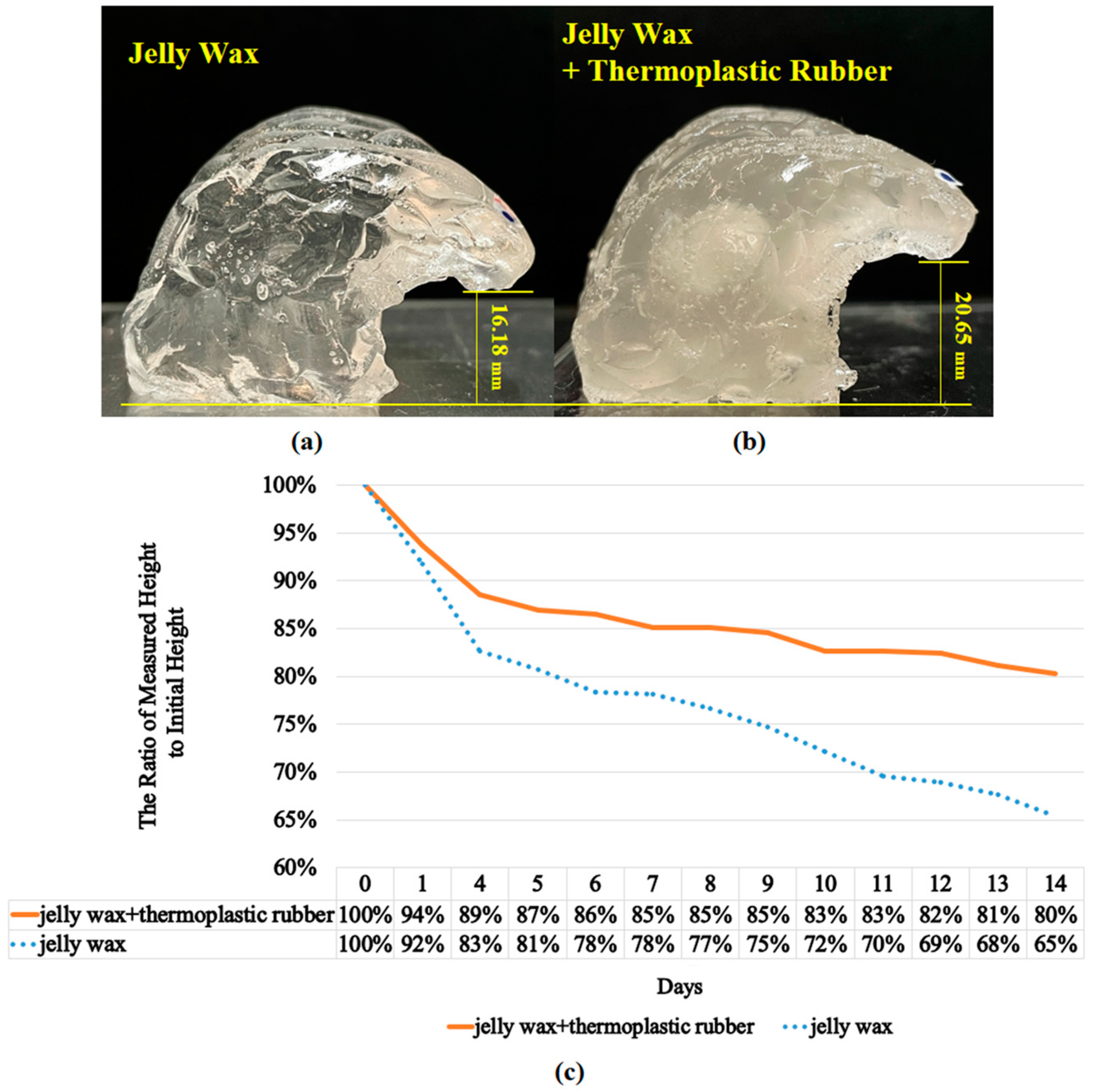
3.1. The Collapse Phenomenon of the Brain Lobe
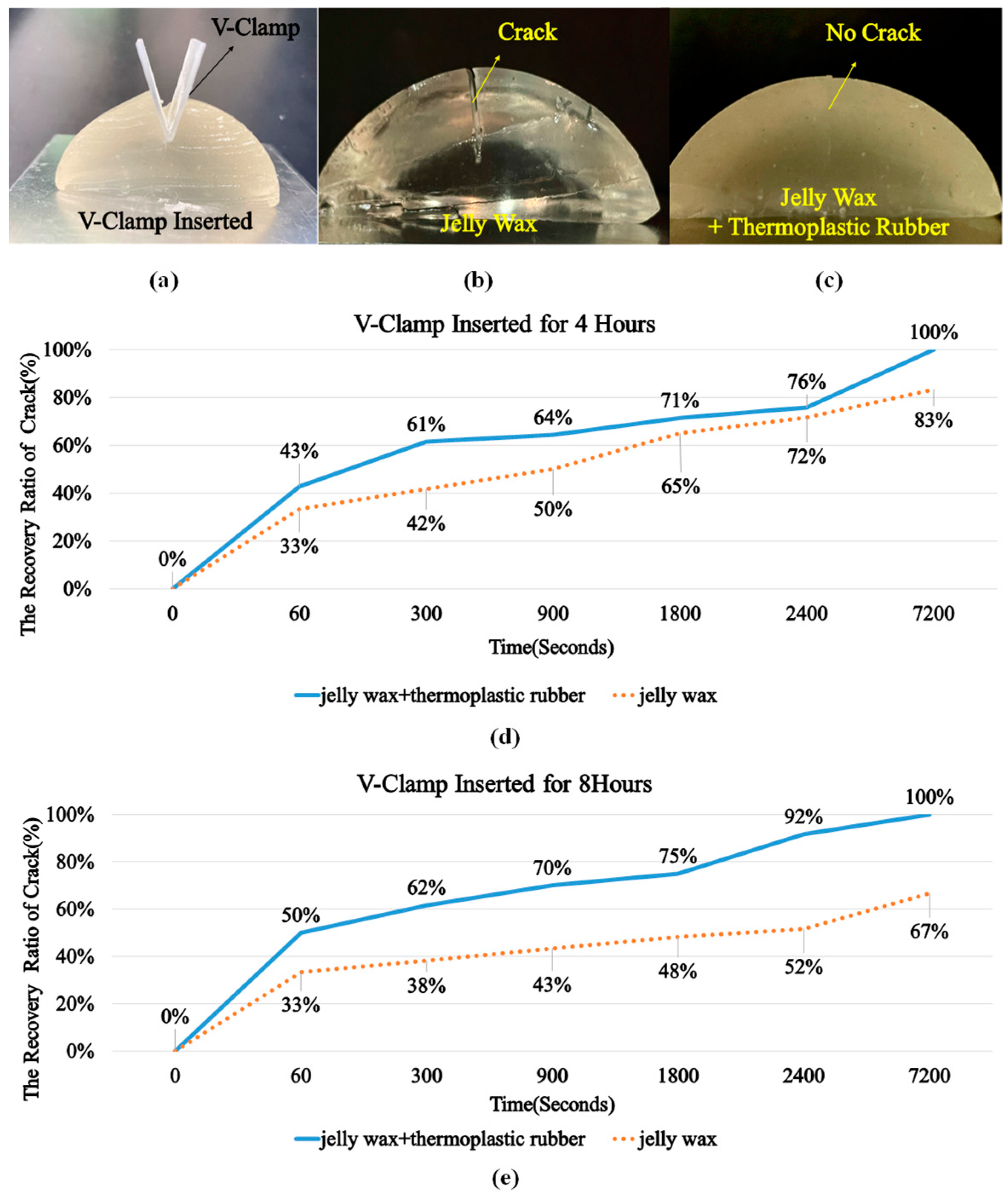
3.2. The Recovery Performance of the Brain Lobe
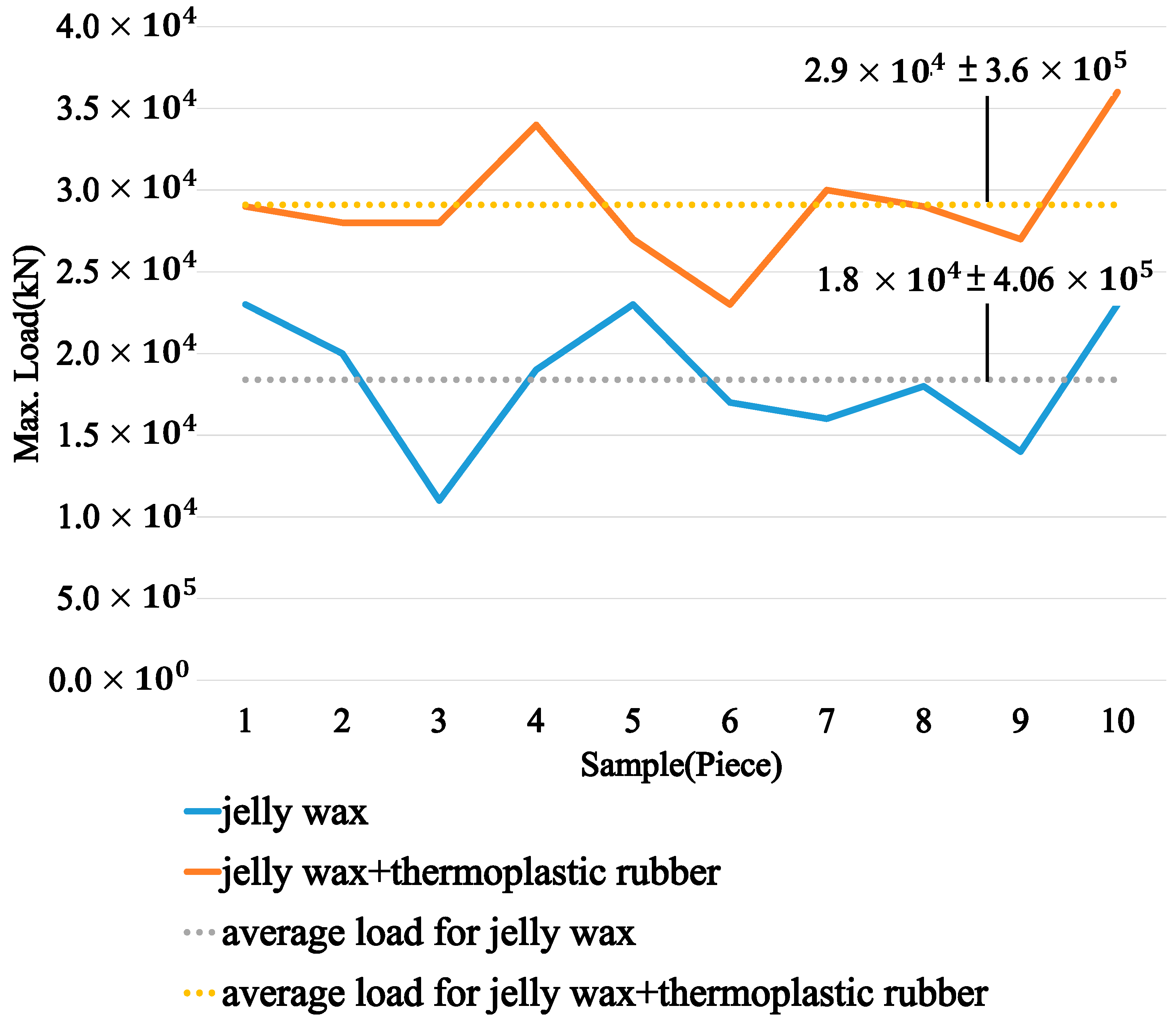
3.3. Tension Test
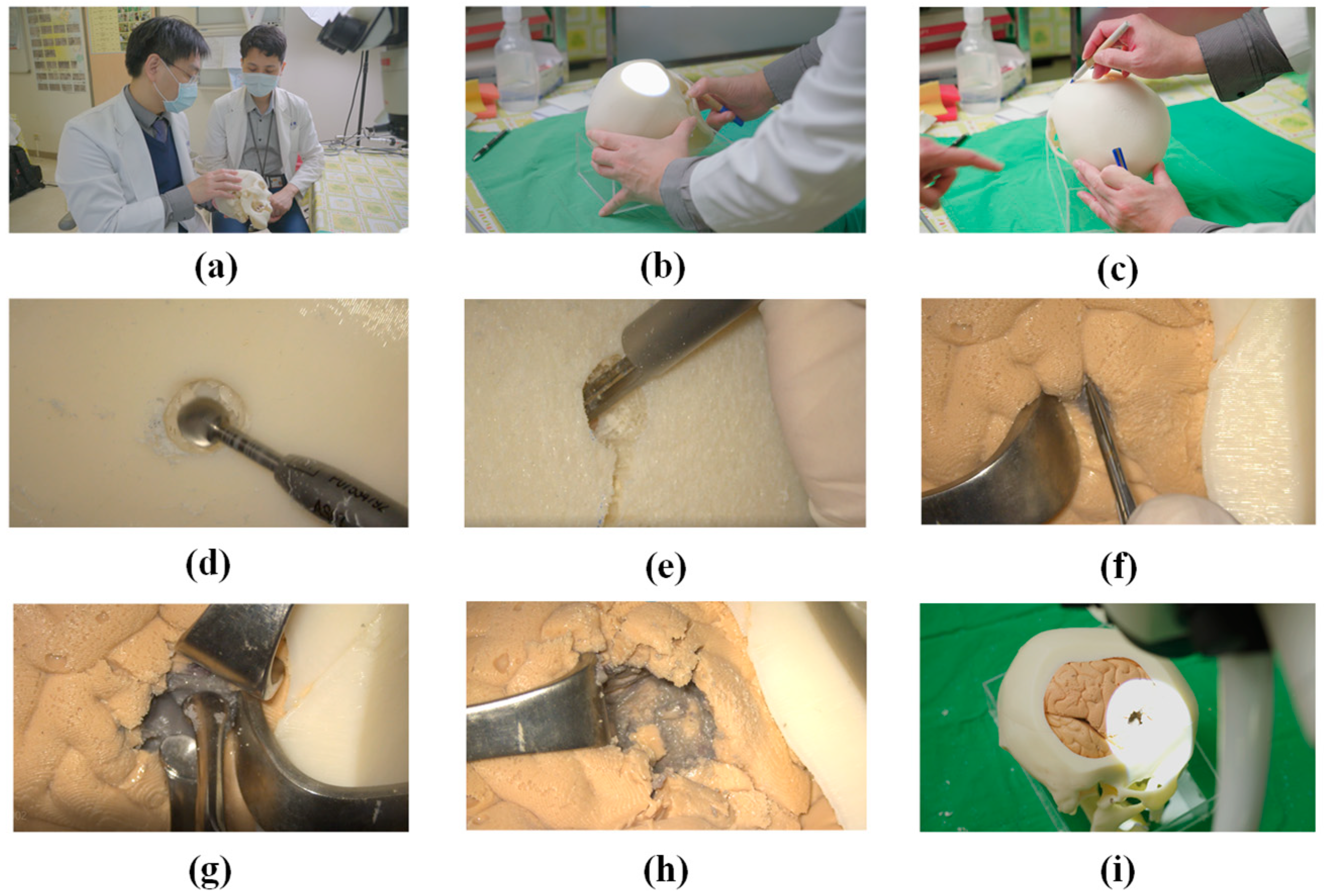
4. Practicing Surgical Techniques
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mashiko, T.; Kaneko, N.; Konno, T.; Otani, K.; Nagayama, R.; Watanabe, E. Training in cerebral aneurysm clipping using self-made 3-dimensional models. J. Surg. Educ. 2017, 74, 681–689. [Google Scholar] [CrossRef] [PubMed]
- Ganju, A.; Aoun, S.G.; Daou, M.R.; El Ahmadieh, T.Y.; Chang, A.; Wang, L.; Batjer, H.H.; Bendok, B.R. The role of simulation in neurosurgical education: A survey of 99 United States neurosurgery program directors. World Neurosurg. 2013, 80, e1–e8. [Google Scholar] [CrossRef] [PubMed]
- El Ahmadieh, T.Y.; Aoun, S.G.; El Tecle, N.E.; Nanney, A.D., 3rd; Daou, M.R.; Harrop, J.; Batjer, H.H.; Bendok, B.R. A didactic and hands-on module enhances resident microsurgical knowledge and technical skill. Neurosurgery 2013, 73, S51–S56. [Google Scholar] [CrossRef] [PubMed]
- Gaba, D.M. The future vision of simulation in healthcare. Simul. Healthc. 2007, 2, 126–135. [Google Scholar] [CrossRef] [Green Version]
- Passiment, M.; Sacks, H.; Huang, G. Medical Simulation in Medical Education: Result of an AAMC Survey; September 2011; Association of American Medical Colleges: Washington, DC, USA, 2011. [Google Scholar]
- Bernardo, A. Virtual reality and simulation in neurosurgical training. World Neurosurg. 2017, 106, 1015–1029. [Google Scholar] [CrossRef]
- Choudhury, N.; Gélinas-Phaneuf, N.; Delorme, S.; Del Maestro, R. Fundamentals of neurosurgery: Virtual reality tasks for training and evaluation of technical skills. World Neurosurg. 2013, 80, e9–e19. [Google Scholar] [CrossRef] [Green Version]
- Davis, G.R.; Illig, K.A.; Yang, G.; Nguyen, T.-H.; Shames, M.L. An approach to EVAR simulation using patient specific modeling. Ann. Vasc. Surg. 2014, 28, 1769–1774. [Google Scholar] [CrossRef]
- Delp, S.L.; Loan, J.P.; Hoy, M.G.; Zajac, F.E.; Topp, E.L.; Rosen, J.M. An interactive graphics-based model of the lower extremity to study orthopaedic surgical procedures. IEEE Trans. Biomed. Eng. 1990, 37, 757–767. [Google Scholar] [CrossRef]
- Pelargos, P.E.; Nagasawa, D.T.; Lagman, C.; Tenn, S.; Demos, J.V.; Lee, S.J.; Bui, T.T.; Barnette, N.E.; Bhatt, N.S.; Ung, N. Utilizing virtual and augmented reality for educational and clinical enhancements in neurosurgery. J. Clin. Neurosci. 2017, 35, 1–4. [Google Scholar] [CrossRef]
- D’Urso, P.S.; Thompson, R.G.; Atkinson, R.L.; Weidmann, M.J.; Redmond, M.J.; Hall, B.I.; Jeavons, S.J.; Benson, M.D.; Earwaker, W.J.S. Cerebrovascular biomodelling: A technical note. Surg. Neurol. 1999, 52, 490–500. [Google Scholar] [CrossRef]
- Gmeiner, M.; Dirnberger, J.; Fenz, W.; Gollwitzer, M.; Wurm, G.; Trenkler, J.; Gruber, A. Virtual cerebral aneurysm clipping with real-time haptic force feedback in neurosurgical education. World Neurosurg. 2018, 112, e313–e323. [Google Scholar] [CrossRef] [PubMed]
- Kimura, T.; Morita, A.; Nishimura, K.; Aiyama, H.; Itoh, H.; Fukaya, S.; Sora, S.; Ochiai, C. Simulation of and training for cerebral aneurysm clipping with 3-dimensional models. Neurosurgery 2009, 65, 719–726. [Google Scholar] [CrossRef] [PubMed]
- Mashiko, T.; Otani, K.; Kawano, R.; Konno, T.; Kaneko, N.; Ito, Y.; Watanabe, E. Development of three-dimensional hollow elastic model for cerebral aneurysm clipping simulation enabling rapid and low cost prototyping. World Neurosurg. 2015, 83, 351–361. [Google Scholar] [CrossRef] [PubMed]
- Ripley, B.; Kelil, T.; Cheezum, M.K.; Goncalves, A.; Di Carli, M.F.; Rybicki, F.J.; Steigner, M.; Mitsouras, D.; Blankstein, R. 3D printing based on cardiac CT assists anatomic visualization prior to transcatheter aortic valve replacement. J. Cardiovasc. Comput. Tomogr. 2016, 10, 28–36. [Google Scholar] [CrossRef] [Green Version]
- Torres, I.; De Luccia, N. A simulator for training in endovascular aneurysm repair: The use of three dimensional printers. Eur. J. Vasc. Endovasc. Surg. 2017, 54, 247–253. [Google Scholar] [CrossRef] [Green Version]
- Wurm, G.; Lehner, M.; Tomancok, B.; Kleiser, R.; Nussbaumer, K. Cerebrovascular biomodeling for aneurysm surgery: Simulation-based training by means of rapid prototyping technologies. Surg. Innov. 2011, 18, 294–306. [Google Scholar] [CrossRef]
- Wurm, G.; Tomancok, B.; Pogady, P.; Holl, K.; Trenkler, J. Cerebrovascular stereolithographic biomodeling for aneurysm surgery. J. Neurosurg. 2004, 100, 139–145. [Google Scholar] [CrossRef]
- Ploch, C.C.; Mansi, C.S.; Jayamohan, J.; Kuhl, E. Using 3D printing to create personalized brain models for neurosurgical training and preoperative planning. World Neurosurg. 2016, 90, 668–674. [Google Scholar] [CrossRef]
- Lan, Q.; Zhu, Q.; Xu, L.; Xu, T. Application of 3D-printed craniocerebral model in simulated surgery for complex intracranial lesions. World Neurosurg. 2020, 134, e761–e770. [Google Scholar] [CrossRef]
- Chanda, A.; Callaway, C.; Clifton, C.; Unnikrishnan, V. Biofidelic human brain tissue surrogates. Mech. Adv. Mater. Struct. 2018, 25, 1335–1341. [Google Scholar] [CrossRef] [Green Version]
- Mussi, E.; Mussa, F.; Santarelli, C.; Scagnet, M.; Uccheddu, F.; Furferi, R.; Volpe, Y.; Genitori, L. Current practice in preoperative virtual and physical simulation in neurosurgery. Bioengineering 2020, 7, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coelho, G.; Chaves, T.M.F.; Goes, A.F.; Del Massa, E.C.; Moraes, O.; Yoshida, M. Multimaterial 3D printing preoperative planning for frontoethmoidal meningoencephalocele surgery. Child’s Nerv. Syst. 2018, 34, 749–756. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, P.-C.; Yang, Y.-W.; Lin, J.-C.; Liu, W.-H. Advanced Manufacturing in the Fabrication of a Lifelike Brain Glioblastoma Simulator for the Training of Neurosurgeons. Polymers 2022, 14, 1072. https://doi.org/10.3390/polym14061072
Chen P-C, Yang Y-W, Lin J-C, Liu W-H. Advanced Manufacturing in the Fabrication of a Lifelike Brain Glioblastoma Simulator for the Training of Neurosurgeons. Polymers. 2022; 14(6):1072. https://doi.org/10.3390/polym14061072
Chicago/Turabian StyleChen, Pin-Chuan, Yu-Wen Yang, Jang-Chun Lin, and Wei-Hsiu Liu. 2022. "Advanced Manufacturing in the Fabrication of a Lifelike Brain Glioblastoma Simulator for the Training of Neurosurgeons" Polymers 14, no. 6: 1072. https://doi.org/10.3390/polym14061072





